REPORT OF HEALTH EVALUATION For Students in Health Occupations Programs
advertisement

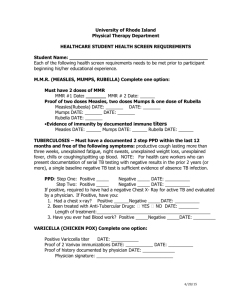
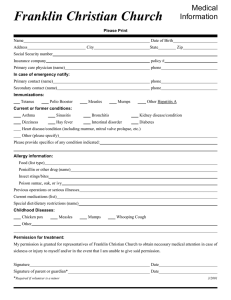
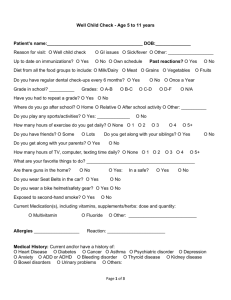
For College Procedure 7.01.03.10: Immunization Tuberculosis Testing and Physical Examination Requirements for Health Career and Nursing Students REPORT OF HEALTH EVALUATION For Students in Health Occupations Programs LAST NAME (PLEASE PRINT) FIRST NAME HOME ADDRESS (Number and Street) MIDDLE CITY PROGRAM STATE DATE OF ENTRY ZIP CODE DOB PATIENT’S HOME NUMBER: CELL NUMBER: EMAIL: Heart Attack: High Cholesterol: High Blood Pressure: Stroke: Mental Health Dz: Other: Pets: Indoor or outdoor Please answer all questions. Comment on all positive answers below. Have you had: ENDOCRINE/METABOLIC NAME, RELATIONSHIP, ADDRESS & PHONE # OF EMERGENCY CONTACT FAMILY Diabetes: HISTORY Cancer: Who do you live with: PERSONAL HISTORY: Have you had: INFECTIOUS DISEASES Measles German Measles Mumps Chicken Pox (at what age) Malaria Tuberculosis Mononucleosis Hepatitis Sexually Transmitted Disease Other (Describe) EYES/EARS/MOUTH Gum or Dental Problems Sinusitis Eye Problems Ear Problems Throat Problems IMMUNOLOGICAL Hay Fever (Seasonal allergies) Asthma Allergies To: Medicines Foods GI AND GU DISORDERS Frequent Nausea Frequent Diarrhea Constipation Frequency of Urination Burning on Urination Gall Bladder Problems Other (Describe) NEUROLOGICAL DISEASES Frequent Headaches Dizziness or Vertigo Head Injury/Unconsciousness Epilepsy/Convulsions Fainting Weakness Paralysis Other BLOOD DISORDERS Clotting Disorder Hemophilia Leukemia Anemia (Type) Reviewed by: Y Y Y Y Y Y Y Y Y Y N N N N N N N N N N Y Y Y Y Y N N N N N Y Y Y Y N N N N Y Y Y Y Y Y Y N N N N N N N Y Y Y Y Y Y Y Y N N N N N N N N Y Y Y Y N N N N Diabetes Thyroid Problems Other (Describe) MUSCULO-SKELETAL Disease or Injury of Joints Arthritis “Trick Knee”/Shoulder, etc. Back Problems Other (Describe) FEMALES ONLY First day of last menstrual period Irregular Periods/Excess Severe Cramps Current Pregnancy Other (Describe) G, P, A, L CARDIO-PULMONARY Shortness of Breath Palpitations Chest Pains/Pressure Chronic Cough High Blood Pressure Rheumatic Fever Heart Murmur Recurrent Colds Other (Describe) MISCELLANEOUS Tumors Cancer Cysts Other (Describe) PSYCHOLOGICAL Mental Health Disorder(s) Insomnia Frequent Depression/Anxiety Alcohol (ETOH) Smoking Recreational Drugs (cocaine/marijuana) Miscellaneous Surgery Hospitalizations overnight Major Accidents Other (Describe) CURRENT MEDICATIONS (List) Y Y Y N N N Y Y Y Y Y N N N N N Y Y Y Y N N N N Y Y Y Y Y Y Y Y Y N N N N N N N N N Y Y Y Y N N N N Y Y Y Y Y N N N N N Y Y Y Y Y N N N N N Date: EPCC does not discriminate on the basis of race, color, national origin, religion, gender, age, disability, veteran status, sexual orientation, or gender identity. Page 7 of 8 A. Has your physical activity been restricted during the past five years? YES B. Have you had difficulty with school studies or teachers? YES C. Have you received treatment or counseling for a nervous condition, personality or character disorder, emotional problems or chemical/alcohol dependence? YES NO (Give details) D Have you had any illness or injury or been hospitalized other than that already noted? YES E. Have you consulted or been treated by clinics, physicians, healers, or other practitioners within the past five years? (Other than routine checkups?) YES NO (Give Details) Have you been rejected or discharged from military service or employment because of physical, emotional, or other reasons? YES NO (If so, give reasons) Do you have any learning disabilities for which you may require assistance? YES NO (Describe) F. G. NO NO (Give reasons) (Describe) NO (Give details) I certify this personal history information to be correct: Student (CLIENT) Signature Date TO THE EXAMINING PHYSICIAN/ADVANCED PRACTICE NURSE/PHYSICIAN ASSISTANT: Please review the student’s history and complete the physical form. Please comment on positive answers. This information is for the use of the Health Careers Programs and will not be released without student consent. Physician/Advanced Practice Nurse/Physician Assistant must be licensed in the United States. LAST NAME (Please Print) Height Weight: Temp Pulse FIRST NAME MIDDLE NAME B/P Resp. IMMUNIZATIONS REQUIRED BY EPCC: GENDER Corrected/Non-Corrected Vision: R O2 Sat on RA L % Corrective Lenses: Y/N Why DATES AGE Both How Long (Immunization Record/Copy must be attached) Varicella: 1st 2nd OR Age of actual Illness OR BLOOD TITER Polio (3 doses up to age 19) Measles, Mumps, Rubella: 1st_ 2nd OR BLOOD TITER Tdap (Tetanus, diphtheria, pertussis) or Td (dose in past 10 years) Tuberculin Skin Test (Chest X-ray, if indicated) NEGATIVE POSITIVE Hepatitis B: 1st 2nd 3rd OR BLOOD TITER Other: Physical Assessment 1. Head, Ears, Nose, or Throat 2. Respiratory 3. Cardiovascular/Blood 4. Gastrointestinal 5. Hernia 6. Eyes 7. Genitourinary (Males only) 8. Musculoskeletal 9. Metabolic/Endocrine 10. Neurological 11. Skin 12. Psychiatric/Emotional Normal Abnormal Not Examine d Comments Recommendations for physical activity (including lifting, carrying, or standing) Unlimited/ Limited Recommendations for accommodations for any learning disabilities, physical disabilities, or emotional disabilities Yes/No (Explain) General Comments: EXAMINER’S SIGNATURE ADDRESS EXAMINER’S NAME and TITLE (typed or printed) PHONE FAX EPCC does not discriminate on the basis of race, color, national origin, religion, gender, age, disability, veteran status, sexual orientation, or gender identity. DATE Page 8 of 8