The Genetics of Introduction
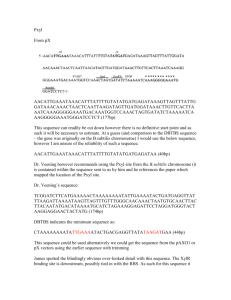
advertisement

Introduction The Genetics of Osteoporosis Mr. Christopher Vidal B.Sc.(Hons.) Supervisor: Prof. Angela Xuereb Ph.D. (Co-supervisor: Prof. Alex Felice Ph.D.) Osteoporosis is a complex metabolic bone disease characterised by a decrease in bone mineral density and deterioration of the microarchitecture of bone leading to an increased risk of fractures. The pathogenesis of osteoporosis depends upon peak bone mass reached early in life and the rate of bone loss in later years, especially in postmenopausal women. An individual’s increased risk of disease depends upon both environmental and genetic factors. Genetics of Osteoporosis Genes associated with osteoporosis Osteoporosis is a polygenic disease where Vitamin D Receptor (VDR) Oestrogen Receptor (ER1) Osteoprotegerin (TNFRSF11B) Collagen Type 1 (COL1A1,COL1A2) Lipoprotein Related Protein-5 (LRP5) Methylenetetrahydrofolate reductase (MTHFR) Transforming growth factor-β (TGFβ) Bone Morphogenic Protein 2 (BMP2) Androgen receptor (AR) Bone Gla Protein (osteocalcin) Sclerostin (SOST) Tumour Necrosis Factor Receptor 2 (TNFR2) Lysyl Hydroxylase (PLOD1) Interleukin 6 (IL-6) Insulin-like Growth factor 1 (IGF-1) T-Cell Immune Regulator (TCIRG1) multiple gene variants each having a small effect contribute to an individual’s increased susceptibility to the disease. A number of chromosomal loci and single nucleotide polymorphisms (SNPs) found within candidate genes have been associated with BMD and/or fracture risk. [Ref.1] [Ref.2] [Ref.3] [Ref.4] [Ref.5] [Ref.6] [Ref.7] [Ref.8] [Ref.9] [Ref.10] [Ref.11] [Ref.12] [Ref.13] [Ref.14] [Ref.15] [Ref.16] Genetic Studies Aims of Study Linkage Studies (gene mapping) To evaluate the role of candidate loci in The search for the co-inheritance of phenotype and genotype in families with multiple affected individuals Analysis for co-inheritance with disease of highly polymorphic markers (STRs) spread at regular intervals in the genome. The LOD score is the probability expressed as a log base 10 of the likelihood ratio of linkage between marker and disease. Whole genome scan Candidate gene approach Association Studies (case-control) The search for association of a marker allele with disease by comparing its frequency in affected and unaffected individuals in a population. Analysis of single nucleotide polymorphisms (SNPs) that can be functional or non-functional. If association is found then determine whether the SNP itself is causing the disease or whether it is in linkage disequilibrium with a nearby mutation. families with multiple affected individuals To confirm the role of candidate loci indicated by previous linkage studies in Maltese families To localise and confirm susceptibility alleles for osteoporosis in the Maltese population 1 Study Approach Patient Recruitment Linkage 125 postmenopausal women were recruited from new subjects study in two extended Maltese families using selected markers at eight candidate regions where known genes for osteoporosis are found (candidate gene approach). Association study in a random population of postmenopausal women. Pedigree 1 Methodology - STR genotyping DNA was extracted from peripheral blood leucocytes by salting out DNA concentration was measured by spectrofluorometry using PicoGreen (Molecular Probes Inc, USA). DNA concentrations were adjusted to a final concentration of 10ng/ul. 39 STRs located on 8 chromosomal regions were analysed in 27 family members from 2 pedigrees. STRs had an average heterozygosity of 0.76 with an average spacing of 8.6cM. PCR was performed using fluorescently labelled primers and fragment analysis was performed by denaturing capillary electrophoresis technique using a 3730xl ABI Genetic Analyser. This work was performed in a commercial laboratory (McGill University and Genome Quebec Innovation Centre, Canada) referred to the Bone Density Unit, St. Luke’s Hospital. Menopause was defined as amenorrhoea of at least six months duration. Two families were recruited from probands selected from individuals that participated in the association study and were observed to have severe osteoporosis as defined by WHO criteria (BMD t-score <-2.5) and low z-score at the LS and/or FN. These individuals were also relatively young in age. All participants from these families answered a detailed questionnaire concerning medical conditions, use of medications, lifestyle and dietary habits as well as family history of osteoporosis. BMD at the LS and FN was measured by DEXA using a Norland 385 densitometer. Peripheral blood was collected for DNA analysis and biochemical tests to exclude secondary osteoporosis. Pedigree 2 Table 1. Chromosomal Regions Analysed in this study Chromosome Locus Genes 1 1p36 MTHFR, TNFR2, PLOD1, ALP, Chloride channel 8 8q24 TNFRSF11B (OPG) 11 11q12-13 LRP5, TCIRG1 12 12q13.1-q13.2 VDR, COL2A1, BMP11, PTH-like hormone 17 17q21.31-q22 COL1A1, SOST 18 18q22.1 RANK 20 20p12 BMP-2 X Xq11.2-q12 AR 2 Methodology – SNP genotyping Statistical Analysis DNA was extracted by salting out from peripheral blood Linkage and Association analyses were performed leucocytes. Target sequences of 17 SNPs found within 6 candidate genes (VDR, ER1, TNFRSF11B, COL1A1, LRP5, MTHFR) were amplified by PCR using appropriate primers. PCR products were then digested using specific restriction enzymes to the polymorphic region. An SNP either introduces or abolishes a cut site for an endonuclease. Digested products were then analysed by agarose or polyacrylamide gel electrophoresis. Serum procollagen type I (Prolagen C) and urinary deoxypyridinoline crosslinks (DpD) were used as biochemical markers of bone formation and resorption. Genotyping was performed at the DNA Laboratory, Medical School, G’Mangia, Malta. Results – Linkage Analysis The pedigrees were analysed separately using both parametric and non-parametric analyses. For the mild phenotype, affected individuals were defined as those having an age and sex matched z-scores of <-1.0. A more severe phenotype was also used, where affected individuals in the first generation were defined according to WHO criteria as osteoporotic (t-score <-2.5), while affected individuals in the second generation (pre-menopausal women and men) were defined by a z-score of <-2.0 (as recommended by the International Society of Clinical Densitometry). Four different penetrances were used in the analysis ranging from a complete dominant to a recessive mode of inheritance. Results – Family 1 using statistical software: Cyrillic v2.1 to construct the pedigrees and input STR genotypes MLINK GENEHUNTER v1.2 to compute LOD and NPL scores Linkage Disequilibrium Analyser (LDA) used to test for LD between different SNPs EH software used to calculate LD between haplotypes and disease by comparing cases and controls SPSS student version 9.0 used to test for correlation between BMD and different genotypes Table 2. Clinical Characteristics Variable Affected Unaffected N (M/F) 17 (5/12) 11 (8/3) Age (years) 50.0 41.8 Weight (Kg) 63.3 67.8 Height (cm) 155.6 162.8 BMI (kg/m2) 26.0 25.7 Obesity (Normal/Obese) 15/2 9/2 Fractures (no/yes) 14/3 10/1 Ionised Calcium (mmol/l) 1.28 1.29 Smokers/non-smokers 3/14 3/8 LS BMD (g/cm2) 0.785 1.000 FN BMD (g/cm2) 0.741 0.879 Fig.1 Inheritance of STRs on Chromosome 8 No evidence of linkage was observed with loci 1p36, 18q22.1, 20p12 and Xq11.2-q12 in this family. An NPL score of 3.69 (p=0.009) and LOD of 1.34 were observed to marker D8S1128 for a dominant mode of inheritance of a low BMD phenotype. When a severe phenotype was tested both NPL and LOD increased to 4.17 and 2.28 (Fig.1 – 3). An NPL of 3.61 (p=0.03) was observed to marker D17S1293 with a LOD score of 1.93 for a dominant mode of inheritance with 90% penetrance (Fig. 4 – 6). Marker D11S2002 gave an NPL score of 2.65 (p=0.04) when a severe phenotype was analysed. 3 Fig. 2 NPL Plot of Chromosome 8 Fig.3 LOD of Chromosome 8 Fig.4 Inheritance of STRs on Chromosome 17 Fig.5 NPL Plot of Chromosome 17 Fig.6 LOD Plot of Chromosome 17 Results – Family 2 No evidence of linkage was observed for markers on chromosomes 1, 8, 11, 12 and X in this family. Highest NPL of 6.11 (p=0.002) was observed to marker D17S1865 with an LOD of 2.04 on chromosome 17, for a low BMD phenotype (Fig. 7 – 10). Suggestive linkage was observed with a severe phenotype and marker D18S484 with an NPL score of 3.24 (p=0.04) and a LOD of 1.47 for a dominant mode of inheritance with penetrance 0.90. When added, the highest NPL score between the two families was of 7.08 for marker D17S1865 on chromosome 17. 4 Fig.7 Inheritance of STRs on Chromosome 17 Fig.8 NPL Score for Chromosome 17 Fig.9 LOD Score for Chromosome 17 Fig.10 Informative Markers on Chromosome 17 Results – Association Study Fig. 11 TNFRSF11B (OPG) T950C Genotype Distribution Between Unaffected and Affected (Osteopenic + Osteoporotic) Individuals All polymorphisms studied in the Maltese population 100 80 83 60 59 40 Percentage (%) were found to be in Hardy-Weinberg equilibrium. No statistical significant difference (p>0.05) was reached for LS and FN BMD between individuals of different genotypes, for all SNPs studied. Statistical significance difference was observed in the distribution of genotypes between affected and unaffected individuals for the TNFRSF11B T950C SNP (χ2 = 9.7; p = 0.01; df = 2) with the TT genotype found more frequently in the affected group (Fig. 11). A significant odds ratio of 2.11 (95% CI: 1.26 – 3.55) was obtained when assuming the T allele of the same polymorphism as a risk for low BMD. 57 43 41 OPG T950C (HpaI) TT 20 17 TC 0 CC Normal Low BMD Bone status LS and FN chi=9.7; df=2; p=0.01 5 Table 3 VDR Gene Haplotype Frequencies in Affected and Unaffected Individuals Linkage Disequilibrium Strong LD was observed between a number of SNPs within the VDR, ER1, TNFRSF11B, COL1A1 and LRP5 genes. Haplotype frequencies within these genes were then compared between affected and unaffected individuals using the EH software. No association was observed between VDR, ER1 and LRP5 haplotypes with an increased risk of osteoporosis (Table 3) Significant association was observed between haplotypes in the TNFRSF11B (Table 4) and COL1A1 genes with an increased risk osteoporosis. The A-T-G haplotype in the promoter region of the TNFRSF11B was more frequently found in affected individuals (51.7%) when compared to normal controls (34.1%) (Table 4). Haplotype G-T-T (B-A-T) Unaffected 0.011 Affected 0.009 G-G-T (B-a-T) G-T-C (B-A-t) G-G-C (B-a-t) A-T-T (b-A-T) 0.011 0.378 0.000 0.156 0.000 0.438 0.000 0.170 A-G-T (b-a-T) A-T-C (b-A-t) A-G-C (b-a-t) 0.444 0.000 0.000 0.384 0.000 0.000 χ2 = 9.18; p = 0.24; df = 7 The Role of OPG in Osteoclast Differentiation and Activation Table 4 TNFRSF11B Gene Haplotype Frequencies in Affected and Unaffected Individuals Haplotype A-T-G Affected 0.517 Unaffected 0.341 A-T-C A-C-G A-C-C G-T-G 0.000 0.052 0.347 0.000 0.015 0.012 0.496 0.080 G-T-C G-C-G G-C-C 0.051 0.024 0.090 0.023 0.105 0.000 χ2 = 24.66; p < 0.001, df = 7 Conclusions In this study evidence of linkage was observed to a marker found in locus 17q21.31-q22 indicating that a gene responsible for osteoporosis might be present in this region. In a family with high incidence of severe osteoporosis and hypertension, suggestive linkage was observed to other loci where candidate genes for both diseases are known to be found. This might help in the identification of a gene that links osteoporosis with hypertension and atherosclerosis (Table 5). Differences in loci identified between the two families is an evidence of genetic heterogeneity in the disease. Association of the A-T-G haplotype with increased risk for low BMD indicates the possible role of the TNFRSF11B gene variants in postmenopausal bone loss. Also an increased frequency in affected individuals of the haplotype in the COL1A1 gene promoter, shows the importance of this structural gene in bone mass. Table 5. Candidate Genes Indicated by Linkage Locus Osteoporosis Hypertension 17q21.31-q22 SOST, COL1A1, NOG Angiotensin 1 converting enzyme (ACE) * 8q24 TNFRSF11B* Angiopoietin 1, Squalene epoxidase 11q12-13 LRP5 Angiotensinase C (PCP) ** •*Genes already associated with both osteoporosis and atherosclerosis •**Essential Hypertension Susceptibility Locus 6 Future Studies Acknowledgments Increasing the number of STRs on chromosome 17 Prof. Angela Xuereb for her constant supervision and where strong evidence of linkage was observed. This helps in narrowing the interval and so increasing the chance to localise the gene (high resolution scan). Sequencing of interesting genes to identify possible mutations that might be responsible for osteoporosis. Gene expression studies to identify the biological effects of polymorphisms found in the promoter region of the TNFRSF11B. support throughout the study. Prof. Alex Felice for his supervision and use of facilities at the Laboratory of Molecular Genetics, University of Malta. Dr. Raymond Galea for his assistance in patient recruitment. Prof. Mark Brincat for his support. Dr. Marios Kambouris for his informative discussions and linkage software. This work was supported by the Research Fund Committee, University of Malta References 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. Morrison NA et al., (1994) Prediction of bone mineral density from vitamin D receptor alleles. Nature 367: 284 – 287. Kobayashi S, et al., (1996) Association of bone mineral density with polymorphism of the estrogen receptor gene. J Bone Miner Res 11: 306 – 311. Langdahl BL, et al., (2002) Polymorphisms in the osteoprotegerin gene are associated with osteoporotic fractures. J Bone Miner Res 17: 1245 – 1255. Grant SF, et al., (1996). Reduced bone density and osteoporosis associated with a polymorphic Sp1 binding site in the collagen type I alpha 1 gene. Nat Genet 14: 203 – 205. Little et al., (2002) A mutation in the LDL receptor-related protein 5 gene results in the autosomal dominant high-bone mass trait. Am J Hum Genet 70: 11 – 19. Jorgensen HL, et al., (2002) Association of a common allelic polymorphism (C677T) in the methylene tetrahydrofolate reductase gene with reduced risk of osteoporotic fractures. A case control study in Danish postmenopausal women. Calcif Tissue Int 71: 386 – 392. Langdahl BL, et al., (2003) Polymorphisms in the transforming growth factor beta 1 gene and osteoporosis. Bone 32: 297 – 310. Styrkarsdottir et al., (2003) Linkage of osteoporosis to chromosome 20p12 and association to BMP-2. PLOS Biology 1: 1 – 10. Yamada, Y., et al., (2005) Associations of polymorphisms of the androgen receptor and klatho gene with bone mineral density in Japanese women. Journal of Molecular Medicine 83, 50 – 57. Dohi, Y., et al., (1998) A novel polymorphism in the promoter region for the human osteocalcin gene, The possibility of a correlation with bone mineral density in postmenopausal Japanese women. Journal of Bone and Mineral Research 13, 1633 – 1639. Uitterlinden, A.G., et al., (2004) Polymorphisms in the sclerosteosis/van Buchem disease gene (SOST) region are associated with bone mineral density in elderly whites. American Journal of Human Genetics 75, 1032 – 1045. Albagha, O.M.E., et al., (2002) Linkage disequilibrium between polymorphisms in the human TNFRSF1B gene and their association with bone mass in perimenopausal women. Human Molecular Genetics 11, 2289 – 2295. Spotila, L.D., et al., (2003) Association analysis of bone mineral density and single nucleotide polymorphisms in two candidate genes on chromosome 1p36. Calcified Tissue International 73, 140 – 146. Moffett, S.P., et al., (2004) Association of the G-174C variant in the interleukin-6 promoter region with bone loss and fracture risk in older women. Journal of Bone and Mineral Research 19, 1612 – 1618. Kim, J.G., et al., (2002) The relationship among serum insulin-like growth factor-I, insulin-like growth factor-I gene polymorphism, and bone mineral density in postmenopausal women in Korea. American Journal of Obstetrics and Gynaecology 186, 345 – 350. Sobacchi, C., et al., (2004) Association between a polymorphism affecting an AP1 binding site in the promoter of the TCIRG1 gene and bone mass in women. Calcified Tissue International 74, 35 – 41. 7