The Malta BioBank: At the Heart of Euro-Mediterranean BioBanking
advertisement

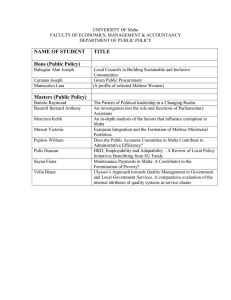
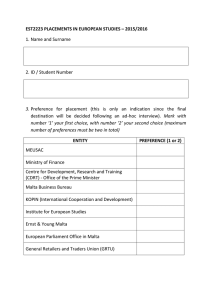
The Malta BioBank: At the Heart of Euro-Mediterranean BioBanking Felice AE, Vella J, Fiott A, Bezzina Wettinger S, Galdies R. Malta BioBank, Laboratory of Molecular Genetics, Department of Physiology & Biochemistry, University of Malta Introduction The Malta BioBank was developed in the context of the National Genetics Program (NGP) that included the Thalassaemia Project and Newborn Testing. The NGP is a partnership between the University of Malta and the Malta Department of Health. The Malta Biobank is a founding member of EuroBioBank and BBMRI and is one of only a few banks in the Euro-Mediterranean region. The additional partnership in the network of Haemoglobin laboratories and clinics (ITHANET & GLOBINBANK) provided a resource for hypothesis based population biobanking, discovery with large informative families and the basis for genomics in the Mediterranean [1]. 1980 1990 2000 2009 Total Population 318028 355,910 382,525 412,970 No. of births/ yr 5602 (MT only) 5368 (MT only) 4392 4143 Non-MT births not listed not listed 137 (3.11%) 430 (10.38%) Crude birth rate 17.6 15.1 11.3 10 Unidentified 7% Hb Camperdown 3% Hb Athens 3% Hb Setif 17% Hb S 35% Hb St Luke's 35% Fig. 1 Hb variants in Adults: 1999; n=29 from 5606 samples Hb O Arab 3% Hb C 3% Hb Camperdown 3% Hb E 11% Hb Marseille 5% HbSt Luke's & β Thal trait 3% Hb S 12% Hb Setif 11% Hb St Luke's 49% Table 1: Population demographics of the Maltese Islands Collections of the Malta BioBank Fig. 2 Hb variants in Adults: 2008 – 2009; n=28 from 6052 samples The Malta BioBank consists of a clinical bank and a population bank. The combination of population and families makes it an essential tool for population based gene discovery research [2]. The genetic origins, epidemiology, mobility and structure of the small island population are well understood, thus adding value to the biobank [3,4]. A summary of the collections is given in (Table 2). Population Bank Clinical Bank Random neonate collection (N~4000; Npools~400) Globin Bank: Thalassaemia & Hb variants (N~300) Twin Malta: Twin/Triplet/ Multiple births (N~700) Type 2 DM (NMalta~200; NLibya~200) Collection of "healthy" senior citizens (N~600) Miscarriage MTHFR mutant allele: 42.4% parents vs 33.9% random neonates (N~150 samples & 53 controls) Geoparkinson's collection: (N~200) & age-matched controls: (N~400) & lifestyle questionnaires Rare disease collections: (DNA + clinical data) Cystic Fibrosis (N~35) Muscular Dystrophy (N~6) Hb Setif & Hb St Luke's 5% HbS 25% FM1 70% Fig. 3 Hb variants in Neonates: 1999; n=79 from 5045 samples Hb St Luke's Hb Setif 8% 2% Hb S 13% FM3 5% FM1 72% Table 2: A list of collections stored in the Malta BioBank The collection of random neonates from the newborn diagnostic program has proven to be a robust and unbiased reference for a number of projects, such as the whole genome evaluation for risk of diabetes. It also anchors a developing collection of representative adults from among random families for genomics and biomarker discovery that is hypothesis driven. Since termination of pregnancies is not preferred, the neonate collection is better representative of genetic risk. The population demographics of the Maltese Islands have changed over the past thirty years (Table 1). The Maltese population has increased by 94942 citizens over 29 years. Although the total number of births is decreasing, there was a significant percentage increase in the number of registered non-Maltese births over 9 years from 3.11% in 2000 to 10.38% in 2009. Out of a total of 2353 registered marriages in 2009, 35.8% (i.e. 842) involved at least one non-Maltese individual [5]. The progressive structured change is quantitatively reflected in the Haemoglobin epidemiology over time. Haemoglobin (Hb) variants Figures 1 to 4 show the difference in percentages of Hb variants in adults who visited the Thalassaemia clinic and neonates born in Malta. Figure 5 shows the recorded percentages of Hb variants in newborns having at least one parent of non-Maltese origin. Based on Hb quantitative epidemiology it is assumed that 2-3 alleles at Fig. 4 Hb variants in Neonates: 2008 – 2009; n=62 from 4500 samples Hb E 12% Hb Setif 16% FM1 40% Hb S 32% Fig. 5 Hb variants in non-Maltese Neonates: 2009 - 2010 2–3 loci could generate a broad range of quantitative complexity in phenotypes and account for trans-selective pressures on the regional shaping of genomes. The hypothesis is being explored in connection with the genetics of complex disease such as T2DM. The Hb partnership (ITHANET) presents a sound basis for co-operation in Human Genomics between Mediterranean and Middle Eastern populations. References 1.Felice AE, Bezzina Wettinger S, Buhagiar S, Cassar W, Galdies R, Grech JL et al. Molecular epidemiology of haemoglobin and the molecular biology of in vivo globin gene expression. Life Chemistry Reports 1997;15(1):27-36. 2.Borg J, Papdopoulos P, Gerogitsi M, Gutierrez L, Grech G, Fanis P et al. Haploinsufficiency for the erythroid transciption factor KLF1 causes hereditary persistence of fetal hemoglobin. Nature Genetics 2010;42(9):801-5. 3.Capelli C, Redhead N, Novelletto N, Terrenato L, Malaspina P, Poulli Z et al. Population structure in the mediterranean basin: A Y chromosome perspective. Ann Hum Genet. 2005;206(70):207-255. 4.http://www.nso.gov.mt/themes/theme_page.aspx?id=77 (accessed 12th August, 2010). 5.http://www.timesofmalta.com/articles/view/20100514/local/third-of-marriages-in-malta involve-at-least-one-foreigner (accessed 15th May, 2010).