Document 14280291
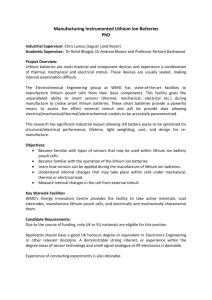
advertisement

0963-6897/09 $90.00 + .00 DOI: 10.3727/096368909X471251 E-ISSN 1555-3892 www.cognizantcommunication.com Cell Transplantation, Vol. 18, pp. 1–100, 2009 Printed in the USA. All rights reserved. Copyright 2009 Cognizant Comm. Corp. Review of Lithium Effects on Brain and Blood Wise Young W. M. Keck Center for Collaborative Neuroscience, Rutgers, State University of New Jersey, Piscataway, NJ, USA Clinicians have long used lithium to treat manic depression. They have also observed that lithium causes granulocytosis and lymphopenia while it enhances immunological activities of monocytes and lymphocytes. In fact, clinicians have long used lithium to treat granulocytopenia resulting from radiation and chemotherapy, to boost immunoglobulins after vaccination, and to enhance natural killer activity. Recent studies revealed a mechanism that ties together these disparate effects of lithium. Lithium acts through multiple pathways to inhibit glycogen synthetase kinase-3β (GSK3β). This enzyme phosphorylates and inhibits nuclear factors that turn on cell growth and protection programs, including the nuclear factor of activated T cells (NFAT) and WNT/β-catenin. In animals, lithium upregulates neurotrophins, including brain-derived neurotrophic factor (BDNF), nerve growth factor, neurotrophin-3 (NT3), as well as receptors to these growth factors in brain. Lithium also stimulates proliferation of stem cells, including bone marrow and neural stem cells in the subventricular zone, striatum, and forebrain. The stimulation of endogenous neural stem cells may explain why lithium increases brain cell density and volume in patients with bipolar disorders. Lithium also increases brain concentrations of the neuronal markers n-acetyl-aspartate and myoinositol. Lithium also remarkably protects neurons against glutamate, seizures, and apoptosis due to a wide variety of neurotoxins. The effective dose range for lithium is 0.6–1.0 mM in serum and >1.5 mM may be toxic. Serum lithium levels of 1.5–2.0 mM may have mild and reversible toxic effects on kidney, liver, heart, and glands. Serum levels of >2 mM may be associated with neurological symptoms, including cerebellar dysfunction. Prolonged lithium intoxication >2 mM can cause permanent brain damage. Lithium has low mutagenic and carcinogenic risk. Lithium is still the most effective therapy for depression. It “cures” a third of the patients with manic depression, improves the lives of about a third, and is ineffective in about a third. Recent studies suggest that some anticonvulsants (i.e., valproate, carbamapazine, and lamotrigene) may be useful in patients that do not respond to lithium. Lithium has been reported to be beneficial in animal models of brain injury, stroke, Alzheimer’s, Huntington’s, and Parkinson’s diseasees, amyotrophic lateral sclerosis (ALS), spinal cord injury, and other conditions. Clinical trials assessing the effects of lithium are under way. A recent clinical trial suggests that lithium stops the progression of ALS. Key words: Lithium; Mechanisms of effects; Mood disorders; Brain effects; Blood effects INTRODUCTION depression as well as prevention of recurrent mania and depression (66). Thus, lithium is recommended for the treatment of both bipolar and unipolar depressive disorders (19). Lithium was one of the first drugs to be approved by U.S. FDA in the early 1970s. Lithium has many effects on brain and blood besides suppressing mania and depression. For many years, the mechanisms of these effects of lithium were not known. Lithium is one of the lightest elements in the periodic table, an alkali metal that is in the same family as sodium and potassium. Why would lithium have any effect on manic depression? However, in the past two decades, several very interesting clues emerged. Many clinicians have noted that patients treated with lithium often had increased white blood cell counts (granulocytosis) and Lithium has been used for over 100 years to treat manic depression (313). In 2001, Burgess, et al. (37) reviewed the Cochrane Collaboration Depression, Anxiety and Neurosis Controlled Trials Register and Cochrane Controlled Clinical Trials for evidence of lithium’s effect on mood disorders. Although the study indicated considerable heterogeneity of results, lithium had consistent and significant beneficial effects on bipolar disorder in all the trials. In unipolar disorder, the direction of effect was in favor of lithium but the effect did not reach statistical significance. Strikingly, no study reported negative effects of lithium. It is the only treatment that has shown efficacy for treatment of acute mania and acute Online prepub date: May 13. 2009. Address correspondence to Wise Young, Ph.D., M.D., W. M. Keck Center for Collaborative Neuroscience, Rutgers, State University of New Jersey, 604 Allison Road, D-251, Piscataway, NJ 08854, USA. E-mail: wisey@mac.com 1 2 reduced blood lymphocyte counts (lymphopenia). Veterinarians began treating animals with lithium after chemotherapy and radiation therapy reduced white blood cell counts. Lithium restored white blood cells and immune function faster. These side effects of lithium led to a better understanding of its mechanisms of action. Scientists began applying lithium to bone marrow stem cells to see why it stimulated greater white blood cell production. These studies revealed that lithium affects phosphorylated inositides, a major cellular messenger system. Further studies showed that lithium stimulates and inhibits several phosphokinases and phosphatases, that all seemed to converge to inhibit a crucial enzyme called glycogen synthetase kinase 3-β (GSK3β). This enzyme ostensibly phosphorylates and inhibits an enzyme called glycogen synthetase, which converts glucose to glycogen. But, more importantly, GSK3β phosphorylates several nuclear factors, including the nuclear factor of activated T cells (NFAT) and WNT/β-catenin. It became clear that GSK3β is the key controller of many cellular programs that control growth, protection, and differentiation of stem cells. This will be the subject of this review. LITHIUM-INDUCED GRANULOCYTOSIS Lithium causes leukocytosis (14,110,276,304,325). At high doses of 50 mg/kg, lithium significantly increases total leukocyte count and neutrophil count, reduces lymphocyte count, and increases erythrocyte count and hematocrit in rats (147). In 1980, Hammond and Dale (113) used lithium to treat canine cyclic hematopoiesis. It eliminated both the recurrent neutropenia and normalized other blood cell counts. In the same year, Levitt et al. (174) assessed the effects of lithium on murine hematopoietic stem cells. They found that adding 1 mM of lithium to cultures of the cells increased murine granulocyte production by 232% of control values (p < 0.001), granulocyte-monocyte progenitor cells (colonyforming units) by 125%, and megakaryocytes by 246%. Prolonged exposure of bone marrow cultures to lithium (3–12 weeks) was associated with a dose-dependent progressive depletion of stem cells and their progeny. They proposed that lithium directly stimulates pluripotent bone marrow stem cells and that prolonged proliferative stress may be associated with diminished replicative potential and depletion of stem cells. Gallicchio et al. (91) showed that lithium increased both pluripotent and committed stem cell colonies, and increases differentiation towards granulocytosis. Finally, lithium increases radiation resistance of mice (312). In healthy human volunteers, lithium did not seem to affect lymphocyte and granulocyte functions but did counteract theophylline-induced inhibition of cellular functions (27). Boggs and Joyce (31) exposed people YOUNG with normal hematopoietic systems to lithium. Blood platelets tended to increase and there was a true neutrophilia, reflected in an increase in mature neutrophils in all body compartments. Lithium did not seem to affect neutrophil function itself. In some mammals, lithium increases certain classes of hematopoietic stem cells, particularly cells producing neutrophils and macrophages. Lithium increases colony-stimulating factors. At 2 mM, lithium enhances megakaryocytopoiesis in marrow culture through accessory marrow cells in vitro (45). Lithium has been used clinically to treat granulocytopenia (112,291), chemotherapy-induced neutropenia (244, 310), aplastic anemia (279), radiation-induced neutropenia (129), childhood neutropenia (57), autoimmune neutropenia (78), agranulocytosis associated with hyperthyroidism (56), hepatitis-associated agranulocytosis (136), and clozapine-induced neutropenia (32,72,109,288). In most of these cases, lithium had beneficial effects, although it paradoxically increased neutropenia duration during cyclic neutropenia (132) by amplifying granulocytic oscillations (322), suggesting that lithium may have complex effects on cyclic phenomena involving suppressor activities and interactions between different populations of white blood cells (319). In some hematopoietic disorders, lithium can be dramatically effective. For example, Robinson et al. (247) found that lithium enhances peripheral blood neutrophil, serum CSA levels, and other symptoms in Felty’s syndrome (284), an autoimmune condition with rheumatoid arthritis, leukopenia, and splenomegaly (248). In some cases, lithium alone cannot reverse this condition and must be given alongside high-dose corticosteroids (284). However, in many cases, a single course of lithium carbonate restored neutrophil counts to normal (227). Lithium did not affect all granulocytes to the same extent. De Vries et al. (60) applied low lithium concentrations (0.1 mM) to myeloid colonies from normal patients and those with overt acute myelomonocytic leukemia (AMML). In myeloid colonies from normal patients, lithium increased the sizes of colonies by 1.5–2.0 times and cell cycle analysis showed a significant increase in percentage of cells in S, G2, and M phases. However, the lithium had no effect on cell colonies grown from patients with AMML. Lithium also did not reverse neutropenia associated with glycogen storage disease (158), drug-induced neutropenia (213,335), neutropenia associated with chemotherapy of acute myelogenous leukemia (260,290), or large granular lymphocyte proliferation (270). In 1984, Yung (340) reviewed the clinical trials that had been carried out to assess lithium effects on 15 medical and psychiatric conditions, including hyperthyroidism, thyroid cancer, inappropriate secretion of antidiuretic hormone, premenstrual tension syndrome, anorexia nervosa, Felty’s syndrome, chemotherapy-induced neu- REVIEW OF LITHIUM EFFECTS ON BRAIN AND BLOOD tropenia, aplastic anemia, seborrheic dermatitis, eczematoid dermatitis, cyclic vomiting, diabetes mellitus, and asthma. Most of the trials yielded negative results except for four conditions: premenstrual tension syndrome, anorexia nervosa, Felty’s syndrome, and chemotherapyinduced neutropenia. The first two may well be related to lithium’s antidepressive effects. The latter two were completely unanticipated and surprising effects of lithium. So, what once was considered a side effect of lithium treatment for bipolar disorders has become an important therapeutic indication for lithium. Lithium turns out to be a potent stimulant of bone marrow stem cells. For example, it is used after chemotherapy, radiation therapy, toxin-induced neutropenia, and even autoimmune neutropenia. Remarkably, the dose of lithium required for this stimulation is relatively low and has few side effects. At these doses, it appears to be safe and does not have dangerous effects on healthy people with normal immune function. Finally, the drug may not be effective for some hematopoietic disorders, such as acute myelogenous leukemia, glycogen storage diseases, drug-induced neutropenia, and granular lymphocytic proliferation. However, it is effective for Felty’s syndrome and chemotherapy-induced neutropenia. LITHIUM-INDUCED LYMPHOPENIA Lithium inhibits T-cell production. In 1980, Fernandez and MacSween (76) reported that therapeutic doses of lithium reduced blood lymphocyte counts in patients. They grew T-cell colonies from normal individuals and people taking lithium, finding that the latter had fewer T-cell colonies than the former. They proposed that lithium shifts maturation from lymphocytes to granulocytes (76). Verma et al. (318) reported that lithium carbonate abrogated human leukocyte interferon-induced granulopoeitic differentiation and this effect is not mediated by T lymphocytes. In psychiatric patients with manic depression (336), lithium did not change marrow granulocyte reserve and may even reduce the percentage of marginal granulocyte pool, without changing serum lysozymal activity, total leukocyte mobilization, and blood granulocyte clearance. Depression itself does not seem affect T-cell immune mechanisms. For example, Albrect et al. (7) studied lymphocyte blastogenesis induced by lectins (PHA, ConA, and PWM) in 27 drug-free patients with unipolar (n = 31) or bipolar (n = 5) depression and 13 normal controls. The groups did not differ significantly from each other. Lithium directly suppresses T-cell production. PerezCruet and Dancey (230) found that lithium causes thymus involution with a significant reduction of gland size in both normal and adrenalectomized mice. Although lithium also increased corticosterone levels in normal 3 mice, the fact that adrenalectomized mice showed thymus involution suggests a direct effect of lithium on the thymus. Wahlin et al. (323) studied T-lymphocyte subsets in 37 lithium-treated patients, 5 prelithium patients, and 12 healthy volunteers. Lithium treatment reduced the absolute and relative number of OKT4 cells. The relative number of OKT8 cells increased. OKT4/OKT8 ratios declined with increasing duration of lithium therapy. Although lithium suppresses T-cell production, it enhances lymphocytic activity. For example, Ridgway et al. (245) showed that lithium enhanced lymphocyte response to phytohemagglutinin (101) in leukemia patients. Lithium prevented inhibitory effects of spontaneous suppressor activity of peripheral blood monocytes on plaque-forming cells (62,63). It counteracts histamine suppression of human T-cell mitogenesis (111). Irvine et al. (131) showed that lymphocytes from lithium-treated patients do not inhibit granulocyte stem cells (CFU-C) growth. Lithium increased mitogen-induced lymphocyte proliferation and inhibited T-suppressor cell activity (99). Lithium enhanced PHA (117), concavalin A (116), and lectin (177) stimulation of lymphoid cells. Lithium increased lymphocyte responses to mitogens (75), reduced bactericidal activity of granulocytes (84), and significantly boosts immune responses of lymphocytes to antigens (273). Lithium enhanced immune function of human mononuclear cells, including thymidine uptake by mitogenstimulated human mononuclear cells (274). Lithium chloride induced partial responsiveness to LPS in nonresponder B cells (134). Lithium also stopped interferonmediated granulopoietic differentiation arrest (318). Lithium boosts immunoglobulin synthesis by human lymphocytes (326), both IgG and IgM (331). Lithium blocked prostaglandin-mediated inhibition of interleukin-2 and proliferation of cultured lymphocytes (182). Lithium prevents activation of suppressor T cells that inhibit granulocyte-macrophage colony-forming cells (317). Lithium also increases production of colony stimulating factor from mitogen-stimulated lymphocytes in vitro (92). Lithium increases natural killer activity of mouse lymphocyte (87). Finally, Hart (115) showed that that lithium potentiates antigen-dependent stimulation of lymphocytes only under suboptimal conditions. Lithium is sometimes used to modulate immune function. For example, it has been used as an oral adjuvant for viral vaccines in humans (135). Interestingly, lithium has also been used to treat autoimmune diseases such a psoriasis (204), although one group reported that lithium exacerbated psoriasis (258). Lithium is presently used topically in dermatology because percutaneous penetration is low and lithium succinate plus zinc sulfate or lithium gluconate may be effective for seborrheic dermatitis (287). Levine and Saltzman (171) reported that 4 YOUNG lithium treatment inhibits experimental allergic encephalomyelitis. Calabrese et al. (40) reported that chronic lithium treatment significantly increased thyroid microsomal antibodies production in five patients and may exacerbate underlying indolent autoimmune thyroiditis, possibly by causing shifts in T-lymphocyte subpopulations. Hassman et al. (121) studied lithium effects on an experimental autoimmune thyroid disease model in rats. Lithium did not change anti-TG antibody levels if they had not been immunized. However, lithium given before and during the immunization markedly increased splenic Tcell blastogenic response. However, lithium reduced proliferation of splenic lymphocytes. They concluded that lithium exerted both positive and negative effects on the immune system of rats immunized with thyroglobulin in adjuvant but did not induce autoantibody production in normal rats. Wilson et al. (332) concluded that lithium does not cause the autoimmune thyroid problem. In summary, lithium paradoxically reduced lymphocyte production but enhanced their function. Lithium has both negative and positive effects on the immune system. Lithium is used to modulate immune conditions. For example, it is given with vaccines, administered topically to treat autoimmune skin conditions such as psoriasis. Claims that lithium cause autoimmune thyroid disease in rats could not be confirmed. LITHIUM MECHANISMS Multiple mechanisms of lithium have been described (142). Activation of Phosphoinositol-3-Kinase (PI3K) Chronic lithium and sodium valproate therapies reduce myoinositol and increase inositol monophosphates in rat brain (220). PI3K phosphorylates and inhibits glycogen synthetase GSK3β (180,305). Inhibition of PI3K induces neurite retraction (253) while PI3K activation induces neurite growth. PI3K also regulated the gap junction intercellular communication (95). Activation of Akt-1 (Serine Threonine Protein Kinase B) Lithium activates Akt-1 (43,282). Akt-1 in turn inhibits GSK3β (16,148,237). Akt is a critical protein kinase that modulates apoptotic and survival pathways (42). Low-K-Lnduced Phosphatase (LKPase) Lithium inhibits many cytosolic phosphatases (205, 223,225,238,306), including the phosphatase that is induced by low K (342). Lithium protects rat cerebellar granule cells against apoptosis induced by low extracellular K concentrations (202,217). Inositol Monophosphatase (IMPase) Lithium inhibits IMPase (23,215,271,292), which contributes to enzymatic breakdown of inositol phosphates to free inositol, discovered more than 150 years ago (5). Chronic lithium treatment paradoxically increases IMPase expression in the brain (150,224). For many years, investigators thought that phosphoinositol depletion was the mechanism of lithium action. However, recent studies suggest that this is not the mechanism of lithium action (26). IMPase plays an important role in stimulating autophagy (81,82,255,256), which stimulates biogenesis of mitochondria in the central nervous system. Glycogen Synthetase Kinase 3β (GSK3β) Lithium activation of PI3K and Akt-1 inhibits GSK3β. Lithium Inhibition of LKP and IMPase prevents activation of GSK3β. In addition, in relatively high concentrations, lithium directly inhibit of GSK3β (143). Thus, lithium inhibits GSK3β through multiple pathways. GSK3β in turn phosphorylates transcription factors that turn on genes for cell growth, inflammation, neuroprotection, and differentiation [i.e., AP-1 (125), CREB (176), HSF-1 (30,337), NFAT (24,77), Myc (144), wnt/βcatenin (299), CCAAT/enhancer binding protein (108, 233,275), FoxO3a (187), ADD1/SREBP1c (155), NFκB (73,163), and IκBα kinase (300). Other Mechanisms Lithium is a potent inhibitor of guanylate cyclase in intact human lymphocytes (262). Exposing human lymphocytes for 72 h to lithium markedly increased Na/K pump numbers (138) and this can be prevented by adding myoinositol. Lithium interferes with subunit associations of G protein, inhibiting adenylate cyclase (67), and affecting cAMP levels (184,246). Lithium prevents cGMP accumulation in human lymphocytes (263). Jope (143) has proposed that lithium’s mechanism of action in bipolar disease is through three interacting systems. First, lithium modulates neurotransmitters by readjusting excitatory and inhibitory systems, decreasing excitatory glutamatergic activity. Second, it modulates messenger systems that affect cellular cytoskeleton, including GSK3β, cAMP-dependent kinase, and protein kinase C, which contribute to neural plasticity, mood recovery, and stabilization. Third, lithium adjusts signals regulating second messengers, transcription factors, and gene expression. Li et al. (175) has proposed that inhibition of GSK3β is the main mechanism of lithium’s neuroprotective actions. Many actions of lithium seem to converge on GSK3β. As depicted in Figure 1, lithium activates the Akt serinethreonine protein kinase B (Akt-PKB) and phosphoinositol-3-kinase (PI3K). It inhibits low-K-induced phospha- REVIEW OF LITHIUM EFFECTS ON BRAIN AND BLOOD 5 Figure 1. Lithium mechanisms. See text for explanation. tase (LKP) and inositol monophosphatase (IMP). The sum of these activities is inhibition of GSK3β, which in turn phosphorylates nuclear factors, including Wnt/βcatenin, T-cell factor, NFAT, and others. When phosphorylated, the nuclear factors do not enter the nucleus. However, when dephosphorylated by stress, inflammation, and other signals, they enter the nucleus and turn on growth, protective, inflammatory, and differentiation programs. LITHIUM AND NEUROTROPHINS Many investigators have reported that depression reduces brain-derived neurotrophic factor (BDNF) in brain (119,235) and that lithium acts by increasing BDNF in the brain (9,10,94,235). Lithium and valproate selectively activate the promoter IV of brain-derived neurotrophic factor (BDNF) in neurons (338) and elevate BDNF levels in the hippocampus (83). Lithium and pilocarpine-induced status epilepticus is associated with widespread increases of BDNF in rat brains (208). Lithium also increases nerve growth factor (74) in the rat hippocampus (9,10,83,122,208), but neither valproate nor amphetamine changed NGF in the brain. Hellweg et al. (122) treated adult rats with lithium (0.72 ± 0.08 mM serum levels) and found significant increases of NGF in frontal cortex (+23.2%), hippocampus (+72%), amygdala (+74%), and limbic forebrain (+46.7%) compared to untreated controls. However, lithium had no effect on NGF levels in striatum, hypothalamus, or midbrain. Acute treatment for 1 day had no effect on NGF concentrations in frontal cortices. Walz et al. (324) has reported that lithium increased levels in neurotrophin-3 (NT-3) in serum and hippocampus of rats that had amphetamine-induced mania, whether lithium was given before, during, or after amphetamine. Valproate increased NT-3 only when given before amphetamine. They concluded that both lithium and valproate modulate NT-3 expression in the serum and hippocampus. A recent study suggested that people with major depressive or bipolar disorders have significantly lower blood glia-derived neurotrophic factor (GDNF) levels than control subjects (302). Some investigators have reported that lithium increases GDNF in brain regions (9), particularly in rats undergoing pilocarpine seizures (96). However, other investigators report that neither acute nor chronic lithium treatment increase GDNF in rat brain (89). 6 Both acute and long-term lithium treatment increase the high-affinity receptor for BDNF (TrkB) in the anterior cingulate but not in the hippocampus (208,240). Moreover, acute lithium treatment significantly reduced phosphorylation of CREB, a major intracellular target of TrkB, suggesting that lithium increases BDNF release and BDNF receptor activation. However, prolonged lithium did not significantly affect BDNF or CREB activation in the anterior cingulate or hippocampus. Lithium antagonizes NGF-induced reorganization of microfilament in PC12 cells (226), as well as NGFinduced neurite outgrowth and phosphorylation of NGFmodulated microtubule-associated proteins (38,157). The inhibitory effect of lithium on cytoskeletal rearrangement associated with cell spreading and migration is mediated by GSK3-dependent phosphorylation via an ERKdependent mechanism (39). In addition, lithium inhibits NGF-induced neuronal differentiation of rat PC12 cells (321). Exposing PC12 cells to lithium increased NGFinduced melanin-concentrating hormone but reduced tyrosine hydroxylase gene expression (236). Lithium attenuates NGF-induced activation of AP-1 DNA binding activity in PC12 cells (311). Likewise, lithium seems to suppress BDNF-induced changes in cells. In 2005, Elliot et al. (69) reported that BDNF-induced dephosphorylation of tau proteins is mediated by PI3K signaling, which is inhibited by lithium. BDNF had no effect of tau proteins in the presence of wortmannin (a PI3K inhibitor) or lithium, which inhibits both PI3K and GSK3β. Lithium reduces FoxO3a activity, a transcription factor that is widely distributed in brain and suppressed by BDNF (187). In 2004, Tsai (307) suggested that overactivity of BDNF may contribute to bipolar affective disorder rather than suppress the mood swings. The effects of lithium on neurotrophin expression in the brain appear to depend on the state of the brain and the animal model used. For example, Hammonds et al. (114) showed that giving 1 mEq/kg of lithium chloride to normal rats for 14 days did not increase BDNF, Bcl2, or CREB in rat hippocampus. The effects of the drug also appear to differ from brain region to brain region. Also, some of the variability may result from failure of investigators to monitor levels of lithium in animals. For example, giving 1 mEq/kg intraperitoneally daily to rats may not be sufficient to achieve sustained therapeutic serum levels of 1 mM. The therapeutic effects of lithium on patients with depression can be predicted by certain polymorphisms of BDNF (267). For example, in 111 patients with bipolar mood disorders (45 male, 68 female), Rybakowski et al. (251) showed a significant association of certain BDNF polymorphism and serotonin transporter (5HTTLPR) with lithium-induced response to depression. This suggests YOUNG that lithium acts through BDNF and also the serotonin transporter. In summary, many investigators have reported that lithium increases neurotrophin levels in the brain, including BDNF, NGF, and NT-3, as well as their receptors. Clinical bipolar disorder is associated with neurotrophin decreases in brain and blood BDNF levels. Chronic lithium treatment seems to restore BDNF levels in animal models of depression and bipolar patients. However, lithium-induced neurotrophin changes in the brain are not always consistent, are dose dependent, and may depend on the condition of the brain and animal model at the time the lithium is given. Neurotrophins are among hundreds of factors that are reported to be abnormal in bipolar depression and that lithium changes. LITHIUM AND NEUROGENESIS Many investigators have reported that lithium stimulates neurogenesis both in vitro and in vivo. For example, short-term lithium induces neurogenesis in rodent striatal injury sites with concomitant decline of proliferating cells in the subventricular zone (266), suggesting that the cells are neural stem cells. The striatal injury was caused by quinolinic acid infusion. Many of the proliferating cells display neuronal or astroglial phenotypes. The subventricular zone is where neural stem cells are located in adult brain. BrdU labeling in lithiumtreated injured striatum revealed large number of proliferating BrdU leveled cells near the quinolic acid injection sites with concomitant reduction of BrdU-labeled cells in the subventricular zone. Chronic lithium treatment enhances hippocampal neurogenesis in rat dentate gyrus (47,286). The number of BrdU+ cells dramatically increased in hippocampal slices after 28 days of lithium treatment. The number of BrdU+ cells increased dramatically in the granular layer and over 90% of the cells are double labeled with neural marker for neuronal nuclear protein. Acute (12 h) treatment with lithium did not increase the number of cells. However, both acute and chronic lithium treatment increased long-term potentiation in rat dentate gyrus (286), suggesting that lithium not only changes neurons but also their interactions with each other. Lithium also selectively increases neuronal differentiation of hippocampal neural progenitor cells in vitro and in vivo (154). In aged rats, chronic lithium enhances long-term potentiation but not neurogenesis (339). The mechanism of lithium-induced neurogenesis was not initially understood. In 2007, Silva et al. (278) examined endocrine and behavioral effects of chronic mild stress on rats, finding decreased proliferation of hippocampal cells. The stress increased GSK3β and other downstream activity. Lithium blocked these effects of chronic mild stress, suggesting that lithium inhibition of REVIEW OF LITHIUM EFFECTS ON BRAIN AND BLOOD GSK-3β prevents the deleterious effects of stress on behavior and cellular functions. Lithium also reduces stress-induced reduction in vascular endothelium growth factors levels (277). More recent studies indicate that the lithium effect on hippocampal neurogenesis requires Wnt/β-catenin activation due to GSK3β inhibition. In 2008, Wexler et al. (329) reported that lithium stimulates proliferation of adult hippocampal progenitor cells, expanding these cells and inducing them to produce new neurons at therapeutically relevant doses. These effects are independent of inositol monophosphatase but depend on Wnt pathway and inhibition of GSK3β. For example, RNAi inhibition of βcatenin abolishes the proliferative effects of lithium. Lithium (321) promotes survival of GABAergic neurons isolated from cerebellum and cerebral cortex. Valproic acid (164) promotes GABAergic neurogenesis in rat forebrain, exceeding the proliferative effects obtained with neurotrophins such as BDNF and NT-3, and slightly exceeding those obtained with lithium. Lithium also enhances GABAergic inputs to granule cells in the rat hippocampal dentate gyrus (169). Su et al. (295) recently reported that lithium enhances proliferation and neuronal production by neural progenitor cells in vitro and after transplantation into adult spinal cords. After transplantation of neural progenitor cells, treatment with lithium markedly increased the number of labeled neurons produced by the transplanted cells at 2 and 4 weeks. Chronic treatment with lithium reduced microglia and macrophage activation, and increased neurogenesis by the transplanted cells. Lithium may not have the same effects on neural stem cells or precursor cells that are cell lines (118). For example, Misiuta et al. (197) studied the effects of retinoic acid and lithium on proliferation and dopaminergic potential of human NT2 cells. These are human cells obtained from a human teratoma cell line. While lithium increased viability and proliferation of NT2 cells, it did not increase expression of transcription factors essential for induction and maintenance of the dopaminergic neuronal phenotype in these cells. Krawetz et al. (161) reported that Wnt6 induces specification and epithelialization of F9 embryonal carcinoma cells to primitive endoderm and that lithium has a similar effect but the cells dedifferentiated when lithium was removed. According to Anton et al. (11), lithium and Wnt3a influence formation of mesoderm and cardiomyocytes but Wnt4a stimulation does not. Much evidence indicates that GSK3β activity is critical for early preimplantation embryonic development (2). Lithium upregulates Notch, a stem cell gene that prevents differentiation. First, lithium activates PI3K-Akt, which increases Notch responsiveness in CHO, primary T cells, and hippocampal neurons, whether induced by 7 insulin, TCR activation, or BDNF-TrkB activation (191). PI3K-Akt serve as a “gain control” for Notch signal (191). Second, GSK3β phosphorylates and inhibits Notch (71). Because lithium inhibits GSK3β, it disinhibits Notch. In summary, lithium causes proliferation of neural stem cells. These effects are robust and occur both in vitro and in vivo. In the hippocampus, lithium stimulates neural progenitor cells by disinhibiting Wnt/β-catenin. However, the results are mixed when lithium is applied to neural stem cells or precursor cells derived from cell lines. Lithium modulates differentiation of cells by regulating Notch. LITHIUM AND BRAIN GRAY MATTER Magnetic resonance spectroscopy studies indicate that patients with bipolar disorders have low levels of N-acetylaspartate (NAA, a marker of neuronal integrity) in dorsolateral prefrontal cortex (34,35,314). In 2000, Moore et al. (199) reported that a 4-week period of lithium treatment increases NAA in brains of 21 adult subjects (12 bipolar and 9 healthy subjects). In 2003, Silverstone et al. (281) showed that chronic lithium therapy likewise increased cortical NAA concentrations in euthymic bipolar patients. Healthy controls (n = 18) were compared against bipolar patients taking lithium (n = 14) or taking valproate (n = 11). Lithium-treated patients had significantly greater NAA concentrations but patients taking valproate did not show a similar NAA increase. Baslow et al. (17) studied rats with Canavan disease (CD), an early onset genetic leukodystrophy that is caused by inability of oligodendroglia to hydrolyze NAA and therefore is associated with NAA buildup in the brains. Using the rat model of CD, they tested seven different drugs and only lithium significantly reduced whole brain NAA level in the rat. After 5 days of therapy, lithium chloride reduced whole brain NAA level by 13%. This was the first report of any treatment that reduces NAA in this model. In 2004, Sassi et al. (259) measured gray matter volumes of untreated and lithium-treated subjects with bipolar disorder, compared with gray matter volumes in healthy subjects. They measured cingulate cortices of 11 bipolar subjects that were not taking any medication (38 ± 11 years, 5 women), 16 bipolar subjects taking lithium (33 ± 11 years, 7 women), and 39 healthy subjects (37 ± 10 years, 14 women). Untreated bipolar subjects had smaller left anterior cingulate volumes compared to healthy subjects and lithium-treated subjects. People with bipolar disorders have increased gray matter concentrations of glutate + glutamine + gaba (GMGlx), compared to healthy controls. In 2004, Friedman et al. (85) showed that both lithium and valproic treatment lowered GMGlx concentrations in subjects with bipolar 8 disorders but only lithium increased myoinositol levels. Serum lithium levels correlated with the GMGlx levels. In 2004, Brambilla et al. (35) found that lithium did not affect brain NAA, phosphocreatine + creatine, glycerophosphocholine, or myoinositol levels in prefrontal cortex (34) of 12 healthy individuals. In a subsequent study, Brambilla et al. (34) assessed the left dorsolateral prefrontal cortex of 10 patients with bipolar disorder (6 lithium and 4 drug free) and found elevated NAA/PCr + Cr ratios in lithium-treated bipolar patients, suggesting that that NAA/PCr + Cr ratios may be a more sensitive indicator of lithium effect. Children with bipolar disorder may have normal levels of NAA/Cr ratios (90). In 2005, Change et al. (44) assessed 20 children with bipolar disorder (mean age 4.6 years, four female) and compared them to 20 healthy matched children. Subjects with bipolar disorders had reduced amygdalar gray matter volumes whereas patients who were treated with lithium or valproate had greater amygdalar gray matter volumes. Lithium also seems to affect activation in certain brain regions. Silverstone et al. (280) used fMRI to study 10 patients who were depressed (n = 5) or euthymic (n = 5). In regions of interest, such as Broca’s area, the left precentral gyrus, and supplemental motor areas, lithium reduced brain activation in euthymic patients during word generation tests but not so in bipolar patients. Bell et al. (22) found that lithium reduced activation in normal patients as well. Lithium increases gray matter density in people with bipolar disorder. In 2005, Monkul et al. (198) described reduced gray matter in prefrontal cortex and amygdala and white matter hyperintensity in patients with bipolar disorders. In 2007, Bearden et al. (20) studied 28 patients with bipolar disorders (mean age 36.1 ± 10.5 years, 13 females), 70% of whom were treated with lithium, who had significantly greater cortical gray matter density than 28 healthy control subjects (mean age 35.9 ± 8.5 years, 11 females). The greatest differences were observed in cingulate and paralimbic cortices, brain regions critical for attention, motivation, and emotional modulation. Further analyses indicated significantly greater gray matter densities in right anterior cingulate among lithium bipolar-treated patients (n = 20) compared to those not taking lithium (n = 8). Chen et al. (50) did a voxel-based morphometric comparison of 26 patients (19–59 years old, 6 males) with bipolar I disorder with 25 control subjects matched for age, sex, and years of education. Bipolar patients had significantly greater gray matter volume in left parahippocampal gyrus and decreased gray matter volume in left middle temporal gyrus. Most of the patients were taking lithium. These studies suggest that patients with YOUNG bipolar disorders may have greater hippocampal gray matter volume than normal subjects. In summary, magnetic resonance studies of patients taking lithium have revealed several fascinating findings. Earlier studies had reported that untreated patients with bipolar disorders have low levels of NAA, a marker of neuronal integrity in the prefrontal cortex. However, bipolar patients treated with lithium, but not valproate, have greater NAA concentration. This is consistent with animal studies that show that lithium restores NAA levels in animal neurodegeneration model. Lithium-treated patients with bipolar disorders may have more neurons (denser and larger volume of gray matter) than non-lithium-treated patients and possibly even more than normal subjects. LITHIUM AND NEUROPROTECTION Lithium has emerged as a robust neuroprotective agent that prevents apoptosis of neurons through multiple mechanisms (51,52). Long-term treatments with lithium effectively protect primary cultures of neurons from glutamate-induced toxicity. Lithium upregulates antiapoptotic Bcl-2 and downregulates proapoptotic p53 and Bax. It activated many cell survival factors and antagonizes glutamate-induced JNK, p38 kinase, AP-1 binding, and phosphorylated CREB loss. Lithium induces the expression of BDNF/TrkB (120) and stimulates neurogenesis in primary cultures of CNS neurons. Lithium has now shown to be neuroprotective in animal models of stroke, Huntington’s disease, and other neurodegenerative diseases. A long-standing model of status epilepticus in rats is the pilocarpine-lithium model (88). In this model, Wistar rats are given lithium (3 mEq/kg) and pilocarpine (30–60 mg/kg) intraperitoneally. At 15 min after onset of seizures, various drugs such as ketamine and phenobarbital can be given to stop or reduce the seizures. In rats that had high-dose pilocarpine (400 mg/kg)-induced seizures without lithium, severe brain damage is present. In rats given lithium-pilocarpine, neuronal damage can be seen in most brain regions. Use of ketamine (a glutamate receptor blocker) not only reduces the amplitude of the seizures but also prevents the neuronal damage. Chronic lithium treatment robustly protects neurons in the central nervous system by inhibiting NMDAmediated influx (216). Long-term exposure of cultured cerebellar, cerebral cortical, and hippocampal neurons to lithium protected them against glutamate-induced excitotoxicity. The neuroprotection is long lasting, occurs at therapeutically relevant concentrations of lithium with an EC50 of about 1.3 mM, and requires 6–7 days of treatment to achieve near complete protection. The effect is not mediated by downregulation of NMDA receptors REVIEW OF LITHIUM EFFECTS ON BRAIN AND BLOOD nor lithium-mediated blockade of inositol monophosphatase activity. Lithium activates the serine-threonine kinase Akt-1, which is well known to inhibit apoptosis in neurons (43). Cerebellar neurons cultured in the presence of serum showed high levels of phosphorylation and Akt-1 activity. Protracted treatment with PI3K inhibitors, wortmannin, and LY294002 abolished the Akt-1 activity and induced neuronal death that could be prevented by longterm lithium. The lithium treatment suppressed glutamate-induced loss of Akt-1 activity and rapidly increased PI3K activity and Akt-1 phosphorylation with correspondingly increased kinase activity that can be blocked with PI3K inhibitors. Thus, lithium seems to increase kinase activity that protects against apoptosis. Long-term lithium treatment suppresses proapoptotic p53 and Bax expression but increases antiapoptotic Bcl2 expression (49) in cerebellar granule cells. The ratios of Bcl-2/Bax protein increased by fivefold after lithium treatment for 5–7 days. Pretreatment with lithium chloride for 7 days prevented glutamate-induced rise in p53 and Bax expression while maintaining Bcl-2 in an elevated state. In addition, lithium pretreatment blocked glutamate-induced mitochondrial cytochrome c and cleavage of lamin B1. Lamin B1 is the nuclear substrate for caspase-3, a critical triggering enzyme for apoptosis. Chronic lithium treatment also prevented glutamateinduced decrease of CREB by reducing protein phosphate 1 and increasing MEK activities (159). CREB and CRE-responsive genes such as bcl-2 may be responsible for lithium’s reported beneficial effects on neuronal survival. Long-term lithium treatment prevents neurotoxic effects of a variety of toxins applied to primary cultured neurons (170). For example, Tseng et al. (308) found that 3–5-day, but not 3-h, exposure to 1.2 mM lithium protected cerebellar granule neurons against α-bungarotoxin-induced neurotoxicity. Lithium ameliorates HIVgp120-mediated (74) and tau-mediated neurotoxicity. Many investigators have consequently proposed that lithium be used to treat acute brain injuries such as stroke and chronic progressive neurodegenerative diseases. Short-term lithium treatment may also be neuroprotective. Kang et al. (146) found that lithium-treated cortical neurons show a marked increase in intracellular calcium within 2 min. Addition of a selective Ca ionic chelator prevented the antiapoptotic effects of lithium. The mechanism by which lithium intracellular calcium appears to be through activation of PI3K, which acts through the phospholipase C gamma (PLCg) pathway because lithium effect can be abrogated by a selective blocker of PLCg (U-73122) or in cells missing the gene for PLCg. 9 Lithium has different neuroprotective mechanisms from valproate, another antidepressive therapy (200). Both drugs protect cultured cerebellar granule cells from low-K-induced apoptosis. Because MK801, a NMDA receptor blocker, does not prevent the apoptosis, the mechanism is probably not due to NMDA receptor-mediated calcium influx. Insulin protects against this injury but the PI3K blocker LY294002 prevented this neuroprotection. The protection by valproate depends on insulin and LY294002 but lithium does not. Leng et al. (170) demonstrated that lithium and valproic acid are synergistic against glutamate excitotoxicity. While both lithium and valproic acid have been to protect cells against cell damage, lithium prevents ouabain-induced cell damage and LDH release while valproic acid does not (124). LITHIUM TOXICITY Clinical experience with the lithium suggests that its effective dose range is 0.6–1.0 mM serum level (289) while toxic levels occur at 1.2 mM or greater. Symptoms associated with serum levels of 1.2–2.0 mM are usually mild (48) and seldom cause death or persistent neurological deficits. Renal or sweat secretion are the only means by which the body eliminates lithium. In general, 500– 1200 mg of lithium per day will yield serum levels of 0.6–1.0 mM, but, because rates of absorption and urinary secretion varies from person to person, lithium must be monitored in blood about 12 h after the last dose of lithium (8). Sex differences are minor (102). Elderly patients have lower clearance (265). Lithium can be accurately measured by flame emission or atomic absorption (55). Acute lithium toxicity can be observed when serum levels exceed 2 mM. In cattle, doses of 250, 500, and 700 mg/kg resulted in serum levels of 19, 40, and 54 ppm (or mg/L) (140). Because 1 mM is 6.941 mg/L, these serum levels are about 2.7, 5.8, and 7.8 mM, respectively. A dose of 250 mg/kg with 2.5 mM serum levels produced only transient signs of toxicity, including salivation, depression, anorexia, hypodipsia, anuria, and diarrhea. Doses of 500–700 mg/kg produced severe depression, ataxia, and death. Autopsies revealed doserelated gastroenteritis, slight interstitial nephritis, and hepatic cirrhosis. Tissue lithium concentrations reached 12 mM in striated muscle, 11 mM in heart, 9.5 mM in kidney, and 7.4 mM in brain of the cattle that died. Lithium does not appear to be mutagenic (221). Banduhn et al. (15) analyzed peripheral blood lymphocytes of 77 patients under lithium therapy and found no elevation in frequency of chromosomal aberrations. It is not mutagenic in the Ames test (bacteria), Chinese hamster ovary cells, or rat primary hepatocytes (283,328). Lithium readily crosses the placental barrier and can 10 have teratogenic effects on the developing fetus. One case report of a 17-year-old bipolar female had 2.6 mM serum levels several hours before birth of her infant. The infant blood levels were 2.1 mM at birth and 1.4 mM 3 days later, suggesting a lithium half-life of greater than 24 h. During the 4 days, the infant was lethargic and exhibited poor suck–swallow coordination and required supplemental enteral feeding. However, by 7 days, the infant was alert and tolerated oral feeding. Mouse studies indicate that lithium treatment decreased brain and spleen weights and induced hepatic neonatal alcohol dehydrogenase (193,194). In general, lithium should be carefully monitored in pregnancy to avoid overdose and should be discontinued 24 h before delivery. There was one report of increased congenital heart disease in newborn infants associated with maternal lithium intake during early pregnancy (12). Lithium does not appear to be carcinogenic. Gould et al. (106) investigated carcinogenic risk by giving lithium to a mouse that has adenomatous polyposis coli (APC). Treating APC mice for 60 days did not produce a significant increase in the number of tumors and only modestly increased the size of the tumors. They suggested that lithium and other GSK3β inhibitors pose a low risk for development cancers of the Wnt pathway. In fact, one study suggests that lithium may suppresses cell proliferation by interrupting E2F–DNA interaction and subsequently reduces S-phase gene expression in prostate cancer (297). At therapeutic levels of 1 mM or less, lithium does not have significant myocardial effects. In 1985, Baandrup et al. (13) examined myocardial changes in rats with lithium-induced uremia. The rats were treated for 6–12 weeks with lithium. They found that rats with uremic changes showed evidence of cardiac damage with infiltration of lymphocytes, histiocytes, and plasma cells. These changes were not present in rats that were not uremic. However, the changes were reversible. The authors concluded that presence of chronic kidney damage and lithium treatment together can lead to reversible myocardial changes. Prolonged exposures to serum lithium level of 2 mM or greater may lead to liver damage (192) and renal damage (190). Serum alcohol dehydrogenase may be increased in patients that take lithium and have alcohol dependence (160). In rats, superoxide dysmutase (SOD) and glutathione peroxidase (Gpx) activity increased in liver but not in brain (152). Regular monitoring of serum concentrations of lithium is essential, particularly in patients with preexisting neurological illness, older age, or receiving medications that may interact with lithium (48). Some patients may be more sensitive to lithium than other (139). For example, patients with Parkinson’s and other neurodegenerative diseases may develop dyskine- YOUNG sias in the absence of other signs of lithium neurotoxicity (53,54), even at normal therapeutic levels (21,303). Increased sensitivity to lithium may also occur in patients with stroke (206) but apparently not in head injury where lithium is sometimes used to treat aggressive behavior (103). Even mildly elevated serum lithium levels of 1.5 mM can lead to persistent cerebellar ataxia (165). Long-lasting lithium intoxication can produce irreversible brain damage (3,4). Cerebellar symptoms, dementia, parkinsonian syndromes, choreoathetosis, brain stem syndromes, and other neuropathies may persist after stopping lithium treatment (316). Electroencephalographic changes (64,97,264) may detect lithium intoxication despite moderate serum levels (93). Oakley et al. (219) assessed 97 cases of lithium poisoning, finding that all had one or more risk factors for overdose. LITHIUM AND MANIC DEPRESSION Bipolar depression is one of the most severe and prevalent forms of mental illness. Its worldwide prevalence is 3–5% and it has a 15% rate of suicide if left untreated (33). The third leading cause of death in young people ages 15–24, it is a life-long disease with a strong genetic disposition. Lithium, valproate, and carbamazepine are currently the main drugs considered for manic depression. Lithium is clearly efficacious for acute mania. Valproate has shown equivocal results and the side effect of weight gain has proven to be intolerable for many people. Carbamazepine is only weakly effective. A number of other drugs have become available recently, including olanzapine, divalproate, ziprasidone, and ariprazole (320). An understanding of the mechanisms of lithium is likely to provide us with specific insights into the mechanisms of manic depression. Although lithium is the most effective drug for manic depression, therapeutic development for manic depression is still revolving around the twin theories of serotonin and norepinephrine neurotransmitter levels (272). However, other data emerged to suggest that the mechanism of manic depression may be related to a growth factor deficiency rather than a neurotransmitter imbalance. Polymorphisms of BNDF and the serotonin transporter gene 5-HTT predict lithium response in patients with manic depression. Rybakowski et al. (251) reported a significant association between certain BDNF and 5HTT polymorphisms with lithium response (250). However, Michelon et al. (195) did not find any association of INPP1, 5-HTT, BDNF, AP-2β, or GSK3β variants with lithium response in bipolar disorders. Masoliver et al. (188) found an association between 5-HTT and antidepressant-induced mania in bipolar disorder but no association of 5-HTT with the lithium responses. DmitrzakWeglarz et al. (61) did not find a significant association REVIEW OF LITHIUM EFFECTS ON BRAIN AND BLOOD of serotonin receptors (5-HT2A, 5-HT2C) with lithium response. Finally, Serretti et al. (268) found a significant association between SERTPR variants and lithium outcomes. So, lithium seems to be pressing a growth factor and serotonin transport button. What is the optimal serum lithium level for long-term treatment of bipolar disorders? Severus et al. (269) reviewed the literature from 1996 to 2006 and report that the minimum effective dose is 0.4 mM while the optimal response appears to be between 0.6 and 0.75 mM. According to their review, doses greater than 0.75 mM may not confer additional protection against overall morbidity but may improve control of interepisode manic symptoms. Abrupt reduction of lithium levels to less than 0.2 mM may be associated with a greater risk of relapse. Therefore, careful monitoring of serum levels and tapering of lithium is advised. Lithium salts are associated with lower adverse drug reaction (118) rates than neuroleptics or antidepressants (109). In fact, lithium is used to treat complications of other drugs, such as alcoholism (257). One complication of lithium and other antidepressive drugs is weight gain (172,214,294). The mechanism of the weight gain is not known. Levine and Saltzman (173) found that lithium increases the weight of the female rats gastrointestinal tract that accounted for the overall body weight gain. Lithium increases gastrointestinal tract weight in males as well but the rats lost weight from other parts of their body and therefore showed no change in overall body weight. Lithium does interact adversely with several drugs, including clozapine (123), levofloxacin (301), COX-2 inhibitors (231,242,285), ziprasidone (196), topiramate (1), and carbamazepine (189). Renal loop diuretics, angiotensin-converting enzymes, and nonsteroidal anti-inflammatory drugs all increase the risk of elevated serum lithium levels (145). Lithium promotes cyclooxygenase 2-dependent polyuria in mice (241). Use of comedication, especially antibiotics, tends to be associated with elevated lithium serum levels (333). Lithium may lower lamotrigine serum concentration to dose ratios (243). Lithium combined with 5-HT1A receptor blockers may cause excessive 5-HT2A receptor stimulation (128). Lithium also may transiently inhibit morphine analgesia (141) and other opioid effects (126). Several clinicians have proposed the use of lithium plus drug combination to treat manic depression. For example, Lin et al. (179) recommended lithium, valproate, and olanzapine, with possible addition of lamotrigine for effective for preventing depressive relapses. Zarate et al. (341) thought that the NMDA receptor blocker riluzole might work well with lithium and went ahead to test this in an open-label trial. In 14 depressed patients, lithium + riluzole was better than lithium alone. Aripiprazole 11 appears to be well tolerated for the treatment of rapidcycling bipolar disorder (211). Divalproex and lithium appear to be similarly cost-effective for adults with bipolar disorders (210). According to Beyer et al. (28) standard mood stabilizers (lithium, valproate, carbamazepine, and lamotrigene) are the most prescribed medications (68%), followed by antipsychotics (54%) and antidepressants (34%). Combination therapies are more common (57%) than monotherapy (38%). These treatments achieve remission in 35% while 32% show no significant improvement. For those with treatment resistant bipolar II depression, lamotrigine may be the drug of choice, resulting in 52% of the patients “very much improved” and 32% “much improved.” Lamotrigene (Lamictal) is an anticonvulsant that may block sodium channels and has significantly more antidepressant potency than valproate or carbamapazine. LITHIUM AND ALZHEIMER’S DISEASE Due to its known effects on depression, lithium has been used to treat neurological disorders that may have depression as a component symptom. Some early studies discouraged such use. For example, in 1984, Kelwala et al. (151) reported that lithium accentuates extrapyramidal symptoms in people with Alzheimer’s disease, although it did not do so in people who did not have preexisting extrapyramidal symptoms. Coffey and Ross (53) describe greater lithium neurotoxicity in patients with degenerative brain disease. Side effects also appeared to be more pronounced in old age due to slower renal clearance (330). Demented patients may have lower renal secretion lithium (149,183). Lithium levels thus must be carefully monitored in elderly patients (79,212). Some studies suggested that lithium might be useful for certain forms of dementia. For example, lithium reversed dementia in one patient with an affective disorder (36). Neurologists began to use lithium to treat depression in patients with Alzheimer’s disease (153). By the late 1990s, several groups began to report lithium mechanisms that may be beneficial for Alzheimer’s disease and other neurodegenerative diseases. In 1999, Manji et al. (185,186) pointed out that lithium is the only drug known to increase the levels of the neuroprotective protein Bcl-2 in rat frontal cortex, hippocampus, and striatum, as well as human cells, and suggested that lithium use may be warranted for long-term treatment of certain neurodegenerative disorders. Munoz-Montano (209) suggested that upregulation of GSK3β contributes to cytoskeletal neuropathology in Alzheimer’s disease by phosphorylation of tau (80) and lithium inhibits GSK3β. Inestrosa et al. (130) pointed out that AchE-Aβ toxicity in hippocampal slices is blocked by lithium, an activator of the Wnt cascade, suggesting that lithium is a thera- 12 peutic candidate for treatment Alzheimer’s disease. Many investigators began to look at lithium effects on various neurodegenerative mechanisms. A majority of familial Alzheimer’s disease cases have now been attributed to mutations of the presenilin (PS1) gene. This gene has a specific site that is phosphorylated by GSK3β. Site-directed mutagenesis of this site Ser397 and inhibition of GSK3β by lithium will increase the Cterminal version of the PS1 protein (156). Van Gassen et al. (315) found that one of the causes of early onset Alzheimer’s disease is inhibition of β-catenin nuclear translation by PS1. GSK3β prevents the Wnt/β-catenin entry into the nucleus and lithium increase Wnt/β-catenin entry by inhibiting GSK3β activity (86). Lithium can overcome PS1 inhibition of Wnt-catechenin (222). Alzheimer’s disease is associated with abnormal increases of GSK3 activity (29). In Drosophila models of tauopathies, lithium reverses axonal transport and locomotor deficits (207). Lithium reduces phosphorylation of proteins known to accumulate in Alzheimer’s and other degenerative diseases. Planel et al. (234) pointed out that hyperphosphorylated tau is a major component of neurofibrillary tangles in Alzheimer’s disease. GSK3β phosphorylates tau (254) but protein phosphatase 2A (PP2A) plays a major role in removing the phosphates. Lithium inhibits GSK3β phosphorylation of tau (293) and stimulates PP2A (104,309). Lithium not only inhibits tau phosphorylation (70,137,181) but also enhances tau cleavage (239). Tau phosphorylation may occur independently of GSK3β and PKA kinase (59). Lithium inhibits amyloid secretion by cells (105, 298). Spherical aggregates of β-amyloid are highly neurotoxic and activate tau protein kinase 1 (PK1) and GSK3β (127), both of which are blocked by lithium. Lithium also blocks integrin-linked kinase-induced aberrant tau phosphorylation (133). Lithium inhibits Akt/ PKB kinase phosphorylation of tau (162). Chronic lithium treatment decreases mutant tau protein aggregation in a transgenic mouse model (228). Lithium reduces production of β-amyloid (Aβ) peptides derived from amyloid precursor protein (APP) by blocking GSK3α (232) and CDK5 (252), which are necessary for APP cleavage. Lithium and valproic acid appears to inhibit Aβ peptide production in HEK293 cells transfected with APP (296). The mechanism is not clear, but Akiyama et al. (6) reported that lithium blocked Pin1 binding, inhibiting Aβ production. Nunes et al. (218) recently studied the risk for Alzheimer’s disease in patients with bipolar disorders receiving lithium or not receiving lithium. Normally, the prevalence of Alzheimer’s disease should be 7% in an age-comparable population but the total sample had approximately 19% prevalence of Alzheimer’s. When they YOUNG compared 66 patients that were on lithium and 48 patients that were not on lithium, they found that only 3 patients (5%) of the lithium-treated group had dementia and 16 patients (33%) of the non-lithium-treated group had dementia. This case-control study suggests that lithium reduced prevalence of Alzheimer’s disease in patients with bipolar disorders. In summary, lithium seems almost designed for Alzheimer’s disease. This disease results from accumulations of toxic proteins called tau and β-amyloid (IAβ). GSK3β is the main enzyme that phosphorylates IAβ. GSK3β also phosphorylates the presenilin (PS1) gene that is the cause of most familial Alzheimer’s disease and inhibits Wnt/β-catenin. GSK3β phosphorylates Wnt/β-catenin nuclear factor, responsible for neuronal growth and proliferation. Lithium also stimulates the PP2A enzyme that removes the phosphates and enhances cleavage of tau. Lithium inhibits amyloid secretion and production. Finally, lithium-treated elderly patients with bipolar disorder have a lower risk of Alzheimer’s disease than those that are not lithium treated. LITHIUM AND OTHER NEURODEGENERATIVE DISEASES GSK3β is now regarded as an important therapeutic target in neurodegenerative diseases (68,107). Through GSK3β, lithium is neuroprotective through many mechanisms (249), including blocking NMDA receptor-mediated calcium current, activation of β-catenin, heat shock factor 1, activator protein 1, CREB protein, and Bcl-2. Lithium inhibition of GSK3β increases tolerance of HT22 cells to oxidative stress (261). Bauer et al. (18) pointed out that lithium not only protects neurons but stimulates neurogenesis in the hippocampus. Wei et al. (327) found long-term lithium treatment prevents βamyloid peptide-induced death of pheochromocytoma and cerebellar granular cells. They attributed this to a doubling of Bcl-2 expression by lithium. De Ferrari et al. (58) proposed that activation of Wnt signaling by lithium rescues neurodegeneration and behavior impairment due to β-amyloid fibrils. Finally, lithium also inhibits Aβ(1–42)-induced JNK and ERK activation in rabbit hippocampus, independently of tau phosphorylation (100). Lithium may even have a role in Parkinson’s disease. For example, Chen et al. (46) reported that GSK3β mediates 6-hydroxydopamine (6-OHDA)-induced neuronal death. Lithium and other GSK3β inhibitors prevent apoptosis of neurons exposed to 6-OHDA. While antioxidants had some neuroprotective effects, they did not stop 6-OHDA-induced GSK3β activation. In another study, GSK3β appears to act downstream of PP2A and PI3K Akt pathways and upstream of caspase-2 in ceramideinduced mitochondria apoptosis (178). Lithium blocks REVIEW OF LITHIUM EFFECTS ON BRAIN AND BLOOD ceramide-induced apoptosis (41) by inhibiting both phosphokinase B and GSK3β dephosphophorylation (203). This lithium effect is specific and not replicated by other antidepression drugs such as valproate (201). Lithium inhibition of GSK3β leads to accumulation of cytoplasmic β-catenin and activation of Wnt target genes, including engrailed-1 and cyclin D1 (98). Woodgett (334) suggested that GSK3 may pay an important role in diabetes and other disorders. Several investigators have proposed the use of lithium to treat Huntington’s disease, a genetic condition where a polyglutamine expansion mutation confers a toxic gain-of-function and causes the protein to aggregate. The proteins are cleared by macroautophagy and rapamycin upregulates this process. However, lithium induces mTOR-independent autophagy by inhibiting inositol monophosphatase, reducing inositol and IP3 levels (255). However, inhibition of GSK3β attenuates autophagy and mutant huntingtin clearance by activating mTOR. Sarkar et al. (256) propose to use a combination of lithium and rapamycin to treat Huntington’s disease. Lithium also rescues neurons from the toxicity of aggregate prone proteins in Drosophila (25). Chuang (51) has pointed out that lithium is a robust neuroprotective agent that also stimulates neurogenesis. They showed this in a quinolinic acid model of Huntington’s disease in the rat striatum (266). Lithium acts through many mechanisms to inhibit NMDA receptormediated calcium influx, upregulation of antiapoptotic Bcl-2, downregulated proapoptotic p53 and bax, and activate multiple cell survival factors. It antagonizes many cell death mechanisms, including glutamate-inducted JNK activation, p38 kinase, and AP-1 binding. Lithium induces expression of BDNF and TrkB signaling. It stimulates neurogenesis. Lithium blocks alcohol-induced neurodegeneration in mice (42). Alcohol induces caspase-3 (an enzyme that causes apoptosis) and reduces phosphorylation of Akt, GSK3β, and AMPK in mice at postnatal day 7. Lithium treatment not only reversed all these changes but also inhibited the alcohol-induced accumulation of cholesterol ester and N-aceylphosphatidylethanolamine in the brain. This suggests that Akt, GSK3β, and AMPK are involved in alcohol-mediated neuropathy and lithium can block these changes. There is a possibility that lithium may be useful for the treatment of prion-mediated neurodegenerative diseases, such as subacute spongiform encephalopathy (166, 168). Perez et al. (229) reported that PrP106-126, a synthetic peptide obtained from the amyloidogenic region of the prion protein, will cause cultured neurons to undergo atrophy and die. Lithium significantly reduces peptide-induced cell death both in primary neuronal cultures and also neuroblastoma cells. Overexpression of a 13 dominant negative mutant of GSK3 (which turns off GSK3 activity) prevents death of cells exposed to PrP106-126. Lithium was in fact suggested as an additive to reduce stress and aggressive behavior in mink and cattle (167). In 2005, Dunn et al. (65) did a case-control study on data from the General Practice Research Database and found that patients who received lithium had a higher risk of dementia and the risk for dementia increased with greater numbers of lithium prescriptions. This correlation, however, may reflect the increasing use of lithium to treat depression in patients with dementia. Finally, in 2008, Fornai et al. (81) reported that lithium delays progression of amyotrophic lateral sclerosis (ALS). They randomized 44 patients to riluzole plus lithium (0.4–0.8 mM serum levels) or riluzole. After 15 months, 29% of the riluzole-treated patients had expired while all the lithium-treated patients were still alive. Assessment of disability scores revealed significant progression of those patients in the riluzole-treated group but not the lithium-treated groups. If confirmed, this would be the first treatment with such dramatic results on ALS. CONCLUSIONS Lithium has an astonishing range of activity on the cells. In fact, it appears almost designed to turn on multiple cellular mechanisms and genes that protect the cells against toxins, stress, ischemia, and injury. At the same time that it protects cells, it also turns genes for growth factors, cellular repair, and regeneration. For much of the history of lithium use, our knowledge of cellular biology was insufficient to allow an understanding of how lithium worked. Now, it seems that lithium is leading us to an understanding of the biology of cellular injury. One of lithium’s most robust effects is its stimulation of stem cells. This effect of lithium was first observed in white blood cells. Patients treated with lithium develop leukocytosis and lymphopenia. It does so by stimulating pluripotent bone marrow stem cells and encouraging the differentiation of cell formation towards granulocytes rather than lymphocytes. This effect turns out to be so robust that lithium is an effective therapy of granulopenia associated with chemotherapy. At the same time that it suppresses lymphocyte production, lithium enhances immune activity of lymphocytes. Lithium is used as an immune modulator for viral vaccines and to treat autoimmune disease. Lithium inhibits a number of kinases and phosphatases that in turn affects many systems including inflammation, metabolism, receptor sensitivity, and adenyl cyclase. For years, lithium was thought to act through three interacting systems: modulating inhibitory and excitatory neurotransmitters, inhibits GSK3β, and regulates tran- 14 scription factors that control gene expression. All these mechanisms appear to converge to inhibit GSK3β, which turns out to have remarkable effects on tau and other amyloid proteins that contribute to Alzheimer’s and other neurodegenerative diseases, including Parkinson’s and Huntington’s disease, alcohol-induced neuronal degeneration, and prion-mediated diseases. One recent clinical trial suggests that lithium delays progression of ALS. Chronic administration of lithium increases the levels of neurotrophic factors in the brain, including all the factors known to stimulate regeneration. Not surprisingly, lithium stimulates not only regeneration but also neurogenesis both in vitro and in vivo. One important place where lithium strongly stimulates neurogenesis is the hippocampus. At therapeutically relevant levels of 0.6–0.8 mM, lithium causes new neurons to be produced in both injured and uninjured hippocampus. The mechanism appears to involve the WNT/β-catenin pathway. The lithium effect on cells is interesting from another perspective. Its effects appear to be most prominent on primary neural stem cells rather than cell lines. Magnetic resonance studies of patients that have taken lithium have shown increased gray matter volume and density, supporting the observations that lithium causes neurogenesis in the brain. While not all studies show such an effect of lithium, other studies indicate that lithium increases NAA, a neuronal marker in brains of patients with manic depression. In fact, one study suggested that lithium-treated bipolar patients might have more gray matter than age-matched normal subjects. If true, this would be a remarkable confirmation of lithium as a general stimulator of neural stem cells in the brain. Given its stimulation of neurotrophic factors and neurogenesis, it is perhaps not surprising that lithium has turned out to be a potent neuroprotective agent. It turns out that lithium upregulates several antiapoptotic genes (such Bcl-2) and downregulates proapoptotic genes (p53 and Bax). It activates many cell survival factors and antagonizes many factors known to contribute to apoptosis, including NJK, p38 kinase, AP-1 binding, and phosphorylated CREB loss. Lithium protects neurons against a variety of neurotoxins including glutamate and NMDA, α-bungarotoxin, HIV-gp120- and tau-mediated cell death, and even calcium entry and low extracellular potassium. Lithium is surprisingly nontoxic in the therapeutic range of 0.6–1.0 mM while toxic levels occur at 1.4 mM or higher levels. Acute toxicity is rare and generally reversible. Because toxic levels are close to therapeutic levels, careful titration of doses with serum measurements is recommended. Oral doses of 500–1200 mg will bring a majority of patients into the therapeutic range. YOUNG While lithium is not mutagenic or carcinogenic, it is potentially teratogenic given its many effects on cell growth and differentiation. Because it passes readily across the placental barrier, lithium use probably should be avoided during the first trimester and must be carefully monitored during pregnancy. Long-lasting lithium intoxication can produce irreversible brain damage. Bipolar depression is one of the most serious and prevalent mental illness in the world. With a worldwide prevalence of 3–5% and a 15% suicide rate when untreated, bipolar disease is the third leading cause of death among young people. Lithium is very effective in about a third of patients, partially effective in a third, and not effective in about a third. For those patients that are not responsive to lithium, several anticonvulsants may be effective. However, despite much research looking for safer and more effective bipolar treatments, lithium is still by far the most effective to date. It continues to one of the most prescribed drugs in the world, resulting in 52% percent of patients “very much improved” and 32% “much improved.” This is not bad for a 100year-old drug. REFERENCES 1. Abraham, G.; Owen, J. Topiramate can cause lithium toxicity. J. Clin. Psychopharmacol. 24(5):565–567; 2004. 2. Acevedo, N.; Wang, X.; Dunn, R. L.; Smith, G. D. Glycogen synthase kinase-3 regulation of chromatin segregation and cytokinesis in mouse preimplantation embryos. Mol. Reprod. Dev. 74(2):178–188; 2007. 3. Adityanjee. The syndrome of irreversible lithium-effectuated neurotoxicity (SILENT). Pharmacopsychiatry 22(2): 81–83; 1989. 4. Adityanjee; Balaraju, K. B.; Ahuja, G. K. Prior neurologic illness and the syndrome of irreversible lithiumeffectuated neurotoxicity (SILENT). Aust. N. Z. J. Psychiatry 23(3):422–424; 1989. 5. Agranoff, B. W.; Fisher, S. K. Inositol, lithium, and the brain. Psychopharmacol. Bull. 35(3):5–18; 2001. 6. Akiyama, H.; Shin, R. W.; Uchida, C.; Kitamoto, T.; Uchida, T. Pin1 promotes production of Alzheimer’s amyloid beta from beta-cleaved amyloid precursor protein. Biochem. Biophys. Res. Commun. 336(2):521–529; 2005. 7. Albrecht, J.; Helderman, J. H.; Schlesser, M. A.; Rush, A. J. A controlled study of cellular immune function in affective disorders before and during somatic therapy. Psychiatry Res. 15(3):185–193; 1985. 8. Amdisen, A.; Schou, M. [The significance of the serum lithium level for lithium therapy of phasic psychoses] (author’s transl). MMW Munch. Med. Wochenschr. 117(36):1417–1420; 1975. 9. Angelucci, F.; Aloe, L.; Jimenez-Vasquez, P.; Mathe, A. A. Lithium treatment alters brain concentrations of nerve growth factor, brain-derived neurotrophic factor and glial cell line-derived neurotrophic factor in a rat model of depression. Int. J. Neuropsychopharmacol. 6(3): 225–231; 2003. 10. Angelucci, F.; Mathe, A. A.; Aloe, L. Neurotrophic factors and CNS disorders: Findings in rodent models of REVIEW OF LITHIUM EFFECTS ON BRAIN AND BLOOD 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. depression and schizophrenia. Prog. Brain Res. 146:151– 165; 2004. Anton, R.; Kestler, H. A.; Kuhl, M. Beta-catenin signaling contributes to stemness and regulates early differentiation in murine embryonic stem cells. FEBS Lett. 581(27):5247–5254; 2007. Arnon, R. G.; Marin-Garcia, J.; Peeden, J. N. Tricuspid valve regurgitation and lithium carbonate toxicity in a newborn infant. Am. J. Dis. Child. 135(10):941–943; 1981. Baandrup, U.; Bagger, J. P.; Christensen, S. Myocardial changes in rats with lithium-induced uraemia. Acta Pathol. Microbiol. Immunol. Scand. [A] 93(6):317–322; 1985. Balon, R.; Berchou, R. Hematologic side effects of psychotropic drugs. Psychosomatics 27(2):119–120, 125– 127; 1986. Banduhn, N.; Obe, G.; Muller-Oerlinghausen, B. Is lithium mutagenic in man? Pharmakopsychiatr. Neuropsychopharmakol. 13(4):218–227; 1980. Barillas, R.; Friehs, I.; Cao-Danh, H.; Martinez, J. F.; del Nido, P. J. Inhibition of glycogen synthase kinase-3beta improves tolerance to ischemia in hypertrophied hearts. Ann. Thorac. Surg. 84(1):126–133; 2007. Baslow, M. H.; Kitada, K.; Suckow, R. F.; Hungund, B. L.; Serikawa, T. The effects of lithium chloride and other substances on levels of brain N-acetyl-L-aspartic acid in Canavan disease-like rats. Neurochem. Res. 27(5):403–406; 2002. Bauer, M.; Alda, M.; Priller, J.; Young, L. T. Implications of the neuroprotective effects of lithium for the treatment of bipolar and neurodegenerative disorders. Pharmacopsychiatry 36(Suppl. 3):S250–254; 2003. Bauer, M.; Whybrow, P. C.; Angst, J.; Versiani, M.; Moller, H. J.; World Federation of Societies of Biological Psychiatry (WFSBP) Task Force on Treatment Guidelines for Biological Treatment of Unipolar Depressive Disorders. World Federation of Societies of Biological Psychiatry (WFSBP) guidelines for biological treatment of unipolar depressive disorders, part 2: Maintenance treatment of major depressive disorder and treatment of chronic depressive disorders and subthreshold depressions. World J. Biol. Psychiatry 3(2):69–86; 2002. Bearden, C. E.; Thompson, P. M.; Dalwani, M.; Hayashi, K. M.; Lee, A. D.; Nicoletti, M.; Trakhtenbroit, M.; Glahn, D. C.; Brambilla, P.; Sassi, R. B.; Mallinger, A. G.; Frank, E.; Kupfer, D. J.; Soares, J. C. Greater cortical gray matter density in lithium-treated patients with bipolar disorder. Biol. Psychiatry 62(1):7–16; 2007. Bell, A. J.; Cole, A.; Eccleston, D.; Ferrier, I. N. Lithium neurotoxicity at normal therapeutic levels. Br. J. Psychiatry 162:689–692; 1993. Bell, E. C.; Willson, M. C.; Wilman, A. H.; Dave, S.; Silverstone, P. H. Differential effects of chronic lithium and valproate on brain activation in healthy volunteers. Hum. Psychopharmacol. 20(6):415–424; 2005. Belyavskaya, N. A. Lithium-induced changes in gravicurvature, statocyte ultrastructure and calcium balance of pea roots. Adv. Space Res. 27(5):961–966; 2001. Benedito, A. B.; Lehtinen, M.; Massol, R.; Lopes, U. G.; Kirchhausen, T.; Rao, A.; Bonni, A. The transcription factor NFAT3 mediates neuronal survival. J. Biol. Chem. 280(4):2818–2825; 2005. Berger, Z.; Ttofi, E. K.; Michel, C. H.; Pasco, M. Y.; 15 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. Tenant, S.; Rubinsztein, D. C.; O’Kane, C. J. Lithium rescues toxicity of aggregate-prone proteins in Drosophila by perturbing Wnt pathway. Hum. Mol. Genet. 14(20):3003–3011; 2005. Berry, G. T.; Buccafusca, R.; Greer, J. J.; Eccleston, E. Phosphoinositide deficiency due to inositol depletion is not a mechanism of lithium action in brain. Mol. Genet. Metab. 82(1):87–92; 2004. Besana, C.; Zocchi, M. R.; Storti, M.; Codazzi, P.; Pardi, R.; Ciboddo, G. Effects of short-term lithium treatment on peripheral blood lymphocytes and granulocytes in healthy volunteers. Ric. Clin. Lab. 13(3):373–379; 1983. Beyer, J. L.; Burchitt, B.; Gersing, K.; Krishnan, K. R. Patterns of pharmacotherapy and treatment response in elderly adults with bipolar disorder. Psychopharmacol. Bull. 41(1):102–114; 2008. Bhat, R. V.; Budd Haeberlein, S. L.; Avila, J. Glycogen synthase kinase 3: A drug target for CNS therapies. J. Neurochem. 89(6):1313–1317; 2004. Bijur, G. N.; Jope, R. S. Opposing actions of phosphatidylinositol 3-kinase and glycogen synthase kinase-3beta in the regulation of HSF-1 activity. J. Neurochem. 75(6): 2401–2408; 2000. Boggs, D. R.; Joyce, R. A. The hematopoietic effects of lithium. Semin. Hematol. 20(2):129–138; 1983. Boshes, R. A.; Manschreck, T. C.; Desrosiers, J.; Candela, S.; Hanrahan-Boshes, M. Initiation of clozapine therapy in a patient with preexisting leukopenia: A discussion of the rationale of current treatment options. Ann. Clin. Psychiatry 13(4):233–237; 2001. Bousono, M.; Baca, E.; Alvarez, E.; Eguiluz, I.; Martin, M.; Roca, M.; Urretavizcaya, M. Consequences of the long-term depression. Actas Esp. Psiquiatr. 36(2):44–52; 2008. Brambilla, P.; Stanley, J. A.; Nicoletti, M. A.; Sassi, R. B.; Mallinger, A. G.; Frank, E.; Kupfer, D.; Keshavan, M. S.; Soares, J. C. 1H magnetic resonance spectroscopy investigation of the dorsolateral prefrontal cortex in bipolar disorder patients. J. Affect. Disord. 86(1):61–67; 2005. Brambilla, P.; Stanley, J. A.; Sassi, R. B.; Nicoletti, M. A.; Mallinger, A. G.; Keshavan, M. S.; Soares, J. C. 1H MRS study of dorsolateral prefrontal cortex in healthy individuals before and after lithium administration. Neuropsychopharmacology 29(10):1918–1924; 2004. Bright-Long, L. E.; Fink, M. Reversible dementia and affective disorder: The Rip Van Winkle syndrome. Convuls. Ther. 9(3):209–216; 1993. Burgess, S.; Geddes, J.; Hawton, K.; Townsend, E.; Jamison, K.; Goodwin, G. Lithium for maintenance treatment of mood disorders. Cochrane Database Syst. Rev. 3:CD003013; 2001. Burstein, D. E.; Seeley, P. J.; Greene, L. A. Lithium ion inhibits nerve growth factor-induced neurite outgrowth and phosphorylation of nerve growth factor-modulated microtubule-associated proteins. J. Cell Biol. 101(3): 862–870; 1985. Cai, X.; Li, M.; Vrana, J.; Schaller, M. D. Glycogen synthase kinase 3- and extracellular signal-regulated kinasedependent phosphorylation of paxillin regulates cytoskeletal rearrangement. Mol. Cell. Biol. 26(7):2857–2868; 2006. Calabrese, J. R.; Gulledge, A. D.; Hahn, K.; Skwerer, R.; Kotz, M.; Schumacher, O. P.; Gupta, M. K.; Krupp, N.; Gold, P. W. Autoimmune thyroiditis in manic-depressive 16 41. 42. 43. 44. 45. 46. 47. 48. 49. 50. 51. 52. 53. 54. 55. 56. YOUNG patients treated with lithium. Am. J. Psychiatry 142(11): 1318–1321; 1985. Centeno, F.; Mora, A.; Fuentes, J. M.; Soler, G.; Claro, E. Partial lithium-associated protection against apoptosis induced by C2-ceramide in cerebellar granule neurons. Neuroreport 9(18):4199–4203; 1998. Chakraborty, G.; Saito, M.; Mao, R. F.; Wang, R.; Vadasz, C. Lithium blocks ethanol-induced modulation of protein kinases in the developing brain. Biochem. Biophys. Res. Commun. 367(3):597–602; 2008. Chalecka-Franaszek, E.; Chuang, D. M. Lithium activates the serine/threonine kinase Akt-1 and suppresses glutamate-induced inhibition of Akt-1 activity in neurons. Proc. Natl. Acad. Sci. USA 96(15):8745–8750; 1999. Chang, K.; Karchemskiy, A.; Barnea-Goraly, N.; Garrett, A.; Simeonova, D. I.; Reiss, A. Reduced amygdalar gray matter volume in familial pediatric bipolar disorder. J. Am. Acad. Child Adolesc. Psychiatry 44(6):565–573; 2005. Chatelain, C.; Burstein, S. A.; Harker, L. A. Lithium enhancement of megakaryocytopoiesis in culture: Mediation via accessory marrow cells. Blood 62(1):172–176; 1983. Chen, G.; Bower, K. A.; Ma, C.; Fang, S.; Thiele, C. J.; Luo, J. Glycogen synthase kinase 3beta (GSK3beta) mediates 6-hydroxydopamine-induced neuronal death. FASEB J. 18(10):1162–1164; 2004. Chen, G.; Rajkowska, G.; Du, F.; Seraji-Bozorgzad, N.; Manji, H. K. Enhancement of hippocampal neurogenesis by lithium. J. Neurochem. 75(4):1729–1734; 2000. Chen, K. P.; Shen, W. W.; Lu, M. L. Implication of serum concentration monitoring in patients with lithium intoxication. Psychiatry Clin. Neurosci. 58(1):25–29; 2004. Chen, R. W.; Chuang, D. M. Long term lithium treatment suppresses p53 and Bax expression but increases Bcl-2 expression. A prominent role in neuroprotection against excitotoxicity. J. Biol. Chem. 274(10):6039– 6042; 1999. Chen, X.; Wen, W.; Malhi, G. S.; Ivanovski, B.; Sachdev, P. S. Regional gray matter changes in bipolar disorder: A voxel-based morphometric study. Aust. N. Z. J. Psychiatry 41(4):327–336; 2007. Chuang, D. M. Neuroprotective and neurotrophic actions of the mood stabilizer lithium: Can it be used to treat neurodegenerative diseases? Crit. Rev. Neurobiol. 16(1–2): 83–90; 2004. Chuang, D. M.; Chen, R. W.; Chalecka-Franaszek, E.; Ren, M.; Hashimoto, R.; Senatorov, V.; Kanai, H.; Hough, C.; Hiroi, T.; Leeds, P. Neuroprotective effects of lithium in cultured cells and animal models of diseases. Bipolar Disord. 4(2):129–136; 2002. Coffey, C. E.; Ross, D. R. Lithium neurotoxicity in patients with degenerative brain disease. J. Clin. Psychiatry 46(8):354; 1985. Coffey, C. E.; Ross, D. R.; Massey, E. W.; Olanow, C. W. Dyskinesias associated with lithium therapy in parkinsonism. Clin. Neuropharmacol. 7(3):223–229; 1984. Cooper, T. B.; Carroll, B. J. Monitoring lithium dose levels: Estimation of lithium in blood and other body fluids. J. Clin. Psychopharmacol. 1(2):53–58; 1981. Cramarossa, L.; Astorre, P.; Ronchi, F. [Therapy of hyperthyroidism: Indications, advantages and disadvantages of treatment of the adult and the elderly]. Recenti Prog. Med. 80(4):219–226; 1989. 57. de Alarcon, P. A.; Goldberg, J.; Nelson, D. A.; Stockman, 3rd, J. A. Lithium therapy in childhood neutropenia. J. Pediatr. 102(1):149–152; 1983. 58. De Ferrari, G. V.; Chacon, M. A.; Barria, M. I.; Garrido, J. L.; Godoy, J. A.; Olivares, G.; Reyes, A. E.; Alvarez, A.; Bronfman, M.; Inestrosa, N. C. Activation of Wnt signaling rescues neurodegeneration and behavioral impairments induced by beta-amyloid fibrils. Mol. Psychiatry 8(2):195–208; 2003. 59. Delobel, P.; Flament, S.; Hamdane, M.; Delacourte, A.; Vilain, J. P.; Buee, L. Modelling Alzheimer-specific abnormal tau phosphorylation independently of GSK3beta and PKA kinase activities. FEBS Lett. 516(1–3):151– 155; 2002. 60. de Vries, E. G.; van Luyn, M. J.; Mulder, N. H.; Bins, M.; Halie, M. R. In vitro effects of lithium on granulocyte colony formation in normal men, in hematological disorders and in small-cell carcinoma of the lung. Acta Haematol. 70(2):97–107; 1983. 61. Dmitrzak-Weglarz, M.; Rybakowski, J. K.; Suwalska, A.; Slopien, A.; Czerski, P. M.; Leszczynska-Rodziewicz, A.; Hauser, J. Association studies of 5-HT(2A) and 5-HT(2C) serotonin receptor gene polymorphisms with prophylactic lithium response in bipolar patients. Pharmacol. Rep. 57(6):761–765; 2005. 62. Dosch, H. M.; Gelfand, E. W. Functional differentiation of B lymphocytes in agammaglobulinemia. III. Characterization of spontaneous suppressor cell activity. J. Immunol. 121(5):2097–2105; 1978. 63. Dosch, H. M.; Matheson, D.; Schuurman, R. K.; Gelfand, E. W. Anti-suppressor cell effects of lithium in vitro and in vivo. Adv. Exp. Med. Biol. 127:447–462; 1980. 64. Dunand, A. C.; Jallon, P. [Pseudoperiodic and paroxysmal electroencephalographic activities]. Neurophysiol. Clin. 32(1):2–37; 2002. 65. Dunn, N.; Holmes, C.; Mullee, M. Does lithium therapy protect against the onset of dementia? Alzheimer. Dis. Assoc. Disord. 19(1):20–22; 2005. 66. Dunner, D. L. Drug interactions of lithium and other antimanic/mood-stabilizing medications. J. Clin. Psychiatry 64(Suppl. 5):38–43; 2003. 67. Ebstein, R. P.; Oppenheim, G.; Ebstein, B. S.; Amiri, Z.; Stessman, J. The cyclic AMP second messenger system in man: The effects of heredity, hormones, drugs, aluminum, age and disease on signal amplification. Prog. Neuropsychopharmacol. Biol. Psychiatry 10(3–5):323–353; 1986. 68. Eldar-Finkelman, H. Glycogen synthase kinase 3: An emerging therapeutic target. Trends Mol. Med. 8(3):126– 132; 2002. 69. Elliott, E.; Atlas, R.; Lange, A.; Ginzburg, I. Brainderived neurotrophic factor induces a rapid dephosphorylation of tau protein through a PI-3 Kinase signalling mechanism. Eur. J. Neurosci. 22(5):1081–1089; 2005. 70. Elyaman, W.; Yardin, C.; Hugon, J. Involvement of glycogen synthase kinase-3beta and tau phosphorylation in neuronal Golgi disassembly. J. Neurochem. 81(4):870– 880; 2002. 71. Espinosa, L.; Ingles-Esteve, J.; Aguilera, C.; Bigas, A. Phosphorylation by glycogen synthase kinase-3 beta down-regulates Notch activity, a link for Notch and Wnt pathways. J. Biol. Chem. 278(34):32227–32235; 2003. 72. Esposito, D.; Rouillon, F.; Limosin, F. Continuing clozapine treatment despite neutropenia. Eur. J. Clin. Pharmacol. 60(11):759–764; 2005. REVIEW OF LITHIUM EFFECTS ON BRAIN AND BLOOD 73. Eto, M.; Kouroedov, A.; Cosentino, F.; Luscher, T. F. Glycogen synthase kinase-3 mediates endothelial cell activation by tumor necrosis factor-alpha. Circulation 112(9): 1316–1322; 2005. 74. Everall, I. P.; Bell, C.; Mallory, M.; Langford, D.; Adame, A.; Rockestein, E.; Masliah, E. Lithium ameliorates HIV-gp120-mediated neurotoxicity. Mol. Cell. Neurosci. 21(3):493–501; 2002. 75. Fernandez, L. A.; Fox, R. A. Perturbation of the human immune system by lithium. Clin. Exp. Immunol. 41(3): 527–532; 1980. 76. Fernandez, L. A.; MacSween, J. M. Lithium and T cell colonies. Scand. J. Haematol. 25(5):382–384; 1980. 77. Feske, S.; Draeger, R.; Peter, H. H.; Rao, A. Impaired NFAT regulation and its role in a severe combined immunodeficiency. Immunobiology 202(2):134–150; 2000. 78. Firkin, F. C. New concepts in management of neutropenia. Aust. N. Z. J. Med. 15(1):93–97; 1985. 79. Flint, A. J. Recent developments in geriatric psychopharmacotherapy. Can. J. Psychiatry 39(8 Suppl. 1):S9–18; 1994. 80. Forlenza, O. V.; Spink, J. M.; Dayanandan, R.; Anderton, B. H.; Olesen, O. F.; Lovestone, S. Muscarinic agonists reduce tau phosphorylation in non-neuronal cells via GSK-3beta inhibition and in neurons. J. Neural Transm. 107(10):1201–1212; 2000. 81. Fornai, F.; Longone, P.; Cafaro, L.; Kastsiuchenka, O.; Ferrucci, M.; Manca, M. L.; Lazzeri, G.; Spalloni, A.; Bellio, N.; Lenzi, P.; Modugno, N.; Siciliano, G.; Isidoro, C.; Murri, L.; Ruggieri, S.; Paparelli, A. Lithium delays progression of amyotrophic lateral sclerosis. Proc. Natl. Acad. Sci. USA 105(6):2052–2057; 2008. 82. Fornai, F.; Longone, P.; Ferrucci, M.; Lenzi, P.; Isidoro, C.; Ruggieri, S.; Paparelli, A. Autophagy and amyotrophic lateral sclerosis: The multiple roles of lithium. Autophagy 4(4):527–530; 2008. 83. Frey, B. N.; Andreazza, A. C.; Rosa, A. R.; Martins, M. R.; Valvassori, S. S.; Reus, G. Z.; Hatch, J. P.; Quevedo, J.; Kapczinski, F. Lithium increases nerve growth factor levels in the rat hippocampus in an animal model of mania. Behav. Pharmacol. 17(4):311–318; 2006. 84. Friedenberg, W. R.; Marx, Jr., J. J. The effect of lithium carbonate on lymphocyte, granulocyte, and platelet function. Cancer 45(1):91–97; 1980. 85. Friedman, S. D.; Dager, S. R.; Parow, A.; Hirashima, F.; Demopulos, C.; Stoll, A. L.; Lyoo, I. K.; Dunner, D. L.; Renshaw, P. F. Lithium and valproic acid treatment effects on brain chemistry in bipolar disorder. Biol. Psychiatry 56(5):340–348; 2004. 86. Fuentealba, R. A.; Farias, G.; Scheu, J.; Bronfman, M.; Marzolo, M. P.; Inestrosa, N. C. Signal transduction during amyloid-beta-peptide neurotoxicity: Role in Alzheimer disease. Brain Res. Brain Res. Rev. 47(1–3):275– 289; 2004. 87. Fuggetta, M. P.; Alvino, E.; Romani, L.; Grohmann, U.; Potenza, C.; Giuliani, A. Increase of natural killer activity of mouse lymphocytes following in vitro and in vivo treatment with lithium. Immunopharmacol. Immunotoxicol. 10(1):79–91; 1988. 88. Fujikawa, D. G. Neuroprotective effect of ketamine administered after status epilepticus onset. Epilepsia 36(2): 186–195; 1995. 89. Fukumoto, T.; Morinobu, S.; Okamoto, Y.; Kagaya, A.; Yamawaki, S. Chronic lithium treatment increases the expression of brain-derived neurotrophic factor in the rat 17 90. 91. 92. 93. 94. 95. 96. 97. 98. 99. 100. 101. 102. 103. 104. brain. Psychopharmacology (Berl.) 158(1):100–106; 2001. Gallelli, K. A.; Wagner, C. M.; Karchemskiy, A.; Howe, M.; Spielman, D.; Reiss, A.; Chang, K. D. N-acetylaspartate levels in bipolar offspring with and at high-risk for bipolar disorder. Bipolar Disord. 7(6):589–597; 2005. Gallicchio, V. S.; Chen, M. G. Influence of lithium on proliferation of hematopoietic stem cells. Exp. Hematol. 9(7):804–810; 1981. Gallicchio, V. S.; Chen, M. G.; Watts, T. D. Specificity of lithium (Li+) to enhance the production of colony stimulating factor (GM-CSF) from mitogen-stimulated lymphocytes in vitro. Cell. Immunol. 85(1):58–66; 1984. Gallinat, J.; Boetsch, T.; Padberg, F.; Hampel, H.; Herrmann, W. M.; Hegerl, U. Is the EEG helpful in diagnosing and monitoring lithium intoxication? A case report and review of the literature. Pharmacopsychiatry 33(5): 169–173; 2000. Gama, C. S.; Andreazza, A. C.; Kunz, M.; Berk, M.; Belmonte-de-Abreu, P. S.; Kapczinski, F. Serum levels of brain-derived neurotrophic factor in patients with schizophrenia and bipolar disorder. Neurosci. Lett. 420(1):45–48; 2007. Gao, Q.; Katakowski, M.; Chen, X.; Li, Y.; Chopp, M. Human marrow stromal cells enhance connexin43 gap junction intercellular communication in cultured astrocytes. Cell Transplant. 14(2–3):109–117; 2005. Gao, X.; Wang, J.; Wei, X. [Expressions of GDNF, GDNFR alpha and Ret proteins in the brain of rats with seizures induced by pilocarpine]. Beijing Da Xue Xue Bao 35(3):296–298; 2003. Garcia-Solana, M. I.; Rodrigo-Sesma, A.; Garcia-Rodriguez, V.; Lloret-Alcaniz, M. A.; Selles-Galiana, F.; Gimenez-Rodriguez, P.; Mora-Rodriguez, E.; MedranoTovar, L.; Ferrandis-Ballester, F. [Neurotoxicity in treatment with lithium. A case report and EEG findings]. Rev. Neurol. 39(6):595–597; 2004. Garrido, J. L.; Godoy, J. A.; Alvarez, A.; Bronfman, M.; Inestrosa, N. C. Protein kinase C inhibits amyloid beta peptide neurotoxicity by acting on members of the Wnt pathway. FASEB J. 16(14):1982–1984; 2002. Gelfand, E. W.; Dosch, H. M.; Hastings, B.; Shore, A. Lithium: A modulator of cyclic AMP-dependent events in lymphocytes? Science 203(4378):365–367; 1979. Ghribi, O.; Prammonjago, P.; Herman, M. M.; Spaulding, N. K.; Savory, J. Abeta(1-42)-induced JNK and ERK activation in rabbit hippocampus is differentially regulated by lithium but is not involved in the phosphorylation of tau. Brain Res. Mol. Brain Res. 119(2):201– 206; 2003. Girod, M.; Phan, T. N.; Charles, L. Microstructural study of a nitroxide-mediated poly(ethylene oxide)/polystyrene block copolymer (PEO-b-PS) by electrospray tandem mass spectrometry. J. Am. Soc. Mass Spectrom. 19(8): 1163–1175; 2008. Giudicelli, J. F.; Tillement, J. P. Influence of sex on drug kinetics in man. Clin. Pharmacokinet. 2(3):157–166; 1977. Glenn, M. B.; Wroblewski, B.; Parziale, J.; Levine, L.; Whyte, J.; Rosenthal, M. Lithium carbonate for aggressive behavior or affective instability in ten brain-injured patients. Am. J. Phys. Med. Rehabil. 68(5):221–226; 1989. Goldbaum, O.; Richter-Landsberg, C. Activation of 18 105. 106. 107. 108. 109. 110. 111. 112. 113. 114. 115. 116. 117. 118. 119. 120. 121. 122. YOUNG PP2A-like phosphatase and modulation of tau phosphorylation accompany stress-induced apoptosis in cultured oligodendrocytes. Glia 40(3):271–282; 2002. Goodenough, S.; Schafer, M.; Behl, C. Estrogen-induced cell signalling in a cellular model of Alzheimer’s disease. J. Steroid Biochem. Mol. Biol. 84(2–3):301–305; 2003. Gould, T. D.; Gray, N. A.; Manji, H. K. Effects of a glycogen synthase kinase-3 inhibitor, lithium, in adenomatous polyposis coli mutant mice. Pharmacol. Res. 48(1):49–53; 2003. Gould, T. D.; Zarate, C. A.; Manji, H. K. Glycogen synthase kinase-3: A target for novel bipolar disorder treatments. J. Clin. Psychiatry 65(1):10–21; 2004. Grimes, C. A.; Jope, R. S. The multifaceted roles of glycogen synthase kinase 3beta in cellular signaling. Prog. Neurobiol. 65(4):391–426; 2001. Grohmann, R.; Hippius, H.; Helmchen, H.; Ruther, E.; Schmidt, L. G. The AMUP study for drug surveillance in psychiatry—a summary of inpatient data. Pharmacopsychiatry 37(Suppl. 1):S16–26; 2004. Gualtieri, R. J.; Berne, R. M.; McGrath, H. E.; Huster, W. J.; Quesenberry, P. J. Effect of adenine nucleotides on granulopoiesis and lithium-induced granulocytosis in long-term bone marrow cultures. Exp. Hematol. 14(7): 689–695; 1986. Hall, T. J.; Heckel, C.; Hudspith, B. N.; Brostoff, J. Lithium counteracts histamine suppression of human T cell mitogenesis. Immunol. Lett. 24(2):103–105; 1990. Hamburger, S.; Covinsky, J.; Uhrig, L.; Shaffer, K. Lithium carbonate therapy for granulocytopenia in a patient with myelofibrosis and septic arthritis. South Med. J. 72(12):1601–1602; 1979. Hammond, W. P.; Dale, D. C. Lithium therapy of canine cyclic hematopoiesis. Blood 55(1):26–28; 1980. Hammonds, M. D.; Shim, S. S.; Feng, P.; Calabrese, J. R. Effects of subchronic lithium treatment on levels of BDNF, Bcl-2 and phospho-CREB in the rat hippocampus. Basic Clin. Pharmacol. Toxicol. 100(5):356–359; 2007. Hart, D. A. Lithium potentiates antigen-dependent stimulation of lymphocytes only under suboptimal conditions. Int. J. Immunopharmacol. 10(2):153–160; 1988. Hart, D. A. Modulation of concanavalin A stimulation of hamster lymphoid cells by lithium chloride. Cell. Immunol. 43(1):113–122; 1979. Hart, D. A. Potentiation of phytohemagglutinin stimulation of lymphoid cells by lithium. Exp. Cell Res. 119(1): 47–53; 1979. Hasgekar, N. N.; Gokhale, P. P.; Amin, M. K.; Seshadri, R.; Lalitha, V. S. Lithium inhibits growth in a murine neural precursor cell line. Cell Biol. Int. 20(12):781–786; 1996. Hashimoto, K.; Shimizu, E.; Iyo, M. Critical role of brain-derived neurotrophic factor in mood disorders. Brain Res. Brain Res. Rev. 45(2):104–114; 2004. Hashimoto, R.; Takei, N.; Shimazu, K.; Christ, L.; Lu, B.; Chuang, D. M. Lithium induces brain-derived neurotrophic factor and activates TrkB in rodent cortical neurons: An essential step for neuroprotection against glutamate excitotoxicity. Neuropharmacology 43(7):1173–1179; 2002. Hassman, R. A.; Lazarus, J. H.; Dieguez, C.; Weetman, A. P.; Hall, R.; McGregor, A. M. The influence of lithium chloride on experimental autoimmune thyroid disease. Clin. Exp. Immunol. 61(1):49–57; 1985. Hellweg, R.; Lang, U. E.; Nagel, M.; Baumgartner, A. 123. 124. 125. 126. 127. 128. 129. 130. 131. 132. 133. 134. 135. 136. 137. Subchronic treatment with lithium increases nerve growth factor content in distinct brain regions of adult rats. Mol. Psychiatry 7(6):604–608; 2002. Hellwig, B.; Hesslinger, B.; Walden, J. Acute brain syndrome after tapering off clozapine in clozapine-lithium combination. Prog. Neuropsychopharmacol Biol. Psychiatry 20(1):179–183; 1996. Hennion, J. P.; el-Masri, M. A.; Huff, M. O.; el-Mailakh, R. S. Evaluation of neuroprotection by lithium and valproic acid against ouabain-induced cell damage. Bipolar Disord. 4(3):201–206; 2002. Hiroi, T.; Wei, H.; Hough, C.; Leeds, P.; Chuang, D. M. Protracted lithium treatment protects against the ER stress elicited by thapsigargin in rat PC12 cells: Roles of intracellular calcium, GRP78 and Bcl-2. Pharmacogenomics J. 5(2):102–111; 2005. Honar, H.; Riazi, K.; Homayoun, H.; Demehri, S.; Dehghani, M.; Vafaie, K.; Ebrahimkhani, M. R.; Rashidi, N.; Gaskari, S. A.; Dehpour, A. R. Lithium inhibits the modulatory effects of morphine on susceptibility to pentylenetetrazole-induced clonic seizure in mice: Involvement of a nitric oxide pathway. Brain Res. 1029(1):48– 55; 2004. Hoshi, M.; Sato, M.; Matsumoto, S.; Noguchi, A.; Yasutake, K.; Yoshida, N.; Sato, K. Spherical aggregates of beta-amyloid (amylospheroid) show high neurotoxicity and activate tau protein kinase I/glycogen synthase kinase-3beta. Proc. Natl. Acad. Sci. USA 100(11):6370– 6375; 2003. Ichikawa, J.; Dai, J.; Meltzer, H. Y. Lithium differs from anticonvulsant mood stabilizers in prefrontal cortical and accumbal dopamine release: Role of 5-HT(1A) receptor agonism. Brain Res. 1049(2):182–190; 2005. Il’in, N. V.; Korytova, L. I.; Filatova, A. M. [Correction of neutropenia with lithium carbonate during the radiation treatment of lymphogranulomatosis patients]. Ter. Arkh. 58(9):65–67; 1986. Inestrosa, N. C.; Alvarez, A.; Godoy, J.; Reyes, A.; De Ferrari, G. V. Acetylcholinesterase-amyloid-beta-peptide interaction and Wnt signaling involvement in Abeta neurotoxicity. Acta Neurol. Scand. Suppl. 176:53–59; 2000. Irvine, A. E.; Crockard, A. D.; Desai, Z. R.; Ennis, K. T.; Fay, A. C.; Morris, T. C.; Bridges, J. M. Lymphocytes from patients receiving lithium do not inhibit CFU-C growth. Br. J. Haematol. 62(3):467–477; 1986. Ishii, E.; Hara, T.; Miyazaki, S.; Fujiwara, T.; Goya, N. Lithium therapy for cyclic neutropenia in children. Scand. J. Haematol. 31(3):193–196; 1983. Ishii, T.; Furuoka, H.; Muroi, Y.; Nishimura, M. Inactivation of integrin-linked kinase induces aberrant tau phosphorylation via sustained activation of glycogen synthase kinase 3beta in N1E-115 neuroblastoma cells. J. Biol. Chem. 278(29):26970–26975; 2003. Ishizaka, S.; Moller, G. Lithium chloride induces partial responsiveness to LPS in nonresponder B cells. Nature 299(5881):363–365; 1982. Ishizaka, S.; Yoshikawa, M.; Kitagami, K.; Tsujii, T. Oral adjuvants for viral vaccines in humans. Vaccine 8(4):337–341; 1990. Iwamoto, J.; Hakozaki, Y.; Sakuta, H.; Kobari, S.; Kayashima, S.; Fujioka, T.; Ooba, K.; Shirahama, T. A case of agranulocytosis associated with severe acute hepatitis B. Hepatol. Res. 21(2):181–185; 2001. Jamsa, A.; Hasslund, K.; Cowburn, R. F.; Backstrom, A.; Vasange, M. The retinoic acid and brain-derived neuro- REVIEW OF LITHIUM EFFECTS ON BRAIN AND BLOOD 138. 139. 140. 141. 142. 143. 144. 145. 146. 147. 148. 149. 150. 151. 152. 153. 154. trophic factor differentiated SH-SY5Y cell line as a model for Alzheimer’s disease-like tau phosphorylation. Biochem. Biophys. Res. Commun. 319(3):993–1000; 2004. Jenkins, R. J.; Aronson, J. K.; Brearley, C. J. Increases in Na/K pump numbers in isolated human lymphocytes exposed to lithium in vitro. Reversal by myo-inositol and by inhibitors of protein kinase C and the Na/H antiport. Biochim. Biophys. Acta 1092(2):138–144; 1991. Johnson, G. F. Lithium neurotoxicity. Aust. N. Z. J. Psychiatry 10(1):33–38; 1976. Johnson, J. H.; Crookshank, H. R.; Smalley, H. E. Lithium toxicity in cattle. Vet. Hum. Toxicol. 22(4):248– 251; 1980. Johnston, I. N.; Westbrook, R. F. Inhibition of morphine analgesia by lithium: Role of peripheral and central opioid receptors. Behav. Brain Res. 151(1–2):151–158; 2004. Jope, R. S. Anti-bipolar therapy: Mechanism of action of lithium. Mol. Psychiatry 4(2):117–128; 1999. Jope, R. S. Lithium and GSK-3: One inhibitor, two inhibitory actions, multiple outcomes. Trends Pharmacol. Sci. 24(9):441–443; 2003. Jope, R. S.; Bijur, G. N. Mood stabilizers, glycogen synthase kinase-3beta and cell survival. Mol. Psychiatry 7(Suppl. 1):S35–45; 2002. Juurlink, D. N.; Mamdani, M. M.; Kopp, A.; Rochon, P. A.; Shulman, K. I.; Redelmeier, D. A. Drug-induced lithium toxicity in the elderly: A population-based study. J. Am. Geriatr. Soc. 52(5):794–798; 2004. Kang, H. J.; Noh, J. S.; Bae, Y. S.; Gwag, B. J. Calciumdependent prevention of neuronal apoptosis by lithium ion: Essential role of phosphoinositide 3-kinase and phospholipase Cgamma. Mol. Pharmacol. 64(2):228–234; 2003. Kanwar, K. C.; Raina, P. Heavy lithium ingestion and haematological changes in rats. J. Environ. Pathol. Toxicol. Oncol. 8(7 Spec. No.):1–5; 1988. Karege, F.; Perroud, N.; Burkhardt, S.; Schwald, M.; Ballmann, E.; La Harpe, R.; Malafosse, A. Alteration in kinase activity but not in protein levels of protein kinase B and glycogen synthase kinase-3beta in ventral prefrontal cortex of depressed suicide victims. Biol. Psychiatry 61(2):240–245; 2007. Katona, C. L. Psychotropics and drug interactions in the elderly patient. Int. J. Geriatr. Psychiatry 16(Suppl. 1): S86–90; 2001. Kaya, N.; Resmi, H.; Ozerdem, A.; Guner, G.; Tunca, Z. Increased inositol-monophosphatase activity by lithium treatment in bipolar patients. Prog. Neuropsychopharmacol. Biol. Psychiatry 28(3):521–527; 2004. Kelwala, S.; Pomara, N.; Stanley, M.; Sitaram, N.; Gershon, S. Lithium-induced accentuation of extrapyramidal symptoms in individuals with Alzheimer’s disease. J. Clin. Psychiatry 45(8):342–344; 1984. Kielczykowska, M.; Pasternak, K.; Musik, I.; Wroniska, J. The effect of lithium administration in a diet on the chosen parameters of the antioxidant barrier in rats. Ann. Univ. Mariae. Curie. Sklodowska. [Med.] 59(2):140– 145; 2004. Kieszek, S. [Trials and perspectives in pharmacotherapy of Alzheimer’s disease]. Psychiatr. Pol. 33(3):331–340; 1999. Kim, J. S.; Chang, M. Y.; Yu, I. T.; Kim, J. H.; Lee, S. H.; Lee, Y. S.; Son, H. Lithium selectively increases neuronal differentiation of hippocampal neural progeni- 19 155. 156. 157. 158. 159. 160. 161. 162. 163. 164. 165. 166. 167. 168. 169. 170. tor cells both in vitro and in vivo. J. Neurochem. 89(2): 324–336; 2004. Kim, K. H.; Song, M. J.; Yoo, E. J.; Choe, S. S.; Park, S. D.; Kim, J. B. Regulatory role of glycogen synthase kinase 3 for transcriptional activity of ADD1/SREBP1c. J. Biol. Chem. 279(50):51999–52006; 2004. Kirschenbaum, F.; Hsu, S. C.; Cordell, B.; McCarthy, J. V. Glycogen synthase kinase-3beta regulates presenilin 1 C-terminal fragment levels. J. Biol. Chem. 276(33): 30701–30707; 2001. Koike, T.; Uno, S.; Ishizawa, M.; Takahashi, H.; Ikeda, K.; Yokota, S.; Makishima, M. The heat shock protein inhibitor KNK437 induces neurite outgrowth in PC12 cells. Neurosci. Lett. 410(3):212–217; 2006. Koletzko, B.; Wendel, U.; Bremer, H. J. Lithium for treatment of neutropenia in glycogen storage disease type Ib. J. Pediatr. 109(5):902–904; 1986. Kopnisky, K. L.; Chalecka-Franaszek, E.; GonzalezZulueta, M.; Chuang, D. M. Chronic lithium treatment antagonizes glutamate-induced decrease of phosphorylated CREB in neurons via reducing protein phosphatase 1 and increasing MEK activities. Neuroscience 116(2): 425–435; 2003. Kravos, M.; Malesic, I.; Levanic, S. Serum alcohol dehydrogenase levels in patients with mental disorders. Clin. Chim. Acta 361(1–2):86–94; 2005. Krawetz, R.; Kelly, G. M. Wnt6 induces the specification and epithelialization of F9 embryonal carcinoma cells to primitive endoderm. Cell. Signal. 20(3):506–517; 2008. Ksiezak-Reding, H.; Pyo, H. K.; Feinstein, B.; Pasinetti, G. M. Akt/PKB kinase phosphorylates separately Thr212 and Ser214 of tau protein in vitro. Biochim. Biophys. Acta 1639(3):159–168; 2003. Kwon, O.; Kim, K. A.; He, L.; Kim, S. O.; Kim, M. S.; Cha, E. Y.; Yoon, B. D.; Sok, D. E.; Jung, M.; Ahn, J. S.; Kim, B. Y. Ionizing radiation can induce GSK3beta phosphorylation and NF-kappaB transcriptional transactivation in ATM-deficient fibroblasts. Cell. Signal. 20(4):602–612; 2008. Laeng, P.; Pitts, R. L.; Lemire, A. L.; Drabik, C. E.; Weiner, A.; Tang, H.; Thyagarajan, R.; Mallon, B. S.; Altar, C. A. The mood stabilizer valproic acid stimulates GABA neurogenesis from rat forebrain stem cells. J. Neurochem. 91(1):238–251; 2004. Lang, E. J.; Davis, S. M. Lithium neurotoxicity: The development of irreversible neurological impairment despite standard monitoring of serum lithium levels. J. Clin. Neurosci. 9(3):308–309; 2002. Ledoux, J. M. Effects on the serotoninergic system in sub-acute transmissible spongiform encephalopathies: Current data, hypotheses, suggestions for experimentation. Med. Hypotheses 64(5):910–918; 2005. Ledoux, J. M. Features of the comparative pharmacokinetics of lithium; a potential application of its use in livestock farming. Med. Hypotheses 61(2):278–281; 2003. Ledoux, J. M. Hypothesis of interference to superinfection between bovine spastic paresis and bovine spongiform encephalopathy; suggestions for experimentation, theoretical and practical interest. Med. Hypotheses 62(3): 346–353; 2004. Lee, S. H.; Sohn, J. W.; Ahn, S. C.; Park, W. S.; Ho, W. K. Li+ enhances GABAergic inputs to granule cells in the rat hippocampal dentate gyrus. Neuropharmacology 46(5): 638–646; 2004. Leng, Y.; Liang, M. H.; Ren, M.; Marinova, Z.; Leeds, 20 171. 172. 173. 174. 175. 176. 177. 178. 179. 180. 181. 182. 183. 184. 185. 186. YOUNG P.; Chuang, D. M. Synergistic neuroprotective effects of lithium and valproic acid or other histone deacetylase inhibitors in neurons: Roles of glycogen synthase kinase-3 inhibition. J. Neurosci. 28(10):2576–2588; 2008. Levine, S.; Saltzman, A. Inhibition of experimental allergic encephalomyelitis by lithium chloride: Specific effect or nonspecific stress? Immunopharmacology 22(3):207– 213; 1991. Levine, S.; Saltzman, A. Lithium increases body weight of rats: Relation to thymolysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 30(1):155–158; 2006. Levine, S.; Saltzman, A. Lithium increases gastrointestinal tract weight of male or female rats but it increases body weight only in females. Prog. Neuropsychopharmacol. Biol. Psychiatry 32(1):29–33; 2008. Levitt, L. J.; Quesenberry, P. J. The effect of lithium on murine hematopoiesis in a liquid culture system. N. Engl. J. Med. 302(13):713–719; 1980. Li, X.; Bijur, G. N.; Jope, R. S. Glycogen synthase kinase-3beta, mood stabilizers, and neuroprotection. Bipolar Disord. 4(2):137–144; 2002. Liang, M. H.; Wendland, J. R.; Chuang, D. M. Lithium inhibits Smad3/4 transactivation via increased CREB activity induced by enhanced PKA and AKT signaling. Mol. Cell. Neurosci. 37(3):440–453; 2008. Licastro, F.; Chiricolo, M.; Tabacchi, P.; Barboni, F.; Zannotti, M.; Franceschi, C. Enhancing effect of lithium and potassium ions on lectin-induced lymphocyte proliferation in aging and Down’s syndrome subjects. Cell. Immunol. 75(1):111–121; 1983. Lin, C. F.; Chen, C. L.; Chiang, C. W.; Jan, M. S.; Huang, W. C.; Lin, Y. S. GSK-3beta acts downstream of PP2A and the PI 3-kinase-Akt pathway, and upstream of caspase-2 in ceramide-induced mitochondrial apoptosis. J. Cell Sci. 120(Pt. 16):2935–2943; 2007. Lin, D.; Mok, H.; Yatham, L. N. Polytherapy in bipolar disorder. CNS Drugs 20(1):29–42; 2006. Lochhead, P. A.; Coghlan, M.; Rice, S. Q.; Sutherland, C. Inhibition of GSK-3 selectively reduces glucose-6phosphatase and phosphatase and phosphoenolypyruvate carboxykinase gene expression. Diabetes 50(5):937–946; 2001. Lovell, M. A.; Xiong, S.; Xie, C.; Davies, P.; Markesbery, W. R. Induction of hyperphosphorylated tau in primary rat cortical neuron cultures mediated by oxidative stress and glycogen synthase kinase-3. J. Alzheimers Dis. 6(6):659–681; 2004. Maca, R. D. The effects of prostaglandins on the proliferation of cultured human T lymphocytes. Immunopharmacology 6(4):267–277; 1983. Maesaka, J. K.; Wolf-Klein, G.; Piccione, J. M.; Ma, C. M. Hypouricemia, abnormal renal tubular urate transport, and plasma natriuretic factor(s) in patients with Alzheimer’s disease. J. Am. Geriatr. Soc. 41(5):501–506; 1993. Manji, H. K.; Bitran, J. A.; Masana, M. I.; Chen, G. A.; Hsiao, J. K.; Risby, E. D.; Rudorfer, M. V.; Potter, W. Z. Signal transduction modulation by lithium: cell culture, cerebral microdialysis and human studies. Psychopharmacol. Bull. 27(3):199–208; 1991. Manji, H. K.; Moore, G. J.; Chen, G. Lithium at 50: Have the neuroprotective effects of this unique cation been overlooked? Biol. Psychiatry 46(7):929–940; 1999. Manji, H. K.; Moore, G. J.; Chen, G. Lithium up-regulates the cytoprotective protein Bcl-2 in the CNS in vivo: 187. 188. 189. 190. 191. 192. 193. 194. 195. 196. 197. 198. 199. 200. 201. 202. A role for neurotrophic and neuroprotective effects in manic depressive illness. J. Clin. Psychiatry 61(Suppl. 9):82–96; 2000. Mao, Z.; Liu, L.; Zhang, R.; Li, X. Lithium reduces FoxO3a transcriptional activity by decreasing its intracellular content. Biol. Psychiatry 62(12):1423–1430; 2007. Masoliver, E.; Menoyo, A.; Perez, V.; Volpini, V.; Rio, E. D.; Perez, J.; Alvarez, E.; Baiget, M. Serotonin transporter linked promoter (polymorphism) in the serotonin transporter gene may be associated with antidepressantinduced mania in bipolar disorder. Psychiatr. Genet. 16(1):25–29; 2006. Mayan, H.; Golubev, N.; Dinour, D.; Farfel, Z. Lithium intoxication due to carbamazepine-induced renal failure. Ann. Pharmacother. 35(5):560–562; 2001. Mazlo, M.; Pataky, I.; Szucs, R. Morphological study of the kidneys of lithium treated rats. Acta Morphol. Hung. 31(4):309–314; 1983. McKenzie, G.; Ward, G.; Stallwood, Y.; Briend, E.; Papadia, S.; Lennard, A.; Turner, M.; Champion, B.; Hardingham, G. E. Cellular Notch responsiveness is defined by phosphoinositide 3-kinase-dependent signals. BMC Cell Biol. 7:10; 2006. McKnelly, Jr., W. V.; Tupin, J. P.; Dunn, M. Lithium in hazardous circumstances with one case of lithium toxicity. Compr. Psychiatry 11(3):279–286; 1970. Messiha, F. S. Effect of pre and postnatal lithium chloride ingestion on the developing mouse. Vet. Hum. Toxicol. 28(6):554–556; 1986. Messiha, F. S. Lithium and the neonate: Developmental and metabolic aspects. Alcohol 3(2):107–112; 1986. Michelon, L.; Meira-Lima, I.; Cordeiro, Q.; Miguita, K.; Breen, G.; Collier, D.; Vallada, H. Association study of the INPP1, 5HTT, BDNF, AP-2beta and GSK-3beta gene variants and restrospectively scored response to lithium prophylaxis in bipolar disorder. Neurosci. Lett. 403(3): 288–293; 2006. Miodownik, C.; Hausmann, M.; Frolova, K.; Lerner, V. Lithium intoxication associated with intramuscular ziprasidone in schizoaffective patients. Clin. Neuropharmacol. 28(6):295–297; 2005. Misiuta, I. E.; Saporta, S.; Sanberg, P. R.; Zigova, T.; Willing, A. E. Influence of retinoic acid and lithium on proliferation and dopaminergic potential of human NT2 cells. J. Neurosci. Res. 83(4):668–679; 2006. Monkul, E. S.; Malhi, G. S.; Soares, J. C. Anatomical MRI abnormalities in bipolar disorder: Do they exist and do they progress? Aust. N. Z. J. Psychiatry 39(4):222– 226; 2005. Moore, G. J.; Bebchuk, J. M.; Hasanat, K.; Chen, G.; Seraji-Bozorgzad, N.; Wilds, I. B.; Faulk, M. W.; Koch, S.; Glitz, D. A.; Jolkovsky, L.; Manji, H. K. Lithium increases N-acetyl-aspartate in the human brain: In vivo evidence in support of bcl-2’s neurotrophic effects? Biol. Psychiatry 48(1):1–8; 2000. Mora, A.; Gonzalez-Polo, R. A.; Fuentes, J. M.; Soler, G.; Centeno, F. Different mechanisms of protection against apoptosis by valproate and Li+. Eur. J. Biochem. 266(3):886–891; 1999. Mora, A.; Sabio, G.; Alonso, J. C.; Soler, G.; Centeno, F. Different dependence of lithium and valproate on PI3K/PKB pathway. Bipolar Disord. 4(3):195–200; 2002. Mora, A.; Sabio, G.; Gonzalez-Polo, R. A.; Cuenda, A.; Alessi, D. R.; Alonso, J. C.; Fuentes, J. M.; Soler, G.; Centeno, F. Lithium inhibits caspase 3 activation and de- REVIEW OF LITHIUM EFFECTS ON BRAIN AND BLOOD phosphorylation of PKB and GSK3 induced by K+ deprivation in cerebellar granule cells. J. Neurochem. 78(1): 199–206; 2001. 203. Mora, A.; Sabio, G.; Risco, A. M.; Cuenda, A.; Alonso, J. C.; Soler, G.; Centeno, F. Lithium blocks the PKB and GSK3 dephosphorylation induced by ceramide through protein phosphatase-2A. Cell. Signal. 14(6):557–562; 2002. 204. Morhenn, V. B.; Orenberg, E. K.; Kaplan, J.; Pfendt, E.; Terrell, C.; Engleman, E. G. Inhibition of a Langerhans cell-mediated immune response by treatment modalities useful in psoriasis. J. Invest. Dermatol. 81(1):23–27; 1983. 205. Morris, A. J.; Storey, D. J.; Downes, C. P.; Michell, R. H. Dephosphorylation of 1D-myo-inositol 1,4-bisphosphate in rat liver. Biochem. J. 254(3):655–660; 1988. 206. Moskowitz, A. S.; Altshuler, L. Increased sensitivity to lithium-induced neurotoxicity after stroke: A case report. J. Clin. Psychopharmacol. 11(4):272–273; 1991. 207. Mudher, A.; Shepherd, D.; Newman, T. A.; Mildren, P.; Jukes, J. P.; Squire, A.; Mears, A.; Drummond, J. A.; Berg, S.; MacKay, D.; Asuni, A. A.; Bhat, R.; Lovestone, S. GSK-3beta inhibition reverses axonal transport defects and behavioural phenotypes in Drosophila. Mol. Psychiatry 9(5):522–530; 2004. 208. Mudo, G.; Jiang, X. H.; Timmusk, T.; Bindoni, M.; Belluardo, N. Change in neurotrophins and their receptor mRNAs in the rat forebrain after status epilepticus induced by pilocarpine. Epilepsia 37(2):198–207; 1996. 209. Munoz-Montano, J. R.; Lim, F.; Moreno, F. J.; Avila, J.; Diaz-Nido, J. Glycogen synthase kinase-3 modulates neurite outgrowth in cultured neurons: Possible implications for neurite pathology in Alzheimer’s disease. J. Alzheimers Dis. 1(6):361–378; 1999. 210. Muzina, D. J. Divalproex and lithium are similarly cost effective for adults with bipolar disorder. Evid. Based Ment. Health 9(1):15; 2006. 211 Muzina, D. J.; Momah, C.; Eudicone, J. M.; Pikalov, A.; McQuade, R. D.; Marcus, R. N.; Sanchez, R.; Carlson, B. X. Aripiprazole monotherapy in patients with rapidcycling bipolar I disorder: An analysis from a long-term, double-blind, placebo-controlled study. Int. J. Clin. Pract. 62(5):679–687; 2008. 212. Naranjo, C. A.; Herrmann, N.; Mittmann, N.; Bremner, K. E. Recent advances in geriatric psychopharmacology. Drugs Aging 7(3):184–202; 1995. 213. Nathwani, D.; Green, S. T. Lithium for zidovudineinduced neutropenia in AIDS. JAMA 262(6):775–776; 1989. 214. Ness-Abramof, R.; Apovian, C. M. Drug-induced weight gain. Drugs Today (Barc.) 41(8):547–555; 2005. 215. Nigou, J.; Besra, G. S. Characterization and regulation of inositol monophosphatase activity in Mycobacterium smegmatis. Biochem. J. 361(Pt. 2):385–390; 2002. 216. Nonaka, S.; Hough, C. J.; Chuang, D. M. Chronic lithium treatment robustly protects neurons in the central nervous system against excitotoxicity by inhibiting Nmethyl-D-aspartate receptor-mediated calcium influx. Proc. Natl. Acad. Sci. USA 95(5):2642–2647; 1998. 217. Nonaka, S.; Katsube, N.; Chuang, D. M. Lithium protects rat cerebellar granule cells against apoptosis induced by anticonvulsants, phenytoin and carbamazepine. J. Pharmacol. Exp. Ther. 286(1):539–547; 1998. 218. Nunes, P. V.; Forlenza, O. V.; Gattaz, W. F. Lithium and risk for Alzheimer’s disease in elderly patients with bipolar disorder. Br. J. Psychiatry 190:359–360; 2007. 21 219. Oakley, P. W.; Whyte, I. M.; Carter, G. L. Lithium toxicity: An iatrogenic problem in susceptible individuals. Aust. N. Z. J. Psychiatry 35(6):833–840; 2001. 220. O’Donnell, T.; Rotzinger, S.; Nakashima, T. T.; Hanstock, C. C.; Ulrich, M.; Silverstone, P. H. Chronic lithium and sodium valproate both decrease the concentration of myoinositol and increase the concentration of inositol monophosphates in rat brain. Eur. Neuropsychopharmacol. 13(3):199–207; 2003. 221. Orgogozo, J. M.; Loiseau, P. [Teratogenic and oncogenic effects of central nervous system drugs]. Rev. Prat. 27(35):2225–2233; 1977. 222. Palacino, J. J.; Murphy, M. P.; Murayama, O.; Iwasaki, K.; Fujiwara, M.; Takashima, A.; Golde, T. E.; Wolozin, B. Presenilin 1 regulates beta-catenin-mediated transcription in a glycogen synthase kinase-3-independent fashion. J. Biol. Chem. 276(42):38563–38569; 2001. 223. Parthasarathy, L.; Vadnal, R. E.; Ramesh, T. G.; Shyamaladevi, C. S.; Parthasarathy, R. myo-inositol monophosphatase from rat testes: Purification and properties. Arch. Biochem. Biophys. 304(1):94–101; 1993. 224. Parthasarathy, L. K.; Seelan, R. S.; Wilson, M. A.; Vadnal, R. E.; Parthasarathy, R. N. Regional changes in rat brain inositol monophosphatase 1 (IMPase 1) activity with chronic lithium treatment. Prog. Neuropsychopharmacol. Biol. Psychiatry 27(1):55–60; 2003. 225. Patel, S.; Martinez-Ripoll, M.; Blundell, T. L.; Albert, A. Structural enzymology of Li(+)-sensitive/Mg(2+)-dependent phosphatases. J. Mol. Biol. 320(5):1087–1094; 2002. 226. Paves, H.; Neuman, T.; Metsis, M.; Saarma, M. Nerve growth factor-induced rapid reorganization of microfilaments in PC12 cells: Possible roles of different second messenger systems. Exp. Cell Res. 186(2):218–226; 1990. 227. Pazdur, R.; Rossof, A. H. Cytotoxic chemotherapy for cancer in Felty’s syndrome: Role of lithium carbonate. Blood 58(3):440–443; 1981. 228. Perez, M.; Hernandez, F.; Lim, F.; Diaz-Nido, J.; Avila, J. Chronic lithium treatment decreases mutant tau protein aggregation in a transgenic mouse model. J. Alzheimers Dis. 5(4):301–308; 2003. 229. Perez, M.; Rojo, A. I.; Wandosell, F.; Diaz-Nido, J.; Avila, J. Prion peptide induces neuronal cell death through a pathway involving glycogen synthase kinase 3. Biochem. J. 372(Pt. 1):129–136; 2003. 230. Perez-Cruet, J.; Dancey, J. T. Thymus gland involution induced by lithium chloride. Experientia 33(5):646–648; 1977. 231. Phelan, K. M.; Mosholder, A. D.; Lu, S. Lithium interaction with the cyclooxygenase 2 inhibitors rofecoxib and celecoxib and other nonsteroidal anti-inflammatory drugs. J. Clin. Psychiatry 64(11):1328–1334; 2003. 232. Phiel, C. J.; Wilson, C. A.; Lee, V. M.; Klein, P. S. GSK3alpha regulates production of Alzheimer’s disease amyloid-beta peptides. Nature 423(6938):435–439; 2003. 233. Piwien-Pilipuk, G.; Van Mater, D.; Ross, S. E.; MacDougald, O. A.; Schwartz, J. Growth hormone regulates phosphorylation and function of CCAAT/enhancer-binding protein beta by modulating Akt and glycogen synthase kinase-3. J. Biol. Chem. 276(22):19664–19671; 2001. 234. Planel, E.; Yasutake, K.; Fujita, S. C.; Ishiguro, K. Inhibition of protein phosphatase 2A overrides tau protein kinase I/glycogen synthase kinase 3 beta and cyclindependent kinase 5 inhibition and results in tau hyper- 22 235. 236. 237. 238. 239. 240. 241. 242. 243. 244. 245. 246. 247. 248. YOUNG phosphorylation in the hippocampus of starved mouse. J. Biol. Chem. 276(36):34298–34306; 2001. Post, R. M. Role of BDNF in bipolar and unipolar disorder: Clinical and theoretical implications. J. Psychiatr. Res. 41(12):979–990; 2007. Presse, F.; Cardona, B.; Borsu, L.; Nahon, J. L. Lithium increases melanin-concentrating hormone mRNA stability and inhibits tyrosine hydroxylase gene expression in PC12 cells. Brain Res. Mol. Brain Res. 52(2):270–283; 1997. Prickaerts, J.; Moechars, D.; Cryns, K.; Lenaerts, I.; van Craenendonck, H.; Goris, I.; Daneels, G.; Bouwknecht, J. A.; Steckler, T. Transgenic mice overexpressing glycogen synthase kinase 3beta: A putative model of hyperactivity and mania. J. Neurosci. 26(35):9022–9029; 2006. Ragan, C. I.; Watling, K. J.; Gee, N. S.; Aspley, S.; Jackson, R. G.; Reid, G. G.; Baker, R.; Billington, D. C.; Barnaby, R. J.; Leeson, P. D. The dephosphorylation of inositol 1,4-bisphosphate to inositol in liver and brain involves two distinct Li+-sensitive enzymes and proceeds via inositol 4-phosphate. Biochem. J. 249(1):143–148; 1988. Rametti, A.; Esclaire, F.; Yardin, C.; Terro, F. Linking alterations in tau phosphorylation and cleavage during neuronal apoptosis. J. Biol. Chem. 279(52):54518–54528; 2004. Rantamaki, T.; Knuuttila, J. E.; Hokkanen, M. E.; Castren, E. The effects of acute and long-term lithium treatments on trkB neurotrophin receptor activation in the mouse hippocampus and anterior cingulate cortex. Neuropharmacology 50(4):421–427; 2006. Rao, R.; Zhang, M. Z.; Zhao, M.; Cai, H.; Harris, R. C.; Breyer, M. D.; Hao, C. M. Lithium treatment inhibits renal GSK-3 activity and promotes cyclooxygenase 2dependent polyuria. Am. J. Physiol. Renal Physiol. 288(4):F642–649; 2005. Ratz Bravo, A. E.; Egger, S. S.; Crespo, S.; Probst, W. L.; Krahenbuhl, S. Lithium intoxication as a result of an interaction with rofecoxib. Ann. Pharmacother. 38(7–8): 1189–1193; 2004. Reimers, A.; Skogvoll, E.; Sund, J. K.; Spigset, O. Drug interactions between lamotrigine and psychoactive drugs: Evidence from a therapeutic drug monitoring service. J. Clin. Psychopharmacol. 25(4):342–348; 2005. Richman, C. M.; Makii, M. M.; Weiser, P. A.; Herbst, A. L. The effect of lithium carbonate on chemotherapyinduced neutropenia and thrombocytopenia. Am. J. Hematol. 16(4):313–323; 1984. Ridgway, D.; Wolff, L. J.; Neerhout, R. C. Enhanced lymphocyte response to PHA among leukemia patients taking oral lithium carbonate. Cancer Invest. 4(6):513– 517; 1986. Risby, E. D.; Hsiao, J. K.; Manji, H. K.; Bitran, J.; Moses, F.; Zhou, D. F.; Potter, W. Z. The mechanisms of action of lithium. II. Effects on adenylate cyclase activity and beta-adrenergic receptor binding in normal subjects. Arch. Gen. Psychiatry 48(6):513–524; 1991. Robinson, W. A.; Entringer, M. A.; Huber, J.; Gupta, R. In vivo and in vitro effects of lithium on granulopoiesis in human neutropenic disorders. Adv. Exp. Med. Biol. 127:281–291; 1980. Rosenstein, E. D.; Kramer, N. Felty’s and pseudo-Felty’s syndromes. Semin. Arthritis Rheum. 21(3):129–142; 1991. 249. Rowe, M. K.; Chuang, D. M. Lithium neuroprotection: Molecular mechanisms and clinical implications. Expert Rev. Mol. Med. 6(21):1–18; 2004. 250. Rybakowski, J. K.; Suwalska, A.; Czerski, P. M.; Dmitrzak-Weglarz, M.; Leszczynska-Rodziewicz, A.; Hauser, J. Prophylactic effect of lithium in bipolar affective illness may be related to serotonin transporter genotype. Pharmacol. Rep. 57(1):124–127; 2005. 251. Rybakowski, J. K.; Suwalska, A.; Skibinska, M.; Dmitrzak-Weglarz, M.; Leszczynska-Rodziewicz, A.; Hauser, J. Response to lithium prophylaxis: Interaction between serotonin transporter and BDNF genes. Am. J. Med. Genet. B. Neuropsychiatr. Genet. 144(6):820–823; 2007. 252. Ryder, J.; Su, Y.; Liu, F.; Li, B.; Zhou, Y.; Ni, B. Divergent roles of GSK3 and CDK5 in APP processing. Biochem. Biophys. Res. Commun. 312(4):922–929; 2003. 253. Sanchez, S.; Sayas, C. L.; Lim, F.; Diaz-Nido, J.; Avila, J.; Wandosell, F. The inhibition of phosphatidylinositol3-kinase induces neurite retraction and activates GSK3. J. Neurochem. 78(3):468–481; 2001. 254. Sang, H.; Lu, Z.; Li, Y.; Ru, B.; Wang, W.; Chen, J. Phosphorylation of tau by glycogen synthase kinase 3beta in intact mammalian cells influences the stability of microtubules. Neurosci. Lett. 312(3):141–144; 2001. 255. Sarkar, S.; Floto, R. A.; Berger, Z.; Imarisio, S.; Cordenier, A.; Pasco, M.; Cook, L. J.; Rubinsztein, D. C. Lithium induces autophagy by inhibiting inositol monophosphatase. J. Cell Biol. 170(7):1101–1111; 2005. 256. Sarkar, S.; Krishna, G.; Imarisio, S.; Saiki, S.; O’Kane, C. J.; Rubinsztein, D. C. A rational mechanism for combination treatment of Huntington’s disease using lithium and rapamycin. Hum. Mol. Genet. 17(2):170–178; 2008. 257. Sartori, H. E. Lithium orotate in the treatment of alcoholism and related conditions. Alcohol 3(2):97–100; 1986. 258. Sasaki, T.; Saito, S.; Aihara, M.; Ohsawa, J.; Ikezawa, Z. Exacerbation of psoriasis during lithium treatment. J. Dermatol. 16(1):59–63; 1989. 259. Sassi, R. B.; Brambilla, P.; Hatch, J. P.; Nicoletti, M. A.; Mallinger, A. G.; Frank, E.; Kupfer, D. J.; Keshavan, M. S.; Soares, J. C. Reduced left anterior cingulate volumes in untreated bipolar patients. Biol. Psychiatry 56(7):467–475; 2004. 260. Scarffe, J. H.; Chang, J. Failure of lithium to reduce period of neutropenia during induction therapy of acute myeloid leukemia. Hematol. Oncol. 7(1):69–75; 1989. 261. Schafer, M.; Goodenough, S.; Moosmann, B.; Behl, C. Inhibition of glycogen synthase kinase 3 beta is involved in the resistance to oxidative stress in neuronal HT22 cells. Brain Res. 1005(1–2):84–89; 2004. 262. Schubert, T.; Muller, W. E. Lithium but not cholinergic ligands influence guanylate cyclase activity in intact human lymphocytes. Biochem. Pharmacol. 39(3):439–444; 1990. 263. Schubert, T.; Stoll, L.; Muller, W. E. Therapeutic concentrations of lithium and carbamazepine inhibit cGMP accumulation in human lymphocytes. A clinical model for a possible common mechanism of action? Psychopharmacology (Berl.) 104(1):45–50; 1991. 264. Schulz, C.; Mavrogiorgou, P.; Schroter, A.; Hegerl, U.; Juckel, G. Lithium-induced EEG changes in patients with affective disorders. Neuropsychobiology 42(Suppl. 1):33–37; 2000. 265. Schumacher, G. E. Using pharmacokinetics in drug ther- REVIEW OF LITHIUM EFFECTS ON BRAIN AND BLOOD 266. 267. 268. 269. 270. 271. 272. 273. 274. 275. 276. 277. 278. 279. 280. 281. apy. VII: Pharmacokinetic factors influencing drug therapy in the aged. Am. J. Hosp. Pharm. 37(4):559–562; 1980. Senatorov, V. V.; Ren, M.; Kanai, H.; Wei, H.; Chuang, D. M. Short-term lithium treatment promotes neuronal survival and proliferation in rat striatum infused with quinolinic acid, an excitotoxic model of Huntington’s disease. Mol. Psychiatry 9(4):371–385; 2004. Serretti, A.; Artioli, P. Predicting response to lithium in mood disorders: Role of genetic polymorphisms. Am. J. Pharmacogenomics 3(1):17–30; 2003. Serretti, A.; Malitas, P. N.; Mandelli, L.; Lorenzi, C.; Ploia, C.; Alevizos, B.; Nikolaou, C.; Boufidou, F.; Christodoulou, G. N.; Smeraldi, E. Further evidence for a possible association between serotonin transporter gene and lithium prophylaxis in mood disorders. Pharmacogenomics J. 4(4):267–273; 2004. Severus, W. E.; Kleindienst, N.; Seemuller, F.; Frangou, S.; Moller, H. J.; Greil, W. What is the optimal serum lithium level in the long-term treatment of bipolar disorder—a review? Bipolar Disord. 10(2):231–237; 2008. Sgarabotto, D.; Dazzi, F.; Girolami, A. Lithium carbonate failed to modify the neutropenia associated with large granular lymphocyte proliferation. Acta Haematol. 81(2): 114–115; 1989. Shamir, A.; Shaltiel, G.; Agam, G. Intracerebroventricular antisense to inositol monophosphatase-1 reduces enzyme activity but does not affect Li-sensitive behavior. Prog. Neuropsychopharmacol. Biol. Psychiatry 26(1): 103–106; 2002. Shastry, B. S. Bipolar disorder: An update. Neurochem. Int. 46(4):273–279; 2005. Shenkman, L.; Borkowsky, W.; Shopsin, B. Lithium as an immunologic adjuvant. Med. Hypotheses 6(1):1–6; 1980. Shenkman, L.; Wadler, S.; Borkowsky, W.; Shopsin, B. Adjuvant effects of lithium chloride on human mononuclear cells in suppressor-enriched and suppressor-depleted systems. Immunopharmacology 3(1):1–8; 1981. Shim, M.; Smart, R. C. Lithium stabilizes the CCAAT/ enhancer-binding protein alpha (C/EBPalpha) through a glycogen synthase kinase 3 (GSK3)-independent pathway involving direct inhibition of proteasomal activity. J. Biol. Chem. 278(22):19674–19681; 2003. Shopsin, B.; Friedmann, R.; Gershon, S. Lithium and leukocytosis. Clin. Pharmacol. Ther. 12(6):923–928; 1971. Silva, R.; Martins, L.; Longatto-Filho, A.; Almeida, O. F.; Sousa, N. Lithium prevents stress-induced reduction of vascular endothelium growth factor levels. Neurosci. Lett. 429(1):33–38; 2007. Silva, R.; Mesquita, A. R.; Bessa, J.; Sousa, J. C.; Sotiropoulos, I.; Leao, P.; Almeida, O. F.; Sousa, N. Lithium blocks stress-induced changes in depressive-like behavior and hippocampal cell fate: The role of glycogensynthase-kinase-3beta. Neuroscience 152(3):656–669; 2007. Silver, B. J.; Zuckerman, K. S. Aplastic anemia: Recent advances in pathogenesis and treatment. Med. Clin. North Am. 64(4):607–629; 1980. Silverstone, P. H.; Bell, E. C.; Willson, M. C.; Dave, S.; Wilman, A. H. Lithium alters brain activation in bipolar disorder in a task- and state-dependent manner: An fMRI study. Ann. Gen. Psychiatry 4:14; 2005. Silverstone, P. H.; Wu, R. H.; O’Donnell, T.; Ulrich, M.; 23 282. 283. 284. 285. 286. 287. 288. 289. 290. 291. 292. 293. 294. 295. 296. Asghar, S. J.; Hanstock, C. C. Chronic treatment with lithium, but not sodium valproate, increases cortical Nacetyl-aspartate concentrations in euthymic bipolar patients. Int. Clin. Psychopharmacol. 18(2):73–79; 2003. Sinha, D.; Wang, Z.; Ruchalski, K. L.; Levine, J. S.; Krishnan, S.; Lieberthal, W.; Schwartz, J. H.; Borkan, S. C. Lithium activates the Wnt and phosphatidylinositol 3-kinase Akt signaling pathways to promote cell survival in the absence of soluble survival factors. Am. J. Physiol. Renal Physiol. 288(4):F703–713; 2005. Slamenova, D.; Budayova, E.; Gabelova, A.; Moravkova, A.; Panikova, L. Results of genotoxicity testing of mazindol (degonan), lithium carbonicum (contemnol) and dropropizine (ditustat) in Chinese hamster V79 and human EUE cells. Mutat. Res. 169(3):171–177; 1986. Slavin, S.; Liang, M. H. Cell mediated autoimmune granulocytopenia in a case of Felty’s syndrome. Ann. Rheum. Dis. 39(4):399–402; 1980. Slordal, L.; Samstad, S.; Bathen, J.; Spigset, O. A lifethreatening interaction between lithium and celecoxib. Br. J. Clin. Pharmacol. 55(4):413–414; 2003. Son, H.; Yu, I. T.; Hwang, S. J.; Kim, J. S.; Lee, S. H.; Lee, Y. S.; Kaang, B. K. Lithium enhances long-term potentiation independently of hippocampal neurogenesis in the rat dentate gyrus. J. Neurochem. 85(4):872–881; 2003. Sparsa, A.; Bonnetblanc, J. M. [Lithium]. Ann. Dermatol. Venereol. 131(3):255–261; 2004. Sporn, A.; Gogtay, N.; Ortiz-Aguayo, R.; Alfaro, C.; Tossell, J.; Lenane, M.; Gochman, P.; Rapoport, J. L. Clozapine-induced neutropenia in children: Management with lithium carbonate. J. Child Adolesc. Psychopharmacol. 13(3):401–404; 2003. Sproule, B. Lithium in bipolar disorder: Can drug concentrations predict therapeutic effect? Clin. Pharmacokinet. 41(9):639–660; 2002. Stein, R. S.; Flexner, J. H.; Graber, S. E. Lithium and granulocytopenia during induction therapy of acute myelogenous leukemia: Update of an ongoing trial. Adv. Exp. Med. Biol. 127:187–197; 1980. Stein, R. S.; Flexner, J. M.; Graber, S. E. Lithium and granulocytopenia during induction therapy of acute myelogenous leukemia. Blood 54(3):636–641; 1979. Stieglitz, K. A.; Johnson, K. A.; Yang, H.; Roberts, M. F.; Seaton, B. A.; Head, J. F.; Stec, B. Crystal structure of a dual activity IMPase/FBPase (AF2372) from Archaeoglobus fulgidus. The story of a mobile loop. J. Biol. Chem. 277(25):22863–22874; 2002. Stoothoff, W. H.; Johnson, G. V. Hyperosmotic stressinduced apoptosis and tau phosphorylation in human neuroblastoma cells. J. Neurosci. Res. 65(6):573–582; 2001. St-Pierre, L. S.; Persinger, M. A. Extreme obesity in female rats following prepuberal induction of lithium-pilocarpine seizures and a single injection of acepromazine. Epilepsy Behav. 7(3):411–418; 2005. Su, H.; Chu, T. H.; Wu, W. Lithium enhances proliferation and neuronal differentiation of neural progenitor cells in vitro and after transplantation into the adult rat spinal cord. Exp. Neurol. 206(2):296–307; 2007. Su, Y.; Ryder, J.; Li, B.; Wu, X.; Fox, N.; Solenberg, P.; Brune, K.; Paul, S.; Zhou, Y.; Liu, F.; Ni, B. Lithium, a common drug for bipolar disorder treatment, regulates amyloid-beta precursor protein processing. Biochemistry 43(22):6899–6908; 2004. 24 297. Sun, A.; Shanmugam, I.; Song, J.; Terranova, P. F.; Thrasher, J. B.; Li, B. Lithium suppresses cell proliferation by interrupting E2F-DNA interaction and subsequently reducing S-phase gene expression in prostate cancer. Prostate 67(9):976–988; 2007. 298. Sun, X.; Sato, S.; Murayama, O.; Murayama, M.; Park, J. M.; Yamaguchi, H.; Takashima, A. Lithium inhibits amyloid secretion in COS7 cells transfected with amyloid precursor protein C100. Neurosci. Lett. 321(1–2): 61–64; 2002. 299. Sutton, L. P.; Honardoust, D.; Mouyal, J.; Rajakumar, N.; Rushlow, W. J. Activation of the canonical Wnt pathway by the antipsychotics haloperidol and clozapine involves dishevelled-3. J. Neurochem. 102(1):153–169; 2007. 300. Takada, Y.; Fang, X.; Jamaluddin, M. S.; Boyd, D. D.; Aggarwal, B. B. Genetic deletion of glycogen synthase kinase-3beta abrogates activation of IkappaBalpha kinase, JNK, Akt, and p44/p42 MAPK but potentiates apoptosis induced by tumor necrosis factor. J. Biol. Chem. 279(38):39541–39554; 2004. 301. Takahashi, H.; Higuchi, H.; Shimizu, T. Severe lithium toxicity induced by combined levofloxacin administration. J. Clin. Psychiatry 61(12):949–950; 2000. 302. Takebayashi, M.; Hisaoka, K.; Nishida, A.; Tsuchioka, M.; Miyoshi, I.; Kozuru, T.; Hikasa, S.; Okamoto, Y.; Shinno, H.; Morinobu, S.; Yamawaki, S. Decreased levels of whole blood glial cell line-derived neurotrophic factor (GDNF) in remitted patients with mood disorders. Int. J. Neuropsychopharmacol. 9(5):607–612; 2006. 303. Tanquary, J. Lithium neurotoxicity at therapeutic levels in an AIDS patient. J. Nerv. Ment. Dis. 181(8):518–519; 1993. 304. Tisman, G.; Herbert, V.; Rosenblatt, S. Evidence that lithium induces human granulocyte proliferation: elevated serum vitamin B 12 binding capacity in vivo and granulocyte colony proliferation in vitro. Br. J. Haematol. 24(6):767–771; 1973. 305. Tong, H.; Imahashi, K.; Steenbergen, C.; Murphy, E. Phosphorylation of glycogen synthase kinase-3beta during preconditioning through a phosphatidylinositol-3kinase-dependent pathway is cardioprotective. Circ. Res. 90(4):377–379; 2002. 306. Tricklebank, M. D.; Singh, L.; Jackson, A.; Oles, R. J. Evidence that a proconvulsant action of lithium is mediated by inhibition of myo-inositol phosphatase in mouse brain. Brain Res. 558(1):145–148; 1991. 307. Tsai, S. J. Is mania caused by overactivity of central brain-derived neurotrophic factor? Med. Hypotheses 62(1):19–22; 2004. 308. Tseng, W. P.; Lin-Shiau, S. Y. Long-term lithium treatment prevents neurotoxic effects of beta-bungarotoxin in primary cultured neurons. J. Neurosci. Res. 69(5):633– 641; 2002. 309. Tsuji, S.; Morinobu, S.; Tanaka, K.; Kawano, K.; Yamawaki, S. Lithium, but not valproate, induces the serine/ threonine phosphatase activity of protein phosphatase 2A in the rat brain, without affecting its expression. J. Neural. Transm. 110(4):413–425; 2003. 310. Turner, A. R.; MacDonald, R. N.; McPherson, T. A. Reduction of chemotherapy-induced neutropenic complications with a short course of lithium carbonate. Clin. Invest. Med. 2(1):51–53; 1979. 311. Unlap, M. T.; Jope, R. S. Lithium attenuates nerve YOUNG 312. 313. 314. 315. 316. 317. 318. 319. 320. 321. 322. 323. 324. 325. 326. growth factor-induced activation of AP-1 DNA binding activity in PC12 cells. Neuropsychopharmacology 17(1): 12–17; 1997. Vacek, A.; Sikulova, J.; Bartonickova, A. Radiation resistance in mice increased following chronic application of Li2CO3. Acta Radiol. Oncol. 21(5):325–330; 1982. Vacheron-Trystram, M. N.; Braitman, A.; Cheref, S.; Auffray, L. [Antipsychotics in bipolar disorders]. Encephale 30(5):417–424; 2004. van Eijsden, P.; Notenboom, R. G.; Wu, O.; de Graan, P. N.; van Nieuwenhuizen, O.; Nicolay, K.; Braun, K. P. In vivo 1H magnetic resonance spectroscopy, T2-weighted and diffusion-weighted MRI during lithium-pilocarpineinduced status epilepticus in the rat. Brain Res. 1030(1): 11–18; 2004. Van Gassen, G.; De Jonghe, C.; Nishimura, M.; Yu, G.; Kuhn, S.; St George-Hyslop, P.; Van Broeckhoven, C. Evidence that the beta-catenin nuclear translocation assay allows for measuring presenilin 1 dysfunction. Mol. Med. 6(7):570–580; 2000. Verdoux, H.; Bourgeois, M. [Irreversible neurologic sequelae caused by lithium]. Encephale 17(3):221–224; 1991. Verma, D. S.; Johnston, D. A.; McCredie, K. B. Evidence for the separate human T-lymphocyte subpopulations that collaborate with autologous monocyte/macrophages in the elaboration of colony-stimulating activity and those that suppress this collaboration. Blood 62(5): 1088–1099; 1983. Verma, D. S.; Spitzer, G.; Gutterman, J. U.; Beran, M.; Zander, A. R.; McCredie, K. B. Human leukocyte interferon-mediated granulopoietic differentiation arrest and its abrogation by lithium carbonate. Am. J. Hematol. 12(1):39–46; 1982. Verma, D. S.; Spitzer, G.; Zander, A. R.; Dicke, K. A.; McCredie, K. B. Cyclic neutropenia and T lymphocyte suppression of granulopoiesis: Abrogation of the neutropenic cycles by lithium carbonate. Leuk. Res. 6(4):567– 576; 1982. Vieta, E. The treatment of mixed states and the risk of switching to depression. Eur. Psychiatry 20(2):96–100; 2005. Volonte, C.; Ciotti, M. T.; Merlo, D. LiCl promotes survival of GABAergic neurons from cerebellum and cerebral cortex: LiCl induces survival of GABAergic neurons. Neurosci. Lett. 172(1–2):6–10; 1994. von Schulthess, G. K.; Fehr, J.; Dahinden, C. Cyclic neutropenia: Amplification of granulocyte oscillations by lithium and long-term suppression of cycling by plasmapheresis. Blood 62(2):320–326; 1983. Wahlin, A.; von Knorring, L.; Roos, G. Altered distribution of T lymphocyte subsets in lithium-treated patients. Neuropsychobiology 11(4):243–246; 1984. Walz, J. C.; Frey, B. N.; Andreazza, A. C.; Cereser, K. M.; Cacilhas, A. A.; Valvassori, S. S.; Quevedo, J.; Kapczinski, F. Effects of lithium and valproate on serum and hippocampal neurotrophin-3 levels in an animal model of mania. J. Psychiatr. Res. 42(5):416–421; 2007. Watanabe, S.; Taguchi, K.; Nakashima, Y.; Ebara, T.; Iguchi, K. Leukocytosis during lithium treatment and its correlation to serum lithium level. Folia Psychiatr. Neurol. Jpn. 28(3):161–165; 1974. Weetman, A. P.; McGregor, A. M.; Lazarus, J. H.; Smith, B. R.; Hall, R. The enhancement of immunoglob- REVIEW OF LITHIUM EFFECTS ON BRAIN AND BLOOD 327. 328. 329. 330. 331. 332. 333. 334. 335. ulin synthesis by human lymphocytes with lithium. Clin. Immunol. Immunopathol. 22(3):400–407; 1982. Wei, H.; Leeds, P. R.; Qian, Y.; Wei, W.; Chen, R.; Chuang, D. beta-amyloid peptide-induced death of PC 12 cells and cerebellar granule cell neurons is inhibited by long-term lithium treatment. Eur. J. Pharmacol. 392(3): 117–123; 2000. Weiner, M. L.; Batt, K. J.; Putman, D. L.; Curren, R. D.; Yang, L. L. Genotoxicity evaluation of lithium hypochlorite. Toxicology 65(1–2):1–22; 1990. Wexler, E. M.; Geschwind, D. H.; Palmer, T. D. Lithium regulates adult hippocampal progenitor development through canonical Wnt pathway activation. Mol. Psychiatry 13(3):285–292; 2008. Williams, G. O. Management of depression in the elderly. Prim. Care 16(2):451–474; 1989. Wilson, R.; Fraser, W. D.; McKillop, J. H.; Smith, J.; O’Reilly, D. S.; Thomson, J. A. The [in vitro” effects of lithium on the immune system. Autoimmunity 4(1–2): 109–114; 1989. Wilson, R.; McKillop, J. H.; Crocket, G. T.; Pearson, C.; Jenkins, C.; Burns, F.; Burnett, A. K.; Thomson, J. A. The effect of lithium therapy on parameters thought to be involved in the development of autoimmune thyroid disease. Clin. Endocrinol. (Oxf.) 34(5):357–361; 1991. Wilting, I.; Movig, K. L.; Moolenaar, M.; Hekster, Y. A.; Brouwers, J. R.; Heerdink, E. R.; Nolen, W. A.; Egberts, A. C. Drug-drug interactions as a determinant of elevated lithium serum levels in daily clinical practice. Bipolar Disord. 7(3):274–280; 2005. Woodgett, J. R. Physiological roles of glycogen synthase kinase-3: potential as a therapeutic target for diabetes and other disorders. Curr. Drug Targets Immune Endocr. Metabol. Disord. 3(4):281–290; 2003. Worthington, M. Lack of effect of lithium carbonate on 25 336. 337. 338. 339. 340. 341. 342. zidovudine-associated neutropenia in patients with AIDS. J. Infect. Dis. 162(3):777–778; 1990. Wysocki, H.; Rybakowski, J.; Wierusz-Wysocka, B.; Szajnerman, Z.; Michta, G.; Kapelski, Z. Influence of lithium on neutrophil granulocyte distribution and turnover. Folia Haematol. Int. Mag. Klin. Morphol. Blutforsch. 108(4):533–538; 1981. Xavier, I. J.; Mercier, P. A.; McLoughlin, C. M.; Ali, A.; Woodgett, J. R.; Ovsenek, N. Glycogen synthase kinase 3beta negatively regulates both DNA-binding and transcriptional activities of heat shock factor 1. J. Biol. Chem. 275(37):29147–29152; 2000. Yasuda, S.; Liang, M. H.; Marinova, Z.; Yahyavi, A.; Chuang, D. M. The mood stabilizers lithium and valproate selectively activate the promoter IV of brainderived neurotrophic factor in neurons. Mol. Psychiatry 14(1):51–59; 2009. Yu, I. T.; Kim, J. S.; Lee, S. H.; Lee, Y. S.; Son, H. Chronic lithium enhances hippocampal long-term potentiation, but not neurogenesis, in the aged rat dentate gyrus. Biochem. Biophys. Res. Commun. 303(4):1193–1198; 2003. Yung, C. Y. A review of clinical trials of lithium in medicine. Pharmacol. Biochem. Behav. 21(Suppl. 1):51–55; 1984. Zarate, Jr., C. A.; Quiroz, J. A.; Singh, J. B.; Denicoff, K. D.; De Jesus, G.; Luckenbaugh, D. A.; Charney, D. S.; Manji, H. K. An open-label trial of the glutamate-modulating agent riluzole in combination with lithium for the treatment of bipolar depression. Biol. Psychiatry 57(4): 430–432; 2005. Zhang, R.; Villeret, V.; Lipscomb, W. N.; Fromm, H. J. Kinetics and mechanisms of activation and inhibition of porcine liver fructose-1,6-bisphosphatase by monovalent cations. Biochemistry 35(9):3038–3043; 1996.