The Physiology of Glucagon-like Peptide 1
advertisement

Physiol Rev 87: 1409 –1439, 2007; doi:10.1152/physrev.00034.2006. The Physiology of Glucagon-like Peptide 1 JENS JUUL HOLST Department of Medical Physiology, The Panum Institute, University of Copenhagen, Copenhagen, Denmark I. II. III. IV. V. VI. Introduction and Historical Overview Proglucagon Gene Expression, Posttranslational Processing, and Chemical Structures Proglucagon Distribution Measurement, Release, and Metabolism Regulation of Secretion Effects of Glucagon-like Peptide 1 A. The GLP-1 receptor B. The incretin effect C. Effects on the beta-cells D. Effects on glucagon secretion E. Effects on the gastrointestinal tract F. Central targets for peripherally released GLP-1 G. Effects on appetite and food intake H. Other effects I. Whole body effects, peripheral effects, and effects on insulin action VII. Glucagon-like Peptide 1 Pathophysiology A. Obesity B. Reactive hypoglycemia C. Diabetes 1409 1411 1412 1413 1414 1416 1416 1417 1418 1420 1421 1422 1423 1424 1426 1427 1427 1428 1428 Holst JJ. The Physiology of Glucagon-like Peptide 1. Physiol Rev 87: 1409 –1439, 2007; doi:10.1152/physrev.00034.2006.— Glucagon-like peptide 1 (GLP-1) is a 30-amino acid peptide hormone produced in the intestinal epithelial endocrine L-cells by differential processing of proglucagon, the gene which is expressed in these cells. The current knowledge regarding regulation of proglucagon gene expression in the gut and in the brain and mechanisms responsible for the posttranslational processing are reviewed. GLP-1 is released in response to meal intake, and the stimuli and molecular mechanisms involved are discussed. GLP-1 is extremely rapidly metabolized and inactivated by the enzyme dipeptidyl peptidase IV even before the hormone has left the gut, raising the possibility that the actions of GLP-1 are transmitted via sensory neurons in the intestine and the liver expressing the GLP-1 receptor. Because of this, it is important to distinguish between measurements of the intact hormone (responsible for endocrine actions) or the sum of the intact hormone and its metabolites, reflecting the total L-cell secretion and therefore also the possible neural actions. The main actions of GLP-1 are to stimulate insulin secretion (i.e., to act as an incretin hormone) and to inhibit glucagon secretion, thereby contributing to limit postprandial glucose excursions. It also inhibits gastrointestinal motility and secretion and thus acts as an enterogastrone and part of the “ileal brake” mechanism. GLP-1 also appears to be a physiological regulator of appetite and food intake. Because of these actions, GLP-1 or GLP-1 receptor agonists are currently being evaluated for the therapy of type 2 diabetes. Decreased secretion of GLP-1 may contribute to the development of obesity, and exaggerated secretion may be responsible for postprandial reactive hypoglycemia. I. INTRODUCTION AND HISTORICAL OVERVIEW The glucoregulatory hormone glucagon was discovered in 1923 as a hyperglycemic substance present in pancreatic extracts (196). Subsequent research indicated that hyperglycemic substances were also present in exwww.prv.org tracts of the gastrointestinal mucosa, and Sutherland and DeDuve suggested in 1948 (276), based on bioassays, that gastric extracts might contain glucagon, a finding that was confirmed in several subsequent studies. Furthermore, endocrine cells that resemble the pancreatic A-cells were reported to be present in the gastrointestinal mucosa (225). Upon the advent of the radioimmunoassay for glu- 0031-9333/07 $18.00 Copyright © 2007 the American Physiological Society 1409 1410 JENS JUUL HOLST cagon, one of the first radioimmunoassays to be developed (296), it was confirmed that the gastrointestinal tract contains substances with glucagon immunoreactivity, i.e., reacting with the antibodies employed in the radioimmunoassay (297). In addition, in immunohistochemical studies, some intestinal endocrine cells could be stained using glucagon antibodies (83), but it was also shown that these cells differed from the pancreatic A-cells with respect to granule morphology (83), and they were hence designated as “L-cells” (26). Furthermore, in 1968, it was established (298) that the glucagon-like immunoreactive material that was secreted in response to an oral glucose load differed from true glucagon both physicochemically and biologically. Furthermore, it was demonstrated that this “gut glucagon-like immunoreactivity” was heterogeneous, consisting of at least two distinct moieties differing in molecular size (301). Through contributions from independent groups, it was eventually demonstrated that the two predominant molecular forms of gut glucagon-like immunoreactivity both contain the entire 29-amino acid glucagon sequence (13, 114, 116, 281) (see Fig. 1). One has a COOHterminal octapeptide extension, and the other has the same COOH-terminal extension plus an NH2-terminal extension of 30 amino acids. The former molecule was named oxyntomodulin because of its effects on the oxyntic mucosa in some species (13), and the latter was designated glicentin partly because of its glucagon-like immunoreactivity and partly because it was first thought to consist of 100 amino acids (274). Full sequence analysis, however, revealed it to consist of 69 amino acids (281). The NH2-terminal extension of glucagon in glicentin was identified also in extracts from the pancreas, from which it was shown to be secreted in parallel with glucagon (193, 282). Conceivably, therefore, glicentin was a proglucagon, a biosynthetic precursor for glucagon, which in the pancreas was cleaved to glucagon and equimolar amounts of the NH2-terminal extension peptide, which was named glicentin-related pancreatic polypeptide (GRPP) (282). From studies of the biosynthesis of glucagon in the pancreatic islets, however, it was evident that a large molecule (mol wt ⬃10,000), subsequently designated “the major proglucagon fragment” (MPGF) that did not contain the glucagon sequence, was also formed in parallel with glucagon (236). As the structures of glucagon-encoding mRNA and of the glucagon gene were determined (14, 15), it became evident that, in mammals, this major fragment of proglucagon contains two glucagon-like sequences, now designated glucagon-like peptides 1 and 2 (GLP-1 and GLP-2, respectively). For a while it was thought that the GLP-2 moiety was an evolutionary late addition to the gene, since fish and bird proglucagon appeared to contain only a single glucagon-like peptide corresponding to GLP-1 (172). Subsequent research, however, established that the proglucagon genes in these species (there are two glucagon encoding genes in fish) also contain the GLP-2 encoding sequence, which, however, is sequestered by differential splicing upon pancreatic expression of the gene (142) but remains in sequence upon intestinal expression. In further studies of the processing and secretion of proglucagon products in humans and other mammals, it was confirmed that, in the pancreas, the two glucagon-like peptides are contained in a single large molecule, the major proglucagon fragment, secreted in parallel with glucagon (121, 189, 227, 229). In the intestinal mucosa, however, the two glucagon-like peptides are formed and secreted separately, whereas the NH2-terminal part of the precursor, i.e., the part that corresponds to glicentin, remains uncleaved (189, 227) or partly cleaved into GRPP and oxyntomodulin (see Fig. 1). This review deals with the physiology and pathophysiology of GLP-1. FIG. 1. Differential posttranslational processing of proglucagon in the pancreas and in the gut and brain. The numbers indicate amino acid positions in the 160-amino acid proglucagon sequence. The vertical lines indicate positions of basic amino acid residues, typical cleavage sites. GRPP, glicentin-related pancreatic polypeptide; IP-1, intervening peptide-1; IP-2, intervening peptide-2. Physiol Rev • VOL 87 • OCTOBER 2007 • www.prv.org THE PHYSIOLOGY OF GLUCAGON-LIKE PEPTIDE 1 II. PROGLUCAGON GENE EXPRESSION, POSTTRANSLATIONAL PROCESSING, AND CHEMICAL STRUCTURES The structure of proglucagon was deduced from the sequence of the cDNA encoding hamster proglucagon (15) and the human proglucagon gene (14). Also the murine and bovine genes were cloned (105, 171). Apparently, only a single gene encodes proglucagon in mammalian species, and identical mRNAs are produced in the pancreas and the intestines (189, 221). The differences in the proglucagon products in these tissues are, therefore, due to tissue-specific, differential, posttranslational processing of proglucagon (189, 227). The proglucagon gene is also expressed in certain neurons in the nucleus of the solitary tract in the brain stem (161). Recent studies have shed some light on the mechanisms that result in the tissue specificity and the mechanisms that regulate the expression of the proglucagon gene in the gut in vivo. Thus it has been established that the transcription factor pax6 is expressed in intestinal endocrine cells and activates proglucagon transcription (292). Mice with a dominant negative pax6 mutation exhibit a total absence of gut endocrine cells expressing GLP-1 or GLP-2. Disruption of the pax6 gene disrupts both islet development and selectively eliminates the endocrine cell population of the small and large bowel, including the proglucagon-producing cells (111, 292). Yi et al. (338) recently demonstrated that -catenin, the major effector of the Wnt signaling pathway, activates proglucagon expression in intestinal, but not in islet cells. Furthermore, this effect was mediated by the transcription factor TCF-4, which is highly expressed in intestinal endocrine cells, but not in islets. Both TCF-4 and -catenin bind to the proglucagon gene promoter, and a dominant negative TCF-4 repressed proglucagon expression in an intestinal cell line that expresses proglucagon and produces GLP-1 (338). It is of interest that ⬃1,250 nucleotides of the rat proglucagon gene promoter direct the expression to pancreatic islets and neurons of the brain, whereas additional upstream sequences extending to ⫺2,250 are required for expression of the gene in intestinal endocrine cells (166). However, the mechanisms regulating tissue specific proglucagon gene expression in humans appear to differ from those described for the rat gene (213, 214), and unfortunately, little is known about the regulation of the human gene. The TCF-4-mediated regulation of proglucagon expression in the gut is of considerable interest in view of the recent demonstration in several unrelated populations of a genetic association of a specific single nucleotide polymorphism (SNP), the microsatellite DG10S478 in intron 3 of the TCF4 gene (now designated TCF7L2), and the development of type 2 diabetes. These findings raise the possibility that this SNP influences disease suscepPhysiol Rev • VOL 1411 tibility through modulation of intestinal proglucagon gene expression and hence possibly plasma levels of GLP-1 (81). The differential posttranslational processing of proglucagon in the pancreas and gut results in the pancreas in the formation of glucagon, the GRPP, a small fragment corresponding to the proglucagon sequence (PG) 64 – 69 and the major proglucagon fragment corresponding to PG 72– 60 (121) (see Fig. 1), and all of these peptide products are secreted in parallel upon stimulation (121). The processing in the alpha cells is due to the coexpression of the prohormone convertase PC2, which has been demonstrated to be both necessary and sufficient for cleaving proglucagon as outlined (256). In agreement with this, animals in which the PC2 gene is disrupted cannot cleave proglucagon in the alpha cells (73) and, as a result, have lower glucose levels than wild-type animals and improved tolerance to glucose, and they develop alpha cell hyperplasia, features that also characterize mice with a deletion of the glucagon receptor gene (77). The intestinal processing results in the formation of glicentin, corresponding to proglucagon residues 1– 69, part of which may be cleaved further to oxyntomodulin, corresponding to PG 33– 69 (9, 227). The proglucagon sequence that corresponds to the major proglucagon fragment contains pairs of basic amino residues, canonical cleavage sites for the prohormone convertases, flanking both of the glucagon-like peptide sequences in the human cDNA, and it was therefore predicted that the prohormone might be cleaved at these sites (227) and that the sequences of GLP-1 and GLP-2 would therefore correspond to PG 72–108 and 126 –158, 126 –159, or 126 –160 (the nucleotide codon encoding residue 160 is found in a separate exon and was therefore overlooked in the first cloning experiments). However, sequencing of the naturally occurring peptides extracted from human gut revealed that the structure of native GLP-1 corresponds to PG 78 –107 (126). This turned out to be of utmost importance, since the truncated peptide was found to be a potent stimulator of glucose-induced insulin secretion, whereas full-length GLP-1 was inactive (126, 191). The truncation also had consequences for the nomenclature, since the naturally occurring peptide was henceforth designated either truncated GLP-1 or GLP-1 7–36amide (or GLP-1 7–37). In current literature, the unqualified designation GLP-1 covers only the truncated peptide. It was also found that the Gly corresponding to PG 108 serves as substrate for amidation of the COOH-terminal Arg (226), but the biological consequences of the amidation are unclear. The amidated and the Gly-extended forms have similar bioactivities and overall metabolism (232), although the amidated form may exhibit slightly improved stability towards plasma enzymes (326). In humans, almost all of GLP-1 secreted from the gut is amidated (231), whereas in many animals (rodents, pigs), part of the 87 • OCTOBER 2007 • www.prv.org 1412 JENS JUUL HOLST secreted peptide is GLP-1-(7–37) (97, 190). This poses special problems with respect to the measurement of GLP-1 secretion in these species (see below). The sequence of naturally occurring GLP-2 was found to correspond to PG 126 –158 (27, 103). A comparison of GLP sequences among species shows that the GLP-1 sequence is preserved 100% in all mammals, where this has been studied, and the sequence homology is pronounced across other classes of animals (149). GLP-2 shows more variation with, e.g., four substitutions between human and porcine GLP-2. The Ala in position 7 of human intervening peptide 2 is also variable with Thr or Asn in, e.g., the porcine and bovine peptides. The processing of proglucagon in the intestinal L-cells results from the actions of coexpressed prohormone convertase (PC) 1/3, which is both necessary and sufficient for the complete processing (295, 344). Interestingly, the NH2-terminal cleavage site of GLP-1 is not a classical pair of basic amino acids, but represents a single Arg residue; however, in vitro coexpression of PC 1/3 and proglucagon has demonstrated efficient cleavage at this site (255). In agreement with this, mutations in PC 1/3 lead to abnormalities in GLP-1 processing and secretion, associated with multiple endocrinopathies (143) (undoubtedly because PC 1/3 is important for processing of many regulatory peptides/hormones), and mice with a targeted deletion of the PC-1/3 gene are unable to process proglucagon to GLP-2 and GLP-1 (295, 344). Interestingly, it was recently demonstrated that adenovirus-mediated expression of PC 1/3 in the pancreatic alpha cells increases islet GLP-1 secretion, resulting in improved glucose-stimulated insulin secretion and enhanced survival in response to cytokine treatment as well as enhanced performance after transplantation to mouse models of type 1 diabetes, a finding of considerable clinical interest (see below) (331). III. PROGLUCAGON DISTRIBUTION It has been known since 1968 that endocrine cells resembling pancreatic A-cells occur in the intestinal mucosa (225). Later research demonstrated cells that are indistinguishable at the electron microscopic level from the pancreatic A-cells in the oxyntic mucosa of some species (275). Particularly in dogs such cells are abundant and appear to secrete apparently true glucagon in appreciable amounts (167). Similar cells have not been found in humans, however (120). The majority of the intestinal proglucagon-derived peptides are secreted from the L-cells, which differ clearly from the A-cells by their granule morphology (224). A-cell granules show a distinct halo of less electron-dense material surrounding a core of dense material, whereas the granules of the L-cells are homogeneous without halo formation. The L-cell is an open-type endocrine cell with a slender triangular form Physiol Rev • VOL with the base resting on the basal lamina and a long cytoplasmic process reaching the gut lumen. This process is equipped with microvilli that protrude into the lumen. It may be via these microvilli that the L-cell can sense the presence of nutrients in the lumen and transform this information into a stimulation of secretion. The peptide products of the A- and L-cells have been identified at the cellular level by immunocytochemistry. As expected, antisera directed against the midregion of glucagon (“side viewing”) stain the pancreatic A-cells as well as the intestinal L-cells, whereas antibodies against the free COOH terminus of glucagon (which is not exposed in the L-cells) only stain the A-cells. Antisera against the NH2-terminal, non-glucagon part of glicentin stain both the A-cells and the L-cells because they react with GRPP in the pancreas and with glicentin in the gut (224). As expected from their common origin, both GLP-1 and GLP-2 show complete coexistence with glucagon (side-viewing antisera) upon immunohistochemical examination (189, 227, 229). GLP-1 and GLP-2 immunoreactivity have been colocalized with glucagon in the electron-dense core of the A-cells, presumably due to their presence in the major proglucagon fragment (302). The density of L-cells shows a maximum in the ileum in most species (25, 62); no or very few cells are present proximal to the ligament of Treitz in humans and other primates. A considerable number is present in the colon (151), particularly the distal part. Surprisingly, the entirely unrelated peptide YY (PYY) has also been localized to the L-cells in all mammals studies so far (23) and was even found to be localized to the same granules as glicentin by immunocytochemistry at the electron microscopic level (23). The distribution was reexamined in a recent study involving combined in situ hybridization, peptide chemistry, and immunohistochemistry. In this study of endocrine cells of the porcine, rat, and human small intestines (195), GLP-1 nearly always (92%) colocalized with either the incretin hormone GIP (glucose-dependent insulinotropic polypeptide, formerly known as gastric inhibitory polypeptide) or the enterogastrone hormone PYY. GIP and PYY were rarely colocalized. In the mid small intestine, 55–75% of the cells staining for either GLP-1 or GIP also expressed the other incretin hormone. Concentrations of extractable GIP and PYY were highest in the midjejunum [154 (95–167) and 141 (67–158) pmol/g, median and range, respectively], whereas GLP-1 concentrations were highest in the ileum [92 (80 –207) pM], but, importantly, GLP-1, GIP, and PYY immunoreactive cells were found throughout the (porcine) small intestine. This finding is of particular interest in view of the finding that GIP can stimulate GLP-1 secretion. GIP is only active in pharmacological concentrations (99), but might act locally in a paracrine or autocrine manner. This study (195) thus suggested that simultaneous, rather than sequential, 87 • OCTOBER 2007 • www.prv.org THE PHYSIOLOGY OF GLUCAGON-LIKE PEPTIDE 1 secretion of these hormones would occur by postprandial luminal stimulation. As mentioned, the proglucagon gene is also expressed in the central nervous system. Thus cells immunoreactive for GLP-1, glucagon, and glicentin have been demonstrated in the nucleus of the solitary tract of the brain stem of rats , monkeys, and humans (52, 144, 145). These neurons project to many regions in the brain, in particular the nuclei of the hypothalamus, including the arcuate and the paraventricular nuclei (161). The processing of proglucagon has been examined both at the level of the cell bodies and at the levels of the fibers projecting to the hypothalamus (161). The pattern was intestinal with a pronounced contribution of processed oxyntomodulin, and this is important, since such neurons would be expected upon stimulation to release simultaneously three hormonal products (oxyntomodulin, GLP-1, and GLP-2), which all have been demonstrated to inhibit food intake when administered intracerebroventricularly (see below). IV. MEASUREMENT, RELEASE, AND METABOLISM As will be apparent from the above, measurement in plasma of the products of proglucagon gene expression will require assays for at least eight different peptides, three from the pancreas (glucagon, GRPP, major proglucagon fragment) and five from the intestine (glicentin, oxyntomodulin, GLP-1, GLP-2, and intervening peptide 2). For estimation of the secretory state of the alpha or L-cells, it might be proposed to measure just a single proglucagon product, because studies involving isolated perfused preparations of the pancreas or the ileum have shown that the pancreatic and intestinal products, respectively, are secreted synchronously and in equimolar amounts. [This does not apply to glicentin and oxyntomodulin, since oxyntomodulin is a breakdown product of glicentin. Therefore, it is the sum of the two moieties which equals the secreted amount of other proglucagonlike GLP-1 and -2 (193, 227)]. However, each of the proglucagon products is being eliminated from the circulation at its own particular rate (see below). A reliable estimate of the secretion and the plasma concentration of any of the products will therefore require specific measurement. Methods for determination of the glucagon-containing products date back to the first descriptions of bioassays and radioimmunoassays for glucagon (104, 117). The cross-reaction of certain antisera with material from the gut caused considerable confusion in these early days. Antisera directed against the midregion of glucagon, also called “side-viewing antisera,” will react with any product that contains this sequence, i.e., glucagon, glicetin, oxyntomodulin, and proglucagon (or glicentin) 1– 61 (10), the Physiol Rev • VOL 1413 last of which may be released in small amounts from both pancreas and gut. With such antisera, it may be possible to measure what might be designated “total glucagon” concentrations. But results obtained in these assays are not easy to interpret, because the peptides measured may be derived from both the pancreas and the gut. Upon oral administration of carbohydrates, pancreatic A-cell secretion is suppressed and L-cell secretion stimulated, and in this case, such assays may provide a reasonable estimate of L-cell secretion. The designation “enteroglucagon secretion” is sometimes coined for the results of such measurements. More specific information may be obtained with antisera that react exclusively with the unmodified and unextended COOH terminus of glucagon. Such antisera do not react with glicentin and oxyntomodulin and therefore mainly measure pancreatic glucagon (117). By subtracting the results obtained with COOH-terminal antisera from those obtained with side-viewing antisera, one gets, at least in principle, the concentration of the gut peptides glicentin and oxyntomodulin (104), and the combined assays, therefore, represent another method for quantification of enteroglucagon or gut glucagon-like immunoreactivity (117). The specificity and accuracy problems that trouble the glucagon assays apply to the assays of GLP-1 and GLP-2 as well. Again, side-viewing antibodies will react with both intestinal and pancreatic products. As mentioned, in humans, almost all of intestinal GLP-1 is COOHterminally amidated, and assays directed against the amidated COOH terminus will therefore reliably measure intestinal GLP-1 secretion [although a small contribution of GLP-1 1–36amide from the pancreas cannot be excluded (121)]. Assays in species where both GLP-1 7–36 amide and GLP-1 7–37 are produced in the gut (rodents, pigs) pose a special problem. In principle, assays directed against the intact NH2 terminus might be useful here (90), as would sandwich assays where one antibody is NH2 terminal and the other COOH terminal but capable of reacting with both the amidated and the Gly-extended forms. A few assays are based on this principle (317), and one is commercially available (Linco, St. Charles, MO; www.lincoresearch.com). The greatest problem with this approach, however, is related to the rapid degradation of GLP-1. GLP-1 is extremely susceptible to the catalytic activity of the enzyme dipeptidyl peptidase IV (DDP-IV), which cleaves off the two NH2-terminal amino acids (44). The metabolite thus generated, GLP-1 9 –36 amide or GLP-1 (9 –37), is inactive and may even act as a competitive antagonist at the GLP-1 receptor (44, 153), although its formation does not seem to result in antagonism in vivo (339). In studies of GLP-1 secretion from isolated perfused porcine ileum, it has been shown that a very large part of the GLP-1 that leaves the gut is already degraded to the inactive metabolite (96) (see Fig. 2). At first, the degradation was calculated to amount to about 87 • OCTOBER 2007 • www.prv.org 1414 JENS JUUL HOLST FIG. 2. The endocrine pathway for the actions of GLP-1. GLP-1 secretion is stimulated by nutrients in the gut lumen (a magnified intestinal villus with an open-type L-cell is shown at the lower left). GLP-1 diffuses across the basal lamina into the lamina propria and is taken up by a capillary, only to be broken down by dipeptidyl peptidase IV (DPP-IV), located on the luminal surface of the endothelial cells (white cells lining the capillary) so that only 25% of the secreted amount reaches the portal circulation. In the liver, a further 40 –50% is destroyed so that only 10 –15% enters the systemic circulation and may reach the pancreas and the brain via the endocrine pathway (perhaps even less because of the continued proteolytic activity of soluble DPP-IV present in plasma). two-thirds of the total amount secreted, but subsequent studies revealed that also the porcine gut releases significant amounts of nonamidated GLP-1 9 –37 (97), which was not taken into account in the original study. Therefore, ⬍25% of newly secreted GLP-1 leaves the gut in an intact, active form. A similar degradation amounting to ⬃40 –50% takes place in the liver (46), and it can therefore be calculated that only ⬃10 –15% of newly secreted GLP-1 reaches the systemic circulation in the intact form (see Fig. 2). This is in contrast to the fact that virtually all of GLP-1 stored in the granules of the L-cells is intact (96). It has been shown that the degradation is due to the actions of the enzyme DDP-IV, which is expressed not only in the enterocyte brush border but also in the endothelial cells lining the capillaries of the lamina propria (96). In agreement with this, inhibitors of DPP-IV can completely prevent this degradation (96). DPP-IV activity is also responsible for the extremely rapid initial whole body metabolism of GLP-1, which results in an apparent half-life for intact GLP-1 in plasma of 1–2 min and a metabolic clearance rate exceeding cardiac output by a factor of 2–3 (46, 309). The metabolite is also cleared rapidly, mainly in the Physiol Rev • VOL kidneys, with a half-life of 4 –5 min (182, 309). It has been established that GLP-1 is also a substrate for the enzyme, neutral endopeptidase 24.11 (134), and recent studies have shown that inhibition of this enzyme will enhance survival of both endogenous and exogenous GLP-1 in vivo (242). However, the enhanced survival will only be apparent if the NH2-terminal degradation by DDP-IV has been prevented. Because of the extensive degradation, the plasma concentrations of the intact hormone are very low and may not even rise significantly in response to small meals (312). However, determination of the concentrations of the metabolite, which will be much higher, may reveal that a stimulation of the L-cells has nevertheless taken place. It follows that for estimation of L-cell secretion it is best to measure the sum of the intact hormone and the primary metabolite. In humans, this can be accomplished with assays for the amidated COOH terminus of the molecule, which is common to the intact hormone and the metabolite, because in humans, all of the GLP-1 released from the gut is amidated (231). Such assays are frequently designated “total” GLP-1 assays. Clearly, for estimation of the impact of circulating intact GLP-1 for insulin secretion via the endocrine route, it is necessary to measure the concentration of the intact hormone, which may be accomplished with sandwich assays as mentioned (often designated “active GLP-1 assays”). However, as will be evident below, this is unlikely to reflect to total influence of L-cell secretion on insulin secretion. V. REGULATION OF SECRETION GLP-1 secretion is clearly meal related (233). In the fasting state, the plasma concentrations are very low. They are not immeasurable though, and it has been demonstrated that the fasting concentrations can be lowered with somatostatin in humans (287), suggesting that there is a certain basal rate of secretion. This also seems evident from studies involving DPP-IV inhibitors, which increase the levels of intact endogenous GLP-1 (174) also in the intervals between meals and in the fasting state (174). This would not have been possible without a significant interdigestive and fasting secretion of GLP-1. Meal intake causes a rapid increase in L-cell secretion, most evident when measured with COOH-terminal assays (233) (see Fig. 3), but often measurable also with assays for the intact hormone (317). The response is noticeable after ⬃10 min, but occurs later than the “cephalic phase” stimulation of insulin secretion (3), suggesting that the neuronal, possibly vagal, signals that cause insulin secretion do not influence GLP-1 (or GIP) secretion. There are many reasons to believe that it is the actual presence of nutrients in the gut lumen and possibly their interaction with the microvilli of the L-cells (62) that are responsible for the GLP-1 response. Thus a very rapid GLP-1 response 87 • OCTOBER 2007 • www.prv.org THE PHYSIOLOGY OF GLUCAGON-LIKE PEPTIDE 1 FIG. 3. Plasma concentrations of insulin, GLP-1 (total), and gastric inhibitory peptide (GIP; total) during the day time in healthy subjects. Note the rather low concentrations of GLP-1 compared with the high concentrations of GIP. Arrows indicate large meals. Values are means ⫾ SE (n ⫽ 8 subjects). [From Orskov et al. (233).] is seen in humans after ileal instillations of lipids or carbohydrate in amounts corresponding to “the physiological malabsorption” of these nutrients (164). The osmolarity of the solutions appears not to be of importance, since hyperosmolar salt solutions have no effect (240). The meal response depends on the size of the meal (317) and is strongly correlated to the gastric emptying rate (187). The response is uninfluenced by minor intestinal resections (which interrupt intramural reflex pathways) (212). It has been suggested that the purpose of having two incretin hormones is related to their location with one, GIP, being predominantly secreted from the upper small intestine, and the other mainly secreted from the lower small intestine where the density of the L-cells is higher. Conceivably, therefore, smaller loads of rapidly absorbable nutrients would preferentially activate the upper incretin hormone, i.e., GIP, whereas ingestion of larger meals containing more complex nutrients requiring more extensive digestive processing would also activate the distal incretin, i.e., GLP-1. Experiments with ␣-glycosidase inhibitors such as acarbose, which delay upper Physiol Rev • VOL 1415 intestinal digestion and absorption of carbohydrates and cause a transfer of nutrients to distal segments of the gut, are consistent with this. Acarbose reduces GIP secretion, but augments GLP-1 secretion (244) and may, partly because of this, improve glucose tolerance in patients with diabetes. Other experiments, however, suggest that the secretion of GIP is closely linked to that of GLP-1 and vice versa. Thus, in the laboratory of the author, volunteers were intubated with long (ileal) or short (duodenal) catheters, and small amounts of glucose were instilled to produce a selective response of either of the incretin hormones. Surprisingly, the glucose instillation resulted in almost equal GIP and GLP-1 responses whether introduced proximally or distally (118; unpublished studies). This may be explained by the fact that both GLP-1- and GIP-producing cells are found throughout the small intestine and by the above-mentioned finding that a significant number of gut endocrine cells in several mammals, including humans, produce both GIP and GLP-1 (195). In agreement with this, a mixed meal will normally cause a release of both peptides, but whereas the GIP concentrations may increase to several hundred picomolar, GLP-1 concentrations (intact ⫹ metabolite) rarely exceed 50 pM (233) (see Fig. 3). In subjects with accelerated gastric emptying, for instance after gastrectomy or gastric bypass operations for obesity, the secretion of GLP-1 may be greatly exaggerated (6, 187, 235) and may in such patients be the cause of reactive hypoglycemia, because of a resulting inappropriate hyperinsulinemia (76, 286) (see below). It has often been said that indirect mechanisms for release were required to explain the rapid onset of the meal response, taking the distal location of the L-cells into consideration. However, although the density of L-cells is higher in the ileum, there are numerous L-cells in the proximal jejunum as already pointed out, and these may very well be responsible for the early response. The dependency of the response on the magnitude of the meal may reflect that a larger area of the gut and thereby an increasing number of L-cells is being exposed with larger meals. Little is known about the mechanisms whereby nutrients stimulate GLP-1 secretion. In canine ileum, blockade of the luminal sodium/glucose cotransporter, SGLT-1, with phlorizin inhibited GLP-1 secretion (273), suggesting that absorption of glucose is essential, but unfortunately the experiment could not distinguish between effects of the blocker on the L-cells or on neighboring cells. Gribble et al. (82) recently found that SGLT-1 was important for glucose-induced GLP-1 secretion in a proglucagon-expressing cell line called GLUTag (82). The GLUTag cell line is derived from a colonic neuroendocrine tumor generated in a transgenic mouse expressing the simian virus 40 (SV40) T-antigen under the control of the proglucagon promoter (53). Unfortunately, this cell line does not ex- 87 • OCTOBER 2007 • www.prv.org 1416 JENS JUUL HOLST hibit the polarity of the L-cell, and it is therefore difficult to extrapolate results obtained with these cells to natural L-cells. GLP-1 secretion from the GLUTag cells may also be stimulated by metabolizable sugars by a mechanism that involves closure of ATP-sensitive K⫹ channels (8). This seems to be consistent with the recent demonstration of stimulation of GLP-1 secretion from isolated segments of porcine ileum by glucose administered both luminally and via the perfusate (98). Fructose stimulates secretion both in vivo and in the GLUTag cells (107), suggesting that GLUT5 transporters may also be involved. Involvement of neurohormonal mechanisms to explain the rapid postprandial onset of secretion has been considered by several authors. In rats, glucose-dependent insulinotropic peptide (GIP) has been shown to stimulate GLP-1 secretion via activation of a neural pathway involving the vagus nerve (254). Administration of muscarinic cholinergic agonists to isolated perfused rat ileum and colon resulted in stimulation of GLP-1 secretion (54, 109), and studies in anesthetized rats and in fetal rat intestinal cells suggested that both M1 and M2 muscarinic receptors could be involved in control of GLP-1 release (7). Catecholamines could also be part of a neural stimulatory pathway in rats, as infusion of a -adrenergic agonist stimulated GLP-1 secretion in isolated perfused rat ileum and colon (54, 241). In humans and pigs, none of the known duodenal peptides (including GIP), in normal physiological postprandial concentrations, is capable of stimulating GLP-1 secretion (68, 99, 206). Indeed, in the author’s laboratory, a systematic search of fractionated (gel and high-performance liquid chromatography) extracts of the duodenal mucosa was carried out using GLP-1 secretion from isolated perfused ileum as bioassay, but no unknown GLP-1 stimulating agents could be identified (95, 99). Infusion of atropine in humans delays the increase of both plasma glucose and GLP-1 after an oral glucose load and reduces the GLP-1 response (12), but these effects likely reflect the effects of atropine on gastrointestinal motility. Studies using the human NCI-H716 cell line have shown that cholinergic agonists stimulated GLP-1 release and suggested, as mentioned above, that M1 and M2 muscarinic receptors are involved (7, 251). In isolated perfused porcine ileum, GLP-1 secretion could be increased by infusion of acetylcholine during coinfusion of phentolamine (an ␣-adrenergic blocker, which will eliminate the sympathetic inhibition of GLP-1 secretion) (97). All this suggests that acetylcholine could be a transmitter in a neural stimulatory pathway for GLP-1 secretion. However, another study in conscious pigs indicated that the vagus nerve is not involved in control of GLP-1 release (18). Finally, in recent extensive studies employing both isolated perfused porcine ileum and intact pigs, a variety of neurally active agents as well as electrical stimulation of the abdominal vagal trunks were employed to investigate Physiol Rev • VOL the importance of the neural regulation (100). It was confirmed that the sympathetic innervation to the gut is inhibitory to GLP-1 secretion (with norepinephrine as the responsible transmitter), whereas the extrinsic vagal innervation had no effect. Intrinsic, cholinergic activity may play a minor role, however. One of the most powerful mechanisms for regulation of GLP-1 secretion appears to be a local paracrine control exerted by neighboring somatostatin producing D-cells (97). Elimination of somatostatin’s restraint (by immunoneutralization) may increase GLP-1 secretion up to eightfold, much more than observed with any other stimulus. It deserves mentioning that the neuropeptide gastrin releasing polypeptide (GRP), as well as its COOH-terminal decapeptide neuromedin C, and the related 14-amino acid frog-skin peptide bombesin (which exhibits strong COOH-terminal homology to GRP) are powerful stimulants of GLP-1 secretion (96, 227). A release of GRP can be measured from vagally innervated organs during vagal stimulation, but as mentioned, vagal stimulation does not result in a release of GLP-1 (154). Lipids provide a rather strong stimulus for GLP-1 secretion (63), and in this connection it is of interest that L-cells were recently reported to express a deorphanized G protein-coupled receptor for long-chain saturated fatty acids, GPR120 (112). Furthermore, activation of this receptor with fatty acids stimulated secretion of GLP-1 both in vitro and in vivo. In recent studies involving the GLUTag cell line, which as mentioned is a model for the L-cells and expresses the GPR120 receptor, the atypical protein kinase C (PKC-), known to be involved in fatty acid signaling in many cells, was found to be required for oleic acid-induced GLP-1 secretion (136). In other recent studies involving GLUTag cells, the neurotransmitters glycine and GABA were reported to provide a strong stimulus for secretion (74). VI. EFFECTS OF GLUCAGON-LIKE PEPTIDE 1 A. The GLP-1 Receptor The GLP-1 receptor is a class 2, G protein-coupled receptor (176) and was first cloned by expression cloning from a rat pancreatic islet library by Bernard Thorens in 1992. Thorens subsequently also cloned the highly homologous human receptor (283, 284) and also confirmed that the 53% homologous lizard peptide exendin 4 is a full agonist and the truncated peptide exendin 9 –39 is a potent antagonist of the receptor (78) (see also sect. VII). The GLP-1 receptor belongs to the same family as the GIP and the glucagon receptors (176). The receptor typically couples via a stimulatory G protein to adenylate cyclase (285, 330). The signaling in beta cells is discussed below. The receptor is widely distributed in pancreatic islets, brain, heart, kidney, and the gastrointestinal tract (5, 28, 33, 322, 87 • OCTOBER 2007 • www.prv.org THE PHYSIOLOGY OF GLUCAGON-LIKE PEPTIDE 1 323) including the stomach, where the receptor is expressed on the parietal cells (262). Its function is not known for all these locations (see below). For instance, in the parietal cells, activation of the receptor increases aminopyrine accumulation, which is an indirect indicator of acid secretion (258), whereas in vivo, GLP-1 strongly inhibits acid secretion (see below). Numerous attempts have been made to identify alternative GLP-1 receptors or subtypes (see below), but at present only a single GLP-1 receptor has been identified, whether expressed in the brain, the stomach, or the pancreas (322). However, since the pulmonary receptor was found to differ from the islet receptor with respect to electrophoretic mobility, whereas the primary sequence was identical, it was concluded that glycosylation patterns might differ (158). Biological consequences of such differences are unknown. As mentioned, exendin 9 –39 acts as a potent and specific antagonist at the GLP-1 receptor (284), and all effects of GLP-1 transmitted via this receptor would be expected to be blocked by the antagonist. However, in certain experiments involving effects of afferent vagus signaling or enterogastrone effects of GLP-1 (see below), this has not been the case (71, 219), raising speculations about the existence of another receptor. Currently, its nature remains elusive. There is considerable controversy with respect to possible effects of GLP-1 on adipose tissue, muscle tissue, and the liver, and coupled to this is of course the question whether the GLP-1 receptor is expressed in these tissues. Some studies have been negative (28), and others less clear (33). In addition, there may be differences between species, with dogs possibly expressing the receptor in muscle and adipose tissue (257) and mice expressing it in liver (33). See below for a further discussion of extrapancreatic effects of GLP-1. B. The Incretin Effect One of the most important functions of GLP-1 is to act as an incretin hormone (124, 310). “The incretin effect” designates the amplification of insulin secretion elicited by hormones secreted from the gastrointestinal tract. In the most strict sense, it is quantified by comparing insulin responses to oral and intravenous glucose administration, where the intravenous infusion is adjusted so as to result in the same (isoglycemic) peripheral (preferably arterialized) plasma glucose concentrations (177, 237). In healthy subjects, oral administration causes a two- to threefold larger insulin response compared with the intravenous route. It is, however, important to realize that the effect varies with the size of the glucose challenge, being small with, e.g., 25 g and very large with 100 g of glucose (208). In these dose-response experiments, the plasma glucose excursions were identical despite the increasing glucose loads. In other words, Physiol Rev • VOL 1417 the incretin effect ensures that postprandial glucose excursions are limited and similar regardless of the carbohydrate load. The increase in insulin secretion is mainly due to the actions of insulinotropic gut hormones (177, 178). The same gut hormones are also released by mixed meals, and given that their postprandial concentrations in plasma are similar and that the elevations in glucose concentrations are also similar, it is generally assumed that the incretin hormones are playing a similarly important role for the meal-induced insulin secretion. Part of the increase in the peripheral insulin concentrations may be due to a decreased hepatic uptake of insulin during oral glucose ingestion, resulting in more insulin being passed on to the peripheral circulation rather than representing an increased secretion. This could be mistaken for an incretin effect. However, if the analysis is based on measurements of insulin’s C-peptide instead of insulin, it is possible to eliminate the influence of the varying hepatic extraction of insulin since C-peptide is not taken up by the liver. Several studies have shown that during isoglycemic glucose challenges in healthy subjects, plasma C-peptide concentrations show very similar changes as do insulin concentrations with much higher response to the oral versus the intravenous challenge. This proves that the larger response to oral versus intravenous glucose is due to increased secretion of insulin. Calculation of the incretin effect can also be based on measurements of actual prehepatic insulin secretion rates. These can be calculated from measurements of C-peptide levels by application of C-peptide elimination kinetics and deconvolution. The actual prehepatic insulin secretion rates also exhibit much larger increases after oral compared with isoglycemic intravenous glucose stimulation (175). Many hormones have been suspected to be responsible for the incretin effect (125), but today there is ample evidence to suggest that the two most important incretins are GIP and GLP-1 (310). Both have been established as important incretin hormones in mimicry experiments in humans, where the hormones were infused together with intravenous glucose to concentrations approximately corresponding to those observed during oral glucose tolerance tests. Both hormones powerfully enhanced insulin secretion, each of them actually to an extent that can fully explain the insulin response (157, 202). Likewise, administration of GLP-1 and GIP receptor antagonists to rodents or immunoneutralization have clearly indicated that both hormones play an important role for the incretin effect (75, 155). However, there has been some uncertainty about the relative roles of the two hormones. GIP is circulating in 10-fold higher concentrations than GLP-1 [and this is true also with respect to the concentrations of the intact hormones (312)], whereas GLP-1 appears more potent than GIP (206). Furthermore, it is often emphasized that both hormones require elevated plasma glucose concentrations for stimulation of insulin secretion, for 87 • OCTOBER 2007 • www.prv.org 1418 JENS JUUL HOLST GIP may be as much as 8 mM. The insulinotropic potential of GLP-1 and GIP was, therefore, reinvestigated in recent human experiments involving clamping of blood glucose at fasting and postprandial levels and exact copying of the meal-induced concentrations of both GLP-1 and GIP by intravenous infusions (See Figs. 4 and 5). The results showed that both hormones are active with respect to enhancing insulin secretion from the beginning of a meal (even at fasting glucose levels) and that they contribute almost equally, but with the effect of GLP-1 predominat- FIG. 5. Insulin and glucagon responses in healthy volunteers to intravenous infusions of GLP-1 and GIP at normal postprandial physiological concentrations (see Fig. 3) carried out during clamping of plasma glucose at fasting levels and at 1 and 2 mM above that (see Fig. 4). The responses to the glucose alone are also shown. Note that both GIP and GLP-1 stimulate insulin secretion even at fasting glucose levels. Also note that whereas GIP has litte effect on glucagon secretion, GLP-1 causes an additional inhibition. [Modified from Vilsboll et al. (315).] ing at higher glucose levels (315). The effects of the two hormones with respect to insulin secretion have been shown to be additive in humans (204). It should be noted that only GLP-1, not GIP, causes an inhibition of glucagon secretion exceeding that elicited by glucose clamping. From studies in mice with targeted lesions of the both GLP-1 and GIP receptors, it was concluded that both hormones are essential for a normal glucose tolerance and that the effect of deletion of one receptor was “additive” to the effect of deleting the other (102, 243). Thus there is little doubt that the incretin effect plays an important role in postprandial insulin secretion and, therefore, glucose tolerance in humans and animals. FIG. 4. Incretin effect of GLP-1 and GIP in humans. Postprandial concentrations of GIP and GLP-1 (see Fig. 3) were copied by intravenous infusion in healthy volunteers, while plasma glucose levels were clamped at fasting levels, and at 1 and 2 mM above that. The insulin and glucagon responses to these infusions are shown in Fig. 5. [Modified from Vilsboll et al. (315).] Physiol Rev • VOL C. Effects on the Beta-Cells GLP-1’s insulinotropic activity, which is strictly glucose dependent, is, at least partly (see below), exerted via 87 • OCTOBER 2007 • www.prv.org THE PHYSIOLOGY OF GLUCAGON-LIKE PEPTIDE 1 interaction with the GLP-1 receptor located on the cell membrane of the beta cells (124). Binding of GLP-1 to the receptor causes activation, via a stimulatory G protein, of adenylate cyclase resulting in the formation of cAMP. Most of the actions of GLP-1 are secondary to the formation of cAMP (see Fig. 6). Subsequent activation of protein kinase A and the cAMP-regulated guanine nucleotide exchange factor II (cAMP-GEFII, also known as Epac2) leads to a plethora of events including altered ion channel activity, elevation of intracellular calcium concentrations, and enhanced exocytosis of insulin-containing granules (130). GLP-1 also stimulates coordinated oscillations in both intracellular calcium and cAMP, and these are potentiated by glucose (56). Furthermore, sustained elevations of cAMP concentrations induce nuclear translocation of the catalytic subunit of the cAMP-dependent protein kinase, presumably leading to CREB activation and likely cell proliferation and survival. The effects of glucose and GLP-1 may converge at the level of the KATP channels of the beta cells. These channels are sensitive to 1419 the intracellular ATP levels and, thereby, to glucose metabolism of the beta cells, but may also be affected (closed, resulting in subsequent depolarization of the plasma membrane and opening of voltage-sensitive calcium channels) by protein kinase A (PKA) activated by GLP-1 (85, 132, 170). Apparently, PKA-mediated phosphorylation of S1448 in the SUR1 subunit leads to KATP channel closure via an ADP-dependent mechanism. In animals with a targeted deletion of the SUR1 subunit of the channels, the incretins can still elevate cAMP levels, but no longer stimulate glucose-induced insulin secretion (199). However, this impairment was thought to be due to a restriction in the beta cells to sense cAMP correctly, since inhibitors of PKA did not inhibit the insulin response to GLP-1 (199). There is also evidence that GLP-1 acts as a glucose sensitizer. Thus GLP-1 has been found to facilitate glucose-dependent mitochondrial ATP production (293). At any rate, it is of potential clinical importance that sulfonylurea drugs, which bind to and close the KATP channels and thereby cause membrane depolariza- FIG. 6. Summary of the cellular actions of GLP-1 that lead to stimulation of insulin secretion. Binding of GLP-1 to its receptors couple to activation of adenylate cyclase; intracellular cAMP levels are elevated leading to activation of protein kinase A (PKA) and cAMP-regulated guanine nucleotide exchange factor II (cAMP-GEFII, also known as Epac2). These two proteins are likely to mediate the plethora of molecular mechanisms (summarized below in points 1– 6). 1) GLP-1 acts synergistically with glucose to close ATP-sensitive K⫹ (KATP) channels and thus facilitates membrane depolarization and the induction of electrical activity. 2) Once electrical activity is initiated, the slower time course of inactivation of the Ca2⫹ channels results in prolonged bursts of action potentials. In addition, each action potential will be associated with a slightly greater Ca2⫹ influx because the amplitude of the Ca2⫹ current is moderately increased (86). 3) Antagonism by GLP-1 of the delayed rectifying K⫹ (Kv) channels will increase excitability and results in prolongation of the duration of action potentials. 4) In the presence of stimulatory levels of glucose and GLP-1, Ca2⫹ influx through the Ca2⫹ channels feeds forward into mobilization of Ca2⫹ from intracellular stores by Ca2⫹-induced Ca2⫹ release through PKAand cAMP-GEFII-dependent mechanisms. 5) Ca2⫹ mobilization from intracellular stores will stimulate mitochondrial ATP synthesis, which will promote further membrane depolarization via closure of KATP channels. ATP is also required for stimulation of exocytosis of the insulin-containing granules. 6) The elevation in the cytoplasmic free Ca2⫹ concentration ([Ca2⫹]i) triggers the exocytotic response that is further potentiated by increased cAMP levels. This effect is principally attributable to the ability of cAMP to accelerate granule mobilization resulting in an increased size of the pools of granules that are immediately available for release. These effects depend both on cAMP binding to PKA and cAMP-GEFII. Quantitatively the last mechanism is by far the most important one and may account for 70% or more of the total insulinotropic activity of GLP-1 and GIP (86). [Modified from Holst and Gromada (124).] Physiol Rev • VOL 87 • OCTOBER 2007 • www.prv.org 1420 JENS JUUL HOLST tion and calcium influx, may uncouple the glucose dependency of GLP-1 (40). Thus GLP-1 administration to isolated perfused rat pancreases at low perfusate glucose concentrations normally does not affect insulin secretion, but resulted in dramatic stimulation of insulin secretion after pretreatment with sulfonylurea drugs (40, 89). Indeed, 30 – 40% of patients treated with both sulfonyl urea compounds and a GLP-1 agonist (exendin 4, see below) experience, usually mild, hypoglycemia. cAMP generated by activation of the GLP-1 receptor may also influence the exocytotic process directly, and this process has been estimated to account for up to 70% of the entire secretory response (124). Also, ATP may directly influence the exocytotic process and may, therefore, represent another site of convergence for the glucose- and GLP-1-mediated signals (86). Other changes that occur in the beta cells appear to be PKA independent. Thus the actions of GLP-1 on the insulin gene promoter appear to be mediated by both PKA-dependent and -independent mechanisms, the latter possibly involving the mitogen-activated protein kinase pathway (146). The effect of GLP-1 on the insulin promoter appears to be mediated by two distinct cis-acting sequences, both in a PKA-dependent and PKA-independent manner (268). There is also evidence that glucose and GLP-1, by increasing intracellular calcium, may potentiate insulin gene transcription in a calcineurin- and nuclear factor of activated T-cells (NFAT)-dependent manner (162). The transcription factor PDX-1, a key regulator of islet growth and insulin gene transcription, appears to be essential for most of the glucoregulatory, proliferative, and cytoprotective actions of GLP-1 (168). In addition, GLP-1 upregulates the genes for the cellular machinery involved in insulin secretion, such as the glucokinase and GLUT2 genes (31). Much attention was aroused by the finding that GLP-1 appeared to be essential for conveying “glucose competence” to the beta cells, i.e., without GLP-1 signaling, beta cells would not be responsive to glucose (86, 133). However, the beta cells of mice with disruption of the GLP-1 receptor gene show preserved glucose competence (69). It is possible, however, that glucagon from neighboring alpha cells may substitute, since glucagon may also provide glucose competence to beta cells (69). As already alluded to, GLP-1 also has trophic effects on beta cells (59). Not only does it stimulate beta-cell proliferation (57, 66, 271, 333), it also enhances the differentiation of new beta cells from progenitor cells in the pancreatic duct epithelium (343). Thus GLP-1 has been demonstrated to be capable of differentiating the pancreatic duct cell line AR42J into endocrine insulin-secreting cells (168, 343). Most recently, GLP-1 has been shown to be capable of inhibiting apoptosis of beta cells including human beta cells (30, 65). Since the normal number of beta cells is maintained in a balance between apoptosis and proliferation (21), this observation raises the possiPhysiol Rev • VOL bility that GLP-1 could be useful as a therapeutic agent in conditions with increased beta-cell apoptosis, which would include type 1 as well type 2 diabetes in humans (32). Thus treatment of mice with the GLP-1 agonist exendin 4 reduced beta-cell apoptosis induced by streptozotocin (while GLP-1 receptor knockout mice were abnormally susceptible to streptozotocin-induced beta-cell apoptosis) (169). Also, cytokine-induced apoptosis may be inhibited, and GLP-1 agonism increased cell survival and reduced caspase activation in BHK fibroblasts expressing a transfected GLP-1 receptor (169). In this connection, it is of considerable interest that exendin treatment (in combination with lisophylline) prior to the development of diabetes markedly improved glucose control in NOD mice, a model of type 1 diabetes, and preserved the number of intact islets and reduced the extent of inflammation in the remaining islets (337), again suggesting that GLP-1 treatment might be able to reduce the beta-cell destruction in human autoimmune diabetes. GLP-1 treatment was demonstrated to delay the onset of diabetes when given to 8-wk-old db/db mice, which develop diabetes secondary to an inactivating mutation of the hypothalamic leptin receptor causing massive obesity (320). Impressively, GLP-1 or exendin 4 administration for 5 days in the neonatal Goto-Kakisaki (GK) rat, a polygenetic and hypoinsulinemic model of type 2 diabetes, resulted in persistent improvement in glucose homeostasis and maintenance of beta-cell mass adult age (290). It is important to note that the trophic effects of GLP-1 agonists in rodents, like their insulinotropic properties, are coupled to the presence of hyperglycemia, and also to note that as GLP-1 alleviates hyperglycemia, which is in itself a very strong stimulus to beta-cell growth in rodents; this growth stimulus is reduced (272). Thus, in nondiabetic rats, the increase in beta-cell mass was transient and disappeared upon prolonged administration (6 wk) of a stable long-acting GLP-1 analog (20). A most striking demonstration of the beta-cell protective/proliferative effects of GLP-1 receptor activation was provided by Stoffers et al. (270), who studied the diabetes developing in rats subjected to intrauterine growth retardation. Treatment with exendin 4 in the neonatal period completely prevented development of diabetes and restored beta-cell mass, which otherwise is strongly reduced in these animals. The complicated and incompletely elucidated mechanisms that could be involved in the GLP-1-induced trophic effects on the beta cells were reviewed recently (24, 51, 267). D. Effects on Glucagon Secretion GLP-1 strongly inhibits glucagon secretion (228). Since in patients with type 2 diabetes there is fasting 87 • OCTOBER 2007 • www.prv.org THE PHYSIOLOGY OF GLUCAGON-LIKE PEPTIDE 1 hyperglucagonemia as well as exaggerated glucagon responses to meal ingestion (288), and since it is likely that the hyperglucagonemia contributes to the hyperglycemia of the patients (265), this effect may be as important clinically as the insulinotropic effects (see below). Indeed, in patients with type 1 diabetes and complete lack of beta-cell activity (C-peptide negative), GLP-1 is still capable of lowering fasting plasma glucose concentrations, presumably as a consequence of a powerful lowering of the plasma glucagon concentrations (35). The mechanism of GLP-1-induced inhibition of glucagon secretion is not completely elucidated. Insulin is generally thought to inhibit glucagon secretion, and local elevations of insulin levels around the alpha cells might inhibit their secretion in a paracrine manner, but the preserved and pronounced inhibitory effect of GLP-1 in type 1 diabetic patients without residual beta-cell function (35) would suggest that other mechanisms must also be involved. Similarly, GLP-1 strongly inhibits glucagon secretion in isolated rat pancreas perfused with low perfusate glucose concentration and immeasurable insulin secretion (41). GLP-1 stimulates pancreatic somatostatin secretion (228), which in turn might inhibit glucagon secretion by paracrine interaction (67), as evidenced by the ability of somatostatin antibodies as well as a somatostatin receptor 2 antagonist to abolish the inhibitory effect of GLP-1 (41). Interestingly, in isolated alpha cells, ⬃20% of which may express the GLP-1 receptor (106) (although this is controversial, Ref. 188), GLP-1 appears to stimulate GLP-1 secretion (50). The inhibitory effect of GLP-1 on glucagon secretion in vivo is only observed at glucose levels at or above fasting levels (see Fig. 5). In studies involving graded hypoglycemic clamping in humans, the inhibitory effect of GLP-1 was lost at glucose levels just below normal fasting levels, and the normal stimulation of glucagon secretion at hypoglycemic levels was unimpeded by GLP-1 (205). This is important because it implies that treatment with GLP-1 (see below) does not weaken the counterregulatory responses to hypoglycemia and, therefore, does not lead to an increased risk of hypoglycemia. 1421 inhibit pancreatic secretion in response to intraduodenal stimulation (84). The inhibitory effect of GLP-1 on acid secretion could be elicited by physiological elevations of the GLP-1 concentrations in plasma and was, remarkably, additive to the inhibitory effects of PYY, which is released from the L-cell in parallel with GLP-1 (324). Together the two peptides almost abolished gastrin-stimulated secretion, indicating that these two peptides are the likely mediators of the “ileal brake effect,” i.e., the endocrine inhibition of upper gastrointestinal functions elicited by the presence of unabsorbed nutrients in the ileum (113, 163, 249). These effects of GLP-1, also designated entergastrone effects, are likely to be physiological, since stimulation of endogenous GLP-1 secretion by intraileal instillation of nutrients corresponding to the “physiological malabsorption,” resulted in concomitant inhibition of gastric and pancreatic secretions (164) (See Fig. 7). Further studies documented that GLP-1 could completely abolish acid secretion resulting from pure vagal stimulation in humans (as elicited by modified sham feeding: the “chewand-spit technique”) (325) and that the inhibitory effect was lost in people that had had a truncal vagotomy for duodenal ulcer disease (329). This would indicate that all of the actions of GLP-1 on gastric functions are mediated via vagal pathways (see below). In recent studies Schirra et al. (260) were able to demonstrate the importance of endogenous GLP-1 for regulation of antroduodenal motility (and pancreatic endocrine secretion) by administration of the GLP-1 receptor antagonist exendin 9 –39 (see Fig. 8). The physiological relevance of the ileal-brake effects of GLP-1 in humans thus seems established. E. Effects on the Gastrointestinal Tract Further important effects of GLP-1 include inhibition of gastrointestinal secretion and motility (211, 327). It was first noted that GLP-1 inhibits gastrin-induced acid secretion in humans (261), and subsequently demonstrated that GLP-1 also inhibits meal-induced secretion as well as gastric emptying and pancreatic secretion (327). The effect on pancreatic exocrine secretion was first suspected to be secondary to the inhibition of gastric emptying, but in subsequent studies, GLP-1 was demonstrated to also Physiol Rev • VOL FIG. 7. Relationship between (total) plasma GLP-1 responses and inhibition of gastric acid secretion in healthy volunteers undergoing ileal instillations of solutions of NaCl, protein, lipid, and carbohydrates (CHO) corresponding to the amounts normally present in this section of the gut after mixed meal ingestion. [From Layer et al. (164), with kind permission of Springer Science and Business Media.] 87 • OCTOBER 2007 • www.prv.org 1422 JENS JUUL HOLST FIG. 8. Antroduodenal motility (pressure waves) in response to intraduodenal glucose infusions in healthy volunteers with or without infusion of a GLP-1 receptor antagonist (exendin 9 –39). The antagonist clearly enhanced to motor responses, indicating removal of a GLP-1-mediated inhibition. [From Schirra et al. (260), with permission from BMJ Publishing Group Ltd.] F. Central Targets for Peripherally Released GLP-1 As alluded to above, very little GLP-1 reaches the systemic circulation in the intact form. One may ask why particularly GLP-1 is degraded so extensively that a rise in the concentration of the intact peptide frequently may not be noticeable after intake of smaller meals. The observation has led to the hypothesis that GLP-1 must act locally in the lamina propria before being degraded (96, 123; see Fig. 9). Once released from the L-cells, GLP-1 diffuses across the basal lamina and enters the lamina propria. Here it is taken up by capillaries, the endothelial membranes of which will then degrade the hormone, because they express DPP-IV (96). However, on its way to the capillary, GLP-1 may interact with afferent sensory nerve fibers arising from the nodose ganglion, sending impulses to the nucleus of the solitary tract and onwards to the hypothalamus (See Fig. 9) (123). Recent observations that the GLP-1 receptor is expressed in nodose ganglion cells support this view (198). In addition, it has been demonstrated that intraportal administration of GLP-1 causes increased impulse activity in the vagal trunks (220). These impulses may be reflexly transmitted to the pancreas (197). Studies in rats employing ganglionic blockers have shown that the insulin response to intraportal administration of GLP-1 and glucose may be reduced to that elicited by glucose alone after ganglionic blockade (11) (see Fig. 10). Similarly, in mice rendered sensory denervated by neonatal administration of the neurotoxin capsaicin, low doses of GLP-1 that augmented glucose-induced insulin secretion in control animals had little effect in the denervated mice, whereas high doses had the same effects in control and denervated animals (1). The interPhysiol Rev • VOL pretation was that physiological amounts of GLP-1 depended on reflex pathways for stimulation of insulin secretion, whereas higher doses leading to higher plasma concentrations might activate islet receptors directly and therefore equally in control and denervated mice. Thus, regarding the mechanism of GLP-1-stimulated insulin secretion under physiological circumstances, the neural pathway may be more important than the endocrine route. However, the concentration of intact GLP-1 does rise after meal intake and rises more the larger the meal is (317). Thus it seems probable that the endocrine route becomes more prominent after extensive L-cell stimulation. The pathways whereby GLP-1 exerts its “ileal brake” effects (119) also seem to depend on signaling via afferent sensory neurons relaying in the brain stem or the hypothalamus and regulating efferent parasympathetic outflow (139, 328). Thus GLP-1 has no effect on vagally stimulated antral motility in isolated perfused preparations of the pig stomach (328) and no effect on vagally stimulated exocrine secretion from isolated perfused porcine pancreas (127). Furthermore, as mentioned, the acid inhibitory activity in humans exclusively depends on vagal mechanisms (325, 329). Finally, the inhibitory effect on gastric emptying in rats is lost after vagal deafferentation (139). Studies in rats have suggested that a hepatoportal glucose sensor may reflexly influence peripheral glucose metabolism and that this sensor is somehow linked to a GLP-1 receptor expression, since its effects on peripheral glucose disposal are abrogated by exendin 9 –39 and cannot be demonstrated in GLP-1 receptor knockout mice (29). In dogs, pharmacological amounts of intraportal GLP-1 were required to elicit changes in peripheral glucose metabolism (218), and in further dog studies, insulin- 87 • OCTOBER 2007 • www.prv.org THE PHYSIOLOGY OF GLUCAGON-LIKE PEPTIDE 1 1423 FIG. 9. The neural pathway for the actions of GLP-1. GLP-1 secretion is stimulated by nutrients in the gut lumen (a magnified intestinal villus with an opentype L-cell is shown at the lower left), and newly released GLP-1 diffuses across the basal lamina into the lamina propria. On its way to the capillary, however, it may bind to and activate sensory afferent neurons (f) originating in the nodose ganglion (c), which may in turn activate neurons of the solitary tract nucleus (a). The same neuronal pathway may be activated by sensory neurons in the hepatoportal region (29) (e) or in the liver tissue (39) (d). Ascending fibers from the solitary tract neurons may generate reflexes in the hypothalamus, and descending impulses (from neurons in the paraventricular nucleus?) may activate vagal motor neurons (b), that send stimulatory (h) or inhibitory (g) impulses to the pancreas and the gastrointestinal tract. Interactions between ascending sensory nerve fibers and vagal motorneurons may also take place at the level of the brain stem. independent effects of GLP-1 on glucose disposal in the liver required long-term (up to 5 h) infusions and were independent of route of administration (portal vs. peripheral) (39). Similar to the findings in mice, intraportal GLP-1 and glucose infusions in other dog studies were found to decrease peripheral glucose levels independently of hyperinsulinemia (140). However, it should be noted that peripheral administration of GLP-1 to dogs at a similar rate is claimed not to enhance glucose-induced insulin secretion in this species (141). This is again in sharp contrast to very consistent findings in humans (135, 157) and therefore suggests that dogs (and possibly mice) differ radically from humans in this respect. G. Effects on Appetite and Food Intake There have been reports on the presence of glucagon in the brain for many years (277), and it has been speculated that the peptide might play a role in regulation of food intake. When GLP-1 was also discovered in the brain (144), it was relevant to investigate the possible central Physiol Rev • VOL actions of the peptide. Early studies indicated an effect on appetite and food intake (259), and subsequent more detailed studies confirmed these effects after intracerebroventricular administration of low doses of the peptide (278, 294). The proglucagon-producing neurons of the brain stem may represent a link in a system whereby enteroceptive stress, but possibly also food ingestion, transmits satiety signals to the brain (160, 253). Thus the cells are activated (show c-fos expression) upon distension of the stomach (319). GLP-1 receptors are expressed in many regions of the brain and in particular in the arcuate nucleus and other hypothalamic regions involved in the regulation of food intake (79). Destruction of the arcuate nucleus with perinatal monosodium glutamate abolishes the inhibitory effect of intracerebroventricularly administered GLP-1 on food intake and appetite (280), indicating that this nucleus is essential for the response. As mentioned earlier, processing of proglucagon in the brain stem neurons leads to the formation of GLP-1 as well as GLP-2 and oxyntomodulin, all of which have been reported to inhibit food intake after intracerebroventricular 87 • OCTOBER 2007 • www.prv.org 1424 JENS JUUL HOLST FIG. 10. Insulin responses to intraportal infusions of glucose and GLP-1 in rats with or without intravenous infusion of a ganglionic blocker (chlorisondamine). Note that the ganglionic blocker completely eliminated the GLP-1-induced enhancement of glucose-stimulated insulin secretion. [From Balkan and Li (11).] administration (37, 279). Thus it is possible that the impact on food intake of activation of these neurons is underestimated when only a single transmitter is studied. Nutrients in the ileum are thought to have a satiating effect, curtailing food intake (249), and GLP-1 is released simultaneously (164). Does peripheral GLP-1 play a physiological role as a satiating agent? Several studies have shown that infusions of GLP-1 significantly and dose dependently enhance satiety and reduce food intake in normal subjects (70, 305). The effect on food intake and satiety is preserved in obese subjects (200) as well as in obese subjects with type 2 diabetes (91, 340). This raises the possibility that GLP-1 is not only a physiological regulator of food intake but also has a therapeutic potential. Recent clinical studies have shown that subcutaneous injections of a stable GLP-1 receptor agonist (exendin 4) given twice daily for several years to people with type 2 diabetes are associated with a gradual and linear weight loss with no signs of impaired efficacy with time (19, 108). The mechanism whereby peripherally administered GLP-1 inhibits food intake is not clear. It is unlikely to be related to the effect on gastric motility and emptying, since appetite reduction can be elicited also in fasting subjects (93). It is more likely that interaction with sensory neurons in the gastrointestinal tract or the hepatoportal bed is involved as discussed above. Another possibility is that peripherally administered GLP-1 can access the brain via leaks in the blood-brain barrier such as the subfornical organ and the area postrema, as demonstrated to occur in rats (230). It has also been claimed that regulatory peptides from the periphery can somehow access the arcuate nucleus Physiol Rev • VOL perhaps via diffusion from the median eminence (160). Recent studies have demonstrated that infusions of the orexigenic peptide ghrelin may dampen the effects of GLP-1 on gastric emptying and food intake, and the authors suggested that the stimulating effect of ghrelin on food intake might derive at least in part from its ability to attenuate the effects of GLP-1 (and PYY 3–36) on gastric emptying and food intake (34). It should be noted that GLP-1 receptor knockout mice do not become obese (263), but this may reflect the redundancy of the appetite regulating mechanisms rather than ineffectiveness of the signal. In fact, the efficacy of the appetite-reducing effect was convincingly demonstrated not only in the clinical studies referred to above but also in recent studies involving life-long administration of exendin 4 to rats. The treated animals survived longer than controls, an effect that was thought to result from decreased food intake and hence a significantly lower body weight (110). Central administration of GLP-1 may also affect drinking behavior. Thus intracerebroventricular GLP-1 profoundly inhibited angiotensin II-induced drinking behavior in rats, and water intake was suppressed by exogenous GLP-1 in rats habituated to a water restriction schedule. In contrast to the effects of GLP-1 on food intake, these effects were reproduced by intraperitoneal administration of GLP-1. Furthermore, intracerebroventricular GLP-1 stimulated urinary excretion of water and sodium (278). Subsequent studies confirmed that intravenous infusion of pharmacological doses of GLP-1 may modulate drinking behavior and increase renal sodium excretion in healthy volunteers as well as in patients with type 2 diabetes (92, 94). However, long-term treatment of patients with type 2 diabetes with GLP-1 analogs does not seem to be associated with disturbances of fluid or electrolyte balance. H. Other Effects 1. Cardiovascular It is well established that there are glucagon receptors in the heart and that glucagon has inotropic and chronotropic actions on the heart. Now it turns out that there are also GLP-1 receptors in the heart (28, 33, 283). GLP-1 was also demonstrated to increase cAMP levels in adult rat cardiac myocytes (307), but in that study GLP-1 decreased contraction amplitude as opposed to isoproterenol, which augmented amplitude and, again unlike isoproterenol, GLP-1 did not bring about any intracellular calcium transients, but did cause a modest intracellular acidification. Further evidence for a role for GLP-1 in cardiac function was derived from studies in mice lacking the GLP-1 receptor (87). At the age of 2 mo, these animals had reduced resting heart rate and elevated left ventricu- 87 • OCTOBER 2007 • www.prv.org THE PHYSIOLOGY OF GLUCAGON-LIKE PEPTIDE 1 lar (LV) end-diastolic pressure, compared with wild-type controls. At the age of 5 mo, echocardiography and histology demonstrated increased LV thickness. In addition, there was impaired LV contractility and diastolic function after insulin administration. LV contractility was also reduced after exogenous epinephrine. These data suggest that GLP-1 exerts physiologically important effects on cardiac function. In a more recent study, Bose et al. (22) demonstrated that GLP-1 significantly reduced infarction size in both in vitro (isolated perfused rat heart) and in vivo models of ischemia-reperfusion damage. The protective effect in vitro was abolished by the GLP-1 receptor antagonist exendin 9 –39, cAMP inhibitors, as well as phosphatidylinositol 3-kinase and mitogen-activated protein kinase inhibitors, suggesting involvement of these pathways in the protective response. Zhao et al. (342) were also able to demonstrate direct effects of GLP-1 on myocardial contractility and glucose uptake in normal and postischemic isolated rat hearts. They measured LV function, myocardial glucose uptake, and lactate production under basal conditions and after low-flow ischemia with or without GLP-1 or buffer or insulin. GLP-1 increased myocardial glucose uptake almost threefold via increased nitric oxide production and GLUT1 translocation, but decreased LV pressure. Furthermore, GLP-1 treatment significantly improved postischemia LV end-diastolic pressure and LV developed pressure. Thus, in the normal resting heart, GLP-1 reduces contractility. However, it increases glucose uptake by mechanisms distinct from insulin, but improves recovery after ischemia in a fashion similar to that of insulin. The cardiac effects of GLP-1 were studied in conscious dogs with pacing-induced dilated cardiomyopathy, which was induced by 28 days of rapid pacing (215). The dogs received a 48-h infusion of GLP-1 (1.5 pmol䡠kg⫺1 䡠min⫺1, a dose that efficaciously lowers plasma glucose in diabetic patients but does not cause significant side effects). The GLP-1 infusion was associated with large improvements in LV performance, stroke volume, and cardiac output as well as significant decreases in LV end-diastolic pressure, heart rate, and, interestingly, systemic vascular resistance. GLP-1 also increased myocardial insulin sensitivity and glucose uptake. The same group also reported (217) effects of a 72-h infusion of GLP-1 (same dose) added to background therapy in 10 patients with acute myocardial infarction (AMI) and LV ejection fraction ⬍40% after successful primary angioplasty compared with placebo. Both groups had severe LV dysfunction [LV ejection fraction (LVEF) ⫽ 29 ⫾ 2%]. GLP-1 significantly improved LVEF (to 39 ⫾ 2%) and also improved global and local wall motion indices. Most recently, the same group studied the effects of a 5-wk infusion of GLP-1 added to standard therapy in 12 patients with heart failure. GLP-1 significantly improved LVEF, Physiol Rev • VOL 1425 myocardial oxygen uptake, 6-min walking distance, and quality of life, and the treatment was well tolerated (269). In other studies (216), again involving pacing-induced dilated cardiomyopathy in conscious dogs as a model, the effects of 48-h infusions of either GLP-1 or its primary metabolite after DPP-IV degradation [which occurs with a half-life of 1–2 min in the circulation of pigs and humans (46, 309)], GLP-1 9 –36 amide, were investigated. The dogs were studied under basal as well as insulin-stimulated conditions (hyperinsulinemic euglycemic clamps). The dogs with dilated cardiomyopathy demonstrated insulin resistance. Surprisingly, both GLP-1 and GLP-1 9 –36 amide significantly and equally reduced LV end diastolic pressure and increased LV performance and cardiac output. Both peptides increased myocardial glucose uptake independently of insulin. Since during the infusion of GLP-1 7–36 amide ⬃80% of the peptide is metabolized to GLP-1 9 –36 amide, these results would suggest that GLP-1 9 –36 is the active peptide. In recent animal and human studies (45, 181), the metabolite GLP-1 9 –36 amide was demonstrated to lower blood glucose slightly and independently of insulin and glucagon secretion, which remained unaffected by the metabolite. The mechanism of action could not be revealed, but may be related to the cardiac effects. The cardiac effect of the metabolite/GLP-1 has potential clinical implication because it would suggest that it would not be observed after administration of analogs of GLP-1 that are stabilized against the actions of DPP-IV and therefore do not lead to the formation of the metabolite (see below). In summary, GLP-1 is likely to have physiological effects on the heart. In the basal state, GLP-1 may inhibit contractility, but after cardiac injury GLP-1 has constantly increased myocardial performance both in experimental animals and in patients. GLP-1 enhances insulin secretion and may enhance myocardial performance via the combined effects of enhanced insulin secretion and action [insulin therapy has been demonstrated to have beneficial effects of its own on the course of myocardial infarction in patients with type 2 diabetes (341) ], but also appears to have direct effects that are independent of insulin action. The potentially important observation that it may be the metabolite of GLP-1 that is the active agent in cardiac protection requires independent confirmation and raises the question of the nature of the receptor involved, but may be consistent with the finding that GLP-1 9 –36 amide appears to lower blood glucose in humans and pigs independent of insulin and glucagon secretion. As discussed above, the GLP-1 receptor is expressed in the lungs (158), but the functions of GLP-1 in the lungs are unclear, although it has been reported to increase the secretion of macromolecules from the neuroendocrine cells (252). 87 • OCTOBER 2007 • www.prv.org 1426 JENS JUUL HOLST 2. Neurotropic and other neural effects GLP-1 may also possess neurotropic effects. Thus intracerebroventricular GLP-1 administration was associated with improved learning in rats and also displayed neuroprotective effects (55, 238), and GLP-1 has been proposed as a new therapeutic agent for neurodegenerative diseases, including Alzheimer’s disease (239). It has been reported that cerebral GLP-1 receptor stimulation increases blood pressure and heart rate and activates autonomic regulatory neurons in rats, leading to downstream activation of cardiovascular responses (335). Furthermore, it has been suggested that catecholaminergic neurons in the area postrema expressing the GLP-1 receptor may link peripheral GLP-1 and central autonomic control sites that mediate the diverse neuroendocrine and autonomic actions of peripheral GLP-1 (334). However, peripheral administration of GLP-1 in humans is not associated with changes in blood pressure or heart rate (340). I. Whole Body Effects, Peripheral Effects, and Effects on Insulin Action After the incretin functions of GLP-1 were established in humans (157) and the hormone was demonstrated to be capable of normalizing the elevated plasma glucose levels in patients with type 2 diabetes (210), several studies were carried out to elucidate in more detail its mechanisms of action. Hvidberg et al. (135) studied glucose turnover in fasting healthy subjects in response to physiological and supraphysiological infusions of GLP-1 and found that insulin secretion was enhanced and glucagon secretion inhibited by both. Concomitantly, hepatic glucose production was inhibited, and therefore, the plasma glucose concentration fell by ⬃1 mM. Glucose clearance was also increased, but this was interpreted to be a consequence of the increased insulin concentrations. The role of the suppression of glucagon was studied further in subjects with type 1 diabetes and no residual beta-cell function (35). In these subjects an infusion of GLP-1 significantly lowered fasting glucose levels, concurrently with a marked lowering of plasma glucagon concentrations. It was concluded that the glucose-lowering action in this case was due to a decreased hepatic glucose production resulting from decreased glucagon secretion. D’Alessio et al. (36) found in a study involving the minimal model approach (a computerized calculation of insulin sensitivity and insulin-independent, glucose-mediated glucose uptake, based on frequent determinations of insulin and glucose concentrations after an intravenous glucose infusion) that GLP-1 was capable of increasing glucose-mediated glucose uptake (glucose effectiveness) in healthy subjects by a mechanism independent of insulin secretion. However, the relevance of Physiol Rev • VOL the chosen approach has been questioned because insulin secretion was markedly stimulated in the GLP-1 experiment, but not in the control experiment. A valid control experiment might involve infusion of insulin to achieve similar levels as those achieved during GLP-1 infusion (ideally identical intraportal concentrations). In further studies, Toft-Nielsen et al. (287) administered GLP-1 to healthy subjects with or without concomitant infusion of 500 g/h somatostatin. Glucose assimilation was then studied by an intravenous glucose tolerance test. It turned out that even with this (high) dose of somatostatin, insulin (and C-peptide) secretion was still slightly stimulated by GLP-1. In agreement with this, the glucose elimination rate (Kg) was increased by GLP-1. Fortuitously, these results documented the exquisite sensitivity of the approach. The somatostatin infusion rate was then increased to 1,000 g/h, and now insulin secretion remained constant. In this case, there was no change of Kg during GLP-1 administration, and it was concluded that GLP-1 had no direct effect on glucose uptake by the peripheral tissues (or at least that any effect must be very small). Subsequently, the effects of physiological elevations of GLP-1 or saline infusions on insulin-stimulated glucose uptake were studied in human volunteers by the euglycemic hyperinsulinemic clamp technique (234). In addition, somatostatin was administered to clamp insulin secretion at a low level, whereas basal glucagon and growth hormone levels were maintained by intravenous infusion. Furthermore, glucose turnover rates were evaluated by a tracer technique. However, there were no differences between GLP-1 and saline infusions with respect to any parameter studied, including glucose infusion rates required to maintain euglycemia, glucose appearance and disappearance rates, as well as forearm arteriovenous glucose differences. Vella et al. (304) studied the effects of pharmacological doses of both the GLP-1 receptor agonist exendin 4 and the native peptide in healthy subjects in three-step hyperinsulinemic clamp experiments. Both peptides increased cortisol secretion, but neither influenced insulin action (304). In further studies, GLP-1 was infused in supraphysiological amounts to patients with type 2 diabetes, and insulin sensitivity was estimated using clamp techniques (4). However, in these experiments, there was no effect of GLP-1 on insulin sensitivity either. In further studies, Vella et al. (303) infused pharmacological (treatment relevant) doses of GLP-1 or saline to subjects with type 2 diabetes while at the same time infusing glucose to mimic postprandial glucose concentrations and clamping insulin and glucagon levels at basal or postprandial levels. Under these conditions, GLP-1 had no influence on glucose disappearance or suppression of endogenous glucose production. On the basis of all these studies, it seems justified to conclude that GLP-1 has very little acute effect on insulin-dependent and -independent glucose turnover when its effects on the endocrine pan- 87 • OCTOBER 2007 • www.prv.org THE PHYSIOLOGY OF GLUCAGON-LIKE PEPTIDE 1 creas are prevented. Zander et al. (340) infused GLP-1 or saline continuously for 6 wk to patients with type 2 diabetes and determined insulin sensitivity by hyperinsulinemic euglycemic clamps before and after the treatment. Insulin sensitivity was unchanged in the saline-treated group, but was almost doubled in the GLP-1-treated group. The study was not designed to elucidate the underlying mechanisms, but it should be noted that GLP-1 was administered during the clamp (and actually resulted in a slightly higher insulin level) and that the GLP-1treated subjects experienced markedly improved glycemic control as well as lower free fatty acid levels and also lost ⬃2 kg of body weight. The weight loss as well as reduced gluco- and lipotoxicity induced by GLP-1 were considered likely explanations for the improved insulin sensitivity. Similar findings were made in a study involving 3 mo of continuous subcutaneous infusion of GLP-1 to diabetic subjects (183). However, the same group reported acute augmentation by GLP-1 of insulin-mediated glucose uptake in elderly patients with diabetes (185) and also reported insulin-mimetic effects of GLP-1 in obese subjects compared with nonobese matched controls (60). Nevertheless, the group was unable to identify effects of GLP-1 on insulin-mediated glucose uptake in patients with type 1 diabetes (184). D’Alessio et al. (36), who were the first to suggest extrapancreatic metabolic effects of GLP-1 in humans, later studied eight healthy subjects using somatostatin clamp and tracer techniques similar to those employed by Orskov et al. (234) and reported a 17% decrease in rate of glucose appearance resulting in a lower blood glucose and concluded that GLP-1 had extrapancreatic metabolic effects, possibly mediated via intraportal GLP-1 receptors (see below). As already discussed, it may be difficult to control GLP-1-stimulated insulin secretion with somatostatin, and the significance of these findings cannot be settled presently. However, in contrast to the human studies, several, mainly in vitro, studies support that GLP-1 may have effects on peripheral tissues and/or the liver that are independent of its effects on the islet hormones. Thus it has been reported that membranes from human adipose tissue express GLP-1 receptors (186), and similar findings have been reported for rats (300). GLP-1 was also reported to enhance fatty acid synthesis in explants of rat adipose tissue (223) and was reported to enhance insulinstimulated glucose uptake in 3T3-L1 adipocytes (61, 321). Evidence was provided, however, that the responsible receptor differed from the GLP-1 receptor (192). Nevertheless, in studies involving direct determination of lipolysis rates in human subcutaneous tissue, Bertin et al. (16) were unable to find any effects of GLP-1. GLP-1 receptors have also been claimed to be present in rat skeletal muscle (49), and GLP-1 was reported to stimulate glucose metabolism in human myocytes (173). Similar observations were made in studies of L6 myotubes, and there was Physiol Rev • VOL 1427 evidence that the effects were transmitted via receptors distinct from the classical GLP-1 receptor (336). Most recently, GLP-1 was again reported to enhance glucose uptake in human myocytes, and evidence for the involved signaling pathways was provided (80). It should be mentioned that other studies failed to identify actions of GLP-1 on glucose metabolism in muscle tissue (72). Some of the cited studies suggested that GLP-1 may activate more than one receptor. As discussed above, a study of the enterogastrone effects of GLP-1 and PYY in dogs, where the GLP-1 receptor antagonist exendin 9 –39 was incapable of blocking the inhibitory actions of GLP-1 (71), suggested that another receptor was involved. In other studies, the local paracrine actions of GLP-1 in the canine ileum could not be blocked by exendin 9 –39 (38). The effects of intraportal GLP-1 on impulse traffic in vagal afferent sensory nerve fibers were also resistant to exendin 9 –39 (219). The liver has repeatedly been reported to be a target for GLP-1, although initial careful studies indicated that hepatocytes did not express GLP-1 receptor (17). Thus GLP-1 has been reported to bind to rat hepatic membranes but without influencing adenylate cyclase activity, as expected from the classical GLP-1 receptor (308). Rather, inositol phosphoglycans were thought to act as mediators (291). The same group also described activation of phosphatidylinositol 3-kinase/protein kinase B, protein kinase C, and protein phosphatase-1 pathways to transmit the actions on glycogen synthase in rat hepatocytes (250). Ikezawa et al. (138) reported inhibition of glucagon-induced glycogenolysis in isolated perivenous rat hepatocytes. Along the same lines, some studies have reported effects of exendin 4 that are not shared by GLP-1. Thus exendin 4, but not GLP-1, was reported to enhance insulin sensitivity in 3T3 adipocytes (137). The two peptides were also reported to activate different signaling pathways in human myotubes (80). Again, it should be noted that these in vitro studies are in sharp contrast to the in vivo studies, particularly in humans, as discussed above. VII. GLUCAGON-LIKE PEPTIDE 1 PATHOPHYSIOLOGY Abnormal function of GLP-1 has been implicated in three pathological conditions: obesity, postprandial reactive hypoglycemia, and type 2 diabetes. A. Obesity A role for GLP-1 in the development of obesity was suggested partly because of the apparently physiological effects of the hormones on appetite and food intake (305), and partly because of the reports that GLP-1 secretion may be reduced in obesity. Thus, in 1983, it was demon- 87 • OCTOBER 2007 • www.prv.org 1428 JENS JUUL HOLST strated that the diurnal L-cell secretion (measured as enteroglucagon secretion) was dramatically decreased in morbid obesity (128), and in a subsequent study, again in morbidly obese subjects, there was no measurable increase in postprandial GLP-1 secretion (201). However, after a jejuno-ileal bypass operation, meal responses were restored to normal values. This should not be interpreted to suggest that the weight loss restored L-cell sensitivity to meal stimulation, since it is known that abnormal exposure of the distal gut to unabsorbed nutrients as occurs after jejuno-ileal bypass as well as gastric bypass operations results in exaggerated L-cell secretion (129, 235). However, obese subjects showing decreased postprandial GLP-1 responses compared with lean controls did exhibit improved secretion after weight loss (306). The mechanism whereby obesity lowers GLP-1 secretion is not known, but may be related to the insulin resistance that accompanies weight gain (248). It has been suggested that particularly the L-cell responsiveness to carbohydrates is affected (247) and that circulating fatty acids could be responsible (246). However, in a large study in both diabetic and nondiabetic subjects, in which body mass index again emerged as a significant negative factor for meal-induced GLP-1 secretion, free fatty acid levels did not appear to influence the responses upon multiple regression analysis (288). Together, the data would suggest that the decreased GLP-1 secretion in obesity, which is not a consistent finding (317), develops secondarily to weight gain. However, in view of the likely role of GLP-1 as a regulator of appetite and food intake, it remains possible that the decreased secretion results in inadequate postprandial satiation and therefore contributes to the positive energy balance of developing obesity. Further support for an important role of GLP-1 (and PYY) in the regulation of appetite and food intake comes from studies of GLP-1 secretion after bariatric surgery. As a rule, the weight loss after surgery does not involve malabsorption, and although the reduced gastric capacity undoubtedly contributes, the secretion of GLP-1 (and PYY) is greatly elevated, particularly after bypass operations, and is believed to result in reduced appetite and food intake and hence weight loss (165, 194, 235). It is of interest that the operations also cause a dramatic improvement in glucose tolerance that occurs very early postoperatively, before a major weight loss has been achieved (88). Again, it is thought that the exaggerated GLP-1 secretion may be responsible, via its effects on insulin and glucagon secretion. B. Reactive Hypoglycemia In agreement with increased exposure to nutrients of the distal small intestinal mucosa, where the density of Physiol Rev • VOL L-cells is highest, as the likely explanation for exaggerated GLP-1 responses after bariatric surgery, GLP-1 secretion is also strongly dependent on gastric emptying rates and hence the rate of exposure of the small intestinal mucosa to nutrients (187). Therefore, conditions with accelerated gastric emptying are also associated with exaggerated GLP-1 responses (187). It was, therefore, proposed that exaggerated GLP-1 secretion might be responsible for the postprandial reactive hypoglycemia that may be observed after gastric surgery (gastrectomy) (187) as well as after gastric bypass operations (264). Indeed, if the postprandial glucose and GLP-1 responses observed in such patients were reproduced in healthy subjects by intravenous infusion, it was possible to create a dramatic hypoglycemic response, partly due to enhanced insulin secretion and partly due to suppressed glucagon secretion (286). In gastrectomized subjects with reactive hypoglycemia, postprandial glucagon concentrations may be elevated compared with nonoperated controls (6), but this is probably a consequence of the generalized sympathetic discharge that accompanies the “dumping syndrome” of which the reactive hypoglycemia is part (76). It has been proposed that the gastric bypass operations in some cases might result in the development of hyperinsulinemic pancreatic nesidioblastosis as a result of the trophic effects of GLP-1 on the beta cells (235, 264). However, in a subsequent reanalysis of the pancreatic sections on which this hypothesis was based, the existence of nesidioblastosis could not be confirmed (179), and the most likely explanation for the hypoglycemic attacks is probably exaggerated GLP-1-stimulated insulin secretion in combination with alleviation of insulin resistance after weight loss and lack of downregulation of functional beta cell mass [which may have been increased because of obesity (32)] after weight loss. The effects of GLP-1 on appetite and food intake show up very strongly in clinical studies involving native GLP-1, GLP-1 analogs, or GLP-1 receptor activators like exendin. Although nearly all studies so far have been aimed at treating type 2 diabetes, an important and constant finding has been a continued and sustained weight loss both in short-term and chronic studies (19, 108, 148, 340). This obviously has important clinical implications. C. Diabetes The main clinical interest in GLP-1 focuses on its role in the development and treatment of type 2 diabetes. Type 2 diabetes is characterized by a severely reduced or absent incretin effect (203), and this undoubtedly contributes to the inappropriate insulin secretion that characterizes the disease. It is now clear that the incretin defect is due to an almost complete loss of the insulinotropic effect of GIP (206, 314), whereas the secretion of GIP is normal 87 • OCTOBER 2007 • www.prv.org THE PHYSIOLOGY OF GLUCAGON-LIKE PEPTIDE 1 or near normal (288). Regarding GLP-1, a significant and sometimes substantial reduction in meal-induced GLP-1 secretion is found whether this is measured as the concentrations of the intact hormone or the metabolite GLP-1 9 –36 amide (see above) (288, 312). In contrast to GIP, the insulinotropic effect of GLP-1 is retained in patients with type 2 diabetes (206), and it is possible with infusions of GLP-1 to completely normalize glucose-induced insulin secretion in the patients as analyzed in hyperglycemic clamp experiments (150, 314). However, from dose-response studies it appears that the potency of GLP-1 with respect to enhancing glucose-induced insulin secretion is greatly reduced (to ⬃20%) in the patients compared with healthy controls (150). Thus both defects in the secretion and actions of the incretin hormones are responsible for the reduced incretin effect and hence the inadequate insulin secretion seen in the patients. The question then arises whether these defects are primary or secondary in relation to diabetes, but the evidence to date suggests that the abnormalities are secondary to the development of diabetes and/or insulin resistance. Thus the secretion of both GIP and GLP-1 is normal in glucose-tolerant first-degree relatives of individuals with type 2 diabetes (222). Similarly, incretin secretion was normal in women with previous gestational diabetes who are at particularly high risk for developing type 2 diabetes (180). In a study in identical twins, discordant for type 2 diabetes (at the time of investigation), only the diabetic twin had decreased GLP-1 secretion (299). And finally, in patients with diabetes secondary to chronic pancreatitis, a similar incretin deficiency develops early in the development of diabetes, and reduced effects of the incretin hormones are also similar to those observed in the classical obese type 2 diabetic patients (311). In a detailed study of 55 patients with type 2 diabetes as well as in individuals with impaired or normal glucose tolerance, mealinduced GLP-1 secretion was negatively associated with body mass index as discussed above, but also with the presence or absence of diabetes (lower responses in diabetic subjects), whereas factors such as the presence or absence of neuropathy and concentrations of free fatty acids in plasma did not seem to play a role (288). As already mentioned, it is possible that insulin sensitivity is of importance (248). The molecular mechanisms underlying the reduced beta-cell sensitivity to GLP-1 and the nearly lost sensitivity to GIP are currently unknown. However, the fact that insulin secretion can be restored to normal levels by administration of GLP-1 (in other words, that the beta-cell responsiveness to glucose is normalized) is clearly of considerable clinical interest and provides part of the background for the clinical use of GLP-1 receptor agonists in diabetes treatment. Intravenous administration of slightly supraphysiological amounts of GLP-1 can completely normalize fasting glucose concentrations in type 2 diabetic patients regardless of the severity and duration of disease (207, 289) and may nearly normalize also postprandial glucose responses (245). It is Physiol Rev • VOL 1429 believed that several of the many actions of GLP-1 are involved in its antidiabetic effects (115). One important mechanism is of course the restoration of glucose-induced insulin secretion. Generally, peripheral insulin levels do not increase during chronic GLP-1 treatment, but these levels are maintained in spite of the concomitant reductions of plasma glucose by up to 5– 6 mM (340). Upon intravenous infusion of GLP-1 to fasting type 2 diabetic subjects, insulin secretion first rises, but then, as plasma glucose concentrations are lowered, decreases again to baseline levels (210). The numerous molecular actions of GLP-1 on the beta cell have been discussed above. Another important factor is the inhibition of glucagon secretion. Again, during intravenous infusion of GLP-1 to fasting type 2 diabetic subjects, glucagon secretion is suppressed as long as plasma glucose is still elevated, but as glucose concentrations approach normal values, glucagon secretion again rises to baseline levels (210). In chronic studies, mean glucagon levels may be significantly lowered or remain at baseline levels, but this again occurs in the face of much lower plasma glucose concentrations which, all others being equal, would have resulted in higher levels of glucagon (340). As already alluded to, the importance of the inhibition of glucagon secretion for the antidiabetic actions of GLP-1 showed up clearly in a study in patients with type 1 diabetes and no residual beta-cell function. In these patients GLP-1 infusion still lowered plasma glucose in parallel with a rather strong reduction in glucagon levels (35). The inhibition of gastric emptying also plays an important role as this greatly reduces postprandial glucose excursions (332). This effect, which in healthy subjects shows rapid tachyphylaxis (181a), is retained also in chronic studies involving short-acting GLP-1 receptor agonists (exendin 4) (147). The clinical results with GLP-1 receptor activators, now often designated incretin mimetics, are promising and suggest that one can expect lasting improvement of glycemic control as evidenced by much improved levels of glycated hemoglobin (HbA1c) (19). Synthetic exendin 4 (exenatide) was approved for diabetes treatment in 2005 and is commercially available under the trade name Byetta (www.byetta.com). Exendin 4 was isolated from the venom of the lizard, Heloderma suspectum, in a systematic search for biologically active peptides (64) and is, as discussed above, a full agonist for the GLP-1 receptor which is equipotent with GLP-1 (284). Unlike GLP-1, it is not degraded by DPP-IV and is cleared in the kidneys only by glomerular filtration (266), whereby the molecule obtains a half-life of ⬃30 min (58). After subcutaneous injection of the maximally tolerated dose, a significant elevation of its plasma concentration may be observed for 5 h (156). Because of its stability relative to GLP-1, exendin 4 has been very useful as a tool for elucidating the actions of GLP-1 particularly in rodents, where the survival of GLP-1 is so brief that it is difficult to detect any 87 • OCTOBER 2007 • www.prv.org 1430 JENS JUUL HOLST effects of the peptide at all. GLP-1 analogs still under clinical development include Liraglutide, which consists of the GLP-1 molecule to which is attached a C-16 acyl chain (via a glutamic acid linker) to Lys-26 (while Lys-33 is substituted by Arg to prevent acylation here) (152). Thereby, the molecule binds to albumin and acquires some of the pharmacokinetics of this molecule. The renal elimination is prevented for the bound molecule, and its half-life after subcutaneous injections is ⬃12 h. Clinically, the molecule has similar actions as continuously infused GLP-1 (48) and appears to have a similar clinical potential as exendin 4 (318). The antidiabetic effects of GLP-1 can also be exploited by protecting endogenous GLP-1 from degradation by the enzyme DPP-IV (122). Administration of inhibitors of this enzyme increases the circulating levels of both active GLP-1 and GIP, and this is associated with the expected antidiabetic effects (43). The inhibitors are small molecules that are active upon oral administration, and they appear to have chronic antidiabetic effects that are very similar to those obtained with the incretin mimetics, which all require parenteral administration (2). However, the inhibitors have little effects on body weight, presumably because the plasma concentrations of active GLP-1 are not elevated sufficiently to exert this effect (42). One explanation for this appears to be a negativefeedback inhibition of L-cell secretion by the elevated levels of active GLP-1 brought about by DPP-IV inhibition (47), an effect which may be mediated by a paracrine action of somatostatin secreted from neighboring D-cells in the gut (97, 98). Because of the negative-feedback inhibition, the concentrations of active GLP-1 only rise by a factor of two to three, where one would have expected an up to fivefold increase if L-cell secretion had been unaltered (122). Elegant experiments in mice with deletions of the genes for the two incretin hormone receptors have shown that whereas DPP-IV inhibitors effectively lowered blood glucose and stimulated insulin secretion in animals with a single deletion, they had no effect in mice in which both receptor genes were deleted (102). Thus their effect in nondiabetic mice can be ascribed to enhancement of the actions of both incretin hormones, while mechanisms beyond protection of these hormones do not appear to play a role. Several specific inhibitors are currently undergoing clinical development, and for two inhibitors [Januvia (www.Merck.com) and Galvus (www.novartis.com)], applications for registration as new drugs were filed with the American Food and Drug Administration in 2006, and Januvia was approved in Mexico and the United States in the fall of 2006. ACKNOWLEDGMENTS Address for reprint requests and other correspondence: J. J. Holst, Dept. of Medical Physiology, The Panum Institute, Physiol Rev • VOL Univ. of Copenhagen, DK-2200 Copenhagen, Denmark (e-mail: holst@mfi.ku.dk). REFERENCES 1. Ahren B. Sensory nerves contribute to insulin secretion by glucagon-like peptide-1 in mice. Am J Physiol Regul Integr Comp Physiol 286: R269 –R272, 2004. 2. Ahren B, Gomis R, Standl E, Mills D, Schweizer A. Twelve- and 52-week efficacy of the dipeptidyl peptidase IV inhibitor LAF237 in metformin-treated patients with type 2 diabetes. Diabetes Care 27: 2874 –2880, 2004. 3. Ahren B, Holst JJ. The cephalic insulin response to meal ingestion in humans is dependent on both cholinergic and noncholinergic mechanisms and is important for postprandial glycemia. Diabetes 50: 1030 –1038, 2001. 4. Ahren B, Larsson H, Holst JJ. Effects of glucagon-like peptide-1 on islet function and insulin sensitivity in noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 82: 473– 478, 1997. 5. Alvarez E, Martinez MD, Roncero I, Chowen JA, GarciaCuartero B, Gispert JD, Sanz C, Vazquez P, Maldonado A, de CJ, Desco M, Pozo MA, Blazquez E. The expression of GLP-1 receptor mRNA and protein allows the effect of GLP-1 on glucose metabolism in the human hypothalamus and brainstem. J Neurochem 92: 798 – 806, 2005. 6. Andreasen JJ, Orskov C, Holst JJ. Secretion of glucagon-like peptide-1 and reactive hypoglycemia after partial gastrectomy. Digestion 55: 221–228, 1994. 7. Anini Y, Brubaker PL. Muscarinic receptors control glucagon-like peptide 1 secretion by human endocrine L cells. Endocrinology 144: 3244 –3250, 2003. 8. Baggio L, Kieffer TJ, Drucker DJ. Glucagon-like peptide-1, but not glucose-dependent insulinotropic peptide, regulates fasting glycemia and nonenteral glucose clearance in mice. Endocrinology 141: 3703–3709, 2000. 9. Baldissera FG, Holst JJ. Glucagon-related peptides in the human gastrointestinal mucosa. Diabetologia 26: 223–228, 1984. 10. Baldissera FG, Holst JJ. Glicentin 1– 61 probably represents a major fraction of glucagon-related peptides in plasma of anaesthetized uraemic pigs. Diabetologia 29: 462– 467, 1986. 11. Balkan B, Li X. Portal GLP-1 administration in rats augments the insulin response to glucose via neuronal mechanisms. Am J Physiol Regul Integr Comp Physiol 279: R1449 –R1454, 2000. 12. Balks HJ, Holst JJ, von zur M, Brabant G. Rapid oscillations in plasma glucagon-like peptide-1 (GLP-1) in humans: cholinergic control of GLP-1 secretion via muscarinic receptors. J Clin Endocrinol Metab 82: 786 –790, 1997. 13. Bataille D, Tatemoto K, Gespach C, Jornvall H, Rosselin G, Mutt V. Isolation of glucagon-37 (bioactive enteroglucagon/oxyntomodulin) from porcine jejuno-ileum. Characterization of the peptide. FEBS Lett 146: 79 – 86, 1982. 14. Bell GI, Sanchez-Pescador R, Laybourn PJ, Najarian RC. Exon duplication and divergence in the human preproglucagon gene. Nature 304: 368 –371, 1983. 15. Bell GI, Santerre RF, Mullenbach GT. Hamster preproglucagon contains the sequence of glucagon and two related peptides. Nature 302: 716 –718, 1983. 16. Bertin E, Arner P, Bolinder J, Hagstrom-Toft E. Action of glucagon and glucagon-like peptide-1- (7–36) amide on lipolysis in human subcutaneous adipose tissue and skeletal muscle in vivo. J Clin Endocrinol Metab 86: 1229 –1234, 2001. 17. Blackmore PF, Mojsov S, Exton JH, Habener JF. Absence of insulinotropic glucagon-like peptide-I (7–37) receptors on isolated rat liver hepatocytes. FEBS Lett 283: 7–10, 1991. 18. Blat S, Guerin S, Chauvin A, Seve B, Morgan L, Cuber JC, Malbert CH. The vagus is inhibitory of the late postprandial insulin secretion in conscious pigs. Auton Neurosci 101: 68 –77, 2002. 19. Blonde L, Klein EJ, Han J, Zhang B, Mac SM, Poon TH, Taylor KL, Trautmann ME, Kim DD, Kendall DM. Interim analysis of the effects of exenatide treatment on A1C, weight and cardiovas- 87 • OCTOBER 2007 • www.prv.org THE PHYSIOLOGY OF GLUCAGON-LIKE PEPTIDE 1 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. cular risk factors over 82 weeks in 314 overweight patients with type 2 diabetes. Diabetes Obes Metab 8: 436 – 447, 2006. Bock T, Pakkenberg B, Buschard K. The endocrine pancreas in non-diabetic rats after short-term and long-term treatment with the long-acting GLP-1 derivative NN2211. APMIS 111: 1117–1124, 2003. Bonner-Weir S. Beta-cell turnover: its assessment and implications. Diabetes 50 Suppl 1: S20 –S24, 2001. Bose AK, Mocanu MM, Carr RD, Brand CL, Yellon DM. Glucagon-like peptide 1 can directly protect the heart against ischemia/ reperfusion injury. Diabetes 54: 146 –151, 2005. Bottcher G, Alumets J, Hakanson R, Sundler F. Co-existence of glicentin and peptide YY in colorectal L-cells in cat and man. An electron microscopic study. Regul Pept 13: 283–291, 1986. Brubaker PL, Drucker DJ. Minireview: glucagon-like peptides regulate cell proliferation and apoptosis in the pancreas, gut, central nervous system. Endocrinology 145: 2653–2659, 2004. Bryant MG, Bloom SR, Polak JM, Hobbs S, Domschke W, Domschke S, Mitznegg P, Ruppin H, Demling L. Measurement of gut hormonal peptides in biopsies from human stomach and proximal small intestine. Gut 24: 114 –119, 1983. Buffa R, Capella C, Fontana P, Usellini L, Solcia E. Types of endocrine cells in the human colon and rectum. Cell Tissue Res 192: 227–240, 1978. Buhl T, Thim L, Kofod H, Orskov C, Harling H, Holst JJ. Naturally occurring products of proglucagon 111–160 in the porcine and human small intestine. J Biol Chem 263: 8621– 8624, 1988. Bullock BP, Heller RS, Habener JF. Tissue distribution of messenger ribonucleic acid encoding the rat glucagon-like peptide-1 receptor. Endocrinology 137: 2968 –2978, 1996. Burcelin R, Da Costa A, Drucker D, Thorens B. Glucose competence of the hepatoportal vein sensor requires the presence of an activated glucagon-like peptide-1 receptor. Diabetes 50: 1720 –1728, 2001. Buteau J, El-Assaad W, Rhodes CJ, Rosenberg L, Joly E, Prentki M. Glucagon-like peptide-1 prevents beta cell glucolipotoxicity. Diabetologia 47: 806 – 815, 2004. Buteau J, Roduit R, Susini S, Prentki M. Glucagon-like peptide-1 promotes DNA synthesis, activates phosphatidylinositol 3-kinase and increases transcription factor pancreatic and duodenal homeobox gene 1 (PDX-1) DNA binding activity in beta (INS-1)cells. Diabetologia 42: 856 – 864, 1999. Butler AE, Janson J, Bonner-Weir S, Ritzel R, Rizza RA, Butler PC. Beta-cell deficit and increased beta-cell apoptosis in humans with type 2 diabetes. Diabetes 52: 102–110, 2003. Campos RV, Lee YC, Drucker DJ. Divergent tissue-specific and developmental expression of receptors for glucagon and glucagonlike peptide-1 in the mouse. Endocrinology 134: 2156 –2164, 1994. Chelikani PK, Haver AC, Reidelberger RD. Ghrelin attenuates the inhibitory effects of glucagon-like peptide-1 and peptide YY (3–36) on food intake and gastric emptying in rats. Diabetes 55: 3038 –3046, 2006. Creutzfeldt WO, Kleine N, Willms B, Orskov C, Holst JJ, Nauck MA. Glucagonostatic actions and reduction of fasting hyperglycemia by exogenous glucagon-like peptide I (7–36) amide in type I diabetic patients. Diabetes Care 19: 580 –586, 1996. D’Alessio DA, Kahn SE, Leusner CR, Ensinck JW. Glucagonlike peptide 1 enhances glucose tolerance both by stimulation of insulin release and by increasing insulin-independent glucose disposal. J Clin Invest 93: 2263–2266, 1994. Dakin CL, Gunn I, Small CJ, Edwards CM, Hay DL, Smith DM, Ghatei MA, Bloom SR. Oxyntomodulin inhibits food intake in the rat. Endocrinology 142: 4244 – 4250, 2001. Daniel EE, Anvari M, Fox-Threlkeld JE, McDonald TJ. Local, exendin- (9 –39)-insensitive, site of action of GLP-1 in canine ileum. Am J Physiol Gastrointest Liver Physiol 283: G595–G602, 2002. Dardevet D, Moore MC, Neal D, DiCostanzo CA, Snead W, Cherrington AD. Insulin-independent effects of GLP-1 on canine liver glucose metabolism: duration of infusion and involvement of hepatoportal region. Am J Physiol Endocrinol Metab 287: E75– E81, 2004. De Heer J, Holst JJ. Sulfonylurea compounds uncouple the glucose dependence of the insulinotropic effect of glucagon-like peptide 1. Diabetes. In press. Physiol Rev • VOL 1431 41. De Heer J, Hoy M, Holst JJ. GLP-1, but not GIP, inhibits glucagon secretion via somatostatin in the perfused rat pancreas (Abstract). Diabetologia 48 Suppl 1: A64, 2005. 42. Deacon CF. MK431 (Merck). Curr Opin Invest Drugs 6: 419 – 426, 2005. 43. Deacon CF, Holst JJ. Dipeptidyl peptidase IV inhibitors: a promising new therapeutic approach for the management of type 2 diabetes. Int J Biochem Cell Biol 38: 831– 844, 2006. 44. Deacon CF, Johnsen AH, Holst JJ. Degradation of glucagon-like peptide-1 by human plasma in vitro yields an N-terminally truncated peptide that is a major endogenous metabolite in vivo. J Clin Endocrinol Metab 80: 952–957, 1995. 45. Deacon CF, Plamboeck A, Moller S, Holst JJ. GLP-1- (9 –36) amide reduces blood glucose in anesthetized pigs by a mechanism that does not involve insulin secretion. Am J Physiol Endocrinol Metab 282: E873–E879, 2002. 46. Deacon CF, Pridal L, Klarskov L, Olesen M, Holst JJ. Glucagon-like peptide 1 undergoes differential tissue-specific metabolism in the anesthetized pig. Am J Physiol Endocrinol Metab 271: E458 –E464, 1996. 47. Deacon CF, Wamberg S, Bie P, Hughes TE, Holst JJ. Preservation of active incretin hormones by inhibition of dipeptidyl peptidase IV suppresses meal-induced incretin secretion in dogs. J Endocrinol 172: 355–362, 2002. 48. Degn KB, Juhl CB, Sturis J, Jakobsen G, Brock B, Chandramouli V, Rungby J, Landau BR, Schmitz O. One week’s treatment with the long-acting glucagon-like peptide 1 derivative liraglutide (NN2211) markedly improves 24-h glycemia and alphaand beta-cell function and reduces endogenous glucose release in patients with type 2 diabetes. Diabetes 53: 1187–1194, 2004. 49. Delgado E, Luque MA, Alcantara A, Trapote MA, Clemente F, Galera C, Valverde I, Villanueva Penacarrillo ML. Glucagonlike peptide-1 binding to rat skeletal muscle. Peptides 16: 225–229, 1995. 50. Ding WG, Renstrom E, Rorsman P, Buschard K, Gromada J. Glucagon-like peptide I and glucose-dependent insulinotropic polypeptide stimulate Ca2⫹-induced secretion in rat alpha-cells by a protein kinase A-mediated mechanism. Diabetes 46: 792– 800, 1997. 51. Drucker DJ. The biology of incretin hormones. Cell Metab 3: 153–165, 2006. 52. Drucker DJ, Asa S. Glucagon gene expression in vertebrate brain. J Biol Chem 263: 13475–13478, 1988. 53. Drucker DJ, Jin T, Asa SL, Young TA, Brubaker PL. Activation of proglucagon gene transcription by protein kinase-A in a novel mouse enteroendocrine cell line. Mol Endocrinol 8: 1646 –1655, 1994. 54. Dumoulin V, Dakka T, Plaisancie P, Chayvialle JA, Cuber JC. Regulation of glucagon-like peptide-1- (7–36) amide, peptide YY, neurotensin secretion by neurotransmitters and gut hormones in the isolated vascularly perfused rat ileum. Endocrinology 136: 5182–5188, 1995. 55. During MJ, Cao L, Zuzga DS, Francis JS, Fitzsimons HL, Jiao X, Bland RJ, Klugmann M, Banks WA, Drucker DJ, Haile CN. Glucagon-like peptide-1 receptor is involved in learning and neuroprotection. Nat Med 9: 1173–1179, 2003. 56. Dyachok O, Isakov Y, Sagetorp J, Tengholm A. Oscillations of cyclic AMP in hormone-stimulated insulin-secreting beta-cells. Nature 439: 349–352, 2006. 57. Edvell A, Lindstrom P. Initiation of increased pancreatic islet growth in young normoglycemic mice (Umea ⫹/?). Endocrinology 140: 778 –783, 1999. 58. Edwards CM, Stanley SA, Davis R, Brynes AE, Frost GS, Seal LJ, Ghatei MA, Bloom SR. Exendin-4 reduces fasting and postprandial glucose and decreases energy intake in healthy volunteers. Am J Physiol Endocrinol Metab 281: E155–E161, 2001. 59. Egan JM, Bulotta A, Hui H, Perfetti R. GLP-1 receptor agonists are growth and differentiation factors for pancreatic islet beta cells. Diabetes Metab Res Rev 19: 115–123, 2003. 60. Egan JM, Meneilly GS, Habener JF, Elahi D. Glucagon-like peptide-1 augments insulin-mediated glucose uptake in the obese state. J Clin Endocrinol Metab 87: 3768 –3773, 2002. 87 • OCTOBER 2007 • www.prv.org 1432 JENS JUUL HOLST 61. Egan JM, Montrose Rafizadeh C, Wang Y, Bernier M, Roth J. Glucagon-like peptide-1 (7–36) amide (GLP-1) enhances insulinstimulated glucose metabolism in 3T3-L1 adipocytes: one of several potential extrapancreatic sites of GLP-1 action. Endocrinology 135: 2070 –2075, 1994. 62. Eissele R, Goke R, Willemer S, Harthus HP, Vermeer H, Arnold R, Goke B. Glucagon-like peptide-1 cells in the gastrointestinal tract and pancreas of rat, pig and man. Eur J Clin Invest 22: 283–291, 1992. 63. Elliott RM, Morgan LM, Tredger JA, Deacon S, Wright J, Marks V. Glucagon-like peptide-1 (7–36) amide and glucose-dependent insulinotropic polypeptide secretion in response to nutrient ingestion in man: acute post-prandial and 24-h secretion patterns. J Endocrinol 138: 159 –166, 1993. 64. Eng J, Kleinman WA, Singh L, Singh G, Raufman JP. Isolation and characterization of exendin-4, an exendin-3 analogue, from Heloderma suspectum venom. Further evidence for an exendin receptor on dispersed acini from guinea pig pancreas. J Biol Chem 267: 7402–7405, 1992. 65. Farilla L, Bulotta A, Hirshberg B, Li CS, Khoury N, Noushmehr H, Bertolotto C, Di MU, Harlan DM, Perfetti R. Glucagon-like peptide 1 inhibits cell apoptosis and improves glucose responsiveness of freshly isolated human islets. Endocrinology 144: 5149 –5158, 2003. 66. Farilla L, Hui H, Bertolotto C, Kang E, Bulotta A, Di MU, Perfetti R. Glucagon-like peptide-1 promotes islet cell growth and inhibits apoptosis in Zucker diabetic rats. Endocrinology 143: 4397– 4408, 2002. 67. Fehmann HC, Goke R, Goke B. Cell and molecular biology of the incretin hormones glucagon-like peptide-I and glucose-dependent insulin releasing polypeptide. Endocr Rev 16: 390 – 410, 1995. 68. Fieseler P, Bridenbaugh S, Nustede R, Martell J, Orskov C, Holst JJ, Nauck MA. Physiological augmentation of amino acidinduced insulin secretion by GIP and GLP-I but not by CCK-8. Am J Physiol Endocrinol Metab 268: E949 –E955, 1995. 69. Flamez D, Van Breusegem A, Scrocchi LA, Quartier E, Pipeleers D, Drucker DJ, Schuit F. Mouse pancreatic beta-cells exhibit preserved glucose competence after disruption of the glucagon-like peptide-1 receptor gene. Diabetes 47: 646 – 652, 1998. 70. Flint A, Raben A, Astrup A, Holst JJ. Glucagon-like peptide 1 promotes satiety and suppresses energy intake in humans. J Clin Invest 101: 515–520, 1998. 71. Fung LC, Chisholm C, Greenberg GR. Glucagon-like peptide-1(7–36) amide and peptide YY mediate intraduodenal fat-induced inhibition of acid secretion in dogs. Endocrinology 139: 189 –194, 1998. 72. Furnsinn C, Ebner K, Waldhausl W. Failure of GLP-1 (7–36) amide to affect glycogenesis in rat skeletal muscle. Diabetologia 38: 864 – 867, 1995. 73. Furuta M, Yano H, Zhou A, Rouille Y, Holst JJ, Carroll R, Ravazzola M, Orci L, Furuta H, Steiner DF. Defective prohormone processing and altered pancreatic islet morphology in mice lacking active SPC2. Proc Natl Acad Sci USA 94: 6646 – 6651, 1997. 74. Gameiro A, Reimann F, Habib AM, O’Malley D, Williams L, Simpson AK, Gribble FM. The neurotransmitters glycine and GABA stimulate glucagon-like peptide-1 release from the GLUTag cell line. J Physiol 569: 761–772, 2005. 75. Gault VA, O’Harte FP, Harriott P, Mooney MH, Green BD, Flatt PR. Effects of the novel (Pro3)GIP antagonist and exendin (9 –39) amide on GIP- and GLP-1-induced cyclic AMP generation, insulin secretion and postprandial insulin release in obese diabetic (ob/ob) mice: evidence that GIP is the major physiological incretin. Diabetologia 46: 222–230, 2003. 76. Gebhard B, Holst JJ, Biegelmayer C, Miholic J. Postprandial GLP-1, norepinephrine, reactive hypoglycemia in dumping syndrome. Dig Dis Sci 46: 1915–1923, 2001. 77. Gelling RW, Du XQ, Dichmann DS, Romer J, Huang H, Cui L, Obici S, Tang B, Holst JJ, Fledelius C, Johansen PB, Rossetti L, Jelicks LA, Serup P, Nishimura E, Charron MJ. Lower blood glucose, hyperglucagonemia, pancreatic alpha cell hyperplasia in glucagon receptor knockout mice. Proc Natl Acad Sci USA 100: 1438 –1443, 2003. Physiol Rev • VOL 78. Goke R, Fehmann HC, Linn T, Schmidt H, Krause M, Eng J, Goke B. Exendin-4 is a high potency agonist and truncated exendin- (9 –39)-amide an antagonist at the glucagon-like peptide 1- (7–36)-amide receptor of insulin-secreting beta-cells. J Biol Chem 268: 19650 –19655, 1993. 79. Goke R, Larsen PJ, Mikkelsen JD, Sheikh SP. Distribution of GLP-1 binding sites in the rat brain: evidence that exendin-4 is a ligand of brain GLP-1 binding sites. Eur J Neurosci 7: 2294 –2300, 1995. 80. Gonzalez N, Acitores A, Sancho V, Valverde I, VillanuevaPenacarrillo ML. Effect of GLP-1 on glucose transport and its cell signalling in human myocytes. Regul Pept 126: 203–211, 2005. 81. Grant SF, Thorleifsson G, Reynisdottir I, Benediktsson R, Manolescu A, Sainz J, Helgason A, Stefansson H, Emilsson V, Helgadottir A, Styrkarsdottir U, Magnusson KP, Walters GB, Palsdottir E, Jonsdottir T, Gudmundsdottir T, Gylfason A, Saemundsdottir J, Wilensky RL, Reilly MP, Rader DJ, Bagger Y, Christiansen C, Gudnason V, Sigurdsson G, Thorsteinsdottir U, Gulcher JR, Kong A, Stefansson K. Variant of transcription factor 7-like 2 (TCF7L2) gene confers risk of type 2 diabetes. Nat Genet 38: 320 –323, 2006. 82. Gribble FM, Williams L, Simpson AK, Reimann F. A novel glucose-sensing mechanism contributing to glucagon-like peptide-1 secretion from the GLUTag cell line. Diabetes 52: 1147–1154, 2003. 83. Grimelius L, Capella C, Buffa R, Polak JM, Pearse AG, Solcia E. Cytochemical and ultrastructural differentiation of enteroglucagon and pancreatic-type glucagon cells of the gastrointestinal tract. Virchows Arch B Cell Pathol 20: 217–228, 1976. 84. Groger G, Unger A, Holst JJ, Goebell H, Layer P. Ileal carbohydrates inhibit cholinergically stimulated exocrine pancreatic secretion in humans. Int J Pancreatol 22: 23–29, 1997. 85. Gromada J, Bokvist K, Ding WG, Holst JJ, Nielsen JH, Rorsman P. Glucagon-like peptide 1 (7–36) amide stimulates exocytosis in human pancreatic beta-cells by both proximal and distal regulatory steps in stimulus-secretion coupling. Diabetes 47: 57– 65, 1998. 86. Gromada J, Holst JJ, Rorsman P. Cellular regulation of islet hormone secretion by the incretin hormone glucagon-like peptide 1. Pflügers Arch 435: 583–594, 1998. 87. Gros R, You X, Baggio LL, Kabir MG, Sadi AM, Mungrue IN, Parker TG, Huang Q, Drucker DJ, Husain M. Cardiac function in mice lacking the glucagon-like peptide-1 receptor. Endocrinology 144: 2242–2252, 2003. 88. Guidone C, Manco M, Valera-Mora E, Iaconelli A, Gniuli D, Mari A, Nanni G, Castagneto M, Calvani M, Mingrone G. Mechanisms of recovery from type 2 diabetes after malabsorptive bariatric surgery. Diabetes 55: 2025–2031, 2006. 89. Gutniak MK, Juntti-Berggren L, Hellstrom PM, Guenifi A, Holst JJ, Efendic S. Glucagon-like peptide I enhances the insulinotropic effect of glibenclamide in NIDDM patients and in the perfused rat pancreas. Diabetes Care 19: 857– 863, 1996. 90. Gutniak MK, Larsson H, Sanders SW, Juneskans O, Holst JJ, Ahren B. GLP-1 tablet in type 2 diabetes in fasting and postprandial conditions. Diabetes Care 20: 1874 –1879, 1997. 91. Gutzwiller JP, Drewe J, Goke B, Schmidt H, Rohrer B, Lareida J, Beglinger C. Glucagon-like peptide-1 promotes satiety and reduces food intake in patients with diabetes mellitus type 2. Am J Physiol Regul Integr Comp Physiol 276: R1541–R1544, 1999. 92. Gutzwiller JP, Hruz P, Huber AR, Hamel C, Zehnder C, Drewe J, Gutmann H, Stanga Z, Vogel D, Beglinger C. Glucagon-like peptide-1 is involved in sodium and water homeostasis in humans. Digestion 73: 142–150, 2006. 93. Gutzwiller JP, Goke B, Drewe J, Hildebrand P, Ketterer S, Handschin D, Winterhalder R, Conen D, Beglinger C. Glucagon-like peptide-1: a potent regulator of food intake in humans. Gut 44: 81– 86, 1999. 94. Gutzwiller JP, Tschopp S, Bock A, Zehnder CE, Huber AR, Kreyenbuehl M, Gutmann H, Drewe J, Henzen C, Goeke B, Beglinger C. Glucagon-like peptide 1 induces natriuresis in healthy subjects and in insulin-resistant obese men. J Clin Endocrinol Metab 89: 3055–3061, 2004. 95. Hansen L. Proksimal styring af den distale tarms hormonsekretion: en duodenoileal loop (Dissertation). Copenhagen: Univ. of Copenhagen, 1999. 87 • OCTOBER 2007 • www.prv.org THE PHYSIOLOGY OF GLUCAGON-LIKE PEPTIDE 1 96. Hansen L, Deacon CF, Orskov C, Holst JJ. Glucagon-like peptide-1- (7–36)amide is transformed to glucagon-like peptide-1- (9 – 36)amide by dipeptidyl peptidase IV in the capillaries supplying the L cells of the porcine intestine. Endocrinology 140: 5356 –5363, 1999. 97. Hansen L, Hartmann B, Bisgaard T, Mineo H, Jørgensen PN, Holst JJ. Somatostatin restrains the secretion of glucagon-like peptide-1 and 2 from isolated perfused porcine ileum. Am J Physiol Endocrinol Metab 278: E1010 –E1018, 2000. 98. Hansen L, Hartmann B, Mineo H, Holst JJ. Glucagon-like peptide-1 secretion is influenced by perfusate glucose concentration and by a feedback mechanism involving somatostatin in isolated perfused porcine ileum. Regul Pept 118: 11–18, 2004. 99. Hansen L, Holst JJ. The effects of duodenal peptides on glucagon-like peptide-1 secretion from the ileum. A duodeno–ileal loop? Regul Pept 110: 39 – 45, 2002. 100. Hansen L, Lampert S, Mineo H, Holst JJ. Neural regulation of glucagon-like peptide-1 secretion in pigs. Am J Physiol Endocrinol Metab 287: E939 –E947, 2004. 102. Hansotia T, Baggio LL, Delmeire D, Hinke SA, Yamada Y, Tsukiyama K, Seino Y, Holst JJ, Schuit F, Drucker DJ. Double incretin receptor knockout (DIRKO) mice reveal an essential role for the enteroinsular axis in transducing the glucoregulatory actions of DPP-IV inhibitors. Diabetes 53: 1326 –1335, 2004. 103. Hartmann B, Johnsen AH, Orskov C, Adelhorst K, Thim L, Holst JJ. Structure, measurement, secretion of human glucagonlike peptide-2. Peptides 21: 73– 80, 2000. 104. Heding LG. Radioimmunological determination of pancreatic and gut glucagon in plasma. Diabetologia 7: 10 –19, 1971. 105. Heinrich G, Gros P, Habener JF. Glucagon gene sequence. Four of six exons encode separate functional domains of rat pre-proglucagon. J Biol Chem 259: 14082–14087, 1984. 106. Heller RS, Kieffer TJ, Habener JF. Insulinotropic glucagon-like peptide I receptor expression in glucagon-producing alpha-cells of the rat endocrine pancreas. Diabetes 46: 785–791, 1997. 107. Henriksen DB, Alexandersen P, Bjarnason NH, Vilsboll T, Hartmann B, Henriksen EEG, Byrjalsen I, Holst JJ, Christiansen C.Role of gastrointestinal hormones in postprandial reduction of bone resorption. J Bone Miner Res 18: 2180 –2189, 2003. 108. Henry RR, Ratner RE, Stonehouse AH, Guan X, Poon T, Malone JK, Kim D, Kendall DM. Exenatide maintained glycemic control with associated weight loss reduction over 2 years in patients with type 2 diabetes (Abstract). Diabetes 55: A116, 2006. 109. Herrmann-Rinke C, Voge A, Hess M, Goke B. Regulation of glucagon-like peptide-1 secretion from rat ileum by neurotransmitters and peptides. J Endocrinol 147: 25–31, 1995. 110. Hiles R, Carpenter T, Serota D, Schafer K, Ross P, Nelsen D, Rebelatto M. Exenatide does not cause pancreatic tumours or malignancies in rats and mice following a 2-year period of exposure (Abstract). Diabetes 53 Suppl 2: A380, 2004. 111. Hill ME, Asa SL, Drucker DJ. Essential requirement for Pax6 in control of enteroendocrine proglucagon gene transcription. Mol Endocrinol 13: 1474 –1486, 1999. 112. Hirasawa A, Tsumaya K, Awaji T, Katsuma S, Adachi T, Yamada M, Sugimoto Y, Miyazaki S, Tsujimoto G. Free fatty acids regulate gut incretin glucagon-like peptide-1 secretion through GPR120. Nat Med 11: 90 –94, 2005. 113. Holst JJ. Enteroglucagon. Annu Rev Physiol 59: 257–271, 1997. 114. Holst JJ. Evidence that glicentin contains the entire sequence of glucagon. Biochem J 187: 337–343, 1980. 115. Holst JJ. Glucagon-like peptide-1: from extract to agent. The Claude Bernard Lecture, 2005. Diabetologia 49: 253–260, 2006. 116. Holst JJ. Evidence that enteroglucagon (II) is identical with the C-terminal sequence (residues 33– 69) of glicentin. Biochem J 207: 381–388, 1982. 117. Holst JJ. Gut glucagon, enteroglucagon, gut glucagonlike immunoreactivity, glicentin— current status. Gastroenterology 84: 1602– 1613, 1983. 118. Holst JJ. On the physiology of GIP and GLP-1. Horm Metab Res 36: 747–754, 2004. 119. Holst JJ. Glucagon-like peptide 1 (GLP-1): an intestinal hormone signalling nutritional abundance, with an unusual therapeutic potential. Trends Endocrinol Metab 10: 229 –234, 1999. Physiol Rev • VOL 1433 120. Holst JJ, Aggestrup S, Loud FB, Olesen M. Content and gel filtration profiles of glucagon-like and somatostatin-like immunoreactivity in human fundic mucosa. J Clin Endocrinol Metab 56: 729 –732, 1983. 121. Holst JJ, Bersani M, Johnsen AH, Kofod H, Hartmann B, Orskov C. Proglucagon processing in porcine and human pancreas. J Biol Chem 269: 18827–18833, 1994. 122. Holst JJ, Deacon CF. Inhibition of the activity of dipeptidylpeptidase IV as a treatment for type 2 diabetes. Diabetes 47: 1663– 1670, 1998. 123. Holst JJ, Deacon CF. Glucagon-like peptide-1 mediates the therapeutic actions of DPP-IV inhibitors. Diabetologia 48: 612– 615, 2005. 124. Holst JJ, Gromada J. Role of incretin hormones in the regulation of insulin secretion in diabetic and nondiabetic humans. Am J Physiol Endocrinol Metab 287: E199 –E206, 2004. 125. Holst JJ, Orskov C. Incretin hormones–an update. Scand J Clin Lab Invest Suppl 75– 85, 2001. 126. Holst JJ, Orskov C, Nielsen OV, Schwartz TW. Truncated glucagon-like peptide I, an insulin-releasing hormone from the distal gut. FEBS Lett 211: 169 –174, 1987. 127. Holst JJ, Rasmussen TN, Harling H, Schmidt P. Effect of intestinal inhibitory peptides on vagally induced secretion from isolated perfused porcine pancreas. Pancreas 8: 80 – 87, 1993. 128. Holst JJ, Schwartz TW, Lovgreen NA, Pedersen O, BeckNielsen H. Diurnal profile of pancreatic polypeptide, pancreatic glucagon, gut glucagon and insulin in human morbid obesity. Int J Obesity 7: 529 –538, 1983. 129. Holst JJ, Sorensen TI, Andersen AN, Stadil F, Andersen B, Lauritsen KB, Klein HC. Plasma enteroglucagon after jejunoileal bypass with 3:1 or 1:3 jejunoileal ratio. Scand J Gastroenterol 14: 205–207, 1979. 130. Holz GG. Epac: a new cAMP-binding protein in support of glucagon-like peptide-1 receptor-mediated signal transduction in the pancreatic beta-cell. Diabetes 53: 5–13, 2004. 132. Holz GG, Kuhtreiber WM, Habener JF. Pancreatic beta-cells are rendered glucose-competent by the insulinotropic hormone glucagon-like peptide-1 (7–37). Nature 361: 362–365, 1993. 133. Holz GH, Kuhtreiber WM, Habener JF. Induction of glucose competence in pancreatic beta cells by glucagon- like peptide-1 (7–37). Trans Assoc Am Physicians 105: 260 –267, 1992. 134. Hupe-Sodmann K, Goke R, Goke B, Thole HH, Zimmermann B, Voigt K, McGregor GP. Endoproteolysis of glucagon-like peptide (GLP)-1 (7–36) amide by ectopeptidases in RINm5F cells. Peptides 18: 625– 632, 1997. 135. Hvidberg A, Nielsen MT, Hilsted J, Orskov C, Holst JJ. Effect of glucagon-like peptide-1 (proglucagon 78 –107amide) on hepatic glucose production in healthy man. Metabolism 43: 104 –108, 1994. 136. Iakoubov R, Izzo A, Yeung A, Whiteside CI, Brubaker PL. Protein kinase C is required for oleic acid-induced secretion of glucagon-like peptide-1 by intestinal endocrine L cells. Endocrinology 148: 1089 –1098, 2006. 137. Idris I, Patiag D, Gray S, Donnelly R. Exendin-4 increases insulin sensitivity via a PI-3-kinase-dependent mechanism: contrasting effects of GLP-1. Biochem Pharmacol 63: 993–996, 2002. 138. Ikezawa Y, Yamatani K, Ohnuma H, Daimon M, Manaka H, Sasaki H. Glucagon-like peptide-1 inhibits glucagon-induced glycogenolysis in perivenous hepatocytes specifically. Regul Pept 111: 207–210, 2003. 139. Imeryuz N, Yegen BC, Bozkurt A, Coskun T, VillanuevaPenacarrillo ML, Ulusoy NB. Glucagon-like peptide-1 inhibits gastric emptying via vagal afferent-mediated central mechanisms. Am J Physiol Gastrointest Liver Physiol 273: G920 –G927, 1997. 140. Ionut V, Hucking K, Liberty IF, Bergman RN. Synergistic effect of portal glucose and glucagon-like peptide-1 to lower systemic glucose and stimulate counter-regulatory hormones. Diabetologia 48: 967–975, 2005. 141. Ionut V, Liberty IF, Hucking K, Lottati M, Stefanovski D, Zheng D, Bergman RN. Exogenously imposed postprandial-like rises in systemic glucose and GLP-1 do not produce an incretin effect, suggesting an indirect mechanism of GLP-1 action. Am J Physiol Endocrinol Metab 291: E779 –E785, 2006. 87 • OCTOBER 2007 • www.prv.org 1434 JENS JUUL HOLST 142. Irwin DM, Wong J. Trout and chicken proglucagon: alternative splicing generates mRNA transcripts encoding glucagon-like peptide 2. Mol Endocrinol 9: 267–277, 1995. 143. Jackson RS, Creemers JW, Farooqi IS, Raffin-Sanson ML, Varro A, Dockray GJ, Holst JJ, Brubaker PL, Corvol P, Polonsky KS, Ostrega D, Becker KL, Bertagna X, Hutton JC, White A, Dattani MT, Hussain K, Middleton SJ, Nicole TM, Milla PJ, Lindley KJ, O’Rahilly S. Small-intestinal dysfunction accompanies the complex endocrinopathy of human proprotein convertase 1 deficiency. J Clin Invest 112: 1550 –1560, 2003. 144. Jin SL, Han VK, Simmons JG, Towle AC, Lauder JM, Lund PK. Distribution of glucagonlike peptide I (GLP-I), glucagon, glicentin in the rat brain: an immunocytochemical study. J Comp Neurol 271: 519 –532, 1988. 145. Kauth T, Metz J. Immunohistochemical localization of glucagonlike peptide 1. Use of poly- and monoclonal antibodies. Histochemistry 86: 509 –515, 1987. 146. Kemp DM, Habener JF. Insulinotropic hormone glucagon-like peptide 1 (GLP-1) activation of insulin gene promoter inhibited by p38 mitogen-activated protein kinase. Endocrinology 142: 1179 – 1187, 2001. 147. Kendall DM, Kim D, Maggs D. Incretin mimetics and dipeptidyl peptidase-IV inhibitors: a review of emerging therapies for type 2 diabetes. Diabetes Technol Ther 8: 385–396, 2006. 148. Kendall DM, Riddle MC, Rosenstock J, Zhuang D, Kim DD, Fineman MS, Baron AD. Effects of exenatide (exendin-4) on glycemic control over 30 weeks in patients with type 2 diabetes treated with metformin and a sulfonylurea. Diabetes Care 28: 1083– 1091, 2005. 149. Kieffer TJ, Habener JF. The glucagon-like peptides. Endocr Rev 20: 876 –913, 1999. 150. Kjems LL, Holst JJ, Volund A, Madsbad S. The influence of GLP-1 on glucose-stimulated insulin secretion: effects on beta-cell sensitivity in type 2 and nondiabetic subjects. Diabetes 52: 380 –386, 2003. 151. Knudsen JB, Holst JJ, Asnaes S, Johansen A. Identification of cells with pancreatic-type and gut-type glucagon immunoreactivity in the human colon. Acta Pathol Microbiol Scand 83: 741–743, 1975. 152. Knudsen LB, Nielsen PF, Huusfeldt PO, Johansen NL, Madsen K, Pedersen FZ, Thogersen H, Wilken M, Agerso H. Potent derivatives of glucagon-like peptide-1 with pharmacokinetic properties suitable for once daily administration. J Med Chem 43: 1664 –1669, 2000. 153. Knudsen LB, Pridal L. Glucagon-like peptide-1- (9 –36) amide is a major metabolite of glucagon-like peptide-1- (7–36) amide after in vivo administration to dogs, it acts as an antagonist on the pancreatic receptor. Eur J Pharmacol 318: 429 – 435, 1996. 154. Knuhtsen S, Holst JJ, Knigge U, Olesen M, Nielsen OV. Radioimmunoassay, pharmacokinetics, neuronal release of gastrinreleasing peptide in anesthetized pigs. Gastroenterology 87: 372– 378, 1984. 155. Kolligs F, Fehmann HC, Goke R, Goke B. Reduction of the incretin effect in rats by the glucagon-like peptide 1 receptor antagonist exendin (9 –39) amide. Diabetes 44: 16 –19, 1995. 156. Kolterman OG, Kim DD, Shen L, Ruggles JA, Nielsen LL, Fineman MS, Baron AD. Pharmacokinetics, pharmacodynamics, safety of exenatide in patients with type 2 diabetes mellitus. Am J Health Syst Pharm 62: 173–181, 2005. 157. Kreymann B, Williams G, Ghatei MA, Bloom SR. Glucagon-like peptide-1 7–36: a physiological incretin in man. Lancet 2: 1300 – 1304, 1987. 158. Lankat-Buttgereit B, Goke R, Fehmann HC, Richter G, Goke B. Molecular cloning of a cDNA encoding for the GLP-1 receptor expressed in rat lung. Exp Clin Endocrinol 102: 341–347, 1994. 160. Larsen PJ, Holst JJ. Glucagon-related peptide 1 (GLP-1): hormone and neurotransmitter. Regul Pept 128: 97–107, 2005. 161. Larsen PJ, Tang-Christensen M, Holst JJ, Orskov C. Distribution of glucagon-like peptide-1 and other preproglucagon-derived peptides in the rat hypothalamus and brainstem. Neuroscience 77: 257–270, 1997. 162. Lawrence MC, Bhatt HS, Easom RA. NFAT regulates insulin gene promoter activity in response to synergistic pathways induced by glucose and glucagon-like peptide-1. Diabetes 51: 691– 698, 2002. Physiol Rev • VOL 163. Layer P. Intestinale Regulation der Pankreasenzymsekretion: Stimulatorische und inhibitorische Mechanismen. Z Gastroenterol 30: 495– 497, 1992. 164. Layer P, Holst JJ, Grandt D, Goebell H. Ileal release of glucagon-like peptide-1 (GLP-1). Association with inhibition of gastric acid secretion in humans. Dig Dis Sci 40: 1074 –1082, 1995. 165. Le Roux CW, Aylwin SJ, Batterham RL, Borg CM, Coyle F, Prasad V, Shurey S, Ghatei MA, Patel AG, Bloom SR. Gut hormone profiles following bariatric surgery favor an anorectic state, facilitate weight loss, improve metabolic parameters. Ann Surg 243: 108 –114, 2006. 166. Lee YC, Asa SL, Drucker DJ. Glucagon gene 5⬘-flanking sequences direct expression of simian virus 40 large T antigen to the intestine, producing carcinoma of the large bowel in transgenic mice. J Biol Chem 267: 10705–10708, 1992. 167. Lefebvre PJ, Luyckx AS. Neurotransmitters and glucagon release from the isolated, perfused canine stomach. Diabetes 29: 697–701, 1980. 168. Li Y, Cao X, Li LX, Brubaker PL, Edlund H, Drucker DJ. -Cell Pdx1 expression is essential for the glucoregulatory, proliferative, cytoprotective actions of glucagon-like peptide-1. Diabetes 54: 482– 491, 2005. 169. Li Y, Hansotia T, Yusta B, Ris F, Halban PA, Drucker DJ. Glucagon-like peptide-1 receptor signaling modulates beta cell apoptosis. J Biol Chem 278: 471– 478, 2003. 170. Light PE, Manning Fox JE, Riedel MJ, Wheeler MB. Glucagonlike peptide-1 inhibits pancreatic ATP-sensitive potassium channels via a protein kinase A- and ADP-dependent mechanism. Mol Endocrinol 16: 2135–2144, 2002. 171. Lopez LC, Frazier ML, Su CJ, Kumar A, Saunders GF. Mammalian pancreatic preproglucagon contains three glucagon-related peptides. Proc Natl Acad Sci USA 80: 5485–5489, 1983. 172. Lund PK, Goodman RH, Dee PC, Habener JF. Pancreatic preproglucagon cDNA contains two glucagon-related coding sequences arranged in tandem. Proc Natl Acad Sci USA 79: 345–349, 1982. 173. Luque MA, Gonzalez N, Marquez L, Acitores A, Redondo A, Morales M, Valverde I, Villanueva-Penacarrillo ML. Glucagonlike peptide-1 (GLP-1) and glucose metabolism in human myocytes. J Endocrinol 173: 465– 473, 2002. 174. Mari A, Sallas WM, He YL, Watson C, Ligueros-Saylan M, Dunning BE, Deacon CF, Holst JJ, Foley JE. Vildagliptin, a dipeptidyl peptidase-IV inhibitor, improves model-assessed -cell function in patients with type 2 diabetes. J Clin Endocrinol Metab 90: 4888 – 4894, 2005. 175. Mari A, Schmitz O, Gastaldelli A, Oestergaard T, Nyholm B, Ferrannini E. Meal and oral glucose tests for assessment of beta-cell function: modeling analysis in normal subjects. Am J Physiol Endocrinol Metab 283: E1159 –E1166, 2002. 176. Mayo KE, Miller LJ, Bataille D, Dalle S, Goke B, Thorens B, Drucker DJ. International Union of Pharmacology. XXXV. The Glucagon Receptor Family. Pharmacol Rev 55: 167–194, 2003. 177. McIntyre N, Holdsworth CD, Turner DS.New interpretation of oral glucose tolerance. Lancet II: 20 –21, 1964. 178. McIntyre N, Holdsworth CD, Turner DS. Intestinal factors in the control of insulin secretion. J Clin Endocrinol Metab 25: 1317– 1324, 1965. 179. Meier JJ, Butler AE, Galasso R, Butler PC. Hyperinsulinemic hypoglycemia after gastric bypass surgery is not accompanied by islet hyperplasia or increased beta-cell turnover. Diabetes Care 29: 1554 –1559, 2006. 180. Meier JJ, Gallwitz B, Askenas M, Vollmer K, Deacon CF, Holst JJ, Schmidt WE, Nauck MA. Secretion of incretin hormones and the insulinotropic effect of gastric inhibitory polypeptide in women with a history of gestational diabetes. Diabetologia 48: 1872–1881, 2005. 181. Meier JJ, Gethmann A, Nauck MA, Goetze O, Schmitz F, Deacon CF, Gallwitz B, Schmidt WE, Holst JJ. The glucagonlike peptide 1 metabolite GLP-1 (9 –36)amide reduces postprandial glycemia independently of gastric emptying and insulin secretion in humans. Am J Physiol Endocrinol Metab 290: E1118 –E1123, 2006. 181a.Meier JJ, Kemmeries G, Holst JJ, Nauck MA. Erythromycin antagonizes the deceleration of gastric emptying by glucagon-like 87 • OCTOBER 2007 • www.prv.org THE PHYSIOLOGY OF GLUCAGON-LIKE PEPTIDE 1 182. 183. 184. 185. 186. 187. 188. 189. 190. 191. 192. 193. 194. 195. 196. 197. 198. 199. peptide 1 and unmasks its insulinotropic effect in healthy subjects. Diabetes 54: 2212–2218, 2005. Meier JJ, Nauck MA, Kranz D, Holst JJ, Deacon CF, Gaeckler D, Schmidt WE, Gallwitz B. Secretion, degradation, elimination of glucagon-like peptide 1 and gastric inhibitory polypeptide in patients with chronic renal insufficiency and healthy control subjects. Diabetes 53: 654 – 662, 2004. Meneilly GS, Greig N, Tildesley H, Habener JF, Egan JM, Elahi D. Effects of 3 months of continuous subcutaneous administration of glucagon-like peptide 1 in elderly patients with type 2 diabetes. Diabetes Care 26: 2835–2841, 2003. Meneilly GS, McIntosh CH, Pederson RA, Habener JF, Ehlers MR, Egan JM, Elahi D. Effect of glucagon-like peptide 1 (7–36 amide) on insulin-mediated glucose uptake in patients with type 1 diabetes. Diabetes Care 26: 837– 842, 2003. Meneilly GS, McIntosh CH, Pederson RA, Habener JF, Gingerich R, Egan JM, Finegood DT, Elahi D. Effect of glucagonlike peptide 1 on non-insulin-mediated glucose uptake in the elderly patient with diabetes. Diabetes Care 24: 1951–1956, 2001. Merida E, Delgado E, Molina LM, Villanueva Penacarrillo ML, Valverde I. Presence of glucagon and glucagon-like peptide-1(7–36)amide receptors in solubilized membranes of human adipose tissue. J Clin Endocrinol Metab 77: 1654 –1657, 1993. Miholic J, Orskov C, Holst JJ, Kotzerke J, Meyer HJ. Emptying of the gastric substitute, glucagon-like peptide-1 (GLP-1), reactive hypoglycemia after total gastrectomy. Dig Dis Sci 36: 1361– 1370, 1991. Moens K, Heimberg H, Flamez D, Huypens P, Quartier E, Ling Z, Pipeleers D, Gremlich S, Thorens B, Schuit F. Expression and functional activity of glucagon, glucagon-like peptide I, glucose-dependent insulinotropic peptide receptors in rat pancreatic islet cells. Diabetes 45: 257–261, 1996. Mojsov S, Heinrich G, Wilson IB, Ravazzola M, Orci L, Habener JF. Preproglucagon gene expression in pancreas and intestine diversifies at the level of post-translational processing. J Biol Chem 261: 11880 –11889, 1986. Mojsov S, Kopczynski MG, Habener JF. Both amidated and nonamidated forms of glucagon-like peptide I are synthesized in the rat intestine and the pancreas. J Biol Chem 265: 8001– 8008, 1990. Mojsov S, Weir GC, Habener JF. Insulinotropin: glucagon-like peptide I (7–37) co-encoded in the glucagon gene is a potent stimulator of insulin release in the perfused rat pancreas. J Clin Invest 79: 616 – 619, 1987. Montrose-Rafizadeh C, Yang H, Wang Y, Roth J, Montrose MH, Adams LG. Novel signal transduction and peptide specificity of glucagon-like peptide receptor in 3T3–L1 adipocytes. J Cell Physiol 172: 275–283, 1997. Moody AJ, Holst JJ, Thim L, Jensen SL. Relationship of glicentin to proglucagon and glucagon in the porcine pancreas. Nature 289: 514 –516, 1981. Morinigo R, Moize V, Musri M, Lacy AM, Navarro S, Marin JL, Delgado S, Casamitjana R, Vidal J. Glucagon-like peptide-1, peptide YY, hunger, satiety after gastric bypass surgery in morbidly obese subjects. J Clin Endocrinol Metab 91: 1735–1740, 2006. Mortensen K, christensen LL, Holst JJ, Orskov C. GLP-1 and GIP are colocalized in a subset of endocrine cells in the small intestine. Regul Pept 114: 189 –196, 2003. Murlin JR, Clough HD, Gibbs CBF, Stokes AM. J Biol Chem 56: 253–296, 1923. Nakabayashi H, Nishizawa M, Nakagawa A, Takeda R, Niijima A. Vagal hepatopancreatic reflex effect evoked by intraportal appearance of tGLP-1. Am J Physiol Endocrinol Metab 271: E808 – E813, 1996. Nakagawa A, Satake H, Nakabayashi H, Nishizawa M, Furuya K, Nakano S, Kigoshi T, Nakayama K, Uchida K. Receptor gene expression of glucagon-like peptide-1, but not glucose-dependent insulinotropic polypeptide, in rat nodose ganglion cells. Auton Neurosci 110: 36 – 43, 2004. Nakazaki M, Crane A, Hu M, Seghers V, Ullrich S, AguilarBryan L, Bryan J. cAMP-activated protein kinase-independent potentiation of insulin secretion by cAMP is impaired in SUR1 null islets. Diabetes 51: 3440 –3449, 2002. Physiol Rev • VOL 1435 200. Naslund E, Barkeling B, King N, Gutniak M, Blundell JE, Holst JJ, Rossner S, Hellstrom PM. Energy intake and appetite are suppressed by glucagon-like peptide-1 (GLP-1) in obese men. Int J Obes Relat Metab Disord 23: 304 –311, 1999. 201. Naslund E, Gryback P, Backman L, Jacobsson H, Holst JJ, Theodorsson E, Hellstrom PM. Distal small bowel hormones: correlation with fasting antroduodenal motility and gastric emptying. Dig Dis Sci 43: 945–952, 1998. 202. Nauck M, Schmidt WE, Ebert R, Strietzel J, Cantor P, Hoffmann G, Creutzfeldt W. Insulinotropic properties of synthetic human gastric inhibitory polypeptide in man: interactions with glucose, phenylalanine, cholecystokinin-8. J Clin Endocrinol Metab 69: 654 – 662, 1989. 203. Nauck M, Stockmann F, Ebert R, Creutzfeldt W. Reduced incretin effect in type 2 (non-insulin-dependent) diabetes. Diabetologia 29: 46 –52, 1986. 204. Nauck MA, Bartels E, Orskov C, Ebert R, Creutzfeldt W. Additive insulinotropic effects of exogenous synthetic human gastric inhibitory polypeptide and glucagon-like peptide-1- (7–36) amide infused at near-physiological insulinotropic hormone and glucose concentrations. J Clin Endocrinol Metab 76: 912–917, 1993. 205. Nauck MA, Heimesaat MM, Behle K, Holst JJ, Nauck MS, Ritzel R, Hufner M, Schmiegel WH. Effects of glucagon-like peptide 1 on counterregulatory hormone responses, cognitive functions, insulin secretion during hyperinsulinemic, stepped hypoglycemic clamp experiments in healthy volunteers. J Clin Endocrinol Metab 87: 1239 –1246, 2002. 206. Nauck MA, Heimesaat MM, Orskov C, Holst JJ, Ebert R, Creutzfeldt W. Preserved incretin activity of glucagon-like peptide 1 [7–36 amide] but not of synthetic human gastric inhibitory polypeptide in patients with type-2 diabetes mellitus. J Clin Invest 91: 301–307, 1993. 207. Nauck MA, Holst JJ, Willms B. Glucagon-like peptide 1 and its potential in the treatment of non-insulin-dependent diabetes mellitus. Horm Metab Res 29: 411– 416, 1997. 208. Nauck MA, Homberger E, Siegel Allen RC, Eaton RP, Ebert R, Creutzfeldt W. Incretin effects of increasing glucose loads in man calculated from venous insulin and C-peptide responses. J Clin Endocrinol Metab 63: 492– 498, 1986. 210. Nauck MA, Kleine N, Orskov C, Holst JJ, Willms B, Creutzfeldt W. Normalization of fasting hyperglycaemia by exogenous glucagon-like peptide 1 (7–36 amide) in type 2 (non-insulindependent) diabetic patients. Diabetologia 36: 741–744, 1993. 211. Nauck MA, Niedereichholz U, Ettler R, Holst JJ, Orskov C, Ritzel R, Schmiegel WH. Glucagon-like peptide 1 inhibition of gastric emptying outweighs its insulinotropic effects in healthy humans. Am J Physiol Endocrinol Metab 273: E981–E988, 1997. 212. Nauck MA, Siemsgluss J, Orskov C, Holst JJ. Release of glucagon-like peptide 1 (GLP-1 [7–36 amide]), gastric inhibitory polypeptide (GIP) and insulin in response to oral glucose after upper and lower intestinal resections. Z Gastroenterol 34: 159 –166, 1996. 213. Nian M, Drucker DJ, Irwin D. Divergent regulation of human and rat proglucagon gene promoters in vivo. Am J Physiol Gastrointest Liver Physiol 277: G829 –G837, 1999. 214. Nian M, Gu J, Irwin DM, Drucker DJ. Human glucagon gene promoter sequences regulating tissue-specific versus nutrient-regulated gene expression. Am J Physiol Regul Integr Comp Physiol 282: R173–R183, 2002. 215. Nikolaidis LA, Elahi D, Hentosz T, Doverspike A, Huerbin R, Zourelias L, Stolarski C, Shen YT, Shannon RP. Recombinant glucagon-like peptide-1 increases myocardial glucose uptake and improves left ventricular performance in conscious dogs with pacing-induced dilated cardiomyopathy. Circulation 110: 955–961, 2004. 216. Nikolaidis LA, Elahi D, Shen YT, Shannon RP. Active metabolite of GLP-1 mediates myocardial glucose uptake and improves left ventricular performance in conscious dogs with dilated cardiomyopathy. Am J Physiol Heart Circ Physiol 289: H2401–H2408, 2005. 217. Nikolaidis LA, Mankad S, Sokos GG, Miske G, Shah A, Elahi D, Shannon RP. Effects of glucagon-like peptide-1 in patients with 87 • OCTOBER 2007 • www.prv.org 1436 218. 219. 220. 221. 222. 223. 224. 225. 226. 227. 228. 229. 230. 231. 232. 233. 234. 235. JENS JUUL HOLST acute myocardial infarction and left ventricular dysfunction after successful reperfusion. Circulation 109: 962–965, 2004. Nishizawa M, Moore MC, Shiota M, Gustavson SM, Snead WL, Neal DW, Cherrington AD. Effect of intraportal glucagon-like peptide-1 on glucose metabolism in conscious dogs. Am J Physiol Endocrinol Metab 284: E1027–E1036, 2003. Nishizawa M, Nakabayashi H, Kawai K, Ito T, Kawakami S, Nakagawa A, Niijima A, Uchida K. The hepatic vagal reception of intraportal GLP-1 is via receptor different from the pancreatic GLP-1 receptor. J Auton Nerv Syst 80: 14 –21, 2000. Nishizawa M, Nakabayashi H, Uchida K, Nakagawa A, Niijima A. The hepatic vagal nerve is receptive to incretin hormone glucagon-like peptide-1, but not to glucose-dependent insulinotropic polypeptide, in the portal vein. J Auton Nerv Syst 61: 149 –154, 1996. Novak U, Wilks A, Buell G, McEwen S. Identical mRNA for preproglucagon in pancreas and gut. Eur J Biochem 164: 553–558, 1987. Nyholm B, Walker M, Grauholt CH, Alberti KGMM, Holst JJ, Schmitz O. Twenty-four hour profiles of insulin, substrates and gut incretin hormones: early defects in glucose tolerant offspring of type II (non-insulin dependent) diabetic patients. Diabetologia 42: 1314 –1323, 1999. Oben J, Morgan L, Fletcher J, Marks V. Effect of the enteropancreatic hormones, gastric inhibitory polypeptide and glucagonlike polypeptide-1 (7–36) amide, on fatty acid synthesis in explants of rat adipose tissue. J Endocrinol 130: 267–272, 1991. Orci L, Bordi C, Unger RH, Perrelet A. Glucagon- and glicentinproducing cells. In: Glucagon, edited by Lefebvre PJ. Berlin: SpringerVerlag, 1983, p. 57–79. Orci L, Pictet R, Forssmann WG, Renold AE, Rouiller C. Structural evidence for glucagon producing cells in the intestinal mucosa of the rat. Diabetologia 4: 56 – 67, 1968. Orskov C, Bersani M, Johnsen AH, Hojrup P, Holst JJ. Complete sequences of glucagon-like peptide-1 from human and pig small intestine. J Biol Chem 264: 12826 –12829, 1989. Orskov C, Holst JJ, Knuhtsen S, Baldissera FG, Poulsen SS, Nielsen OV. Glucagon-like peptides GLP-1 and GLP-2, predicted products of the glucagon gene, are secreted separately from pig small intestine but not pancreas. Endocrinology 119: 1467–1475, 1986. Orskov C, Holst JJ, Nielsen OV. Effect of truncated glucagonlike peptide-1 [proglucagon- (78 –107) amide] on endocrine secretion from pig pancreas, antrum, and nonantral stomach. Endocrinology 123: 2009 –2013, 1988. Orskov C, Holst JJ, Poulsen SS, Kirkegaard P. Pancreatic and intestinal processing of proglucagon in man. Diabetologia 30: 874 – 881, 1987. Orskov C, Poulsen SS, Moller M, Holst JJ. Glucagon-like peptide I receptors in the subfornical organ and the area postrema are accessible to circulating glucagon-like peptide I. Diabetes 45: 832– 835, 1996. Orskov C, Rabenhoj L, Wettergren A, Kofod H, Holst JJ. Tissue and plasma concentrations of amidated and glycine-extended glucagon-like peptide I in humans. Diabetes 43: 535–539, 1994. Orskov C, Wettergren A, Holst JJ. Biological effects and metabolic rates of glucagonlike peptide-1 7–36 amide and glucagonlike peptide-1 7–37 in healthy subjects are indistinguishable. Diabetes 42: 658 – 661, 1993. Orskov C, Wettergren A, Holst JJ. Secretion of the incretin hormones glucagon-like peptide-1 and gastric inhibitory polypeptide correlates with insulin secretion in normal man throughout the day. Scand J Gastroenterol 31: 665– 670, 1996. Orskov L, Holst JJ, Moller J, Orskov C, Moller N, Alberti KG, Schmitz O. GLP-1 does not acutely affect insulin sensitivity in healthy man. Diabetologia 39: 1227–1232, 1996. Patti ME, McMahon G, Mun EC, Bitton A, Holst JJ, Goldsmith J, Hanto DW, Callery M, Arky R, Nose V, Bonner-Weir S, Goldfine AB. Severe hypoglycaemia post-gastric bypass requiring partial pancreatectomy: evidence for inappropriate insulin secretion and pancreatic islet hyperplasia. Diabetologia 48: 2236 – 2240, 2005. Physiol Rev • VOL 236. Patzelt C, Schug G. The major proglucagon fragment: an abundant islet protein and secretory product. FEBS Lett 129: 127–130, 1981. 237. Perley M, Kipnis DM. Plasma insulin responses to oral and intravenous glucose: studies in normal and diabetic subjects. J Clin Invest 46: 1954 –1962, 1967. 238. Perry T, Haughey NJ, Mattson MP, Egan JM, Greig NH. Protection and reversal of excitotoxic neuronal damage by glucagonlike peptide-1 and exendin-4. J Pharmacol Exp Ther 302: 881– 888, 2002. 239. Perry TA, Greig NH. A new Alzheimer’s disease interventive strategy: GLP-1. Curr Drug Targets 5: 565–571, 2004. 240. Petersen B, Christiansen J, Holst JJ. A glucose-dependent mechanism in jejunum inhibits gastric acid secretion: a response mediated through enteroglucagon? Scand J Gastroenterol 20: 193– 197, 1985. 241. Plaisancie P, Bernard C, Chayvialle JA, Cuber JC. Regulation of glucagon-like peptide-1- (7–36) amide secretion by intestinal neurotransmitters and hormones in the isolated vascularly perfused rat colon. Endocrinology 135: 2398 –2403, 1994. 242. Plamboeck A, Holst JJ, Carr RD, Deacon CF. Neutral endopeptidase 24.11 and dipeptidyl peptidase IV are both mediators of the degradation of glucagon-like peptide 1 in the anaesthetised pig. Diabetologia 48: 1882–1890, 2005. 243. Preitner F, Ibberson M, Franklin I, Binnert C, Pende M, Gjinovci A, Hansotia T, Drucker DJ, Wollheim C, Burcelin R, Thorens B. Gluco-incretins control insulin secretion at multiple levels as revealed in mice lacking GLP-1 and GIP receptors. J Clin Invest 113: 635– 645, 2004. 244. Qualmann C, Nauck MA, Holst JJ, Orskov C, Creutzfeldt W. Glucagon-like peptide 1 (7–36 amide) secretion in response to luminal sucrose from the upper and lower gut. A study using alpha-glucosidase inhibition (acarbose). Scand J Gastroenterol 30: 892– 896, 1995. 245. Rachman J, Barrow BA, Levy JC, Turner RC. Near-normalisation of diurnal glucose concentrations by continuous administration of glucagon-like peptide-1 (GLP-1) in subjects with NIDDM. Diabetologia 40: 205–211, 1997. 246. Ranganath L, Norris F, Morgan L, Wright J, Marks V. Inhibition of carbohydrate-mediated glucagon-like peptide-1 (7–36)amide secretion by circulating non-esterified fatty acids. Clin Sci 96: 335– 342, 1999. 247. Ranganath LR, Beety JM, Morgan LM, Wright JW, Howland R, Marks V. Attenuated GLP-1 secretion in obesity: cause or consequence? Gut 38: 916 –919, 1996. 248. Rask E, Olsson T, Soderberg S, Johnson O, Seckl J, Holst JJ, Ahren B. Impaired incretin response after a mixed meal is associated with insulin resistance in nondiabetic men. Diabetes Care 24: 1640 –1645, 2001. 249. Read N, French S, Cunningham K. The role of the gut in regulation food intake in man. Nutr Rev 52: 1–10, 1994. 250. Redondo A, Trigo MV, Acitores A, Valverde I, VillanuevaPenacarrillo ML. Cell signalling of the GLP-1 action in rat liver. Mol Cell Endocrinol 204: 43–50, 2003. 251. Reimer RA, Darimont C, Gremlich S, Nicolas-Metral V, Ruegg UT, Mace K. A human cellular model for studying the regulation of glucagon-like peptide-1 secretion. Endocrinology 142: 4522– 4528, 2001. 252. Richter G, Feddersen O, Wagner U, Barth P, Goke R, Goke B. GLP-1 stimulates secretion of macromolecules from airways and relaxes pulmonary artery. Am J Physiol Lung Cell Mol Physiol 265: L374 –L381, 1993. 253. Rinaman L. Interoceptive stress activates glucagon-like peptide-1 neurons that project to the hypothalamus. Am J Physiol Regul Integr Comp Physiol 277: R582–R590, 1999. 254. Rocca AS, Brubaker PL. Role of the vagus nerve in mediating proximal nutrient-induced glucagon-like peptide-1 secretion. Endocrinology 140: 1687–1694, 1999. 255. Rouille Y, Kantengwa S, Irminger JC, Halban PA. Role of the prohormone convertase PC3 in the processing of proglucagon to glucagon-like peptide 1. J Biol Chem 272: 32810 –32816, 1997. 87 • OCTOBER 2007 • www.prv.org THE PHYSIOLOGY OF GLUCAGON-LIKE PEPTIDE 1 256. Rouille Y, Westermark G, Martin SK, Steiner DF. Proglucagon is processed to glucagon by prohormone convertase PC2 in alpha TC1– 6 cells. Proc Natl Acad Sci USA 91: 3242–3246, 1994. 257. Sandhu H, Wiesenthal SR, MacDonald PE, McCall RH, Tchipashvili V, Rashid S, Satkunarajah M, Irwin DM, Shi ZQ, Brubaker PL, Wheeler MB, Vranic M, Efendic S, Giacca A. Glucagon-like peptide 1 increases insulin sensitivity in depancreatized dogs. Diabetes 48: 1045–1053, 1999. 258. Schepp W, Schmidtler J, Riedel T, Dehne K, Schusdziarra V, Holst JJ, Eng J, Raufman JP, Classen M. Exendin-4 and exendin- (9 –39)NH2: agonist and antagonist, respectively, at the rat parietal cell receptor for glucagon-like peptide-1- (7–36)NH2. Eur J Pharmacol 269: 183–191, 1994. 259. Schick RR, vorm Walde T, Zimmermann JP, Schusdziarra V, Classen M. Glucagon-like peptide 1: a novel brain peptide involved in feeding regulation. In: Obesity in Europe 1993, edited by Ditschuneit H, Gries FA, Hauner H, Schusdziarra V, Wechsler JG. Libbey, 1994, p. 363–367. 260. Schirra J, Nicolaus M, Roggel R, Katschinski M, Storr M, Woerle HJ, Goke B. Endogenous glucagon-like peptide 1 controls endocrine pancreatic secretion and antro-pyloro-duodenal motility in humans. Gut 55: 243–251, 2006. 261. Schjoldager BT, Mortensen PE, Christiansen J, Orskov C, Holst JJ. GLP-1 (glucagon-like peptide 1) and truncated GLP-1, fragments of human proglucagon, inhibit gastric acid secretion in humans. Dig Dis Sci 34: 703–708, 1989. 262. Schmidtler J, Dehne K, Allescher HD, Schusdziarra V, Classen M, Holst JJ, Polack A, Schepp W. Rat parietal cell receptors for GLP-1- (7–36) amide: northern blot, cross-linking, radioligand binding. Am J Physiol Gastrointest Liver Physiol 267: G423–G432, 1994. 263. Scrocchi LA, Brown TJ, MaClusky N, Brubaker PL, Auerbach AB, Joyner AL, Drucker DJ. Glucose intolerance but normal satiety in mice with a null mutation in the glucagon-like peptide 1 receptor gene. Nat Med 2: 1254 –1258, 1996. 264. Service GJ, Thompson GB, Service FJ, Andrews JC, CollazoClavell ML, Lloyd RV. Hyperinsulinemic hypoglycemia with nesidioblastosis after gastric-bypass surgery. N Engl J Med 353: 249 – 254, 2005. 265. Shah P, Vella A, Basu A, Basu R, Schwenk WF, Rizza RA. Lack of suppression of glucagon contributes to postprandial hyperglycemia in subjects with type 2 diabetes mellitus. J Clin Endocrinol Metab 85: 4053– 4059, 2000. 266. Simonsen L, Holst JJ, Deacon CF. Exendin-4, but not glucagonlike peptide-1, is cleared exclusively by glomerular filtration in anaesthetised pigs. Diabetologia 1–7, 2006. 267. Sinclair EM,Drucker DJ. Proglucagon-derived peptides: mechanisms of action and therapeutic potential. Physiology 20: 357–365, 2005. 268. Skoglund G, Hussain MA, Holz GG. Glucagon-like peptide 1 stimulates insulin gene promoter activity by protein kinase A-independent activation of the rat insulin I gene cAMP response element. Diabetes 49: 1156 –1164, 2000. 269. Sokos GG, Nikolaidis LA, Mankad S, Elahi D, Shannon RP. Glucagon-like peptide-1 infusion improves left ventricular ejection fraction and functional status in patients with chronic heart failure. J Card Fail 12: 694 – 699, 2006. 270. Stoffers DA, Desai BM, DeLeon DD, Simmons RA. Neonatal exendin-4 prevents the development of diabetes in the intrauterine growth retarded rat. Diabetes 52: 734 –740, 2003. 271. Stoffers DA, Kieffer TJ, Hussain MA, Drucker DJ, BonnerWeir S, Habener JF, Egan JM. Insulinotropic glucagon-like peptide 1 agonists stimulate expression of homeodomain protein IDX-1 and increase islet size in mouse pancreas. Diabetes 49: 741–748, 2000. 272. Sturis J, Gotfredsen CF, Romer J, Rolin B, Ribel U, Brand CL, Wilken M, Wassermann K, Deacon CF, Carr RD, Knudsen LB. GLP-1 derivative liraglutide in rats with beta-cell deficiencies: influence of metabolic state on beta-cell mass dynamics. Br J Pharmacol 140: 123–132, 2003. 273. Sugiyama K, Manaka H, Kato T, Yamatani K, Tominaga M, Sasaki H. Stimulation of truncated glucagon-like peptide-1 release Physiol Rev • VOL 274. 275. 276. 277. 278. 279. 280. 281. 282. 283. 284. 285. 286. 287. 288. 289. 290. 291. 292. 293. 1437 from the isolated perfused canine ileum by glucose absorption. Digestion 55: 24 –28, 1994. Sundby F, Jacobsen H, Moody AJ. Purification and characterization of a protein from porcine gut with glucagon-like immunoreactivity. Horm Metab Res 8: 366 –371, 1976. Sundler F, Alumets J, Holst J, Larsson LI, Hakanson R. Ultrastructural identification of cells storing pancreatic-type glucagon in dog stomach. Histochemistry 50: 33–37, 1976. Sutherland EW, De Duve C. Origin and distribution of the hyperglycemic-glycogenolytic factor of the pancreas. J Biol Chem 175: 663– 674, 1948. Tager H, Hohenboken M, Markese J, Dinerstein RJ. Identification and localization of glucagon-related peptides in rat brain. Proc Natl Acad Sci USA 77: 6229 – 6233, 1980. Tang-Christensen M, Larsen PJ, Goke R, Fink-Jensen A, Jessop DS, Moller M, Sheikh SP. Central administration of GLP-1(7–36) amide inhibits food and water intake in rats. Am J Physiol Regul Integr Comp Physiol 271: R848 –R856, 1996. Tang-Christensen M, Larsen PJ, Thulesen J, Romer J, Vrang N. The proglucagon-derived peptide, glucagon-like peptide-2, is a neurotransmitter involved in the regulation of food intake. Nat Med 6: 802– 807, 2000. Tang-Christensen M, Vrang N, Larsen PJ. Glucagon-like peptide 1 (7–36) amide’s central inhibition of feeding and peripheral inhibition of drinking are abolished by neonatal monosodium glutamate treatment. Diabetes 47: 530 –537, 1998. Thim L, Moody AJ. The amino acid sequence of porcine glicentin. Peptides 2 Suppl 2: 37–39, 1981. Thim L, Moody AJ. Purification and chemical characterization of a glicentin-related pancreatic peptide (proglucagon fragment) from porcine pancreas. Biochim Biophys Acta 703: 134 –141, 1982. Thorens B. Expression cloning of the pancreatic beta cell receptor for the gluco-incretin hormone glucagon-like peptide 1. Proc Natl Acad Sci USA 89: 8641– 8645, 1992. Thorens B, Porret A, Buhler L, Deng SP, Morel P, Widmann C. Cloning and functional expression of the human islet GLP-1 receptor. Demonstration that exendin-4 is an agonist and exendin- (9 – 39) an antagonist of the receptor. Diabetes 42: 1678 –1682, 1993. Thorens B, Widmann C. Signal transduction and desensitization of the glucagon-like peptide-1 receptor. Acta Physiol Scand 157: 317–319, 1996. Toft-Nielsen M, Madsbad S, Holst JJ. Exaggerated secretion of glucagon-like peptide-1 (GLP-1) could cause reactive hypoglycaemia. Diabetologia 41: 1180 –1186, 1998. Toft-Nielsen M, Madsbad S, Holst JJ. The effect of glucagonlike peptide I (GLP-I) on glucose elimination in healthy subjects depends on the pancreatic glucoregulatory hormones. Diabetes 45: 552–556, 1996. Toft-Nielsen MB, Damholt MB, Madsbad S, Hilsted LM, Hughes TE, Michelsen BK, Holst JJ. Determinants of the impaired secretion of glucagon-like peptide-1 in type 2 diabetic patients. J Clin Endocrinol Metab 86: 3717–3723, 2001. Toft-Nielsen MB, Madsbad S, Holst JJ. Determinants of the effectiveness of glucagon-like peptide-1 in type 2 diabetes. J Clin Endocrinol Metab 86: 3853–3860, 2001. Tourrel C, Bailbe D, Lacorne M, Meile MJ, Kergoat M, Portha B. Persistent improvement of type 2 diabetes in the Goto-Kakizaki rat model by expansion of the beta-cell mass during the prediabetic period with glucagon-like peptide-1 or exendin-4. Diabetes 51: 1443–1452, 2002. Trapote MA, Clemente F, Galera C, Morales M, Alcantara AI, Lopez Delgado MI, Villanueva Penacarrillo ML, Valverde I. Inositolphosphoglycans are possible mediators of the glucagon-like peptide 1 (7–36)amide action in the liver. J Endocrinol Invest 19: 114 –118, 1996. Trinh DK, Zhang K, Hossain M, Brubaker PL, Drucker DJ. Pax-6 activates endogenous proglucagon gene expression in the rodent gastrointestinal epithelium. Diabetes 52: 425– 433, 2003. Tsuboi T, da Silva X, Holz GG, Jouaville LS, Thomas AP, Rutter GA. Glucagon-like peptide-1 mobilizes intracellular Ca2⫹ and stimulates mitochondrial ATP synthesis in pancreatic MIN6 beta-cells. Biochem J 369: 287–299, 2003. 87 • OCTOBER 2007 • www.prv.org 1438 JENS JUUL HOLST 294. Turton MD, O’Shea D, Gunn I, Beak SA, Edwards CM, Meeran K, Choi SJ, Taylor GM, Heath MM, Lambert PD, Wilding JP, Smith DM, Ghatei MA, Herbert J, Bloom SR. A role for glucagon-like peptide-1 in the central regulation of feeding. Nature 379: 69 –72, 1996. 295. Ugleholdt R, Zhu X, Deacon CF, Orskov C, Steiner DF, Holst JJ. Impaired intestinal proglucagon processing in mice lacking prohormone convertase 1. Endocrinology 145: 1349 –1355, 2004. 296. Unger RH, Eisentraut AM, McCall RH, Madison LL. Glucagon antibodies and an immunoassay for glucagon. J Clin Invest 40: 1280 –1289, 1961. 297. Unger RH, Ketterer H, Eisentraut AM. Distribution of immunoassayable glucagon in gastrointestinal tissues. Metabolism 15: 865– 867, 1966. 298. Unger RH, Ohneda A, Valverde I, Eisentraut AM, Exton J. Characterization of the responses of circulating glucagon-like immunoreactivity to intraduodenal and intravenous administration of glucose. J Clin Invest 47: 48 – 65, 1968. 299. Vaag AA, Holst JJ, Volund A, Beck-Nielsen HB. Gut incretin hormones in identical twins discordant for non-insulin-dependent diabetes mellitus (NIDDM)– evidence for decreased glucagon-like peptide 1 secretion during oral glucose ingestion in NIDDM twins. Eur J Endocrinol 135: 425– 432, 1996. 300. Valverde I, Merida E, Delgado E, Trapote MA, Villanueva Penacarrillo ML. Presence and characterization of glucagon-like peptide-1 (7–36) amide receptors in solubilized membranes of rat adipose tissue. Endocrinology 132: 75–79, 1993. 301. Valverde I, Rigopoulou D, Exton J, Ohneda A, Eisentraut A, Unger RH. Demonstration and characterization of a second fraction of glucagon-like immunoreactivity in jejunal extracts. Am J Med Sci 255: 415– 420, 1968. 302. Varndell IM, Bishop AE, Sikri KL, Uttenthal LO, Bloom SR, Polak JM. Localization of glucagon-like peptide (GLP) immunoreactants in human gut and pancreas using light and electron microscopic immunocytochemistry. J Histochem Cytochem 33: 1080 – 1086, 1985. 303. Vella A, Shah P, Basu R, Basu A, Holst JJ, Rizza RA. Effect of glucagon-like peptide 1 (7–36) amide on glucose effectiveness and insulin action in people with type 2 diabetes. Diabetes 49: 611– 617, 2000. 304. Vella A, Shah P, Reed AS, Adkins AS, Basu R, Rizza RA. Lack of effect of exendin-4 and glucagon-like peptide-1- (7, 36)-amide on insulin action in non-diabetic humans. Diabetologia 45: 1410 –1415, 2002. 305. Verdich C, Flint A, Gutzwiller JP, Naslund E, Beglinger C, Hellstrom PM, Long SJ, Morgan LM, Holst JJ, Astrup A. A meta-analysis of the effect of glucagon-like peptide-1 (7–36) amide on ad libitum energy intake in humans. J Clin Endocrinol Metab 86: 4382– 4389, 2001. 306. Verdich C, Toubro S, Buemann B, Lysgard MJ, Juul HJ, Astrup A. The role of postprandial releases of insulin and incretin hormones in meal-induced satiety-effect of obesity and weight reduction. Int J Obes Relat Metab Disord 25: 1206 –1214, 2001. 307. Vila Petroff MG, Egan JM, Wang X, Sollott SJ. Glucagon-like peptide-1 increases cAMP but fails to augment contraction in adult rat cardiac myocytes. Circ Res 89: 445– 452, 2001. 308. Villanueva-Penacarrillo ML, Delgado E, Trapote MA, Alcantara A, Clemente F, Luque MA, Perea A, Valverde I. Glucagonlike peptide-1 binding to rat hepatic membranes. J Endocrinol 146: 183–189, 1995. 309. Vilsboll T, Agerso H, Krarup T, Holst JJ. Similar elimination rates of glucagon-like peptide-1 in obese type 2 diabetic patients and healthy subjects. J Clin Endocrinol Metab 88: 220 –224, 2003. 310. Vilsboll T, Holst JJ. Incretins, insulin secretion and Type 2 diabetes mellitus. Diabetologia 47: 357–366, 2004. 311. Vilsboll T, Knop FK, Krarup T, Johansen A, Madsbad S, Larsen S, Hansen T, Pedersen O, Holst JJ. The pathophysiology of diabetes involves a defective amplification of the late-phase insulin response to glucose by glucose-dependent insulinotropic polypeptide-regardless of etiology and phenotype. J Clin Endocrinol Metab 88: 4897– 4903, 2003. 312. Vilsboll T, Krarup T, Deacon CF, Madsbad S, Holst JJ. Reduced postprandial concentrations of intact biologically active gluPhysiol Rev • VOL 314. 315. 317. 318. 319. 320. 321. 322. 323. 324. 325. 326. 327. 328. 329. 330. 331. 332. cagon-like peptide 1 in type 2 diabetic patients. Diabetes 50: 609 – 613, 2001. Vilsboll T, Krarup T, Madsbad S, Holst JJ. Defective amplification of the late phase insulin response to glucose by GIP in obese Type II diabetic patients. Diabetologia 45: 1111–1119, 2002. Vilsboll T, Krarup T, Madsbad S, Holst JJ. Both GLP-1 and GIP are insulinotropic at basal and postprandial glucose levels and contribute nearly equally to the incretin effect of a meal in healthy subjects. Regul Pept 114: 115–121, 2003. Vilsboll T, Krarup T, Sonne J, Madsbad S, Volund A, Juul AG, Holst JJ. Incretin secretion in relation to meal size and body weight in healthy subjects and people with type 1 and type 2 diabetes mellitus. J Clin Endocrinol Metab 88: 2706 –2713, 2003. Vilsboll T, Zdravkovic M, Le-Thi T, Krarup T, Schmitz O, Courreges J, Verhoven Buganova IR, Madsbad S. Liraglutide significantly improves glycemic control, lowers body weight without risk of either major or minor hypoglycemic episodes in subjects with type 2 diabetes (Abstract). Diabetes 55: A27–A28, 2006. Vrang N, Phifer CB, Corkern MM, Berthoud HR. Gastric distension induces c-Fos in medullary GLP-1/2-containing neurons. Am J Physiol Regul Integr Comp Physiol 285: R470 –R478, 2003. Wang Q, Brubaker PL. Glucagon-like peptide-1 treatment delays the onset of diabetes in 8-week-old db/db mice. Diabetologia 45: 1263–1273, 2002. Wang Y, Kole HK, Montrose-Rafizadeh C, Perfetti R, Bernier M, Egan JM. Regulation of glucose transporters and hexose uptake in 3T3-L1 adipocytes: glucagon-like peptide-1 and insulin interactions. J Mol Endocrinol 19: 241–248, 1997. Wei Y, Mojsov S. Tissue-specific expression of the human receptor for glucagon-like peptide-I: brain, heart and pancreatic forms have the same deduced amino acid sequences. FEBS Lett 358: 219 –224, 1995. Wei Y, Mojsov S. Distribution of GLP-1 and PACAP receptors in human tissues. Acta Physiol Scand 157: 355–357, 1996. Wettergren A, Maina P, Boesby S, Holst JJ. Glucagon-like peptide-1 7–36 amide and peptide YY have additive inhibitory effect on gastric acid secretion in man. Scand J Gastroenterol 32: 552– 555, 1997. Wettergren A, Petersen H, Orskov C, Christiansen J, Sheikh SP, Holst JJ. Glucagon-like peptide-1 7–36 amide and peptide YY from the L-cell of the ileal mucosa are potent inhibitors of vagally induced gastric acid secretion in man. Scand J Gastroenterol 29: 501–505, 1994. Wettergren A, Pridal L, Wojdemann M, Holst JJ. Amidated and non-amidated glucagon-like peptide-1 (GLP-1): non-pancreatic effects (cephalic phase acid secretion) and stability in plasma in humans. Regul Pept 77: 83– 87, 1998. Wettergren A, Schjoldager B, Mortensen PE, Myhre J, Christiansen J, Holst JJ. Truncated GLP-1 (proglucagon 78 –107amide) inhibits gastric and pancreatic functions in man. Dig Dis Sci 38: 665– 673, 1993. Wettergren A, Wojdemann M, Holst JJ. Glucagon-like peptide-1 inhibits gastropancreatic function by inhibiting central parasympathetic outflow. Am J Physiol Gastrointest Liver Physiol 275: G984 –G992, 1998. Wettergren A, Wojdemann M, Meisner S, Stadil F, Holst JJ. The inhibitory effect of glucagon-like peptide-1 (GLP-1) 7–36 amide on gastric acid secretion in humans depends on an intact vagal innervation. Gut 40: 597– 601, 1997. Wheeler MB, Gelling RW, McIntosh CH, Georgiou J, Brown JC, Pederson RA. Functional expression of the rat pancreatic islet glucose-dependent insulinotropic polypeptide receptor: ligand binding and intracellular signaling properties. Endocrinology 136: 4629 – 4639, 1995. Wideman RD, Yu IL, Webber TD, Verchere CB, Johnson JD, Cheung AT, Kieffer TJ. Improving function and survival of pancreatic islets by endogenous production of glucagon-like peptide 1 (GLP-1). Proc Natl Acad Sci USA 103: 13468 –13473, 2006. Willms B, Werner J, Holst JJ, Orskov C, Creutzfeldt W, Nauck MA. Gastric emptying, glucose responses, and insulin secretion after a liquid test meal: effects of exogenous glucagon-like peptide-1 (GLP-1)- (7–36) amide in type 2 (noninsulin-dependent) diabetic patients. J Clin Endocrinol Metab 81: 327–332, 1996. 87 • OCTOBER 2007 • www.prv.org THE PHYSIOLOGY OF GLUCAGON-LIKE PEPTIDE 1 333. Xu G, Stoffers DA, Habener JF, Bonner-Weir S. Exendin-4 stimulates both beta-cell replication and neogenesis, resulting in increased beta-cell mass and improved glucose tolerance in diabetic rats. Diabetes 48: 2270 –2276, 1999. 334. Yamamoto H, Kishi T, Lee CE, Choi BJ, Fang H, Hollenberg AN, Drucker DJ, Elmquist JK. Glucagon-like peptide-1-responsive catecholamine neurons in the area postrema link peripheral glucagon-like peptide-1 with central autonomic control sites. J Neurosci 23: 2939 –2946, 2003. 335. Yamamoto H, Lee CE, Marcus JN, Williams TD, Overton JM, Lopez ME, Hollenberg AN, Baggio L, Saper CB, Drucker DJ, Elmquist JK. Glucagon-like peptide-1 receptor stimulation increases blood pressure and heart rate and activates autonomic regulatory neurons. J Clin Invest 110: 43–52, 2002. 336. Yang H, Egan JM, Wang Y, Moyes CD, Roth J, Montrose MH, Montrose-Rafizadeh C. GLP-1 action in L6 myotubes is via a receptor different from the pancreatic GLP-1 receptor. Am J Physiol Cell Physiol 275: C675–C683, 1998. 337. Yang Z, Chen M, Carter JD, Nunemaker CS, Garmey JC, Kimble SD, Nadler JL. Combined treatment with lisofylline and exendin-4 reverses autoimmune diabetes. Biochem Biophys Res Commun 344: 1017–1022, 2006. 338. Yi F, Brubaker PL, Jin T. TCF-4 mediates cell type-specific regulation of proglucagon gene expression by beta-catenin and glycogen synthase kinase-3. J Biol Chem 280: 1457–1464, 2005. Physiol Rev • VOL 1439 339. Zander M, Madsbad S, Deacon CF, Holst JJ. The metabolite generated by dipeptidyl-peptidase 4 metabolism of glucagon-like peptide-1 has no influence on plasma glucose levels in patients with type 2 diabetes. Diabetologia 49: 369 –374, 2006. 340. Zander M, Madsbad S, Madsen JL, Holst JJ. Effect of 6-week course of glucagon-like peptide 1 on glycaemic control, insulin sensitivity, and beta-cell function in type 2 diabetes: a parallelgroup study. Lancet 359: 824 – 830, 2002. 341. Zarich SW. The role of intensive glycemic control in the management of patients who have acute myocardial infarction. Cardiol Clin 23: 109 –117, 2005. 342. Zhao T, Parikh P, Bhashyam S, Bolukoglu H, Poornima I, Shen YT, Shannon RP. Direct effects of glucagon-like peptide-1 on myocardial contractility and glucose uptake in normal and postischemic isolated rat hearts. J Pharmacol Exp Ther 317: 1106 – 1113, 2006. 343. Zhou J, Wang X, Pineyro MA, Egan JM. Glucagon-like peptide 1 and exendin-4 convert pancreatic AR42J cells into glucagon- and insulin-producing cells. Diabetes 48: 2358 –2366, 1999. 344. Zhu X, Zhou A, Dey A, Norrbom C, Carroll R, Zhang C, Laurent V, Lindberg I, Ugleholdt R, Holst JJ, Steiner DF. Disruption of PC1/3 expression in mice causes dwarfism and multiple neuroendocrine peptide processing defects. Proc Natl Acad Sci USA 99: 10293–10298, 2002. 87 • OCTOBER 2007 • www.prv.org
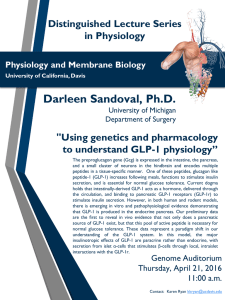
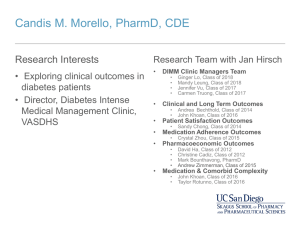
![Anti-GLP1 antibody [1B7B4] ab36598 Product datasheet 2 Images Overview](http://s2.studylib.net/store/data/011965712_1-746457d50999eb2b6a5b0653f270ecad-300x300.png)