PET Site Planning and Radiation Safety Practice of PET Shielding in 2000:
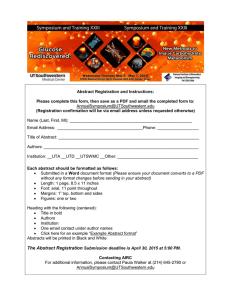
advertisement

Practice of PET Shielding in 2000: First We Had Chaos PET Site Planning and Radiation Safety Jon A. Anderson, PhD Department of Radiology The University of Texas Southwestern Medical Center at Dallas AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 1 July 2006 -- AAPM Annual Meeting Excerpts from a web discussion thread on shielding control areas at PET facilities: "...requirements were determined to be 1" and 1/2" of lead..." "...we don't have any special shielding..." "...most do not shield the control room..." "...this leads to lead thicknesses...of about 2 cm..." "...we don't have any lead shielding..." "...we have 2 mm Pb in the walls..." "... we have ...a lead glass window ... 1/4" of lead shielding on this wall..." AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 2 What Is Different When You Have PET or PET/CT in Your Facility? Then We Had TG-108 1) 511 keV energy -increases exposure rate from doses, patients -greatly increases thickness of required shielding 2)Requirements for patient handling during injection and uptake phase 3) Combined modality scanners (PET/CT) require consideration of both gamma-ray and x-ray hazard Med. Phys. 33(1),January 2006 AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 3 AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 4 1 The 18F-Injected Patient as a Source (average of different investigators, 2003) µSv/hr)/MBq Superior 0.075 (µ 0.279 (mrem/hr)/mCi #HVL's all at 1 m from surface of body, average value from all applicable reports Lateral A Revealing Comparison of Lead Requirements: X-Ray vs PET Lead Thickness Required mm (in) Anterior 0.104 (µ µSv/hr)/MBq 0.383 (mrem/hr)/mCi 0.103 (µ µSv/hr)/MBq 0.383 (mrem/hr)/mCi not as anisotropic as it might seem 0.018 (µ µSv/hr)/MBq Inferior 0.065 (mrem/hr)/mCi 5 30-60 min AAPM Annual Meeting, 2006 PET Facility Tour: University of Texas Southwestern Medical Center at Dallas * Assay of dose Radioactive Materials Uptake of pharmaceutical Dock 10-60 min Position Pt * Scan QA Check of Scan Scan Utility Future Camera Office 1 Room Reading Room East Corridor Have Pt empty bladder Release Pt 6 Receive doses Injection of Pt Transport Pt to scanner 10 min jon.anderson@utsouthwestern.edu * * steps with highest technologist exposure Hot Toilet Hot Lab Injection Scan Room 1 #2 Injection #1 Scan Room 2 Control South Corridor Arrival of patient 5.3 (1/4) 9.9 (7/16) 19.0 (3/4) 32.5 (1 5/16) 46.0 (1 13/16) Even a single halfvalue layer for PET is an expensive proposition! 1. NCRP 147: Structural Shielding Design for Medical X-Ray Imaging Facilities 2. Simpkin, 2004, developed for AAPM Task Group on PET Facility Shielding Workflow at the PET Center (FDG Whole Body Scans) Pt instruction and prep 0.044 (< 1/16) 0.103 (< 1/16) 0.278 (< 1/16) 0.718 (< 1/16) 1.366 (< 1/16) 1 2 4 8 10 compare this to 0.014 (µ µSv/hr)/MBq or 0.05 (mrem/hr)/mCi for 99mTc: factor of 8! jon.anderson@utsouthwestern.edu PET2 Laundry AAPM Annual Meeting, 2006 X-ray 1 (average primary for rad room) West Corridor Storage Read study Break Room Office 3 Office 2 Patients Business Office Reception & Waiting Print for file and referring; distribute to PACS AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 7 AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 8 2 Hot Lab Details: Dose Storage alternative W Area transport carrier AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu Notes: 1) Floor protection (containers weigh > 66 lbs) 2) Space needed depends on how often deliveries are made; may have >100 mCi here at a time, even for one scanner 3) Extra shielding may be required 9 Hot Lab Details Hot Lab Details: Dose Assay and Preparation Area Notes: 1) Calibrator convenient to dose storage 2) L Block close to calibrator 3) Note use of special PET carrier for syringe 4) Note L Block: thick window, 2" lead, 2" lead wrap-around AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 10 Injection Room Details, UTSW Notes: 1) Injection room Hot lab PET/CT bay are most likely areas to need shielding Notes: 1) All this lead requires solid support -- have a heart-toheart talk with the cabinet maker 2) Counter mount of calibrator decreases tech exposure 3) Extra shielding required on well counter to shield from sources in scanner, calibration sources, patient in scanner, etc. 4) Use tungsten syringe shields for dose reduction to fingers. AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 11 2) To minimize anomalous uptake -minimize external stimuli (false uptake!) -keep patient quiet and still on gurney or in injection chair 3) Need adjacent hot toilet for patients to use after uptake period. AAPM Annual Meeting, 2006 4) Indirect lighting,curtains, noise control are desirable jon.anderson@utsouthwestern.edu 12 3 Scan Bay: PET and PET/CT Imaging - uses rotating isotopic sources in gantry to make attenuation correction - 70 % E/30% T time split - typical 15 cm axial FOV - 2D or 3D acquisitions Conventional PET - uses coupled CT scanner to make attenuation correction - provides auto registration of anatomic and functional images - faster scans through reduced transmission image time AAPM Annual Meeting, 2006 GE Discovery Series Philips GEMINI PET/CT jon.anderson@utsouthwestern.edu 13 Uses of adjacent spaces (including above and below) and occupancy factors for them AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 14 Calculation Formalism Proposed by Task Group B, the required barrier transmission factor, will be calculated as B= # patients/week isotopes to be used, activity/pt types of PET studies to be performed (heads, WB, cardiac) uptake time and scan time for this equipment/study dose delivery schedule (once a day?, multiples?); maximum activity on hand CT technique factors (kVp, mAs/scan [depends of # beds]) # scans per patient (additional diagnostic scans?) amount of "non-PET" CT workload expected jon.anderson@utsouthwestern.edu Siemens Biograph Series You need to know which one you're getting! Site Evaluation for PET Shielding AAPM Annual Meeting, 2006 Current PET/CT Implementations 15 P * d2 Γ * T * Nw * (A0 * F * t * Rt) P = target dose in protected area (per week, hour, etc.) [µ µSv] d = distance to protected point [m] Γ = dose rate constant [(µ µSv/hr)(m2/MBq)] T = occupancy factor (NCRP 147 or specific information) Nw = number of patients per time period corresponding to P A0 = initial activity (patient or point source) at start of integration time [MBq] F = factor encompassing physical decay of the dose prior to time period t = integration time (time the source (patient) is in the room) [hr] Rt = "reduction factor" (accounts for decay during integration period) AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 16 4 P: Radiation Protection Targets N: Maximum Workload Estimation Limitations ALARA per 10CFR20 Action Limit 50 mSv/yr (5000 mrem/yr) Pregnant worker's fetus 5 mSv/9 mo (500 mrem/9 mo) Members of public (from each licensed operation) in any hour, not to exceed 1 mSv/yr (100 mrem/yr) .02 mSv (2 mrem) 1 Hour Uptake, 30 M inute Scan 5 mSv/yr (500 mrem/yr) 16 Targets controlled areas: 0.1 mSv/wk or 10 mrem/wk uncontrolled areas: 0.02 mSv/wk or 2 mrem/wk GUIDANCE: ALARA -- As Low As Reasonably Achievable AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu Patient Number Radiation workers PET Facility Throughput Example: This facility needs two uptake areas 13 10 Phase 7 Uptake 4 Scanning 1 8:00 9:00 10:00 11:00 12:00 13:00 14:00 15:00 16:00 17:00 Time of Day #pts/day = (Twork - Tuptake)/Tscan_rm 17 A0: Example Schedule for 18F FDG Administered Activities for WB will depend on which scanner you have! Scans Weight [kg] Weight [lb] Dose [mCi] Dose [mBq] AAPM Annual Meeting, 2006 Doses (pre-injection) in Hot Lab Calibration sources for scanner 330 20 740 130 286 17.5 648 110 242 15 555 90 198 12.5 462 TX Sources in scanner (PET) 70 154 10 370 CT x-ray source (for PET/CT) jon.anderson@utsouthwestern.edu Patient (post injection, in uptake rm) Patient (in scanner, hot toilet) 19 18 Possible Radiation Sources to Include in the Shielding Plan 150 AAPM Annual Meeting, 2006 # uptake areas = Tuptake/Tscan_rm jon.anderson@utsouthwestern.edu AAPM Annual Meeting, 2006 require isotopic workload parameters require CT x-ray workload factors, including additional (nonPET) CT work jon.anderson@utsouthwestern.edu 20 5 18F: A Plethora of Dose Rate Constants for Point Sources (TG-108) 18F Rate Constants SI Units 15.5 (µ µR/hr) m2/MBq Air Kerma Rate Constant Conventional Units Rate Constants SI Units Conventional Units Exposure Rate Constant 15.5 (µ µR/hr) m2/MBq 0.134 (µ µ Sv/hr) m2/MBq 0.4958 (mrem/hr) m2/mCi Air Kerma Rate Constant 0.134 (µ µ Sv/hr) m2/MBq 0.4958 (mrem/hr) m2/mCi Effective Dose Equivalent (ANS1991) 0.143 (µ µ Sv/hr) m2/MBq 0.5291 (mrem/hr) m2/mCi Effective Dose Equivalent (ANS-1991) 0.143 (µ µ Sv/hr) m2/MBq 0.5291 (mrem/hr) m2/mCi Tissue Dose Constant 0.148 (µ µ Sv/hr) m2/MBq 0.5476 (mrem/hr) m2/mCi Tissue Dose Constant 0.148 (µ µ Sv/hr) m2/MBq 0.5476 (mrem/hr) m2/mCi Deep Dose Equivalent (ANS-1977) 0.183 (µ µ Sv/hr) m2/MBq 0.6771 (mrem/hr) m2/mCi Deep Dose Equivalent (ANS-1977) Maximum Dose (ANS1977) 0.188 (µ µ Sv/hr) m2/MBq 0.6956 (mrem/hr) m2/mCi Maximum Dose (ANS1977) AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 21 HalfLife [min] Photon (511 keV) Intensity per Decay [%] Positron Energy [MeV] γ -Ray Dose [(µ µ Sv/hr)/MBq] ([(mrem/hr)/mCi]) at 1 meter 11 C 20.3 200 0.961 0.194 (0.717) 13 N 9.97 200 1.19 0.194 (0.717) 15 O 2.03 200 1.72 0.194 (0.717) Ge 4.1e5 68 Ga (288 d) 180 1.9, 0.8 0.179 (0.662) 68 Rb 1.25 192 3.35,2.5 0.5735 (mR/hr) m2/mCi 0.6771 recommends (mrem/hr) m2/mCi 0.183 (µ µ Sv/hr) m2/MBqTG-108 0.143 (mSv/hr)/MBq (mrem/hr)/mCi 0.6956 (mrem/hr) m2/mCi 0.188 (µ µ Sv/hr) m2/MBq0.53 for F-18 AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 22 Γ: The 18F-Injected Patient as a Source (retained activity) Γ: Dose Rate Constants from Other Point Source Positron Emitters 82 18F 0.5735 (mR/hr) m2/mCi These values, from Unger and Trubey (ORNL/RSIC-45) are given in µSv of deep dose as defined in 10CFR20. (a somewhat different measure than the Task Group recommended for 18F) Dose Rate from 0.600 Dose Rate [(µ Sv/hr)/MBq] [(mrem/hr)/mCi] Exposure Rate Constant 18F: A Plethora of Dose Rate Constants for Point Sources (TG-108) 0.500 18 F Injected Patient at 1 m sources of variation: delay time to measurement, micturation status, exposure-todose conversion, etc. TG-108 recommends (0.092 µSv/hr)/MBq (0.34 mrem/hr)/mCi 0.400 0.300 0.200 0.100 0.000 White 2000 Yester * 2005 (attenuation) SI Units 0.075 0.055 0.100 0.150 0.137 0.08866 0.097 0.100 Conventional Units 0.279 0.203 0.370 0.553 0.508 0.328 0.359 0.372 Kearfott 1992 0.210 (0.778) Chisea 1997 Cronin 1999 Benetar 2000 Massoth 2003 (unpubl.) Average Source about 20% of dose will be in bladder after 1-2 hours AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 23 AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 24 6 Sources in the Gantry: Isodose Curves from Vendor may need for transmission or calibration in either PET or PET/CT! Correction for Decay: The Reduction Factor Reduction Factor Rt with line source in place with transmission rods extended jon.anderson@utsouthwestern.edu 25 0 t 0.8 0 0 0.6 0.4 0.2 0 0 20 AAPM Annual Meeting, 2006 Dose [mrem] B= Corrected for Physical Decay, Self-Shielding Corrected for Physical Decay, Self-Shielding, Voiding 10 60 80 100 120 140 A factor of 2 = 1/8" of lead jon.anderson@utsouthwestern.edu Inject @ 5 minutes Void @ 60 minutes 0 0 20 40 60 80 100 120 140 160 180 jon.anderson@utsouthwestern.edu 26 B= 10.9 * P * d2 T * Nw * (A0 * F * t * Rt) 10.9 is 1/Γ in [(hr/µSv)(MBq/m2)]; F=1 Image: 12.8 * P * d2 B= T * Nw * (A0 * F * t * Rt) 12.8 includes 15% void before imaging; F=exp(-0.693tU/T1/2), the physical decay during uptake 200 Time [minutes] AAPM Annual Meeting, 2006 200 P * d2 Γ * T * Nw * (A0 * F * t * Rt) 6 2 180 Uptake: 8 4 160 B, the required barrier transmission factor, will be calculated as Initial Activity Corrected for Physical Decay 40 Time [minutes] 18 12 dT A dT Effect of Corrections Cumulative Dose 1 m from Patient, 10 mCi F-18 14 ln( 2) A ⋅e Calculation Formalism Proposed by Task Group: Now We Have It All Effects of Adding Corrections to Dose Calculation 16 T T half 0 1 Cautions: The phantoms for PET and for CT isodose curves do not look very much like patients; the CT values may be for bare CT gantry. AAPM Annual Meeting, 2006 − Correction for Decay of F-18 1.2 R with phantom in place t 27 AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 28 7 Going from Barrier Transmission Monte Carlo to Shield Thickness calculations by Douglas Simpkin (2004) Lead Monte Carlo Simulation (Broad Parallel Beam) 1.0000 Constant TVL 16.6 mm −γ Transmission + B 0.1000 x( B) := 1 α⋅γ ⋅ ln 1+ 0.0100 0.0010 0.0001 0 5 10 15 20 25 30 35 Thickness(mm) AAPM Annual Meeting, 2006 40 45 50 β α β α Curves and fitting parameters for iron and concrete are also found in the report jon.anderson@utsouthwestern.edu 29 Example 2: How Much Shielding for a An uncontrolled area with Scan Room? 100% occupancy is 3m from −6 Protection Goal: P := 20⋅ 10 Distance: d := 3⋅ m Number of Patients per Week: N := 40 Occupancy: T := 1 1hr 6 Activity: Source Duration: t := 0.5hr Reduction Factor: R(t ) = 0.91 Gamma Constant: Γ := .092⋅ 10 −6 ( P⋅ d ( ) ⋅ T half 1 ⋅ 0.85 2 the patient. 40 patients a week are injected with 555 MBq (15 mCi) of FDG and held elsewhere for a 1hr uptake time. The patients void about 15% of the dose at 1 hr. The scan lasts 30 minutes. 2 Sv⋅ m 6 hr⋅ 10 Bq ) xl Br = 0.807cm Br = 0.334 ( ) xc Br = 11.278 cm AAPM Annual Meeting, 2006 P := 20⋅ 10 Distance: d := 4⋅ m Number of Patients per Week: N := 40 Occupancy: T := 1 An uncontrolled area with 100% occupancy is 4m from the patient. 40 patients a week are injected in this room with 555 MBq (15 mCi) of FDG and held for a 1hr uptake time. Sv 6 Activity: A 0 := 555 10 Bq Source Duration: t := 1hr Reduction Factor: R ( t) = 0.831 Gamma Constant: Γ := .092⋅ 10 −6 2 ⋅ Sv⋅ m 6 hr⋅ 10 Bq Br := ( P⋅ d 2 N⋅ T⋅ A 0⋅ R( t ) ⋅ t ⋅ Γ ( ) How much shielding is needed? Br = 0.188 ) xl Br = 1.184 cm ( ) xc Br = 15.165 cm AAPM Annual Meeting, 2006 Ans: 1.2 cm of Pb or 15.2 cm of concrete jon.anderson@utsouthwestern.edu 30 A Shielding Paradigm for Mixed PET/CT Applications (Just a personal opinion) 1) Identify magnitude and location (x,y) of all sources, including CT. Integrate over appropriate decay period that source is in location. Express as dose/wk or dose/hr at one meter, given workload. 2) Identify all barriers that will contribute to shielding, including pigs, shipping containers, etc. How much shielding ? 2 N⋅ T⋅ A 0⋅ R( t) ⋅ t⋅ Γ −6 Protection Goal: Sv A 0 := 555⋅ 10 ⋅ Bq ⋅ Br := Example 1: How Much Shielding for an Uptake Room? Ans: 0.8 cm of Pb or 11.3 cm of concrete jon.anderson@utsouthwestern.edu 31 3) Establish test points (x,y) at perimeter, sensitive locations. Identify which barriers will shield each point. AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 32 8 A Shielding Paradigm (cont) Example Spreadsheet 3) Calculate doses (summed over all sources, including CT) without attenuation. 4) Start adding lead or concrete as necessary to the barriers, recalculating the doses as you go. 5) Stop when you have met goals (100 mrem/yr, 2 mrem/hr) jon.anderson@utsouthwestern.edu be exposed to more than 100 mrem/yr Sx -14.4 -4.43 -17.6 -17.6 -15.9 -8.83 -18.7 -17.8 -22.8 -5.04 source definitions Sy 10.49 8.6 7.77 8.81 8.58 9.88 11 11 6.56 9.11 Total Target mR/wkmR/wk Loc_ID Occupancy Status Area 1 1 OK control 12.66 2 1 OK control 9.05 3 0.25 OK hot lab 7.61 4 1 OK reading room 3.62 5 1 OK reading room 2.03 6 1 OK reading room 2.44 7 1 OK E wall 1.97 8 1 OK E wall 1.81 9 1 OK E wall 1.97 10 1 OK E wall 1.97 11 1 OK E wall 1.74 12 1 OK E wall 1.70 13 1 OK E wall 1.56 14 1 OK E wall 1.41 15 1 OK E wall 1.28 16 1 OK E wall 1.14 17 1 OK E wall 1.13 100 100 100 100 100 100 2 2 2 2 2 2 2 2 2 2 2 test point results A spreadsheet can do all of this (including corrections for anisotropic sources). Special purpose programs can be developed to do the same. Pencil and paper can be used, but it is tedious! AAPM Annual Meeting, 2006 Verification that no member of the public will avg per hour Input Data Source XRate@1m 1 scan1 3.15 2 scan2 2.6 3 inj 1 3.8 4 inj 2 3.8 5 phan 1 1.1 6 phan 2 1.1 7 lab 54 8 hot_ws 0.13 9 bath 0.45 10 CT NPETSources 9 PathID 1 2 3 4 33 Grid Calculation: No Shielding XConst Source Area 3.15 scan1 control 2.60 scan2 control 3.80 inj 1 control 3.80 inj 2 control 511 Calculation Matl Mu/Rho Rho Mu Concrete 0.0877 1.84 0.1614 Lead 0.161 11.34 1.8257 Lead tranmissions for CT Calc (NCRP49) d[cm] B 0 1 0.159 2.63E-03 0.3180 5.47E-05 0.4760 1.09E-06 0.6350 1.00E-06 shielding material definitions Tot/Targ Ratio 0.12664 0.09049 0.0761 0.03618 0.02026 0.02444 0.98403 0.90567 0.98286 0.98251 0.86885 0.85039 0.77788 0.70582 0.64054 0.57104 0.56277 Tx -10.83 -9.60 -17.84 -12.80 -10.99 -9.60 -20.12 -18.29 -16.46 -14.63 -12.80 -10.97 -9.14 -7.32 -5.49 -3.66 -1.83 Ty 10.06 8.23 11.52 15.55 17.36 15.55 18.29 18.29 18.29 18.29 18.29 18.29 18.29 18.29 18.29 18.29 18.29 -7 -6 -5 -4 -3 -2 -1 0 1 2 3 4 5 6 7 8 0 0 0 0 2.54 3.105 2.54 0 0.159 0.159 0.636 0.636 0.636 0.159 0.318 0.636 0 0 0 0 0 0 0 0 0 0 0 90 0 0 0 0 0 0 0 0 0 0 0 0 0 0 0 1.571 B7 B8 barrier definitions B4 CT Calculation CT Angle 320 degrees CT mAs/hr 40000 mAs Exposure Tolerance: Barrier# Thick Orient q[rad] n [cm] B2 B3 Loc_IDOccupancy Length θ[rad] TotReqL,WTotL, NS d(concreted(lead)B1 1 1 3.57595 3.021053 1.02 1.12 0 0.16 1 1 1 6.56442 6.058898 0.92 1.02 0 0.163 2 1 1 7.12787 3.468667 0.66 1.23 0 0.84 5 1 1 1 6.86477 3.324703 0.68 1.23 0 0.809 4 1 AAPM Annual Meeting, 2006 Buildup Factor Coefficients B2 B1 B0 0.049 0.473 0.994 -0.01 0.198 1.05 B5 B6 1 Comment 1 1 4 4 4 1 2 4 L-Block PET-Net shipping case + local shield 1" lead storage case no barriers counted n control s control s hot lab s inj 2 s inj 1 n inj area s scan 2 e hot lab barriers for each test point jon.anderson@utsouthwestern.edu 34 Grid Calculation: Shielded Office/Lab Inj C Scan T H Corridor Reading Office/Lab Corridor Lobby Elevator Elevator Reading Y image Ratio of calculated dose to target dose, adjusted for occupancy DoseToTargetRatio DoseToTargetRatio Sources: Injection room, HL, HWC, Scanner, CT, Cal Source 4 pts/day, 1 hr in uptake, 2 hrs in scan room AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 35 No shielding in walls in excess of 5/16" Pb AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 36 9 A Suggested Design Philosophy Look Up, Down, and Sideways Electrical Electrical Corridor Elevator, Lobby Corridor Mechanical Space Mechanical Space Glass Wash Exterior Floor Plan AAPM Annual Meeting, 2006 -Keep the hot areas in interior of space, away from adjacent, uncontrolled occupancies to reduce shielding requirement Relative Dose Map on Floor Above jon.anderson@utsouthwestern.edu 37 Where to Put the Lead: Shadow vs Complete Coverage -Alternatively, place the hot areas against exterior walls adjacent to very low occupancy spaces (exterior landscaping, etc.); may need to control area (fence) -Be prepared to use both inclusive (lead-lined or concrete walls) and spot (shadow) shielding in order to meet protection goals and to minimize lead requirements. AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 38 Examples of Shadow Shields Alternatives: Complete coverage -- like most x-ray shielding -contractors are familiar with technique -facility previously shown had lead thicknesses of 1.6 mm to 6.3 mm, easily managed - makes sense for PET/CT where CT must be shielded Shadow shielding -- big slabs next to trouble spots -can reduce overall cost when thick shield needed - provides flexibility when remodeling old work AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 39 from JA Anderson, RJ Massoth, and LL Windedahl, 2003 AAPM AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 40 10 Magnitude of Technologist Consistent with conventional nuclear medicine Exposure practice, most of technologist dose comes from positioning, transport, and injection. More on Technologist Exposure 1) It is often seen that the technologist dose per mBq handled drops as a function of experience in the PET clinic. Dose/Activity Handled µ Sv/MBq (mrem/mCi) Technologist Doses A 2004 update to the previous UTSW data for the same two technologists as shown on preceding slide showed a normalized WB dose of 0.011 µSv/MBq (0.041 mrem/mCi), down by 40% since 2002. average dose/procedure < 10 µSv (1 mrem) 0.150 0.100 0.050 0.000 Chisea McElroy UTSW Roberts Guillet Biran Yester Average SI Units 0.018 0.012 0.023 0.019 0.019 0.011 0.009 0.029 0.021 0.018 Conventional Units Benetar Chisea 0.067 0.044 0.085 0.069 0.069 0.041 0.032 0.107 0.077 0.066 Reference AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 41 Operating Suggestions to Minimize Technologist Dose Lay out hot lab to minimize handling time. Use unit doses. Complete patient instruction, interaction before injection. Minimize time near patient after injection. Establish IV access with butterfly infusion set before injection. Use other personnel for patient transport. Shield control area to reduce dose during scan. jon.anderson@utsouthwestern.edu AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 42 jon.anderson@utsouthwestern.edu Acknowledgements Use syringe shields, syringe carriers, carts, etc. to reduce exposure during dose transport, injection. AAPM Annual Meeting, 2006 2) Assuming an average dose of 0.018 µSv/MBq injected, 8 pt/day and 370 MBq (10 mCi) injected/pt, this would yield a yearly dose of 13.3 mSv (1330 mrem), within regulation but above usual ALARA investigational limits. Over nine months, it would be 10.4 mSv (1040 mrem), well above the declared pregnancy limit. 43 • • • • • • • • Tammy Pritchett, RT, CNMT Michael Viguet, CNMT Dana Mathews, MD Thomas Lane, PhD Richard Massoth, PhD Larry Windedahl Doug Simpkin, PhD Mark Madsen, PhD AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 44 11 The End AAPM Annual Meeting, 2006 jon.anderson@utsouthwestern.edu 45 12