Document 13310896
advertisement

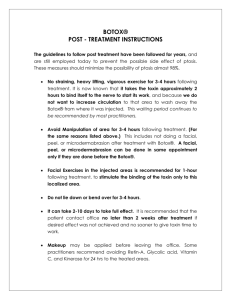
Int. J. Pharm. Sci. Rev. Res., 37(1), March – April 2016; Article No. 28, Pages: 155-162 ISSN 0976 – 044X Review Article Botox: Its Illuminating Frontiers of Dentistry 1 2 Kala S. Bhushan, *Nagunuri Divya, Prakash Shobha MDS, Professor, Department of periodontics, College of Dental Sciences, Davangere, Karnataka, India *BDS, Post graduate student, Department of periodontics, College of Dental Sciences, Davangere, Karnataka, India. 2 MDS, Professor and head, Department of Periodontics, College of Dental Sciences, Davangere, Karnataka, India. *Corresponding author’s E-mail: diiivv@gmail.com 1 Accepted on: 30-01-2016; Finalized on: 29-02-2016. ABSTRACT Down the lane of rapidly evolving medical therapeutic modalities, Botox (FDA-approved) has emerged as a significant agent for the cosmetic treatment of wrinkles, cervical dystonia, severe primary axillary hyperhidrosis, blepharospasm etc. Commercially available botulinum toxin is the purified exotoxin of the anaerobic bacteria, Clostridium botulinum and acts by the inhibition of the release of acetylcholine (ACH), a neurotransmitter responsible for the activation of muscle contraction and glandular secretions thus resulting in reduction of tone in the injected muscle. In the recent times, botulinum toxin has been attributed as a minimally invasive procedure and also conferred considerable role in the multiple zones of dentistry for the management of various oro-facial conditions such as temporo-mandibular disorders, bruxism, masseter hypertrophy, implant surgery etc and is also being used to treat esthetic clinical situations like deep nasolabial folds, gummy smiles and black triangles between teeth. An extensive internet research was done for the implications of botulinum toxin used in dentistry and all related significant articles and studies were extracted and summarized. This review article throws considerable light on various promising therapeutic applications of botox in multiple disciplines of dentistry. Keywords: Clostridium botulinum, Dentistry, Esthetics, Exotoxins, Hyperhidrosis Hypertrophy. INTRODUCTION B otox possess a significant and elaborate history of medically therapeutic usage in various conditions like cervical dystonia, hyperhidrosis, strabismus, blepharospasm etc1. Although botulinum toxin is a lethal, naturally occurring substance, it can be used as an effective and powerful medication when administered in approved dosage (FDA)2. In the recent years, Botox has been increasingly used in dentistry as well due to its promising therapeutic effects in treatment of temporomandibular disorders (TMD), dental implants surgery, Masseteric hypertrophy, Mandibular spasm etc and also in management of unaesthetic clinical situations like deep nasolabial folds, gummy smiles and black triangles. History An idea of possible therapeutic use for botulinum toxin was first developed by German physician, Justinus Kerner (1786-1862) who deduced that it acted by interrupting signal transmission within peripheral sympathetic nervous system, leaving sensory transmission intact. In 1949, Burgen was the first to discover that the toxin was able to block neuromuscular transmission. Botulinum toxin is a protein and neurotoxin produced by the bacterium Clostridium botulinum3. Currently, seven botulinum neurotoxin serotypes (A, B, C1, D, E, F, and G) produced by Clostridium botulinum are recognized2. Three forms of botulinum toxin type A (Botox, Dysport and Xeomin) and one form of botulinum toxin type B (MyoBloc) are available commercially for various cosmetic and medical procedures.4 Each vial of BOTOX contains4 1. 100 Units (U) of Clostridium botulinum type A neurotoxin complex 2. 0.5 milligrams of Albumin 3. And 0.9 milligrams of sodium chloride in a sterile, vacuum-dried form without a preservative. Mechanism of Action of Botulinum Injecting overactive muscles with minute quantities of botulinum toxin type-A results in decreased muscle activity. The release of acetyl choline at neuro-muscular junction is inhibited by the toxin resulting in reduced intensity or complete elimination of overall contraction of 5 the muscle, depending on the amount of toxin used . It prevents the vesicle where the acetylcholine is stored from binding to the membrane where the neurotransmitter can be released. Botulinum toxin achieves this effect by its endopeptidase activity against SNARE proteins, which are 25-kd synaptosomal associated proteins that are required for the docking of the ACH vesicle to the presynaptic membrane6. This effectively weakens the muscle for a period of three to four months & as the muscle initiates new acetylcholine receptors and the growth of branches from the neurons to form new synaptic contacts, slowly and steadily the muscle returns to its full function and with no side-effects4. International Journal of Pharmaceutical Sciences Review and Research Available online at www.globalresearchonline.net © Copyright protected. Unauthorised republication, reproduction, distribution, dissemination and copying of this document in whole or in part is strictly prohibited. 155 Int. J. Pharm. Sci. Rev. Res., 37(1), March – April 2016; Article No. 28, Pages: 155-162 ISSN 0976 – 044X Safety and Adverse Effects Treatment Protocol For Tmd In general, adverse reactions are uncommon and relatively mild and transient which are more common at or near the site of injection. These include dry mouth, dysphagia, dysphonia, transient muscle paralysis, headache, urticaria and nausea7 and these side effects are noted when the dose exceeds that recommended. The treatment begins with a lower dose, because it is always possible to titrate up to a higher dose, if necessary. The FDA revised the prescribing information for the commercially available botulinum toxin A products to include a “Boxed Warning” highlighting potentially adverse reactions related to distant spread of the toxin effect from the injection site.8 These highlight botulismlike symptoms such as muscle weakness, hoarseness or dysphonia, dysarthria, loss of bladder control, difficulty breathing, difficulty swallowing, double or blurred vision and drooping eyelids. These effects can occur anywhere from a day to several weeks after treatment at unrelated 9-12 sites. Uses Botulinum toxin type A can be used in following dental conditions:- (Table-1) 1. Temporo-mandibular joint disorders 2. Bruxism 3. Masseteric hypertrophy 4. Oral surgery The temporalis component of pain is treated with bilateral injections of 7.5 U into the anterior vertical fibers of each temporalis muscle. In more severe cases, 2.5 U are given into the middle and posterior third of the temporalis muscles. Pain relief for the tendon of temporalis is achieved with multiple injections of 2.5 U equidistantly spaced in the temple area outside the orbital rim. Bruxism Bruxism (excessive eccentric grinding of teeth) can affect the muscles solely and/or lead to the formation of TMD causing joint damage. The symptoms are exacerbated by external factors such as fatigue, stress, and emotional 19 extremes. If sleep bruxism is present, the most effective way to protect the teeth is with an occlusal appliance. The problem with occlusal covering appliances is that they do little or nothing to stop the bruxism and offer only a brief respite from headaches and bruxism induced TMJ derangement or arthritis. In general, because of the numerous presentations of bruxism, the current treatments available are neither uniform nor universally successful20. Techniques currently employed for aesthetic, conservative restorations may not withstand the parafunctional forces continually applied by some patients. Thus, many of these treatment options are not ideal for all patients, and muscular relaxation with botulinum toxin A is a viable alternative. When a muscle relaxant is used with the muscles of mastication, this clenching reflex can be reduced or eliminated.21 5. Dental implants 6. Gummy smile 7. Mandibular spasm 8. Oro-mandibular dystonia 9. Myofacial Pain And Neck Pain 10. Headache, migraine, and trigeminal neuralgia 12. Dento-facial Aesthetics Because a very small percentage of available force is required to masticate food, a slight relaxation of muscle function reduces bruxism and is usually insufficient to affect chewing and swallowing.22 13. Pathologic Clenching Masseteric Hypertrophy 14. Retraining Muscles during Orthodontic Treatment Masseteric hypertrophy refers to enlargement of the masseter muscles which often leads to clenching and 26 bruxism . The masseter component of pain is treated with 5 U injected into the belly of the masseter below an imaginary line joining the tragus of the ear and the corner of the mouth23 11. Sialorrhea 15. Recurrent Dislocation of the Mandibular Condyle Temporo-Mandibular Joint Disorders Temporo-mandibular disorders (TMD) may include true pathology of the temporo-mandibular joint as well as 13,14 masticatory muscle dysfunction. TMD manifests with facial pain, joint sounds, headache, peri-auricular pain, neck pain, and/or decreased joint excursions.15,16 The majority of TMD cases include a myogenic component17 and muscular spasticity secondary to bruxism, external stressors, oro-mandibular dystonia, and psychomotor behaviours are common aetiologic factors of TMD. In several short but well-documented clinical trials by (1) Al-Ahmad, Al-Qudah,27 (2) Mandel and Tharakan,28 and (3) Rijsdijk and Vanes29, injection of small aliquots of BOTOX into the masseter muscles resulted in a sustained reduction of masseter hyperactivity. There are several case reports, which are supporting the efficacy of BOTOX treatment for TMD: International Journal of Pharmaceutical Sciences Review and Research Available online at www.globalresearchonline.net © Copyright protected. Unauthorised republication, reproduction, distribution, dissemination and copying of this document in whole or in part is strictly prohibited. 156 Int. J. Pharm. Sci. Rev. Res., 37(1), March – April 2016; Article No. 28, Pages: 155-162 Freund conducted a large open-label trial with 46 patients suffering from TMD and found that 150 U injections of BOTOX to the temporalis and masseter muscles significantly decreased pain and tenderness and improved function and mouth opening.22 Tan and Jankovic conducted a long-term open-label trial on 18 patients with a history of severe bruxism. Injections of BOTOX given to the masseter muscle (mean dose: 61.7 U/side; range 25-100 U), yielded a total duration of therapeutic response of 19 weeks.24 Lee conducted a small open-label trial study to evaluate the effect of BOTOX on pain in six patients with limited mouth opening due to TMD. All patients showed clinical remission of pain symptoms without any adverse effects during the 5-12 months follow-up 25 period. Oral Surgery Maxillofacial fracture repair often requires multiple fixation sites and hardware to overcome the strong forces of masticatory musculature. Overloading of these muscles can prevent fracture callus formation. The muscular relaxation achieved with prophylactic use of BOTOX injections to the masticatory muscles can be beneficial by allowing fracture healing in a more stable environment.30 Low doses of BOTOX can potentially limit the parafunctional clenching and its intensity and thus allow traumatized tissues to heal. High doses can be used as a ''pharmaceutical splint,'' limiting muscle contraction before resetting and during rehabilitation after fracture of the facial bone, e.g., fractured mandibular condyle.15 Kayikvioglu and colleagues conducted a small open-label study to prospectively examine the use of BOTOX in five patients as an adjunct to zygomatic fracture fixation surgery, in an attempt to reduce the number of fixation sites and to prevent dislocation of the zygomatic bone. Pre-operatively 100 U of BOTOX was injected into the masseter muscle of the fractured side. After 12-48 h of injection, patients were operated and muscle denervation was confirmed by EMG. The temporary paralysis of the masseter muscle allowed for fewer miniplates and/or microplates inserted among the patients and resulted in no complications. The Kayikvioglu group also found similar benefits of adjunct BOTOX treatment for surgical 30 reduction of mandibular condylar bone fractures . Dental Implants Implant patients will benefit from pre-surgical BOTOX treatment. After multiple implants or when immediate loaded implants are placed, osseo-integration can be impeded by excessive functional forces in patients with para-functional habits. Over loading of the implants results in implant failure by loosening of the implant components or prevention of osseo-integration. The muscular relaxation achieved with prophylactic use of BOTOX injections to the masticatory muscles can be ISSN 0976 – 044X beneficial by allowing implant structures better osseointegrated31,32 Gummy Smile When an excess of gingiva superior to the maxillary anterior teeth is displayed upon full smile, it is termed a gingival smile /gummy smile/full denture smile.33 The exposure of more than 3 mm of the gum during the smile is known as gummy smile.3 It poses a significant risk for oral hygiene maintenance and cosmetic outlook with no easy and effective remedy. Excessive gum exposure is frequently attributable to over-contraction of the upper lip muscles, particularly the levator labii Superioris alaeque nasi. In general, the most common surgical corrections currently used are the LeFort I maxillary osteotomies with impaction for skeletal vertical maxillary excess, and gingivectomies for delayed passive dental eruption with excessive gingival display. Botulinum toxin should be injected in small, carefully titrated doses to limit muscular over-contraction of upper lip, thus reducing exposure of the upper gums when smiling. Hwang at Yonsei University College of dentistry, Seoul, Korea have proposed a injection point for botulinum toxin and named it as Yonsei point37. It is basically a point located at the centre of triangle formed by levator labii superioris, levator labii superioris alaeque nasi and zygomaticus minor. A dose of 3U is recommended at each injection site.38 In a small open-label trial, five patients with excessive gingival display resulting from hyper-functional upper-lip elevator muscles were treated with Botox injections under electromyographic guidance. Patients received one 0.25 U per muscle bilaterally into the levator labii superioris, levator labii Superioris alaeque nasi, and at the overlap areas of the levator labii superioris and zygomaticus minor muscles. All of the patients were pleased with the results and the effective increase in upper-lip length upon smiling averaged 124.2%. The duration of effect ranged from 3 to 6 months, and no adverse effects were reported or observed. However, the improvement is temporary and must be repeated every 35 six months to one year. Mandibular Spasm It is a condition when the mandibular closing musculature remains semi-contracted or in spasm, resulting in restricted mouth opening. This type of muscular spasm limits completing the basic oral hygiene necessary to prevent oral disease and places restrictions on dental treatment. BOTOX treatment to the masticatory musculature diminishes the effects of hyper-functional or spastic muscles, that can significantly improve function and mouth opening, and effectively decrease pain and 22,23 tenderness to palpation. Oro-Mandibular Dystonia Oro-mandibular dystonia (OMD) is a movement disorder characterized by involuntary spasms and muscle International Journal of Pharmaceutical Sciences Review and Research Available online at www.globalresearchonline.net © Copyright protected. Unauthorised republication, reproduction, distribution, dissemination and copying of this document in whole or in part is strictly prohibited. 157 Int. J. Pharm. Sci. Rev. Res., 37(1), March – April 2016; Article No. 28, Pages: 155-162 contractions. It manifests as distorted oral position and function resulting in difficulty in speaking, swallowing, and eating. Although it is a neurologic disorder, it is included as a subset of TMD because of its involvement of 39 the masticatory apparatus . Most of the reported literature on OMD has been open-label studies, but all have reported improvement with botulinum toxin injections.40-44 The largest study to date was a prospective open-label conducted by Tan and Jankovic that treated 162 patients with OMD over a 10-year period. Botulinum toxin type A was injected into the masseters and/or the submental is complex. Improvement in function for chewing and speaking was reported in 67.9% of the patients, and mean duration of clinical improvement was 16.4 ± 7.1 wk.44 Myofacial Pain and Neck Pain The etiology of myofacial pain syndrome is incompletely understood. Some clinicians believe that it characteristically results from either an acute episode of muscle overload or from chronic and/or repetitive muscle overload. Active myofacial trigger points, which cause pain, exhibit marked localized tenderness and often refer pain to distant sites and disturb motor function. Injection of muscles with BOTOX has been reported to be effective for myofacial pain caused by trigger points.45 Headache, Migraine, and Trigeminal Neuralgia Standard medications used in the treatment of headache and migraine causes a number of side effects, such as stomach upset, drowsiness, and weight gain. Such side effects for BOTOX treatment are relatively rare. BOTOX 25-75 U injected into peri-cranial muscles relieves headache by relaxing the over active muscles by blocking nerve impulses that trigger contractions. For migraines, there is no muscle component involved. It is believed that BOTOX works by blocking the protein that carries the message of pain to the brain and relief typically takes effect in 2-3 weeks after injection.46 According to Elcio, excruciating pain associated with inflammation of the trigeminal nerve of the head and face 48 can be substantially relieved by injections of BOTOX. According to Lawrence Robbins, BOTOX actually is an anti-inflammatory substance, decreasing, or antagonizing the inflammatory (neuronal/brain) effects of W (Calcitonin gene-related peptide).47 Sialorrhea This toxin also blocks the release of acetylcholine at the cholinergic synapses of the autonomic nervous system; thus, this toxin can block cholinergic parasympathetic secreto-motor fibers of the salivary gland. Hence, botulinum toxin has been tested in some autonomic disease, such as achalasia, hyperhidrosis and gustatory 49 sweating (Frey syndrome). Lim and Choi have reported that injection of botulinum toxin type A is a highly effective and relatively safe primary method of treatment for an acute post-parotidectomy salivary fistula that, if ISSN 0976 – 044X treated with conventional pressure dressings, takes long to subside.50 Dentofacial Aesthetics Botox and Dermal fillers can provide immediate volume to areas around the mouth, such as the naso-labial folds, marionette lines, and lips to create the proper lip lines, smile lines, and phonetics. Dermal fillers, such as Juvéderm® and Restylane®, are volumizers—or plumpers—that fill out lips and static folds in the face caused by loss of collagen and fat. Botox can also be used in a lip deformity where the lip rises more on one side than the other. It has to be injected at a specific site controlling where the lip goes and how much of it is raised and where and finally, the dreaded “black triangles” which is one of the most challenging aesthetic problems, for which there are very limited successful treatment options. Food particles accumulate in the space and create aesthetic issues. Dermal fillers can be injected into the interdental papilla to plump it and close the interdental space51. Treatment outcome usually last for eight months or longer—at which point the treatment needs to be repeated. Pathologic Clenching Para-functional clenching contributes to periodontal trauma, botulinum toxin type A can limit clenching before and after periodontal surgery to improve healing. Further, in this application, the use of a splint is often contraindicated because the teeth should be functional during healing, so Botulinum toxin acts as a pharmaceutical splint. Orthodontic treatments on patients who are clenchers or have a deep or crossed bite are prolonged if the vertical component of muscular force is greater than the force of the fixed or removable appliance. These cases often require the use of removable functional retainers in combination with regular fixed braces in an attempt to control the component of vertical force22. With the use of botulinum toxin, orthodontic treatment time can be reduced, and patients would be far more comfortable and functional (eating, speaking, swallowing). Retraining Muscles during Orthodontic Treatment Botox can be used to prevent relapse of orthodontic treatment in case of patients with stronger muscle activity such as that of mentalis muscle. Botox can be used to reduce the intensity of the muscle post treatment and over time, the muscle may be retrained to a more physiological movement. Recurrent Dislocation of the Mandibular Condyle It poses a difficult problem for affected patients. In the course of time, dislocations often become more frequent and more difficult to avoid. Even with good patient compliance, conservative treatment is often not sufficient. Operative procedures have also been described for the treatment of temporo-mandibular joint International Journal of Pharmaceutical Sciences Review and Research Available online at www.globalresearchonline.net © Copyright protected. Unauthorised republication, reproduction, distribution, dissemination and copying of this document in whole or in part is strictly prohibited. 158 Int. J. Pharm. Sci. Rev. Res., 37(1), March – April 2016; Article No. 28, Pages: 155-162 dislocation. On the other hand, BOTOX injections into the lateral pterygoid muscles offer the option of a predictable and prolonged period without renewed dislocation.52 Diagnostic Application of Botox It can be used to verify whether the correct diagnosis has been established or not. The pain originating from the ISSN 0976 – 044X pulp will not be relieved when BOTOX is injected into the muscles. Hence, the patients will be certain about the muscular or pulpal origin of the toothache. The diagnostic applications are limited only for the elimination of pain originating from muscles and the pain originating from other structures are not relieved and can be clearly differentiated.17 Table 1 Clinical Applications Mode of Treatment TMJ Disorders Mild-moderate casesBilateral injections of 7.5 U into the anterior vertical fibres of each temporalis muscle. Severe cases2.5 U are given into the middle and posterior third of the temporalis muscles. Tendonitis of temporalismultiple injections of 2.5 U equidistantly spaced in the temple area outside the orbital rim. Masseteric Hypertrophy 5 U injected into the belly of the masseter below an imaginary line joining the tragus of the ear and the corner of the mouth Headache, Migraine & Trigeminal Neuralgia 25-75 U injected into peri-cranial muscles Sialorrhea Autonomic diseases such as achalasia, hyperhidrosis and gustatory sweating (Frey syndrome) Mandibular Spasm 35 units for each lateral pterygoid muscle & 30 units for the sub-mentalis complex Pathologic Clenching five or six injections into the masseter and temporalis muscles, and less often into the lateral pterygoids Dental Implants Prophylactic use of BOTOX injections to the masticatory muscles for relaxation-better implant osseo-integration Oral Surgery Low doses of BOTOX allow traumatized tissues to heal. High doses ''pharmaceutical splint,'' limiting muscle contraction before resetting and during rehabilitation after fracture of the facial bone e.g. fractured mandibular condyle Gummy Smile 0.25 U per muscle bilaterally into the levator labii superioris, levator labii Superioris alaeque nasi, and at the overlap areas of the levator labii superioris and zygomaticus minor muscles. Recurrent Dislocation Mandibular Condyle of the BOTOX injections into the lateral pterygoid muscles. Diagnostic Applications Injection of BOTOX into the muscles aids in differentiation of muscular or pulpal origin of the toothache Myofacial and Neck Pain Injection of muscles with BOTOX effective for myofacial pain caused by trigger points Patient Selection musicians and other media personalities). BOTOX therapy is appropriate for patients in whom other preventive treatments and medications are poorly tolerated or contraindicated, patients who are refractory to other treatments, special patient populations, and patients who simply prefer this treatment.20 Contraindications Afflicted with a neuromuscular disorder (e.g. myasthenia gravis, Eaton-Lambert syndrome). Allergic to any of the components of BTX-A or BTX-B (i.e. BTX, • human albumin, saline, lactose and sodium succinate). Taking certain medications that can interfere with neuromuscular • impulse transmission and potentiate the effects of BTX (e.g. aminoglycosides, penicillamine, quinine, and calcium blockers). Pregnant or lactating (BTXs are classified as pregnancy category • C drugs). Patients should not be treated or treated with extreme 53 caution who are : Psychologically unstable or who have questionable motives and unrealistic expectations. Dependent on intact facial movements and expressions for their livelihood (e.g. actors, singers, International Journal of Pharmaceutical Sciences Review and Research Available online at www.globalresearchonline.net © Copyright protected. Unauthorised republication, reproduction, distribution, dissemination and copying of this document in whole or in part is strictly prohibited. 159 Int. J. Pharm. Sci. Rev. Res., 37(1), March – April 2016; Article No. 28, Pages: 155-162 DISCUSSION ISSN 0976 – 044X Centre for MSK ultrasound) Botox is a safe, conservative, non- surgical, reversible, minimally invasive treatment modality to achieve cosmetic results. Training is absolutely necessary for dentists to administer injections, but learning curve is very short, because dentists can already achieve profound anaesthesia in the orofacial region, thus making patient more comfortable and at ease. Botulinum toxin A is kept frozen (2–40C) in a vial until it is ready to use. The drug is put into solution, following manufacturer’s guidelines, by adding normal saline (preservative-free 0.9% saline solution). Once prepared it should be used within four hours. The preferred syringe is a calibrated 1.0-mL tuberculin syringe, and the needle selected for injection usually is between 26 and 30 gauge. Skin preparation involves alcohol wipes and dry sterile gauze sponges. Aspiration before injection is recommended to avoid involuntary deposition of toxin into the facial arteries. Botulinum Toxin A achieves close to immediate results in one short appointment, but the results are not permanent and last for 6 months, with a range of 4-8 months.55 BOTOX produces partial chemical denervation of the muscle resulting in localized reduction in muscle activity. BOTOX can be used as a sole therapy or as an adjunct to oral medication. The potency of BOTOX is expressed as mouse units. A unit of BOTOX is defined as the LD50 for a colony of 20 gm Swiss-Webster mice, extrapolated to the 70 kg human and each 0.1 ml contain 2.5 U of BOTOX. It is dispensed in small vials containing 100 U or 500 U. The lethal dose of BOTOX in humans is not known. Although it has been estimated to be about 3000 U.20,23 The usual maximum dose recommended for dental applications at an injection session is about 80-100 U. It means that 30 vials of BOTOX will have to be injected before a potentially lethal outcome. There is such a huge disproportion between the clinical dose and the lethal dose that a fatal overdose is almost impossible.56 At the cellular level, 3 to 4 weeks after a single injection of Botulinum toxin A in mice, there is sprouting of new processes along the nerve axon, with formation of multiple synapses with the muscle and up regulation of the muscle nicotinic receptors. Subsequently, the neuronal sprouts undergo regression and the original synaptic connection is restored, with restoration of the original neuromuscular junction. Injections are spaced out for a minimum of 3 months to minimize the risk of antibody formation to the protein, which would prevent BOTOX from working the subsequent time. Specialized equipment can be used for more accurate injections that include: EMG-guided injections (with the NeuroMax 1004) Peripheral nerve stimulator (NS 272) Ultrasound-guided injections (including the Canadian MD injectors (Botox Therapeutic)56 Botulinum toxin type A is marketed worldwide under the name BOTOX (Allergan, Inc. Irvine, CA, USA) and in Europe as Dysport (SpeyWood Pharmaceuticals Ltd., Maiden head, UK).20,23 Hands-on training is essential in learning proper techniques of administration and intertwining them with dental treatment plans. With proper training, dentists are usually more proficient than any of other healthcare professionals in providing these treatments to patients, both for dental and cosmetic needs. The American Academy of Facial Aesthetics is conducting more than 50 local courses a year, has trained more than 6,000 dental professionals from 48 states and 28 countries through comprehensive hands-on live patient two-day facial aesthetic training sessions with Botox and dermal fillers57. The Indian Academy of Facial Aesthetics (IAOFE) in conjunction with the American Academy of Facial Aesthetics (AAFE) is also offering Botox and dermal fillers training course for dentists and physicians.58 CONCLUSION It is evident that the use of Botulinum toxin in the dental profession has a great potential. BOTOX has important clinical uses as an adjunct therapy in temporo-mandibular joint (TMJ) and bruxism cases, and for patients with chronic TMJ and facial pain. BOTOX is also used to complement aesthetic dentistry cases, as a minimally invasive alternative to surgically treating high lip-line cases, for denture patients who have trouble adjusting to new dentures, periodontal cases, gummy smiles, lip augmentation, and also for orthodontic cases where retraining of the facial muscles is necessary. However, much more is still to be discovered before its routine use in dentistry for various conditions. There are still many dental conditions which require FDA approval to be treated by botulinum toxin. They provide patients with most significant, predictable, minimally invasive, aesthetic and therapeutic outcomes available for many everyday clinical situations. Botulinum toxin is no doubt, significant ray of hope which is taking the various dental treatment strategies into an improvised advanced dimension. REFERENCES 1. Pranav Nayyar, Pravin Kumar. BOTOX: Broadening the Horizon of Dentistry. J Clin Diagn Res. 8(12), 2014 Dec, ZE25–ZE29. 2. Barbano, Richard. Risks of erasing wrinkles: Buyer beware! Neurology. 67(10), 2006 Nov, E17–18. 3. Montecucco C, Molgo. J. Botulinal neurotoxins: revival of an old killer. Current Opinion in Pharmacology. 5(3), 2005, 274–79. 4. Meunier FA, Schiavo G, Molgo J. Botulinum neurotoxins: From paralysis to recovery of functional neuromuscular transmission. J Physiol Paris, 96, 2002 Jan-Mar, 105-13. International Journal of Pharmaceutical Sciences Review and Research Available online at www.globalresearchonline.net © Copyright protected. Unauthorised republication, reproduction, distribution, dissemination and copying of this document in whole or in part is strictly prohibited. 160 Int. J. Pharm. Sci. Rev. Res., 37(1), March – April 2016; Article No. 28, Pages: 155-162 5. Aditya Sinha, Megha Hurakadli. Botox and derma fillers: The twin-face of cosmetic dentistry Int J Contemp Dent Med Rev Vol. 2015 6. Edwards, Michael (2006). "Anal fissure". Dumas Ltd. Retrieved. 21, 2006 Aug, 2010. 7. Early Communication about an Ongoing Safety Review of Botox and Botox Cosmetic (Botulinum toxin Type A) and Myobloc (Botulinum toxin Type B). April, 2009 - [accessed 1 December 2010] Available from: http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSaf etyInformationforPatientsandProviders. DrugSafetyInformationforHeath careProfessionals/ucm070366 htm. 8. 9. New Safety Information Regarding Botox and Botox Cosmetic Products. Health Canada. http://www.hcsc.gc.ca/ahcasc/media/advisories-avis/_2009/2009_02eng/php Schames J, Prero YD, Schames D, Schames M, Gabriel W, Reed R. Uncontrollable distant effects of botulinum neurotoxin injections. Calif. Dent J. 37, 2009, 44-45. 10. Bakheit AM. The possible adverse effects of intramuscular botulinum toxin injections and their management. Curr Drug Saf 1(3), 2006, 271-279. 11. Information for Healthcare Professionals: OnabotulinumtoxinA (marketed as Botox/Botox Cosmetic), AbobotulinumtoxinA (marketed as Dysport) and RimabotulinumtoxinB (marketed as Myobloc). FDA Alert Rockville, MD: FDA. 2009. 12. Unclassified Therapeutic Agents. Health Canada. http://www.hcsc. gc.ca/fniah-spnia/nihb-ssna/providefournir/pharmaprod/ med-list/92-00-eng.php 13. Bentsianov BL, Francis A, Blitzer A. Botulinum toxin treatment of temporomandibular disorders, masseteric hypertrophy, and cosmetic masseter reduction. Operative Techniques in Otolaryngology-Head and Neck Surgery. 15(2), 2004, 110-13. 14. Olivo S, Bravo J, Magee DJ, Thei NMR, Major PW, Mir FC. The association between head and cervical posture and temporomandibular disorders: A systematic review. J Orofac Pain. 20(1), 2006, 9-23. 15. Blumenfeld A. Botulinum toxin type A in the treatment of Dental conditions. Inside Dent, 2, 2007, 1-5. 16. Schwartz M, Freund B. Treatment of temporomandibular disorders with botulinum toxin. Clin J Pain, 18, 2002, 198203. 17. Schwartz M, Freund B. Botulinum Toxin A Therapy for Temporomandibular Disorders. Philadelphia, Pa: Lippincott Williams & Wilkins, 2002. 18. Castenada R. Occlusion. In: Kaplan A, Assael L (eds). Temporomandibular Disorders. Philadelphia, Pa: Saunders, 1992. 19. Van Zandijcke M, Marchau MM. Treatment of bruxism with botulinum toxin injections. J Neurol Neurosurg Psychiatry, 53, 1990, 530. 20. Katz H, Blumenfeld A. Can Botulinum toxin A (BOTOX) save your teeth and enhance your smile? Available from: http://sci.tech-archive.net/Archive/sci.med. ISSN 0976 – 044X dentistry/2004-06/0484.html. 21. Gobel H, Heinze A, Heinze-Kuhn K. Botulinum Toxin A is effective in cases of oromandibular dysfunction even if previous bite splint therapy has proved unsuccessful. Cephalalgia. 2001, 514-15. 22. Freund B, Schwartz M, Symington JM. The use of botulinum toxin for the treatment of temporomandibular disorders: Preliminary findings. J Oral Maxillofac Surg. 57(8), 1999, 916-21. 23. Katz H. Botulinum toxin in Dentistry- the new paradigm for masticatory muscle hypertonicity. Singapore Dent, 27, 2005, 7-12. 24. Tan EK. Treating severe bruxism with botulinum toxin. Am Dent Assoc, 131, 2000, 211-6. 25. Lee KM, Chow J, Hui E, Li W. Botulinum toxin type A injection for the management of myofascial temporomandibular pain disorder. Asian J Oral Maxillofac Surg, 17, 2005, 100-3. 26. Kim HJ, Yum KW, Lee SS, Heo MS, Seo K. Effects of botulinum toxin type A on bilateral masseteric hypertrophy evaluated with computed tomographic measurement. Dermatol Surg, 29, 2003, 484-9. 27. Al-Ahmad HT, Al-Qudah MA. The treatment of masseter hypertrophy with botulinum toxin type A. Saudi Med J, 27, 2006, 397-400. 28. Mandel L, Tharakan M. Treatment of unilateral masseteric hypertrophy with Botulinum toxin: Case report. J Oral Maxillofac Surg, 57 1999, 1017-9. 29. Rijsdijk BA, van ES RJ, Zonneveld FW, Steenks MH, Koole R. Botulinum toxin type A treatment of cosmetically disturbing massetric hypertrophy. Ned Tij dschr Geneeskd, 142, 1998, 529-32. 30. Kayikvioglu A, Erk Y, Mavili E, Vargel I, Ozgur F. Botulinum toxin in the treatment of zygomatic fractures. Plast Reconstruct Surg, 111, 2003, 341-6. 31. Ihde S. Prophylactic use of botulinum toxin in dental implantlogy. Cranio-maxillofacial Implant Dir 2007. 32. Nishimura K, Itoh T, Takaki K, Hosokawa K, Naito T, Yakota M. Periodontal parameters of Osseo integrated dental implants: A 4-year controlled follow-up study. Clin Oral Implants Res, 8, 1997, 272-8. 33. Peck S, Peck L, Kataja M. The gingival smile line. Angle Orthod. 62(2), 1992, 91-100. 34. Mazzuco and Hexsel: Gummy smile and botulinum toxin: A new approach based on the gingival exposure area. J AM Acad Dermatol, vol 63, no 6, 1042-1051. 35. Polo M. Botulinum toxin type A in the treatment of excessive gingival display. Am J Orthod Dentofacial Orthop. 127(2), 2005, 214-18. 36. Amin V, Amin V, Swathi, Jabir A, Shetty P. Enhancing the smile with Botox-case report. Global Journal of Medical Research. 13(2), 2013, 14-18. 37. Hwang, et al. Surface anatomy of the lip elevator muscles for the treatment of gummy smile using botulinum toxin. Angle Orthod. 79(1), 2009, 70-77. International Journal of Pharmaceutical Sciences Review and Research Available online at www.globalresearchonline.net © Copyright protected. Unauthorised republication, reproduction, distribution, dissemination and copying of this document in whole or in part is strictly prohibited. 161 Int. J. Pharm. Sci. Rev. Res., 37(1), March – April 2016; Article No. 28, Pages: 155-162 38. http://www.vancouverlaser.com/procedurestreatments/botox-before-after-photos-05/ 39. Blitzer A, Brin MF, Greene PE, Fahn S. Botulinum toxin injection for the treatment of oromandibular dystonia. Ann Otol Rhinol Laryngol. 98(2), 1989, 93-97. 40. Brin MF, Fahn S, Moskowitz C ,Friedman A, Shale HM, Greene PE, Blitzer A, List T Localized injections of botulinum toxin for the treatment of focal dystonia and hemifacial spasm. Mov Disord. 2(4), 1987, 237-54. 41. Hermanowicz N, Truong DD. Treatment of oromandibular dystonia with botulinum toxin. Laryngoscope. 101(11), 1991, 1216-18. ISSN 0976 – 044X 48. Elcio JP. BOTOX injections relieve severe facial pain. Available from: http://www.newsmedical.net/news/2005/10/25/14010.aspx. 49. Laskawi R, Drobik C, Schönebeck C. Up-to-date report of botulinum toxin type A treatment in patients with gustatory sweating (Frey's syndrome). Laryngoscope. 108(3), 1998, 381-84. 50. Lim YC, Choi EC. Treatment of an acute salivary fistula after parotid surgery: [43] botulinum toxin type A injection as primary treatment. Eur Arch Otorhinolaryngol. 265(2), 2008, 243-45. 51. http://www.dentaltown.com/dentaltown 42. Jankovic J, Orman J. Botulinum toxin for cranial-cervical dystonia: a double-blind, placebo-controlled study. Neurology. 27, 1987, 616-23. 52. Moore AP, Wood GD. Medical treatment of recurrent Temporomandibular joint dislocation using botulinum toxin A. Br Dent J, 183, 1997, 415-7. 43. Laskawi R, Rohrbach S. Oromandibular dystonia. Clinical forms, diagnosis and examples of therapy with botulinum toxin. Laryngorhinootologie. 80(12), 2001, 708-13. 53. Patel D, Mehta F, Trivedi R, Thakkar S, Suthar J. Botulinum Toxin and Gummy -A Review. IOSR Journal of Dental and Medical Sciences. 4(1), 2013, 1-5. 44. Tan EK, Jankovic J. Botulinum toxin A in patients with oromandibular dystonia: Long-term follow-up. Neurology. 53(9), 1999, 2102-07. 54. Binder WJ, Brin MF, Blitzer A, Schoenrock LD, Pogoda JM. Botulinum toxin type A (BOTOX) for treatment of migraine headache: an open-label study. Otolaryngol Head Neck Surg, 123, 2000, 669-76. 45. Jeynes LC, Gauci CA. Evidence for the use of botulinum toxin in the chronic pain setting-a review of the literature. Pain Pract, 8, 2008, 269-76. 46. Silberstein S, Mathew N, Saper J, Jenkins S. Botulinum toxin type A as a migraine preventive treatment. For the BOTOX Migraine Clinical Research Group. Headache, 40, 2000, 445-50. 47. Lawrence R. BOTOX for Headache: Mechanism of Action? (Available from: http://www.headachedrugs.com.Migrainepage.formulatio n.net) 55. Grover S, Malik V, Kaushik A, Diwakar R, Yadav P. A Future perspective of Botox in Dentofacial Region. J Pharm Biomed Sci. 04(05), 2014, 525-31. 56. Dr. G. Ko How Botox works for the treatment of chronic pain: Available from: http://www.drkoprp.com/pdfs/botox Info.pdf –Canada 57. www.FacialAesthetics.org 58. http://www.iaofe.com/about.html Source of Support: Nil, Conflict of Interest: None. International Journal of Pharmaceutical Sciences Review and Research Available online at www.globalresearchonline.net © Copyright protected. Unauthorised republication, reproduction, distribution, dissemination and copying of this document in whole or in part is strictly prohibited. 162