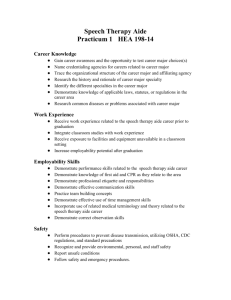
Section 6 HEALTH AIDE PROGRAM Subject Page
advertisement

Section 6 HEALTH AIDE PROGRAM Subject Page The Health Aide Program................................................................................................ 2 Primary Responsibilities .................................................................................................. 2 Approved Health Aide Actions......................................................................................... 2 Things You Should Always Do & Things You Should Never Do ..................................... 2 Questions and Answers .................................................................................................. 3 Health Aide Skills ............................................................................................................ 4 Guide to Hospital Referrals ............................................................................................. 5 Directions to area hospitals ............................................................................................. 6 Health Aide Kit Contents ................................................................................................. 7 Medications ..................................................................................................................... 8 Health Aide Report ........................................................................................................ 10 Personal Data and Emergency Information Form ......................................................... 11 Bloodborne Pathogen Exposure Control Plan............................................................... 12 Meningitis on Campus................................................................................................... 14 Eating Disorders............................................................................................................ 15 Anorexia Nervosa.................................................................................................... 15 Bulimia Nervosa ...................................................................................................... 16 How to Help a Friend............................................................................................... 17 Emotional and Mental Concerns/Referral...................................................................... 18 Guidelines for Responding to Emotional Crisis/Suicide................................................. 19 Important Phone Numbers ............................................................................................ 20 University of Northern Iowa THE HEALTH AIDE PROGRAM ...Obtaining a history of the problem, which a student presents by determining: ­When the problem began? ­What symptoms are present? ­How severe are the symptoms? ...is a cooperative project of University Health Services and the Department of Residence at the University of Northern Iowa. ...serves as an adjunct of the Student Health Center under the supervision of the Health Aide Coordinator and the University Health Services Director. ...Taking temperature. ...Applying an elastic bandage to an extremity. ...Providing appropriate, over­the­counter medications for symptomatic relief until the student can seek professional care or provide his/her own medication. ...provides a source of health information for residents of University Residence Halls on a well­informed lay person's level of competence when the Health Clinic is closed. ...Making timely and appropriate referrals. ...seeks to promote healthful living habits and health awareness for university students. THINGS YOU SHOULD ALWAYS DO! ...Determine symptoms. AS A HEALTH AIDE YOUR PRIMARY RESPONSIBILITIES ARE TO: ...Obtain a brief history of the problem. ...Recognize your limitations. ...Ask the student if they are allergic to any medications. ...Assist students who request your help in the management of health concerns. ...Provide assistance as indicated and/or referral to other resources. ...Identify any need for, and assist in referral to appropriate medical or health care resources. ...If in doubt about appropriate, safe course of action, contact the Health Center or call Covenant Nurse On­Call for advice. ...Maintain and submit Health Aide Reports for all students who receive Health Aide services. ...Wear rubber gloves whenever there is the possibility of having contact with blood. ...Report environmental, safety or public health concerns to the Hall Coordinator and/or Health Aide Coordinator. THINGS YOU SHOULD NEVER DO! ...Post health related information sent to you by the Health Aide Coordinator. ...Discuss student health concerns with anyone other than a qualified referral source such as the Hall Coordinator, Medical Personnel or Health Aide Coordinator. ...Participate in an American Red Cross Standard First Aid Course. ...Attend the Health Aide Orientation and Inservice Programs. ...Give any medications to students other than those in the Health Aide Kit. APPROVED HEALTH AIDE ACTIONS INCLUDE: ...Loan the Health Aide Kit to others. ...Open a blister. ...Assisting with the cleansing and dressing of minor wounds without having direct contact. ...Diagnose...e.g., "You have mono.", "You probably have an ulcer." 2 University of Northern Iowa QUESTIONS? ANSWERS! provide First Aid or symptom relief only until the Health Clinic opens or until they can reasonably obtain their own supply from a local pharmacy. The amount given should never exceed the recommended dosage for a 24 hour period. WHICH HOSPITAL EMERGENCY SERVICE SHOULD STUDENTS VISIT? ...There are three area hospitals with emergency services. Sartori Hospital is located in Cedar Falls and is in close proximity to the University Campus. Allen Hospital and Covenant Medical Center are located in Waterloo and have more comprehensive services. Directions to area hospitals and Urgent Care Clinics are on page 6. HOW DO I GET A RELUCTANT STUDENT TO GO TO THE HEALTH CENTER? ...The student does have the right to refuse medical care. ...The decision to seek professional medical care is the personal responsibility of each student. This decision may be influenced by an individual's attitudes toward medical care, past experience with a health care system, the influence of peer groups and his/her ability to tolerate not feeling well. ...Transportation by the Cedar Falls ambulance is to whatever hospital the student requests. If the student's condition is critical the ambulance will go to the nearest emergency room. ...Your role as a Health Aide is to identify for the student when you believe, based on your level of knowledge, that medical care is advised. WHO PROVIDES TRANSPORTATION FOR THE ILL/INJURED STUDENT? ...Students requiring transportation to the Health Center or hospital are encouraged to provide their own car or have a friend transport them. ...You are encouraged to explore with a student the possible concerns they have about seeing a physician. ...If no student transportation is available and it is not an emergency situation, University Police will provide transportation to the Health Clinic or Sartori Hospital. ...In some situations, accompanying the student to the Health Clinic may serve to decrease that individual's anxiety by providing a more personalized approach to their particular health problem. ...For the transportation of the seriously ill or injured, call 911. ...If a student refuses to seek medical attention identify clearly on the Health Aide Report your recommendations and the student's response. ...Resident Assistants are not to transport students in need of medical care. HOW MUCH MEDICATION OR HOW MANY SUPPLIES SHOULD I GIVE TO A STUDENT? ...Health Aide services are intended to supplement the Health Clinic when the Center is not open. Medications and supplies should be given in amounts to 3 University of Northern Iowa Health Aide Skills · 1. Treatment of an Open Wound · · Due to the risk of bloodborne diseases, you need to instruct each resident to wash and dress his/her own wound. · · · Instruct the victim to do the following: Rinse wound with water. Using an antiseptic towelette, wash wound in a circular motion starting directly on top of the wound working outward. Rinse wound again with water. Place dry dressing on wound being careful not to touch the area of the dressing which will have direct contact with the wound. · · 3. Using an Elastic Wrap An elastic wrap is used to prevent swelling in an extremity following an injury. The R.I.C.E. treatment will slow the swelling, reduce pain and shorten recovery. Observe wound for signs of infection: ü increased pain and redness ü pus ü red streaks ü hot to touch ü difficulty in healing ü fever · Keep dressing dry and intact. · Change dressing several times each day. The peak temperature should be reached in approximately 60 seconds. Opening the mouth or improper placement of the tip could result in a longer time for a reading. When the peak temperature is reached the thermometer will beep continuously. Read and document temperature. Remove the plastic cover and discard Clean thermometers with an alcohol wipe and turn the unit off. Document the reading on the Health Aide Report. R.I.C.E. Treatment REST ­ Limit movement of the impaired area. ICE ­ Apply immediately around entire injured area. Protect skin from ice burn with the elastic bandage or towels. ***Check tetanus status. A person should have a tetanus booster at least every ten years.*** COMPRESSION ­ Apply elastic wrap. Start at the toes, use a figure eight at the ankle and work up. This bandage should be re­wrapped when it become loose. Bandage should not impair circulation; therefore, check for color and complaints of numbness. ***If there is any possibility that you might have direct contact with the wound, gloves must be worn. ELEVATION ­ Entire injured limb should be elevated at least to the level of the hip or above the hip. 2. Temperature Taking · Wipe thermometer with an alcohol wipe. Place plastic cover over the tip. · Push the on­off button located besides the display window. The last measured temperature will be displayed for approximately 2­seconds. · The unit will flash when ready to use. · Place the thermometer in one of the back pockets under the tongue. ***Contact the Health Center or Emergency Room for more information.*** 4. Phoning the Emergency Medical Services · · · 4 Make the call (9­911) Stay on the phone after you have given all the information listed below in case the EMS dispatcher has any further questions. Be prepared to tell the dispatcher ­ University of Northern Iowa · · · · ü The location of the emergency (exact address, name of building, floor, room (number). ü The telephone number of the phone being used. ü The caller's name. ü What happened. ü The number of victims. ü The victim's condition. ü The help being given. While waiting for the ambulance stay with victim and monitor his/her vital signs; send a person to meet the ambulance. If the paramedics believe it is not necessary to transfer the person to the hospital, there is no charge. If this is not an emergency, however, a resident needs to be transported to the hospital. University Police will transport students to Sartori Hospital. Resident Assistants are instructed not to transport residents to the hospital. Delegate a roommate, friend, or call University Police. symptoms such as shaking, rapid breathing and shortness of breath. ...Ingestion of medication or substances in excess of the recommended amounts. ...Chest pain or shortness of breath. ...High fever. ...Vomiting and or diarrhea which has persisted for more than 12 hours. ...An abrasion or wound of any size imbedded with foreign material which cannot be easily removed using approved First Aid procedures. ...Third degree burn on any area of the body. ...Second degree burn (blistering) larger than a fifty­cent piece, or on the face of any size. ...Severe sun­burn over large body area. ...Laceration which might affect cosmetic appearance. A GUIDE TO HOSPITAL REFERRALS ...Laceration on the hand or finger which affects the normal movement or sensation of the fingers. When the Health Clinic is closed, students need to make a decision regarding the need for immediate medical care for problems which may be serious but are not life threatening. …An allergic reaction which causes wheezing or shortness of breath and/or extensive hives or swelling. Students with any of the following conditions should be encouraged to visit the hospital. A combination of these symptoms may indicate a more serious condition: ...Has abnormal, profuse vaginal bleeding. ...Symptoms of any nature which become increasingly severe, and the Health Clinic will be closed for more than 12 hours. ...Severe pain. ...Suicidal threats. ...Severe anxiety which is not controlled by reassurance, presence of others or is accompanied by uncontrollable physical 5 University of Northern Iowa DIRECTIONS TO AREA HOSPITALS TO SARTORI HOSPITAL: Go north on College Street past the College Hill area. Drive to 6th Street and Sartori Hospital will be on your left. TO ALLEN HOSPITAL: Go north on Hudson Road. Turn right on Highway 57. This becomes 218 and goes east. Highway 218 will exit right. You will travel straight on Broadway. Turn left onto Burton Ave. then turn right on Donald Street. Allen Hospital will be on your right. TO COVENANT MEDICAL CENTER: Go south on Hudson Road. Take Highway 20 East exit. You will be on Highway 20 until you take the Hawkeye Tech/Highway 21 exit. Turn left onto Highway 21 and then left onto San Marnan at the stoplight. At the next stop­ light turn Right onto Kimball Ave. and then a Right on Park Lane. Park Lane will take you straight to Covenant. URGENT CARE: Phone numbers on Page 20. 6 University of Northern Iowa HEALTH AIDE KIT ­ FIRST AID SUPPLIES •Advil (Ibuprofen) *Alcohol Pads •Antibiotic ointment •Antiseptic Towelettes •Bandaids (small) •Bandaids (large) *Benadryl (Coordinator’s Kit) •Calamine Lotion (Coordinator’s Kit) •Elastic bandage •Gauze pads •Gauze wrap (3" roller gauze) •Ice Pack •Medicine cup •Paper sack •Pepto Bismol •Plastic bags •Rubber gloves •Safety pins •Scissors •Tape •Thermometer *Thermometer covers •Throat lozenges/cough drop •Triangle Bandage •Tweezers •Tylenol (acetaminophen) *Face shield in top cover RESIDENTS MUST BE INSTRUCTED TO READ ALL WARNINGS AND DIRECTIONS BEFORE USE OF ANY MEDICATION. 7 University of Northern Iowa absorb nutrients and medications. Sodium and sugar free.) · Do not take if you are allergic to aspirin. If taking medications for anticoagulation, diabetes or gout, call a physician. · Those recovering or who have chicken pox should not use this to treat nausea and vomiting. · May darken tongue or stool. HEALTH AIDE KIT ­ MEDICATIONS Calamine Lotion · Topical astringent · Recommended as a soothing and protective application for minor skin irritations. · Stops oozing, reduces inflammation and promotes healing. Acetaminophen · Analgesic/Antipyretic (reduces fever) · For temporary relief from simple headache, minor aches and pains and discomfort of fever due to colds and "flu". Usage: Shake well before using. Soak a gauze pad and apply on the irritated area. Apply morning and night to the affected area. Triple Antibiotic Ointment · Recommended to help prevent infection in minor cuts, burns and abrasions. Dosage: One­two tablets three­four times per day. Usage: After gentle washing, apply a small amount (an amount equal to the surface area of the tip of a finger) directly to the affected area and cover with a sterile dressing. May be applied one to three times daily. · ***As with any drug, seek advice of a health professional if you are pregnant or nursing. ***Before giving out any medication, ask: 1. Are you taking any other medications? 2. Are you allergic to any medications? 3. Do you have any medical problems? In case of deep or puncture wounds or serious burns, consult a physician. If redness, irritation, swelling or pain persists or increases or if infection occurs, discontinue use and consult a physician. Do not use in eyes. Ibuprofen *Temporarily relieves minor aches and pains due to: headache, the common cold, toothache, muscular aches, backache, arthritis, and menstrual cramps. *Temporarily reduces fever Cough Drops · Temporarily relieves coughs and minor throat irritations due to colds and inhaled irritants and protects irritated areas of sore throat. Dosage: 1 tablet every 4 to 6 hours. If pain or fever does not respond to 1 tablet, 2 tablets may be used. Do not exceed 6 tablets in 24 hours unless medically directed. Dosage: One lozenge every hour as needed. Allow cough drop to dissolve slowly into the mouth. Benadryl *Relieves symptoms of allergy reactions Pepto Bismol (Generic) · Antacid/Anti­Diarrheal. Provides soothing relief for heartburn, indigestion, nausea, upset stomach and diarrhea. Dosage: 2 tablets every 4­6 hrs. Drowsiness can occur; avoid alcoholic drinks when taking this medication. Excitability may occur in some people. Dosage: Two tablets. Chew or dissolve in Mouth. Repeat every 1/2 to one hour. (Maximum of eight doses in 24 hours. May 8 University of Northern Iowa Health Aide Report All contacts with residents regarding health related problems must be considered confidential and should not be discussed with other residents. Complete a Health Aide Report immediately following the visit with the resident. Submit the competed form to your Residence Life Coordinator or other designated R.A. by the end of the week. The next page is a copy of the health aide report, formatted to fit this manual. However, the actual duplicate health aid reports are available from Joan Thompson. 9 University of Northern Iowa University of Northern Iowa Health Aide Form RA Name: _______________________________ Hall: _________________________________ Student’s Name: __________________________ Date: _________________________________ Problem (check all that apply): r Minor cut (no bleeding) r bleeding wound r headache r sore throat r runny nose r congestion r fever r body aches r upset stomach r bruises / swelling r loft injury r alcohol related r other (please explain): r menstrual cramps r diarrhea r vomiting ________________________________________________________ Supplies Used (include numbers used): r alcohol pads _____r medicine cup _____r antibiotic ointment _____r paper sack _____ r small band­aids ____r plastic bag _____ r large band­aids _____ r safety pins _____ r roller gauze _____r elastic bandage _____r rubber gloves _____ r ice pack _____ r micro shield _____r small gauze pads _____r large gauze pads _____r Acetaminophen__ r scissors _____ r triangle bandage _____r tweezers _____ r roll of tape _____ r cough drops _____r Advil_____r antiseptic towelette r thermometer and cover r Dio Tame (Pepto Bismol) _____ 10 University of Northern Iowa Personal Data and Emergency Information Each Resident should fill out a personal information form when they move into the Residence Hall. The Resident Assistant should collect completed forms and place them in an accessible location determined by the Hall Coordinator. Completion of the medical information on this form is not mandatory; however, it may be helpful to the resident in a medical emergency. A copy of the personal information form is provided below. Hall__________________________ Room #_______________________ Telephone #___________________ Date of Birth___________________ Student ID #___________________ Personal Information Sheet Department of Residence University of Northern Iowa Student Information: __________________ Name____________________________________________________Social Security # Last First MI Permanent Address___ _________________________________________________________________ Street City State ZIP Class Rank: ___Freshman ___Sophomore ___Junior ___Senior ___Graduate Major(s)____________________________________Minor(s)_____________________ Interest Survey: Would you like to be contacted with information about any of the following? ___ Hall government positions (house and hall­wide) ___ Campus leadership opportunities Please place a check mark by those programs you would be interested in attending/learning more about: ___ personal relationships ___ financial commitments ___ the arts ___ community service ___ diversity ___ learning skills ___ academic advising ___ health/wellness ___ social opportunities ___ career planning ___ personal development ___ university resources Please list any other areas of interest_______________________________________________ __________________ ____________________________________________________________________________ __________________ Medical Information: Insurance Provider______________________________________ Policy# _________ __________________ Any condition(s) the residence hall staff should be aware of________________________ __________________ _______________________________________________________________________ __________________ Please list any allergies___________________________________________________________________ Parent or Guardian Information: In case of emergency, I give permission for the following person(s) to be contacted: _________________________________________________ Name __________________________________ Telephone Number ____________________________________________________________________ Street City State ZIP This information may be used to identify interests, special needs, or to contact you in case of emergency. It will only be available to necessary officials, such as staff in the Department of Residence, University Police, University Health Services, and emergency medical personnel. 11 University of Northern Iowa Resident Assistant's Exposure Control Plan for Bloodborne Pathogens University Health Services University of Northern Iowa with blood or body fluids and preventive measures are not taken. Resident Assistants who come in contact with blood or PIM need to consider the source as potentially infected with HIV and/or other bloodborne pathogens. They need to adhere to infection control precautions to minimize the risk of an exposure incident. The purpose of this policy is to eliminate or reduce the risk of exposure to infectious disease and familiarize Resident Assistants with the procedures to follow if an exposure occurs. Definitions: The Resident Assistants are trained in Standard First Aid and CPR. However, it is not a job expectation for a Resident Assistant/Health Aide to respond to a situation that may put him/her at risk of contact with blood or other PIM. In the event of an emergency, the Resident Assistant/Health Aide, as any other student, would make a decision whether to make physical contact or to provide appropriate care without contact. The Emergency Medical System (EMS) can be activated by calling 911. Bloodborne Pathogens ­ Pathogenic microorganisms that are present in human blood and can cause disease in humans. These pathogens include, but are not limited to hepatitis B virus (HBV) and human immunodeficiency virus (HIV). Exposure Incident ­ A specific eye, mouth, other mucous membrane, non­intact skin or parenteral contact with blood or other potentially infectious materials (PIM). Universal Precautions, an approach to infection control, must be observed when contact with blood or other PIM is anticipated. According to the concept of Universal Precautions, all human blood and PIM are treated as if known to be infectious for HIV, HBV and other bloodborne pathogens. PIM (Potentially Infectious Materials) ­ This includes blood, blood fluids, semen, vaginal secretions, pleural, cerebrospinal, synovial, pericardial, amniotic fluids, saliva in dental procedures, any other fluids visibly contaminated with blood, tissues and organs, HIV and HBV cultures, cells and tissues. For minor abrasions or lacerations the Resident Assistant will instruct individuals to wash and dress their own wound and will provide information on the signs of infection. In this situation the Resident Assistant will have no physical contact with the wound or PIM. All incidents with blood and/or PIM as a by­product need to be documented on a Health Aide Report. RAs having contact with blood will be offered the Hepatitis B Vaccine. Non Infectious Materials ­ This includes nasal secretions, sputum, sweat, tears, urine, feces and vomitus unless they contain visible blood. Universal Precautions ­ A method of infection control in which all human blood and certain human body fluids are treated as if known to be infectious for HIV, HBV and other bloodborne pathogens. There has been an increase in the prevalence of Hepatitis B Virus (HBV) and Human Immunodeficiency Virus (HIV) in the blood of the general public. This has increased the risk to Resident Assistants who give first aid care to other individuals. This is especially true when the Resident Assistant/Health Aide comes in contact 12 University of Northern Iowa I. Direct Contact With Blood II. Exposure Incidents By activating EMS in an emergency and training victims to treat their own wounds, Resident Assistants greatly reduce their risk of exposure to bloodborne pathogens. Resident Assistants/Health Aides who make a personal decision to make contact with blood and/or PIM should use the skills and procedures learned in the Health Aide Training. A Resident Assistant who feels he/she may have had an exposure incident should follow the procedure outlined below. · · · · · 1. Contact the Resident Life Coordinator. 2. Phone Occupational Medicine & Wellness at Arrowhead Medical Center – 575­5600 (226 Bluebell Road) or Sartori Emergency Room at 268­3000 (during evening or weekend hours) to validate the exposure. It is mandatory for Resident Assistants to use disposable gloves when there is a possibility of having contact with blood or body fluids. After use, gloves shall be removed by reversing them and disposed of in a biohazard bag along with any contaminated dressings. 3. If an exposure has occurred a confidential medical evaluation and follow­up will be made available to the Resident Assistant at no charge. Resident Assistants will wash their hands thoroughly as soon as possible after removal of the gloves and after hand contact with blood or other potentially infectious materials. Avoid touching your mouth, eyes, or nose while providing care or before you wash your hands. Any Resident Assistant who has had contact with blood (with or without gloved hands) will be offered the Hepatitis B vaccine. The Health Aide Coordinator should be called at 273­2198 as soon as possible following the incident to discuss receiving the vaccine. A microshield mouth barrier must be used if a Resident Assistant chooses to perform artificial respiration. Resident Assistants are not responsible for cleaning up blood. Blood spills will be cleaned up by custodians with appropriate cleansers. If a blood spill occurs during the night or weekend, the area should be isolated until custodians are able to deal with it properly. Items contaminated with blood that cannot be properly disinfected due to cracks and crevices should be disposed of in a hazardous waste bag. · When medically indicated, Hepatitis B Immune Globulin will be given and the Hepatitis B vaccine series started at no cost to the R.A. · The University will notify the source individual of the incident and attempt to obtain consent to collect and test the source's blood to determine the presence of HIV and/or HBV infection. · Collection of blood from the exposed Resident Assistant will be offered as soon as possible after the exposure incident for determination of HIV and or HBV/status. · Repeat HIV testing will be offered on a periodic basis thereafter (6 weeks, 3 months, 6 months and 12 months after exposure). · Follow­up of the exposed Resident Assistant shall include counseling and instructions for reporting illness following the exposure. (The Resident Assistant has a choice whether or not to receive the medical evaluation and follow­up testing offered by the University ­ There is no cost to the Resident Assistant.) 13 University of Northern Iowa · III. INFORMATION AND TRAINING The training program is designed to present information on the nature of bloodborne diseases and help Resident Assistants reduce or eliminate potential exposure to themselves and others from bloodborne pathogens in their environment. Resident Assistants will be provided information and training in the following areas: · · · · · · · The Bloodborne Pathogens Standard. Transmission and symptoms of bloodborne diseases. A review of methods that will prevent or reduce exposure. The use of biohazard labels, signs and container "color­coding". An explanation of the procedures to follow if an exposure incident occurs, including reporting and medical follow­up. Information on the post­exposure evaluation and follow­up that is provided in case of an exposure incident. · · The training is incorporated into annual Health Aide training. Questions or concerns regarding Bloodborne Pathogens should be directed to Joan Thompson at 273­2198. MENINGITIS ON CAMPUS Know Your Risk Learn About Vaccination · Who is at risk? Certain college students, particularly freshmen who live in dormitories or residence halls, have been found to have an increased risk for meningococcal meningitis. Other undergraduates can also consider vaccination to reduce their risk for the disease. · For more information: To learn more about meningitis and the vaccine, visit the UNI Student Health Center or call (319) 273­ 2009. You can also visit the websites of the Centers for Disease Control and Prevention (CDC), www.cdc.gov/ncidod/dbmd/diseaseinfo, and the American College Health Association, www.acha.org. Certain college students are at increased risk for meningococcal disease, a potentially fatal bacterial infection commonly referred to as meningitis. Freshmen living in residence halls are found to have a six fold increased risk for the disease. It is estimated that 100 to 125 cases of meningococcal disease occur annually on college campuses in the United States, and 5 to 15 students die as a result. A U.S. health advisory panel recommends that college students, particularly freshmen living in residence halls, learn more about meningitis and vaccination. 14 Can meningitis be prevented? Yes. A safe and effective vaccine is available to protect against four of the five most common strains of the disease. The vaccine provides protection for approximately three to five years. As with any vaccine, vaccination against meningitis may not protect 100 percent of all susceptible individuals. The vaccine is available at the Student Health Center. To make an appointment, call (319) 273­7425. What is meningococcal meningitis? Meningitis is rare. But when it strikes, this potentially fatal bacterial disease can lead to swelling of fluid surrounding the brain and spinal column as well as severe and permanent disabilities, such as hearing loss, brain damage, seizures, limb amputation and even death. How is it spread? Meningococcal meningitis is spread through the air via respiratory secretions or close contact with an infected person. This can include coughing, sneezing, kissing or sharing items like utensils, cigarettes and drinking glasses. What are the symptoms? Symptoms of meningococcal meningitis often resemble the flu and can include high fever, severe headache, stiff neck, rash, nausea, vomiting, lethargy and confusion. University of Northern Iowa Eating Disorders Anorexia Nervosa Definition: An obsession with weight and food in which the person craves food, but refuses to eat or retain it, because of an intense fear of weight gain. Anorexia nervosa is not only a physical, but also a psychological eating disorder where the unrealistic pursuit of the "ideal" body form can result in illness, or possibly, death. Signs and Symptoms: Behavioral · Obsessive interest in food and weight; talks about food, weight; may hoard food, dream about food, cook elaborate meals for others, or collect recipes. · Withdrawal from social situations; especially occasions that include food. · Frequently weighing self, sometimes every hour. · Distorted body image, always feeling too fat. · Rigorous exercise routine, always on the go; any change in this schedule usually results in anger, frustration, or panic. · Seemingly pleased at being told they are too thin. · Eating from a regimented list of safe foods (non­ fattening) · Frequently skipping meals, using excuses why they can't eat, lying about what has already been eaten. · Denial of illness; resistance to treatment. · Neurotic eating patterns­ cutting food into tiny pieces, disposing of food secretly to give the impression that food has been eaten. · Compulsive behaviors ­ a need to have everything orderly or perfect. · Vomiting or using laxatives or diuretics after eating. · Distorted perception of events ­ perceiving things as "much worse" than they really are. · Extreme reactions to normal happenings. · · · · · · Physical People with Anorexia Nervosa can outwardly appear well. The following physical signs and symptoms may be present. · · · · · · · · · · · · · · · Emotional · Low self­esteem. · Frequent mood swings usually depending on weight loss or gain. · Depression, social withdrawal, irritability, defiance, stubborn. · Frequent whining or crying episodes over seemingly trivial matters. · · 15 Decrease in ability to concentrate. Difficulty in tolerating change. Intense fear of becoming obese. Decreased interest in sex. Delayed psycho­sexual development (in teens). Nonassertive, "people­pleasers". Loss of menstrual periods (amenorrhea). This is the body's attempt to prevent ovulation and pregnancy in an under­nourished body. It is also an early indication that weight loss has preceded too far for that individual. Low body temperature, feel cold all the time. 20 to 25% weight loss. Low blood pressure (hypotension) and slow pulse (bradycardia), may bruise easily. Lanugo: a soft, downy­like hair on face, back, and limbs; this is the body's attempt to keep itself warm in the absence of needed fat. Loss of hair from scalp, lack of sheen, body. Brittle nails or dry skin and lips. Anemia: a decrease in circulating hemoglobin and oxygen in the blood; this results in a pale ashen color. Muscle Atrophy: a decrease in the body's protein reserves leads to a noticeable loss in strength. Many anorexics, however, still continue their strenuous, rigid exercise schedule. Increase in dental lesions (in vomiters­ due to the acids in the stomach passing over teeth). Edema: swelling caused by collection in tissues of fluid which has escaped from blood capillaries. Constipation. Abdominal distress, gastric complaints. Cyanosis: skin and mucous membranes are bluish from lack of oxygen in the blood. Yellowish skin (which usually indicates that a high level of carotene is present in the blood). Muscle weakness, abdominal distension, nervous irritability, apathy, drowsiness, mental confusion, and irregular heartbeat related to potassium deficiency. Swollen parotid glands and submandibular or submaxillary glands ("chipmunk cheeks") probably related to vomiting. University of Northern Iowa Bulimia Nervosa Definition: An eating disorder similar to chemical dependency. A person with bulimia regularly consumes large amounts of food (binge or gorge) and then purge themselves after each binge through self­induced vomiting and/or laxative or diuretic abuse, fasting, or excessive exercise. · · · · · Signs and Symptoms: Behavioral · Frequently weighing of self, sometimes before and after a binge. · Eating in seclusion. · Stealing food from stores or roommates. · Stealing money to buy food. · Frequent bathroom trips, indicating possible vomiting or laxative abuse. · Inconspicuous eating binges often followed by vomiting; may eat a normal meal and binge in secret afterwards. · Rapid eating during a binge; for many, bingeing is not pleasurable. · Great concern with outward appearance. · Alcoholism or drug abuse. · · · · · · · · Emotional · Awareness that eating behavior is abnormal. · Intense fear of inability to quit eating voluntarily. · Depressed, irritable, angry, frightened, dishonest, and secretive. · Severe mood changes, self­deprecation. · "Out­of­control" feelings. · Loneliness. · Low self­esteem. · Apathy. · Guilt. disease, gastrointestinal disorders, cardiac arrest. Anemia. Rupture of stomach or esophagus resulting in peritonitis. Ulcers. Mouth sores. Increased dental lesions; dental erosion caused by vomiting affects the inner side of the upper teeth, starting with the molars and moving forward to the front teeth. Edges of front teeth begin to shorten producing a faulty bite; jaw scrunches up toward nose. Calluses on fingers and hands from inducing vomiting. Difficulties breathing and swallowing. Dizziness, weakness, tremors. Grayish skin, acne and other sores that do not heal. Hiatal hernia (the stomach pushes through the diaphragm creating the sensation of choking). Frequent weight fluctuations (up to 10 pounds or more) due to alternating binges and purges. Irregular menstrual cycles. Acute gastric dilation (stomach is so full it threatens to burst). Abuse of laxatives can lead to: · Pain · Infections · benign and malignant tumors · massive dehydration · abnormal bowel functioning, loss of intestinal muscle tone · dependency · "heart flutters" abuse of diuretics can lead to damage to the kidneys, fluid and electrolyte abnormalities, dependency and water retention once the diuretics are stopped. Physical Continued vomiting can lead to: · Constant sore throat. · Destruction of tooth enamel. · Chronic puffiness under eyes. · Swollen glands ("chipmunk cheeks"). · Ruptured blood vessels in face. · Stomach aches. · Dehydration. · Low electrolyte balance of body chemicals that may result in muscle spasms, kidney For more information, please contact one of the following resources: Counseling Center Health Aide Coordinator 16 273­2676 273­2198 University of Northern Iowa How to Help a Friend With an Eating Disorder · DO NOT: · Tell her she's crazy · Blame her · Gossip about her · Follow her around to check on her eating or purging behavior · Ignore the problem · Reject her · Tell her to "just quit" doing it · Feel compelled to solve the problem for her Pick a place that is free of distraction, that is private and that is comfortable. It is best to catch your friend somewhat off guard. If she knows you plan to discuss her eating disorder, her defenses will kick in full force. Find out your friend's schedule. Make sure that you will have several hours free in case she is willing to confide in you. You don't want to open the issue and then have to leave pre­maturely because of some commitment. DO: · Listen to her with understanding · Appreciate her openness and her trust in sharing with you her distress · Learn more about eating disorders · Support and be available · Give her hope that with help and with determination she can free herself from this disorder · Give her literature about eating disorders · · Collect information about anorexia nervosa and bulimia and about places at UNI or in the community where your friend could get help. Get support from others Your friend will be most likely to seek help if a number of people express concern. She can not as easily discount what several people have observed. Talk to others who are also worried. Talk to a professional who can assist you in helping your friend. · Rehearse what you plan to say This is very important. Before you approach your friend with your concerns, prepare for what you will say, how you will say it, and how you will respond if your friend is defensive, denies the problem, or leaves the room. Tell her how you feel about this problem. "I'm frightened. I care about you and this is upsetting me a great deal. Eating disorders are very serious." · · In a caring, nonjudgmental way, tell the person what you have observed that concerns you. Use specific examples. For example: ü I've noticed that you eat extremely small portions at meal time. ü You've lost a great deal of weight recently. ü You're losing your hair. ü You look pale and have been sick so often this semester. ü I hear you purging when you use the restroom. ü You have been moody and depressed. ü You often express that you feel fat, but you are actually frighteningly thin. If your friend agrees to seek help, you will want to make referrals immediately. Call the Counseling Center right away to schedule an appointment, 273­2676. · Use "I" statements "Jenny, I need to talk to you because I'm really concerned about some things I've seen." Expressing Concern to Someone with an Eating Disorder · Choose a time and a place carefully. Reassure her that you support her and are available for your friend. "Anytime you need to talk, I'll listen." 17 University of Northern Iowa Emotional and Mental Health Concerns How to Refer a Student to the Counseling Center: The Counseling Center provides individual counseling, group counseling, couples counseling, crisis counseling, consultation, and outreach programs for currently enrolled UNI students. Services are free of charge. The Counseling Center is located in 213 East Bartlett and the hours are 8:00 a.m. to 4:45 p.m., Monday through Friday. In many cases, it may be sufficient to tell the student that free, confidential counseling is available from licensed psychologists and mental health counselors. Encourage the student to visit the Counseling Center so he or she can complete the brief initial paperwork and be scheduled to meet with a counselor as soon as possible. When to Refer a Student to the Counseling Center: If the student is reluctant to seek counseling, it may help if you explore his or her concerns about counseling. Many times fears about seeking help may be overcome with accurate information. In some situations a student may be more willing to come to the Counseling Center if you or a trusted friend accompanies them. Students may also call the Counseling Center to ask questions about our services. As with many of life's problems, earlier intervention is often better. A person, who receives appropriate help sooner, rather than later, may be less likely to experience more severe symptoms or problems. Students should be referred for counseling if they are exhibiting significant symptoms of depression, suicide, substance abuse, or other serious mental disorders. Symptoms could be considered "significant" if they cause some impairment in a student's daily functioning. To read more about some of the common mental health problems college students face, visit the Counseling Center's Helpful Websites page (www.uni.edu/counseling/links.html). If you believe that it is an urgent situation, call the Counseling Center at 273­2676 and we will consult with you about what to do. In most cases, we will recommend that you send or bring the student to the Counseling Center to meet with an on­duty crisis counselor. With any counseling situation, contact your coordinator immediately. They can help with the referral and also work closely with you so that you do not need to go it alone. Students could also benefit from counseling if they are having difficulty coping with a loss (e.g., death or relationship breakup), if they have experienced a traumatic incident (e.g., assault or accident), if they have experienced a significant stressor, or whenever emotional difficulties interfere with daily functioning. About Counseling and Confidentiality: Mental Health Counseling is confidential and we cannot legally or ethically release information about a student to anyone without his or her permission (with certain legally granted exceptions). If you would like us to confirm that a student has come to the Counseling Center, we recommend that you contact us by phone and inform our staff that you are referring a student and we will ask the student for permission to communicate with you. 18 University of Northern Iowa ü "That sounds like a lot for one person to take; has it made you think about killing yourself to escape?" ü "Has all your pain made you think about hurting yourself?" Guidelines for Responding to Emotional Crises/Suicide Stress is a major factor in the lives of nearly all college students, though most find a way out of their own crises. Suicide attempts are at the end of a continuum of emotional stress and usually indicate that a person isn't coping, often as a result of some event or series of events they find overwhelmingly traumatic. Here are some answers to the most frequently asked questions about suicide: 4. What sort of things can contribute to someone feeling suicidal? Risk factors include: Significant changes or losses in: ü relationships ü well­being of self or family member ü body image ü job, school, home ü financial situation 1. Why do people attempt suicide? Suicide attempts generally occur when a person's coping mechanisms have broken down, when they have run out of emotional energy and are desperately looking for any remaining avenues to control an unbearable level of pain. It is often a cry for help, as a person contemplating suicide is often so distressed that they are unable to see that they have other options. Most suicidal people give warning signs in the hope that they will be rescued, because they are intent on stopping their pain­­not on dying. Perceived abuse: ü physical ü emotional/psychological ü sexual ü social 5. How could I know if someone near me was contemplating suicide? About 80% of the time suicidal people give warning signs, usually in clusters, and often in the hope that they will be rescued. Typical warning signs include: ü withdrawing from friends/family ü loss of interest in usual activities ü signs of sadness, hopelessness, or irritability ü changes in appetite, weight, behaviors, or sleep patterns ü loss of energy ü frequent negative self talk ü talking, writing, or joking about suicide ü giving away possessions 2. Aren't all suicidal people crazy? No. Acutely distressed, but not crazy. The majority of individuals who commit suicide do NOT have a diagnosable mental illness. They are people just like you and me who at a particular time are feeling isolated, desperately unhappy and alone. 3. Doesn't talking about suicide encourage it? It depends on what you talk about. Talking exclusively about how to commit suicide can give ideas to people who hadn't yet thought of a plan. On the other hand talking about the feelings surrounding suicide promotes understanding and can greatly help reduce the distress the suicidal person is feeling. In particular, it is good to ask someone directly if they are considering suicide if you suspect they are. Here are some possible approaches: **Do not be thrown off track by a sudden change from extreme depressed behaviors to happy­go­lucky ones, as this change may only indicate the peace of mind which has come because the person has definitely decided to kill him/herself. If a person is highly disturbed, has formed a potentially lethal plan and has the means available to carry this plan out immediately, they should be considered a high risk of suicide. ü "Are you feeling so bad that you're considering suicide?" 19 University of Northern Iowa IMPORTANT PHONE NUMBERS 6. So what can I do to help? · · · · Suicidal people, like all of us, need love, understanding and care. If someone you know tells you they feel suicidal, above all, listen to them. Then listen some more. Tell them "I don't want you to die." Try to form a no­suicide contract: ask them to promise you they won't attempt to hurt themselves unless they contact either you or someone else who can support them. Emergency ­ Ambulance Fire Police 9­911 Allen Urgent Care ­ (Ridgeway) 833­5888 ­ (Off Greenhill Rd) 553­0828 Covenant Nurse On Call 272­2600 Take them seriously and refer them to someone in the Counseling Center (273­ 2676) equipped to help most effectively. Don't try to rescue them or handle the situation on your own, and remember that while you can continue to support them what happens is ultimately their responsibility. Counseling Center 273­2676 If the crisis happens in the middle of the night, as it so often does, you can consult with your Hall Coordinator, someone on the Counseling staff by calling the University Police Office 273­2712, or you can give the student the Crisis Line number 233­8484 so they can reach someone 24 hours a day if they need to. Hospitals: Crisis Line 1­800­332­4224 Health Aide Coordinator 273­2198 Health Center 273­2009 Allen Hospital Covenant Medical Center Sartori Hospital 235­3941 272­8000 268­3000 Poison Information 1­800­352­2222 Substance Abuse/Sexual Abuse Education Office 273­2137 20 University Police 273­2712 273­4000 Wellness Resource Lab 273­6119 WRS 273­6275