Antiplatelet and Anticoagulation Treatment for Non-ST-Elevation Acute Coronary Syndromes
advertisement

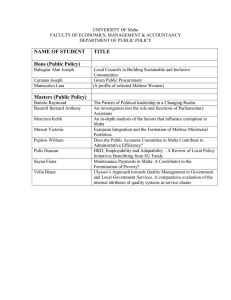
DEPARTMENT OF PHARM ACY UNIVERSI TY OF MA LTA Antiplatelet and Anticoagulation Treatment for Non-ST-Elevation Acute Coronary Syndromes Giorgia Mason*, Francesca Wirth**, Lilian M. Azzopardi**, Robert G. Xuereb***, Andrea Cignarella* Department of Pharmacy University of Malta *Università degli Studi di Padova, Italy **Department of Pharmacy, Faculty of Medicine and Surgery, University of Malta, Malta ***Cardiac Catheterisation Suite, Cardiology Department, Mater Dei Hospital, Malta Email: giorgiamason5888@gmail.com INTRODUCTION AIM The 2011 European Society of Cardiology (ESC) guidelines on the management of acute coronary syndromes without persistent ST-elevation (NSTE-ACS) define fundamental steps regarding pharmacological management in the acute phase of NSTE-ACS during hospitalisation, including 1 antithrombotic treatment. To assess compliance with the ESC guidelines for antiplatelet and anticoagulation therapy in patients diagnosed with NSTE-ACS at the time of coronary angiogram at Mater Dei Hospital (MDH). METHOD University Research Ethics Committee approval was obtained. A data collection form (DCF) to gather information about patient demographics, social and medical history, laboratory investigations and prescribed medications was developed and psychometrically evaluated. Inpatients diagnosed with NSTE-ACS were recruited by convenience sampling from the Cardiac Catheterisation Suite, MDH, over a 5-month period. The DCF was completed for each patient by reviewing patient treatment files, following discussions with consultant cardiologists and nurses and by attending procedures performed. RESULTS RESULTS Patient demographic information Compliance to guidelines for antiplatelet treatment + proton pump inhibitors A total of 165 patients were recruited. 73% of the patients were male, 37% were between 66 and 75 years and 44% were current smokers. Common risk factors for cardiovascular disease were hypertension (BP >140/90 mm Hg) (27%), dyslipidaemia (LDL cholesterol >2 mmol/L; triglycerides >2.26 mmol/L) 2 and obesity (BMI >30 kg/m ) (both 16%). Following coronary angiogram, 41% of the patients underwent a percutaneous coronary intervention, either ad hoc (34%) or elective (7%). Eighty patients were prescribed a proton pump inhibitor (PPI) with dual antiplatelet therapy (DAPT). Sixty-five of these patients were given PPIs against guideline recommendations since they were given omeprazole, which is preferably not recommended in the guidelines to be used with clopidogrel. Four patients were prescribed alternative PPIs (2 pantoprazole, 2 rabeprazole), which are not available on the Maltese GFL. Compliance to guidelines for antiplatelet treatment Compliance to guidelines for anticoagulant treatment Prescription of aspirin 300mg loading dose (LD) and 75mg daily dose (DD) was according to guidelines in the majority of patients (95% and 97% respectively). Prescription of clopidogrel 300mg LD and 75mg DD was also according to guidelines in the majority of patients (88% and 97% respectively). In patients (4) scheduled for an invasive strategy immediately post-hospital admission, a 600mg LD of clopidogrel was required and was given according to guideline recommendations. Prasugrel was only prescribed in 2 patients since it is not available on the Maltese Government Formulary List (GFL). The majority of patients were prescribed heparin anticoagulation treatment in combination with DAPT according to guidelines (95%). With regards to anticoagulation treatment, evaluation of ischaemic and bleeding risk was undertaken according to guidelines in 96% of the patients. Enoxaparin 1mg/kg twice daily SC was prescribed according to guidelines in 81% of the patients. Alternative antithrombotic drugs recommended in the guidelines, such as ticagrelor, glycoprotein IIb/IIIa receptor inhibitors, fondaparinux and bivalirudin were never prescribed since they are not yet available in Malta. CONCLUSION Prescription of antiplatelet and anticoagulation therapy for NSTE-ACS at MDH is predominantly in accordance with ESC guidelines. Alternative antiplatelet drugs, anticoagulants and PPIs should be considered for inclusion in the Maltese hospital formulary to improve NSTE-ACS management in line with European guidelines. Reference 1. Hamm CW, Bassand JP, Agewall S, Bax J, Boersma E, Bueno H, et al. European Society of Cardiology (ESC) guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J 2011; 32: 2999–3054.