filing activities Standardising pharmacist patient-pro in a rehabilitation hospital in Malta
advertisement

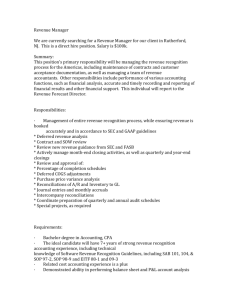
Research ORIGINAL ARTICLE Standardising pharmacist patient-profiling activities in a rehabilitation hospital in Malta Maria Mamo, Francesca Wirth, Lilian M Azzopardi, Anthony Serracino-Inglott Department of Pharmacy, University of Malta, Msida, Malta Correspondence to Maria Mamo, Department of Pharmacy, University of Malta, Msida, Malta; mmam0004@um.edu.mt Received 12 June 2013 Revised 27 August 2013 Accepted 9 September 2013 ABSTRACT Objectives To develop, validate, test for applicability and practicality, implement and undertake a preliminary evaluation of a standard operating procedure (SOP) for pharmacist patient-profiling activities at Rehabilitation Hospital Karin Grech (RHKG). Methods Following direct observation of pharmacist patient-profiling activities in the hospital, a draft SOP was developed. The SOP was validated twice using a self-administered validation questionnaire and was amended according to suggestions proposed during validation. The validated SOP was tested for applicability and practicality through an observation study. Pharmacists were trained to follow the SOP correctly and the SOP was subsequently implemented. Preliminary evaluation of the SOP was undertaken using a selfadministered evaluation questionnaire 1 and 4 months post implementation. Results A ‘patient-profiling’ SOP for pharmacists was developed. Validation was beneficial since constructive suggestions were proposed and improvements with respect to SOP content, length, presentation, layout and comprehensiveness were implemented to develop the final version of the SOP. The SOP was found to be practical and applicable for use at RHKG. Preliminary evaluation showed that all pharmacists (nine) found the SOP fit for purpose, easy to follow for training new pharmacists, user friendly, easy to understand and promotes consistency in patient-profiling activities. Conclusions The ‘patient-profiling’ SOP provides a comprehensive approach to standardisation of pharmacist patient-profiling activities at RHKG to improve the quality of patient care. The SOP will need to be regularly reviewed and updated and can be transferred to other hospital settings with minor amendments. INTRODUCTION To cite: Mamo M, Wirth F, Azzopardi LM, et al. Eur J Hosp Pharm Published Online First: [ please include Day Month Year] doi:10.1136/ejhpharm2013-000351 Quality in healthcare is accomplished when patient care conforms to current regulations, provides services consistent with current professional knowledge and results in optimal patient outcomes, with the fewest possible adverse effects and at reduced costs.1 2 Hospitals worldwide are becoming increasingly aware of the importance of accountability and transparency in healthcare, motivating the implementation of standard operating procedures (SOPs) for healthcare processes.3 4 Documentation, standardisation and validation processes allow assessment of hospital services and ensure that the service provided is targeted towards the quality of patient care.5 The importance of introducing quality and standardisation in healthcare has been recognised, however it is occurring at a relatively slow pace in European Mamo M, et al. Eur J Hosp Pharm 2013;0:1–5. doi:10.1136/ejhpharm-2013-000351 countries,6 particularly with respect to clinical pharmacy services. Examples of initiatives in Northern Ireland and Sweden have been reported from the Intregrated Medicines Management project,7 the Lund Integrated Medicines Management project8 and Uppsala projects, respectively.9 Hudson et al10 emphasised that “there continues to be a need to establish documented standards of clinical pharmacy” to sustain such a service. Within a clinical setting, written SOPs provide evidence that the hospital is working within requirements of clinical governance. Regularly updated, well written, efficiently organised and well formatted SOPs demonstrate commitment to high standards of performance and documentation.11 SOPs should be implemented to assure safety and consistency of a service, ensure good practice, clarify job descriptions, facilitate audit review of clinical practice, provide an opportunity to analyse existing working procedures and implement improved procedures, and serve as a tool for training new recruits.11 12 Additionally, SOPs lead to development of standardised documentation systems which ensure that patient medication records are complete and accessible to pharmacists and other members of the healthcare team.13 The main limitations of documented standards are that they may be perceived as time consuming to follow and produce a large amount of paperwork.11 14 Clinical pharmacists proactively participate in patient care through interaction with other members of the healthcare team to support safe and effective medication use.15 Pharmacists make recommendations to physicians in various hospital settings with respect to dosing and administration of medications, current evidence-based treatment guidelines, adverse drug reactions (ADRs), drug interactions, intravenous drug compatibility and drug therapy monitoring.16 Documentation of interventions is important to enable pharmacist accountability and continuity of care, and to demonstrate the value of clinical pharmacy service provision to high-quality care and improvement of patient outcomes.17–19 ‘Patient profiling’ was selected as an activity for standardisation because, from a time and motion study undertaken at Rehabilitation Hospital Karin Grech (RHKG), 15% of the pharmacists’ time dedicated to clinical pharmacy activities was for patient profiling. During this study a lack of consistency between pharmacists with regards to documentation of pharmaceutical care issues was identified.20 ‘Patient profiling’ is an activity undertaken by pharmacists which involves filling in a new ‘pharmacy patient profile’ for each patient admitted to RHKG and updating it during the patient’s stay in hospital. 1 Research A pharmacy patient profile is a paper-based patient record used by pharmacists as a medication-review tool by documentation of patient information, medications, laboratory investigations and pharmaceutical care issues (table 1). This record is filled in using consulting patient notes, treatment charts, laboratory investigations and also during patient/carer interviews. Emphasis on documentation of pharmaceutical care issues is made to prepare for interventions in collaboration with physicians during ward rounds. The aim of this study was to develop, validate, test for applicability and practicality, implement and undertake preliminary evaluation of a SOP for pharmacist patient-profiling activities in a rehabilitation hospital. METHOD Setting The study was undertaken at RHKG, a 155-bed hospital consisting of four geriatric rehabilitation wards and one adult rehabilitation ward. The pharmacy department consists of 12 members: nine pharmacists (Head of Pharmacy Services, Clinical Pharmacy Coordinator and five full-time and two part-time pharmacists), two pharmacy technicians and a pharmacy clerk. All pharmacists have clinical pharmacy duties and these cover around 60% of their time.20 Patient care at RHKG is provided through an interdisciplinary team approach, including physicians, nurses, pharmacists, physiotherapists, occupational therapists, speech language pathologists and social workers. Development of SOP Approval to carry out the study was obtained from the RHKG Research Committee and the Head of Pharmacy Services. The investigator carried out direct observation of 11 patientprofiling sessions (each session involving one patient), observing (three) different pharmacists over an 18-day period to develop the SOP content. A detailed list of steps carried out by the pharmacists during patient profiling was documented. Following this observation, inconsistencies among pharmacists and weaknesses in the current patient-profiling process that needed to be strengthened were identified. Points for improvement in consistency, particularly with regards to documentation of pharmaceutical care issues, were discussed with the pharmacists for inclusion in the SOP. The SOP was divided into a ‘title page’ and nine sections: ‘Scope’, Table 1 Information collected during ‘patient profiling’ Patient information Patient medication records Active medication problems Pharmaceutical care issues Laboratory investigations Therapeutic drug monitoring First and last name, address, identification card number, age, consultant responsible for patient, date of admission, place from where patient was admitted, reason for referral, carer/s name and telephone number Past medical history, drug history, ADRs/sensitivities, current medications—noting start and stop date (if applicable), presence/absence of catheter, presence/ absence of enteral tube Date of onset, problems identified, comments, date resolved Date when pharmaceutical care issue arose, care issue, date when action is taken, action taken, date of outcome, outcome Weight, height, laboratory investigations within range are ticked, serum creatinine, estimated glomerular filtration rate, potassium, urea, calcium, albumin+any abnormal results are always recorded Medication, reference range, result, date and time of last dose administered, date and time of last sample taken, comments ADR, adverse drug reaction. 2 ‘Objective’, ‘Definitions’, ‘Responsibility’, ‘Competences’, ‘Procedure’, ‘References’, ‘Revision history’ and ‘Appendices’. Details of the process were described in the ‘Procedure’. This section was structured in a ‘hierarchical steps’ format with a flowchart because it was long, detailed and required many decisions. Steps were written as short, direct sentences in the imperative form with emphasis on accuracy, comprehensiveness and user friendliness. Validation of SOP Validation was undertaken to confirm the robustness, comprehensiveness, presentation and consistency of the SOP. Communication with the pharmacists was sought during the entire validation process to ensure user satisfaction, which results in an improved sense of responsibility to follow the SOP. The draft SOP was validated twice by a validation panel consisting of the nine pharmacists. Each member was given a consent form and contact details of the investigator, SOP draft, validation sheet (divided according to the SOP sections with instructions to tick appropriately if they agree or disagree with the selected statements, with the possibility to include other remarks) and self-administered validation questionnaire (divided into five sections to rate presentation, comprehensiveness, topic specificity, statement validity with the possibility to include other comments). Font clarity and size, readability of layout, line spacing, SOP length and order of sections were validated with regards to presentation. The pharmacists were given 1 month to complete the first validation and 2 weeks to complete the second validation. Amendments suggested were considered and a third draft of the SOP was developed. The questionnaires of both validations were scored out of a total score of 12. Descriptive comparative analysis using the one-way analysis of variance test was undertaken. Applicability and practicality testing of SOP Applicability and practicality testing was undertaken to ensure relevance of the SOP to be used in practice at RHKG. An observation study using a checklist was undertaken over 5 days on the five wards. The SOP was tested by observing four pharmacists complete 12 patient profiles (three each) and comparing their actions with the steps included in the third draft of the SOP. This step compared the normal routine patient-profiling activity with that documented in the SOP. Discrepancies were clarified and discussed with the pharmacy staff and a final SOP draft was developed and subsequently implemented. Implementation of SOP and training The final version of the SOP was authorised for implementation following applicability and practicality testing. Implementation involved training pharmacists to familiarise themselves with the SOP and follow it correctly, and distribution of authorised copies in specific distribution points. Reading copies of the original, in hard and soft copy format, were issued, marked as such and used for pharmacist training. An electronic reading copy was placed on the main computer system in the pharmacy to allow access to the SOP by all pharmacists. Authorised copies of the original were subsequently issued, marked as such, and placed in seven distribution points: the pharmacy, the office of the hospital clinical director and the five wards. The pharmacists were given 1 week to read and understand the SOP, clarify any ambiguous areas of the SOP with the Head of Pharmacy Services and sign a ‘Read and Understood Form’. Preliminary evaluation of SOP The implemented SOP was evaluated twice: a preliminary evaluation 1 and 4 months post implementation. A group discussion Mamo M, et al. Eur J Hosp Pharm 2013;0:1–5. doi:10.1136/ejhpharm-2013-000351 Research session between the pharmacists and the investigators (MM, FW) was held to evaluate the SOP during both evaluations. A self-administered evaluation questionnaire was distributed. The questionnaire consisted of 11 ‘Yes/No’ and 2 open-ended questions relating to the SOP sections, SOP characteristics (user friendliness, detail, length), experience from implementation, SOP value to service provision and frequency of referral to the SOP. The results obtained from both evaluations were compared. RESULTS Rationale of ‘patient-profiling’ SOP The ‘patient-profiling’ SOP developed describes in detail the procedure to be followed by pharmacists when filling in a pharmacy patient profile to ensure that it is complete and accurate to be used as a medication review tool during the patient’s stay in hospital. The procedure section was divided into three main sections: completing the pharmacy patient profile; documentation of pharmaceutical care issues; and a flowchart which summarises the entire procedure. In the first section, the pharmacist is guided to fill in the patient profile with information including patient and carer details, reason for referral, past medical history, medication history, current medications, ADRs and sensitivities, mental score, presence/absence of a catheter, presence/ absence and type of enteral tube, active problems, weight, height, ideal body weight, laboratory investigations and therapeutic drug monitoring (TDM). In the second section, the pharmacist is guided to classify and document pharmaceutical care issues identified during patient-profiling activities. Improvements in patient profiling activities implemented A new version of the paper-based pharmacy patient profile, with an improved layout, was designed and implemented. The layout of the patient profile was modified to allow more space to document pharmaceutical care issues, active problems, laboratory investigations and TDM. A classification system for pharmaceutical care issues, adapted from the one developed at the University of Strathclyde in Scotland,10 was implemented at RHKG to improve identification, implementation, classification and documentation of pharmaceutical care issues by pharmacists during patient profiling. The pharmaceutical care issues identified were classified into five main categories based on ‘Indication’, ‘Effectiveness’, ‘Safety’, ‘Compliance’ and ‘Administration’ of medications. Such a system is important to provide a standardised and consistent classification and documentation of pharmaceutical care issues identified by pharmacists at RHKG, and across institutions, if the process were to be adapted in other institutions, allowing for comparability. A paper-based ‘pharmaceutical care issues daily log sheet’ was developed to document the pharmaceutical care issues identified by each pharmacist per day (figure 1). This document enables the pharmacists to capture trends in pharmaceutical care issues to be discussed with other healthcare professionals. The sheet is divided into the established pharmaceutical care issue categories and the pharmacist classifies and documents each identified care issue into the respective category, together with the outcome (accepted, modified, not accepted) using tally marks. Drugs involved are also documented. An electronic system for documentation of these pharmaceutical care issues was developed using Microsoft Excel. This system was uploaded on each computer in the pharmacy, allowing access by each pharmacist. A separate Excel file divided into 12 sheets ( January–December) was created for each ward. Each sheet is divided into the established pharmaceutical care issue categories and lists the days of each month. Each file is linked to a master file uploaded on the Mamo M, et al. Eur J Hosp Pharm 2013;0:1–5. doi:10.1136/ejhpharm-2013-000351 Figure 1 Pharmaceutical care issues daily log sheet. computer of the Head of Pharmacy Services which collects data inputted from all the wards. At the end of the day, each pharmacist is required to input the data which was documented on the paper documentation sheet into the file of their respective ward, calculating the total number of care issues identified. These data can be accessed immediately by the Head of Pharmacy Services from the master file. Validity, applicability and practicality of SOP The validity, applicability and practicality of the SOP were confirmed. Face and content validation resulted in the improvement of various criteria relating to SOP presentation and content. Major improvements following validation of the SOP draft were the inclusion, modification and/or elimination of information, arrangement of the sequential order of sections in the procedure, and improvement in SOP presentation and comprehensiveness. The scoring system for validation ranged from 0 to 12, with a higher score indicating higher validity. The mean validation score for validation 1 and 2, out of a total score of 12, was 10.444 (range 9.0–11.50) and 11.500 (range 10.50–12.0), respectively, meaning that there was a stastistically significant improvement in mean validation score between validaton 1 and 3 Research 2 ( p=0.005). The SOP was found to be applicable and practical for use at RHKG since all the steps required to carry out patient profiling were included in the procedure section of the SOP and the pharmacists found the SOP comprehensive and easy to follow and understand. Preliminary evaluation of SOP Both preliminary evaluations showed that all nine pharmacists agreed that the SOP was fit for purpose, easy to follow for training of new pharmacists, user friendly for reference during daily activities and supported development of consistent patient-profiling activities. Moreover, all nine pharmacists agreed that the ‘Scope’ and ‘Objective’ were clearly outlined, the ‘Procedure’ was easy to understand, no steps were ambiguous or omitted, the SOP was not too detailed or too long, it did not need to be further split into other SOPs and no other datasheets were required in the ‘Appendices’ section. The numbers of pharmacists who referred to the SOP during the first months of implementation are given in table 2. Within a quality system, SOPs are meant for use as a training tool for pharmacists to perform a procedure in a standardised way; SOPs are available for referral by the user as required. DISCUSSION The ‘patient-profiling’ SOP was developed with the rationale of achieving standardisation and consistency in the way pharmacists at RHKG carry out patient-profiling activities. Accurately and consistently completing pharmacy patient profiles facilitates pharmaceutical care planning and pharmacist participation during ward rounds and improves continuity of care between pharmacists.21 An important benefit of the developed SOP is that it can be used as an audit tool to ensure that patientprofiling activities are being performed accurately and consistently, to identify risk areas and provide a basis for continuous improvement of patient-profiling activities. During development and validation of the SOP there was no gold standard implemented locally or internationally to refer to for comparison. The SOP developed is robust and comprehensive and following further studies to demonstrate its impact it may be proposed as a gold standard. The validation process was important in SOP development since there was a statistically significant improvement in the mean validation score between validation 1 and 2. This improvement can be explained by the fact that many new improvements to the activity were implemented and that the activity is relatively complex. Applicability and practicality testing showed that the SOP was relevant and practical for use at RHKG. However, the vision for developing this SOP was set on an international dimension and was not limited to RHKG. International evidence-based literature was consulted during SOP development to apply the concept of cross-cultural adaptability. The SOP was based on experiences from the pharmaceutical industry and by consulting guides on the development and implementation of SOPs.22–24 The SOP is detailed to be used in practice at RHKG. However, Table 2 Pharmacist referral to the SOP post implementation Time postimplementation Number of pharmacists who referred to SOP (N=9) 1 month 4 months 7 7 SOP, standard operating procedure. 4 Frequency of referral Once Twice >Twice 5 2 2 4 0 1 it is adaptable since the basic processes within the activity are comparable to those in various hospitals. Nevertheless, some details included in this SOP are dependent on the hospital policy and the geriatric-rehabilitation speciality for which it was developed. Consequently, minor adjustments are required to apply the SOP to other hospital settings and specialities. A positive evaluation of the SOP was obtained by the pharmacists. There was no resistance from the pharmacists to implement the SOP since they were constantly consulted during the development and validation process. Although the design of the pharmacy patient profile was modified, it still remained paper based. Creating more space on the paper pharmacy patient profile, for example to document all medication checks, was not possible. Electronic pharmacy patient profiles are required to suit this purpose. Discussion on the computerisation of patient profiles in this hospital was attempted in a previous study25 in which the feasibility of a computerised programme for patient profiles was considered. Although all the pharmacists agreed that computerisation of patient profiles was the way forward, they were reluctant to implement the program suggested by hospital management at the time, since they perceived it to be very basic with many shortcomings, especially with regards to user interface. The program proposed was viable for calculating the cost of patient treatment; however, the pharmacists felt that it would not improve the quality and safety of patient care since it lacked basic important clinical features. Further collaboration among the pharmacists, hospital management and software companies is required to develop a suitable electronic patient profile for RHKG. It has been reported that while manual documentation using paper forms is the most extensively used method of documentation, this type of documentation may be incomplete and inconsistent, and subsequent manual transfer of interventions from paper form to the electronic system is inefficient, time consuming and may lead to errors.18 26 27 Having a computerised system to document interventions immediately at the point of care, such as handheld computers, is more effective and efficient and facilitates data collection, compilation and analysis.27 28 The successful application of handheld computers, such as personal digital assistants (PDAs) and tablet computers, to document pharmacists’ clinical interventions and activities in hospital has been described in recent years, predominantly in the USA. The PDA-based method of documentation has been reported to be convenient, efficient, sustainable and feasible to monitor care, easy to use with appropriate training, and makes data entry and manipulation faster and easier to perform compared with the paper-based method. In addition, data inputted are standardised and data transfer to the main computer system is not complicated.18 27 29 30 Reported limitations of PDAs include a small screen size, which may limit the length of the form if all data fields need to fit on one screen without scrolling, confidentiality concerns and the cost of the system.18 29 30 Electronic patient profiles and documentation tools for pharmaceutical care issues should be considered as a possible improvement in this hospital. LIMITATIONS The aim of this study was to develop and implement the SOP with a preliminary evaluation. The long-term impact of the SOP on pharmacist activities and on patient care is still being evaluated. It is recommended that after 1 year of implementation, the SOP is re-evaluated by carrying out a time and motion study and assessing key performance indicators for medication safety and rational use. During the study period no new pharmacists Mamo M, et al. Eur J Hosp Pharm 2013;0:1–5. doi:10.1136/ejhpharm-2013-000351 Research were employed at RHKG to use the SOP as a training tool. Validation and evaluation required the pharmacists to fill out a questionnaire; therefore, accuracy relies on the respondents’ enthusiasm and truthfulness. 5 6 7 CONCLUSION The implemented ‘patient-profiling’ SOP is robust, comprehensive, user friendly, applicable and practical for use within a hospital practice for the provision of standardised clinical pharmacy services. The implemented SOP is dynamic and needs to be regularly reviewed and updated. 8 9 10 11 Key messages 12 What is already known on this subject ▸ Development of tools to ensure standardisation in delivery of clinical pharmacy services contribute to ensuring safe and effective patient care. ▸ Documented standards, particularly for clinical pharmacy services, are lacking, especially for the European scenario. ▸ Documentation of clinical pharmacist interventions in patient-profiling activities during a patient’s stay in hospital enables pharmacist accountability and improves patient outcomes. What this study adds ▸ Implementation of a dynamic, robust and comprehensive standard operating procedure (SOP) to improve consistency in patient-profiling activities by pharmacists. ▸ A proposed system for standardised documentation of pharmaceutical care issues during patient profiling. ▸ The developed SOP is adaptable to other hospital settings. 13 14 15 16 17 18 19 Acknowledgements The authors are greatly indebted to Professor Steve Hudson from the University of Strathclyde in Glasgow who sadly passed away before this study was completed. We truly appreciate discussions we had with him on aspects of quality in clinical pharmacy practice which have helped us to widen our perspective on the practice. The authors acknowledge the assistance of Mr Aaron Camilleri, Head of Pharmacy Services and all the pharmacy staff at RHKG, pharmacist Mr Simon Serge and all the healthcare professionals for their participation in the SOP development process, and Dr Liberato Camilleri from the Department of Statistics and Operations Research within the Faculty of Science at the University of Malta for his expert guidance in the statistical analysis. 23 Contributors I declare that all the authors have contributed to the development of this article. 24 Competing interests None. 25 20 21 22 Provenance and peer review Not commissioned; externally peer reviewed. 26 REFERENCES 1 2 3 4 Hughes RG. Tools and strategies for quality improvement and patient safety. In: Hughes RG. ed. Patient safety and quality: an evidence-based handbook for nurses. Rockville, MD: Agency for Healthcare Research and Quality (US), 2008:1–23. Wagner C, Gulacsi L, Takacs E, et al. The implementation of quality management systems in hospitals: a comparison between three countries. BMC Health Serv Res 2006;6:1–11. Øvretveit J, Gustafson D. Total quality management in European healthcare. Int J Health Care Qual Assur 2000;13:74–9. Wirth F, Azzopardi LM, Serracino-Inglott A. Quality management system for clinical pharmacy services: quality assurance for pharmacist professional services. Germany: Scholars’ Press, 2013:18–31. Mamo M, et al. Eur J Hosp Pharm 2013;0:1–5. doi:10.1136/ejhpharm-2013-000351 27 28 29 30 Dean P, Robson J, Walters P. Pharmacist intervention monitoring: a clinical tool. Hosp Pharm 2004;11:201–6. Scott AI, Poole PJ, Jayathissa S. Improving quality and safety of hospital care: a reappraisal and an agenda for clinically relevant reform. J Intern Med 2008;38:44–55. Scullin C, Scott MG, Hogg A, et al. An innovative approach to integrated medicines management. J Eval Clin Pract 2007;13:781–8. Hellström LM, Bondesson A, Höglund P, et al. Impact of Lund Integrated Medicines Management (LIMM) model on medication appropriateness and drug-related hospital revisits. Eur J Clin Pharmacol 2011;67:741–52. Gillespie U, Alassad A, Henrohn D, et al. A comprehensive pharmacist intervention to reduce morbidity in patients 80 years or older: a randomized control trial. Arch Intern Med 2009;169:894–900. Hudson SA, McAnaw JJ, Johnson BJ. The changing roles of pharmacists in society. IeJSME 2007;1:22–34. Hayes P. Writing and implementing procedures. In: Stuart MC, ed. The complete guide to medical writing. London: Pharmaceutical Press, 2007:301–16. De Treville S, Antonakis J, Edelson NM. Can standard operating procedures be motivating? Reconciling process variability issues and behavioural outcomes. Total Qual Manag Bus Excellence 2005;16:231–41. Australian Commission on Safety and Quality in Healthcare. Safety and quality improvement guide standard 4: medication safety. Sydney: Australian Commission on Safety and Quality in Healthcare, 2012:31–41. http://www.safetyandquality.gov. au/wp-content/uploads/2012/10/Standard4_Oct_2012_WEB.pdf (accessed 26 Aug 2013). François P, Peyrin JC, Touboul M, et al. Evaluating implementation of quality management systems in a teaching hospital’s clinical departments. Int J Qual Health Care 2003;15:47–55. Stuchbery P, Kong DCM, Desantis GN, et al. Identification by observation of clinical pharmacists’ activities in a hospital inpatient setting. Pharm Pract 2007;5:10–16. Viktil KK, Blix HS. The impact of clinical pharmacists on drug-related problems and clinical outcomes. Basic Clin Pharmacol Toxicol 2008;102:275–80. Hutchinson LC, Castleberry A. The pharmacist’s new role as part of an interdisciplinary care team. Generations: J Am Soc Ageing 2011;35. http://www. asaging.org/blog/pharmacists-new-role-part-interdisciplinary-care-team (accessed 26 Aug 2013). Fox BI, Felkey BG, Berger BA, et al. Use of personal digital assistants for documentation of pharmacist’s interventions: a literature review. Am J Health-Syst Pharm 2007;64:1516–25. Zierler-Brown S, Brown TR, Chen D, et al. Clinical documentation for patient care: models, concepts and liability considerations for pharmacists. Am J Health-Syst Pharm 2007;64:1851–8. Wirth F, Azzopardi LM, Gauci M, et al. Time and motion study for pharmacists’ activities in a geriatric hospital. Int J Pharm Pract 2009;17:373–6. Baum C, Forbes MB, Kennedy DL, et al. Patient drug profiles and medical records as sources of hospital drug-use information. Am J Hosp Pharm 1983;40:2191–3. European Medicines Agency (EMA). Creating flow charts for standard operating procedures and work instructions. London: EMA, 2010. http://www.ema.europa.eu/ docs/en_GB/document_library/Work_Instruction_-_WIN/2009/09/WC500002742. pdf (accessed 26 Aug 2013). Kolman J, Meng P, Scott G. eds. Good clinical practice: standard operating procedures for clinical researchers. West Sussex: John Wiley & Sons Ltd, 1998. Wieringa D, Moore C, Barnes V. Procedure writing: principles and practices. Columbus, OH: Battelle Press, 1998. Bondin R. Assessing the feasibility of computerising patient profiles at Karin Grech Hospital [ project]. Msida, Malta: Department of Pharmacy, University of Malta, 2010. Nystrom KK, Foral PA, Wilson AF, et al. Personal digital assistant clinical intervention documentation system: Development, implementation and comparison to a previous paper-based system. Hosp Pharm 2006;42:143–50. Patel RJ, Lyman AE Jr, Clark DR, et al. Personal digital assistants for documenting primary care clinical pharmacy services in a health maintenance organisation. Am J Health-Syst Pharm 2006;63:258–61. Lane SJ, Heddle NM, Arnold E, et al. A review of randomised controlled trials comparing the effectiveness of handheld computers with paper methods for data collection. BMC Med Inform Decis Mak 2006;6:23. Bosinski TJ, Campbell L, Schwartz S. Using a personal digital assistant to document pharmacotherapeutic interventions. Am J Health-Syst Pharm 2004;61:931–4. Dasgupta A, Sansgiry SS, Sherert JT, et al. Pharmacists’ utilisation and interest in usage of personal digital assistants in their professional responsibilities. Health Info Libr J 2009;27:37–45. 5