Implementation of Delirium Monitoring in the PACU
advertisement

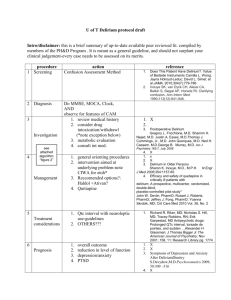
Implementation of Delirium Monitoring in the PACU Elizabeth Card, RN, CPAN, CCRP; Christine Tomes RN; Jeannie M. Wood, RN, BSN; Cathy Lee RN, CPAN, CAPA ; Lisa M. Allen, RN, BSN, CCRN; Lindsay R. Kellum RN, BS; Donna Nelson, RN, CAPA; Pratik Pandharipande, MD, MSCI PROCEDURE OF IMPLEMENTATION Background • Delirium is an acute brain organ dysfunction and is associated with poor clinical outcomes. Delirium is a state of acute changes/fluctuation in a patient’s consciousness, accompanied by inattention, disorganized thinking, or perceptual disturbances in thinking. • In prior studies, prevalence of delirium has been reported between 16 to 80% depending on patient population (see figure 1). In these studies, delirium has been shown to be associated with longer hospital stays, readmissions, poor cognitive and functional outcomes, and increased mortality. • Risk factors caused fall into two major categories: patient related factors (e.g. age, previous dementia, diabetes, etc.) or iatrogenic risk factors (e.g. psychoactive medications, hypoxemia, length of surgery >3 hours, etc.). Of note, benzodiazepines and opiates have been associated with development of delirium the post-surgical population. • The CAM-ICU allows for the rapid diagnosis of delirium by bedside nurses and has been used in several research studies to detect the prevalence of and risk factors for delirium in ICU. A tool was developed adapting the steps of the CAM-ICU for use in the PACU (figure 2). • Recognition of the prevalence of emergence and post-operative delirium in the adult population, during the recovery period. OBJECTIVES • To assess PACU staff knowledge of delirium • To educate staff increasing awareness of the risk factors, complications, and current recommended treatments for delirium • To educate PACU nurses how to use the CAM-ICU to detect delirium in their patients. • To detect the prevalence and risk factors for delirium in the PACU using the CAM-ICU DEPARTMENT OF ANESTHESIOLOGY • IRB approval was obtained for the study , this approval allowed for waiver of consent. • The CAM-ICU tool was adapted for use in the PACU setting. Worksheets and checklists were also developed for use with the study. • Bedside sub-investigator nurses received certification in CITI training, • (Good Clinical Practice) as well as training in the use of the CAM-ICU. • A pre-training anonymous survey on delirium was given to all nurses in the MAIN and MCE PACUs to assess baseline knowledge. • In-services, training manuals, and videos were used to educate all of the staff on risk factors, complications, and treatment recommendations for delirium. • Due to the waiver of consent, the bedside nurse sub-investigator were able to assess and collect de-identified data on all of their patients. • Nurse champions were trained in use of the CAM-ICU, and served as experts along with the sub-investigators in their PACUs, training all remaining bedside nurses in the use of the CAM-ICU tool. • The CAM-ICU and RASS were subsequently added to the electronic charting system (VPIMS). Figure 2, PACU CAM-ICU tool PRELIMINARY RESULTS A post-training survey will be collected once the training of the PACU staff on the CAM-ICU tool is complete. At the time of this submission, 227 subjects had been entered into the Red Cap data base. Of these 72 have experienced delirium as detected by the CAM-ICU tool, while in the PACU. This is roughly 26% of the study population. The need for the use of the PACU CAM-ICU tool for detection of delirium, has been recognized from the pre-education survey and through put the education and implementation process IMPLEMENTATION AND FUTURE RESEARCH NEEDS • Training of all PACU staff currently being completed. Post-training Prevalence of Delirium 80% 70% • 60% 50% 40% 30% 20% 10% 0% Ventilated ICU Patients Post Operative Hip Surgery Coronary artery bypass grafting (CABG) General Surgery Figure 1, prevalence of delirium in patient populations survey will be given again. Data will be analyzed from bedside sub-investigators for the prevalence of and risk factors for emergence and post-operative delirium. Additional areas which could benefit Endoscopy lab, Interventional, Radiology Recovery Room, cardiac cath lab. Further research is needed to identify risk factors and treatments. References: • Ely, E.W., Margolin, R., Francis, J., & et al. (2001). Evaluation of delirium in critically ill patients: validation of the Confusion Assessment Method for the Intensive Care Unit (CAM-ICU). Crit Care Med.;29(7):1370-1379. • Pandeharipande, P.; Cotton, B.; Shintani, A.; Thompson, J.; Pun, B.; Morris, J.; Dittus, R.; & Ely, W. (2008). Prevalence and risk factors for developing delrium in surgical and trauma intensive care patients. The Journal of Trauma, Injury, Infection, and Critical Care. 65, 34-41.