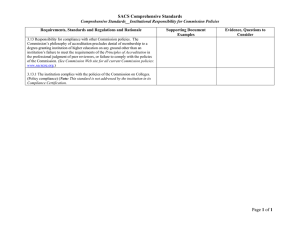
MR Accreditation Programs - E. Jackson Educational Objectives MRI Accreditation Programs:
advertisement

MR Accreditation Programs - E. Jackson Diagnostic - MRI Safety and Accreditation Educational Objectives MRI Accreditation Programs: An Overview of Each and Specifics of One At the conclusion of this presentation, the attendee should: – understand the MIPPA Advanced Diagnostic Imaging Accreditation requirements and choices of accrediting organizations – understand the current clinical and physics requirements of the modular d l ACR MRI accreditation di i program Edward F F. Jackson Jackson, PhD Department of Imaging Physics – understand the specific ACR program requirements for medical physicists / MR scientists, including CME requirements – understand the testing requirements for both the large and small ACR MRI accreditation phantoms, and – understand the annual physics testing requirements for the ACR MR accreditation program 1 2 Requirements of MIPPA Requirements of MIPPA • MIPPA – Medicare Improvements for Patients and Providers Act (passed in 2008) • Currently, the Centers for Medicare and Medicaid Services (CMS) specifically indicates that the advanced diagnostic imaging (ADI) accreditation can be provided by: • Section 135(a) calls for advanced diagnostic imaging accreditation of all facilities that bill the technical component of diagnostic MRI, CT, and nuclear medicine such as PET services – The Joint Commission – The Intersocietal Accreditation Commission – The American College of Radiology • Facilities must be accredited by January 1, 2012 • However, “all facilities” does not include hospitals • Each of these accreditation programs has its own requirements 3 4 The Joint Commission The Joint Commission • The Joint Commission provides Advanced Diagnostic Imaging accreditation as part of its program for accreditation of diagnostic imaging centers. • Per Joint Commission posted information, providers already accredited by The Joint Commission do not need to be accredited (for ADI) until their current accreditation expires.* • The ADI accreditation cost depends on the number of annual patient visits and number of sites (branches). Additional fees may be incurred for multiple modalities and sites.** • With respect to Standard EC.02.01.01 – The organization manages safety and security. – At a minimum, the organization manages safety risks in the magnetic resonance environment associated with the following: • Patients P ti t who h may experience i claustrophobia, l t h bi anxiety, i t or emotional ti l distress • Patients who may require urgent or emergent medical care • Metallic implants and devices • Ferrous objects entering the MRI environment * TJC online resource: Accreditation Handbook for Diagnostic Imaging Centers ** TJC online resource: Accreditation for Your Freestanding Imaging Center TJC online resource: Changes to Standards & EPs for Advanced Imaging Requirements 5 6 1 MR Accreditation Programs - E. Jackson The Joint Commission The Joint Commission • With respect to Standard EC.02.04.01 – The organization manages medical equipment risks. • No specific additional information is available regarding the specifics of The Joint Commission ADI accreditation for MRI. – The organization identifies activities and frequencies to maintain the reliability, clarity, and accuracy of the technical quality of diagnostic images produced. produced y conducted under the • It is stated that “All initial surveys Advanced Diagnostic Imaging Services survey option will be conducted on an unannounced basis.”* • With respect to Standard EC.02.04.03 – The organization inspects, tests, and maintains medical equipment. – The organization maintains the reliability, clarity, and accuracy of the technical quality of diagnostic images produced. TJC online resource: Changes to Standards & EPs for Advanced Imaging Requirements * TJC online resource: Accreditation Handbook for Diagnostic Imaging Centers 7 8 Intersocietal Accreditation Commission Intersocietal Accreditation Commission • Intersocietal Commission for the Accreditation of Magnetic Resonance Laboratories (ICAMRL) – created in 2000 • As of February 2012, the new name is “ICA MRI” • Offers accreditation in the areas of: – – – – – Cardiovascular MRI Breast MRI Body MRI (chest (non-cardiac), abdomen, pelvis, extremity) Musculoskelatal MRI Neurological MRI and MRA http://www.icavl.org/iac/forms/MIPPA_FAQ_Key_Elements.pdf http://www.intersocietal.org/mri/seeking/fees.htm 9 10 Intersocietal Accreditation Commission Intersocietal Accreditation Commission • Part I of the standard addresses: • The ICA MRI accreditation process does not “require purchase of a specific phantom. However, through the application process participating laboratories must provide documentation of their ongoing, comprehensive quality assessmentt programs.”” – Supervision and Personnel (training and CME requirements) • • • • – – – – • The ICA MRI standards are available online at: http://www.intersocietal.org/mri/seeking/mri_standards.htm http://www.intersocietal.org/mri/seeking/fees.htm Medical Director Medical Staff Technical Director Technical Staff Support Services (clerical, nursing, transport, etc.) Physical Facilities Examination Interpretation, Reports, and Records Safety and Patient Confidentiality http://www.intersocietal.org/mri/seeking/mri_standards.htm 11 12 2 MR Accreditation Programs - E. Jackson Intersocietal Accreditation Commission Intersocietal Accreditation Commission • Part I of the standard addresses (continued): • Part I of the standard addresses (continued): – Instrumentation – Quality Assurance • Devices must be FDA approved • MRI unit must be capable of performing multiplanar T1, T2, and STIR sequences with a FOV large enough to consistently image all relevant anatomy in the region of interest • The equipment specifications and performance must meet all state, federal, and local requirements (dB/dt, B0,max, max SPL, max SAR) • There must be a quality assurance program in the MR laboratory – Quality Assurance Committee role Quality y control tests,, standards,, thresholds,, timelines,, and results review – Q – Quality control tests should be performed according to the manufacturer’s performance standards by the MR technologist, service engineer, medical physicist, or qualified expert on a timely basis – Quality assurance documentation must be maintained at the MR laboratory and made available to all personal – Multiple Sites http://www.intersocietal.org/mri/seeking/mri_standards.htm http://www.intersocietal.org/mri/seeking/mri_standards.htm 13 14 Intersocietal Accreditation Commission Intersocietal Accreditation Commission • Part I of the standard addresses (continued): • Part I of the standard addresses (continued): – Quality Assurance – Quality Assurance • The quality assurance program must consist of MR system installation acceptance testing and major upgrade acceptance testing – Acceptance testing must be performed as part of the system installation and after major upgrades, prior to patient clinical use. – The manufacturer’s representative, service engineer, or the MR siteappointed medical physicist, or qualified expert, should perform the acceptance testing. – Acceptance testing should include, but is not limited to: B0 homogeneity, gradient and RF calibration, resonance frequency, slice thickness and accuracy, image quality (SNR for all coils, spatial resolution, artifacts, image uniformity, geometric distortion, monitor/processor QC) • Written report of the acceptance tests, signed and dated, must be maintained • Routine (daily and periodic) QC tests p function of audible and visual ppatient safety y equipment q p – Proper – Center frequency tests – SNR – Image uniformity – Artifact assessment – Deviations from established thresholds must be documented and corrective action taken where appropriate http://www.intersocietal.org/mri/seeking/mri_standards.htm http://www.intersocietal.org/mri/seeking/mri_standards.htm 15 16 Intersocietal Accreditation Commission Intersocietal Accreditation Commission • Part I of the standard addresses (continued): • Part II of the standard addresses: – Quality Assurance – Indications (body, cardiovascular, MSK, neurological, breast, MRA) – Techniques • Periodic preventive maintenance (PM) service is recommended for each MR scanner – PM quality control assessment should include, but is not limited to: • SNR, B0 homogeneity, RF calibration of all coils, spatial resolution, artifact assessment • General equipment inspection, e.g., RF coil cables, RF shielding, etc. – A complete report of PM, QC tests, and service records must be maintained and must be signed and dated by the person(s) performing the tests. • Ancillary equipment must be included as part of the QA program • • • • Positioning and coil selection Appropriate protocol & optimization of pulse sequence(s) for the indication Utilization of appropriate software, workstations, techniques, and measurements A complete, written description of each protocol must be maintained, including acquisition details, contrast agent administration, filming, etc. – Procedure Volumes – Technical and Interpretative Quality Assessment • Technical / Administrative Quality Assessment, including appropriate use criteria • Interpretative Quality Assessment – over-reads, correlation with outcomes, etc. http://www.intersocietal.org/mri/seeking/mri_standards.htm http://www.intersocietal.org/mri/seeking/mri_standards.htm 17 18 3 MR Accreditation Programs - E. Jackson Intersocietal Accreditation Commission Intersocietal Accreditation Commission • Application • Application – IAC agreement – Copies of various site policies – Acceptance testing results (at installation and/or after major upgrade). All acceptance tests completed after January 5, 2011 must include submission of the QC test t t results lt with ith the th phantom h t images. i – 5 days of daily quality control tests with the results and the phantom images – Preventative maintenance (PM) report (performed six months prior to application submission) – Two (2) months of QA meeting minutes (for facilities applying for reaccreditation) Note: All phantom images must be submitted on CD or DVD with a DICOM viewer. – Case Studies • EFFECTIVE 1/1/12 | Applicant facilities must submit six (6) total case studies for each MRI unit. Cases must represent each area of testing that is performed on the scanner, i.e., Cardiovascular MRI, Breast MRI, Body MRI [chest (noncardiac), abdomen, bd pelvis, l i extremity], i ] M Musculoskeletal l k l l MRI MRI, N Neurological l i l MRI, MRI MRA. MRA For example, if your facility is applying in two of the following testing areas you must submit 3 cases for each testing area; if your facility is applying in one testing area, you must submit 6 case studies total. • In addition, the printed or electronic final reports and MRI Scan Parameter Forms must be submitted. • Cases must have been obtained within the 12 months prior to the date of submission http://www.intersocietal.org/mri/seeking/case_studies.htm http://www.intersocietal.org/mri/seeking/required_items.htm 19 20 ACR Accreditation Programs ACR MRI Accreditation Overview – Purpose: • to set quality standards for practices and to help continuously improve the quality of patient care • to be educational in nature • History – – – – – 1996 – ACR MR program accreditation launched 2001 – Initial MR QC Manual released 2004 – Q QC Manual update p 2005 – 3-T magnets included 2006 – Documentation of QC and annual system performance evaluation required – 2008 – Modular program introduced – Beneficial for accrediting body and site • ACR assists sites improve practice • Site obtains PR benefit • Sites assist ACR in gathering information about MRI practices. 21 22 ACR MRI Modular Program ACR Accreditation Process Overview Submission materials: • Head • Spine • Musculoskeletal • Body • MR angiography • Cardiac Whole body (brain, C-spine, L-spine L spine, knee) – Scanner information – Most recent annual medical physicist performance report – Personnel qualifications q alifications and CME information – Clinical images for each module submitted – Phantom images with associated site scanning data form – Most recent quarter of QC data – $$$$ “Every unit must apply for all modules routinely performed on that unit for a facility to be accredited.” Note: Breast MR accreditation is included in the Breast Imaging Accreditation program 23 24 4 MR Accreditation Programs - E. Jackson ACR CME Requirements ACR MRAP Cost 25 Accreditation – First Unit $2400 (1-4 modules) $2600 (5 modules) $2800 (6 modules) Accreditation – Second Unit $2300 (1-4 modules) $2500 (5 modules) $2700 (6 modules) Repeat $800 per unit for clinical or phantom $1600 for both Add units or module (mid-cycle) $1600 per unit 26 Clinical Images Clinical Images Examination Choices for MRAP by module: Examination Choices for MRAP by module: - see “MRI Accreditation Program Requirements” file on ACR website, p. 12 of 15 - see “MRI Accreditation Program Requirements” file on ACR website, p. 12 of 15 27 28 ACR Accreditation Process Overview Clinical Images Evaluated for 1) appropriate pulse sequence and contrast, 2) filming technique (if appropriate), 3) anatomic coverage and imaging planes, 4) spatial resolution, 5) artifacts, and 6) appropriate labeling of images Must be submitted in DICOM format on CD with embedded viewer. Requirements for viewer must are provided in the ACR MRI Clinical Image Quality Guide. 29 30 5 MR Accreditation Programs - E. Jackson ACR Accreditation Process Overview ACR Accreditation Process Overview Phantom Images – Discussed in detail on subsequent slides • Annual MRI System Performance Evaluation – Must be performed by a medical physicist / MR scientist – Includes MRAP phantom scans and tests required for weekly QC and specific tests of: • Magnetic field homogeneity • Slice thickness and position accuracy • Radiofrequency coils – Acquired on ACR MR Accreditation Phantom using specified T1- and T2-weighted protocols plus the site’s T1- and T2weighted protocols (for brain imaging). – Must be submitted in DICOM format on CD-ROM (w/o embedded viewer; no image compression) – Evaluated for 1) geometric accuracy, 2) high contrast spatial resolution, 3) slice thickness accuracy, 4) slice position accuracy, 5) signal uniformity, 6) ghosting, 7) low contrast detectability. – SNR – all coils – Uniformity – all volume coils • Soft-copy displays (monitors) – Should also provide an assessment of MR safety issues at the facility 31 32 ACR MR Accreditation Phantom ACR Phantom Scan Documentation Contains information on: • Phantom position • Pulse sequences q to be used • Filming and data preparation instructions Sent to site with Full Application Large Phantom: $1050 Small Phantom: $ 780 (Ortho) Available from the ACR (as of 2/10/2012) http://www.acr.org/accreditation/mri/mri_qc_forms.aspx 43 44 ACR Phantom Scan Documentation Alignment of the ACR Phantom Alignment is important! Contains information on: • Test analysis • Performance criteria • Common reasons for failure • Center phantom in head coil – use foam, stack of paper, paper towels, or cardboard • Make sure phantom is straight – use bubble level • Make sure phantom is centered SI, LR & AP Sent to site with Full Application – make localizer images in all 3 planes – use grid to check centering Available from the ACR http://www.acr.org/accreditation/mri/mri_qc_forms.aspx • Record position for future use 45 46 6 MR Accreditation Programs - E. Jackson ACR Phantom Scans ACR Accreditation Process Overview • Sagittal Localizer #1 #7 #8 #10 #11 – TE/TR=20/200ms, 25 cm FOV, 256x256, 1 20-mm, 1 NEX, 0:56 • ACR T1 Axial Series – TE/TR TE/TR=20/500ms, 20/500 25 cm FOV FOV, 256x256, 256 256 11 55-mm slices li (graphically prescribed), 1 NEX, 2:16 #9 #5 • ACR T2 Axial Series – TE1/TE2/TR=20/80/2000ms, 25 cm FOV, 256x256, 11 5-mm slices (same locations as for ACR T1 series), 1 NEX, 8:56 #1) Slice thickness and position, geometric accuracy, high contrast resolution #5) Geometric accuracy #7) Percent image uniformity, ghosting #8-11) Low contrast object detectability, and slice position (in #11) • + Site T1 and T2 Axial Brain Series 47 48 Geometric Accuracy ACR T1 Slice 1 Slice Position ACR T1 & T2 True Dimension: 190 mm True Dimension: 148 mm Sag Loc Slice 5 Set WW & WL to min, then raise WL until 1/2 water is dark (mean) Set WW to mean and WL to 1/2(mean) Criterion: ± 2 mm Slice 1 49 Slice 11 Criterion:<5mm 50 Slice Thickness Slice Thickness ACR T1 & T2 Slice 1 Measurements: • lower level to ½ average • set window width to minimum • measure lengths of top and bottom ramps • calculate slice thickness Two 10:1 ramps 2 4x •Magnify image by 2-4x. •Define two ROIs, one on each ramp. •Obtain average intensity from the two ROIs. Criterion: 5.0±0.7 mm 51 52 7 MR Accreditation Programs - E. Jackson Spatial Resolution Matrix: Registration with Phantom High Contrast Spatial Resolution ACR T1 & T2 Slice 1 • Magnify by 2-4x. • Use UL for horizontal resolution and LR for vertical resolution. • Must be able to resolve 1.0 mm holes vertically and horizontally. Resolution Holes UL 1.1 1.0 0.9 mm Image Matrix LR Image compliments of Geoff Clarke, PhD 53 54 Low Contrast Detectability Low Contrast: High vs. Low Field ACR T1 & T2 0.3 T 1.5 T Slices 8-11 Slice 8: Slice 9: Slice 10: Slice 11: 1.4% 2.5% 3.6% 5.1% ≤1.5T Criterion ≥ 9 spokes 3.0T Criterion ≥ 37 spokes Slice 11 - ACR T1 series 55 56 Percent Image Uniformity Ghosting ACR T1 & T2 ACR T1 Slice 7 Slice 7 Ghost ratio = |(top+bottom) - (left+right)| (2 large ROI) (~1 cm2) Large ROI (195-205 cm2) ≤1.5T (high low) percent integral uniformity = 100 1 (high low) Criterion: PIU 87.5% Criterion: 0.025 3.0T Criterion: PIU 82% ROIs ~ 10 cm2 with ~4:1 length:width 57 58 8 MR Accreditation Programs - E. Jackson Ghosting Common Problems and Artifacts Window and level to make sure ROIs are in background noise! (Warping of image space due to gradient nonlinearity corrections.) 59 60 Potential Causes of Geometric Accuracy Failures • Poor phantom positioning - relatively common problem • Poor gradient calibration • Bo inhomogeneity • • Poor Positioning Rotation (in-plane) F Ferromagnetic ti objects bj t in i magnett Poor magnet shimming • Gradient non-linearity (not appropriately corrected) • Inappropriate receiver bandwidth • Poor eddy current compensation • Combination of two or more of above 61 62 Poor Positioning Poor Positioning Rotation (through-plane, RL) Rotation (through-plane, AP) 63 64 9 MR Accreditation Programs - E. Jackson Sources of Geometric Distortion Spatial Accuracy • System Limitations – Poor Bo homogeneity Be sure to make sagittal measurements at the center of the phantom (or as close as possible to the center). – Linear scale factor errors in the gradient fields – Field distortion due to induced eddy currents – Nonlinearities of the gradient fields • Object-Induced – Chemical shift effects – Magnetic susceptibility variations (patient induced) 65 66 Air Bubbles Low Acquisition Bandwidth When a large air bubble is present in the phantom, geometric distortion measurement may have to be taken along diagonal instead of vertical. Note distortion as well as increased susceptibility artifacts. 67 68 Spatial Resolution Matrix: Registration with Phantom Air Bubbles Resolution Holes Image Matrix 16 kHz 8 kHz Image compliments of Geoff Clarke, PhD 69 70 10 MR Accreditation Programs - E. Jackson High-Contrast Spatial Resolution Image Intensity Uniformity Common causes of failure; • Incorrect FOV or matrix size • Poor P gradient di t calibrations lib ti • Excessive filtering (smoothing) • Poor eddy current compensation • Gradient amplifier instability Big ROI ~ 195 cm2 (19,500 mm2) Small ROI’s ~ 1 cm2 (100 mm2) Max Signal Min Signal ACR phantom - Slice #7 71 72 Image Intensity Uniformity Percent Signal Ghosting Common causes of failure: Poor phantom centering in coil (usually in AP direction) Ghosting Motion or vibration Mechanical failure in head coil • Must pass on slice #7 of ACR T1-weighted axial series. • Ghost signal is measured and reported as percentage of the signal in the true image • Excessive ghosting in other images may be counted as “Unacceptable Artifact” Note: Uniformity becomes poorer with increasing Bo (especially above 2 T) because of dielectric field focusing phenomenon (aqueous phantom). 73 74 Ghosting is Nonspecific Phase Ghosting • Instability in MRI signal from pulse to pulse NOISE Phase • Phantom motion • Loose connections or bad cable GHOST GHOST Readout • Partial failure of radiofrequency coils or gradient subsystem • Pulse sequence calibration error – Eddy currents in Fast Spin Echo series NOISE Image compliments of Geoff Clarke, PhD 75 76 11 MR Accreditation Programs - E. Jackson Ghosting Low Contrast Detectability ACR T1 & T2 Ghosting may obscure otherwise visible LCD spokes Slice 8: 1.4% Slice 9: 2.5% Slice 10: 3.6% Slice 11: 5.1% Image compliments of Geoff Clarke, PhD 77 78 Low Contrast Detectability DC Offset Artifacts Some common causes of failure: – Incorrectly positioned slices Contrast based on partial volume averaging Large artifact off to side. NEX=1; frequency shifted – Tilted phantom – Incorrect slice thickness – Ghosting – Inadequate SNR Image compliments of Geoff Clarke, PhD 79 80 Susceptibility Artifacts Details of the ACR MRI QC Manual Small inclusions in LCD insert can make analysis difficult. 81 82 12 MR Accreditation Programs - E. Jackson MRI QC Manual Overview Quality Assurance Manual Current Version: 2004 Should contain the following: • Responsibilities and procedures for QC testing. • Records of the most recent QC tests. • A description of the orientation program procedures for use and maintenance of the equipment. • MRI techniques to be used. • Precautions in place to protect the patient. • Proper maintenance of records, including records of testing, equipment service, and QA meetings. • Procedures for cleaning and disinfection. • Radiologist’s Section Describes requirements and the role in a QA program • Technologist’s Section Outlines the recommended daily and weekly QC tests • Physicist’s / MRI Scientist’s Section Suggestions for setting up a QC program Outlines recommended annual equipment performance tests 83 84 Radiologist’s Responsibilities Radiologist’s Responsibilities (cont.) • To ensure adequate training and continuing education in MRI • To arrange staffing and scheduling so that QC tests can be carried out. • To provide an orientation program for technologists • To provide feedback to the technologists. • To ensure that an effective quality control program exists for all MRI procedures • To review the technologist’s test results • To select the technologist to be the primary quality control technologist • To oversee or designate a qualified individual to oversee the safety program. • To ensure that appropriate test equipment and materials are available to perform the technologist’s QC tests. • To ensure that records are properly maintained and updated in the MRI QC procedures manual. • To T select l a qualified lifi d medical di l physicist h i i or MRI scientist. i i 85 86 Technologist’s Responsibilities Technologist’s Responsibilities • Medical Physicist/MR Scientist interactions: • Daily (weekly*) MR image QC procedures – Physicist assures correct implementation an execution of the QC procedures – Physicist reviews QC notebook at least annually (quarterly preferred) • QC of hard and soft copy images • Routine visual inspection of equipment • Radiologist interactions: – Radiologist informs technologist about image quality problems – Radiologist decides whether or not patient studies can continue – Radiologist participates in the initial assessment of image quality and regularly monitors the QC results in the intervals between annual reviews • Note: Effective May 2, 2002, the performance of daily QC tests is NOT required. All daily tests mentioned in the QC Manual are now required at least weekly (but daily testing is encouraged). 87 88 13 MR Accreditation Programs - E. Jackson Medical Physicist’s Responsibilities Details of the Technologist’s Responsibilities • Write purchase specifications • Perform acceptance testing and establish baseline QC measurements • Determine action limits for measured parameters • Setup daily/weekly QC tests • Perform annual MRI equipment performance reviews 89 90 Technologist’s Section Technologist’s Section • Identification of the designated QC technologist(s) • Maintenance of the QC Notebook – Q QC ppolicies and pprocedures – Data forms where QC procedure results are recorded – Notes on QC problems and corrective action(s) • Document QC data review • Alternative phantoms and procedures • Action limits 91 92 Technologist’s Section Technologist’s Section • Routine tests using ACR phantom and ACR T1-weighted head scan: – Center frequency – Geometric and ppositioningg accuracyy – Image quality (daily/weekly) ((daily/weekly) y y) (daily/weekly) 17 min • High contrast resolution • Low contrast object detectability – Artifact evaluation (daily/weekly) • Plus: – Processor sensitometry – Physical and mechanical inspection (weekly) (weekly) 93 94 14 MR Accreditation Programs - E. Jackson Technologist’s Section Technologist’s Section Daily (Weekly) Daily (Weekly) (cont) – Record central frequency and transmit gain (attenuation) settings for the ACR axial T1 series. – Check position accuracy by ensuring central grid structure is within 2 mm of the center of the image – Verify geometric accuracy by ensuring length (sagittal localizer image) and vertical/horizontal diameter (axial slice #5) measures are within 2 mm of true values – Verify high contrast resolution (vertical and horizontal) using T1 series axial slice #1 – Verify low contrast object detectability levels using T1 series axial slice #8, 9, 10, or 11 (as determined by physicist/MR scientist) – Assess level of image artifacts in axial T1 series • Phantom should appear circular • There should be no ghost images in the background or overlying the phantom image • There should be no streaks or artifactual bright or dark spots in the image • There should be no unusual or “new” features in the image. 95 96 Daily Tests - Transmitter Gain and Frequency Daily Axial ACR T1 Series • • • • • • • • Spin-echo sequence TE/TR=20/500ms Slice thickness / gap = 5/5 mm 11 slices graphically prescribed from sagittal localizer FOV = 25 cm Matrix: 256x256 1 average (NEX, NSA, etc.) Scan time: 2:16 min • During the prescan for the T1 series, the scanner determines the appropriate transmitter gain (or attenuation) and transmit (center) frequency. • On some scanners, these h values l are easily il obtained b i d at the h end of prescan and/or from the series text page. • On other scanners, these values will need to be obtained from special options (see service engineer). • The transmit gain (attenuation) value and center frequency value should be recorded daily. 97 98 Daily Tests - High Contrast Spatial Resolution Daily Tests - Geometric Accuracy True Dimension: 190 mm • Magnify by 2-4x. • Use UL for horizontal resolution and LR for vertical resolution. • Must be able to resolve 1.0 mm holes vertically and horizontally. True Dimension: 148 mm UL 1.1 1.0 0.9 mm Sag Loc Slice 5 Set WW & WL to min, then raise WL until 1/2 water is dark (mean) Set WW to mean and WL to 1/2(mean) LR Criteria: ± 2 mm 99 100 15 MR Accreditation Programs - E. Jackson Daily Tests - Low Contrast Detectability Daily Tests - Assessment of Artifacts Count and record the number of spokes in the slice determined by the Medical Physicist or MR Scientist. (Typically (T i ll slice li 11 for f low l field and slice 8 or 9 for high field.) • Look at all slices from the localizer and axial T1 series. • Modify window width and level to look for ghosting artifacts if andd radiofrequency di f interference i f artifacts. if • Note any change in image quality relative to baseline scans. Action criteria: Change of more than 3 spokes (or as determined by QC procedure). 101 102 Technologist’s QC Log - Daily Tests Weekly Tests - Processor QC Weekly y Tests SMPTE Pattern Gray Level Ring 103 104 Weekly Tests - Processor QC Weekly Tests - Processor QC Weekly Hard Copy QC Tests: • Display SMPTE test pattern. • Visually examine the SMPTE pattern (0/5% and 95/100% patches). • Measure the optical density (OD) of the 0, 10, 40, and 90% gray level patches with a densitometer. • Plot OD values on the Laser Film QC Chart. • Inspect film for streaks, uneven densities, and other artifacts. 105 107 16 MR Accreditation Programs - E. Jackson Weekly Tests - Visual Inspection RF Shielded Room Door At least weekly visual inspection tests: • The RF door “fingers” provide good electrical contact of the shielded door and the rest of g shield. the Faradayy cage • Check patient table, patient communication, patient “panic buttons”, transport, alignment, and system indicator lights • Check RF room integrity (particularly RF doors) • If the fingers are damaged, as they will inevitably be, the effectiveness of the shield decreases and will ultimately give rise to RF interference artifacts (or cause them on an adjacent scanner!). • Check that emergency cart, safety lights, signage, and patient monitors (and supplies) are present and in working order • Check that all RF coils are present and in apparent good working condition (no frayed cables, etc.) 108 109 RF Coil Weekly Checks • Be sure to check all cables on RF coils, particularly high use and/or flexible coils. coils • Any suspicious coils, cables, or connector boxes should be reported immediately to your service organization and/or vendor’s service engineer. 110 Technologist’s QC Summary Some Details of the Medical Physicist’s / MR Scientist’s Responsibilities • Technologist runs QC runs on a daily (weekly) basis, and records the results in the QC logbook. • If any test result exceeds the appropriate action limit (established by Medical Physicist/MR Scientist), repeat QC test. If still fails, notify service (and log service call). • Action criteria are usually set based on 10 or more repeated measurements. 112 113 17 MR Accreditation Programs - E. Jackson Medical Physicist/MR Scientist Responsibilities Medical Physicist/MR Scientist Responsibilities • Performs acceptance tests – New systems before first patient scan – Following any major hardware or software upgrade • Laser camera QC – Establish operating levels (in consultation with laser film system service engineer) • Acquires baseline QC data acquisition and establishes action limits – – – – – • Acquire baseline data (using SMPTE test pattern) Central frequency Transmitter gain / attenuation Geometric accuracy High contrast resolution Low contrast object detectability • Corrective actions – Determination of whether problem lies in the camera, processor, and/or MR system • Artifact analysis 114 115 Medical Physicist/MR Scientist Responsibilities Magnetic Field Homogeneity Annual Physics Tests – – – – Ideal Homogeneity Magnetic field homogeneity Slice position accuracy Slice thickness accuracy RF coil il checks h k Poor Homogeneity FWHM FWHM • Signal-to-noise ratio (all coils) • Image uniformity (volume coils) – – – – Good Homogeneity o Interslice RF interference Phase stability (ghosting) Soft copy displays (monitors) Assessment of MR safety program Denotes a totally uniform magnetic field. All signal is at resonant frequency, o. 116 o o Fourier transform of signal produces a Lorentzian peak in well-shimmed magnet Magnet field homogeneity can be characterized using FWHM of resonance peak 117 Magnetic Field Homogeneity Magnetic Field Homogeneity One vendor’s “head equivalent” phantom. With sphere in head coil, use manual prescan. p can be Insert sphere used for homogeneity test. Adjust center frequency twice to determine the “full width at half maximum” of the spectrum. (Remove sphere from cylindrical “loader” first. Place at isocenter in head coil.) 118 119 18 MR Accreditation Programs - E. Jackson Magnetic Field Homogeneity Magnetic Field Homogeneity LVshim Report Phase images from GRE sequences with 10ms difference in TE’s Exam 50196, Series 2, Image 1 (Fri Jan 24 20:35:23 1997) Sc dw d = 200 00 Hz Scan Bandwidth Field of View = 50 cm Phase and Unwrapped Phase Images The change in phase across the phantom is proportional to the inhomogeneity of the magnetic field. Sampling Diameter = 22 cm Inhomogeneity 3.19 Hz (0.050 ppm) Harmonic Coefficients given for Z1, Z2, Z3, Z4, Z5, Z6, X, Y, ZX, ZY, X2-Y2, XY, Z2X, Z2Y, ZXY, etc. 120 121 Magnetic Field Homogeneity Slice Position Accuracy • Either the FWHM technique (on a given spherical phantom) or the phase difference technique can be used to assess homogeneity if possible at a given site. Slice Spacing Slice Position • Alternative: Use the service engineer’s report on homogeneity for your site records of homogeneity. SLICE #11 SLICE #1 Crossed wedges should be of equal length if position and spacing are accurate (and phantom is not tilted!) 122 123 Slice Thickness MRI Equipment Performance Evaluation Site & Equipment Data Site: _____________________________ MRAP Number: ____________________ Date: ________ Serial Number: ___________ Equipment: MRI System Manuafacturer: _________________ Model : ________ Processor Manufacturer : _________________ Model: _________ PACS Manufacturer: Measurements: _________________ Model: _________ ACR MRAP Phantom Number used: _________ 1. Magnetic Field Homogeneity Bo Homogeneity • lower level to ½ average • set window at minimum • measure lengths of top and bottom ramps • calculate slice thickness Method Used (check one): Spectral Peak ___ Phase Difference ___ Other (desc ribe) __________________________ Measured Homogeneity: Diameter of Spherical Volume (cm) Homogeneity (ppm) ________ ________ ________ Slice Position Accuracy Slice Thickness Accuracy 124 _______ _______ _______ 2. Slice Position Accuracy From Slice Positionss #1 and #11 of the ACR Phantom: - Wedge (mm) =- =+ Slice Location #1 ________ Slice Location #11 ________ = =+ 3. Slice Thickness Accuracy From Slice Position #1 of the ACR Phantom: Slice Thickness Top ______ Bottom ______ (fwhm in mm) Thickness (mm) ______ Duplicate these forms so they will be available for repeated use. 19 Calculated slice MR Accreditation Programs - E. Jackson Volume Coils SNR, Uniformity, and Ghosting Volume RF Coil Measurements • Uniformity performance criteria: PIU 90% Must assess SNR, uniformity, and ghosting h i ratio i for every volume coil. (high low) percent integral uniformity = 100 1 (high low) • SNR (no fixed criteria) (Mean Signal ROI) / (SD of Noise ROI) • Percent Signal Ghosting Left Right Top Bottom ACR Phantom Slice #7 100 126 2 Mean Signal 127 Phased-Array Coils Breast Phased Array Phased-Array Coils Wrist Phased Ph dA Array Torso Phased Array Example of a particular vendor’s C-T-L spine phased array coil QC phantom Head-Neck-Spine Phased Array 128 129 Surface RF Coil Measurements Volume Coil Data % Image Uniformity Max Signal Min Signal Signal-to-Noise Mean Signal SD of Background Signal Percent Signal Ghosting Ghost Signal M Mean Si Signall Background Signal Maximum Signal-to-Noise Maximum signal SD of Background Signal Surface Coil Data 130 20 MR Accreditation Programs - E. Jackson Soft Copy Displays 4 . RF Coil Perform ance Evaluation A. VOLUME R F CO IL RF Coil D escription: __________________________ Date: ____________ Phantom Description: ___________________________________________ Volume Coil Pulse Sequence: degrees Type: ____ FO V: _____ cm 2 TR: _____ TE: ______ flip angle _____ Matrix: ___________ BW : _________kHz ; N SA ___ Slice thickness ______m m; spacing _______ mm Calculated Values: Uniformity SNR Ghosting TX attenuation (or gain) __________ Data Collected: Mean Signal M axim um Signal Minim um Signal Background Signal Noise Standard Deviation G host Signal • Requires precision luminance meter Calculated Values: Signal-to-Noise Ratio Percent Image Uniformity Percent Signal G hosting B. R F SU RFACE CO IL - • Four tests: RF Coil D escription: __________________________ Date: ____________ Phantom Description: ___________________________________________ Pulse Sequence: Surface Coil Calculated Value: Maximum SNR Type: ____ TR : _____ TE: ______ FO V: _____ cm – – – – 2 Matrix: ___________ BW : _________kHz ; NSA ___ - Slice thickness ______m m; spacing _______ mm TX attenuation (or gain) __________ M axim um Signal Noise Standard D eviation Image uniformity distribution O K? ________ Image ghosting O K? ________ HARD CO PY IMAG E: W indow width ________ Maximum Signal-toNoise Ratio Maximum and minimum luminance Luminance uniformity Resolution (SMPTE) Spatial accuracy (SMPTE) W indow level _______ Several copies of this page m ay be required to report on all RF coils. 133 Soft Copy Displays 5. Interslice RF Interference Phantom Description: ___________________________________________ Pulse Sequence: Type: ____ TR: _____ TE : ______ FOV: _____ cm 2 M atrix: ___________ BW : _________kHz ; NSA ___ RF Slice Interference S li c e Gap (m m ) 10 0 % S i g na lto - N o i s e R a tio M e a sure d SNR • Max luminance (WL/WW min): 90 Cd/m2 Number of slices______ S e rie s Num ber 1 2 90 % 80 % 3 • Min luminance: <1.2 Cd/m2 4 • Luminance uniformity: Each of the lluminance minance values al es obtained at the fo fourr corners of the screen should be within 30% of the maximum value measured at the center (WL/WW min). 70 % 0% 25 % 50% 7 5% 1 00 % In te r- sl ic e G a p (p e r c e n t o f sl ic e th ic k n e s s ) 6. Soft Copy Displays M onitor Description: __________________________________________ Soft S ft Copy C Displays -2 2 M axim i um L Luminance: i ________________________ Cd m . -2 M inim um Luminance: _________________________ Cd m . Lum inance Uniform ity: -2 Average of values obtained in four corners of screen: ______ Cd m . Lum inance measured in center of screen: -2 ______ Cd m . Percent difference: ________ % - Review of Routine QC Program • Resolution: Use SMPTE 100% contrast patterns (see QC manual, p. 117). • Spatial accuracy: Use SMPTE grid pattern (see QC manual, p. 117). |(Center – Average Corners)/(Center) x 100% < 30% | 7. Evaluation of Site’s Technologist Q C Program 4) Set up and positioning accuracy: (daily) 5) Center Frequency: (daily) 6) Transm itter Attenuation or G ain: (daily) 7) Geom etric Accuracy M easurements: (daily) _________ _________ _________ _________ 8) Spatial Resolution Measurem ents: (daily) _________ 9) Low Contrast Detectability: (daily) _________ 10) Film Q uality Control (weekly) _________ Visual Checklist: (weekly) _________ 134 ACR MRI QC Program Summary M RI Equipm ent Evaluation Sum m ary Site ___________________ Report Date: __________ System MRAP #_____________ Survey Date: __________ M RI System Manufacturer ___________ Model: __________ Physicist/M RI Scientist: ____________________ Signature: ________________________________ • Technologist Equipm ent Evaluation Tests Summary Sh t Sheet 1. Magnetic Field Homogeneity: 2. Slice Position A ccuracy 3. S lice Thickness Accuracy 4. RF Coils’ Performance a. Volume Coils’ S ignal-to-Noise Ratio b. Volume Coils’ Image Uniformity c. V olum e Coils’ Ghosting Ratios d. Surface Coils’ Signal-to-Noise Ratio 5. Inter-slice RF Interference 6. S oft copy displays P ass / Fail _________ _________ _________ – Performs daily (weekly) tests to assess image quality using the ACR phantom – Performs weekly tests of hard copy output – Maintains M i t i QC notebook!! t b k!! _________ _________ _________ _________ _________ _________ M di l Ph Medical Physicist’s i i t’ or MRI S Scientist’s i ti t’ R Recom m endations d ti for f Q uality Im provem ent: ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ ______________________________________________ • Medical Physicist / MR Scientist – – – – Runs baseline tests of system performance Sets action limits for daily ACR phantom tests Performs annual system performance tests Reviews all QC program data annually 137 21 MR Accreditation Programs - E. Jackson ACR MRI QC Program Summary • Radiologist – Ultimately responsible for all QA for the facility • All measurements, problems reported, and actions required to resolve the problems must be recorded for review, as must all preventive maintenance and repair records from the vendor or service organization. 138 22