Educational Objectives TG113: Improving Treatment Consistency and Data Quality for Clinical Trials
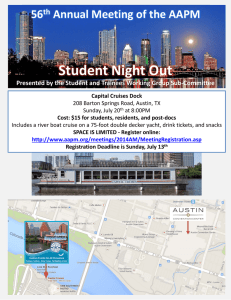
advertisement

TG113: Improving Treatment Consistency and Data Quality for Clinical Trials Educational Objectives 1. 2. Jean M. Moran, Ph.D. To describe the goals of TG#113: Physics Practice Standards for Clinical Trials To highlight some factors that directly impact clinical trials that involve IMRT and IGRT The University of Michigan Department of Radiation Oncology AAPM 2007 Moran AAPM 2008 2 Task Group 113 Members Robert Dryzmala Jon Kruse Jean Moran (Chair) Art Olch Mark Oldham Robert Jeraj Outline Liaisons James Galvin – RTOG Andrea Molineu – RPC Jatinder Palta – RCET, TG100 James Purdy – ITC Marcia Urie – QARC Moran AAPM 2008 3 Motivation Challenges for multi-institutional trials Factors impacting clinical trials Examples for imaging, localization Role of benchmarks Summary Moran AAPM 2008 4 1 Motivation Expected Users of TG113 Physics QA for clinical trials Physicists & Others Assure consistency in each part of the treatment planning and delivery process Advanced Technology Consortium ITC, QARC, RCET, RTOG, and RPC Organizations provide QA services and some trial and benchmark design However, there are no standard guidelines for the physics aspects of clinical trials Implement trials at department level Involved in all parts of the treatment planning and delivery process Can significantly improve data consistency if guidelines are available QA Organizations Credentialing Benchmarks - Dry run, phantom Moran AAPM 2008 5 Cooperative Groups Trial Design Make trials more specific with respect to physics aspects Vendors Data export: Dosimetric, imaging, localization Dose calculation quality – heterogeneity corrections Plan assessment tools Delivery software and devices Equipment Moran AAPM 2008 6 Factors Impacting Data for Clinical Trials Factors Impacting Data for Clinical Trials Patient immobilization Patient immobilization Imaging for Volume definition Imaging for Volume definition Patient localization: Setup accuracy Patient localization: Setup accuracy Treatment planning Treatment planning Treatment guidance Treatment guidance Treatment delivery Treatment delivery Moran AAPM 2008 7 What is the clinical trial designed to study? What are the clinical endpoints? What data are collected? What level of accuracy is required for the treatment planning and delivery chain? Will we want to know more later? e.g. NTCP modeling of lung Moran AAPM 2008 8 2 Challenges TG113 Challenges to clinical trials Can changes be made to improve the consistency of clinical trials (better data) without overwhelming: Accrual Time Expense Physics issues are not always explicitly included in the design of clinical trials These exclusions may dilute the quality of data from a clinical trial Imaging Homogeneous vs. heterogeneous dose calculations Patient setup details Physicians and physicists designing clinical trials? The treatment team participating in trials? The QA centers supporting clinical trials? Our work focuses on external beam radiation therapy Moran AAPM 2008 9 Contouring Targets: Effect of Window on Target Volume Moran AAPM 2008 10 Contouring Targets: Effect of Window on Target Volume Bowden et al. IJROBP 53: 566-573, 2002. To improve consistency in trials Protocols can provide guidance for window/gray levels in the trial design Bowden et al. IJROBP 53: 566-573, 2002. Moran AAPM 2008 11 Moran AAPM 2008 12 3 SBRT Dry Run Study: 11 institutions Effect of Delivery Technique Minimum PTV: 35-46 Gy Homogeneity index: 1.05-1.4 Breath hold CT 2 mm slices - lung Matsuo et al. IJROBP 68: 416-425, 2007. Matsuo et al. IJROBP 68: 416-425, 2007. Moran AAPM 2008 13 Moran AAPM 2008 14 Bowden et al. compared mean tumor volume values for volumes drawn with a lung window compared to a mediastinal window for 6 physicians on 6 datasets. Dry Run: SBRT (continued) Inter-institutional variations in planning for SBRT for lung cancer, Matsuo et al. IJROBP, 2007, 416-425 16.6% variation in target volumes Significant differences Treatment delivery technique Dose calculation algorithms The average ratio of the lung window to mediastinal window (LW/MW) was: 25% 1. 25% 2. 25% 3. 25% 4. 100% (no difference) 120% 150% 180% Chose to use 1-D methods rather than mix; recalc with CVSP when available ATC supporting digital data submission 10 Moran AAPM 2008 15 Moran AAPM 2008 16 4 Patient Immobilization and Localization To improve consistency in clinical trials: Contouring instructions must be explicit A range of acceptable values can be given Treatment planning guidelines must be explicit (1) Intra-fraction reproducibility (2) Inter-fraction variations over the course of treatment (3) Inter-institutional variations Frequency of assessment Surrogates for tumor position One size fits all may not be appropriate target and OAR margins Some trials specify dose-volume constraints and minor and major variations Moran AAPM 2008 17 Moran AAPM 2008 18 Initial Position: Prostate setup assessed from imaging 3 gold BBs What is the true delivered dose? Do we know? How can we interpret the data? Moran AAPM 2008 19 Prone 4 LR AP IS 2 0 -2 -4 1 2 3 4 5 6 Ave Patient # Supine Position (cm) Should a single margin be specified for all trials? What about immobilization? What about imaging protocol? Is it off-line or adaptive? Is it daily or weekly? Should clinics use the same margin because the patient is on a multi-institutional trial even if their methods are different? Position (cm) What margin should be used in the clinical trial? Litzenberg et al. 4 2 0 -2 -4 7 8 9 Patient # 10 Ave Moran AAPM 2008 20 5 Position (cm) Final Position: Patient setup assessed based on imaging 3 gold BBs Prone Treatment Guidance 4 2 LR AP IS 0 -2 -4 2 1 3 4 5 6 Ave Supine Position (cm) Patient # Image guidance methods Cameras RF beacons kV fluoroscopic imaging MV cine loops Type of intervention depends on the frequency of the event 4 2 Real-time evaluation is needed to address intra-fraction motion Fiducials 0 -2 -4 7 8 9 10 Ave Patient # Litzenberg et al. Moran AAPM 2008 21 Example: Image Guidance – HN MVCT: Bony anatomy registration Moran AAPM 2008 22 Example: Treatment Guidance Error As a Function of % Image Guidance • 3 transponders 100 Error > 3 mm Error > 5 mm Error > 10 mm % of Times Error Occurs 90 80 • Implanted transrectally under ultrasound guidance 70 60 50 • 10 minute procedure 40 30 • Consistent with gold marker implant effects 20 10 • Good positional stability over 8 weeks (σave = 0.8 mm) 0 0 10 20 30 40 50 60 70 80 90 100 % Image Guidance Slide courtesy of Zeidan MDACC-Orlando, (IJROBP, 2007) Moran AAPM 2008 23 Slide courtesy of Litzenberg Moran AAPM 2008 24 6 Prostate: Necessary PTV margin PTV Margin (mm) 12 IS AP LR 10 8 To improve consistency in trials: Margins should be based on each institution’s image guidance protocols Or The trial should specify the acceptable methods and frequency of interventions 6 4 2 0 Skin Marks Skin Marks + Motion Initial Setup Pre-Beam Intra-fraction Correction Correction Litzenberg Int J Radiat Oncol Biol Phys 2006 Patient enrollment information should include immobilization method and localization information Frequency Action level Moran AAPM 2008 25 Treatment Delivery Moran AAPM 2008 26 Credentialing for Clinical Trials Does it matter if the treatment is: Facility questionnaire Delivered with a conventional Linac or something else (Tomotherapy, Cyberknife)? Static, IMRT, or arc delivery? Is motion management needed? Some part of the credentialing process may be dependent on delivery technique Process appropriate margins can be used incorporating other factors Moran AAPM 2008 27 Information about department, equipment and software used for patient care Dry run Hard copy or electronic submission of a treatment plan that intends to meet the guidelines of the protocol Additional testing depends on the trial and QA organization Benchmarks, e.g. phantom irradiation Moran AAPM 2008 28 7 Importance of Credentialing RPC: IMRT H&N Phantom Results RPC: IMRT H&N Phantom •Primary PTV 4 cm diameter 4 TLD •Secondary PTV 2 cm diameter 2 TLD •Organ at risk 1 cm diameter 2 TLD •Axial and sagittal radiochromic films • 163 irradiations were analyzed • 115 irradiations passed the criteria • 28 institutions irradiated multiple times Primary PTV Secondary PTV Organ at Risk •1º PTV treated to 6.6 Gy •2º PTV treated to 5.4 Gy •OAR limited to < 4.5 Gy • 48 irradiations did not pass the criteria • 128 institutions are represented ~30% of institutions fail the criteria on the first irradiation. Designed in collaboration with RTOG; Molineu et al, IJROBP, October 2005 Courtesy of Molineu, RPC Moran AAPM 2008 29 RPC: Explanations for Failures Explanation Min # of occurrences Incorrect output factors in TPS 1 Incorrect PDD in TPS 1 Inadequacies in beam modeling at leaf ends (Cadman, et al; PMB 2002) 14 Not adjusting MU to account for dose differences measured with ion chamber 3 Errors in couch indexing with Peacock system 2 2 mm tolerance on MLC leaf position 1 Setup errors 7 Target malfunction 1 Courtesy of Molineu, RPC Courtesy of Molineu, RPC Moran AAPM 2008 30 Effect of Leaf Position Offset on IMRT Cadman et al PMB: 3001-3010 (2002). Moran AAPM 2008 31 Moran AAPM 2008 32 8 The number institutions who pass the benchmark irradiation of the RPC head and neck phantom is: Effect of Leaf Position Offset on IMRT Uncorrected leaf offset -3-12% errors 25% 1. 25% 2. 25% 3. 25% 4. Leaf offset corrected +/- 5% 5% 10% 30% 45% 10 Cadman et al PMB: 3001-3010 (2002). Moran AAPM 2008 33 Inaccuracy in the modeling of curved multileaf collimator leaves was shown to result in dosimetric errors up to: 25% 1. 25% 2. 25% 3. 25% 4. 2% 12% 25% 30% Moran AAPM 2008 34 To improve consistency in clinical trials There is a clear role for dosimetric verification when complex technologies are being introduced RPC phantom found dosimetric errors that would have adversely affected trial results Request immobilization and setup information as part of patient enrollment on a clinical trial 10 Moran AAPM 2008 35 Moran AAPM 2008 36 9 How should new technologies be incorporated into clinical trials? We do not want to limit participation in clinical trials, but we do want delivery to be as accurate as possible Results should also represent how patients will be treated in a variety of hospital settings Focus is on physics issues that affect the consistency of data acquired during clinical trials Expect improved confidence in the data submitted as part of a clinical trial Should improve interpretation of studies looking at tissue response Moran AAPM 2008 37 TG 113 Summary Emphasis on process improvements to decrease the variability in clinical trials (and improve our knowledge of differences) Design of trials: Allow for variable margins based on immobilization and localization methods Continue to require credentialing as new technologies are implemented at different centers and as benchmarks continue to show significant failures Looking forward: Trials on treatment assessment We are in the process of completing our written report for submission to Therapy Physics Committee and then submission for publication. Moran AAPM 2008 38 10