Gamma Knife and CyberKnife: Physics and Quality Assurance y Q
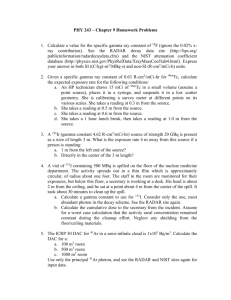
advertisement

Gamma Knife and CyberKnife: y and Quality Q y Assurance Physics David Shepard Swedish Cancer Institute Seattle, WA A k Acknowledgements l d t • • • • • • • • • Cristian Cotrutz , Swedish Cancer Institute Peng Zhang, Hillcrest Medical Center Steven Goetsch, Goetsch San Diego GK Center Paula Petti, Washington Hospital GK Center Jean Régis, g Timone University y Hospital p Bill Main, Accuray Inc. Chad Lee, CK Solutions M tin Murphy, Martin M ph VCU Michelle Lee, Elekta Objectives 1)) To p provide an overview w of f the p physics y of f Gamma Knife and CyberKnife radiosurgery. 2) To review the quality assurance procedures f th for the Gamma G Knife K if and d CyberKnife. C b K if Gamma Knife - Basics • • A treatment unit designed specifically for intracranial radiosurgery. radiosurgery First Gamma Knife built in 1967 under direction of Lars Leksell in Stockholm, Sweden. Leksell Gamma Knife® 269 Units installed Worldwide- May 2009 Europe - 38 N th America North A i - 123 Japan - 52 Middle East-7 China - 17 Other Asia - 31 South America 2 Gamma Knife f Evolution 1968 Model S 1986 Model U 2 delivered 27 delivered Sh ff Sheffield, , Buenos Aires D cr as Decreased Improved mpro body dose collimator design Computer dose planning Courtesy of David Larson 1987 Model B 127 delivered 1999 Model C 2004 Model 4C 2006 Perfexion 152 delivered 49 delivered 36 delivered S m ro ot c Semi-robotic patient positioning Improved dose conformity St in Still n production Improved software M Merge/fusion /f i capability Improved mpro conformity Larger cavity Very low body d dose Rapid treatment Full automation Expert panel Recent Advances in Gamma Knife Technology Model 4C 2006 P f Perfexion 2004 Model 4C Gamma Knife Procedure Step 1: A stereotactic head frame is attached to the patient patient’ss head under local anesthesia. Step 2: The patient is imaged using either MRI or CT with a fiducial box attached to the patient’s stereotactic frame. Step p 3: A treatment plan p is developed. p Step 4: The patient’s stereotactic head f frame is affixed ff d to the h Gamma Knife’s f automatic positioning system. Step 5: The doors to the treatment unit open. The patient is advanced into the shielded hi ld d treatment vault. l • Inside the shielded vault,, the beams from 201 Co-60 sources are focused so that they intersect at a single location. • An elliptical region of high dose is produced with a rapid falloff in dose outside the boundary y of the ellipse. p • Each exposure is referred to as a shot of radiation. • F Four focusing f h helmets l are available. l bl • Each focusing helmet includes 201 collimators that dictate the size of the shot of radiation (4, 8, 14, or 18 mm). Creating g the Treatment Plan (1) • F For sm small ll sspherical h i l llesions, si s th the planning l i is straightforward. p , here a single g 8mm shot • For example, covered the target (6mm in diameter). Creating the Treatment Plan (2) • For tumors that are large or irregularly shaped, the planning process becomes more complex. • These cases typically require several shots of radiation. radiation • Through an iterative trial-and-error approach, the user must determine how many shots h t to t use along l with ith their th i sizes, i locations and weights. M t – 8 shots Met h t (18mm) (18 ) Meningioma – 12 shots h (8mm) ( ) Leksell Gamma Knife® Perfexion™ Gamma Knife Perfexion • Major redesign of the Gamma Knife. Knife • July 2006 – 1st system became operational at Timone University Hospital of Marseille France. • August 2006 - FDA approval Gamma Knife Perfexion Beam Collimation (1) • The most critical change in the Perfexion is the new collimator system. • The new system replaces the multi-helmet collimator setup with a single integrated permanent collimator system that incorporates openings for 4mm, 8mm, and 16mm treatment beams. Gamma Knife Perfexion Beam Collimation (2) • The collimator is partitioned into 8 independently moveable sectors each delivering 24 beams of radiation (192 total sources). • Beam B size i can b be changed h d dynamically d i ll b by sector. • Individual sectors can be blocked to provide further shaping of each shot of radiation. Gamma Knife Perfexion Collimator system 16-16-16-16-16-16-16-16 16 16 16 16 16 16 16 16 Collimator system 8-16-16-16-16-16-16-16 8 16 16 16 16 16 16 16 Collimator system 8-16-8-16-16-16-16-16 8 16 8 16 16 16 16 16 Collimator system 8-16-8-16-8-16-16-16 8 16 8 16 8 16 16 16 Collimator system 8-16-8-16-8-16-8-16 8 16 8 16 8 16 8 16 Single Shot Dynamic Dose Shaping Courtesy of David Larson Positioning g System y Design g • The GK Perfexion positions the patient by moving the couch rather than moving the patient patient’ss head within an APS. • The transition between shot locations is typically under 3 seconds Courtesy of David Larson Perfexion – Key Advantages 11. Improved d patient i throughput. h h 2. Improved patient comfort. 3 Extended anatomical reach. 3. reach Improved Patient Throughput • No helmet changes. changes • The patient no longer needs to moved out of the unit between shots because the beams can b moved be d to the h off ff position. i i Courtesy of Jean Régis Improved Patient Comfort • Increased space p inside collimator m body y leads to reduced patient anxiety. • The need for eccentric frame positioning is eliminated. eliminated Courtesy of Jean Régis Larger Collimator Size Leksell Gamma Knife® PerfexionTM Leksell Gamma Knife® C Extended Anatomical Reach • Most M peripheral p p lesions can now w be treated.. • Elekta is developing a fixation device for cervical spine lesions. • Lesions L i in i and d around d th the paranasall sinuses, i th the orbits, and the cervical spine are now accessible. Courtesy of Jean Régis Decreased Body Dose Compared to Previous GK Models Model B Model C Perfexion Courtesy of David Larson Decreased Body Dose (x10-100) Compared to Other RS Apparatus Cyberknife Corvus Model C Novalis Perfexion Courtesy of David Larson • First Perfexion in US installed at Washington Hospital, Fremont, CA. • First Fi t patient ti t ttreated t dJ June 2007 First Perfexion™ Patient at WHHS 3 Mets,, 1 Run Multi-shot Dose Conformity Courtesy of David Larson Multi-target Multi target Dose Conformity (22 mets) Courtesy of David Larson Gamma Knife eXtend™ • Elekta will soon offer a toolkit for fractionated treatments in the head and upper upper-neck neck region. region • The system will use a stereotactic frame with a vacuum assisted bite block. • The system has received its CE Mark and FDA approval is pending. Expected U.S. release is Octoberr 2009. Octo 9. Gamma Knife eXtend eXtend™ Step 1: A dental imprint is taken. Gamma Knife eXtend eXtend™ Step 2: Patient is set up with the vacuum assisted mouth piece attached to a carbon fiber frame. Gamma Knife eXtend eXtend™ Step 3: A high resolution probe is used to obtain reference distances that will later be used to validate the accuracy of the repositioning at the time of treatment. treatment CT images are then obtained with the fiducial box in place. Gamma Knife eXtend eXtend™ Step 4: At the time of treatment, a reposition check is performed with the data automatically transferred to the Gamma Knife control system. The treatment is then delivered. Gamma Knife Routine Q Quality y Assurance Gamma Knife Routine Q QA Procedures Model 4C or Earlier Daily QA • • • • • Warmup Door interlock Emergency g y off AV communications Radiation monitor Weekly QA • • • • Monthly QA • • • • • Radiation output C mputer output Computer utput vs. vs measured Emergency rod release Medical UPS battery check Ti Timer constancy, st li linearity, it and d accuracy Couch release handle Helmet microswitches Helmet trunions Automatic positioning system accuracy Annual QA • • • Relative helmet factors Isocenter coincidence Film measurements Gamma Knife – APS QA Q Gamma Knife – APS QA Q B Basic QA Tests for f P Perfexion f 1) Coincidence C i id of f the th mechanical h i l iisocenter t of f th the patient--positioning system (PPS) with the patient radiation--focal p radiation point (RFP) ( ) 2) Agreement of measured beam profiles with Leksell GammaPlan calculations for all collimator sizes in the XY, XY YZ and XZ planes 3) Measurement of the absolute dosedose-rate calibration for largest g collimator 4) Confirmation of the relative output factors (ROFs) for smaller collimators. Courtesy of Paula Petti Testing Coincidence Between PPS and RFP • The patient is not positioned via an automatic positioning iti i system t b butt rather th th through h very precise couch motions • Collimator settings (4 (4, 8 and 16) are independent • Therefore, the must check the coincidence of the h PPS PP and d RFP for f each h individual i di id l collimator lli Courtesy of Paula Petti Perfexion - Diode Test Tool Coincidence of PPS and RFP • Attaches to patient frame adapter which then adapter, attaches to the PPS • One central diode • Tool is used to perform scans for all 3 major axes. Courtesy of Paula Petti GK QA Notes • Task Group No. 178 - Gamma Stereotactic Radiosurgery Dosimetry and Quality Assurance p g a calibration • TG-178 is developing protocol for GK units based on ADCL calibrated ionization chambers Courtesy of Paula Petti Additional GK Information at AAPM • TU-E-213A-1 – 4-5:30 PM – “Quality Assurance f th for the Leksell L k ll Gamma G Knife K if Perfexion” P f i ” - Paula P l Petti - Washington Hospital, Fremont, CA • SU-FF-T-532 FF 5 – “Immobilization mm zat n Accuracy ccuracy of fa Novel Re-Locatable Head Frame Investigated with a Real-Time Optical Tracking System” Nazanin Nayebi Nayebi, Princess Margaret Hospital Hospital, Toronto Gamma Knife - Summary • Radiosurgery delivery technique using beams from Co Co-60 60 sources to deliver highly conformal dose distributions. • Well established technology used for treating patients since 1967. • More than 270 units installed worldwide (36 Perfexion systems) with over 500,000 500 000 patients treated. CyberKnife CyberKnife - Basics • A treatment unit designed for both intracranial and extracranial radiosurgery. radiosurgery • CyberKnife uses a compact linear accelerator mounted on n a robotic b ti arm, m which hi h h hass 6-degrees of freedom. • Pencil beams of radiation are delivered sequentially as the robot moves around patient. Image Guidance • The CyberKnife delivers frameless radiosurgery. • During delivery, the patient position is monitored and the delivery is modified to correct for patient movement. • Orthogonal kilvoltage (kV) x x-ray ray sources are mounted to the ceiling and directed at amorphous silicon detectors on either side of the table. • kV images are obtained before and during the treatment to monitor the alignment of the patient. TARGETING SYSTEM X-ray sources Manipulator Synchrony® camera Treatment Couch Linear accelerator ROBOTIC DELIVERY SYSTEM Image d t t detectors CyberKnife y – Treatment Delivery y F Frameless l Radiosurgery R di • Intracranial lesions: – Immobilization with aquaplast mask – Patient positioning is monitored using bony landmarks • Extracranial lesions: – Immobilization with vacuum bag – Patient positioning is monitored using either: 1) implanted fiducial markers 2)) spine p tracking g (Xsight (X g spine) p ) 3) synchrony lung tracking 4) soft tissue lung tracking (Xsight lung) Skull tracking g window: Fiducial tracking window: CyberKnife y – Beam Characteristics • 6 MV accelerator • 12 interchangeable circular c llim t s collimators • At an SSD of 80cm, collimators provide a beam diameter from 5 to 60 mm • SSD can be varied from 65 to 100 cm CyberKnife – Delivery • Radiation is delivered at a discrete set of linac positions ( ll d nodes). (called d ) • A typical treatment plan will use 110 nodes distributed approximately uniformly over about one half of a sphere centered on the treatment site. Meningioma Nasopharyngeal Tumor Prostate ™ Respiratory Synchrony S h R s i t T Tracking ki System S st m • Patient wears a vest with optical p markers that serve as a surrogate for tumor position. • Camera system monitors position of markers. Synchrony™ Respiratory Tracking System • Before the treatment, a correspondence model between the markers and the tumor position pos t on iss constructed using us ng the camera and multiple orthogonal x-rays. • Model is updated continuously during treatment by further x-ray x ray imaging. imaging • During delivery, the tumor position is tracked using the live camera signal and the correspondence model. • The robot is moved in real-time to maintain alignment with the tumor. Recent CyberKnife Features • • • • • Sequential Optimization 800 MU/min accelerator Monte Carlo Dose Calculation Iris Variable Aperture Collimator RoboCouch 800 MU/min. / LINAC • Provides reduced treatment times relative to existing 600 MU/min design. design • More compact Monte Carlo Dose Calculation • This provides a significant improvement in dose accuracy relative to their current ray-tracing y g algorithm. g m. Dose Comparison – MC and Ray Ray-tracing tracing Courtesy of Charlie Ma Dose Comparison – MC and Ray Ray-tracing tracing Courtesy of Charlie Ma Iris™ Variable Aperture Collimator Iris • Description – 2 stacked banks of 6 tungsten s segments ts creates t s a 12-sided 12 sid d variable aperture Variable able aperture automatically automat cally – Var replicates sizes of the existing 12 fixed collimators (5 to 60 mm) – All segments t are d driven i b by a single motor I i ™V Iris™ Variable i bl A Aperture t C Collimator lli t • Benefits B fi – Reduces treatment time by consolidating multiple path sets and multiple-collimators multiple-path multiple collimators into a single path set – Improved plan quality – Automatically changes the size of the variable aperture p without having g to re-enter the treatment suite CK - G4 with 8.0 8 0 Delivery Software • Hillcrest Medical Center (Tulsa, (Tulsa OK) became 1st center to treat with Iris Collimator on 7/10/2008. Comparison of Iris™ Variable Aperture with Fixed Collimator • Chad Lee from CK Solutions has performed plans l s comparisons is s between b t fixed fi d collimator lli t plans (created in MP 2.1) and IRIS plans (created in n MP M 3.0). 3. ). • The goal was to achieve similar plan quality and compare the plans based on # of beams, # of MUs, and delivery time. Case 1: Pancreas – IRIS Collimator Delivery time = 80 minutes/fraction Case 1: Pancreas – Fixed Collimator Delivery time = 102 minutes/fraction Case 1: Pancreas • Rx: 11 Gy x 3 • MP 2.1 – 3 even paths: 7 7.5, 5 10 10, 15mm fixed – 238 beams minutes/fraction f – 102 m • MP 3.0 – 1 full p path,, IRIS (7.5, ( , 10,, 12.5,, 15,, 20mm)) – 164 beams – 80 minutes/fraction Courtesy of Chad Lee Case 2: Axilla – IRIS Collimator Delivery time = 85 minutes/fraction Case 2: Axilla – Fixed Collimator Delivery time = 107 minutes/fraction Case 2: Axilla • Rx: 7 Gy x 5 • MP 2.1 – 2 sh shortt p paths: ths: 20, 20 40mm fixed fix d – 283 beams – 85 min/fraction • MP 3.0 – 1 full path path, IRIS (20 (20, 25 25, 30 30, 35 35, 40 40, 50mm) – 162 beams – 107 min/fraction Courtesy of Chad Lee CyberKnife Routine QA Procedures Daily QA • • • • • Linac Output Various voltages and currents Robot perch position Safety interlocks Test coincidence of treatment beam with imaging center (AQA) Monthly QA • • • • Annual QA Quarterly QA • • Laser/radiation coincidence Imaging system alignment Beam Energy Flatness/symmetry/penumbra Robot p pointing g End-to-end test • • Spot p check beam data Treatment planning system beam data and calculation checks. Daily QA – Linac Output Constancy • In air measurement using “birdcage” phantom. • CyberKnife’s ion chambers are vented to the atmosphere. Monthly QA - End-to-end Test • QA test designed to measure total accuracy of the system including localization, localization mechanical targeting, and planning errors. • Measurements are performed using an anthropomorphic head phantom loaded with a target ball and orthogonal pieces of gafchromic gafchrom cf film. m. Anthropomorphic Head Phantom A th Anthropomorphic hi H Head/Neck d/N k phantom h t 2.5” Ball Cube in cranium for g QA Q fiducial and skull tracking 1.25” Ball Cube in neck for Xsight g Spine p QA Q Courtesy of Accuray Inc. Ball-Cube Film Cassette • Allows accuracy measurements using only two films • Contains fiducials for QA for extracranial treatments. treatments Courtesy of Accuray Inc. End-to-end Test • The head phantom is imaged using CT. • A treatment plan is developed with the goal of conforming the 70% isodose line to the target ball. ball • After the delivery, the orthogonal films are scanned and analyzed using software from Accuray that d t determines i th the shift hift between b t th the centroid t id of f th the 70% isodose curve and the center of the film. p for each tracking g technique: q skull • Test is repeated tracking, fiducial tracking, spine tracking, and synchrony based tracking. TPS Images 70% contour aiming at 31 31.75 75 mm ball target. target Courtesy of Accuray Inc. Digital Centroid Analysis Software Additional CK Information • TU-E-213A-3 – Rm 213A – 4-5:30 PM – “E “Everything thi Y You N Need d tto K Know Ab Aboutt th the Cyberknife, But Were Afraid to Ask” – Mary Ellen Masterson-McGary, y, Cyberknife y Center of Tampa p Bay, Tampa, FL CyberKnife y f - Summary y • Radiosurgery delivered using an x-band linear accelerator mounted on a robotic arm. • Uses a frameless approach and is capable of intracranial and extracranial radiosurgery. radiosurgery • Real time image-guidance is accomplished using 2 kilovoltage imagers. • The total error should be below 0.9mm for skull tracking fiducial tracking, tracking, tracking and X X-sight sight spine tracking. tracking • The total error should be less than 1.5mm for tracking using Synchrony. Synchrony End-to-end Test Ball Phantom and Ball Cube Perfexion vs. 4C – Prospective Study • At Timone University Hospital 59 patients were enrolled in a prospective study comparing the Perfexion and the Gamma Knife 4C. 4C • With Perfexion the median total treatment time was reduced from 65 minutes to 44.5 minutes. • With Wi h Perfexion P f i there h were no collision lli i issues i while hil with i h the 4C 21% patients treated in trunion mode. • The Perfexion unit on average reduced dose to the gonads by a factor of 15. Courtesy of Jean Régis RoboCouch® RoboCouch® • 6D robotic couch • Converts between seated and flat positions • 500lb weight capacity 251 Units Installed Worldwide – June 2007 North America = 118 Europe = 33 China = 17 Middle East = 4 Japan = 51 Other Asia = 26 South America = 2 ©ELEKTA INSTRUMENT AB - Sales & Marketing (www.elekta.com) - LGK – June 2007 116 Gamma Knife® units in the U.S. F b February 2008 AK H I 19 Leksell Gamma Knife® Perfexion™ units J June 2008 AK H I 111 Leksell Gamma Knife® units installed U.S. November 2006 AK HI %Dosse Collimator Dose Profiles x (mm) M t – 11 shots Met h t (18mm) (18 ) Perfexion vs. 4C – Prospective Study • At Timone University Hospital 59 patients were enrolled in a prospective study comparing the Perfexion and the Gamma Knife 4C. 4C • With Perfexion the median total treatment time was reduced from 65 minutes to 44.5 minutes. • With Wi h Perfexion P f i there h were no collision lli i issues i while hil with i h the 4C 20.7% patients treated in trunion mode. • The Perfexion unit on average reduced dose to the gonads by a factor of 15. Courtesy of Jean Régis Courtesy of Jean Régis Target g 1 Shot 2 Shots 3 Shots 4 Shots 5 Shots Defining the Prescription • When multiple shots of radiation are used, the target dose will be highly non-uniform due to the overlap between the spherical dose distributions. • Target is covered by typically 50% of the maximum dose. • Advantages of the CyberKnife – Frameless • Fractionated delivery – C Can be b used d for f both b th intracranial i t i l and d extracranial stereotactic delivery. • Disadvantages of the CyberKnife – The use of a pencil beam based delivery is inefficient and can lead to treatment times that can be up to several hours. hours • 192 sources • 8 sectors t • 72 Collimators per sector • 3 shots ssize ze – 4,, 8, 16 6 mm Ball-Cube Film Cassette Film is indexed on the edge of the ball cube Courtesy of Accuray Inc. Stereotactic Targeting Accuracy Measurement Single axis targeting error 70% Target Sphere Dose Distribution Courtesy of Accuray Inc. Gamma Knife eXtend™ • Carbon fiber frame with a vacuum assisted mouth piece and a vacuum pillow. Reposition Check Tool (RCT) ( ) • • • • Electro mechanical QA High resolution Mitutoyo probe Reference values Reposition measurements MRI Position reference Dental imprint CT imaging Patient setup Coregistratio n Position Treatment verificatio For each n fraction Treatment planning Dental imprint Patient setup – at Perfexion PCU connected to control system Treatment – First session • S Support pport in GUI for fractionated treatments • Reference values from CT entered • At least two reference f values l per RCT plate (R,L,F,T) are needed Treatment Evaluation of accuracy y of Non-clinical tests Extend™ Frame System performed - ongoing at Princess Margeret - Six volunteers, Hospital, Toronto 10 sessions each Clinical use at Synergy ongoing - Comparison with CBCT Clinical use at Perfexion™ in the Fall of 2009 G Gamma Knife K if eXtend™ Xt d™ G Gamma Knife K if eXtend™ Xt d™ PCU standalone – at CT • Patient docked with vacuum • Vacuum surveillance active • Probe readings on PCU displa display • Value locked when stable Position reference – at CT Treatment – First session • Patient is docked using the patient specific parts • Vacuum surveillance handled by control system; can not continue without activating surveillance Treatment – First session • Position to be measured is displayed together g with corresponding reference value • Probe is locked when h value l iis stable, result is p y displayed • List of measurement result needs to be confirmed to be able to start G Gamma Knife K if eXtend™ Xt d™ G Gamma Knife K if eXtend™ Xt d™ Gamma Knife – Spherical p Phantom Gamma Knife – Spherical p Phantom Leksell Gamma Knife® Perfexion™ • • • • • • The patient is positioned via precise couch motions A frame adapter attaches the Leksell coordinate frame (affixed to the patient’s skull) to the treatment couch Collimation system is built into the unit 3 Collimator sizes: 16 16-mm, mm 8 8-mm mm and 4 4-mm mm 192 60Co sources 60Co sources not fixed in space: they reside on 8 moveable sectors Collimator Patient Frame Adapter Patient Couch: 3-axis positioning system Courtesy of Paula Petti Sector Positions : S Sources i movable in bl 5 different sector positions (listed from back to front): 1) Home: Sources are here when machine is off 2) 8-mm 8 3) Sector Blocked 4) 4 mm 5) 16 mm sectors Back of unit Sources shielded when patient is not in planned position, even when shielding doors are open At the beginning of treatment, the sources move from “Home” position to “Sector Blocked” position Sources move to “Sector Blocked” position while patient coordinates are Courtesy of Paula Petti changed Perfexion™ Perfexion ™ Sector Design 8 independent, identical sectors Sectors slide back and forth on outside of collimator 24 sources per sector Sector Drives Sources are arranged in 5 rings The sources in each sector can be aligned with a different collimator size or blocked completely Courtesy of Paula Petti Example of PinPin-Point Films to Check RFP PPS Coincidence for 1616-mm Collimator New-Style Film Holder Old Style Film Holder Old-Style Y X Z Y Courtesy of Paula Petti Test Specifications and Frequency • Elekta’s specification p for the 4-mm collimator is that Δx,, Δy and Δz are all ≤ 0.3mm and that Δr = Δx 2 + Δy 2 + Δz 2 ≤ 0.4mm Frequency of tests: 1) Master Diode test is done bi-annually by Elekta service engineers i as partt preventative t ti maintenance i t 2) Films are usually irradiated annually by the on-site GK physicist Courtesy of Paula Petti Example of Results using Different Tools to Check PPS and RFP Coincidence for WHHS Perfexion™ Perfexion™ GK Δr = Δx 2 + Δy 2 + Δz 2 (mm) Collimator = 4-mm 8-mm 16-mm Master Diode Tool 0.098 0.16 0.16 New-Style Film Holder 0.09 0.15 0.30 Old-Style y Film Holder 0.11 0.20 0.38 Courtesy of Paula Petti Beam Profiles (film): Measurement Tools New-style Spherical Phantom Old-style Spherical Phantom 1) Attaches to patient frame adapter 1) Attaches to dosimetry adapter 2) Film positioned between 2 rods 2) Film positioned in central insert 3) Can irradiate a 3D stack of films 3) Can irradiate only one film at a time 4) Composed of certified Therapy Grade Solid Water® 4) Presumably composed of polystyrene 5) 3 adapters provided for ion chambers or other detectors 5) Additional inserts are supplied for ion chambers and other detectors Courtesy of Paula Petti Specifications and Frequency for B Beam Profile P fil measurements Specification: According A di tto El Elekta: kt M Measured d and d LGP values l ffor FWHM should be within ± 1 mm of each other Frequency: Beam profiles should be measured upon acceptance of the GK unit and annually thereafter Courtesy of Paula Petti Results from last Annual QA: • All FWHM were between ± 0.1 0 1 mm and ± 0.4 mm of Leksell GammaPlan Courtesy of Paula Petti 16--mm Dose Rate Measurement 16 Performed in spherical phantom Calibration Protocols: • TG-21: Ion chamber calibrated 60Co in-air – Can be used for various phantom materials – Can be used for various geometrical setups • TG TG-51: 51 IIon chamber h b calibrated for 60Co in water. – Designed to facilitate linear accelerator calibration and QA – phantom must be water, – 10 cm × 10Courtesy cm field size of Paula Petti LGK Dose Rate Measurement: Some Recent Publications • R Drzymala y R Wood,, J Levy: y Calibration of the Gamma Knife using a new phantom following AAPM TG51 and TG21 protocols, Med. Phys Med Phys. 35:514 35:514-521;2008 521;2008 – Compared the 2 protocols in the Elekta old-style spherical phantom and in a newly designed water phantom h t – TG-51 in water phantom results were 1.4% lower polystyrene y y p phantom than TG-21 in p Courtesy of Paula Petti LGK Dose Rate Measurement: Some Recent Publications • S Griffin Meltsner and LA DeWerd: Air Kerma based dosimetry calibration for the Leksell Gamma Knife, Med Phys 36:339350;2009 – Proposes an air-kerma-based dosimetry protocol using either an in-air or in-acrylic phantom measurementt – Modified version of TG-21 specific to LGK calibration geometry g y – With new protocol, measured dose rates were between 1.5% and 2.9% higher than those used clinically by at 7 LGK sites (Models B and C) Courtesy of Paula Petti 16-mm Dose Rate Measurement: Practical 16I Issues: Choice Ch i off new or oldold ld-style t l phantom h t Old-style y p phantom requires q dosimetry adapter Bhatnagar, et al Bhatnagar al. (Med Phys 36:1208-1211;2009): The dosimetry adapter attenuates some beams in the lateral (3 and 7) sectors off the th Perfexion™ P f i ™ unit, it causing the overall 16-mm dose rate to be underestimated by approximately 1%. Courtesy of Paula Petti Choice of phantom New spherical phantom • Does not require dosimetry adapter • Attaches to patient adapter Patient P ti t Frame F Adapter – More precise – Provides better check of entire system Courtesy of Paula Petti 16--mm Dose Rate Measurement: 16 Practical Issues • Checking measured dose rate: compare results to – TLD: either in-house or outside service (e.g., RPC SRS phantom) – EBT GafChromic Courtesy of Paula Petti Practical Method for Checking GK Dose Rate Calibration using EBT Film Note that EBT film exhibits very little energy dependence 4.0 Gy 5.0 Gy 6 MV Mini 6-MV Mini-Calibration Calibration Net Cou unts in Red Ch hannel (Backgroun nd subtracted) Irradiate films in 6-MV linear accelerator beam at 3 dose levels, e.g. 4, 5 and 6 Gy to obtain a mini calibration curve 140 130 120 110 100 6-MV Mini-Calibration 90 80 3 4 5 6 7 Dose (Gy) 6.0 Gy Red channel extracted, Background subtracted, film intensity inverted Courtesy of Paula Petti Practical Method for Checking Dose Rate Calibration 6 MV Mini 6-MV Mini-Calibration Calibration Net Cou unts in Red Ch hannel (Backgroun nd subtracted) IIrradiate di t film fil with ith 16 16-mm collimator, 5.0 Gy @ maximum 140 130 120 110 100 6-MV Mini-Calibration 90 80 3 4 5 6 7 Dose (Gy) Determine dose at center of peak region from minicalibration lib i curve Compare to expected value (e g 4 (e.g. 4.96 96 Gy) Expect ± 2% Courtesy to 3% agreement of Paula Petti Relative Output Factors (ROF) for the h 8 8-- and d4 4--mm Collimators C lli • Relative output factor for Gamma Knife is defined as: dDC / dt dD16 / dt (100 ,100 ,100 ) i.e., ROF = dose rate of collimator C relative to 16mm collimator, where both are measured at isocenter = (100,100,100) in spherical, 80 mm radius phantom 80-mm Courtesy of Paula Petti Unique Features of Perfexion Perfexion™ ™ Geometry 1 2 3 4 5 Co-60 sources distributed in 5 rings for each identical sector Ring Number Number of Sources 1 2 3 4 5 48 32 40 32 40 Courtesy of Paula Petti ROF: Unique Feature of Perfexion Perfexion™ ™ Geometry Each collimator within each ring h a diff has differentt beam b geometry t Courtesy of Paula Petti Beam Geometry: There are, therefore, 15 distinct beam geometries: 5 rings multiplied by 3 beam beam-on on positions per ring ring. This is in contrast to previous LGK designs for which all of the beam channels were identical identical, and there was only one type of beam. Each of the 15 beam types yp has a different: 1) Virtual source-to-isocenter distance (SAD) 2) Output factor Elekta determined these values by fitting a beam model to Monte Carlo generated data data. Courtesy of Paula Petti Fitted Values for Relative Output Factor (ROF) and Virtual SourceSource-to to--focus distance (Rvsf) Collimator Size Ring ROF Rvsf (mm) Collimator Size Ring ROF Rvsf (mm) 4 1 0.799 521 8 4 0.808 480 4 2 0 815 0.815 546 8 5 0 730 0.730 522 4 3 0.792 533 16 1 0.961 481 4 4 0.725 595 16 2 1.000 459 4 5 0.663 607 16 3 0.986 455 8 1 0.957 431 16 4 0.920 488 8 2 0.946 437 16 5 0.851 519 8 3 0.901 468 Courtesy of Paula Petti Relative Output Factor for Each Collimator Size • We cannot measure the 15 ROFs individually • The ROF for the 88 and 4 4-mm mm collimators relative to the 16-mm collimator is determined from the equation: 5 ROF (c ) = ∑ n × OF (c ) i =1 i i 5 ∑ n × OF (c = 16mm) i =1 i ,ni = ( 48,32,40,32,40) i Where the sum is taken over all 5 rings ni represents the number of sources in each ring ROF(8mm) = 0.924 ROF(4mm) = 0.805 Courtesy of Paula Petti Two Ways to Determine ROF Measure dose, Dc, delivered by each collimator at ((100,, 100,, 100)) for: • A given treatment time: ROFc = Dc/D16 • The same prescription dose: Dc / Tc ROFc = D16 / T16 Dc ROFc ≈ × ROFcno min al D16 Tc is the irradiation time for each collimator The approximately equal sign is replaced by an equality if the dose is prescribed to (100,100,100) instead of the point of Courtesy of Paula Petti maximum dose Relative Output Factors: Measurement Techniques • • • • Pin-point ion chamber G fCh GafChromic i Fil Film TLDs (rods and LiF microcubes) Glass Rods (Perks, et al.) Some References: • • • Mack et al., Precision dosimetry for narrow photon beams used in radiosurgery - determination of Gamma Knife® output factors, Med. Phys. 29: 2080-9; 2002 Perks et al al., Glass rod detectors for small field, field stereotactic radiosurgery dosimetric audit, Med. Phys. 32:726-32; 2005 Novotny et al. Measurement of relative output factors for the 8 and 4 mm collimators of the Leksell Gamma Knife Perfexion by film dosimetry, Med Phys. 36:1768-1774;2009 Courtesy of Paula Petti ROF Meas: EBT Film and Fixed Dose ¾ Cut and mark Films ¾ Scan un un-irradiated irradiated films to obtain background correction ¾ Irradiate 2 films at the 3 dose levels, e.g., 4.5, 5.0 and 5.5 Gy for 16 collimator to obtain mini-calibration curve (choose either axial, coronal or sagittal plane). It is reasonable to assume that the calibration curve is piece-wise linear between measured points (6 films) ¾ Irradiate 2 films the 4- and 8-mm collimators to a dose in the middle of the minicalibration range in the same plane as calibration films (4 films) ¾ “Process” films with ImageJ: extract red channel, invert intensity values, subtract background CourtesyROF of Paula Petti ¾ Sample intensity values in center of films, convert to dose, calculate My Results: Average of 7 sets of ROF Measurements 8-mm Collimator: 0.888 ± 0.012 (∼3.9% lower than Elekta) 4-mm Collimator: 0.792 ± 0.007 (∼2.5% lower than Elekta) Used constant time for 3 sets of measurements, constant dose for 4 sets Used different measurement planes (axial, coronal or sagittal) Did not change values in LGP Courtesy of Paula Petti Results Reported in Literature: Average of 5 sets of ROF Measurements Collimator EDR 2 Film EBT Film MD-V2-55 MD V2 55 Film 8 mm 0.904 0 904 ± 0.012 0 012 (-2.1%) 0.917 0 917 ± 0.014 0 014 (-0.8%) 0.906 0 906 ± 0.018 0 018 (-2.0%) 4 mm 0.769 ± 0.010 (-4.5%) 0.810 ± 0.007 (+0.6%) 0.819 ± 0.009 (+1.7%) Novotny et al al., Med Med. Phys Phys.2009 2009 Courtesy of Paula Petti Error levels in ROF Measurement • Neglecting g g transit dose: • Neglecting the difference between maximum dose and dose at (100,100,100) • Standard deviation in film pixel values around point of measurement 0.03Gyy = 0.6% 5Gy < 1% Between 0.5 and 1 count Courtesy of Paula Petti What order of magnitude error in film reading causes a 4% error in dose? Film Reading Calibration Curve Read ding minus Background (inv verted) 160 140 120 100 Slope in vicinity of 5 Gy ~ 7 counts/Gy 80 Y-intercept ~ 85 counts 60 Calibration Curve from 16mm Data 40 20 0 0 1 2 3 4 5 6 7 8 9 Dose (Gy) at (100, (100 100 100, 100) Courtesy of Paula Petti What order of magnitude error in film reading causes a 4% error in dose? From calibration curve on previous slide: 5 Gy ⇒ a reading of 120 counts 48G 4.8 Gy ⇒ a reading di off 118.6 118 6 counts t ∴ A difference of only 1.4 counts results in a p y 4% dose discrepancy Courtesy of Paula Petti Alignment of PatientPatient-Positioning System (PPS) with Radiation Focal Point (RFP) Master Diode Tool: Tool: Old-Style OldFilm Holder: Holder Service instrument used during bi-annual preventative maintenance Field instrument: used for annual QA and acceptance t ti testing Diode Tool: Field New Film Holder: Holder Service and Field instrument used for annual QA and acceptance testing Courtesy of instrument used for routine checks (at least monthly, but is usually done more often)Petti Paula Master Diode Tool Used byy Elekta during g Commissioning to allign the RFP to the PPS Attaches directly to the PPS Accomodates up to 5 diodes There are programmed scannning sequences for all three collimators Courtesy of Paula Petti Film Holders New Model Old Model Dosimetry adapter More precise than old old-style style film holder because: 1) Uses the same frame adapter that is used for patient treatments (not shown above) which is machined to very high tolerance 2) Has larger film compartment – easier to interpret 16-mm films 1)) Requires q special p dosimetry y adapter, p , which is not machined to the same high tolerances as the patient frame adapter 2) Provides QA for RFP reproducibility, but d does nott provide id QA ffor patient ti t setup, t since i patient adapter is not employed Courtesy of Paula Petti QA Reports R t and dR Recommendations d ti 1 ASTRO/AANS Consensus 1. C St Statement t t on stereotactic t t ti radiosurgery quality improvement, 1993 g y QA Q Guidelines,, 1993 2. RTOG Radiosurgery 3. AAPM Task Group Report 54, 1995 4. European Quality Assurance Program on Stereotactic R di Radiosurgery, 1995 5. DIN 6875-1 (Germany) Quality Assurance in Stereotactic Radiosurgery/Radiotherapy u g y/ py 6. AAPM Task Group 68 on Intracranial stereotactic positioning systems, 2005 Courtesy of Steven Goetsch 16--mm Dose Rate Measurement 16 • Currently no official calibration protocol specific to the LGK • Charges of AAPM Task Group 178: – Suggest a protocol for calibration with ionization chambers calibrated at an ADCL that can be used with all Gamma Stereotactic Radiosurgery (GSR) devices – Work W k with i h the h working ki group on d dosimetry i calibration protocol for beams that are not compliant with TG-51 TG 51 Courtesy of Paula Petti 134 CyberKnife Units Installed Worldwide Asia 35 Installed CK U.S. 87 Installed CK Europe 12 Installed CK *June 2008 Coincidence of PPS and RFP for Perfexion™ Perfexion™ • No helmets or microswitches to check • Collimator ll settings (4, 8 and 16) are independent • Therefore, Therefore the must check the coincidence of the PPS and RFP for each individual collimator Courtesy of Paula Petti Iris™ Variable Aperture Collimator Iris • Benefits f – Can use up to 12 different aperture sizes in a single treatment path – Reduces treatment time by consolidating multiplepath sets and multiple-collimators into a single path set – Better plan quality can be achieved by using multiple collimators – Automatically changes the size of the variable aperture without having to re-enter the treatment suite