1999 CSTE ANNUAL MEETING POSITION STATEMENT # ENV 4
advertisement

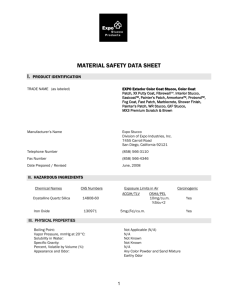
1999 CSTE ANNUAL MEETING POSITION STATEMENT # ENV 4 COMMITTEE: Environmental Committee TITLE: Silicosis Surveillance and Case Definition ISSUE: The U.S. Public Health Service’s Healthy People targets pneumoconiosis for prevention [USPHS 1998]. Among the various types of pneumoconioses, the occurrence of silicosis is most widely dispersed across the U.S. [NIOSH 1996]. It is estimated that more than one million U.S. workers are exposed to crystalline silica, and that 100,000 workers are exposed in high-risk occupations [USDOL and NIOSH 1997]. Since 1987, the National Institute for Occupational Safety and Health (NIOSH) has funded several states to develop approaches to silicosis surveillance and intervention using various data sources [Maxfield et al. 1997]. A standard silicosis surveillance case definition is needed to allow comparability of surveillance data. In 1996, CSTE adopted a position statement recommending that silicosis be reportable to the National Public Health Surveillance System (NPHSS) [CSTE 1996]. This position statement builds on that earlier CSTE position, providing more specific guidance to states on silicosis surveillance. POSITION TO BE ADOPTED: 1. The following silicosis indicators should be put under nationwide surveillance as part of the NPHSS: a) deaths (ICD-9 code 502); and b) hospital discharges (ICD-9-CM code 502). (Corresponding ICD-10 codes should be used when they replace ICD-9 codes.) 2) That, as resources permit and with consultation from NIOSH, states should: a) conduct more comprehensive silicosis surveillance, applying the adopted case definition/classification; and b) undertake follow-back investigations of selected cases to identify ongoing silica hazards that warrant preventive intervention. 3) That the adopted silicosis case definition should be published in the Morbidity and Mortality Weekly Report (MMWR) along with the other CSTE-approved noninfectious disease/condition surveillance definitions. BACKGROUND AND JUSTIFICATION: Clinical Description: Silicosis is an occupational lung disease caused by the inhalation of respirable dust containing crystalline silica. There are two forms of the disease: nodular silicosis and silicoproteinosis [ATS 1997]. Nodular silicosis is slowly progressing and manifests as scarring of the lung tissue. It is typically evident on chest x-ray only after 10 or more years of exposure (chronic silicosis), but may be seen after as little as five years (accelerated silicosis). Nodular silicosis may present without symptoms; shortness of breath and cough typically accompany advanced disease. Silicoproteinosis (acute silicosis), a less common form of silicosis, is an alveolar filling process which becomes evident within weeks to months after a very intense initial exposure; death usually occurs within a few years of onset. Except in acute silicosis, lung biopsy is rarely needed for diagnosis, as the radiologic picture is often sufficiently distinct to permit diagnosis of silicosis in persons with a clear history of exposure. Individuals with silicosis are at increased risk of tuberculosis and lung cancer. Silica exposure and/or silicosis has also been associated with autoimmune diseases such as lupus erythematosis, rheumatoid arthritis, scleroderma, and with glomerulonephritis. Silicosis is a progressive, incurable, and potentially fatal disease that can be effectively prevented by limiting exposure to respirable crystalline silica dust. Since 1987, NIOSH has funded several states to conduct silicosis surveillance and intervention. These states have demonstrated the utility of silicosis surveillance using death certificates, hospital discharge records, workers compensation claims, and physician reports [Maxfield et al. 1997]. The silicosis case definition provides uniform case classification criteria for silicosis cases identified from different sources. To help set priorities for preventive interventions (i.e., targeted educational outreach and training; selected workplace investigations to identify worksites with continuing problems of excessive worker exposure to silica; provision of recommendations for remediation; etc.), public health officials should collect additional clinical and workplace information on cases ascertained through surveillance. GOALS FOR SURVEILLANCE Describe the demographic and geographic distribution of silicosis Monitor trends Target preventive intervention at the state/local level (where resources permit) METHOD OF SURVEILLANCE State death certificate records State hospital discharge records State workers’ compensation claim records (where resources permit) Health care professionals’ reports of silicosis (where resources permit) SILICOSIS SURVEILLANCE DEFINITION: Case Classification Probable: Death certificate record listing ICD-9 code 502 (as underlying or contributing cause of death); or Hospital discharge record listing ICD-9-CM code 502 (as primary, secondary, or other diagnosis); or Workers’ compensation claim with a diagnosis of silicosis; or Health care professional’s report of an individual diagnosed with silicosis. (Corresponding ICD-10 codes should be used when they replace ICD-9 codes.) Confirmed: History of occupational exposure to airborne silica dust; and Chest radiograph (or other radiographic image, such as computed tomography) showing abnormalities interpreted as consistent with silicosis; or Lung histopathology consistent with silicosis. COMMENTS: This case definition was developed for public health surveillance purposes and should not be used as the sole criteria for establishing clinical diagnoses or eligibility for workers’ compensation. Since the confirmed category may be infrequently used in the face of limited resources, states are advised to combine the probable and confirmed cases to tabulate silicosis counts. To make appropriate interpretations/comparisons of the silicosis surveillance data, it is important for each state to clearly describe data source(s) used. States are encouraged to obtain work history and clinical information on ascertained cases to permit confirmation. Each record in the NPHSS silicosis surveillance database should include the case ascertainment source (i.e., death record or hospital discharge record, etc.), demographic and other relevant data from the administrative record, where available (e.g., age, sex, race/ethnicity, county of residence, industry and occupation, and whether the ICD code qualifying the case as “probable” or “possible” silicosis represents the underlying cause of death or a contributing cause of death (or the primary, secondary, or other diagnosis). If obtained during individual case follow-up, additional relevant data (e.g., case identification, case classification clinical criteria met, the years of silica exposure, and specifics on the job, worksite, and employer associated with the exposure to silica) should also be included or (if confidential) maintained in state files. Given the Healthy People 2000 and (draft) 2010 objectives to reduce pneumoconiosis mortality [USPHS 1998], states are encouraged to carry out silicosis surveillance as a component of pneumoconiosis surveillance, whereby data from death certificate records are summarized overall (i.e, for ICD codes 500 to 505, aggregated), as well as for each category of pneumoconiosis (i.e., for ICD codes, 500, 501, 502, 503, 504, and 505, separately). (Corresponding ICD-10 codes should be used when they replace ICD-9 codes.) Individual case follow-up of silicosis deaths occurring at younger ages is especially encouraged, as resources permit [CDC 1998]. Use of multiple case ascertainment sources, where resources permit, not only provides a more complete assessment of the occurrence of silicosis, but also offers the opportunity to estimate the total number of cases in the population using capture-recapture methods [Geidenberger and Socie 1997]. Additional Information: For additional information about silicosis, the SENSOR Program, and related issues, call 1-800-35-NIOSH or visit the NIOSH Internet site: http://www.cdc.gov/niosh/homepage.html. REFERENCES ATS (American Thoracic Society) [1997]: Adverse effects of crystalline silica exposure. Am J Respir Crit Care Med. 155:761-765. CDC (Centers for Disease Control and Prevention) [1998]: Silicosis deaths among young adults—United States, 1968-1994. Morb Mort Weekly Rept 47:331-335. CSTE (Council of State and Territorial Epidemiologists) [1996]: CSTE Position Statement #2: Adding silicosis as a reportable condition to the National Public Health Surveillance System. Environmental/Occupational/Injury Committee. Geidenberger C, Socie E. Use of capture-recapture methods to estimate the prevalence of silicosis in Ohio. Am J Epidem 145:S62. Maxfield R, Alo C, Reilly MJ, Rosenman K, et al. [1997] Surveillance for silicosis, 1993—Illinois, Michigan, New Jersey, North Carolina, Ohio, Texas, and Wisconsin. Morb Mort Weekly Rept 46(no SS-1):13-28. NIOSH (National Institute for Occupational Safety and Health) [1996]: Work-Related Lung Disease Surveillance Report, 1996. Cincinnati, OH: DHHS (NIOSH) publication no. 96-134. U.S. Department of Labor and NIOSH. [1996] A Guide to Working Safely with Silica. U.S. Public Health Service [1998]: Healthy People 2010 Objectives: Draft for Public Comment. September 15, 1998. (http://www.health.gov/healthypeople/2010Draft/object.htm) COORDINATION WITH OTHER AGENCIES: Agency for Response: Centers for Disease Control and Prevention Epidemiology Program Office (EPO) National Institute for Occupational Safety and Health (NIOSH) Agencies for Information: CSTE CONTACT: National Center for Health Statistics, NCHS Department of Labor (DOL), Occupational Safety and Health Administration, (OSHA) Department of Labor (DOL), Mine Safety and Health Administration (MSHA) Henry Anderson, MD Wisconsin Division of Health One W. Wilson Street Madison, WI 53703 Phone: 608-266-1253 Fax: 608-266-1253 E-mail: anderha@dhfs.state.wi.us Silicosis Surveillance and Case Definition: Terms Used APPENDIX Silica -- The chemical name of silica is silicon dioxide. It can be either crystalline or amorphous. Crystalline silica is fibrogenic In the lung (i.e., scar tissue develops in response to inhaled particles of crystalline silica that deposit in the alveolar region). Amorphous silica is thought to have low fibrogenic potential, but under conditions of high heat and pressure, amorphous silica can be converted into crystalline forms. There are three medically important forms of crystalline silica: quartz, tridymite, and cristobalite. Tridymite and cristobalite, which tend to be more fibrogenic than quartz, usually occur together and are found naturally in volcanic rock. They can also be created in industrial processes by heating quartz or amorphous silica. Quartz, the primary mineral form of crystalline silica in the earth’s crust, is a component of many rocks, including (but not limited to) sandstone, granite, slate, shale, and some limestones. Flint, agate, chert, and chalcedony are cryptocrystalline (microcrystalline) forms of silica, in which fine grains of quartz are bonded together by amorphous silica. Ground silica (also referred to as silica flour), is a finely pulverized form of quartz used as a filler in numerous manufactured products. Exposure -- Crystalline silica has been associated with, but is not limited to, the following industries and activities: construction (abrasive blasting, rock drilling, masonry and concrete work, jack hammering, tunneling); mining and quarrying (cutting or drilling through rocks such as sandstone and granite, movement of silica-containing material); quartz milling; foundry work (grinding, molding, shakeout, mulling, core making); ceramics, clay, and pottery work; glass manufacturing; agriculture; shipyards (abrasive blasting); railroads (laying and maintaining rail beds); manufacturing and use of abrasives; and manufacturing of abrasive soaps and detergents. Even when silica substitutes are used as abrasive material, silica exposure can result from abrasive blasting when the substrate surface being blasted is a silica-containing material, such as concrete. Products or materials that contain silica include: fill dirt and topsoil, pumice, sand, concrete, bricks and masonry products, mortar, pet litter, roofing granules, municipal water filtering beds, jewelers’ rouge, and investment powder used in molds for fine metal and jewelry castings. Many other products contain silica, including some scouring powders, art clays and glazes, paints, asphalt fillers, caulks, puttys, cosmetics, plasters, and plastics. Radiographic Abnormalities -- Nodular silicosis can be classified as simple or complicated. Simple silicosis is present if the largest radiographic opacity is < 1 cm in diameter. Complicated silicosis (also known as progressive massive fibrosis [PMF]) is present if the largest opacity is > 1 cm in diameter. Common radiographic findings of nodular silicosis include multiple, bilateral, and rounded small opacities predominating in the upper lung zones; other patterns have been described. In affected individuals with a history of mixed (silica and other) dust exposure, irregular opacities may be present or even predominate. Chest radiographs classified as profusion categories of 1/0 or greater using the 1980 International Labour Office (ILO) classification system (1), meet the case criteria for surveillance purposes. [Physicians whose competence in the use of the ILO classification system has been certified by NIOSH, are known as “B-Readers” (2).] Acute silicosis characteristically presents as a bilateral alveolar filling pattern, with or without bilateral small or large opacities. Histopathology -- Characteristic lung tissue pathology (3) in nodular silicosis consists of fibrotic nodules that are composed of concentrically arranged whorled bundles of collagen fibers, hyalinized in the center with a cellular peripheral zone. Polarized light microscopy reveals weakly (dull) birefringent particles, consistent with crystalline silica, primarily in the central hyalinized zone (particles below the resolution of the microscope and lying embedded in a thick section may not be revealed by polarized light). Acute silicosis is characterized by an alveolar exudate (alveolar lipoproteinosis) that stains by the periodic acid-Schiff reaction, accompanied by a cellular infiltrate of the alveolar walls. Addendum on Carcinogencity of Silica -- The International Agency for Research on Cancer has classified inhaled crystalline silica as carcinogenic to humans (Group 1). This classification is specific for occupational exposures to two forms of crystalline silica-quartz and cristobalite (4). References 1. International Labour Office. Guidelines for the use of ILO international classification of radiographs of pneumoconioses. Revised ed. Geneva, Switzerland: International Labour Office, 1980. Occupational Safety and Health Series 22 (Rev 80). 2. Wagner GR, Attfield MD, Kennedy RD, Parker JE. The NIOSH B-reader certification program: an update report. J Occup Med 1992;34:9:879-884. 3. Silicosis and Silicate Disease Committee. Diseases associated with exposure to silica and nonfibrous silicate minerals. Arch Pathol Lab Med 1988; 112:673-720. 4. IARC Monographs on the Evaluation of Carcinogenic Risks to Humans: Silica, Some Silicates, Coal Dust and para-.Aramid Fibrils (Vol. 68). Internet 1997. http://www.iarc.fr/publications/vol68.htm.