Wednesday Case of the Day Physics
advertisement

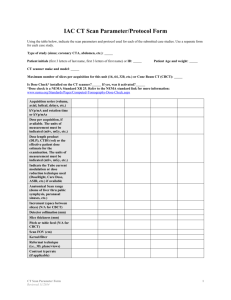
Wednesday Case of the Day Physics Authors: Michael F. McNitt-Gray, PhD,1 Erin Angel, MS,1 Mitchell M. Goodsitt, PhD,2 Clinton V. Wellnitz, MD3 1Department of Radiological Sciences, David Geffen School of Medicine at UCLA, Los Angeles, CA. 2Department of Radiology, University of Michigan, Ann Arbor. 3Mayo Clinic, Scottsdale, AZ. History: 32-year-old female (approximately standard-sized female) undergoes CT scan of abdomen and pelvis after motor vehicle accident. Later she discovers she was 7 weeks pregnant at time of scan. CT scan info: GE LightSpeed 16 scanner. 120 kVp; fixed tube current, 400 mA; 0.5-sec rotation time; pitch, 0.9875; 16 x 1.25-mm collimation; 5-mm reconstructed slice thickness; standard reconstruction filter. CTDI100 (mGy/100 mAs) in 16-cm-diameter phantom: center = 16.0; peripheral = 17.2. Scan ranged from top of liver through to pubic symphysis. Estimate the radiation dose received by the fetus: a) 0.5–1 mGy. b) 10–15 mGy. c) 15–30 mGy. d) 30–50 mGy. e) 100–150 mGy. Gestational Sac Uterus Figure 1. Axial and sagittal views of gestational sac and uterus from patient who is 7 weeks pregnant at time of CT. Correct Answer (c) 15–30 mGy. Next several slides will go through three different methods of estimating radiation dose to fetus for this case: 1. 2. 3. Felmlee, Gray, et al method [AJR 1990 Jan;154(1):185–90] Using ImPACT dose spreadsheet method (www.impactscan.org) Monte Carlo simulation method with pregnant patient model (E. Angel, et al, RSNA 2006) Final slides will discuss implications of this level of radiation dose on fetus and recommendations. Fetal Radiation Dose: Clinical Context Most often this calculation is requested in the context of a woman who didn’t know she was pregnant when she underwent a CT scan; sometimes this is requested ahead of time when the CT is scheduled for a woman who is known to be pregnant. Fetal Radiation Dose: Scan Protocol and Information In the scenario presented, the following details were provided: 1. 2. 3. 4. 5. 6. 7. GE LightSpeed 16 (16–detector row) CT scanner. 120 kVp. 400 mA. 0.5-second rotation time. Helical scan with pitch = 0.9875. 16 x 1.25-mm collimation (20-mm nominal beam width). CTDI100 in 16-cm-diameter phantom of 16.0 mGy/100 mAs at center and 17.2 mGy/100 mAs at a peripheral (12:00) position under the above conditions. 8. Because scan ranged from top of liver through to pubic symphysis, the fetus was definitely in the x-ray beam. 9. The woman was standard female size—approximately 58 kg; 160 cm (128 lb; 5’3”). 10. The gestational age at the time of scan was later determined to be approximately 7 weeks. 11. No mention of additional risk factors to mother or fetus. Felmlee, Gray, et al Method This paper [AJR 1990 Jan;154(1):185–90] first describes the normalized fetaldose ratio (NFDR): – Defined as the measured fetal-dose contribution from a single CT scan divided by the CTDI measured (16-cm-diameter phantom) with the same scanning parameters. – Determined at various distances from the fetus. Felmlee, Gray, et al Method Then the paper describes an integrated normalized fetal-dose ratio (INFDR): – Defined as the sum of individual NFDR(d) located from 0 cm to an offset distance, assuming 1-cm scans at 1-cm incrementation. – Determined at various distances from the fetus. Felmlee, Gray, et al Method For example: • At z = 0 cm offset (ie, directly over fetus), – INFDR(0) = 0.255. • At z = 10 cm offset (say, 10 cm inferior), – INFDR(10) = 0.453. • At z = 40 cm offset (say, 40 cm superior), – INFDR(40) = 0.481. Scan begins 40 cm superior to location of fetus. Z-axis location of fetus Scan ends 10 cm inferior to location of fetus. Felmlee, Gray, et al Method Fetal dose (mGy) = CTDI * INFDRE where: CTDI = center value from 16-cm phantom. INFDRE = INFDR0 + INFDRInf + INFDRSup. – – – – – – – INFDR0 = NFDR (from Table 3 of Felmlee) at 0 offset. INFDRInf = INFDR for scan locations inferior to fetal location. INFDRSup = INFDR for scan locations superior to fetal location. INFDRSup or Inf = (T/I) [INFDR(M) – INFDR(N–1)] T = nominal beam width (in mm). I = table increment per rotation (also in mm). INFDR(M) = INFDR at the maximum offset distance M (cm) from fetal location. – INFDR(N–1) = INFDR at the minimum offset distance N (cm) minus 1 cm from the fetal location. Felmlee, Gray, et al Method Under the conditions specified: 1. 2. 3. 4. CTDI at center position of 16-cm phantom is 32 mGy. – CTDI at center position of 16-cm phantom was 16.0 mGy/100 mAs. – 200 mAs. Superior location is approximately 40 cm superior to fetus. Inferior location is approximately 10 cm inferior to fetus. Pitch = 0.9875 = T/I, T = 20 mm, so I = 19.75 mm. Therefore, INFDRE = INFDR0 + INFDRInf + INFDRSup = 0.255 + (20/19.75)*(0.453 − 0.255) + (20/19.75)*(0.481 − 0.255) = 0.255 + 0.201 + 0.229 = 0.685 Fetal Dose = CTDI * INFDRE = 32 mGy * 0.685 = 21.9 mGy ImPACT Spreadsheet Method Results are based on Monte Carlo simulations performed by National Radiological Protection Board (NRPB) as described in NRPB report 250. – Original work done in 1991. Modern scanners are “matched” to original scanners based on CTDI values measured in air and in phantom. Helical scans modeled using pitch values: – (Jones DG, Shrimpton PC. Survey of CT practice in the UK: Part 3. Normalized organ doses calculated using Monte Carlo techniques. National Radiological Protection Board, NRPBR250, 1991). (table travel per rotation)/(total nominal beam collimation). MIRD patient model: – – Hermaphrodite standard man representation. Geometrically shaped organs, including uterus. ImPACT Spreadsheet Method To obtain an estimate of fetal dose: 1. Choose scanner manufacturer and model. o 2. Choose scanner parameters. o o 3. 4. Matched to a scanner make and model from original simulations. kVp, body region (which selects the bowtie filter), mAs, beam collimation, pitch. Choose start/end location of scan on patient model. Provides an estimate of dose to all ICRP 60 organs, including uterus. For early gestational age, estimate to uterus is approximately equal to fetal dose. See www.impactscan.org for more details on this method. ImPACT Spreadsheet Method 90 80 70 60 50 40 Start location 30 20 10 0 -10 Uterus End location ImPACT Spreadsheet Method Uterus Dose in mGy Monte Carlo Simulation Method (Angel et al, RSNA 2006) Monte Carlo simulations based on: – Detailed description of scanner. – Detailed description of pregnant patient. – Simulate arbitrary scan protocol. Monte Carlo Simulation Method (Angel et al, RSNA 2006) Monte Carlo model: – – – – MCNPX software from Los Alamos National Lab. Uses a detailed voxelized model of pregnant patient (next slide). Description of scanner geometry (fan angle, SID, etc). Simulates photon transport from modified x-ray source through patient model. Modified CT x-ray source: – – Source model previously published in: • Jarry, et al. Phys Med Biol 2003;48(16):2645–63. • DeMarco, et al. Phys Med Biol 2005;50(17):3989–4004. Detailed descriptions of source: • X-ray spectra (from manufacturer). • Beam filtration including the bowtie filter (from manufacturer). • Beam collimation in the longitudinal (z) direction. • Source movement for helical scan of arbitrary pitch. Agreement between simulation and measurement shown to be within 3.5% in phantom (Jarry et al and DeMarco et al). Monte Carlo Simulation Method: Creating a Voxelized Model Using CT image data from patients who were scanned for clinical indications (such as motor vehicle accident), create voxelized models for simulation. Radiologist contoured uterus and gestational sac (when visible). Original Image Contoured Image Voxelized Model Monte Carlo Simulation Method: Modeling the CT Source Modeled GE LightSpeed 16 120 kVp, body bowtie filter 4 x 5-mm nominal beam collimation Dose reported on a per-100-mAs basis Monte Carlo Simulation Method: Modeling the Scan Abdomen/pelvis scan: Just above liver to below pubic symphysis Helical scan, pitch = 1 (for reference) Can be adjusted for pitch = 0.9875 Only one series Monte Carlo Simulation Method: Results In our inventory of cases, we had two patients who were 7 weeks pregnant: Patient 1 was 134 pounds (no info on height, but perimeter was approximately 95 cm at level of fetus). Patient 2 was 137 pounds (no info on height, but perimeter was approximately 86 cm at level of fetus). Estimated fetal doses for 200-mAs 0.9875-pitch scan: – Patient 1: 17.8 mGy – Patient 2: 24.3 mGy Comparing Results Felmlee, Gray, et al (standard-sized patient): 21.9 mGy ImPACT method (standard-sized patient): 29 mGy Monte Carlo method (Angel et al): 17.8–24.3 mGy Implications of Results With estimated radiation dose to fetus in the 15–30-mGy range, what are the implications for a 7-week-old fetus? While there may be a wide variation among individual patients and in estimates from different methods: Fetal doses from a single abdomen/pelvis CT exam are still below the consensus levels for negligible risk (50–150 mGy) and well below “actionable” levels of 150 mGy. References: McCollough CH, Schueler BA, Atwell TD, et al. Radiation exposure and pregnancy: when should we be concerned? RadioGraphics 2007;27(4):909–17. Wagner, et al. Exposure of the pregnant patient to diagnostic radiations. Madison, WI: Medical Physics Publishing, 1997.