Enhancing mental capacity Dr Sarah JL Edwards Senior Lecturer in Research Governance
advertisement

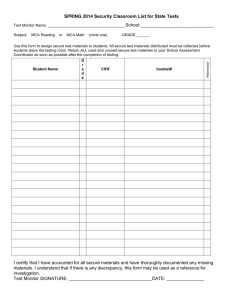
Enhancing mental capacity Dr Sarah JL Edwards Senior Lecturer in Research Governance Contents • Patients’ understanding medical information • Assessing mental capacity • Treating those without capacity • Informational manipulation Patients’ understanding • cancer screening “the 5-year survival of patients diagnosed with early stage cancers is much greater than that of patients diagnosed with later stage cancers” (Schwartz 1999, p.128). • People usually believe that this shows screening is beneficial, but patients diagnosed earlier live with a cancer diagnosis longer. Understanding Risk • Grimes and Snively (1999) asked 633 women in a gynaecology outpatient’s clinic to compare which of the risk levels represented by 8.9 per 1000 and 2.6 per 1000 was the higher • Risks stated as rates were better understood than as proportions (Lloyd 2001, p.i16) Goal of treatment • Gattellari et al. (2002) reported that 80% of patients who had been told by their physician that there was no chance of cure stated that there was actually some chance of cure, while 15% stated that their chance of cure was at least 75%. Assessing Capacity A person lacks capacity in relation to a matter if at the material time he is “unable to make a decision for himself in relation to the matter because of an impairment of, or a disturbance in the functioning of, the mind or brain.” s2(1) In practice… • Assume patient has various degrees of ability along certain dimension that can be measured • ‘Expert’ judgement/impression • Neurological predictive factors • 18 different ‘objective’ instruments • Constructs have different meanings • First- or third-person scenarios • • • • • • • • • • • • • • • • • • • • • • • • • • The Mini-Mental State Exam Patient___________________________________ Examiner ____________________________ Date____________ Maximum Score Orientation 5 ( ) What is the (year) (season) (date) (day) (month)? 5 ( ) Where are we (state) (country) (town) (hospital) (floor)? Registration 3 ( ) Name 3 objects: 1 second to say each. Then ask the patient all 3 after you have said them. Give 1 point for each correct answer. Then repeat them until he/she learns all 3. Count trials and record. Trials ___________ Attention and Calculation 5 ( ) Serial 7’s. 1 point for each correct answer. Stop after 5 answers. Alternatively spell “world” backward. Recall 3 ( ) Ask for the 3 objects repeated above. Give 1 point for each correct answer. Language 2 ( ) Name a pencil and watch. 1 ( ) Repeat the following “No ifs, ands, or buts” 3 ( ) Follow a 3-stage command: “Take a paper in your hand, fold it in half, and put it on the floor.” 1 ( ) Read and obey the following: CLOSE YOUR EYES 1 ( ) Write a sentence. 1 ( ) Copy the design shown. _____ Total Score ASSESS level of consciousness along a continuum ____________ Alert Drowsy Stupor Coma McArthur competence tool • Semi-structured interview • In conjunction with clinical assessment • Measure on scale 0-6 – understanding of the disorder and its treatment, including associated risks and benefits – Appreciation of the disorder and its treatment (belief) – Ability to compare treatment with alternatives – Ability to express a choice • TRAT fictional vignettes Grisso and Appelbaum Am J Psychiatry 1995; 152:1033-37 Re C (1994) 1 All ER 819 • Case Law • Schizophrenic refusing amputation for gangrenous leg • Believed he was world class surgeon • Court ruled he was competent to decide • Not treated under Mental Health Act for his schizophrenia! Statue s3(1) “A person is unable to make a decision for himself if he is unable to: 1)understand the information relevant to the decision; 2)retain the information; 3)use or weigh that in formation as part of the process of making the decision; or 4)communicate his decision (whether by talking, using sign language or any other means).” Still no belief requirement • No express requirement in test that person believes the information or has insight into illness • If false belief results from psychotic delusion then assessed formally under mental health legislation • Denial of the facts itself not sufficient to render incapable – (remember Jo and denial of his daughter’s death?) Marginal or fluctuating capacity • Protect person’s position in event s/he is likely to regain capacity • New right to have all ‘practical’ help • New role for statutory Independent Mental Capacity Advocate service (IMCA) • May be duty to provide specialist help outside normal fiscal restraints • The decision-maker should make sure that all practical means are used to enable and encourage the person to participate as fully as possible in the decision-making process and any action taken as a result, or to help the person improve their ability to participate. Help to restore capacity • The explanation must be in the most appropriate and effective form of communication for that person. • There are different methods for people who use nonverbal means of communication (for example, observing behaviour or their ability to recognise objects or pictures). Use of equipment? • It may be important to provide access to technology. For example, some people who appear not to communicate well verbally can do so very well using computers. MCA Code of Practice chapt 3 • using simple language and/or illustrations or photographs • asking them about the decision at a time and location where the person feels most relaxed and at ease • breaking the information down into easyto-understand points • using specialist interpreters or signers to communicate with the person. Yes/No • Avoid questions that need only a ‘yes’ or ‘no’ answer (for example, did you understand what I just said?)....But there may be no alternative in cases where there are major communication difficulties. In these cases, check the response by asking questions again in a different way. Treating non-competent adults: best interests • Decisions made under the MCA must be made in the person’s best interests • Sole exception is in event of valid and applicable advance decision/statement • Competent person may nominate another (donee of Lasting Power of Attorney) to make decisions in case of incompetence Common law doctrine of necessity • Act in best interests of non-competent patient but treatment must be ‘necessary’ • Protect doctor from liability for acts which could otherwise amount to battery • Re F (Mental Patient: Sterilisation) [1990] 2 AC 1 Assessing best interests • New statutory criterion s4 – Consider person’s past and present wishes and feelings (particularly any advance statements) – Consider beliefs and values that would be likely to influence his decision if he had capacity – Consider the other factors that he would be likely to consider if he were able to do so • Not complete checklist • No order of priority given • But assessment must be ‘reasonable’ in the circumstances Process of Consultation • When ‘practical and appropriate’, decisionmaker must also consult following people as to what would be in person’s best interests – Anyone named by person – Anyone engaged in caring for person or interested in his welfare – Any donee of a lasting power of attorney – Any deputy appointed for person by Court • Code of practice encourages as wide a range of people who are close to the person except in research where single ‘consultee’ Persuasion paradox • Patient unaware that information has been manipulated which could itself undermine autonomy Framing risk • Schwartz (1999) “simple changes in the format of otherwise identical numerical information can profoundly influence its interpretation” (p. 127). • Given a choice between surgery and radiotherapy, patients would tend to choose surgery despite probable outcomes being the same but framed differently: Whose interests? • Manipulating information truly in patient’s best interests? • Hard vs soft paternalism • Fairness and statistics • Evaluating effects