CEN Education Day Discussion Session
advertisement

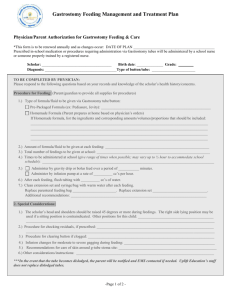
CEN Education Day Discussion Session What do we mean by “risk assessment” • Something that we wish we had done better when things go badly. • Something we forget if things go well. Considerations • • • • • • • What the family want Anxieties of professionals and other carers What is “best” for the child Risks - v - Benefits Life expectancy - v - Quality of life Autonomy and Advocacy What is the evidence? Risks - v - Benefits What could go wrong? What outomes do we hope for? • Exacerbated gut dysmotlity • More frequent / severe resp problems • Inadequate nutrition • Reduced life expectancy • Adequate nutrition • Eating a pleasure for child and family • Health improved or at least maintained Case A Age 2 • Undiagnosed severe hypotonia (low tone) • Poor head control leading to problems with head position for feeding • Poor oro-motor control, xs drooling • Epilepsy which can be poorly controlled some days • Weight beginning to fall from 50th to 25th centile • Mother wants to maintain oral feeding, father wants to start tube feeding Case B Age 5 • Parents very much want to continue oral feeding • Feeds can take up to 1 hour and require a high degree of skill • Video-fluoroscopy shows slow swallow with tendency to aspirate with liquids and towards the end of the examination • School want to have training, but can not guarantee one person regularly to feed the child • Over the past 6 months the child has had 3 admissions to hospital with chest infections Case C Age 18 • Severe cerebral palsy ,4 limb involvement with increased tone • Gastrostomy in situ • At risk swallow, so only having small tasters orally and most of nutrition via gastrostomy • Bolus feeds via gastrostomy at mealtimes • Known to be prone to reflux, has had previous fundoplication, when gastrostomy sited • No problem with chest infections over past 18 months. • Weight continues on 10th centile Consider case A: • What investigations could/ should be done? comprehensive assessment needed • How long is a reasonable time to take to feed? • Should we worry about the weight? • What other factors could be considered? Need to be clear about parents understanding of condition and views. Clarify benefits and risks of tube / oral feeding • What should we do if professionals and parents can’t agree? Explore both parents understanding and emotional position. Sensitive issues should not be discussed in MDT meetings Consider case B • Will investigations help, and if so which? • How will you evaluate risk and benefit of oral feeding to the child? Need to ensure that family are aware of limited life expectancy • Are the expectations for management at school reasonable? • What process will you follow to make a decision? Particular importance of good communication / agreement between professionals • Is the same decision relevant for school and home? Need to address school carers anxieties • Importance of good communication in this scenario Consider case C • Do things need to change moving to the ‘adult’ world? Many practical changes e.g. supply arrangemnts. Learn to deal with the diferent way adult services work • What factors might need re-evaluated? Cognitive level and advocacy atonomy. Need to address some practical / policy differences • Who will provide training and support to the young person and his/her carers? Need for transitional care worker • Do parents also need to change how they meet the young person’s nutritional needs? • Does the risk evaluation process change once a child reaches 16years? Possible need for liability insurance • How long is a reasonable time to take to feed? Various suggestions up to 45mins • Should we worry about the weight? Consider SD scores Discussion summary • Importance of key worker • Need for “anticipatory discussions early on • Important to raise issues in advance of them becoming imminent • Key worker role. In communication • Include in CSP • Anticipation where possible • Information leaflets and web sites • Parent groups • Email communication • Key worker appointment process variable and transition to adult services is problematic • Some professionals involved from cradle to grave but geographically variable • More primary care involvement esp in rural situation