Urinary lipoarabinomannan (LAM) detection as a diagnostic test for TB
advertisement

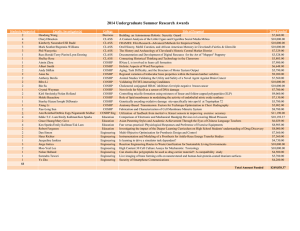
Urinary lipoarabinomannan (LAM) detection as a diagnostic test for TB Dr Ankur Gupta-Wright Clinical Research Fellow London School Hygiene & Tropical Medicine/Malawi-Liverpool-Wellcome Trust Clinical Research Programme Overview • • • • • • What is LAM? How do we detect LAM? How accurate are urine LAM assays for diagnosing TB? How does LAM end up in the urine of TB patients? In whom should and shouldn’t we use LAM assays? Can using LAM assays impact patient outcomes? Background • HIV-TB still causes significant morbidity and mortality • TB causes between 1/3 and 2/3 deaths in HIV+ adults admitted to hospital in SSA • 50% of this TB disease is undiagnosed at the time of death • Current (sputum-based) diagnostics are inadequate in this population • Need improved diagnostic strategies to reduce TB deaths What is lipoarabinomannan (LAM)? How do we detect LAM in urine? Determine TB-LAM Ag assay Negative Positive Control band Patient sample result Sample pad Lawn et al Lancet Infect Dis 2012 Positive How accurate is Urine TB-LAM testing? 100 • Overall sensitivity is ‘inadequate’ (<30% sensitivity) • Moderate to good sensitivity in advanced HIV, linked to CD4 cell count • Good specificity (>99%) when correct reference standard is used • Diagnoses sickest patients at the highest risk of death 90 80 Sensitivity (%) 70 60 50 40 30 20 10 0 <50 50-150 >150 All patients Lawn et al. JAIDS 2012 How does LAM end-up in urine of TB patients? • Filtration of LAM from blood in the kidney was the early hypothesis • Bound LAM is too large to be filtered by healthy kidneys • Evidence of renal TB from post-mortem studies (e.g. Cox et al PLoS One 2015) • Microbiology supports the renal TB hypothesis -evidence of whole TB bacilli in urine of LAM positive patients -strong association with MTB bacteraemia Images courtesy of Prof. Sebastian Lucas Observations explained by haematogenous renal TB • Utility of the assay is restricted to HIV+ patients with low CD4 cell counts -target the correct patient population • Urine-LAM antigenuria is a predictor of mortality in HIV-TB • Specificity is sub-optimal when the reference standard does not include extra-pulmonary samples In whom should and shouldn’t we use LAM assays? • WHO policy guidance November 2015 • Shouldn’t be used for the diagnosis of TB except… • may be used to assist in the diagnosis of TB in HIV positive adult in-patients with signs and symptoms of TB who have a CD4 <100 cells/µL, are seriously unwell (conditional recommendation; low quality of evidence) • Shouldn’t be used as a screening test for TB Can using LAM assays impact patient outcomes? • LAM RCT- adjunctive LAM testing for hospitalised patients ‘suspected of having TB’ • 4 sites (SA, Zim, Zambia, Tanzania) • Randomised 2659 patients • 2 month mortality: -no LAM arm 24.9% -LAM arm 20.8% -aRR 0.83 (95%CI 0.03-0.96, p=0.012) • One of the first trials of a TB diagnostic to show an impact on mortality STAMP trial • RAPID URINEBASED SCREENING FOR TB TO REDUCE AIDS-RELATED MORTALITY IN HOSPITALIZED PATIENTS IN AFRICA • 2 sites: -Zomba, Malawi -PMB, South Africa Summary • • • • • Need for better diagnostics for HIV-associated TB Detectable LAM in urine is a marker of renal TB Potential utility in advanced HIV (when disseminated/renal TB is more common) Needs to be applied to the correct patient population Potential to improve patient outcomes, as demonstrated by a recent RCT Questions? • Thanks for listening • Thanks to funders: Global Health Trials (MRC/WT/DfID) Royal College of Physicians London • Thanks to my supervisors: Prof Stephen Lawn Prof Liz Corbett