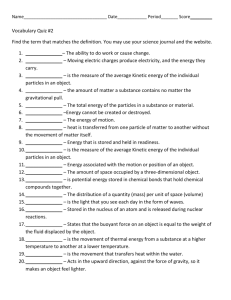
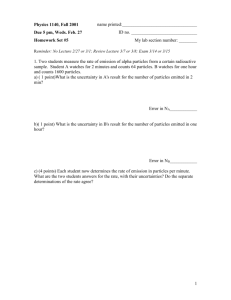
Document 13612263
advertisement

Massach usetts Massachu setts Ins Institute of Technolo Technology Harva Harvarrd Me Medical dical School hool Brig ham m an Brigha and Women men’s Ho Hospital VA Bo thca are Sy Boston Heal Healthc System 2.782J/3.961J/BEH.451J/HST524J BIOCOMPATIBILITY: LOCAL AND SYSTEMIC EFFECTS M. Spector, Ph.D BIOMATERIALS-TISSUE INTERACTIONS BIOMATERIAL TISSUE Strength Modulu ticitty Moduluss of Elas Elastici Fracture mechanic mechanicss 10nm 100 100nm 1µm 1 sec sec 1 da day Protein Adsorption Cell Response Response Ion Release Time Scale Scale 10 days 100 100 days days Tissue Remodeling Particles Particles Wear Metal Metal corr corrosion Polymer degradation degradation Length Scale Scale 10 µm 100 100 µm 1mm CellCell-cell cell interaction interactionss ECM pr proteins otein Cytokine Cytokines Eicosanoids Enzy Enzymes Page 1 BONE BIOMATERIALS-TISSUE INTERACTIONS: Tissue Response to Implant Breakdown IMPLANT Fracture Wear TISSUE RESPONSE Fibroblast Degradation: Fibrous Tissue (Cell Cont Contracti raction?) Bone Particles Macrophage Metal Corrosion Polymer Degradation Degradation Products/Ions Osteoclast RESPONSE TO IMPLANTS: WOUND HEALING Injury Mild Moderate/Severe Vascularized Tissue Non-vasc. Resolution (Inflammation) No Healing Reparative (Healing) Process Repair (Scar) Regeneration Page 2 RESPONSE TO IMPLANTS: WOUND HEALING Injury Mild Moderate/Severe Vascularized Tissue Non-vasc. Resolution (Inflammation) No 4 Ti Tissue Ca Categor tegoriies Healing Connecti ve Tissue Connectiv Reparative (Healing) Epithelium Epithelium Nerve Process Muscle Muscle Repair (Scar) Regeneration RESPONSE TO IMPLANTS: WOUND HEALING Injury Mild Moderate/Severe Vascularized Tissue Non-vasc. CT: Resolution (Inflammation) Art. Cart. rt. No 4 Ti Tissue Ca Categor tegoriies Healing Connecti ve Tissue Connectiv Reparative (Healing) Epithelium Epithelium Nerve Process Muscle Muscle CT: Derm Dermis, Lig. Lig. CT:Bone Mu: ., Card. Mu: SM SM Mu: Skel Skel., Card. Mu: Repair (Scar) Ep: Ep: Epidermi Epidermiss Regeneration Page 3 RESPONSE TO IMPLANTS: WOUND HEALING Injury Regeneration Repair Tissue of Labile and Stable Cells Tissue of Permanent Cells Framework* Framework* Framework Framework Intact Destroyed Scar Regeneration Scar * “Stroma ” Stroma” RESPONSE TO IMPLANTS: WOUND HEALING Surgical Implantation Acute Inflammation Inflammation Vascular Response Clotting Phagocytosis Neovasculariza Neovascularization New Collagen Synthesis Tissue of Labile and Stable Cells Inc. time Granulation Tissue Tissue of Perm Permanent anent Cells Cells Implant Implant Movement Movement Fram Framework Framework Framework Intact Destroyed Regen. Scarring Regen. (incorp. (fibrous encapsulation; incorp. encapsulation; of implant) synovium implant) novium) Chronic Inflammat Inflammation Page 4 Scarring (fibrous encapsulation; synovium) synovium) Chronic Inflammation Inflammation I. Metchnikoff First identified “macrophages” and “microphages” (polymorphonuclear neutrophils, PMNs) in an organism around a foreign body I. Metchnikoff Page 5 In 1923 a piece of glass was removed from a patient’s back; it had been there for a year. It was surrounded by a minimal amount of fibrous tissue, lined by a glistening synovial sac, containing a few drops of clear yellow fluid. Photo removed due to copyright restrictions. Smith-Peterson J. Bone Jt. Surg., 30-B:59 (1948) Diagrams removed due to copyright restrictions. I. Silver Page 6 Synovium: Macrophage-like (Type A) and Fibroblast-like (Type B) Cells Photo removed due to copyright restrictions. Tissue response to a cylindrical implant of polysulfone in lapine skeletal muscle, 2 yrs. post-op Fibrous tissue Photo removed due to copyright restrictions. Skeletal muscle Page 7 Polyethylene implant, 6 mos. post-op Polyethylene Photo removed due to copyright restrictions. MΦ MFBGC Polyethylene Porous Coated Co-Cr Tibial Component (retrieved 1 yr. post-op) Photo removed due to copyright restrictions. Page 8 RESPONSE TO IMPLANTS: WOUND HEALING Surgical Implantation Acute Inflammation Inflammation Vascular Response Clotting Phagocytosis Neovasculariza Neovascularization New Collagen Synthesis Tissue of Labile and Stable Cells Inc. time Granulation Tissue Tissue of Perm Permanent anent Cells Cells Implant Implant Movement Movement Fram Framework Framework Framework Intact Destroyed Regen. Scarring* Regen. Scarring* (incorp. (fibrous encapsulation; incorp. encapsulation; of implant) synovium implant) novium) Chronic Inflammat Inflammation Page 9 Scar* Scar* (fibrous encapsulation; synovium) synovium) Chronic Inflammation Inflammation * Inc ion Including uding cont contract raction FIBROBLAST BEHAVIOR IN FIBROUS TISSUE AROUND IMPLANTS • Proliferation and increased matrix synthesis of fibroblasts leads to an increase in the thickness and density of the scar tissue. • Fibroblast contraction results in scar contracture. BREAST IMPLANTS Capsular Contracture Photo removed due to copyright restrictions. Photograph shows Grade IV capsular contracture in the right breast of a 29year-old woman seven years after subglandular (on top of the muscle and under the breast glands) placement of 560cc silicone gel-filled breast implants. http://www. impllantforu m.com/capsular /capsular--cont http://www.imp antforum.com contracture/ racture/ BREAST IMPLANTS Capsular Contracture What is Caps Capsular Contra Contracture? Scar tissu nd the implan tissuee that that form forms arou around implantt which causes the brea breasts to harden (simila le feels like) imilarr to what what a cont contrracted musc muscle like) as the the natura aturallly formi ng scar nd th formin scar ti tissue arou around the impla plant tigh tightens tens and squ squeezes eezes it. Whil While capsul ar co ble complication, it is al capsular contract ntracture is is an unpredicta unpredictable also the most common licat atio ion n of breast augmentat mmon comp complic entatiion. How can Caps nted? Capsular ular Cont Contracture be preve preven ted? Textured Textured implants plants help dete deterr contra contracture because of thei their rough surface which is in age a ha intend tended to discour discourage hard ca capsule from from form forming. ing. Under the muscle (sub -pecttoral al sub musccular') (sub-pec oral or 'p 'parti artia sub--mus ular') placement of the implan es risk implantt reduc reduces risk of ca capsular psular contra contracture by an avera average of 8 - 10%. 10%. Whereas over the muscle (in -mamm mmar ary' y')) has (in front front of the muscle or 'sub 'sub-ma has 10 - 25% or more more chance of ca capsule contra contracture. CAUSE OF CAPSULAR CONTRACTION Myofibroblasts, and the regulatory protein TGF-β, were found in the contracted capsules around silicone breast implants but not in non-contracted capsules. Mature skin scar tissue did not contain TGF-β or myofibroblasts. Lossing C, and Hansson HA, Plast Recons Reconstr Surg Surg 91:1277 (1993) (1993) Page 12 α-smooth muscle actin-fusion peptide (SMA-FP) inhibits the tension exerted by lung fibroblasts on silicone substrates. After washing our of the FP, cells contract again. Video removed due to copyright restrictions. Hinz B, et al., J Cell Biol 157:657 (2002) http://www. implan lantforu tforum.com m.com/capsular /capsular--cont http://www.imp contracture/ racture/ BREAST IMPLANTS Capsular Contracture How can Capsul ar Cont nted? ? Capsular Contracture be preve prevented Massage Massage and or compressi ression. This is usually usually only only done with smooth mooth implants implants and may be suggested ggested for a period period between between a few few weeks to to as long long as you have your implants. plants. Do not ma massage bruises bruises! The "no-touc h" techni od includes ulousl sly y "no-touch" technique. que. This meth method ncludes metic meticulou rewashi ng surg re handl rewashin surgical glove glovess befo before ndling any any instrument rument and and implan ts.. Only t, using a unique implants Only the head surg surgeon touches touches the implan implant, unique Teflon Teflon cutting cutting boar board and im immedi mediately inserting inserting the implan plantt undernea ures help underneath the muscle. All of these meas measures help en ensure that no foreign subs tance attach themsel ves to the implant, substance themselv implant, which which could inflame inflame the surrounding tiss tissue and cause complicatio mplications su such as capsul ar co capsular contract ntracture. Page 13 Chondrocytes (P2 Canine) in a Type I Collagen-GAG Matrix: Contraction Photo removed due to copyright restrictions. 40 min B Kinner Page 14 Non-Seeded: 8 days Cell-Seeded: 8 days Photo removed due to copyright restrictions. 21 days Non-Seeded and Cell-Seeded Collagen-GAG Scaffolds S. Vickers Human Articular Chondrocytes in Monolayer Culture IH - Green: α-smooth muscle actin; Orange: type II collagen Photo removed due to copyright restrictions. Chondrocytes express the gene for α-smooth muscle actin and this enables them to contract B. Kinner, et al. JOR 2001;19:233 Page 15 MUSCULOSKELETAL CELLS THAT CAN EXPRESS α-SMOOTH MUSCLE ACTIN AND CAN CONTRACT • • • • • • • • Articular chondrocyte Osteoblast Meniscus fibroblast and fibrochondrocyte Intervertebral disc fibroblast and fibrochondrocyte Ligament fibroblast Tendon fibroblast Synovial cell M. Sp Spector ector, Mesenchymal stem cell Wound Repair Repair Regen. Regen. 9:119:11-18 (2001) POSSIBLE ROLES FOR α-SMOOTH MUSCLE ACTIN-ENABLED CONTRACTION Musculoskeletal Connective Tissue Cells • Tissue engineering Contracture of scaffolds • Healing Closure of wounds (skin wounds and bone fractures) • Disease processes Contracture (Dupuytren’s) • Tissue formation Modeling of ECM architecture and remodeling (e.g., crimp in ligament/tendon?) Page 16 IMPLANT MATERIALS/BIOMATERIALS TISSUE RESPONSE Soft Tissue (that does not regenerate) • Fibrous capsule (scar) Synovium: fibrous tissue interspersed with macrophages Wound healing response of repair (scar formation) coupled with macrophage accretion at the “dead space” - chronic inflammation Bone • Tissue integration and tissue bonding TISSUE INTEGRATION TISSUE BONDING • Tissue Integration (Oss (Osseointegr eointegration) Apposition of tissue (bone) to the implant (con (contact of bone wi with the surface but not necessarily bonding) Regeneration of tissue up to the surface of the implant • Tissue Bond Bonding (Bone Bonding) Chemical bonding of tissue (viz ., bo (viz., bone) to the surface Protein adsorption and cell adhesion Biomaterials: calcium phosphates and and titanium (?) Page 17 Photos removed due to copyright restrictions. Why Whyare arethere thereno nomacrophages macrophages on onthe thesurface surfaceofofthe theimplant? implant? Hydroxyapatite-Coated Implants Photos removed due to copyright restrictions. Page 18 Plasma-Sprayed Hydroxyapatite Coating Photos removed due to copyright restrictions. Photos removed due to copyright restrictions. Plasma-sprayed HA coating on a canine femoral stem, 6 mos. post-opc Page 19 Photos removed due to copyright restrictions. PROGRESSION OF OSTEOLYSIS: “HYLAMER” CUP Photos removed due to copyright restrictions. Page 20 J. Charnley, 1979 Photos removed due to copyright restrictions. Titanium Wear Debris Co-Cr Particles Photos removed due to copyright restrictions. Page 21 MACROPHAGE RESPONSE TO MOTION AND PARTICLES UNSTABLE PROSTHESIS Motion Particles Oste obla asts Osteobl Bone Resorption (Osteolysis) BONE Enz Enzymes PGE2 ILIL-1 Macrophage (15(15-25µ 25µm) Chemoattractants Chemoattractants Oste ocla ast Osteocl precursor precursor cell cells Oste ocla ast Osteocl POLYETHYLENE WEAR PARTICLES H. McKellop, 1994 Hip Society The number of particles generated by a hip prosthesis 7 x 1011 particles/yr. 700,000 particles/step Page 22 NUMBER OF INHALED PARTICLES Avg. particle burden of urban atmosphere: 105 particles/liter Respired volume in man = 1 liter/min. Therefore, 105 particles are inhaled/min. 10% of the inhaled particles are deposited in the lungs. Therefore, 104 particles are deposited in the lungs per min. 5 x 109 particles/yr. RESPONSE TO PARTICLES • Type of material • Size – mm, µm, nm • Location – Joint fluid – PeriPeri-prosthetic prosthetic tissues – Synovium – Lymphatic system • Number Page 23 RESPONSE TO PARTICLES • Size – mm No adverse response. – µm Able to be phagocytosed by macrophages; macrophages release molecules that stimulate bone resorption. – nm Sub-micrometer (nanoparticles) interfere with function of cell organelles; enter into the nucleus and interfere with genetic functions. Light Microscopy Polyethylene Particles in Peri-prosthetic Tissues Polyethylene Particles Nucleus in Peri-prosthetic Photos removed due to copyright restrictions. Tissues Transmission Electron Microscopy, TEM 1 µm Page 24 The total of 15 cemented and uncemented total hip replacement prostheses. 100 25 76% < 0.5µm 90 92% < 1.0 µm 80 70 60 15 50 40 10 Percentile Frequency (%) 20 30 20 5 10 0 0 0 .1 .2 .3 .4 .5 .6 .7 .8 .9 1 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.81.9 2.0 2.1 2.2 2.3 2.4 2.5 Benz E, et al., Biomat. 2001;22:2835 Particle Length (µm) The total of 3 total knee replacement prostheses. 16 100 43% < 0.5µm 90 80 12 72% < 1.0µm 10 70 60 8 50 6 40 4 30 20 2 10 0 0 .1 .2 .3 .4 .5 .6 .7 .8 .9 1 Benz E, et al., Biomat. 2001;22:2835 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 1.9 2.0 2.1 2.2 2.3 2.4 2.5 Particle Length (µm) Page 25 0 Percentile Frequency (%) 14 PARTICLE SIZE • A large percentage of polyethylene particles in periprosthetic tissues are of nanometer size – less than 200 nm • These nanometer size particles would go through the filters often used to capture particles from joint fluid – 200 nm diameter pores in the filter ISOLATION OF PARTICLES FROM JOI NT JOIN T FLUID Page 26 NANOPARTICLE TOXICITY • Particles from prostheses have become smaller (from micrometer to nanometer). • Introduction of nanotechnolgy into medicine (i.e., engineered nanoparticles for various applications) has raised questions about the biological response to nanoparticles. • Several federal agencies (NIH, EPA) are looking into this issue. • 2 major causes of death are cancer and heart disease; there are indications that nanoparticles can adversely contribute to these processes NANOPARTICLE TOXICITY “Nano's Troubled Waters:” Waters:” “Latest toxi toxic wa warning shows shows nanoparticles nanoparticles cause brain damage in aquatic species and highlights need for a moratoriu m on the release moratorium release of new nanomaterials. nanomaterials. • A new study revealing rbon molecules revealing that engineered ca carbon molecule cause brain damage in fish is one more brick in the wa wall of evidence suggesting that that manufactured manufactured nanoparticles nanoparticles are harmful to the environment and to health. health. • How many warnings do government regulator regulators require before they take ac action to ensure that that uses of nanoparticles are safe before wo workers in production production facilities are harmed and and before consumers are further exposed? ” http://online.sfsu.edu/~rone/Nanotech/nanobraindamage.htm Genotype; Thursday, 1 April 2004; www.etcgroup.org Page 27 RESPONSE TO PARTICLES • Type of material • Size – mm, µm, nm • Location – Joint fluid – PeriPeri-prosthetic prosthetic tissues – Synovium – Lymphatic system • Number LYMPHATIC SYSTEM • Filters out organisms and particles. • The lymphatic vessels are present wherever there are blood vessels. • More than 100 tiny, oval structures (called lymph nodes). – scattered all along the lymph vessels. – filter out particles • Particles that pass through the lymph node enter into the blood circulation. Page 28 Lymphadenopathy Photos removed due to copyright restrictions. Benz EB, et al., J. Bone Jt. Surg. 1996;78-A:588 Photos removed due to copyright restrictions. Benz EB, et al., J. Bone Jt. Surg. 1996;78-A:588 Page 31 SMALL PARTICLE DISEASE: LYMPHADENOPATHY • Enlargement of the node. • Particles drained from tissue by the lymphatic system are phagocytosed by macrophages in the nodes. • No adverse clinical sequelae yet noted, but can confound differential diagnosis of other diseases. • Concern about the clinical sequelae of nanoparticles that gain access to the vascular system. LOCAL AND SYSTEMIC RESPONSES SMALL PARTICLE DISEASE • Local Component Particle induced focal destruction of tissue around the imlant • Systemic Component Lymphadenopathy Page 32 BIOLOGICAL RESPONSE TO METAL DEBRIS • Immune responses PATIENT CONCERNS ABOUT METAL DEBRIS Am I allergic to my metal implant? Page 33 IMMUNE RESPONSE TO METAL IONS • "Metal allergy" has been incriminated as the cause of failure in certain patients. • However, results obtained to date are not definitive. METAL SENSITIVITY IN PATIENTS • 10-15% of population have dermal sensitivity to metal (14% to Ni) • Metal ions bind to proteins to form immunogenic complexes • Metals known as sensitizers: – Ni > Co and Cr >>> Ti and V • 60% of pts. with failed TJRs were metal sensitive vs. 25% with well-functioning implants – Did metal sensitivity cause failure or did the failed implant cause metal sensitivity? Halla b, Merritt, Hallab Merritt, Jacobs, JBJS JBJS 83-A:428 A:428 (2001) 2001) Page 34 METAL SENSITIVITY IN PATIENTS • “May exist as an extreme complication in only a few highly susceptible patients (< 1%), or it may be a more common subtle contributor to implant failure.” • “It is likely that cases involving implant-related metal sensitivity have been underreported because of the difficulty of diagnosis.” • Patients who have displayed sensitivity to metal jewelry are at higher risk. Halla b, Merritt, Hallab Merritt, Jacobs, JBJS JBJS 83-A:428 A:428 (2001) 2001) CELL RESPONSE TO METAL PARTICLES • • • • Macrophages in vitro Particles of Ti alloy not toxic; Co-Cr highly toxic Ti induced more release of PGE2 than Co-Cr Exp. to Ti increased the release of PGE2, IL-1, TNF, and IL-6; exp. to Co-Cr decreased release of PGE2 and IL-6 and had little effect on IL-1 and TNF • “release of Ti....worse than....Co-Cr” D.R. Haynes, et al al., JBJS 7575-A: 825 (1993) Page 35 CELL RESPONSE TO METAL PARTICLES • • • • Bovine articular chondrocytes Co was toxic to cells at all conc. At high conc. Cr, Ti, and Ti alloy were toxic At high conc. all metals decreased enzyme activity • PGE2 increased with conc., except for Ti alloy W.J. Malone Maloney, et al., J. Appl Appl.. Biomat. Biomat. 5: 109 (1994) BIOLOGICAL RESPONSE TO METAL PARTICLES AND IONS • • • Summary Metal particles and ions are released from TJR prostheses; the amounts can be reduced by careful design and manufacturing Cellular response to metal particles has some of the same elements as the response to particles of other materials No indication yet that metal particles and ions are responsible for profound adverse responses Page 36