Haptic Body-Powered Upper-Extremity Prosthesis Simulator with Tunable Stiffness and Sensitivity Lee-Kuen Chua
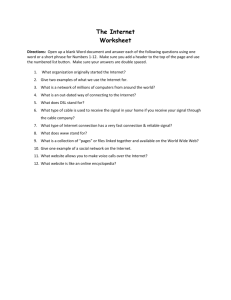
advertisement

Haptic Body-Powered Upper-Extremity Prosthesis Simulator with Tunable Stiffness and Sensitivity Lee-Kuen Chua∗ John A. Martinez† Ozkan Celik‡ Department of Kinesiology San Francisco State University School of Engineering San Francisco State University Department of Mechanical Engineering Colorado School of Mines A BSTRACT In this paper, we present the design, implementation, and characterization of a haptic body-powered prosthesis simulator. A novel aspect of our design is enabling real-time adjustment of gripper stiffness and control cable sensitivity parameters via software based on a haptic teleoperation control algorithm. Adjustment of these parameters across a continuum of values can assist the user to decide on the optimal parameters that can best fulfill the user’s functional needs, rendering the device a body-powered prosthesis prescription tool. Additionally, a switching capability between the voluntaryclosing (VC) mode and the voluntary-opening (VO) mode is incorporated into the software interface. With design and operation characteristics that closely replicate the form and mechanics of an actual body-powered upper-extremity prosthesis, our haptic prosthesis enables parameter optimization for individual prosthesis users and various human-subject-based research experiments involving both amputees and non-amputees on task-based optimization of prosthesis parameters and selection of operation mode. Keywords: Upper-extremity prosthesis, body-powered prosthesis, haptic teleoperation. 1 I NTRODUCTION Despite the advancement in medical techniques that enables the preservation of maximal residual limb following decapitating injuries or diseases, amputation, when necessary, continue to impact upon the quality of a person’s functional life after surgical procedures. In the United States alone, one in every 190 persons is an amputee and the total number of amputees is expected to reach a significant figure of 3.6 million in 2050, as shown by Ziegler-Graham et al. [1]. Specifically, an estimated 1,908 upper-extremity amputations are performed annually in the United States with trauma injury as the main cause [2]. Trauma amputees tend to comprise of economically active young people [3] and approximately 70% of all traumatic amputations are cases of upper-extremity loss [1]. Of concern, Biddiss and Chau [4] reported high rates of dissatisfaction with upper-extremity prosthetic use from various literatures, with inadequate functionality as an often-cited contributing factor. Consider, for example, the rejection rate for body-powered hook prostheses is 50% as presented in a survey study of 242 participants [5]. The high rejection and abandonment rates of upperextremity prosthetic use underscores the challenging task of designing highly functional upper-extremity prostheses that are acceptable by amputees. Even though the variety of body-powered upper-extremity prostheses made available to amputees has been increasing steadily, amputees’ choices are still limited by the design specifications of ∗ e-mail: leekuen@mail.sfsu.edu jn.martinez110@gmail.com ‡ e-mail: ocelik@mines.edu † e-mail: IEEE Haptics Symposium 2014 23-26 February, Houston, Tx, USA 978-1-4799-3130-9/14/$31.00 ©2014 IEEE each individual product set by the respective manufacturers. In fact, prosthetic components for upper-extremity amputees have not achieved substantial design breakthroughs for the past 40 years [2]. Research has shown that the rejection and abandonment rates for body-powered upper-extremity prostheses can vary from 16% [6] to as high as 87% [7] due to failure to satisfy the user’s needs. The amputee is only able to select a body-powered upper-extremity prosthesis, from within a limited range of commercially-available choices, with a gripper stiffness as well as a control cable sensitivity that most closely match the specific requirements to fulfill the intended functional needs. The inability to find a suitable match that permits the practical application of the prosthetic device in meeting the functional requirements of the amputee in a vocational or recreational setting, or even in performing basic tasks in activities of daily living (ADLs), is highly likely to bring about the outright rejection of a body-powered prosthetic device. Similarly, it is very unlikely to prevent the eventual abandonment of the prosthetic device over time [4], [8], [9]. Survey evidence from several studies of upperextremity amputees and amputation professionals lends strong support to functionality being the consideration of highest priority in an upper-extremity prosthetic device [5], [7], [10], [11]. Associated with this issue, the use of standard components in the mass fabrication of upper-extremity prosthetic devices was identified by LeBlanc [10] as a critical factor affecting the success of prosthetic fitting because the inputs of amputees could not be considered in the design process of third-party manufacturers, which have no direct contact with the end-users. Personal involvement in the design of one’s own prosthesis is identified as one of five major factors contributing to the enhancement of the quality of life of a prosthetic user [12]. Resnik [13] evaluated that a prosthesis that has involved users in all stages of its development is more likely to have improved product safety, functional usability and effectiveness, and user acceptability. A body-powered upper-extremity prosthesis is primarily operated by a combination of glenohumeral flexion and biscapular abduction to move a control cable that is linked to a terminal device [14]. Multiple parameters influence its overall functionality and controllability. These parameters include the stiffness of the restoring spring (or rubber band equivalence) in the terminal device to bring the gripper to a closed or open position, and the sensitivity of the movement of the gripper in relation to the movement of the control cable as activated by the contralateral shoulder via the harness system. As every amputee is unique, the prosthetist is faced with the challenging task of determining the optimal combination of the aforementioned parameters of a body-powered upper-extremity prosthesis that can best meet the requirements in enabling each individual user to achieve personal and employment goals. The availability of a prescription instrument, which permits tuning of the stiffness of the gripper that allows the opening and closing of a hook prehensor as well as the sensitivity of the control mechanism that dictates the amount of proportionate movement of the contralateral shoulder to operate a hook prehensor, will enable the prosthetist to incorporate the inputs of the user in real-time to improve the cru- 545 extremity prosthesis with a hook terminal device, our haptic prosthesis serves a platform for parameter optimization for individual prosthesis users and various human-subject-based research experiments involving both amputees and non-amputees on task-based optimization of prosthesis parameters and selection of operation mode. The rest of this paper is structured as follows: Section 2 describes the design principles and development approaches. The performance of the device is characterized and potential applications are discussed in Section 3. Section 4 concludes the paper with a summary and recommendations. 2 2.1 Figure 1: Haptic body-powered prosthesis simulator is a novel device enabling real-time adjustment of gripper stiffness and control cable sensitivity parameters via software across a continuum of values to assist the user to decide on the optimal parameters that can best fulfill the user’s functional needs. 546 AND D EVELOPMENT Mechanical Design We carefully addressed the challenging task of providing a wide range of device settings to meet the various unique needs of users while ensuring an easy and straightforward tuning operation. At the same time, the similarity of the activation of the gripper in our device to the typical body-powered hook prehensor is ensured. Technically, this is achieved by replacing the direct mechanical cable linkage between the gripper and the shoulder harness in traditional body-powered upper-extremity prostheses with two direct current (DC) motors in the haptic prosthesis, as depicted in Fig. 2. One DC motor actuates the gripper while the second one applies scaled forces to the contralateral shoulder and vice versa. A cable anchor plate with a stepped design further allows the user to manually select from five different cable sensitivity levels. Cable sensitivity remains further adjustable via software. Continuous haptic feedback through bilateral teleoperation control re-establishes the linkage between the gripper and the shoulder harness, however, in a way that allows easy access and adjustment of teleoperation parameters and virtual spring stiffness for default position of the thumb (either normally closed or normally open). 2.2 cial accuracy of finding an optimal prosthetic fit during the prescription process. Correct fitting made possible by prescriptive precision has also been reported to protect the contralateral unaffected limb from excessive stresses of long-term prosthetic use on the affected limb [15]. The facilitation of individuality of user preferences and improvement of fit accuracy via enhanced two-way interaction between the prosthetist and the user, which can be realized by employing the use of a testing instrument with a continuum capacity, thus hold vast potential in making significant contribution towards the overall effectiveness of the prosthetic fitting process. In this paper, we present the design, development, and characterization of a haptic body-powered prosthesis simulator, for prosthetic prescription and task-based device parameter optimization studies (see Fig. 1). The term “simulator” is used to underline the fact that the device is designed to fit non-amputees, to enable greater flexibility in recruitment of human subjects in future experiments. However, it should be noted that the device can easily be modified to fit transradial amputees without interfering with any of the functional parts/assemblies. Based on this property of the device, the terms “prosthesis” and “prosthesis simulator” are used interchangeably to address the device in this manuscript. A novel aspect of our design is enabling real-time adjustment of gripper stiffness and control cable sensitivity parameters via software control, coupled with haptic feedback, across a continuum of values to assist the user to decide on the optimal parameters that can best fulfill the user’s functional needs. Additionally, a switching capability between the voluntary-closing (VC) mode and the voluntary-opening (VO) mode is incorporated into the software interface. With design and operation characteristics that closely replicate the form and mechanics of an actual body-powered upper- D ESIGN Materials and Manufacturing The need for simplicity and reliability selects against cost in our material usage and manufacturing considerations for the haptic prosthesis, which uses a modular system consisting of a number of components containing structural parts, mechanisms, sensors and necessary electronics. A majority of the mechanical and structural parts was designed using 3D CAD software (SolidWorks) and then manufactured from ABSplus material using a 3D printer (uPrint Plus). ABSplus is a light and durable thermoplastic that is well suited for functional rapid prototyping. The design characteristics and material thicknesses for all the manufactured parts were first carefully selected and subsequently adjusted, if necessary, to minimize the cost, weight, and actuation inertia of the device, without compromising structural rigidity and integrity. Support surfaces or frames were incorporated into the design to achieve the optimal balance for this trade-off. The main frame for the device comprised of an industrial-grade extruded aluminum bar that is combined with a custom-made 3D-printed plate for a lightweight and sturdy support structure to hold and attach other key elements of the haptic prosthesis. In view of wear comfort and adjustable fitting, a short arm fracture brace by Exos Medical (see Figs. 1 and 2) was modified for use with our haptic prosthesis. It consists of a soft foam material that has a waterproof outer shell and an adjustable lace-tightening system using BOA tightening technology to hold the limb snugly in place. As such, it provides the flexibility of use on individuals with different arm sizes (dependent on the level of amputation and whether it is to be used on an affected or non-affected limb) and the suitability of accommodation for arm volume changes over time, for example, owing to muscle atrophy or hypertrophy with disuse or growth. The terminal device is a hook prehensor that is modeled after the Grip 3 Prehensor by TRS Inc. and specifically designed for compatibility with the commercially-available TRS Inc.’s Grip (a) (b) Figure 2: (a) CAD model of the haptic body-powered prosthesis. (b) Manufactured and assembled haptic body-powered prosthesis. Shoulder motor actuates the shoulder pulley via a cable drive transmission. Shoulder pulley includes a cable anchor plate allowing five cable sensitivity levels. Gripper motor drives the gripper pulley, hence the thumb side of the Grip 3 fingers by TRS Inc. 3 fingers with polyurethane gripping surface demonstrating nonslip contact, anti-staining quality, and easy replaceability. Other retail-grade materials include a bicycle rubber handle used for more robust attachment for non-amputee users as well as a bicycle cable of 1-mm diameter (with Bowden cable housing) and a Griplock 151420-S lock mechanism with a maximum tension capacity of 498N that are used in the shoulder harness transmission. The harness consists of a relatively low-cost strap and buckle system made of lightweight and durable nylon material. 2.3 Motors and Encoders Implementation of well-developed bilateral teleoperation control algorithms [16] on both motors virtually (via control software) rebuilds the mechanical linkage between the gripper and the shoulder harness. Gripper actuation is provided by a Maxon RE 30 DC (24V, 3.81A) motor with a maximum continuous output torque of 85.0 mNm whereas shoulder actuation comes from a Maxon Amax 32 DC (24V, 1.35A) motor with a maximum continuous output torque of 45.5 mNm. The former uses an Avago Technologies MR 500CPR (counts per revolution) encoder and the latter uses an Avago Technologies HEDL 5540 500CPR encoder for accurate measurement of the angular positions of the gripper and the shoulder cable respectively. Both motors are small (diameter of 30 mm and 32 mm for the gripper and shoulder motors respectively) and lightweight (nominal weight of 238 g and 240 g for the gripper and shoulder motors respectively) for compact integration into the prosthetic device. Two-way transmission of torque is achieved through a cable drive mechanism. The cable drive mechanism allowed amplification of achievable output torques via a 12:1 gear ratio. 2.4 Control and Data Acquisition The control and data acquisition architecture has to be sufficiently comprehensive yet flexible enough to support the real time change of device setting via graphical user interface (GUI) commands, corresponding computation of control loops, and accurate delivery of sensory feedback. Mathworks MATLAB/Simulink and Quanser QuaRC were used to implement the control software that allows the user to choose between a VC or VO mode of operation as well as toggle between multiple values of gripper stiffness and cable sensitivity via a computer interface to match individual preferences. The values of output torque and angle position for both gripper and shoulder connection were recorded by a Quanser Q8-USB 16-bit data acquisition card performing at a servo loop rate of 1 kHz. 2.5 Safety Safety features are implemented for the haptic prosthesis as a precautionary measure to protect the user against possible device haz- ards. These safety features include: • Mechanical means via an easily accessible and visibly prominent emergency stop button for instantaneous deactivation of all operation of the device. • Electrical means via saturation blocks in the control algorithm to limit the amount of torque output for each of the motors. 3 C HARACTERIZATION AND D ISCUSSION 3.1 Gripper Stiffness In order to test the variation of the torque output at the gripper motor with gripper stiffness, we set the operation mode to VC and measured the output torques as a rigid object was grasped by the gripper using a power grip, and varied the stiffness values via software with desired stiffness values provided as a staircase function consisting of five steps/values. Results of this test is shown in Fig. 3, where it can be observed that the amount of torque required to actuate the gripper increases proportionally in steps with higher values of desired gripper stiffness, indicating successful regulation of gripper stiffness via implementation of a virtual spring at the gripper motor in the software interface. 3.2 Cable Sensitivity Fig. 4 shows the variation of the gripper thumb position with cable travel over time using three different sensitivity ratios of 0.67, 1.00, and 1.33, in the VC mode. In this test, a sinusoidal reference position input was fed into the shoulder motor under PD position control to simulate shoulder angle variation at each sensitivity setting. When the sensitivity ratio is set to 1.00, the position trajectory the gripper motor follows due to the haptic teleoperation algorithm almost exactly coincides with the trajectory produced by the shoulder motor, implying that the gripper movement is closely matched to the shoulder cable movement. It can be further observed that the gripper movement is proportionately greater than the shoulder cable movement at a ratio of 0.67 from the similar but larger waveform of the gripper motor as compared to the waveform of the shoulder motor. This relationship is reversed at a higher sensitivity ratio of 1.33. Results of this test confirm that the developed device and control algorithm successfully enable software adjustment of device cable sensitivity. 3.3 Gripper Specifications The gripper has a pinch grip aperture size of 100.50 mm from thumb tip to index finger tip for precision prehension and a power grip aperture size of 97.80 mm from thumb mid-point to index finger mid-point for cylindrical prehension in the fully open position, 547 14 Shoulder Angle GA at R=0.67 GA at R=1.00 GA at R=1.33 30 1000 800 8 600 6 400 4 200 2 Position (degrees) 20 10 Torque (mNm) Gripper Stiffness (mNm/degree) 12 10 0 −10 −20 Gripper Stiffness Torque 0 0 0.5 1 1.5 2 2.5 Time(s) 3 3.5 4 4.5 0 5 Figure 3: Gripper stiffness values are varied in steps while a rigid object was grasped in power grip by the gripper. The proportional relationship between the torques applied at the gripper on the object and the spring stiffness values confirm successful tunability of gripper spring stiffness via software. and an internal diameter (from thumb center to index finger center) of 30.20 mm in the fully closed position. We investigated the gripper speed by applying maximum torque to the gripper motor in two directions, namely, from a fully open position to a fully closed position and from a fully closed position to a fully open position. The closing and opening times for the gripper thumb to travel through 90 deg are measured to be the same at 0.06 sec, which is equivalent to a closing or opening speed of 1,475 deg/sec, when a maximum motor torque of 45.5 mNm is commanded to the gripper motor. In comparison, a review of four commercial (body-powered and externally-powered) and eleven research (externally-powered) prosthetic hands conducted by Belter [17] showed that the average closing time and speed are 0.36-5.00 sec and 23-775 deg/sec respectively. It is apparent that not only is our prosthetic device able to close much faster than the maximum closing time of 0.8 sec recommended for prosthetic terminal devices [18] or the typical closing speed of 172-200 deg/sec required in normal daily tasks of picking and placing objects [14], it can also cover the full range of speed capacity found in commonly available prosthetic terminal devices, which is a fundamental hallmark of a suitable apparatus for prescriptive purposes. The maximum pinch grip and power grip forces our prosthesis can generate are characterized at 11,747 mN and 26,697 mN respectively. Even though these values are far below maximum grip strength of healthy individuals, they are comparable to various commercial or experimental prosthetic devices. 3.4 Shoulder Cable Specifications The movement and force information arriving at the shoulder pulley via the haptic teleoperation algorithm connecting the shoulder and gripper ends of the device is further transmitted to the shoulder harness that is worn on the contralateral shoulder via a Bowden cable. This is similar to the Bowden cable transmissions found on all body-powered prostheses. We have characterized the maximum cable tension and cable travel, together with the resolution in cable tension and in cable travel, based on the maximum continuous torque specifications of the motor, resolution of the data acquisition board, and five different cable attachment diameter options for the shoulder pulley. Results of this characterization are summarized in Table 1. As can be observed from this table, the shoulder actuation mechanism spans a significant range of force and cable travel options with high resolution position sensing. 548 −30 0 0.5 1 1.5 2 2.5 Time(s) 3 3.5 4 4.5 5 Figure 4: Variation of the gripper thumb position (GA: gripper angle) with shoulder pulley position over time using three different sensitivity ratios of R=0.67, 1.00, and 1.33, in the VC mode. In this test, a sinusoidal reference position input was fed to the shoulder motor under PD position control to simulate shoulder angle variation at each sensitivity setting. Thumb movement is exactly equal to the shoulder movement for R=1.0, while it moves more for R=0.67 and less for R=1.33, demonstrating successful regulation of shoulder to gripper movement sensitivity. 3.5 Applications A haptic prosthetic device with a tuning capability can provide the specialized instrument required in harnessing accurate user feedback during the prescription process for a new prosthesis. Instead of having to use a costly toolkit consisting of a large variety of commercial body-powered upper-extremity prostheses and adopting a trial-and-error approach of necessitating the user to the tedious experience of repeated try-ons in the hope of finding a fit with a satisfactory combination of gripper stiffness and control sensitivity, the prosthetist essentially needs to have only one tool. Our tunable device accords the prosthetist with an all-in-one tool to determine not just the optimal combination of the abovementioned two features but the ideal operation mode (VO or VC) as well, that will best serve the effective and efficient use of the to-be-fitted prosthesis (in the functional opinion of the user). Furthermore, the measurement and data collection of nominal values of gripper stiffness and cable sensitivity that characteristic groups of users prefer for performing specific functional tasks can be made possible with our tunable device. Research work invested in this area can create better understanding of how body-powered prostheses are utilized to accomplish functional tasks and can therefore produce the reward of creating a useful source of technical database for commercial manufacturers of body-powered prostheses to refer to in their design effort to optimize function-enhancing usability and acceptance of the end-products. Such a database will also allow prosthetists to select appropriate initial references to begin the prescription process, based on evidence-supported scientific information, so as to ensure that the prescription process can be carried out accurately and expeditiously, so as to prevent undue distress to the user. The proposed haptic tunable prosthesis can serve as a highly effective simulator for the realistic training of amputees and therapists, too. While waiting for the arrival of a new prosthesis, the person with an upper limb loss or deficiency can attain taskspecific training by employing the haptic prosthesis in a feedbackaugmented rehabilitation setting. The prosthetic simulator can be tuned to the same operation mode (VC or VO), gripper stiffness, and cable sensitivity as the body-powered prosthesis that the user Table 1: Cable tension and travel specifications of the shoulder harness actuation system under five different possible cable attachment settings. Cable Setting 1 2 3 4 5 Maximum Tension (mN) 53,064 33,165 22,110 16,582 13,266 Minimum Tension Resolution (mN) 35.99 22.49 14.99 11.25 9.00 will be fitted with eventually so as to provide an early opportunity for the user to learn the correct body movements to achieve functional usage of the to-be-fitted prosthesis as well as to explore task limitations imposed by the inherent design features of this prosthetic choice. This familiarization serves the twofold goal of minimizing maladaptive disuse of the affected limb, and hence increasing the potential of skillful employment of the to-be-received prosthesis in ADLs, as well as raising the level of realistic expectation of the new prosthesis. 4 C ONCLUSION In view of the unmet needs of the upper-extremity amputee population with the current state-of-the-art prosthetic fitting and training resources, there is a need for a prosthesis with tunable parameters in real-time. In this paper, we presented the design, implementation and characterization of a haptic body-powered prosthetic device with adjustable gripper stiffness, control cable sensitivity, and operation mode (VC/VO) to address this need. Based on experimental tests, we confirmed successful operation of the device in fulfilling the design requirements as a prosthetic prescription tool and a research testbed. Our haptic prosthesis enables task-specific optimization and user-centered customization via selectable gripper stiffness and/or control cable sensitivity as well as operation mode selection. Hence the device establishes a platform for future research involving human subject experiments to inform prosthetic fitting protocols and task-based optimization of device parameters. 5 ACKNOWLEDGEMENTS We gratefully acknowledge the feedback and assistance of Dr. Marilyn Mitchell from the Department of Kinesiology at San Francisco State University during device development. R EFERENCES [1] K. Ziegler-Graham, E. J. MacKenzie, P. L. Ephraim, T. G. Travison, and R. Brookmeyer, “Estimating the prevalence of limb loss in the united states: 2005 to 2050,” Archives of Physical Medicine and Rehabilitation, vol. 89, no. 3, pp. 422–429, 2008. [2] T. R. Dillingham, L. E. Pezzin, and E. J. MacKenzie, “Limb amputation and limb deficiency: epidemiology and recent trends in the united states,” Southern Medical Journal, vol. 95, no. 8, pp. 875–883, 2002. [3] A. Esquenazi, “Amputation rehabilitation and prosthetic restoration. from surgery to community reintegration,” Disability and Rehabilitation, vol. 26, no. 14-15, pp. 831–836, 2004. [4] E. A. Biddiss and T. T. Chau, “Upper limb prosthesis use and abandonment: a survey of the last 25 years,” Prosthetics and Orthotics International, vol. 31, no. 3, pp. 236–257, 2007. [5] E. Biddiss, D. Beaton, and T. Chau, “Consumer design priorities for upper limb prosthetics,” Disability and Rehabilitation: Assistive Technology, vol. 2, no. 6, pp. 346–357, 2007. [6] K. Bhaskaranand, A. K. Bhat, and K. N. Acharya, “Prosthetic rehabilitation in traumatic upper limb amputees (an indian perspective),” Archives of Orthopaedic and Trauma Surgery, vol. 123, no. 7, pp. 363–366, 2003. Maximum Travel (mm) 0.63 1.01 1.52 2.03 2.53 Minimum Travel Resolution (μm) 0.95 1.52 2.28 3.04 3.80 [7] G. Kejlaa, “Consumer concerns and the functional value of prostheses to upper limb amputees,” Prosthetics and Orthotics International, vol. 17, no. 3, pp. 157–163, 1993. [8] S. Millstein, H. Heger, and G. Hunter, “Prosthetic use in adult upper limb amputees: a comparison of the body powered and electrically powered prostheses,” Prosthetics and Orthotics International, vol. 10, no. 1, pp. 27–34, 1986. [9] A. E. Schultz, S. P. Baade, and T. A. Kuiken, “Expert opinions on success factors for upper-limb prostheses,” Journal of Rehabilitation Research and Development, vol. 44, no. 4, pp. 483–490, 2007. [10] M. A. LeBlanc, “Innovation and improvement of body-powered arm prostheses: a first step,” Clinical Prosthetics and Orthotics, vol. 9, no. 1, pp. 13–16, 1985. [11] D. J. Atkins, D. C. Heard, and W. H. Donovan, “Epidemiologic overview of individuals with upper-limb loss and their reported research priorities,” Journal of Prosthetics and Orthotics, vol. 8, no. 1, pp. 2–11, 1996. [12] J. W. Michael and J. H. Bowker, “Prosthetics/orthotics research for the twenty-first century: summary of 1992 conference proceedings,” Journal of Prosthetics and Orthotics, vol. 6, no. 4, pp. 100–107, 1994. [13] L. Resnik, “Development and testing of new upper-limb prosthetic devices: research designs for usability testing.” Journal of Rehabilitation Research and Development, vol. 48, no. 6, pp. 697–706, 2011. [14] R. Weir, “Design of artificial arms and hands for prosthetic applications,” Standard Handbook of Biomedical Engineering and Design, pp. 1–61, 2003. [15] C. Lake and R. Dodson, “Progressive upper limb prosthetics,” Physical Medicine and Rehabilitation Clinics of North America, vol. 17, no. 1, pp. 49–72, 2006. [16] Y. Yokokohji and T. Yoshikawa, “Bilateral control of master-slave manipulators for ideal kinesthetic coupling-formulation and experiment,” IEEE Transactions on Robotics and Automation, vol. 10, no. 5, pp. 605–620, 1994. [17] J. Belter and A. Dollar, “Performance characteristics of anthropomorphic prosthetic hands,” in Proc. IEEE International Conference on Rehabilitation Robotics (ICORR 2011), 2011, pp. 1–7. [18] R. Vinet, Y. Lozac’h, N. Beaudry, and G. Drouin, “Design methodology for a multifunctional hand prosthesis,” Journal of Rehabilitation Research and Development, vol. 32, no. 4, pp. 316–324, 1995. 549