Amidst the Confusion: Posterior Reversible Leukoencephalopathy Syndrome
advertisement
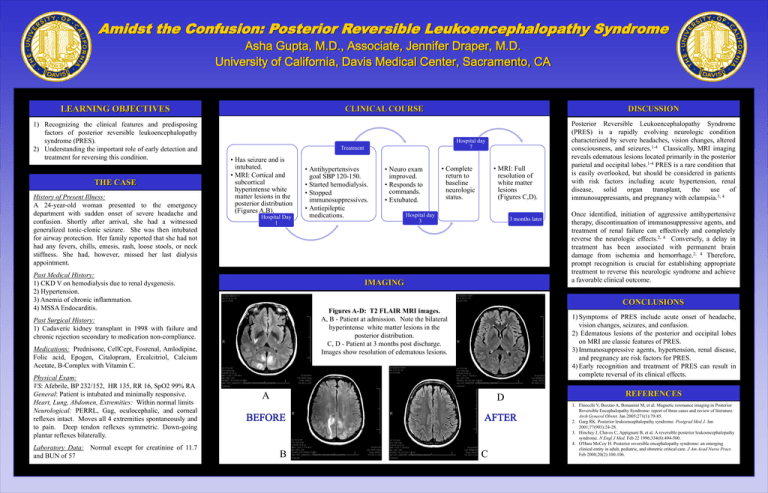
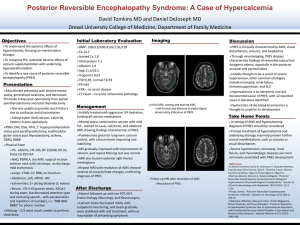
Amidst the Confusion: Posterior Reversible Leukoencephalopathy Syndrome Asha Gupta, M.D., Associate, Jennifer Draper, M.D. University of California, Davis Medical Center, Sacramento, CA LEARNING OBJECTIVES 1) Recognizing the clinical features and predisposing factors of posterior reversible leukoencephalopathy syndrome (PRES). 2) Understanding the important role of early detection and treatment for reversing this condition. THE CASE History of Present Illness: A 24-year-old woman presented to the emergency department with sudden onset of severe headache and confusion. Shortly after arrival, she had a witnessed generalized tonic-clonic seizure. She was then intubated for airway protection. Her family reported that she had not had any fevers, chills, emesis, rash, loose stools, or neck stiffness. She had, however, missed her last dialysis appointment. Past Medical History: 1) CKD V on hemodialysis due to renal dysgenesis. 2) Hypertension. 3) Anemia of chronic inflammation. 4) MSSA Endocarditis. Past Surgical History: 1) Cadaveric kidney transplant in 1998 with failure and chronic rejection secondary to medication non-compliance. Medications: Prednisone, CellCept, Fosrenal, Amlodipine, Folic acid, Epogen, Citalopram, Ercalcitriol, Calcium Acetate, B-Complex with Vitamin C. Physical Exam: VS: Afebrile, BP 232/152, HR 135, RR 16, SpO2 99% RA General: Patient is intubated and minimally responsive. Heart, Lung, Abdomen, Extremities: Within normal limits Neurological: PERRL, Gag, oculocephalic, and corneal reflexes intact. Moves all 4 extremities spontaneously and to pain. Deep tendon reflexes symmetric. Down-going plantar reflexes bilaterally. Laboratory Data: Normal except for creatinine of 11.7 and BUN of 57 CLINICAL COURSE DISCUSSION Hospital day 7 Treatment • Has seizure and is intubated. • MRI: Cortical and subcortical hyperintense white matter lesions in the posterior distribution (Figures A,B). Hospital Day 1 • Antihypertensives goal SBP 120-150. • Started hemodialysis. • Stopped immunosuppressives. • Antiepileptic medications. • Neuro exam improved. • Responds to commands. • Extubated. • MRI: Full resolution of white matter lesions (Figures C,D). • Complete return to baseline neurologic status. Hospital day 3 3 months later IMAGING Posterior Reversible Leukoencephalopathy Syndrome (PRES) is a rapidly evolving neurologic condition characterized by severe headaches, vision changes, altered consciousness, and seizures.1-4 Classically, MRI imaging reveals edematous lesions located primarily in the posterior parietal and occipital lobes.1-4 PRES is a rare condition that is easily overlooked, but should be considered in patients with risk factors including acute hypertension, renal disease, solid organ transplant, the use of immunosuppressants, and pregnancy with eclampsia.3, 4 Once identified, initiation of aggressive antihypertensive therapy, discontinuation of immunosuppressive agents, and treatment of renal failure can effectively and completely reverse the neurologic effects.2, 4 Conversely, a delay in treatment has been associated with permanent brain damage from ischemia and hemorrhage.2, 4 Therefore, prompt recognition is crucial for establishing appropriate treatment to reverse this neurologic syndrome and achieve a favorable clinical outcome. CONCLUSIONS Figures A-D: T2 FLAIR MRI images. A,Stenting B - Patient at admission. Note the bilateral Polyflex Esophageal hyperintense white matter lesions in the posterior distribution. C, D - Patient at 3 months post discharge. Images show resolution of edematous lesions. 1) Symptoms of PRES include acute onset of headache, vision changes, seizures, and confusion. 2) Edematous lesions of the posterior and occipital lobes on MRI are classic features of PRES. 3) Immunosuppressive agents, hypertension, renal disease, and pregnancy are risk factors for PRES. 4) Early recognition and treatment of PRES can result in complete reversal of its clinical effects. A D Re-Stenting of the Esophagus B C REFERENCES 1. Finocchi V, Bozzao A, Bonamini M, et al. Magnetic resonance imaging in Posterior Reversible Encephalopathy Syndrome: report of three cases and review of literature. Arch Gynecol Obstet. Jan 2005;271(1):79-85. 2. Garg RK. Posterior leukoencephalopathy syndrome. Postgrad Med J. Jan 2001;77(903):24-28. 3. Hinchey J, Chaves C, Appignani B, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. Feb 22 1996;334(8):494-500. 4. O'Hara McCoy H. Posterior reversible encephalopathy syndrome: an emerging clinical entity in adult, pediatric, and obstetric critical care. J Am Acad Nurse Pract. Feb 2008;20(2):100-106.