Methodological issues Methodological issues and key results in the QUANTEC 2010 qu
advertisement

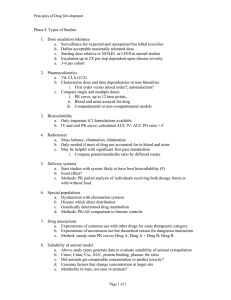
8/16/2011 Methodological issues Methodological issues and key results in the QUANTEC 2010 review of quantitative analysis of normal tissue effects in the clinic (The QUANTEC steering committee:) Soeren Bentzen, Sandy Constine, Joe Deasy, Avi Eisbruch, Andrew Jackson, Larry Marks, Randy Ten Haken, Ellen Yorke 1. 2. 3. 4. 5. 6. 7. Avoiding xerostomia (‘dry-mouth syndrome’) in H&N patients A sample of key results • Xerostomia and salivary parotid gland irradiation • Late rectal bleeding • Radiation pneumonitis and lung irradiation • Erectile dysfunction and penile bulb irradiation No consensus on best NTCP models (e.g., simple vs. large model) Results not stated in comparable terms (e.g., NTCP model vs. DVH thresholds) Sometimes the ‘target’ tissues aren’t known Endpoint definitions can be questionable Results depend on typical dose distributions, which are evolving Implicit assumption of organ uniformity (ignoring stem cell rescue, etc.) Assumption that spatial dose pattern doesn’t matter “OK” “Worse” • Salivary function is stimulated or unstimulated • Stimulated flow is dominated by parotid gland contributions • Unstimulated consists of contributions from submandibular salivary glands and multiple smaller glands 1 8/16/2011 (In press, IJROBP) (Blanco et al. IJROBP 2005) 2 8/16/2011 Test of QUANTEC “20/20” recommendation No Grade 4 xerostomia at 3 months Grade 4 xerostomia at 3 months Predictor 70 Sensitivity: 23/27=85% Specificity: 19/23=83% LP mean dose, Gy 60 50 40 30 20 10 0 0 10 20 30 40 50 60 70 RP mean dose, Gy (In press, IJROBP, Vitali Moiseenko, John Wu, et al., BCCA) Radiotherapy alone PROs scores correlation with the mean dose to contralateral parotid gland XEROSTOMIA PATIENT REPORTED OUTCOMES ARE A LINEAR FUNCTION OF CONTRALATERAL PAROTID GLAND MEAN DOSE CHEWING SWALLOWING DRYNESS Ziad H Saleh1, Wade Thorstad2 , Aditya Apte1 , and Joseph O. Deasy1 1- Memorial Sloan-Kettering Cancer Center (Department of Medical Physics) , New York , USA 2 -Washington University School of Medicine (Department of Radiation Oncology) , St. Louis , USA 8/16/2011 ESTRO 2011 Slope = 0.93 Slope = 1.41 Slope = 1.26 %/Gy %/Gy %/Gy PROs increases linearly as a function of the mean dose to the contralateral mean dose 11 8/16/2011 ESTRO 2011 12 3 8/16/2011 Induction + Concurrent ChemoRT PROs scores correlation with the mean dose to Contralateral parotid gland CHEWING SWALLOWING DRYNESS Slope = 2.04 Slope = 0.66 Slope = 2.07 %/Gy %/Gy %/Gy PROs response as a linear function is steeper compared to RT alone 8/16/2011 ESTRO 2011 13 Continued benefit to patient by reducing mean dose Plus: + g E U D d d dd . . . / N 123 n V o x e l s a a a a 1 / a Results in different relative contributions to gEUD within the DVH: 4 8/16/2011 e s tim a te s o f L K B vo lu m e e ffe c t p a ra m e te r n fo r re c ta l c o m p lic a tio n s Are IMRT rectal dose-volume limits a problem? R T O G 9 4 -0 6 Typical 3DCRT plan (sagittal) Typical IMRT plan (sagittal) S tu d y Tucker R a n c a ti P e e te rs Sohn 0 .0 1 0 .1 1 v o lu m e e ffe c t p a ra m e te r, n (Slide courtesy A. Jackson et al.) (Note: a = 1/n) Rectal gEUD = 53 Gy (a= 10) Rectal gEUD = 24 Gy Variation in rectal DVHs for daily Fx’s (Rad Oncol 2005) 5 8/16/2011 Purpose/background: • Validating a predictive model for late rectal bleeding would enable safer treatments or dose escalation. • We tested the normal tissue complication probability (NTCP) model recommended in the recent QUANTEC review (Michalski et al., IJROBP, 2010 (76) S123-9). Materials/Methods: • 161 prostate cancer patients were treated with 3D conformal radiotherapy for prostate cancer at the British Columbia Cancer Agency in a prospective protocol. • Total prescription dose for all patients was 74 Gy, delivered in 2 Gy/fraction. • Rectal dose volume histograms were extracted and fitted to a Lyman-Kutcher-Burman NTCP model. Two treatment plans could not be extracted. • Late rectal bleeding (>=grade 2) was observed in 12/159 patients (7.5 %). 6 8/16/2011 Results: • Multivariate logistic regression with dose-volume parameters (V50, V60, V70, etc.) was non-significant. • Among clinical variables, only age was significant on a Kaplan-Meier log-rank test (p = 0.007, with an optimal cut point of 77 years). • Best-fit Lyman-Kutcher-Burman model parameters (with 95% confidence intervals) were: n = 0.068 (0.01, +infinity); m = 0.14 (0.0, 0.86); and TD50 = 81 (27, 136) Gy. • The peak values fall within the 95% QUANTEC confidence intervals. Results: On this dateset, both models had only modest ability to predict complications: • the best-fit model had a Spearman’s rank correlation coefficient of rs=0.099 (p=0.11) and AUC of 0.62; • the QUANTEC model had rs=0.096 (p=0.11) and a corresponding AUC of 0.61. • Although the QUANTEC model consistently predicted higher NTCP values, it could not be rejected according to the chi-square test (p=0.44). Int. J. Radiation Oncology Biol. Phys., Vol. 78, No. 4, pp. 1253–1260, 2010 7 8/16/2011 Tucker et al., Int. J. Radiation Oncology Biol. Phys., Vol. 78, No. 4, pp. 1253–1260, 2010 Identifying the most influential tissues 8 8/16/2011 Trismus in 480 H&N pts., MSKCC (S. Rao, Z. Saleh et al.) Which tissues are most influential? Correlation map shows hotspot just outside of contoured muscles – surprise! (Ziad Saleh et al., poster this meeting) 9 8/16/2011 P n e u m o n itis , m e a n d o s e re s p o n s e - w h o le lu n g P ro b a b ility o f p n e u m o n itis 1 .0 M S K C C (1 0 /7 8 ) D u k e (3 9 /2 0 1 ) M ic h ig a n (1 7 /1 0 9 ) M D A n d e rs o n (~ 4 9 ? /2 2 3 ) N K I (1 7 /1 0 6 ) W U (5 2 /2 1 9 ) M a rte l e t a l. (9 /4 2 ) O e z te l e t a l. (1 0 /6 6 ) R a n c a ti e t a l. (7 /5 5 ) K im e t a l. (1 2 /6 8 ) lo g is tic fit 0 .9 0 .8 0 .7 0 .6 0 .5 0 .4 WUSTL RP dataset • 228 patients with non-small cell lung cancer (NSCLC) treated definitively with radiation +/- chemotherapy between 1991-2001 • 48 cases of RP (steroids or more intensive intervention) • 3D treatment plan archives available 0 .3 0 .2 – Non-heterogeneity corrected dose distributions 0 .1 0 .0 0 10 20 30 M e a n d o s e (G y ) • Minimum six months follow-up post-treatment unless patient developed pneumonitis < 6 mos. Consistent – but not very predictive. Tumor location is associated with risk of pneumonitis Superior/Inferior Position 1 Superior 25%: 15.9% (7/44) 0.8 upper-mid 25%: 30.2% (42/139) 0.6 0.4 0.2 0 0 Inferior 50%: 44.4% (20/45) Right Lung: 47/137 (34.3%) 0.2 Left Lung: 22/91 (24.2%) 0.4 0.6 Right/Left Position 0.8 Multi-variate modeling of combined WUSTL and RTOG 93-11 datasets (Bradley et al. IJROBP 2007) • Chosen from many candidate models; logistic function of: 1 . 5 + 0 . 1 1 M e a n L u n g D o s e 2 . 8 P o s S u p I n f • Spearman’s rank correlation coefficient 0.3 (on cross validation data) 1 (Hope et al, IJROBP 2007) 10 8/16/2011 Dataset • Heart volumes of WUSTL archived plans were re-contoured within CERR by a single physician (n = 209, with 48 RP events). • Heart and normal lung (lung minus gross tumor volume) dosevolume parameters were extracted for further modeling using CERR. • Evaluated factors included: – clinical (age, gender, race, performance status, weight loss, smoking, histology) – dosimetric parameters for heart and normal lungs (D5-D100, V10-V80, mean dose, maximum dose, and minimum dose) – treatment factors (chemotherapy, treatment time, fraction size) – location parameters (heart center-of-dose, sup-inf within the heart; and center-of-target mass within the normal lungs.) Highest univariate correlations Variable Spearman Corr. Significance D5_Heart 0.256 <0.0002 D10_Heart 0.24 <0.0003 V70_heart 0.239 <0.0003 gEUD_Heart (a=10) 0.249 <0.0001 Maximum Heart Dose 0.227 <0.0006 Superior -Inferior position of GTV 0.219 <0.0008 11 8/16/2011 Are simple NTCP models sophisticated enough? (2010) 12 8/16/2011 13 8/16/2011 Conclusion • Heart irradiation may be an important risk factor for radiation pneumonitis, as previously seen in animal studies (Luijk et al., IJROBP 2007). • In this single-institution dataset, RP is better associated with high-dose heart irradiation factors than previously reported lung dosimetry factors. • The lung ‘location effect’ was not selected in multivariate modeling when heart factors were included. • Obviously, these observations need to be tested on independent datasets. Another validation study: acute esophagitis (dysphagia) 14 8/16/2011 Nomogram to predict dysphagia Radiation-induced dysphagia: multivariate analysis Table 1. Odds ratio's for developing dysphagia Variable Coefficient Odds ratio Age -0.03 0.97 Gender male ref female 0.50 1.65 WHO-PS 0-1 ref >=2 0.57 1.76 Chemotherapy no/sequential ref concurrent 0.93 2.53 MED 0.06 1.06 MAXED 0.03 1.03 OTT -0.06 0.94 95% CI 0.95 - 0.99 P 0.003 0.011 1.12 - 2.43 0.012 1.13 - 2.75 <0.001 1.64 1.04 1.01 0.92 - 3.91 1.09 1.05 0.96 <0.001 0.0002 <0.001 C-statistic = 0.77 (bootstrap) C. Oberije et al, Radiotherapy and Oncology, 2010 C. Oberije et al, Radiotherapy and Oncology, 2010 External validation Washington University/Mallinckrodt data (n=216) 1.0 ≥ Grade 2 (n=85) AUC=0.75 0.6 0.4 Ideal Logistic calibration Nonparametric Grouped observations Ideal Logistic calibration Nonparametric Grouped observations 0.0 0.0 0.2 0.4 0.6 0.8 0.0 0.2 0.4 0.6 Actual Probability 0.8 ≥ Grade 3 (n=22) AUC=0.77 0.2 Actual Probability 0.8 1.0 External validation Washington University/Mallinckrodt data (n=216) 0.0 0.2 0.4 0.6 0.8 1.0 Predicted Probability 1.0 Predicted Probability C. Oberije et al, Radiotherapy and Oncology, 2010 C. Oberije et al, Radiotherapy and Oncology, 2010 Courtesy of J. Deasy, J. Bradley, I. El Naqa, E. Huang Courtesy of J. Deasy, J. Bradley, I. El Naqa, E. Huang 15 8/16/2011 External validation Ghent data (n=100) External validation Ghent data (n=100) ≥ Grade 3 (n=8) ≥ Grade 2 (n=19) AUC=0.94 AUC=0.86 C. Oberije et al, Radiotherapy and Oncology, 2010 Courtesy of J. van Meerbeeck, K. Vandecasteele, W. De Neve C. Oberije et al, Radiotherapy and Oncology, 2010 Courtesy of J. van Meerbeeck, K. Vandecasteele, W. De Neve Methodological issues 1. 2. 3. 4. 5. 6. 7. No consensus on best NTCP models (e.g., simple vs. large model) Results not stated in comparable terms (e.g., NTCP model vs. DVH thresholds) Sometimes the ‘target’ tissues aren’t known Endpoint definitions can be questionable Results depend on typical dose distributions, which are evolving Implicit assumption of organ uniformity (ignoring stem cell rescue, etc.) Assumption that spatial dose pattern doesn’t matter 16