Tracer Record Review - Periop Only 3-21-2016
advertisement
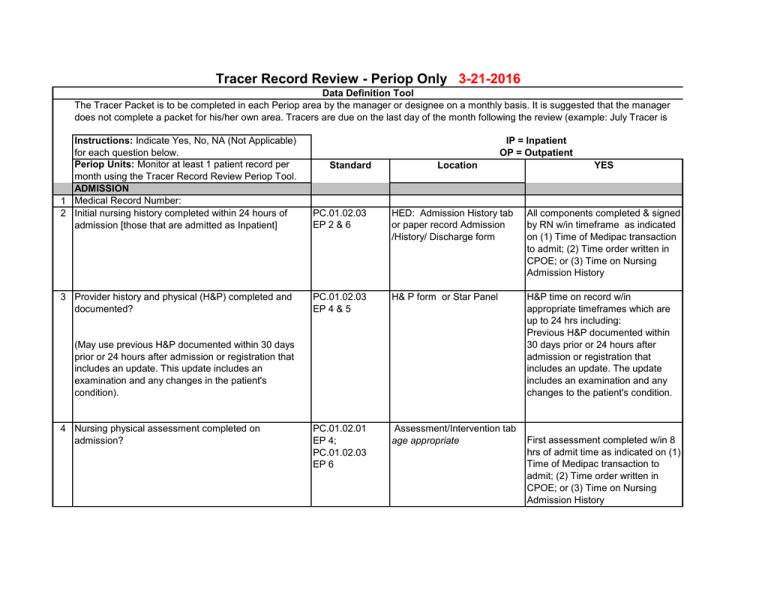
Tracer Record Review - Periop Only 3-21-2016 Data Definition Tool The Tracer Packet is to be completed in each Periop area by the manager or designee on a monthly basis. It is suggested that the manager does not complete a packet for his/her own area. Tracers are due on the last day of the month following the review (example: July Tracer is IP = Inpatient OP = Outpatient Instructions: Indicate Yes, No, NA (Not Applicable) for each question below. Periop Units: Monitor at least 1 patient record per month using the Tracer Record Review Periop Tool. ADMISSION 1 Medical Record Number: 2 Initial nursing history completed within 24 hours of admission [those that are admitted as Inpatient] PC.01.02.03 EP 2 & 6 HED: Admission History tab or paper record Admission /History/ Discharge form All components completed & signed by RN w/in timeframe as indicated on (1) Time of Medipac transaction to admit; (2) Time order written in CPOE; or (3) Time on Nursing Admission History 3 Provider history and physical (H&P) completed and documented? PC.01.02.03 EP 4 & 5 H& P form or Star Panel H&P time on record w/in appropriate timeframes which are up to 24 hrs including: Previous H&P documented within 30 days prior or 24 hours after admission or registration that includes an update. The update includes an examination and any changes to the patient's condition. PC.01.02.01 EP 4; PC.01.02.03 EP 6 Assessment/Intervention tab age appropriate Standard Location (May use previous H&P documented within 30 days prior or 24 hours after admission or registration that includes an update. This update includes an examination and any changes in the patient's condition). 4 Nursing physical assessment completed on admission? YES First assessment completed w/in 8 hrs of admit time as indicated on (1) Time of Medipac transaction to admit; (2) Time order written in CPOE; or (3) Time on Nursing Admission History 5 Functional screen complete PC.01.02.01 EP 4; PC.01.02.03 EP 8 1) Admission History StarForm in StarPanel for units that chart in HED (nurseries do not complete Functional Screen on newborns); 2) paper admission history if completed in area that does not document in HED(IP) VMG Clinic Intake Form (OP) Functional Screen complete within 24 hours(IP). Activities of Daily Living Section completed (OP) 6 If functional screen positive, plans for follow-up documented PC.01.02.01 EP4; Admission History tab (IP); VMG Assesssment & Followup for Positive Intake Screen (OP) in PT, OT, ST sections. 7 Nutritional screen complete PC.01.02.01 EP 4; PC.01.02.03 EP 7 PC.01.02.01 EP 4; PC.01.02.03 EP 7 PC.01.02.07 EP 1 & 2 Admission History/Discharge Plan (IP); VMG Clinic Intake Form (OP) Positive screen & provider contacted, MD notified documented as free text note (IP), Positive Screen follow-up documented on form (OP). NA = negative screen or preexisting condition (i.e, blind, Cerebral Palsy, or ADHD) Nutritional screen 8 hours (IP) Nutrition Screen completed (OP) 8 If nutritional screen positive, plans for follow-up documented (OP Only) 9 Pain screen complete 10 If pain screen positive, plans for follow-up documented PC.01.02.01 EP 23; PC.01.02.07 EP 3 VMG Assesssment & Followup for Postive Intake Screen (OP) (OP only) Positive screen follow up documented on form ; or negative screen = NA Nursing Assessment in HED (IP); VMG Clinic Intake Form (OP) Nursing Assessment in HED (IP); VMG Assesssment & Follow-up for Postive Intake Screen (OP) Pain screen completed within 8 hours (IP) Pain screen completed (OP). Positive screen (score ≥4) follow up of section of initial screen completed (IP); Positive screen (Option 3 and score >3) follow up documented on form (OP); or negative screen = NA (IP, OP) 11 Abuse screen complete PC.01.02.09 EP4 12 If abuse screen positive, plans for follow-up documented PC.01.02.09 EP 5, 6, & 7 13 Falls screen complete PC.01.02.08 EP 1 14 If falls screen positive, plans for follow-up documented PC.01.02.08 EP 2 15 Preferred language for discussing health care PC.02.01.21 documented. EP 1 16 Learning needs/education screen complete PC.02.03.01 EP 1, 4, & 5 17 If education screen positive, plans for follow-up documented (OP only) PC.02.03.01 EP 10 18 Discharge planning initiated within 24 hours of admission (IP only) PC.04.01.03 EP1 ADVANCE DIRECTIVES (IP Only) 19 Advance Directives Progress Notes (MC#4137) signed RC.02.01.01 and completed EP 4 RI.01.05.01 EP 9 Admission History age appropriate tab (IP); VMG Clinic Intake Form (OP) Admission History age appropriate tab (IP); VMG Assesssment & Follow-up for Postive Intake Screen (OP) VMG Assessment & Followup. VMG Assessment & Followup. In admission history Social Work screen completed (IP); Social Environment screen completed ( OP) Positive screen & check in "social work ordered" box (IP); positive screen follow up documented on form (OP); or negative screen = NA (IP, OP) Falls screen completed for pts >/= 65 yrs. (OP) Positive screen follow-up documented on form. (OP) Documented Learning needs completed within 8 Admission History tab (IP); VMG Clinic Intake Form (OP) hours (IP); Educational screen completed (OP) VMG Assessment & Follow- Positive screen follow-up documented on form or negative up screen = NA Plan of Care Plan initiated w/in timeframe or Case Management & Socical Work screen negataive Advance Directives Progress Notes and HED Admission / History Extended Data (both completed) Both Advance Directives Progress Notes form and HED data completed to be Yes. 20 Copy in chart or substance of directive in physician's progress notes or on Advance Directives Progress Notes (MC#4137)? PLAN OF CARE (IP Only) 21 Perioperative Services Plan of Care is completed and present in the patient record? NURSING ASSESSMENT (IP Only) 22 Physical assessment per shift or unit standard RI.01.05.01 EP 9 & 11 Clear plastic advance directive sleeve at the front of the chart (1st item) or on Advance Directives Progress Notes or physician progress notes or scanned in star panel under legal documents and in HED Adm/History extended data Choice of: -Copy present or directive signed by physician OR - Copy in STAR Panel from previous admission under "ALL" and then "legal Documents" OR - Answer "NA" if patient has no Advance Directive PC.01.03.01 EP 1 VPIMS Plan of Care completed PC.01.02.01 EP 23; PC.01.02.03 EP 3 Assessment/Intervention age appropriate tab 24 Pain assessment at least every shift; when there is a change in patient condition or primary caregiver. PC.01.02.07 EP 1 Date, nurse signatuare & title, time and initials are documented and check mark placed beside "Standards Met" or "Except as Noted" for each section. Assessment/Intervention age Date, nurse signatuare & title, time and initials are documented and appropriate tab check mark placed beside "Standards Met" or "Except as Noted" for each section. Assessment/ Intervention age Time, Date, Pain Score/indicators appropriate or Pain tab are documented 25 Interventions r/t pain management are documented PC.01.02.07 EP 4 Assessment/Intervention age appropriate tab or Pain tab 26 Pain is reassessed after administration of pain med/comfort measures PC.01.02.07 EP3 Assessment/Intervention age Interventions, date time, pain score, appropriate tab or pain tab and initials are documented within 2 and/or Controlled Drug Record hrs of intervention. Exception: PCA or continuous infusion IV analgesia assessment documented every 4 hrs. 23 Each patient is reassessed as necessary based on his PC.01.02.03 or her plan for care or changes in his or her condition. EP3 Interventions, date, time, initials are documented. PATIENT EDUCATION 27 Pain management addressed, as appropriate (IP only) 28 All "teaching/education" fields complete, as appropriate (excluding pain management) PC.02.03.01 EP 10 PC.02.03.01 EP 10 Education Record "other" 29 Documentation by all disciplines involved in the patient's care, treatment, or services? MEDICATION ADMINISTRATION 30 "Do Not Use" Abbreviations are NOT found in the MR on date of service? PC.02.03.01 EP 5 Same as above. Paper and individual discipline notes IM.02.02.01 EP 3 All entries in the medical No " Do Not Use" abbreviations are record on date of review found in the medical record on the including medication orders, date of review. MAR, problem list, flowsheets, progress notes,etc. 31 Supporting documentation (diagnosis, condition, or indication for use) for every order for "current" medications. MM.04.01.01 EP 9 Physician orders, H&P, progress notes RI.01.03.01 EP 13 RI.01.03.01 EP 13 PC.01.02.03 EP 5 Consent Form Consent form/ Anesthesia Care Record H& P form OPERATIVE & OTHER PROCEDURES 32 Consent form present and signed, dated, and timed. 33 Type of sedation/anesthesia included on consent form? 34 Provider history and physical (H&P) completed and documented prior to procedure? (May use previous H&P documented within 30 days prior or 24 hours after admission or registration that includes an update. The update includes an examination and any changes to the patient's condition) Education Record "other" All teaching fields specific to pain are completed. All teaching fields are appropriately completed except pain management teaching. Signature(s) & initials are present for appropriate disciplines. Diagnosis, condition or indications for use are documented anywhere in the medical record including the H&P consent form present and signed, dated and timed Type of sedation/anesthesia consent is documented H&P on record prior to procedure/ surgery and w/in appropriate timeframes: 35 Pre-procedural education documented before operative or high-risk procedures or before moderate or deep sedation or anesthesia. 36 Patient's condition is re-evaluated before administering moderate or deep sedation. PC.03.01.03 EP 4 37 "Time Out" documented before procedure. UP.01.03.01 EP 5 PC.03.01.03 EP 8 38 Immediate Post Operative/procedural Note is present RC.02.01.03 EP 7 and includes the following: 1. Name of surgeon, proceduralist and assistants; 2. Procedure(s) performed and description of the procedure; 3. Findings 4. Estimated blood loss; 5. Specimen(s) removed, if any. 6. Postoperative diagnosis; Documented Sedation & Analgesia Record, ASA class and Pre-Sedation Status Anesthesia record completed for moderate or deep sedation. For OR area Anesthesia Care Record ASA score prior to induction completed. Area Specific documentation systems. Sedation/ Analgesia Completed including date and time. form. Post surgical progress notes All elements are documented in the record before the patient moves to the next level of care irregardless of physical location. NA=Operative/Procedural report completed before the patient is transferred to the next level of care or if the proceduralist accompanies the patient from the procedure room to the next level of care, the note can be written in that unit or area of care. 39 The Operative/Procedural report is dictated or electronically entered in the pt record within 24 hrs of the procedure and includes: 1. Patient’s name and medical record number; 2. Date of procedure; 3. Name of surgeon, proceduralists and assistants; 4. Pre-operative diagnosis, 5. Postoperative diagnosis; 6. Anesthetic agent used; 7. Description of the techniques and procedure; 8. Description of the findings; 9. Estimated blood loss; 7. Specimen(s) removed, if any; 8. Any laboratory or diagnostic procedure ordered; 9. Complications, if any; 10. Condition of patient. RC.02.01.03 EP 5, 6 & 7 Surgical / procedure Report All elements are documented in the report and dictated or electronically entered within 24 hours of the procedure. The attending physician has signed the report within 14 days of the procedure. 40 For operative or high-risk procedures and/or the administration of moderate or deep sedation or anesthesia, patients are discharged from recovery area by LIP or by criteria. (Procedural Areas) 41 Discharge instructions form present and complete (Outpatient areas) 42 Patients who receive sedation or anesthesia are discharged in the company of an individual who accepts responsibility for the patient. PC.03.01.07 EP 4 Discharge Criteria documentation Discharge criteria documented PC.04.01.05 need EP PC.03.01.07 EP 6 Discharge instruction form Form completed, dated, and timed. CMS.482.51.(b) Wiz or paper Patient Discharge Instructions or discharge letters per specialty Form completed, dated, and timed.