Quantitative PET and SPECT Conflict of Interest Disclosure Imaging for Targeted Radionuclide Therapy
advertisement

8/3/11
Quantitative PET and SPECT
Imaging for Targeted
Radionuclide Therapy
Treatment Planning
Eric C. Frey, Ph.D.
Division of Medical Imaging Physics
Russell H. Morgan Department of Radiology
and Radiological Science
Johns Hopkins University
Acknowledgements
• Funding: NIH Grants
– R01 EB 000288
– R01 CA109234
– R01 EB 000168
• People
– Bin He, Ph.D. (now at New
York Hospital)
– Yong Du, Ph.D.
– Na Song, Ph.D. (Now at
Montefiore Medical Center)
– Lishui Cheng
– Xing Rong
– Geprge Fung, Ph.D.
– Benjamin M.W. Tsui, Ph.D
– George Sgouros, Ph.D.
– W. Paul Segars, Ph.D.
(Duke University)
Conflict of Interest Disclosure
Under a licensing agreement between the GE Healthcare
and the Johns Hopkins University, I (Eric Frey) am entitled
to a share of royalty received by the University on sales of
iterative reconstruction software used to obtain some
results in this presentation. The terms of this arrangement
are being managed by the Johns Hopkins University in
accordance with its conflict of interest policies.
Outline
• Background: Targeted Radionuclide
Therapy Treatment Planning and Inputs
Required from ECT Imaging
• Obtaining Quantitative ECT Images
• Quantitative SPECT Reconstruction
• Challenges in Quantifying TRT
Radionucludes with PET
• Quantifying Y-90 Activity Distributions with
PET and SPECT
• Summary
1
8/3/11
TRT Treatment Planning
Flow Chart
Targeted Radionuclide Therapy (TRT)
!
!
Agents (e.g., monoclonal
antibodies, peptides,
microspheres) that target tumors
Administer
Planning
Dose
Bound to radionuclides whose
emissions can kill tumor cells
!
!
Measure
Distribution
over Time
Calculate
Dose (Dose
Rate)
Distribution
Administer
Therapeutic
Dose
Calculate
Therapeutic
Activity
Crossfire effect
Bystander effect
!
Dose is patient dependent
!
Treatment planning to determine
administered activity
Calculating Dose
MIRD (Organ-based) Dosimetry
!
• Organ-Based (MIRD) Dosimetry
• Voxel (3D) Dosimetry
!
Reference Phantom
"
Fixed geometry
"
Standard mass, shape
"
Uniform activity distribution in
organs
"
Uniform density in organs
Formula
DoseT =
All SourceOrgan
∑
A s ⋅ S(OT ← Os )
s
Cumulated Activity
A =
S-value
∞
∫ A(t) dt
t=0
Cherry SR, Sorenson JA, and Phelps ME, 2003, Physics in Muclear Medicine (3rdEdtion)
2
8/3/11
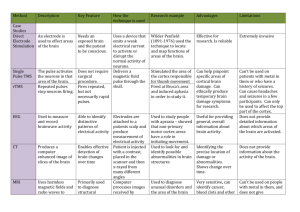
Common Therapeutic
Radionuclides for TRT
Cumulated Activity and Residence Time
Activity A(t) (MBq)
A=
∫ A(t ) dt = A0τ where τ = A / A0
Radionuclide!
Halflife !
(hr)!
A0 : Injected activity (MBq)
I-131!
192.5!
βEnergy
(MeV)!
0.6 0!
τ : Residence Time (sec)
Y-90!
64 .0!
2.28!
none!
Sm-153!
46.3!
0.81!
103 (30), …!
Lu-177!
161.5!
0.50!
208 (11), …!
Re-188!
17.0!
2.12!
155 (15), …!
t
A : Cumulated activity (MBq ⋅sec)
A
Time t (sec)
Imaging to Measure
Activity Distribution
!
γ Energy !
(keV) (% yield)!
364 (82), …!
SPECT Residence Time Estimation
Therapeutic
Radionuclide
Surrogate
Radionuclide
Imaging Modality
I-131
I-131
SPECT
I-131
I-124
PET
Y-90
In-111
SPECT
Y-90
Y-86
PET
Y-90
Y-90
Brehmsstrahlung SPECT
PET
SPECT
Proj. CT
0.12
0.1
0 hr
4 hr
0.08
Aorgan (t )
A0 0.06
SPECT
Activity
Estimation
0.04
0.02
0
0
50
100
Time (hours)
150
Curve Fitting
24 hr
0.12
0.1
72 hr
0.08
Aorgan (t )
0.06
A0
144 hr
Residence
Time
0.04
0.02
0
0
50
100
Time (hours)
150
3
8/3/11
Limitations of Organ Dosimetry
Voxel Dosimetry
• Calculates dose for the reference phantom
• Does not account for:
– Exact organ size and geometry
– Non-uniform organ activity or density distributions
Measure
Time-Activity
Distribution
Calculate
Dose Rate in
Each Voxel at
Each Time
Register
Dose-Rate
Images
Integrate
Dose Rate
over Organ
Integrate
Dose Rate
over Time
• Does not model or provide information about
dose non-uniformity
• Does not account for dose rate effects
Summary of Imaging
Requirements for TRT
Treatment Planning
• Organ Dosimetry: Organ Activity at Each
Time Point
• Voxel Dosimetry: Requires Registered 3D
Activity Distribution at Each Time Point
Outline
• Background: Targeted Radionuclide
Therapy Treatment Planning and Inputs
Required from ECT Imaging
• Obtaining Quantitative ECT Images
• Quantitative SPECT Reconstruction
• Challenges in Quantifying TRT
Radionucludes with PET
• Quantifying Y-90 Activity Distributions with
PET and SPECT
• Summary
4
8/3/11
Computed Tomography
p ( t,θ ) = ∫∫ a ( x,t )δ ( y cosθ − x sin θ − t ) dx dy
y"
p(t,θ)!
a(x,y)!
θ
x"
t"
Goal: Recover function a(x,y) from projections p(t,θ)!
Matrix Formulation of
Image Reconstruction
Activity Distribution Image
Projection
Matrix
Ca = p + n
Poisson Noise
Measured Projection Data
Image Reconstruction: Solve for a given m=p+n
Image Degrading Factors
• Projections are no longer simple line
integrals
• Physical Image Degrading Factors
– Attenuation (PET and SPECT)
– Scatter (PET and SPECT)
– Scanner Spatial Resolution (PET and SPECT)
– Partial Volume Effects
– Random conicidences (PET)
– Statistical Noise (PET and SPECT)
• Ignoring these degrades quantitative
reliability
Outline
• Background: Targeted Radionuclide
Therapy Treatment Planning and Inputs
Required from ECT Imaging
• Obtaining Quantitative ECT Images
• Quantitative SPECT Reconstruction
• Challenges in Quantifying TRT
Radionucludes with PET
• Quantifying Y-90 Activity Distributions with
PET and SPECT
• Summary
5
8/3/11
Physical Image Degrading Factors
in SPECT
•
•
•
•
•
Ideal Projection from Point
Source
Attenuation
Scatter
Collimator-Detector Response (CDR)
Partial Volume Effects
Statistical Noise
Ideal Collimator"
Source"
Attenuation in Patient
Ideal Collimator"
Absorbed"
Effects of Attenuation
• Without attenuation compensation,
sources at depth appear dimmer
• Reduces quantitative accuracy
Scattered"
Source"
Phantom
FBP Reconstruction
(no attenuation compensation)
6
8/3/11
Object Scatter
Quantitative Effects of Scatter
Scatter +
Unscattered Unscattered
Phantom
Unscattered"
Collimator"
Multiply"
Scattered"
Reconstructed Intensity
Absorbed"
Source"
Scattered"
Primary+Scatter
2500.0
2000.0
1500.0
1000.0
500.0
0.0
Collimator-Detector Response
(CDR)
Phantom
Primary
3000.0
0
8 16 24 32 40 48 56 64
Pixel Number
Properties of the Geometric CDR
Opaque Septa (no septal penetration or scatter)
6 cm
Real Collimator"
Septal Scatter"
Geometrically"
Collimated"
Septal Penetration"
Source"
LEGP
LEHR
Distance from
Collimator Face
5 cm
10 cm
15 cm 20 cm
Total detected counts are independent of distance
7
8/3/11
Properties of the Full CDR
I-131 Point Source
Effect of CDR on SPECT Images
30 cm
MEGP
Collimator
HEGP
Collimator
Point Source
Phantom
Distance from
Collimator Face
5 cm
10 cm
15 cm
20 cm
FBP Reconstruction
from Projections with
LEHR Collimator
Total detected counts are a function of distance
Partial Volume Effects
Phantom
Statistical (Quantum) Noise
Reconstruction
Spill Out
0.16
Image Intensity (Arbitrary Units)
Spill In
0.14
Phantom
Reconstruction
0.12
0.1
0.08
0.06
0.04
• Radioactive decay is a random process
• Counts in projection data are Poisson
random variable: variance=mean # counts
• Noise is in projections is uncorrelated
• Reconstruction results in correlated noise
• Affects precision of activity estimates
• Compensating for noise can produce bias
0.02
0
0
50
100
150
Pixel
200
250
8
8/3/11
Effect of Poisson Noise on
SPECT Images
Effect of Poisson Noise
FBP Reconstruction
• Ramp filter used in FBP amplifies high
frequencies
• Combine with low-pass to reduce high this
effect
0.5
• Ramp filter amplifies high frequencies
• Use low pass filter to reduce high
frequency noise
Rectangular, ν =0.5
Relative Magnitude
m
Noise Free
FBP w/
Ramp & Butterworth
FBP Ramp
0.4
Ramp-Butterworth,
ν =0.23, n=6
0.3
m
Ramp-Hann,
ν =0.5
m
0.2
0.1
0
0
0.1
0.2
0.3
0.4
0.5
Frequency (cycle/pixel)
33
34
Compensating for Image
Degrading Factors
• Pre-Reconstruction
– PET Attenuation Compensation (AC)
– Scatter Compensation
• Post-Reconstruction
– Low Pass Filtering
– Partial Volume Compensation
• Reconstruction-Based
– Unified compensation for all factors
– Theoretically rigorous
– Computationally demanding
Maximum Likelihood
Reconstruction
n −m
• Poisson Likelihood P ( n m ) = m n!e
m = Mean counts (not necessarily integer)
n = Recorded counts (integer)
p = Cx
p j = Mean detected counts in projection bin j
xi = Mean decays in image voxel i
Cij = Probability that decay in voxel i gives rise to detected photon in projectin bin j
P ( p | x ) = ∏
j
[Cx ] pj
j
e
−[ Cx ] j
p j !
ln P ( p | x ) = L ( p | x ) = ∑ p j ln [ Cx ] j − [ Cx ] j − ln p j !
j
arg max P ( p | x ) = arg max L ( p | x ) = arg max
x
x
x
∑ p ln [Cx ] − [Cx ]
j
j
j
j
9
8/3/11
Practical Iterative Reconstruction
( n+1)
xi
(n)
= xi
• C is very big
– Calculate Cx and CTp on the fly (projector/backprojector)
• Convergence is very slow (many hundreds of iterations
– Use subsets of projection data (OS-EM): multiple updates per
iteration
xi( n+1,m+1) = xi( n,m )
p j
1
Cij
∑
∑ Cij′ j ∑ Ci′j xi(′n)
j′
• Model CDR in projection and
backprojection operations
– Convolution in planes parallel to detector
– Various methods for accelerating
• Allows modeling spatial variance of CDR
Reconstruction Matrix
Rotate
ta
Ro
Σ
c
Re
on
M
ix
str
on
⊗
Σ
ted
ti
uc
atr
⊗
⊗
Σ
⊗
Σ
⊗
Σ
⊗
y
y
Σ
⊗
ra
Ar
ra
Ar
Σ
⊗
Σ
⊗
n
o
cti
n
o
cti
Σ
⊗
oje
Pr
oje
Pr
Σ
⊗
Σ
⊗
Σ
CD
RF
s
∑C
–
–
–
–
–
ij
j∈Sk
j ′∈Sk
i′
Reconstruction-Based
CDR Compensation
1
∑ Cij′
p j
∑ Ci′j xi(′n,m)
i′
Choice of subsets is important
Typically use >4 angles per subset
Speedup approximately equal to # subsets
Not provably convergent
Problematic for very low noise data
Triple Energy Window (TEW)
• Idea:
– Estimate scatter from 2
auxiliary windows and
trapezoidal approximation
1
( h1 + h2 ) w p
2
1 ⎛ psw1 psw2 ⎞
pse = ⎜
+
wp
2 ⎝ w1
w2 ⎟⎠
psw1 = projection in scatter window 1
psw2 = projection in scatter window 2
Win dow 1 Photopeak Window
s=
w1 = width of scatter window 1
w2 = width of scatter window 2
w p = width of photopeak window
Win dow 2
700
600
Counts
• Can maximize log-likelihood using
Expectation-Maximization (EM) algorithm
Counts
ML-EM
500
400
Scatter
300
200
100
0
120
h1 Scatter
Estimate
130
h2
140
150
Energy (keV)
160
wp
10
8/3/11
Modeling Scatter: Effective
Scatter Source Estimation
(ESSE)
Geometric Transfer Matrix (GTM) PVC
Phantom
SPECT image
ROI
1
2
3
4
Ti : True count in ROI i, (i=1,…4)
ti : Measured count in ROIs,
W : GTM
elements are object-dependent recovery coefficients
{ Diagonal
Off-diagonalelements are object-dependent spill-in factors
Winv: ‘Inverse’ of W
Noise ‘Compensation’
• Post-reconstruction filtering
• Statistical image reconstruction
– Maximum Likelihood Reconstruction
Required Compensations
Factor
Large Object
Small Object
Commercially
Available
Attenuation
Yes
Yes
Yes
Scatter
Yes
Yes
Energy-based:
yes
Model-based:
limited
Geometric
Response
Compensation
No
Yes
Yes
Full CDR
Compensation
(High Energy)
Desirable
Desirable
No
Partial volume
compensation
No
Yes
No
Noise
Regularization
No
Yes?
Filtering
• ML-EM algorithm
• OS-EM
– Maximum a Posteriori (MAP) Reconstruction
• Uses penalty function (prior) to regularize
reconstruction
• Regularization trades increased bias for
decreased variance
– Not essential for organ quantification
11
8/3/11
Reconstructed Pixel Value
From
Unscattered+
Scattered
Photons
From
Unscattered
Photons
Efficacy of Attenuation and
Scatter Compensation
No Comp
Atten
Comp
Atten &
Scatter
Comp
Efficacy of CDR Compensation
• Resolution improves with iteration but remains limited:
cannot totally recover resolution
• Resolution remains spatially varying
• Resolution for LEHR better than for LEGP
Unscattered-NC
Scattered+Unscattered-NC
Unscattered-AC
Scattered+Unscattered-AC
Scattered+Unscattered-ASC
150
OS-EM w/CDR compensation
100
FBP
Updates
128
320
640
1280
50
LEGP
Phantom
0
0
20
40 60 80 100 120
Pixel Number
LEHR
Effect of Compensation on
Image Noise
• Noise increases w/
iteration
• Attenuation Comp
has larger noise
where attenuation is
greatest
• CDR comp results in
lumpy noise
• Texture of noise w/
CDR comp
– varies spatially
– depends on
collimator
Updates
128
320
640
Quantitative Accuracy of SPECT:
In-111 Imaging
1280
•
No
Comp
•
Atten
•
CDR
LEGP
CDR
LEHR
•
•
•
111InCl
solution placed in the heart,
lungs, liver, and background with ratios
of 19:5:20:1
Two spherical lesions with diameters 25
mm and 35 mm were placed in the
phantom (concentrations relative to
background were 17:1 and 156:1).
The total activity used was ~185 MBq (5
mCi)
Imaged Using GE Discovery VH SPECT/
CT system with 1” thick crystal
MEGP collimator
Manually defined VOIs using SPECT and
CT images
RSD Torso Phantom
12
8/3/11
Sample Reconstructed Images
Accuracy of Activity Quantitation:
RSD Phantom and In-111
% Error in total activity estimation: (true-estimate)/true x 100%
A
AS
AGS
NC=No Compensation
A=Attenuation Compensation
AD=Attenuation and CDR Comp
ADS
AS=Attenuation and Scatter Compensation
ADS=Attenuation, CDR and Scatter Comp
Accuracy and Precision of Activity
Estimates: In-111 SPECT
• 3D NCAT phantom:
Organ
No
Comp
Atten
Comp
Atn+
Scat
Comp
Atn +
CDR
+ Scat
Comp
Atn +
CDR
+ Scat
+ PVC
Heart
-77.60%
24.63%
-11.76%
-3.72%
-2.11%
Lungs
-62.78%
31.39%
-0.96%
4.23%
6.45%
Liver
-74.38%
29.22%
-7.47%
2.71%
4.14%
20.6 cc
sphere
-78.88%
-14.85%
-29.81%
-3.36%
-1.97%
5.6 cc
sphere
-88.24%
-51.53%
-56.75%
-21.55%
-11.95%
Accuracy and Precision
In-111 SPECT
– Organ activity concentrations based on 8 clinical studies using In-111 Zevalin
– Non-uniform activity distribution in heart and lungs.
• Simulation:
– Experimentally validated Monte Carlo simulation w/detailed collimator modeling
– Parameters for a GE VH/Hawkeye camera (1” crystal, MEGP collimator)
– Generated 50 realizations of Poisson noise corresponding to noise level of
• 5 mCi In-111 injected activity
• 30 seconds per view
• 120 views over 360°
Phantom
Attenuation
Map
Low-noise
Projection
Reconstructed using
OS-EM w/attenuation,
scatter, CDR and
partial volume
compensation
Error bars show
standard deviations of
activity estimates
• Used true organ VOIs to estimate organ activities
Activity
Distribution
Heart
5%
Noisy
Projection
% Error in Residence Time Estimate
(Estimated-True)/True *100%
NC
Atn Map
Lungs
Liver
Kidneys
Spleen
Marrow
3%
1%
-1%
-3%
-5%
Heart
Lungs
Liver Kidneys Spleen Marrow
QSPECT
Precision better than accuracy for most organs
13
8/3/11
Ensemble Bias and Variance
• 2.2 cm diameter tumors
0%
0
-5
-10
-15
Marrow
Spleen
Kidneys
-20
• Estimation of Activity in objects much
smaller than the resolution (e.g. a voxel) is
not reliably
Tumor 3 (2.2 cm, ratio 5.2)
-4%
-40%
-6%
Tumor 4 (0.9 cm, ratio 12)
-45%
-8%
-10%
T2
-12%
Tumor 9 (2.2 cm, ratio 10.5)
-14%
T4
T3
T9
-16%
-18%
% Error in Activity Estimates
% Error in Activity Estimates
5
Quantification of
Very Small Objects
Quantification of Small Objects
-2%
10
Liver
Different Anatomies
15
Heart
Different Biodistributions
• Used all possible combinations of anatomic and biokinetic
parameters (7x7=49 total phantoms)
20
Lungs
– Organ activity at time 0
– Effective half-life of organ activity
OS-EM Reconstruction w/Attenuation, CDR and Scatter Compensation
% Error in Residence Time Estimate
Phantom Variations
• Anatomic parameters obtained from 7 Zevalin patient studies
– Gender: 3 males and 4 females
– Body, rib, liver, stomach, spleen, kidneys, heart size
• Bio-kinetics parameters from 7 Zevalin patient studies
-50%
-55%
-60%
-65%
-70%
Tumor 2 (0.9 cm, ratio 11)
-75%
-80%
-85%
-90%
-20%
0
5
10
15
20
25
30
35
# of Iterations (24 subsets/iteration)
40
45
50
OS-EM w/attenuation, CDR and scatter compensation (no PVC)
0
5
10
15
20
25
30
35
40
45
50
# 0f Iterations (24 subsets/iteration)
In-111, MEGP collimator
OS-EM w/ Atten, CDR, and Scatter Compensation
14
8/3/11
I-131 Physical Phantom
I-131 Physical Phantom
Percent errors of activity estimates for Anthropomorphic torso phantom
Philips Precedence SPECT/CT system with HEGP collimator
Heart
Chamber
Myocardium
Large
Sphere
Small
Sphere
Background
17.5
5.7
9580
Volume (ml)
59.7
115.3
(r =1.61 cm)
(r =1.11 cm)
Activity(mCi)
0.562
0.471
0.136
0.044
8.15
Activity
concentration
(mCi/µl)
9.38
4.08
7.77
7.72
0.851
#
#
128 projection views
Acquisition time: 40s / view
(%)
Heart
Large sphere
(r = 1.61 cm)
Small sphere
(r = 1.11 cm)
AGS
-15.21
-26.12
-32.72
ADS
4.75
-17.63
-25.77
ADS+Dwn+
-5.20
-21.10
-31.17
ADS+Dwn+PVC*
-2.88
-15.49
-19.28
50 iterations
24 subsets/iteration
!
AGS
ADS
ADS + Dwn
ADS+Dwn+PVE
+DWN=model-based
downscatter compensation
*PVC=reconstruction-based PVC compensation
I-131 MC Simulation Study
I-131 MC Simulation Study
Effects of Compensation Methods
and Poisson Noise
30%
20%
10%
0%
-10%
-20%
-30%
-40%
Heart
Lungs
Liver
Kidneys
Spleen
Background
-50%
AGS
3D NCAT phantom population (49 phantoms) to model
various patient anatomies and organ uptakes
50 Noise realizations for each phantom/uptake combination
ADS
ADS+Dwn
ADS+Dwn+PVE
Mean of % Error and % STD over all noise realizations averaged over phantom
population for each organ and for each compensation method.
% Error = (Estimate - True) / True
% STD = STD / True
50 iterations
24 subsets/iteration
!
15
8/3/11
Limitations of ECT for Voxel
Dosimetry
Limitations of Quantitative
SPECT for Organ Dosimetry
• Limited resolution
• Noise
• Voxel activities are “not estimable”
• Activity distribution in organs corrupted by
– Noise
– Partial Volume Effects
– No unbiased estimator exists
– Very poor precision
Simulated 24 hr
In-111 Zevalin Images
• Dose-volume histogram is severely
degraded
OS-EM
30 iterations
32 subsets
Results for 95% VDR Error
Results: 0 hour
Cumulative Dose-Rate Volume Histogram of Liver
Cumulative Dose-Rate Volume Histogram of Kidney
1.2
1.2
Phantom
OS-EM w/ 10 iter
OS-EM w/20 iter
OS-EM w/30 iter
OS-EM w/40 iter
Fraction of Kidney Volume
1
Fraction of Kidney Volume
Fraction
ofofLiver
Volume
Fraction
Liver Volume
OS-EM
5 iterations
32 subsets
0.8
0.6
0.4
0.2
0
0.01
0.03
0.05
0.07
0.09
Dose Rate/AA (Aribitrary Units)
Dose Rate (Arbitrary Units)
0.11
Phantom
OSEM w/10 iter
OS-EM w/20 iter
OS-EM w/30 iter
OS-EM w/40 iter
1
95% VDR Error
Optimal OS-EM w/o
filtering
Optimal OS-EM w/
filtering
Liver
26%
15%
Kidney
28%
28%
0.8
0.6
0.4
0.2
0
0
0.01
0.02
0.03
0.04
0.05
0.06
0.07
0.08
Dose Rate/AA (Aribitrary Units)
Dose Rate (Arbitrary Units)
16
8/3/11
Methods to Improve Activity
Distribution Estimates
Results: Sample Images
• Maximum a Posteriori (MAP)
Reconstruction
– Maximize P(a|m):
– Apply Baye’s Law, use Gibb’s Prior, Take
Logaritim
– Edge Preserving, 4D, and Anatomic Priors
May Be Useful in Controlling Noise and
Reducing PVEs
Truth
Phantom
4D MAP
OS-EM w/filtering
1
Fraction of Kidey Volume
1
Fraction of Liver Volume
1.2
Phantom
4D MAP
OS-EM w/filtering
0.8
0.6
0.4
0.2
0.8
0.6
0.4
0.2
0
0
0.1
0.3
0.5
0.7
0.9
0
Dose Rate/Aribitrary Units
0.1
0.2
0.3
0.4
0.5
0.6
Dose Rate/AA (Aribitrary Units)
The Sum of Squared
Error of Histogram
4D MAP
OS-EM w/filter
Kidney
0.45
0.58
Liver
0.11
0.49
4D-MAP
Quantitative SPECT
Results: CDVH, 0 hour
Cumulative Dose-Rate Volume Histogram of Liver
Cumulative Dose-Rate Volume Histogram of Kidney
1.2
OS-EM
0.7
0.8
Summary
• With careful attention to compensation for image
degrading factors excellent (better than 5%)
accuracy for organs with In-111 and I-131 is
achievable
• Good accuracy (better than 10%) for tumors with
size greater than or equal to resolution
• Very challenging to estimate activity for tumors
smaller than resolution
• Patient variations are a significant source of
imprecision
• Obtaining suitable activity distribution estimates
for voxel dosimetry requires further work
17
8/3/11
Level Schemes
Outline
• Background: Targeted Radionuclide
Therapy Treatment Planning and Inputs
Required from ECT Imaging
• Obtaining Quantitative ECT Images
• Quantitative SPECT Reconstruction
• Challenges in Quantifying TRT
Radionuclides with PET
• Quantifying Y-90 Activity Distributions with
PET and SPECT
• Summary
Abundances
I-124
Y-86
• Multiple positrons
• Many Prompt Gammas
• Relatively high positron energies (~20% larger FWHM resolution for
clinical PET)
From M. Lubbering and H. Herzog, “Quantitative imaging of 124I and 86Y with PET”, EJNM, vol 38, Sup 1. S:10-18, 2001.
Effects of Prompt Gammas
• Multiple Coinicidence
• False Coinicidence with
Prompt Gamma
• Positron decay relatively scarce
• Many other gamma emissions6
From M. Lubbering and H. Herzog, “Quantitative imaging of 124I and 86Y with PET”, EJNM, vol 38, Sup 1. S:10-18, 2001.
18
Fig. 3 Normalized line source profiles derived from sinograms of 124I or 18F line sources inside a cylindrical phantom filled with water. Reprinted
from [10] with permission from Elsevier
Effects of Prompt Gammas
Y-86
Cylindrical
Phantom
False
Coincidence
Scaled
Single Scatter
Scatter
simultaneously with at least two photons, and all other
positrons are emitted simultaneously with at least one
photon. Most of these photons have energies greater than
600 keV. Even if the primary energy of a prompt gamma is
above the higher energy level of the energy discrimination
window, the prompt gamma may be accepted after being
scattered within the patient or septa and having lost part of
its energy. For both isotopes, electron capture decays lead to
multiple gamma photons emitted simultaneously, which
might cause a so-called multiple coincidence. In addition, a
multiple coincidence is recorded if a true coincidence is
detected simultaneously with a prompt gamma. The probability of multiple coincidences is rather low, but increases
with a larger spatial angle of the PET detectors. Such events
are discarded in most PET scanners.
For 89Zr, on the other hand, prompt gamma coincidences
do not occur since the metastable 0.91 MeV level of 89Zr
has a half-life of 14 s [8], as shown in Fig. 1.
As illustrated in Fig. 3, which compares the background
caused by 124I with that of 18F, the background is greater in
3-D PET than in 2-D where the septa limit the acceptance
angle for photons not being within a plane perpendicular to
the scanner’s axis. Therefore, random and scattered
coincidences as well as gamma coincidences are decreased.
On the other hand, simulation studies have shown that the
8/3/11
principle advantage of 2-D imaging is to some extent
counterbalanced by an increase in the relative effect of
prompt gamma radiation due to down-scatter of high
energy photons in the septa [9].
Earlier generation PET scanners, such as the Scanditronix
PC4096 WB (Scanditronix, Uppsala, Sweden), had very long
and thick septa so that the recorded rate of gamma
coincidences became very low despite possible downscatter. The advantage of this kind of 2-D PET became
obvious by the papers of Pentlow et al., Herzog et al. and
Lubberink et al. [4, 10–13], and it can be concluded that
early studies using the PC4096 WB scanner for quantitative
imaging of nonstandard positron emitters provided valid
results even without any corrections for prompt gamma
coincidences.
The effect on quantitation due to the background caused
by the gamma coincidences depends on the specific
nonstandard positron emitter and on the specific tissue or
target to be examined. In the case of 124I and imaging of
Teflonthe radioactivity distribution is limited to a
thyroid cancer,
few foci, whereas the backgound is distributed across the
entire image and thus contributes little to the activity
concentration in a lesion. This situation is similar to that
Water in Fig. 3,Airwhere the ratio of counts measured at
displayed
the maximum of a 124I point source in water and of the
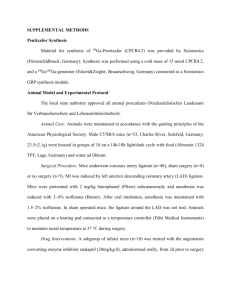
Effects of Prompt Gammas
Fig. 4 Images of a NEMA 1994
phantom with cold Teflon (top),
water (left) and air (right)
inserts. The measurements were
done with an ECAT Exact HR+
(Siemens/CTI, Knoxville, TN,
USA) PET scanner in 3-D
acquisition mode. There is a
clear bias in the Teflon and
water inserts for 86Y and, to a
lesser extent, for 124I. Reprinted
with permission from [16],
©2008 Edizione Minerva
Medica
From Beattie et al, ‘Quantitative imaging of bromine-76 and yttrium-86 with PET: A method for the removal of spurious activity
introduced by cascade gamma rays’, Med Phys, vol 30(9), 2410-23, 2003.
Quantitative PET for TRT
Summary
• Radionuclides for TRT PET have unique
challenges
• Resolution and noise will be superior to
SPECT, but be careful to verify
compensation for effects of prompt
gammas
From M. Lubbering and H. Herzog, “Quantitative imaging of 124I and 86Y with PET”, EJNM, vol 38, Sup 1. S:10-18, 2001.
Outline
• Background: Targeted Radionuclide
Therapy Treatment Planning and Inputs
Required from ECT Imaging
• Obtaining Quantitative ECT Images
• Quantitative SPECT Reconstruction
• Challenges in Quantifying TRT
Radionucludes with PET
• Quantifying Y-90 Activity Distributions with
PET and SPECT
• Summary
19
8/3/11
Applications of Y-90 Imaging
• Y-90 is used as therapeutic radionuclide
for for:
Y-90 Bremsstrahlung SPECT
• Challenges: continuous and broad energy
distribution
– Limited scatter rejection using energy windows
# substantial scatter fraction in detected photons
– Photon energies up to ~2 MeV
– Radioimmunotherapy agents (e.g., Zevalin)
– Radioembolization (Y-90 labeled
microspheres for liver cancer therapy)
– Radiolabeled peptides (e.g., Y-90 DOTATOC)
# substantial septal penetration, scatter and backscatter from the
back compartment behind the crystal
• Imaging Y-90 of interest for dose
verification
78
Modeling Image Formation
Bckgnd
Relative
Activity
Total Activity
(MBq)
1657.7
21x30
1
Small
1.2
20
5.9
Medium
3.0
10
27.4
Large
6.0
10
121.9
Philips Precedence SPECT/CT: HEGP
Acquisition time per view: 45s/view
Crystal thickness: 0.9525 cm
128 projection views over 360o
Matrix size per view: 128*128
Pixel size: 4.664mm
30 cm
21 cm
Diameter
(cm)
25 cm
Physical Phantom Study
20
8/3/11
Bremsstrahlung SPECT
Bremsstrahlung SPECT
Image Quality and Quantitative Accuracy
Monte Carlo Simulation Evaluation
Attenuation
Map
!
(16 subsets)
% Error In Total Sphere Activity after
400 Iterations with 16 Subsets
Error
Large
Medium
Small
-7.0%
9.7%
10.2%
Spleen
(10.2±2.1)% (-11.9±2.3)%
90Y
!
Kidneys
Liver
Heart
(-6.4±5.0)%
(-4.5±0.7)%
(-5.8±0.9)%
Results: 90Y Phantom Trues
Rates
Simplified decay
scheme for 90Y.
ββ99.999 %
Reconstruction Reconstruction Conventional
Low Noise Data Noisy Data
Reconstruction
Errors in Activity Estates after 50 Iterations (16 Subsets)
Lung
PET Imaging of Y-90
• Yttrium-90 primarily
decays via beta emission.
• In addition to β decay, an
extremely small positron
decay mode has been
identified.
• Nickles (2004) have
demonstrated the
potential of 90Y PET in
phantom studies.
Phantom
0+
β+ β- 34×10-4%
0+
90Zr
• Despite high activity in the FOV,
90Y true coincidence count rates
were very low.
– 50-250 cps (not kcps)
– Comparable to literature
reports from patient studies
• Randoms exceeded trues
(stable)
Courtesy of M.A. Lodge, Division of Nuclear Medicine, Dept of Radiology, Johns Hopkins
Courtesy of M.A. Lodge, Division of Nuclear Medicine, Dept of Radiology, Johns Hopkins
21
8/3/11
Results: 90Y PET Images
• Total trues 461 ± 69 kcounts
(total).
• ≈ 1.5 % of total counts
from typical FDG scan
Results: Quantitative Accuracy
ROI over
6 cm diameter
sphere
ROI over background
• Activity concentration obtained from 90Y PET was highly
correlated with data from the ionization chamber.
Courtesy of M.A. Lodge, Division of Nuclear Medicine, Dept of Radiology, Johns Hopkins
Comparison of
Y-90 SPECT and PET
•
•
•
•
Comparable accuracies for large objects
SPECT: higher sensitivity, larger FOV
PET: better resolution
More detailed comparison in process
Courtesy of M.A. Lodge, Division of Nuclear Medicine, Dept of Radiology, Johns Hopkins
Summary
• Targeted radionuclide therapy treatment
planning requires estimates of
– Organ activities for MIRD dosimetry
– Activity distributions for voxel (3D) dosimetry
• Accurate organ activity estimates can be
obtained from PET and SPECT with
careful attention to reconstruction and
compensation methods
• PET and SPECT provide the potential to
directly quantify Y-90 activities
22