Building for the Future SPECIAL ISSUE 2011
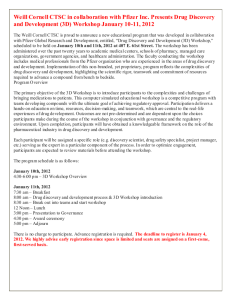
advertisement

c1-c1WCMspecial11.1_WCM redesign 11_08 12/12/11 3:23 PM Page 1 THE MAGAZINE OF WEILL CORNELL MEDICAL COLLEGE AND WEILL CORNELL GRADUATE SCHOOL OF MEDICAL SCIENCES Building for the Future The transformative leadership of Dean Antonio Gotto SPECIAL ISSUE 2011 c2-c2WCMspecial11_special issue 2011 12/12/11 3:24 PM Page c2 01-02WCspecial11toc_WCM redesign 11_08 12/12/11 2:48 PM Page 1 weillcornellmedicine THE MAGAZINE OF WEILL CORNELL MEDICAL COLLEGE AND WEILL CORNELL GRADUATE SCHOOL OF MEDICAL SCIENCES SPECIAL ISSUE 2011 30 22 30 DISCOVERY CENTER BETH SAULNIER FEATURES 22 PASSING THE TORCH BETH SAULNIER At the end of December, Dean Antonio Gotto steps down after a decade and a half of service. They’ve been transformative years for Weill Cornell—physically, financially, academically, and scientifically. During Gotto’s tenure, the Medical College has seen an overhaul of its curriculum; record-setting fundraising campaigns; a renaming in honor of foremost benefactors Joan and Sanford Weill; the establishment of the Qatar campus; and much more. This fall, Gotto sat down for a conversation with Weill Cornell Medicine, offering thoughts on topics from his professional legacy to his fondness for spy novels. “I would like to think that I have helped make Weill Cornell a gentler, more collaborative place,” he says, “but also one that was transformed in its academic endeavors.” •Twitter: @WeillCornell •Facebook.com/WeillCornell MedicalCollege •YouTube.com/WCMCnews For address changes and other subscription inquiries, please e-mail us at wcm@med.cornell.edu 34 On an unseasonably warm and sunny day in early November, Weill Cornell celebrated the dedication of its $650 million medical sciences facility and unveiled its name: the Belfer Research Building. Named in honor of Robert and Renée Belfer in recognition of their $100 million gift, the building is the centerpiece of Weill Cornell’s $1.3 billion Discoveries that Make a Difference Campaign and its Research Leads to Cures Initiative. The 480,000square-foot facility, which has been under construction since spring 2010, is scheduled to open in spring 2014. “Coupled with the brilliant scientists already on staff and with additional ones being recruited,” Robert Belfer said at the event, “the building is certain to house discoveries that will benefit my family, New Yorkers, and all mankind.” 34 CREATIVE SOLUTIONS SHARON TREGASKIS Microbiologist Carl Nathan, MD, has been fascinated by scientific discovery since he was a young teenager working in the lab of an NYU pathologist. Now, he’s marshalling a myriad of weapons— including novel partnerships with industry—in the ongoing battle against tuberculosis. It’s no easy fight: Mycobacterium tuberculosis resides in one in three people worldwide and causes another infection every second. The disease costs 1.8 million lives per year—making it the third leading cause of premature death and the leading cause of death from a curable infection. SPECIAL ISSUE 2011 1 01-02WCspecial11toc_WCM redesign 11_08 12/12/11 2:48 PM Page 2 weillcornellmedicine THE MAGAZINE OF WEILL CORNELL MEDICAL COLLEGE AND WEILL CORNELL GRADUATE SCHOOL OF MEDICAL SCIENCES www.weill.cornell.edu Published by the Office of Public Affairs Weill Cornell Medical College and Weill Cornell Graduate School of Medical Sciences WEILL CORNELL SENIOR ADMINISTRATORS Antonio M. Gotto Jr., MD, DPhil The Stephen and Suzanne Weiss Dean, Weill Cornell Medical College; Provost for Medical Affairs, Cornell University David P. Hajjar, PhD Dean, Weill Cornell Graduate School of Medical Sciences Myrna Manners Vice Provost for Public Affairs Larry Schafer Vice Provost for Development WEILL CORNELL DIRECTOR OF COMMUNICATIONS John Rodgers WEILL CORNELL SENIOR MANAGER OF PUBLICATIONS 18 Anna Sobkowski WEILL CORNELL EDITORIAL COORDINATOR Andria Lam Weill Cornell Medicine is produced by the staff of Cornell Alumni Magazine. PUBLISHER DEPARTMENTS 3 LIGHT BOX Portrait of a partnership Jim Roberts EDITOR Beth Saulnier CONTRIBUTING EDITORS Chris Furst Adele Robinette Sharon Tregaskis EDITORIAL ASSISTANT Tanis Furst ART DIRECTOR Stefanie Green ASSISTANT ART DIRECTOR Lisa Banlaki Frank ACCOUNTING MANAGER Barbara Bennett EDITORIAL AND BUSINESS OFFICES 401 E. State St., Suite 301 Ithaca, NY 14850 (607) 272-8530; FAX (607) 272-8532 4 CAPITAL CAMPAIGN UPDATE 6 DEANS MESSAGES Comments from Dean Gotto & Dean Hajjar 8 SCOPE Meet Dean Glimcher. Plus: Welcoming the white coats, the iPad revolution, Chervenak elected to IOM, intercampus collaboration, $5.5 million NIH grant, the annual art show, and Dean Gotto’s final “State of the Medical College” address. 11 TALK OF THE GOWN Walking tall. Plus: Studying the horrors of the Holocaust, food-borne illness in Qatar, two tuneful docs, new hope for infertile men, Muslim modesty and medicine, health IT, and the latest prosthetic retina. Cover photograph by John Abbott 40 NOTEBOOK News of Medical College alumni and Graduate School alumni 47 IN MEMORIAM Printed by The Lane Press, South Burlington, VT. Copyright © 2011. Rights for republication of all matter are reserved. Printed in U.S.A. Alumni remembered 48 POST DOC Food, fitness, fun 2 WEILL CORNELL MEDICINE Weill Cornell Medicine (ISSN 15514455) is produced four times a year by Cornell Alumni Magazine, 401 E. State St., Suite 301, Ithaca, NY 14850-4400 for Weill Cornell Medical College and Weill Cornell Graduate School of Medical Sciences. Third-class postage paid at New York, NY, and additional mailing offices. POSTMASTER: Send address changes to Public Affairs, 525 E. 68th St., Box 144, New York, NY 10065. 03-03WCMspecial11lightbox_WCM redesign 11_08 12/12/11 2:50 PM Page 3 Light Box Picture perfect: A portrait of Sanford Weill and Dean Gotto by artist Everett Raymond Kinstler was installed in the lobby of the Weill Greenberg Center in September 2009. I EVERETT RAYMOND KINSTLER t is very difficult to write just a few words about how much Tony Gotto means to my wife Joan and me. Most importantly, Tony would be the first to say that he would not be the person he is if it were not for the support of his beautiful wife, Anita, and his terrific family. I wholeheartedly agree. It has been a pleasure getting to know them over the last fifteen years. The Gotto family truly epitomizes class. Weill Cornell has soared to new heights under Tony’s leadership. He and our great team have worked tirelessly to position Weill Cornell as a world-renowned institution for medical education, medical research, and clinical care. As a result of Tony’s vision and passion, Weill Cornell has raised more than $2 billion; developed key partnerships around the globe in Qatar, Tanzania, Turkey, Haiti, and Houston; strengthened ties with Ithaca to enhance research, education, and patient care; and forged a strong bond with NewYork-Presbyterian. I have enjoyed each and every day working with Tony, and there is no question he is one of the smartest people I have ever met. I always like to tell people that they have the luxury of turning to Google for answers to tough questions, while I just need to turn to Gotto. My partnership with Tony has been one of the special highlights of my life and something I will cherish forever. We have traveled the world together, and I have seen firsthand the respect and admiration that world leaders, as well as ordinary people from all walks of life, have for him. I will never forget a trip we took to visit our doctors at Weill Bugando Medical Centre in Tanzania, and seeing Tony perform rounds before the sun came up one morning. He examined a young girl who had malaria, HIV, and tuberculosis—and to this day I still cannot believe all of that could exist in one person’s body. Tony had the ability to make this young girl smile, and he reminded those of us with him that people become doctors to improve lives. Tony has certainly followed this credo for the last fiftyfive years of his life. The mark of a good leader is to leave something better off than it was found. Tony has certainly done this and much more. We all owe him and his family a deep debt of gratitude, and we look forward with much anticipation to the exciting days ahead for Weill Cornell. Sandy Weill Chairman, Board of Overseers Tributes to Dean Gotto by other distinguished members of the Weill Cornell community begin on page 24. SPECIAL ISSUE 2011 3 04-05WCMspecial11dev_WCM redesign 11_08 12/12/11 3:07 PM Page 4 4 WEILL CORNELL MEDICINE 04-05WCMspecial11dev_WCM redesign 11_08 12/12/11 3:07 PM Page 5 SPECIAL ISSUE 2011 5 06-07WCMspecial11deans_WCM redesign 11_08 12/12/11 3:09 PM Page 6 Deans Messages The Best Is Yet to Come JOHN SAMPLES / WCMC-Q I t has been a profound honor to serve as dean of Weill Cornell Medical College over the past fifteen years and to lead our institution into the twenty-first century. When we moved to New York at the end of 1996, my wife, Anita, expected that we would return to Houston to retire after I had completed a five-year term. We could not have imagined that I would end up continuing as dean for an additional ten years. It has been an adventure that we Words of wisdom: Dean Antonio Gotto addresses the graduating class at the 2010 commencement for Weill Cornell Medical College in Qatar. 6 WEILL CORNELL MEDICINE Antonio M. Gotto Jr., MD, DPhil, Dean of the Medical College have enjoyed every step of the way, and we are happy to have made a home in New York. This has been a period of dramatic transformation for the Medical College, and I am extremely proud of all that we have accomplished together. I have been very fortunate and blessed to have the friendship and support of countless individuals from within the Weill Cornell community, at Cornell University in Ithaca, and from our partnering institutions. These relationships have greatly enriched my time as dean. I am especially thankful to Joan and Sandy Weill, who allowed us to rename the Medical College in their honor; to Hank and Corinne Greenberg and the Starr Foundation; to Bob Appel, who is chairing our current campaign; and to our Board of Overseers. At Ithaca, I deeply appreciate the support of our University Board of Trustees, under the successive leadership of Stephen Weiss, Harold Tanner, and Pete Meinig, and of Cornell presidents Rawlings, Lehman, and Skorton. It has been a true pleasure to work with Herb Pardes, former president and CEO of NewYork-Presbyterian Hospital, to strengthen the Medical Center in keeping with our shared values. In addition, our senior administration and department chairs at Weill Cornell, our faculty and staff, our students and alumni, and our many other generous donors and friends have all contributed on multiple levels to the successes of the past decade and a half. For that I am very grateful. Together we have improved student education by continually modernizing our curriculum. Weill Cornell remains a national leader in the recruitment of students underrepresented in medicine, and increasing faculty diversity is a high priority. We have expanded our clinical services by opening our first ambulatory care facility, the beautiful Weill Greenberg Center. We entered into a period of great collaboration between the Medical College and NewYorkPresbyterian, with our Medical Center ranking as a preeminent site for patient care in New York and in the nation. Numerous advances in basic, clinical, and translational research have been made, and top investigators have joined our faculty to launch new programs. I am confident that the opening of the Belfer Research Building, named in honor of our generous benefactors Renée and Bob, will lead to even greater discoveries. Finally, Weill Cornell has vastly expanded its reach, with new affiliations in New York City, Houston, and Tanzania and a branch campus in Qatar. Our commitment to improving health around the world represents an investment in our shared future. Today’s medical students are able to help patients in ways that we never dreamed about when I first entered medical school in the Sixties. The past fifteen years have been an exciting time of growth and transformation for Weill Cornell and for modern medicine, but I believe the best is yet to come. After all is said and done, when we sum up our careers and our lives, the things that really matter most are our faith, our family, our friends, and our good name. 06-07WCMspecial11deans_WCM redesign 11_08 12/12/11 3:32 PM Page 7 The Power of Research Partnerships I n recent years, pharmaceutical companies have begun to re-examine their model for drug research and development, including their relationships with universities. As the cost of developing drugs continues to rise and the flow of new products in the pipeline slows, the biomedical industry is under pressure to find more effective and efficient ways to bring promising therapeutic compounds and diagnostic methods to market. In this new landscape, pharmaceutical and biotech companies, as well as medical device manufacturers, have turned to academic medical centers in search of new ways to collaborate. These partnerships are creating new opportunities for us in the Graduate School to advance health care through science. Until recently, the traditional model for pharmaceutical companies was to acquire potential drugs only in the late stages of development, once chemical compounds had been shown in an early clinical trial to be safe and effective. Today, academic researchers and industry experts are collaborating at earlier stages. As our faculty members validate targets, they can partner with industry experts. For example, there are new interactions at Pfizer’s Centers for Therapeutic Innovation, an initiative the Medical College joined earlier this year. Pfizer has agreed to sponsor the research of two of our leading scientists: Barbara Hempstead, MD, PhD, the O. Wayne Isom Professor of Medicine, who is researching a novel target with implications for the treatment of acute coronary disease, and Katherine Hajjar, MD, the Brine Family Professor of Cell and Developmental Biology, who will be studying new cellular targets to manage diabetic retinopathies. Their work will be done in tandem with Pfizer scientists who bring experience in the use of therapeutic biologics, pharmacokinetics, and toxicology to the table. Other more recent collaborations extend across our Tri-Institutional stem cell research efforts with Memorial Sloan-Kettering and Rockefeller University. And this issue of Weill Cornell Medicine details the work of Carl Nathan, MD, the R. A. Rees Pritchett Professor of Microbiology, who has pioneered models of collaboration with nonprofit organizations and industry, David P. Hajjar, PhD, Dean of the Graduate School of Medical Sciences JOHN ABBOTT including pilot programs with GlaxoSmithKline, Lilly, and Sanofi-Aventis, to bring to market drugs to treat tuberculosis and other infectious diseases that, under the old model, were sometimes neglected. There are many other existing relationships with our professors and industrial partners. Caren Heller, MD, who oversees the development of new industry initiatives at the medical school, recently attended an open house hosted by a global biopharmaceutical company. At the event, representatives emphasized that this particular company is open to collaborations with academic researchers at any stage. As understanding of human biology has deepened, they said, academic researchers offer industry much greater scope. The firm cannot cover every area of medical research—but if it collaborates with academic medical centers, it can put smaller bets in a wider range of areas. Those bets could pay off with enormous advances in the diagnosis and treatment of disease. Our research scientists welcome new and creative collaborations, as we continue our efforts to translate basic science into clinical outcomes that improve health care for all. SPECIAL ISSUE 2011 7 08-10WCMspecial11scope_WCM redesign 11_08 12/12/11 3:13 PM Page 8 Scope News Briefs A Physician-Scientist Named Dean fter an extensive search that yielded dozens of highly qualified candidates, Weill Cornell has chosen a nationally renowned immunologist and translational medicine pioneer as its next dean. As of January 1, physician-scientist Laurie Glimcher, MD, will serve as Cornell University provost for medical affairs and the Stephen and Suzanne Weiss Dean of the Medical College. In announcing Glimcher’s hiring in early September, Cornell President David Skorton, MD, called her the ideal choice to lead the institution as it expands its biomedical research enterprise—citing the construction of the new Belfer Research Building and the near-completion of the $1.3 billion Discoveries that Make a Difference Campaign. “I am honored and delighted that Dr. Glimcher has accepted the challenge of guiding our great institution,” Skorton said. “Her passion for accomplishment and her many research and clinical strengths Laurie Glimcher, MD make her ideally suited to build on Tony Gotto’s strong foundation and lead Weill Cornell’s bright JOHN ABBOTT future in clinical care, education, and translational Academy of Sciences. A past president of the American Association research as well as participate at the highest level of Cornell of Immunologists, she has been elected to numerous professional University in fostering excellence in the life sciences.” societies including the American Association for the Advancement Glimcher graduated magna cum laude from Harvard in 1972 and of Science. She has authored more than 350 scientific articles and earned her MD cum laude from Harvard Medical School. She went chapters, publishing in leading journals such as Science and Nature. on to join the Harvard faculty, becoming the Irene Heinz Given At Harvard, her lab used biochemical and genetic approaches to Professor of Immunology at the Harvard School of Public Health, elucidate the molecular pathways that regulate lymphocyte develwhere she directed the Division of Biological Sciences, and profesopment and activation in the immune system—work that could sor of medicine at Harvard Medical School, where she headed one lead to treatment of autoimmune, infectious, allergic, and maligof the world’s leading immunology programs. Her research lab is nant diseases. One of her publications, a landmark paper in Cell on credited with myriad discoveries including the T-bet transcription the T-bet transcription factor, has been cited more than 1,100 times. factor, which regulates immune functions, and the Schnurri-3 Glimcher has pledged to continue Weill Cornell’s efforts to adapter protein, which controls adult bone mass. Board certified in increase faculty excellence and strengthen research ties to the internal medicine and rheumatology, Glimcher is known as a pioIthaca campus, while tapping her experience in working with the neer in partnering with the private sector; she is the longest-standing private sector to foster partnerships with industry. “I am convinced member of the board of directors of the biopharmaceutical compathat Weill Cornell Medical College is perfectly positioned, thanks to ny Bristol-Myers Squibb. the great work of Tony Gotto, Sandy Weill, and the Board of “This is great news for the medical school and for the city,” said Overseers, to be a leader in academic medicine in this country,” Board of Overseers Chairman Sanford Weill. “With her thorough Glimcher said. “I have a clear vision for how that can happen, but appreciation of the management and financial challenges of comI also am excited that the president of Cornell—David Skorton, plex organizations, I am confident she will lead the college with the who is a physician-scientist—the Board of Overseers and the same creativity and acumen she demonstrated when she pioneered WCMC faculty will work with me to shape that vision. I also look the establishment of Bristol-Myers’s science and technology commitforward to leveraging the enormous strengths in life sciences, the tee, which is widely credited for transforming its stake in research.” physical sciences, and engineering at Cornell University’s Ithaca Glimcher is a fellow of the American Academy of Arts and campus to raise the bar even higher across the university.” Sciences and a member of the Institute of Medicine of the National 8 WEILL CORNELL MEDICINE 08-10WCMspecial11scope_WCM redesign 11_08 12/12/11 3:13 PM Page 9 Dean Gotto Gives Final State of the College Address Speaking to a standing-room-only audience in Uris Auditorium in late November, outgoing dean Antonio Gotto used his final State of the Medical College address to reflect on his fifteen years in office. Gotto went on to detail Weill Cornell’s growth and progress in a number of arenas, including student admissions, clinical care, biomedical research, and fundraising. He noted that Weill Cornell’s endowment has quadrupled to $1.1 billion, including $45 million endowed for scholarships, and that the Medical College created 122 new faculty endowments, including commitments for sixtyfour professorships and forty-six clinical, education, and research scholars. He also outlined positive trends in student recruitment—the mean science GPA for the Class of 2015 is 3.77, tied for highest in Medical College history—and in the number of faculty and staff, which has grown from some 3,000 in 1997 to more than 5,600 today. At the event, Graduate School Dean David Hajjar presented Gotto with a plaque in his honor; it included the line, “No greater devotion has been exemplified by any provost or dean in the history of this institution.” Student iPad Tablets Mark Shift to Digital WCMC White-coat welcome: The 103 aspiring doctors of the Class of 2015 donned the traditional garb of the medical student at the August ceremony marking the beginning of their studies. Chervenak Elected to Institute of Medicine Frank Chervenak, MD, the Given Foundation Professor and chairman of the Department of Obstetrics and Gynecology, has been elected to the Institute of Medicine of the National Academies—one of the highest honors in health and medicine. Chervenak has published more than 260 peer-reviewed papers and co-authored or coedited twenty-eight textbooks on topics including ultrasound and ethics in ob/gyn. He currently serves as president of the International Society of the Fetus as a Patient and of the World Association of Perinatal Medicine, among other leadership positions. As of fall semester, instead of receiving printed course notes and texts, all first- and second-year students have been given an iPad 2—making Weill Cornell one of the first medical colleges to make the leap from paper to digital. In addition to sparing students the burden of hauling heavy texts, the tablets will allow them to download course materials, submit electronic course evaluations, access their grades, collaborate TIP OF THE CAP TO. . . with other students, and save their notes and coursework. Jason Korenkiewicz, director of educational computing, noted that “the iPad is also a green alternative, saving about 2 million Phyllis August, MD, the Ralph A. Baer pages and copies without being any more Professor of Medical Research, and expensive.” ob/gyn professor Daniel Skupski, MD, On the iPad, students can view 3-D molecnamed Outstanding Physicians for ular models rather than flat photos on a page; Hypertensive Disorders of Pregnancy images being discussed during training, such as by the Preeclampsia Foundation. views through a scope, can be transmitted wirelessly to all the tablets in the room. In the Charles Bardes, MD, associate dean of future, they could be synched with electronic admissions and professor of clinical medical record systems during student clerkmedicine, winner of the Siegel Family ships. According to Vinay Patel ’14, who was Faculty Award, which recognizes a part of a pilot group that tested the device last Weill Cornell professor who demonspring, some students were initially apprehenstrates excellence in teaching and sive about shifting away from paper—but overresearch. all, he says, “the response has been extremely positive.” The iPad initiative echoes the curAndrew Dannenberg, MD, director of rent trend toward electronic record-keeping, the Weill Cornell Cancer Center and which will be the standard in students’ future the Henry R. Erle, MD–Roberts Family practice. Says Patel, “With an iPad, it will be Professor of Medicine, winner of an easy to keep personal and patient records award for excellence in cancer prevenupdated in real-time as you’re meeting with tion research from the American the patient, checking reference information, Association for Cancer Research. and even looking up body-scan images on the fly, while making rounds.” Joseph Fins, MD ’86, the E. William Davis Jr., MD, Professor of Medical Ethics, installed as president of the American Society for Bioethics and Humanities. Incoming Medical College dean Laurie Glimcher, MD, given honorary lifetime membership in the International Cytokine Society, the group’s highest honor. Dermatologist Marie Jhin, MD ’94, winner of the Entrepreneurial Leadership Award from Asian Women in Business. Michael Stewart, MD, chairman of the Department of Otolaryngology–Head and Neck Surgery and the E. Darracott Vaughan Jr., MD, Senior Associate Dean for Clinical Affairs, appointed editor-in-chief of the Laryngoscope. SPECIAL ISSUE 2011 9 08-10WCMspecial11scope_WCM redesign 11_08 12/12/11 3:13 PM Page 10 LINDSAY FRANCE / CORNELL UP Panel Touts Intercampus Collaborations In October, biomedical sciences professor Robin Davisson, PhD— who holds appointments at both Weill Cornell and Ithaca—moderated a panel discussion on the benefits of collaborations between the two campuses. Speakers at the event, held in Ithaca during the Trustee-Council Annual Meeting, included two Veterinary College professors—Paula Cohen, PhD, associate professor of biomedical sciences and director of Cornell’s intercampus Center for Reproductive Genetics, and molecular microbiologist David Russell, PhD—as well as Weill Cornell’s Anne Moscona, MD, professor of pediatrics and of microbiology and immunology and vice chair for research of pediatrics. The panelists discussed their collaborative efforts, including Moscona’s work with veterinary researchers to study viral infections in dogs and cats—which could shed light on how an animal virus can adapt to infect humans. Efforts to promote cooperation between the two campuses have been stepped up in recent years, with initiatives including startup grant funding for collaborative projects and the establishment of a direct bus service offering work space, wifi, and power for electronic devices. FROM THE BENCH $5.5 million NIH Grant for Spina Bifida Research Weill Cornell researchers have received a five-year, $5.5 million Transformative Research Project (T-R01) Award from the NIH to fund investigations into risk factors for spina bifida and related congenital defects in which an area of a baby’s spine or brain is not fully enclosed. The project will be led by Margaret Ross, MD ’79, PhD ’82, director of the Laboratory of Neurogenetics and Development and professor and vice chair for research in the Department of Neurology and Neuroscience, and Christopher Mason, PhD, an assistant professor of computational genomics in the Department of Physiology and Biophysics. In collaboration with a colleague at the University of Texas, Austin, they aim to identify which genes are modified by folic acid levels and how those patterns can be used to assess risk for having a child with spina bifida or other serious neural tube defects. Varicoceles Linked to Lower Testosterone In the journal BJU International, Weill Cornell physician-scientists report that varicoceles, masses of enlarged and dilated veins in the testicles long known to cause infertility, also interfere with testosterone production. Along with low energy, decreased muscle strength, and sexual problems, says urologist Marc Goldstein, MD, the Matthew P. Hardy Distinguished Professor of Reproductive Medicine, low testosterone is a major risk factor for osteoporosis and can cause cognitive and psychological issues such as depression. However, the 10 WEILL CORNELL MEDICINE Working together: The panel discussion, held in Ithaca and moderated by Robin Davisson, PhD (far right), included Weill Cornell researcher Anne Moscona, MD (center). researchers found that microsurgery can increase testosterone levels in 70 percent of patients. Lessons from COURAGE Trial Rarely Applied systems and access to HIV prevention, testing, and treatment services,” says Laith Abu-Raddad, PhD, an assistant professor of public health at WCMC-Q. “We need to be ahead of the epidemic, not trailing behind it and wishing we had acted earlier.” In a review of nearly 500,000 cardiac cases nationwide, researchers at NYP/Weill Cornell found that the lessons learned from a major, widely publicized study are not being well implemented. Despite the findings of the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial—that patients should receive a combination of common cardiac drugs such as aspirin and a beta blocker before and after stenting—the researchers reported in JAMA that the number of patients receiving the optimal therapy had increased by less than 3 percent. Says cardiologist William Borden, MD, the Nanette Laitman Clinical Scholar in Public Health: “This snapshot of what is happening in the real world should be a call for physicians, as well as policymakers, to look at how patient care can be improved.” ‘Spinach’ Sheds Light on RNA HIV Emerging in Middle East Protein Plays a Vital Role in Lung Regeneration HIV infection levels have been steadily rising among men who have sex with men in several countries in the Middle East and North Africa, including Egypt, Sudan, and Tunisia. In a study published in PLoS, researchers found that transmission of the virus via anal sex among men was responsible for more than a quarter of reported HIV cases in many countries in the region. The men studied were also shown to engage in several types of high-risk behavior including minimal condom usage. “There is no escaping that countries in the region need to massively expand HIV surveillance Researchers have developed a fluorescent tool that can track the ways in which RNA both sustains human life and contributes to disease. The tool, a green fluorescent protein dubbed “Spinach,” tags cellular RNA, allowing researchers to track it—and gain a deeper understanding of its still-mysterious role. “Scientists used to think that RNA’s function was limited to making proteins and that these proteins alone dictated everything that happened in cells,” says Samie Jaffrey, MD, PhD, an associate professor of pharmacology and the study’s senior author. “But now we are understanding that cells contain many different forms of RNA—and some RNAs influence cell signaling and gene expression without ever being used for synthesizing proteins.” A protein known as MMP14 may be crucial for the production of new lung alveoli, the tiny sacs where oxygen exchange takes place. In a study published in Cell, researchers led by Shahin Rafii, MD, the Arthur B. Belfer Professor of Genetic Medicine and co-director of the Ansary Stem Cell Institute, have identified endothelial cells that trigger lung regeneration in mice. The findings may eventually point to a way to induce regeneration in patients with chronic obstructive pulmonary disease (COPD), which currently has no effective therapy. 11-21WCMspecial11totg_WCM redesign 11_08 12/12/11 3:14 PM Page 11 Talk of the Gown A Leg Up Insights & Viewpoints Orthopaedic surgeon S. Robert Rozbruch, MD ’90, is a leader in a burgeoning field devoted to lengthening N ancy Napurski was twentyfive and on a climbing date in the Connecticut Traprocks when the accident happened. Though a novice, she was leading the climb; during the hardest part of the ascent, she somehow lost her grip. “I learned much later that when you fall, you’re supposed to be like Spider-Man and hang onto the cliff as tight as you can, but I jumped away from it,” recalls Napurski, now fifty. “I swung back, and the impact was taken by my left ankle. It dislocated and I was hanging by my rope, terrified and screaming.” Luckily, two teenagers were being trained in mountain rescue nearby; their instructor came to Napurski’s aid and supervised her removal via litter, since there was nowhere to land a PROVIDED helicopter. She was eventually moved to a hospital in Westchester, where she had surgery. “The next morning, my surgeon said I had a 50 percent chance of walking normally,” she says. “At the time I was playing competitive volleyball, I had been a gymnast, I skied. I was so active, and the news was frightening.” Napurski eventually resumed normal walking. But over the next two decades she developed painful bone spurs and other complications—including an equinus deformity that required walking on the ball of her foot. Ankle surgery didn’t solve her problems; she was forced to wear either an orthotic insert or high heels. She made the best of it by throwing herself into competitive swing dancing. She earned a bachelor’s degree, began a career in public relations, and eventually moved to Upstate New York to be with her fiancé. By her late forties, she stunted limbs and repairing old injuries PROVIDED BY NANCY NAPURSKI Climb every mountain: Nancy Napurski climbs Breakneck Ridge in the Hudson Valley after her ankle was repaired by surgeon S. Robert Rozbruch, MD ’90 (left). SPECIAL ISSUE 2011 11 11-21WCMspecial11totg_WCM redesign 11_08 12/12/11 3:14 PM Page 12 Talk of the Gown who had had a fracture as a child; they’re walking around with a leg that’s crooked and short, and they’ve been told by doctors over the years that there’s nothing that can be done, they just have to live with it. And then they find out that it can be repaired; we can straighten the leg, lengthen it, and make it normal. The emotion that people display is fabulous.” The field’s progenitor was Gavriil Ilizarov, MD, an orthopaedic surgeon in the Siberian city of Kurgan who developed fixators—which the patients could adjust themselves—to treat poorly healed war wounds, using the basic physiological principle that compression facilitates bone healing. “The story goes that he went away for two weeks and left instructions HOSPITAL FOR SPECIAL SURGERY on how to adjust the frame, but the patient turned it the wrong Attitude adjustment: Napurski’s artist husband way,” explains Rozbruch. “When decorated her fixator so strangers would be less he came back two weeks later and frightened of the device. took an X-ray, he found the bone was pulled apart—was ‘distracted’—yet there was new bone growing in was facing the daunting prospect of having the gap. That was the beginning of the the joint fused when she heard about a prothought that you could regenerate bone gram at Hospital for Special Surgery that with distraction—and that led to the might offer hope. whole idea of limb lengthening.” Enter S. Robert Rozbruch, MD ’90, an During the Cold War, Ilizarov’s techassociate professor of clinical orthopaedic nique didn’t get much exposure in the surgery at Weill Cornell. Rozbruch is a pioWest; it made its way to Italy in the neer in the nascent specialty of limb Eighties, and the first such procedure was lengthening and complex reconstruction. performed in the U.S. in 1988. Rozbruch Based on techniques developed in Russia became interested in the field after comafter World War II, the field aims to correct pleting his orthopaedic training in the midthe lingering effects of orthopaedic trauma, Nineties; he took a sabbatical from HSS in from shortened limbs due to childhood 1999 to study the technique at the only growth-plate injury to the complications of facility, at the time, with a dedicated limb poorly healed fractures or postsurgical lengthening service: Sinai Hospital in infection. Using external fixators—scaffolds Baltimore. HSS launched its own program that surround the limb and require tiny in 2000; it became a dedicated service in daily adjustments to pins inserted through 2005, with Rozbruch as chief. In addition the skin—Rozbruch and his colleagues are to post-trauma repair, he and his team treat able to replace bone, add inches to arms patients with conditions such as dwarfism and legs, and restore function almost to and children with limb discrepancies and pre-injury levels. “This is life-changing for deformities related to birth defects and people—that’s part of what’s so exciting for trauma. They also conduct research on a me,” says Rozbruch, president-elect of the variety of topics, including the develophundred-member Limb Lengthening and ment of internal fixators and the basic sciReconstruction Society. “You see an adult 12 WEILL CORNELL MEDICINE ence of bone healing. “We’re a dynamic group,” he says “We’re asking questions and doing research. We’re training fellows, med students, and residents. It’s an exciting field and this is an exciting time.” Napurski had her surgery in July 2009—timing it, in part, so she could avoid the slippery sidewalks of a Rochester winter while sporting the fixator. During the procedure, Rozbruch used a technique called ankle distraction, separating the joint and injecting stem cells taken from her hip to promote re-growth of cartilage. “The day after, the pain was terrible,” she recalls. “I had a morphine drip, and it was appropriate. When I had to unlock the fixator and move my joints, I made sure that I was on codeine, but otherwise I was able to manage my pain with Tylenol. Some days were better than others.” She wore the fixator for twelve weeks, cleaning the pin sites and making adjustments several times daily. “One interesting thing I found is that the fixator scared people,” she recalls. “It’s not that scary when you have it on. But when strangers saw it, it made them afraid.” Her husband is an artist, and he decorated the fixator with whimsical trappings like colorful pipe-cleaners and a clown head. “Suddenly people were attracted to it—they would smile at it and compliment me on my mobile sculpture,” she says. “It was a completely different experience.” For Napurski, the procedure was a resounding success. As Rozbruch promised, she was “shoe to shoe” in nine months—walking in normal footwear by the following March. While she occasionally gets stiff if she’s been on her feet all day, it’s nothing that can’t be handled with ibuprofen. “I’ve had such a miraculous recovery,” says Napurski, whose testimonial is one of many on the service’s website. “I can stand flat-footed—I hadn’t been able to do that for twenty years. I can balance on one foot at a time. I can walk in heels, flip-flops, and sneakers without any problem. When people see my story online, they often ask, ‘Is it really painful to have the fixator on?’ I tell them, ‘It’s not any more painful than when you broke your leg in the first place.’ ” — Beth Saulnier 11-21WCMspecial11totg_WCM redesign 11_08 12/12/11 3:53 PM Page 13 Bearing Witness An ethics fellowship brings a student to Auschwitz to confront medicine’s role in the Holocaust STEPHANIE PURISCH Sacred space: At Auschwitz, Stephanie Purisch ’12 and the other fellows visited the infamous gates proclaiming that “work makes you free.” Below: Purisch at the Berlin Wall. I n the research room of Berlin’s House of the Wannsee Conference, fourthyear medical student Stephanie Purisch felt a sense of dread creeping over her as she read documents detailing the crimes of Nazi doctors complicit in the Final Solution. She felt it again, profoundly, on a strangely cold and overcast day in July as she toured the grounds and buildings of Auschwitz-Birkenau, where those atrocities were carried out. The unseasonable weather seemed part of the place, she says, as if that vast campus of death were forever under an evil pall. Purisch was one of fifty students chosen by the Fellowships at Auschwitz for the Study of Professional Ethics (FASPE) for a two-week program of profound instruction. Founded in 2010, the fellowship uses the Holocaust as a framework for exploring the responsibilities of professionals to maintain ethical standards even in the face of war, social unrest, and personal risk. About a dozen students were chosen from each of four fields: medicine, law, journalism, and religion. This past summer, the 2011 FASPE fellows attended workshops, lectures, and seminars in New York, Berlin, and Poland. “As physicians we’re in a powerful position; people put their lives in our hands and depend on what we say and do,” she says. “The fellowship has definitely helped solidify my commitment to treating my patients as individuals, to making every effort to learn about who they are.” FASPE is designed to use the history of the Holocaust—when doctors, lawyers, journalists, and even religious leaders collaborated with Nazi authorities to commit systematic crimes against humanity—as a framework for an exploration of contemporary ethics. Purisch studied such issues as the complicity of physicians in establishing and carrying out Nazi policies; the relationship between state authority and medicine; and the role and limits of con- temporary bioethics, including physicianassisted suicide. The fellowship’s ultimate goal is to make students aware of the ethical challenges that they will confront in their working lives. That possibility seems remote to Purisch, a Maryland native and frequent volunteer at Weill Cornell’s Community Clinic who plans to specialize in obstetrics and gynocology. But she is well aware that ethics are a vital part of medicine—and that she may face hurdles she can scarcely imagine. “Ob/gyn is an emotionally and ethically charged field,” she says. “As a doctor I will have obligations to a pregnant mother, a fetus—life itself. I know there will be difficult cases that will test my ability to do the right thing for my patients in life-and-death situations.” Purisch lauds the medical training she has had so far and says she’s gratified that advocating for patients seems to come naturally to her. But nothing could have prepared her for what she learned about Nazi doctors who performed brutal experiments on prisoners and ushered helpless victims to the gas chamber, lying to them all the way. “I’m Jewish and have extended family who survived the camps, and I thought I knew a lot about the Holocaust,” she says. “But the idea that doctors were so deeply involved in conceiving and orchestrating the Final Solution was new to me.” It is estimated that at least 350 German physicians—and probably hundreds more—participated in the killing of millions of people under the concept of lebensunwertes Leben, “life unworthy of life.” The genocide began with the idea of purifying the Aryan race through coercive sterilization. It was followed by the killing of “impaired” children, then adults in mental hospitals. In Auschwitz-Birkenau alone, an estimated 1.1 million people perished, 90 percent of them Jews. Purisch was sickened to learn how doctors—people sworn to do no harm—sterilSPECIAL ISSUE 2011 13 11-21WCMspecial11totg_WCM redesign 11_08 12/12/11 3:14 PM Page 14 Talk of the Gown ized female prisoners by injecting chemicals into their uteruses and exposing them to massive levels of X-rays. At the Auschwitz-Birkenau museum she read how the notorious Dr. Josef Mengele, the “Angel of Death,” performed brutal experiments on sets of twins, including killing one with induced diseases and then executing the other and performing comparative autopsies. These and other ghastly details—including clinical notes written in Mengele’s own hand—stunned Purisch. She could not fathom how anyone, least of all medical professionals, could do such things. “We’re at a very idealistic phase of our training, and it just over whelmed me,” she says. “Doctors not much older than we are committed murder and provided a so-called ‘calming presence’ for prisoners as they were escorted to their deaths. They were at each and every point in the chain of command at the death camps. How could that happen?” The twelve-day FASPE program began with a visit to the Museum of Jewish Heritage in New York, where fellows explored exhibits and met with scholars and Holocaust survivors. Next stop: Berlin, where workshops were held at the House of the Wannsee Conference, the chateau where Nazi officials planned the Final Solution. The fellows then traveled to Oswiecim, Poland—the town the Germans called Auschwitz—where they toured Auschwitz-Birkenau and worked with the education staff at its museum. In Krakow, they met with a Righteous Among the Nations rescuer, one of the last surviving people who risked their lives to save Jews from the Nazis, and attended sessions at Jagiellonian University on contemporary ethical issues facing their professions. Purisch notes that the fellowship is not meant to numb by over-exposure to horror; the goal is heightened awareness and sensitivity. To that end, she joined in troubling discussions on a question no one wants to confront: what if she found herself in a situation where resistance to evil meant imprisonment, torture, or death? “It’s hard to imagine—very hard,” says Purisch, who followed up the FASPE fellowship with a final project examining the “dehumanization” of the Jews and other Holocaust victims by the Nazi regime. “It’s easy to say that we would never betray our commitment, but the real truth is that no one knows. The best we can do is be prepared to act in the interest of life.” — Franklin Crawford 14 WEILL CORNELL MEDICINE Dietary Detectives Researchers in Doha and Ithaca team up to study food-borne illness in Qatar Q atar is seeing an era of remarkable growth. Between the 2004 and 2010 censuses, its population rose from about 775,000 to 1.7 million, mainly due to an influx of expatriate workers from around the globe. The nation is taking an increasing role on the world stage, is hosting the FIFA World Cup soccer competition in 2022, and is in the running to host the 2020 Summer Olympics. Under a three-year, $1 million grant from the Qatar Foundation, two researchers are tackling a little-heralded subject—food safety—that is becoming increasingly vital as the nation grows. The project brings together a pair of Cornell scientists working on opposite sides of the globe: Ali Sultan, PhD, an associate professor of microbiology and immunology at WCMC-Q, and Hussni Mohammed, PhD, an epidemiologist in the College of Veterinary Medicine on the Ithaca camLISA BANLAKI FRANK pus. “The idea is to look at the food chain from farm to fork,” says Sultan. “This is the first study in Qatar to look in such a meticulous, scientifically detailed way at the food chain, define any sources of contamination, and come up with a riskassessment model.” According to figures from Qatar’s Department of Public Health, incidents of foodborne illness are on the rise; about 1,600 cases were reported in 2007, Sultan says, compared with fewer than 200 in 2004. “The increase could probably be attributed to many factors,” he says. “It might be because of the rapid rise in population, the increased practice of reporting incidents, or the opening of new food outlets.” In any given case of food poisoning, the researchers note, it can be hard to track down the source, due to such factors as the ease of cross-contamination. “If you bring home contaminated meat and cut it up, you can contaminate the kitchen,” Mohammed says. “So after you cook it, although you killed the pathogen in the meat, it is still living in the surrounding environment.” The researchers are focusing on four of the most common pathogens implicated in foodborne illness: E. coli, Salmonella, Campylobacter, and Listeria monocytogenes. They’re taking samples from such sites as dairy operations, milk processing plants, abattoirs, restaurants, and food suppliers, as well as analyzing strains isolated from food poisoning cases at Hamad Medical Corporation, the medical center affiliated with WCMC-Q. Other collaborators in Qatar include the Department of Public Health Supreme Council of Health and the Department of Animal Resources. “Our preliminary studies show that these four pathogens are prevalent in the food animal sources and among human cases with gastroenteritis,” Mohammed reports. “On completion of the investigations, we hope to shed light on how these patients contracted the infections in the hope of making recommendations to mitigate risk.” The researchers note that although food-borne illness was once seen as a localized issue, nowadays—with people and products becoming increasingly mobile—it is a matter of international concern. “Our goal is to help the public, to preserve health in general,” Mohammed says. “Although we’re working in Qatar, the world is getting smaller and smaller—so the issues become global.” — Beth Saulnier 11-21WCMspecial11totg_WCM redesign 11_08 12/12/11 3:14 PM Page 15 T he song is sung to the tune of “Be Our Guest” from Beauty and the Beast. But it has a new title: “Have a Test.” You’ll feel lots more healthy We’ll be lots more wealthy Be our guest! Have a test! Have a test! In their cabaret show Damaged Care, Greg LaGana, MD ’71, and Barry Levy, MD ’71, offer a witty musical take on the modern health-care system—from the promise and pitfalls of technology to the role of business in medicine. The satirical “Spare Parts Blues,” with original music by Brad Ross, contemplates the promise of cloned pig organs sold on eBay; “Send in the Dogs” (complete with Levy in canine costume) spoofs the rise of pet therapy. One of the most popular parodies is the heartfelt “No Time”; sung to “Somewhere” from West Side Story, it laments the harried life of the physician: A chocolate bar and fries No lunch, no exercise There’s no time left to heal myself . . . Someday, when we are retired, Maybe then we’ll be inspired . . . to take time “I’ve had physicians tell me they cried after they heard that song,” says LaGana. “It’s a modern dilemma in health care.” Damaged Care evolved from the class shows that LaGana and Levy produced as students; after meeting on the second day of med school, says Levy, ”we realized we were kindred spirits.” Both went on to train in internal medicine; the New Jerseybased LaGana shifted to volunteer teaching after retiring from active practice, while Levy is a Boston-area specialist in occupational and environmental medicine and public health. After taking musical theater courses at the New School in the mid-Nineties, the pair pledged to write a class show for their 25th Reunion. Facing a deadline, they holed up for the weekend with pizza and a laptop—and quickly realized a large-scale production would be impossible to rehearse. “I said, ‘I think this is a two-man show,’ ” LaGana recalls. “And Barry said, ‘But I don’t sing.’ And I said, ‘Well, you do now.’ ” They structured the show around two contrasting characters: LaGana plays an oldschool workaholic who cares deeply for his patients but neglects himself, while Levy is comically fixated on technology as a boon Music Men Longtime pals pen and perform a parody on modern medicine PROVIDED not only to human health but his own bottom line. In the end, the characters embrace a middle ground. “The ideal physician,” Levy concludes, “might be someone who is entrepreneurial but retains the human touch in the face of the technology and time limitations.” Both share anecdotes from real life: LaGana recalls a caring doctor who made a house call to treat his childhood asthma attack, while Levy describes a story that he grew up with: “When my Uncle Lou delivered me, he turned to my mother and said, ‘It’s a doctor.’” LaGana and Levy have performed the forty-five-minute show more than 120 times nationwide—not only at their 25th Reunion but their 35th as well. They have mounted Damaged Care for Weill Cornell students, medical societies, health systems, hospital associations, and numerous other audiences; it has been featured in such media as the New York Times, CNN Headline News, and ABC’s “Nightline.” While the two have contemplated licensing the show so it can be performed more widely, LaGana says that “it seems to have a lot more credibility, impact, and resonance when it’s performed by physicians.” They’ve recorded a CD and DVD and—in the tradition of satirical productions like Forbidden Broadway—regularly update the show with new material. “The problem is trying to stay ahead of the rapid changes in medicine,” LaGana says. Adds Levy: “Some years ago we wrote songs about medical tourism and about writing prescriptions over the Internet. These have become mainstream. Now, we have parodies about the health-care policy that covers nothing and hospitals telling low-income patients, ‘Go away, you’re sick!’” — Beth Saulnier Let’s put on a show: Barry Levy, MD ’71 (left), and Greg LaGana, MD ’71, created and star in the musical revue Damaged Care. SPECIAL ISSUE 2011 15 11-21WCMspecial11totg_WCM redesign 11_08 12/12/11 3:14 PM Page 16 Talk of the Gown Father’s Day A technique developed at Weill Cornell allows some men, long considered infertile, to have biological children JOHN ABBOTT Peter Schlegel, MD T he man had survived testicular cancer in his twenties, but a decade later he was facing a different kind of crisis: infertility. “Having children was critically important to him and his wife,” recalls Peter Schlegel, MD, professor and chairman of urology and professor of reproductive medicine at Weill Cornell. Because of his cancer’s advanced state, the patient had been rushed into chemotherapy without being offered the option of banking his sperm; now he’d been diagnosed as infertile. But thanks to a technique developed and refined at Weill Cornell, there was hope that he—as well as others who lack sperm in their semen for a variety of reasons—could conceive with their own DNA. “Until fifteen years ago, this was an untreatable medical problem,” Schlegel says. “It was assumed that all these men were sterile. They had to use donor sperm or adopt.” Now, he says, “their fertility options may be far better.” The technique, an outpatient procedure called microdissection testicular sperm extraction (microTESE), involves opening up the testicles and looking for sperm in a targeted way. Since there are hundreds of sperm-making tubules in each testicle, Schlegel explains, some may still produce sperm even if most do not. Those that still 16 WEILL CORNELL MEDICINE work tend to be larger, whiter, and thicker—distinctions an operating microscope can reveal. “In the past we’d do random biopsy of the testicle where you had no idea what you were sampling,” Schlegel says. “This is a completely new avenue of treatment that most people didn’t think was feasible.” The success of microTESE depends on the cause of a man’s azoospermia, the medical term for absence of sperm in the ejaculate. Overall, Schlegel and his team are able to retrieve sperm from 60 percent of men. Those retrievals lead to pregnancies nearly half the time, usually resulting in live births; random biopsies allow sperm to be found only half to two-thirds as often as microTESE does. Schlegel stresses that the technique is sorely needed. About 1 percent of men have no sperm in their ejaculate, and the problem affects twothirds of those who are treated for cancer. Despite awareness of the side effects of chemotherapy on fertility, only about a third of men bank their sperm before treatment, Schlegel says. And while prepubescent boys who are treated for cancer may ultimately be able to produce sperm and conceive naturally, sperm-preservation techniques for that age group are still experimental, involving removing testicular tissue and freezing it for future grafting. Other causes of azoospermia include undescended testicles, hormonal problems, and genetic conditions such as Klinefelter’s syndrome (in which men have an extra X chromosome) or deletions of certain areas on the Y chromosome. “Some of those men, depending on the location or type of deletion, will have sperm, and some will have zero chance of sperm,” Schlegel says. “We can quantify the chance of retrieval based on the cause.” The first published report of the microdissection procedure was in 1999. Schlegel and his colleagues published the results of microTESE among seventeen male cancer survivors in 2001, finding it successful in 43 percent of them. After trying microTESE among fifty-six more survivors, they updated their findings in March 2011 in the Journal of Clinical Oncology. Retrieval rates ranged from 85 percent among men treated for testicular 11-21WCMspecial11totg_WCM redesign 11_08 12/12/11 3:14 PM Page 17 cancer to 30 percent among those who had lymphoma, with the variation likely due to whether they were treated with platinum-based drugs that can be toxic to the testicles. Since Weill Cornell began offering the procedure fifteen years ago, it has treated some 1,400 men, about 7 percent of whom survived cancer. Patients are put under general anesthesia and anywhere from ten to 10,000 sperm are retrieved over one to two and a half hours—compared to seven hours when doctors first started performing it, Schlegel says. Usually, the sperm is used immediately to fertilize a partner’s eggs and the resulting embryos implanted, with any remaining embryos frozen for future use. Patients are given local anesthetics and anti-inflammatories to reduce swelling, but many don’t need pain medication, Schlegel says. Most return to work within three to five days and can resume everyday activities, even cycling, within a month. Fluid collection around the testicle is less common with microTESE than with random biopsies, he adds. And refinements of the procedure have reduced tissue damage, even as doctors are able to search the testicles more thoroughly than in the past. When the thirty-something cancer survivor and his wife came to Weill Cornell four years ago, their prospects looked dim. The man had undergone a random biopsy Fertile ground: Advanced techniques have allowed urologists to identify the tubules most likely to contain viable sperm. sperm-retrieval procedure elsewhere, and no sperm were found. His hormone levels and other tests also suggested little chance of finding usable sperm. But Schlegel arrived at the opposite conclusion. “We saw he’d actually be a good candidate for treatment,” he says. “Ninety-nine percent of the testicle may show no cells developing toward sperm, but even 1 percent of the testicle marginally working is a highly PROVIDED encouraging finding for us.” Doctors were able to retrieve sperm from the man—on Father’s Day, no less—and immediately injected it into four eggs collected from his wife. One fertilized and ultimately developed into the couple’s daughter, now three. When they saw Schlegel at a party for doctors and patients after their daughter’s birth, the normally stoic man was tearyeyed, and his wife broke down. “The two of them were just ecstatic,” he says. “That they went from being a happy couple together to one with children made a huge difference in their lives. It was everything.” — Jordan Lite Making Accommodations A Muslim doctor explores how medicine can honor faith-based requirements for physical modesty T a im Padela, MD ’05, was a fourth-year medical student when the legal battle over Terri Schiavo’s life made national headlines. Schiavo had been in a persistent vegetative state since 1990; her husband was seeking to respect her prior wishes by having her feeding tube removed. As the case sparked ethical debates around the country, Padela found himself called upon to provide a unique perspective. “Because I was a Muslim medical student, all of a sudden people expected me to know what the guidelines of my faith would be,” Padela recalls. “I was supposed to be an expert in Muslim health-care behavior: ‘What does Islam say about feeding tubes at the end of life?’ Having my feet in both cultures—not only being a medical practitioner, but being of the Muslim faith—I should be able to speak to both communities.” Today, such questions are at the center of Padela’s professional life. In addition to being board-certified in emergency medicine, Padela has done extensive research at the intersection of medicine and Islam. As a Robert Wood Johnson Clinical Scholar at the University of Michigan, Padela studied health-care disparities in Muslim and Arab-American populations and ways in which hospitals and physicians can accommodate the cultural needs of such patients; he has also served as a fellow with the Institute for Social Policy & Understanding, an American Muslim think-tank, working to reduce cultural barriers to clinical care for Muslim patients. This summer, he joined the faculty at the University of Chicago’s MacLean Center for Clinical Medical Ethics as well as its newly established Program in Medicine and Religion. “My interest is in how patients are treated by physicians and the health-care system,” says Padela. “Using the Muslim patient experience as a lens to look at these larger issues around health-care disparities and cultural accommodation seemed like a natural fit.” Born in New York to Pakistani parents, Padela spent part of his childhood in Pakistan; he has also lived in Egypt, where he studied Arabic and Islamic law. A double major in biomedical engineering and Arabic language and literature at the University of Rochester, SPECIAL ISSUE 2011 17 11-21WCMspecial11totg_WCM redesign 11_08 12/12/11 3:14 PM Page 18 Talk of the Gown titioner while the male physician observes, based on accommodations of these sorts of or even if he simply dons gloves to avoid he speaks Urdu, Hindi, Arabic, Spanish, things,” he says. “Many women might delay skin-to-skin contact. “The recommendaand his parents’ regional dialect. During his seeing an ob/gyn because they’re trying to tions are common sense, and they’re very final year at Weill Cornell, he became the find a female doctor. There are low rates of simple,” says Rodriguez del Pozo, who first medical student to do an elective on screening for breast, cervical, and colorectal notes that such guidelines can also apply the new Qatar campus, studying Islamic cancer in South Asian Americans, because of to treatment of observant Jews and membioethics and how the medical system feeling uncomfortable uncovering their genbers of other faiths that require modesty. accommodates Muslim patients, under the italia in front of someone else.” “As in every doctor-patient interaction, it’s mentorship of associate professor of public While all health-care institutions operall about fostering trust. A simple gesture health Pablo Rodriguez del Pozo, MD. ate under resource constraints—and it isn’t can go a long way.” That work has inspired several papers, always possible to offer a same-gender And conversely, Padela stresses, negative including one published last year in the provider—the researchers say that such interactions can have lasting consequences. Journal of Medical Ethics entitled “Muslim issues can often be ameliorated through “Patients will talk to me about being in a Patients and Cross-gender Interactions in communication and minor adjustments. nursing home after a stroke, and what they Medicine: An Islamic Bioethical PerFor example, a patient can be allowed to remember most was being bathed by a perspective.” The article, which garnered covwear his or her own clothes, or a more son of the opposite sex—for them, that was erage in the New York Times and USA Today, modest robe, rather than a revealing hospia daily humiliation,” he says. “Or a Muslim opens with a theoretical case: a thirty-fivetal gown, and uncover only those body female who comes to the ED with vaginal year-old African American woman comes parts that are clinically necessary for exambleeding, and all she’s told into an urgent care clinic comis, ‘We can’t assign a woplaining of leg pain after a fall. man to take care of you.’ Accompanied by a male relaThat can have lasting tive, she’s wearing a Muslim effects on whether they go headscarf and refuses to to a health-care provider remove her clothes or don an next time—and the real exam gown. When the male issue is how they felt they physician tries to introduce were treated. People may himself, she asks, “Are there not mind that they couldany woman doctors around?” n’t find an accommodaThe paper goes on to tion so much as the way it explore the various Islamic was delivered.” rules surrounding modesty and Instead of dismissing a gender interaction that can patient’s concerns for the affect medical treatment; they sake of expediting treatinclude the prohibition against ment, Padela says, proan unrelated woman and man viders can often bridge the being alone together, physical gap by assuring patients contact between the genders, or WEILL CORNELL MEDICAL COLLEGE that they respect their cusuncovering certain body parts, Modernity meets modesty: At WCMC-Q, students can practice examination toms and will do their best such as a woman’s hair. “There on a simulator—but when it comes to seeing a patient of the opposite to honor them. As Rodis a preference that, ideally, a gender, they’re trained to inquire if the person feels comfortable with it. riguez del Pozo puts it: patient should be treated by a “Efficiency and modesty Muslim physician of the same are not always 100 percent compatible— ination. “Here in Doha, a male doctor or sex—a man by a man or a woman by a and we probably need to be a little bit less student does not go in to see a female woman,” Rodriguez del Pozo notes. “If that efficient to satisfy the patient’s request for patient unless he has first asked a female is not possible, the second best is a nonmodesty. As in many other instances, that’s nurse, doctor, or classmate to inquire if the Muslim of the same gender. The third prefersimply good medicine.” Padela points out patient minds being seen by a male,” ence is by religion again. And in last place, a that medicine has a long tradition of Rodriguez del Pozo notes. “It’s not the law, non-Muslim of the opposite sex.” He notes accommodating religious requirements— but it’s the custom of the place. My stuthat among observant Muslims, such issues from the development of bloodless surgery dents have to learn it very early on: you aren’t just a matter of discomfort or personal for Jehovah’s Witnesses to the use of don’t go into a room without asking.” preference. “In Islamic traditions,” he says, Sabbath elevators for observant Jews. “In To avoid breaking the prohibition “these are commands.” our medical encounters, we’re playing the against being fully alone with a member of As Padela has found in his research, role of doctor, no matter where we come the opposite sex, physicians can use a priincluding focus groups he has conducted from,” he says. “Whatever I can do to make vacy curtain instead of closing the exam with Muslim Americans, lack of accommothe patient experience better, as long as it room door. As in the resolution to the dation for modesty rules can have marked doesn’t compromise my own values, I will paper’s theoretical case, strictures against effects on health outcomes. “Studies have try to do.” touching can be satisfied if the physical shown that Muslim women in Michigan — Beth Saulnier exam is conducted by a female nurse pracchange their health-care-seeking habits 18 WEILL CORNELL MEDICINE 11-21WCMspecial11totg_WCM redesign 11_08 12/12/11 3:14 PM Page 19 Data Plan With electronic records key to health-care reform, a Weill Cornell program aims to train a new generation of health IT professionals Jessica Ancker, PhD, MPH ABBOTT K aren Gonta has a vision of medical information without borders. “Once we’re able to share electronic data across the entire system and put an end to the fragmentation of information, we’ll transform health care as we know it,” says Gonta, a caseworker at an Ithaca-based mental health clinic. “We stand to learn a lot about what’s working and what isn’t, and to compare newer treatments with standard ones.” Now in its second year, the Weill Cornell Health Information Technology Certificate Program is training professionals like Gonta for careers at the nexus of health care and IT. The six-month program is a collaboration between the Weill Cornell Graduate School of Medical Sciences and Columbia University’s Department of Biomedical Informatics. Faculty on the two campuses collaborate to develop shared educational materials, but admit and train separate classes of students. In early 2010, it was one of nine programs nationwide to receive a federal health IT stimulus grant to establish one of these advanced training programs. Health IT is a national priority—and a major feature of the American Recovery and Reinvestment Act of 2009, with an investment of up to $30 billion. As such, it promises to improve the way patients receive, experience, and benefit from health care in the twenty-first century, says program director Jessica Ancker, PhD, MPH, an assistant professor of pediatrics and public health. “It may seem surprising,” says Ancker, “but fewer than half of the private medical practices in the country have converted from paper to electronic record-keeping—and even the ‘wired’ minority still may not be reaping the full benefits of the technological revolution in health care.” The main focus of health IT is the development and implementation of electronic health records (EHRs). The Office of the National Coordinator for Health IT, the government agency funding the health IT initiative, has developed a program to incentivize physicians and hospitals for the “meaningful use” of EHRs to improve the quality, safety, and efficiency of care. To accomplish this, EHRs must provide important functions such as decision support, must be compliant with privacy and security regulations, and must be interoperable— that is, able to share data with all players on a patient’s health-care team. “Electronic health records offer much more than just the electronic storage of patient data,” says Rainu Kaushal, MD, MPH, the program co-director and the director of the Center for Healthcare Informatics and Policy at Weill Cornell. “They have the ability to potentially transform care by making sure the right thing is done for the right patient at the right time in more efficient ways.” To accelerate the conversion from paper to electronic records, the federal government is offering monetary incentives to health-care providers and hospitals that can demonstrate that they have purchased EHR software and are using it effectively and appropriately. At the same time, Ancker says, EHRs must be designed to match the needs of real-world clinical care—needs that vary with specialty, geography, and patient population, among other factors. “When you consider the many components of patient care—hospitals, pharmacies, insurance plans, public health departments, and thousands of private medical practices scattered across the country—you begin to get a sense of the complexity of our health-care system,” Ancker says. “Without rigorous training in the specific needs and parameters of health care, even the most sophisticated IT specialist could get lost in the labyrinth.” The Weill Cornell program offers a rigorous curriculum with a mix of health informatics theory, pragmatic application SPECIAL ISSUE 2011 19 11-21WCMspecial11totg_WCM redesign 11_08 12/12/11 3:14 PM Page 20 Talk of the Gown of that theory, and team-based collaboration on multidisciplinary projects. Students become versed in the legal and financial dimensions of EHR technology, along with the policy implications of the national push to connect all the elements of the health-care system through technology. Online lectures cover topics as diverse as the culture and politics of health care, data-sharing and security, reporting requirements, and project management. The program also includes facilitated teamwork with experts in academia and industry; one Saturday per month, students convene in either New York City or Ithaca for intensive collaboration on a project, with the two groups teleconferenced together. “For example, we might present them with an EHR that has weaknesses and challenge them to think through a variety of solutions to the problem,” Ancker says. “In a small-group environment, they’ll decide whether the system needs to be modified, overhauled entirely, or replaced with another type of software. They also learn to enter data, requiring them to get down to the granular level around the codes pertaining to particular medical conditions, and retrieve data that might be useful for quality reporting or public health.” The Weill Cornell program graduated twenty-six students last summer, with a new class set to finish in March 2012. They include physicians, nurses, other health professionals, and administrators, along with IT specialists seeking new careers in health care—one of the fastest growing fields even in this sluggish economy, according to the Bureau of Labor Statistics. An estimated 55,000 new health IT jobs are expected to be created in the next five years, industry analysts say, spanning such diverse positions as quality assurance engineer, EHR software trainer, and clinical analyst. Ancker stresses that students don’t need to be tech wizards to do well in the program and gain the necessary skills to succeed on the job. Recent graduate Mary Koval, a registered nurse who manages the clinical quality program for the Weill Cornell physician organization, confesses that she used to find computers intimidating. “I’ve been involved in quality management for more than fifteen years,” she says. “When I started, we used manual chart reviews to assess quality of care. I didn’t know whether I’d take to the technology when I entered the program—but it quickly became second nature for me.” 20 WEILL CORNELL MEDICINE The program’s combination of distance and on-site learning worked well for Koval and also for Gonta, who’s raising a sevenyear-old daughter in addition to working full-time. Its flexible structure also appealed to Joseph Wu, who attended while studying for a master’s in health administration through Cornell’s Sloan Program. With his certificate in hand, he jumped into a summer internship at PricewaterhouseCoopers in New York City, where he further honed his skills in health IT strategy and implementation. “When I applied to the certificate program, the field was growing so fast that I didn’t know what would be offered,” says Wu, who is on track to complete his master’s this spring. “It was only afterward, during my internship, that I saw the total relevance and quality of my training.” — Margaret Crane Blind Faith With a radical new prosthetic retina, Sheila Nirenberg, PhD, aims to help millions with degenerative eye disease ABBOTT Sheila Nirenberg, PhD S ome ten million Americans have degenerative retinal disease; of those, 1.9 million suffer from advanced-stage blindness. Historically, there has been little that doctors can do. Medications help only a small subset of patients—and then just slightly improve vision or slow the disease’s progress. So far, prosthetic retinas 11-21WCMspecial11totg_WCM redesign 11_08 12/12/11 3:14 PM Page 21 have had limited appeal: they reveal high-contrast edges and spots of light, allowing people to orient themselves within spaces they already know but hardly approximating normal vision. But now an experimental, next-generation artificial retina developed by Sheila Nirenberg, PhD—associate professor of computational neuroscience in the HRH Prince Alwaleed Bin Talal Bin Abdulaziz Alsaud Institute for Computational Biomedicine and in the Department of Physiology and Biophysics—is currently in the animal testing phase and showing great promise, producing images so sharp and subtle that they closely resemble what a fully sighted person would see. In healthy eyes, the retina serves as the entryway for visual information to travel to the brain. At its front end, photoreceptors pick up patterns of light and dark. In the middle, complicated circuitry extracts information from those patterns, “converting it into a code the brain can read,” Nirenberg explains. From there, the retina’s ganglion cells send that neural code to the brain in the form of electrical signals called spikes. Any image can be converted into its own corresponding code, or pattern of spikes, using a set of mathematical equations. Existing artificial retinas, which have been around for about two decades, have tried to replicate the work of the photoreceptors with surgically implanted, light-receiving electrodes. But without incorporating the neural code to decipher what’s in front of the eye, Nirenberg says, “they’re very limited—it’s nothing close to normal vision.” She and postdoc Chethan Pandarinath, who earned a PhD in Nirenberg’s lab, have taken a different, two-pronged tack: a device that processes the code plus gene therapy that activates the ganglion cells. Surgically implanted electrodes are not the main focus of Nirenberg’s design. Instead, a patient would receive gene therapy that makes the ganglion cells—which are typically spared by retinal diseases—express a light-sensitive protein called channelrhodopsin. “Surgery won’t need to be involved,” Nirenberg says, “just a quick injection into the eye.” About three weeks later, after the therapy has taken hold, a patient would don glasses containing a camera and a chip (similar to the microprocessors inside cellphones) that processes the code. The camera “sees” the images and sends them to the chip, which converts them to light pulses. Those pulses are actually image-specific neural code, and they activate the light-sensitive channelrhodopsin in the ganglion cells. In so doing, the cells can fire the right code to the brain so the patient can see. “Other people have also used this light-sensitive gene, but they don’t have the retina’s code, which is our key ingredient,” Nirenberg notes. “We’ve brought it back to life so it can fire like a normal retina.” Until she began testing the artificial retina, Nirenberg’s focus was largely on basic science, focusing on two fundamental conceptual challenges in neuroscience: understanding the neural code and determining how populations of retinal neurons work together to encode scenes such as faces and landscapes. In 2009, one of her students mentioned improvements in channelrhodopsin technology—and Nirenberg had a eureka moment. “I thought, Wow, now we can put our knowledge of the code with channelrhodopsin and this will work,” she remembers. “I almost fell off my chair. I realized I knew exactly how to make a prosthetic.” When Nirenberg and Pandarinath tested the concept in mice later that year, it worked as anticipated. In findings she presented at last year’s Society for Neuroscience meeting, Nirenberg showed that the retinas of completely blind mice were able to produce normal firing patterns and animals treated with the technology could discern moving images. The results led to a $250,000 prize from the BioAccelerate NYC A B C D PROVIDED BY SHEILA NIRENBERG contest to develop the technology for commercial use. Nirenberg plans to collaborate with scientists from Harvard, the University of Florida, and a German company to develop it for monkeys—and, ultimately, people. “It’s exciting to know that what you’ve been working on suddenly has human value,” Nirenberg says of her shift from basic science to clinical applications, “especially as the years go by and you realize you need to do something for people, not just because it’s intellectually interesting.” Tests of the retina in monkeys have begun, and if all goes well, it could be on the market within five years, Nirenberg says. The coding aspect of the technology could also be used to drive the electrodes in patients with older prosthetic retinas. If the device sounds like science fiction, Nirenberg says, its results would be unmistakably real to the people who receive it. She admits that patients wearing the glasses might “look sort of dorky.” But the ultimate hope, she says, is that “they’d be able to see—see patterned images, see faces, walk through the supermarket and pick out a box of cereal, recognize their children.” — Jordan Lite In sight: An image of a child’s face seen in its original form (A), as it has been encoded by the new prostethic device (B), and how it is reconstructed from those signals and “seen” by the patient (C). D shows the same image reconstructed from the signals of a blind retina treated with the standard prosthetic. SPECIAL ISSUE 2011 21 22-29WCMspecial11gotto_WCM redesign 11_08 12/12/11 3:36 PM Page 22 Passing the Torch A conversation with Dean Antonio Gotto By Beth Saulnier A t the end of December, Antonio M. Gotto Jr., MD, DPhil, steps down after fifteen years as dean of the Medical College. The decade and a half since Dean Gotto took office have been transformative years for Weill Cornell—physically, financially, academically, and scientifically. During his tenure, the Medical College has seen an overhaul of its curriculum; record-setting fundraising campaigns; a renaming in honor of foremost benefactors Joan and Sanford Weill; the establishment of the Qatar campus and of a medical school in Tanzania; affiliation with the Methodist Hospital in Houston; and the development of state-of-the-art facilities including the Weill Greenberg Center and the Belfer Research Building, which will double the institution’s lab space when it’s completed in 2014. Gotto was born in Nashville, the son of a schoolteacher and a publishing company employee. He earned his undergraduate degree in chemistry from Vanderbilt University with minors in English and math. As a Rhodes Scholar, he earned a doctorate in biochemistry 22 WEILL CORNELL MEDICINE from Oxford under Sir Hans Kornberg, PhD, and Nobel laureate Sir Hans Krebs, MD, before returning to Vanderbilt for his MD. An expert in lipid science whose work helped establish statins as a standard of cardiac care, Gotto came to Weill Cornell from Houston’s Baylor College of Medicine and Methodist Hospital, where he served as chairman of medicine for two decades. He and his wife, Anita, have been married for fifty-two years; they have three daughters and five grandchildren. After retiring as dean, Gotto will remain on the faculty, continue his research, and serve as a Cornell University vice president and as co-chairman of the Weill Cornell Medical College Board of Overseers. This fall, Dean Gotto sat down for a conversation with Weill Cornell Medicine, offering thoughts on such varied topics as his legacy, the landmark Weill gift, the relationship between the Medical College and the Ithaca campus, his yen for spy novels—and what he hopes the New York Times will leave out of his obituary. JOHN ABBOTT JOHN ABBOTT 22-29WCMspecial11gotto_WCM redesign 11_08 12/15/11 11:26 AM Page 23 SPECIAL ISSUE 2011 23 22-29WCMspecial11gotto_WCM redesign 11_08 12/12/11 3:36 PM Page 24 To mark Dean Gotto’s retirement, Weill Cornell Medicine asked prominent members of the Medical College community to share their encomia. For Sanford Weill’s remarks, see page 3. Weill Cornell Medicine: What do you find most gratifying about academic medicine? Antonio Gotto: There’s excitement in discovery, but also in passing on knowledge to the next generation—seeing them stimulated in intellectual curiosity, which they will apply whether they’re doing research or practicing medicine. It’s our intention that our students have inquiring minds, and in practice they will continue the process of learning; by being curious they’ll find things that help their patients. A WCM: How was your medical school experience different from that of today’s students? How have you seen medical education evolve? AG: It was based very much on a large lecture approach, and there are fewer lectures today. Our new curriculum, when it was introduced fifteen years ago, moved away from that and toward small-group, problem-based learning. Now we’re in the process of changing again, toward competency training—letting people move at different paces. Another difference is that for residents and students there are limited hours. There weren’t any regulations like that; you could be on as long as you had to be on. This has obvious disadvantages of fatigue, but there’s an advantage in the continuity and the experience that you get. When I was a student at Vanderbilt, the only way an intern could get a vacation was to get a medical student to fill in. It was good clinical experience for students, but you can’t do that today without breaking some regulations. s dean and provost for medical affairs, Tony Gotto has advanced clinical care, research, education, and outreach, including major global health initiatives. He has helped bring significant new resources to the College, recruited outstanding new faculty, and developed and renovated clinical and research space. He was a driving force behind the construction of our new Belfer Research Building. And he expanded the College’s mission globally, with the establishment of Weill Cornell Medical College in Qatar. He is also a superb role model for our students. A world leader in atherosclerosis research, he has shown enormous dedication to the public good, disseminating information about cardiovascular disease to the general public as well as to the medical profession. And he has led Weill Cornell to greater contributions in global health, advancing our efforts in Doha, at Weill Bugando Medical Centre in Tanzania, and in Haiti, Brazil, and elsewhere. I’m delighted that Tony has agreed to stay on for three years as University vice president and co-chair of the Board of Overseers. His leadership will be invaluable. David Skorton, MD President, Cornell University A lthough Dr. Gotto and I were in Houston at the same time, we did not know each other then. However, before coming to Weill Cornell, I heard a great deal about him—all positive—and it has all proven true. What I have learned since is that he has a remarkable knack for pushing things forward, even though people don’t always realize they are being (gently) pushed. He was missed a great deal when he left Baylor and Methodist, and he will be missed here as well. Michael Stewart, MD Professor and chairman, Department of Otolaryngology–Head & Neck Surgery E. Darracott Vaughan, MD, Senior Associate Dean for Clinical Affairs 24 WEILL CORNELL MEDICINE WCM: Why is medicine still a gratifying career for young people to go into? One hears about physicians telling their kids, “Don’t go into medicine, it’s managed care, it’s not the same.” AG: Medicine enables you to help people, and at the same time you’re learning new things, which goes on throughout your career. You have curiosity about discovery—whether it’s in the laboratory, in the clinic, or just observing your patients. I think that combination will continue to stimulate the best and the brightest to go into medicine, even with all of the restrictions and various negative things that you may hear about it. WCM: Is it true that you originally wanted to be a lawyer? AG: It’s true. I was on the debating and forensics teams in school and at Vanderbilt, so I thought the legal profession and politics would naturally follow. My father did not have a high regard for lawyers, so after discussions with him, I decided I would pursue medicine instead. I thought about engineering and other possibilities, but I felt that medicine would be more interesting and challenging. Growing up, I was a great fan of Sherlock Holmes; I read all of his stories and got interested in using chemistry and other techniques to solve crimes—which is not that different from using chemistry to solve medical mysteries. WCM: At Oxford, you worked under the legendary biochemist Hans Krebs, who won the Nobel Prize for discovering the citric acid cycle known as the Krebs Cycle. What was that like? AG: My direct supervisor was [the eminent biochemist] Sir Hans Kornberg; Sir Hans Krebs was the professor and my internal examiner. Professor Krebs was very Germanic. Every morning he would come by and say, “Vat are you doing?” and I would explain to him what I was doing. During the course of my research, which was to determine how microorganisms grew on a particular two-carbon compound, I discovered a new enzyme and managed to crystallize it. After convincing myself these were real crystals by repeating it several times, I got up in the middle of the night and made fresh preparation, which were beautiful structures, and set up a phase-contrast microscope. So when Professor Krebs came in sharply at eight, he asked me the usual question and I said, “I have something I’d like to show you.” He looked it at and said, “Satisfactory, quite satisfactory.” Kornberg, who was my tutor, asked, “What did the professor say?” I said, “I don’t think he was too impressed. He said, ‘Quite satisfactory.’ ” Kornberg said, “When I discovered the glyoxylate cycle, he only said ‘Satisfactory’—so that’s the highest praise you’ll ever get.” WCM: What excited you about lipid science? Why did you devote your research career to that field? AG: One reason is it offered the opportunity to study a disease at a basic science level and also at a clinical level, to treat patients. Number two, lipids play a central role in cardiovascular disease, which is our major killer. It’s been gratifying to see the development of statin drugs, which 22-29WCMspecial11gotto_WCM redesign 11_08 12/12/11 3:36 PM Page 25 JANET CHARLES W White coat to black tie: Gotto accepts the Greenberg Award in May 2010. have been so effective not only in reducing cholesterol and modifying lipids, but also in treating and preventing disease. WCM: Because you were involved in some of the major trials that demonstrated that efficacy, you have helped prolong millions of lives, which is something that your average physician can’t say. How does that feel? AG: I believe I’ve made some contribution to the field, but there are a lot of others also. It feels good to be working on something that has turned out to be so beneficial. It’s not as if after ten years they found out the drugs cause cancer or cause people to go blind—both of which were feared at the time. WCM: So in the early days, it was feared that statins could be dangerous? AG: It was thought that if you interfered with cholesterol or metabolism you were likely to cause some bad effects. In 1989, an investigative reporter named Thomas Moore wrote an article in the Atlantic called “The Cholesterol Myth” that said lowering your cholesterol won’t make you live any longer and may cause you harm. Much of what he claimed turned out to be incorrect. Lowering cholesterol doesn’t cause cancer, can be treated with drugs, and does prolong life. He claimed the “cholesterol myth” was part of a giant conspiracy concocted by scientists in NIH who wanted more government funding, as well as by pharmaceutical companies, the American Heart Association, and the American College of Cardiology—and that this whole conspiracy was masterminded by a small group of academics that he called the Cholesterol Mafia. My name was Antonio Gotto, so I was not surprised to be included. WCM: Have you been able to keep up with your research, with the demands of your job as dean? AG: To a limited extent. I had a large specialized center of research for atherosclerosis the entire time I was in Houston. I maintain some research collaboration and involvement in hat is the secret to Tony Gotto’s uncanny ability to recruit so effectively and to surround himself with such remarkable talent? It’s quite simple. (His absolute integrity, fairness, and values go without saying.) Once Tony develops confidence in a faculty member, he lets him or her “fly.” He guides, mentors, and remediates by nudging, not browbeating. He frees his faculty to blossom and meet their potential. Micromanagement is not in his vocabulary. So, in my opinion, Tony Gotto’s most important contribution to our Medical College has been not so much the magnificent clinical and research buildings that have revitalized an aging campus, not his infusion of a Texas-style “can do” attitude toward fundraising, nor his ability to bring meaningful stability to this academic medical center during a period of external turbulence. Of course, those are all important and they will be remembered. But his most important contribution to WCMC has been his legacy of academic and clinical excellence in an environment that nurtures individual creativity within a vibrant community of collective scholarship. Andrew Schafer, MD Chairman, Department of Medicine E. Hugh Luckey Distinguished Professor I have always been amazed at how Tony can not just master arcana, but can turn around and use this information effectively. Here is but one example: At one time, to construct the Belfer Research Building, the Medical College was going to amend the ZLDA by going through ULURP to extend the LSCFP. In the end, we decided to go directly to BSA to get the required FAR. Now, Dr. Gotto, being a busy guy, could not possibly have heard these arcane real estate terms more than once. Nonetheless, he stood up in front of a group of donors (many of whom were in the real estate business) and, in response to a question about zoning, delivered a completely cogent and amazingly accurate summary of the college’s process, using every term with precision! Stephen Cohen Executive Vice Provost SPECIAL ISSUE 2011 25 22-29WCMspecial11gotto_WCM redesign 11_08 12/12/11 3:36 PM Page 26 I met Dean Gotto many years ago when he presented his “State of the Medical College” address to the Alumni Association board. I was impressed that the dean took the time out of his busy schedule to address a group of alumni with a detailed and well-thoughtout presentation. I cannot overstress the goodwill it created. It made alumni in general, and the board in particular, feel relevant to the Medical College and the students. Many programs have been started and expanded under his watch, including the Stethoscope Initiative, Alumni to Student Knowledge program, and the Dean’s Circle, which now boasts more than 162 members. Dean Gotto is affable and self-effacing, exemplified by his recounting of the newspaper report of his hiring as, “Famous cookbook author hired as dean of Cornell Medical College.” Michael Alexiades, MD ’83 President, WCMC Alumni Association D r. Gotto and I have worked closely together on fundraising for Weill Cornell. We have had some tremendous successes, a few surprises, and some disappointments. Human nature being what it is, we have also had some laughs. He has been a superb fundraiser for several reasons: he has been dean at the right time, at the right institution, and with the right leadership. Weill Cornell’s mission and its location in New York City have been catalysts for support, and the leadership of our Medical College is outstanding. He has built thoughtful and productive collaborations with Cornell University and with NewYork-Presbyterian Hospital. He has encouraged, and put his trust in, a skilled development team. I believe, however, that the real key to his success lies in his character. I’m no expert, but I spend a lot of time around powerful and successful people. Among august types such as these, Dr. Gotto stands out. He is a man of great integrity, passion, and grace. He also has natural kindness and humility, attributes that cannot be taught. He approaches donors as valued friends—and when gifts come in, he is as happy for the donor as he is for Weill Cornell, because he knows that a special bond has been created. Larry Schafer Vice Provost for Development 26 WEILL CORNELL MEDICINE AMELIA PANICO Global vision: Gotto with Tanzanian President Jakaya Kikwete in April 2010 clinical trials, but to a much lesser degree. I do think that it’s a good idea for administrators to maintain contact with their roots. WCM: Have you been able to keep a hand in patient care? AG: Yes, I still see consultations. WCM: How has that informed your work as dean? AG: You see the move from paper records to the electronic medical record, you see more regulations, reporting requirements, and red tape. This allows you to experience the problems the practicing physician is facing. WCM: How did you come to be recruited to Weill Cornell in the first place? AG: After I’d been at NIH for about three years, I started getting offers from medical schools and universities. In 1970, I received an offer from Cornell for an endowed professorship in cardiology. After several visits, I ended up going to Texas. At that time, we had three young children and thought Houston would be a good place to rear them; our oldest daughter had been diagnosed with juvenile diabetes, which requires a lot of attention. While Cornell had a long and excellent history, Baylor was a newer medical college; it had a frontier spirit and seemed to offer opportunities to build programs. Seven or eight years later, I was invited back to look at the chairmanship of medicine, but I wound up staying in Texas. Then when Dr. Gordon Douglas retired as chairman, I came for another visit. So that was the third attempt to recruit me. And finally the fourth time . . . WCM: So we had to woo you four times before you said yes? AG: Four times before I left Texas, yes. WCM: Was it hard for a Southern gentleman to move to New York? AG: I had been chair of medicine for twenty years at Baylor and Methodist Hospital, and 22-29WCMspecial11gotto_WCM redesign 11_08 12/12/11 3:37 PM Page 27 thought I had accomplished most of what I would be able to do there. What was also different from the three earlier recruitment attempts was that our daughters had grown up and were no longer living at home. In 1970 I had actually timed the commute from Ridgewood, New Jersey, to the medical center and decided it was too long to do every morning. So I knew I wanted to live near the medical center, where I’d be spending most of my hours. We wound up living ten years at Payson House, which is just across the street. WCM: In a nutshell, what’s special about Weill Cornell? AG: The collegiality of the faculty. It’s small enough that people get to know their peers quite well. It has a nurturing atmosphere toward students, faculty, staff, and patients. It has a reputation as a good place to work and a good place to be. It has an enthusiastic board that has been enormously generous, and a supportive university board and president in Ithaca. WCM: What did the Weills’ landmark gift mean to the institution? AG: It had a transforming effect, because it triggered a series of successful philanthropic campaigns, including one of the largest fundraising campaigns any medical school has ever carried off. WCM: How has the college evolved during your tenure? AG: When I came, it had a reputation for high-quality clinical work and education, but it had a small research platform and not much research space. It was financially strapped. We had not had a large fundraising campaign in some time. Our activities were restricted here in Manhattan; we’d had an affiliation with North Shore University Hospital, but that had been terminated. And so we had to develop a series of teaching sites in the NewYork-Presbyterian/Weill Cornell network, at affiliated hospitals that hadn’t been used much for teaching. We’ve moved to a much greater extent on the international scene, as well as nationally with an affiliation with the Methodist Hospital in Houston. We also started a series of fundraising campaigns, each targeted toward specific projects—scientific and clinical objectives or capital projects, such as the Weill Greenberg Center and currently the Belfer Research Building. WCM: How is the experience of the average Weill Cornell student different now compared to when you arrived? AG: Almost half of our students now take an overseas elective. A lot of them do research; there’s more research going on at the Medical College and more of the MD-PhD students are working in labs here. The MCATs and GPAs of entering students are higher than they were then. The average age of entering students is 23.7 years; most have done volunteer work, worked in a laboratory, or served in the Peace Corps. It’s a highly qualified group. It’s a different profile than before; as physicians, I hope they will be equally successful as our distinguished alumni. WCM: The Qatar branch was established during your deanship. Why is the campus important to Weill Cornell? AG: It represents a partnership with the Qatar Foundation with the aim of establishing an academic medical center in an Arab country in the Middle East, and I think it was a wonderful opportunity. It has enabled us to test our curriculum, which at that time had been in effect only five years, in a different cultural environment but with the same academic standards. It has allowed our doctors, students, and scientists to do research in a population we had not had access to before. And I think that if anything can create better relationships among different cultures and different parts of the world, it’s medicine. Medicine knows no boundaries. WCM: How has the relationship between Weill Cornell and the Ithaca campus evolved? AG: I like to think that the relationship and interactions with Cornell in Ithaca have grown and increased during my tenure. This has been a high priority. We will have space in the new building dedicated to joint projects. We’ve given a number of seed grants to stimulate research between investigators on the two campuses, and they have paid off; they have usually led to large follow-up funding from NIH or foundations. WCM: What about the relationship between Weill Cornell and NewYork-Presbyterian? AG: To have a great medical center, a hospital and a medical college have to work hand in hand. We’ve been joined at the hip since 1927, after Payne Whitney bought this property I t is a huge honor to follow in the distinguished footsteps of Dean Antonio Gotto. Thanks to the great work of Dean Gotto, WCMC is poised to be one of the leaders in academic medicine in this country. With the new Belfer Research Building under construction because of Tony’s immense success in attracting resources, this institution is ready to achieve the preeminence in the biomedical sciences that it has already achieved in clinical medicine. Thanks to Dean Gotto, WCMC is also unique among academic medical centers in having forged meaningful partnerships here and abroad. Every one of these partnerships has been groundbreaking. WCMC has benefited from Dr. Gotto’s superb leadership, and I will have the tremendous advantage of his continued engagement, advice, and wisdom over the next several years. If I can be half as effective as he has been over the last fifteen years, I will count my tenure as dean a success. Laurie Glimcher, MD Incoming Dean T ony Gotto was responsible for quantum qualitative and quantitative growth in research, clinical care, and the educational experience at Weill Cornell. He accomplished this by garnering great philanthropy and directing it to support a multiplicity of research, clinical, educational, and even lifestyle programs. He oversaw the recruitment of numerous gifted scientists and developed the infrastructure necessary to facilitate a marked increase in NIH and other extramural funding. He recruited several clinical chairs and significantly grew the full-time faculty. He led the Medical College through two successful LCME accreditation reviews and oversaw curriculum reform. With his great success in attracting philanthropy to build the Belfer Research Building, he has positioned us to become one of the ten leading medical schools in the U.S. Daniel Knowles, MD David D. Thompson Professor and Chairman, Department of Pathology and Laboratory Medicine CMO, Weill Cornell Physician Organization SPECIAL ISSUE 2011 27 22-29WCMspecial11gotto_WCM redesign 11_08 12/12/11 3:37 PM Page 28 T ony is remarkable; he is dynamic with enormous energy and leadership ability. He has fostered an environment of collegiality and collaboration within the Medical College and with its partners in the Tri-Institutional area on York Avenue and around the world. He is able to engage with a wide variety of individuals, bringing out the best in them to enlist their support. This is not a skill that can be easily learned; I believe that it distinguishes leaders who will leave a lasting legacy from those who will not. A hundred years from now, Tony Gotto will be remembered for leading Weill Cornell into the twenty-first century and helping to forge a new model for academic medical centers in the world. David Hajjar, PhD Dean, Graduate School of Medical Sciences I have been impressed with Dean Gotto’s deep appreciation and respect for our students and how he made them feel supported and welcomed. Each year he attended the annual boat ride for matriculating students, an opportunity to welcome them to the Medical College. The next day, he always presided over opening ceremonies—something the students really appreciated. Dean Gotto and his wife, Anita, hosted a reception for the first-year class at their home, purposefully arranging it without a lot of administrators present so that he had a chance to meet the students. The teaching faculty also grew to respect and admire Dean Gotto. They appreciated the fact that he carved out time every year to attend the annual education retreat. Dean Gotto regularly supported the Excellence in Teaching Awards, another reason why the faculty respected his engagement at WCMC. There are so many things that Dean Gotto championed to make WCMC a better place for our students and faculty. He made WCMC a special place and promoted extraordinary growth in all of its missions. We must also thank Anita for lending him to us for these many years. Carol Storey-Johnson, MD ’77 Senior Associate Dean for Education Associate Professor of Clinical Medicine 28 WEILL CORNELL MEDICINE RENE PEREZ Life partners: Gotto with his wife, Anita, a former school teacher and avid volunteer when it was a swamp and gave it to New York Hospital and Cornell University with the condition they come together, move up here from lower Manhattan, and form the New York Hospital-Cornell Medical Center. The chairs of the clinical departments are the chiefs of services, so they are jointly selected by the Medical College and the hospital. Our faculty are the doctors at the hospital; we occupy different parts of the same building, so we’re closely tied. I’ve been fortunate to work with Herb Pardes, who during most of my tenure was president and CEO of the hospital. We had known each other a long time and had shared values about what an academic medical center should be. WCM: Why is the Belfer Research Building so vital to Weill Cornell? AG: Research not only generates new knowledge, it attracts students. It also attracts patients, who want to go where new things are being done and where, in some cases, they can get into clinical protocols that aren’t available elsewhere. The reputation of an institution depends not only on its clinical prowess, but also on the new knowledge that comes out of it. So it’s important for the future of this institution that we build on research and not just be an education and clinical service organization. WCM: What will retirement look like for you? Will you be able to pursue interests, both professional and otherwise, that you haven’t had time for? AG: Well, I’m retiring as dean, but I’m not retiring. There’s a transition period of three years when I’ll continue working with the new dean and President Skorton, however I can be helpful to them—but particularly, I imagine, in philanthropy and in some of the affiliations I’ve helped establish, as well as with interactions with life sciences in Ithaca. 22-29WCMspecial11gotto_WCM redesign 11_08 12/12/11 3:37 PM Page 29 WCM: What words of advice might you have for your successor? AG: The advice I would give is not to forget that we have a tri-partite mission, and we have to pursue it on all fronts. WCM: What are your interests and passions outside of work? AG: My wife, children, and grandchildren. From a recreational standpoint, I enjoy tennis and water sports. I like to play golf, but I haven’t had the opportunity to play much, and I’m a very poor golfer. I do like to fish, and I keep a sailboat in Maine. We have a house in Wayne, a little village about an hour and a half north of Portland, where we go in August. Maybe we’ll spend more time there. Also, my wife and I enjoy travel. We’re interested in history, including the history of medicine, and various other things like spy stories. WCM: Who’s your favorite spy novelist? AG: Daniel Silva. He writes about a Mossad operative who is an art restorer. WCM: And Mrs. Gotto? What are her interests? AG: She was an elementary school teacher; she taught school in England when we were there. But with two of our three daughters with juvenile diabetes and my career having such time demands, she has devoted her life to the family. She has been a vital part of my career; her interactions with faculty, staff, students, overseers, and potential donors have been indispensable. She has also supported the various organizations that I’ve been involved with, and she has been active with the Juvenile Diabetes Foundation. She also worked with the American Heart Association, has always had an interest in libraries, and has been an elder at Fifth Avenue Presbyterian Church. Most of all, she has been my life partner, main confidante, critic, and friend. WCM: Did any of your daughters follow you into medicine? AG: My eldest is a liaison psychiatrist with cancer patients at City of Hope outside Los Angeles. She went to Baylor, and she didn’t want to be treated differently because her father was head of medicine, so she’d wear her name tag inverted. My second daughter, who has been incapacitated since 2003 due to a stroke, was a medical social worker before she was disabled. So two of the three went into some aspect of medicine. My third daughter is an investment banker with Goldman Sachs. She was in Hong Kong for three years, and she’s just moved back, so she and four of our grandchildren are living a few blocks from us. WCM: One day, hopefully decades from now, the New York Times will run your obituary. What would you like it to say about your legacy to Weill Cornell? AG: I don’t want to be remembered for what they wrote when I came, which was: “Cornell selects cookbook author.” That’s what they pulled out of my bibliography. So you never know with the New York Times. WCM: You’re a cookbook author? AG: Dr. Michael DeBakey and I wrote several books for the general public on the Living Heart Diet. WCM: And as to your legacy? AG: It’s hard to do this without seeming immodest. I would like to think that I have helped make Weill Cornell a gentler, more collaborative place, but also one that was transformed in its academic endeavors. The legacy, to some extent, will depend on what happens to these things—if the Belfer Research Building recruits superb medical scientists and there’s great work coming out of that. I hope that we’ll see an academic medical center in the Middle East. I hope we’ll see stronger relations with Ithaca, Tanzania, and the Methodist Hospital in Houston—that these things will continue to flourish. I hope that this is a place where students will want to come, where doctors will want to practice and do research, and where patients will want to be treated. A sked what was the biggest test for leaders, the British prime minister Harold Macmillan is said to have replied, “Events, dear boy, events.” Everyone knows that Tony Gotto’s service as dean and provost catalyzed the evolution of Weill Cornell into the wonderful institution that it is today. But his accomplishments are all the more impressive when one recalls that his tenure was marked by three financial market crashes, two recessions, innumerable political meddlings in health care, the merger of Weill Cornell’s primary teaching hospital into a larger health-care system, and the tragic events of 9/11. What is it about Tony that enabled him to navigate those turbulent times with such success? Tony naturally induces people to want to help him and to do the right thing for him. He invites loyalty and excellence by being an unassuming gentleman and exemplifying high standards. He is authentic and true to his values as a scholar, a leader, a physician, and a family man. In a position of great power, he is unfailingly respectful and kind to others. It is a truism that either autocratic or avuncular leaders can succeed if they are consistent, because those around them adapt. But Tony’s kind of leadership is by far the more admirable. H. Dirk Sostman, MD Executive Vice Dean, Weill Cornell Executive Vice President and CMO, The Methodist Hospital System D r. Gotto’s commitment and dedication to Weill Cornell will last many lifetimes. He was instrumental in my appointment as dean for student affairs and equal opportunity programs and, at the same time, was an important figure in ensuring that the Medical College remain diverse. From the moment he mentioned diversity at my interview—with pride in his eyes—I knew that he was special and that he felt Weill Cornell was special as well. I was always supported in initiatives that my office undertook to ensure that students were considered across every committee that would help shape the college. Carlyle Miller, MD ’75 Associate Dean for Student Affairs and Equal Opportunity Programs Assistant Professor of Medicine • SPECIAL ISSUE 2011 29 30-33WCMspecial11researchbld_WCM redesign 11_08 12/12/11 3:15 PM Page 30 Discovery Center At a festive ceremony, Weill Cornell dedicates the Belfer Research Building Namesake: Robert Belfer speaks at the dedication ceremony as Congresswoman Carolyn Maloney (on the dais) and his family (seen on the video monitor) look on. Right: The construction site after the unveiling of a banner with the building’s official name. 30 WEILL CORNELL MEDICINE 30-33WCMspecial11researchbld_WCM redesign 11_08 12/12/11 3:15 PM Page 31 By Beth Saulnier Photographs by John Abbott O n a surprisingly warm and sunny day in early November, several hundred guests gathered in a tent decorated with festive red banners. The dignitaries, donors, faculty, staff, and students had come to East 69th Street to celebrate the latest milestone in the $650 million project: the recognition of Robert and Renée Belfer’s $100 million gift and the dedication of the research building that will bear their family’s name. For more photos of the dedication see Notebook, which begins on page 40. “The new medical research building will not only double the amount of research space available [at Weill Cornell],” Robert Belfer said in his remarks. “More importantly, as a state-of-the-art medical research facility, it will house the newest cutting-edge equipment needed to fully utilize breakthroughs in medical technology. We can now see more, see more deeply, and focus and analyze data on a scale that boggles the mind. Coupled with the brilliant scientists already on staff and with additional ones being recruited, the building is certain to house discoveries that will benefit my family, New Yorkers, and all mankind.” Under construction since spring 2010, the Belfer Research Building is the centerpiece of Weill Cornell’s $1.3 billion Discoveries that Make a Difference Campaign and its Research Leads to Cures Initiative. At the dedication, campaign chair Robert Appel noted that Discoveries is nearing the finish line, with more than $1.1 billion raised thus far. “When we launched our campaign five years ago with a goal of $1.3 billion, we thought that might be a little farreaching, particularly in the beginning of a recession,” said Appel, vice chair of the Board of Overseers. “But we knew that if we were successful we would make a major transformation in this institution, and more importantly bring about some major breakthroughs in medical science. Well, the dream has become a reality.” Located on the north side of East 69th Street between First and York avenues, the 480,000-square-foot building will rise eighteen stories and include such features as an indoor terrace, an airy twostory lobby, and an innovative double-paned glass curtain wall. The building, which will have thirteen floors of research laboratories, is scheduled to open in spring 2014. “It will be one of the hallmarks of the twenty-first century for this medical college,” Dean Antonio Gotto said at the ceremony. “This will be home to thirty new researchers who will carry out discoveries that we hope will lead to new and improved ways of diagnosing, treating, and curing disease. These new researchers will work with the clinicians in the hospital SPECIAL ISSUE 2011 31 30-33WCMspecial11researchbld_WCM redesign 11_08 12/12/11 3:15 PM Page 32 Master of ceremonies: The event was also an opportunity to honor outgoing Dean Antonio Gotto, who announced the building’s name as Sanford Weill and Robert Belfer observed. across the street; they will be mentors and tutors to our medical students, fellows, and residents. So they’ll have a big impact on this campus over the succeeding generations.” In addition to marking the building’s dedication, the ceremony served as an opportunity to honor Gotto, who steps down from the deanship at the end of 2011 after fifteen years of service. “Somehow or other we got lucky, and Tony decided to come up here from Houston and from the chair of medicine at Baylor,” foremost benefactor and Board of Overseers chairman Sanford Weill said in his remarks, “and we’ve had one heck of a fifteen years.” He went on to laud Gotto—who will remain on the Weill Cornell faculty, be cochair of the Board of Overseers, and serve as a Cornell University vice president—for his many accomplishments. They include supporting three successful campaigns raising a combined total of well over $2 billion, attracting top students and faculty, and establishing medical education programs in Qatar and Tanzania. Said Weill: “Tony has taken this school from being something just on 68th Street to really an international institution.” T he Discoveries campaign aims to support bench-to-bedside research in seven areas: cancer; cardiovascular disease; children’s health; global health and infectious diseases; neurosciences; obesity, diabetes, and metabolic disorders; and stem cell, developmental biology, reproductive, and regenerative medicine. The new building is designed to foster collaborations, and many floors will be connected by open staircases to encourage interdisciplinary research. The building will also house core facilities in such areas as high-throughput cell screening, genomics, and imaging technology, as well as a tissue bank. “While planning for this building has been years in the making, much of the construction has taken place since my peers and I arrived on campus a mere three years ago,” noted student overseer Jeffrey Russ, an MD-PhD student and the event’s opening speaker. “And just as hundreds of Weill Cornell medical students have poured so much effort into their education to realize their potential as future physicians and scientists, so Weill Cornell has poured so 32 WEILL CORNELL MEDICINE many resources and so much dedication into this building in order to realize our potential as a world-class research institution.” The Belfer Research Building is designed to reflect the way science is conducted today: rather than having fixed, individual labs, it will feature adaptable spaces with workbenches that can be easily uncoupled from utilities and relocated as scientists move around or priorities change. The facility is intended to foster “productive collisions” among researchers from different fields—a concept that underpins the building’s design, from the café in the lobby to the break rooms on each floor to the terrace out back. Such spaces are intended not only to coax the building’s occupants out of their labs but also to draw faculty and students from elsewhere on campus and beyond. “The building is merely a vessel,” Starr Foundation president Florence Davis said at the dedication, standing in for benefactor and overseer Maurice Greenberg, who was unable to attend. “It’s a beautiful and functional building, to be sure. But what we’re really excited about are the people who will fill the building to do the sort of cutting-edge research and collaborative translational research that has made this one of the most exciting parts of the world to be in.” The new building will feature design touches rarely seen in academic research facilities, such as a limestone lobby, workbenches made of American cherry, and an urban garden with plantings, seating, and fountains. Like the nearby Weill Greenberg Center, its curtain wall will be made of “water white” glass (whose low iron content keeps it from having a greenish hue) covered in a white ceramic coating known as a frit. The building has many environmentally friendly features—from incorporating locally sourced materials to collecting rainwater for irrigation to offering bicycle storage on site—making it eligible for Leadership in Energy and Environmental Design (LEED) certification at the silver or gold level. While the building will be primarily devoted to research, it will also enhance Weill Cornell’s educational mission, with several areas of student space such as lounges and seminar rooms—and since clinical research will also be conducted there, it will further the clinical mission as well. “This state-of-the-art facility will help to speed the rate at which discoveries may be translated into advanced treatments to help people in New York, across the country, and across the globe,” President David Skorton, MD, said at the dedication, calling the project “a crucial milestone in the growth and development of this college of medicine, and also a milestone for Cornell University as a whole.” The ceremony also featured remarks from New York Congresswoman Carolyn Maloney, who called the building “a powerful catalyst for scientific discoveries that address some of today’s biggest health challenges” and touted its benefits to the city and state. “We are already one of the leading research centers in our country,” she said. “It will help us cement that standing and build on it. I believe we will be the research, high-tech, medical science center not only for our country, but for the world.” A graduate of Columbia College and Harvard Law School, Robert Belfer is the former chairman of Belco Petroleum Corporation, a company that later merged with InterNorth, Inc. In 1992, Belfer founded Belco Oil & Gas Corporation; he is currently chairman of Belfer 30-33WCMspecial11researchbld_WCM redesign 11_08 12/12/11 3:16 PM Page 33 Management, LLC, a private investment firm specializing in the energy, real estate, and financial services sectors. Renée Belfer, a Vassar College alumna, is an avid philanthropist whose activities include serving as a trustee of the Metropolitan Museum of Art and as a member of the NewYork Weill Cornell Council. The Robert A. and Renée E. Belfer Family Foundation supports such institutions as the Harvard Kennedy School, Lincoln Center for the Performing Arts, and the Dana-Farber Cancer Institute. The couple has three children—Rachelle, Laurence, and Elizabeth—and five grandchildren. “They’ve been involved with the Medical Center for many years, going back to Bob’s first visit to [professor of clinical medicine] Rees Pritchett as a physician,” Dean Gotto said in announcing the building’s name, “and the Belfers have supported many different aspects of our Medical College, from professorships to gene therapy.” In his remarks, Belfer recalled his first visit to the Medical College and its teaching hospital. “A little over fifty years ago, I entered Weill Cornell and NewYork-Presbyterian as a patient whose parents thought I was in mortal danger—but then again, I had very loving parents,” he said, garnering a laugh. “Happily, through the good medical skills of Dr. R. A. Rees Pritchett, I came out of this in good shape. I was fortunate enough a month or so later to meet my loving Renée, with whom I’ve celebrated fifty wonderful years of marriage. Over that period of time my family’s involvement with Weill Cornell grew and grew. My parents, my spouse, my children and their spouses, my grandchildren, and many of my nieces and nephews have all been patients of the doctors of Weill Cornell. So in many ways what I’m celebrating here is recogni- Honored guests: The audience was surrounded by bright red banners celebrating the building’s vital role in campus research. tion of a true family-doctor relationship.” After the ceremonial sealing of a time capsule, the dedication culminated in the raising of a banner at the construction site (viewed via TV screens) proclaiming the building’s name. Gotto closed the event by inviting the audience for refreshments—deftly including a light-hearted pitch to support Weill Cornell’s next major construction project. “We invite you to join us for brunch in Olin Hall gym,” he said with a smile. “And one day, at some point in the future, we will be replacing Olin Hall.” • BACK TO THE FUTURE Time capsule offers a taste of 2011 In the year 2098, a future generation of Weill Cornellians will open a container full of history. As part of the dedication for the Belfer Research Building, the Medical College created a time capsule—a metal box, roughly the size of a footlocker, containing artifacts from 2011. The capsule includes such items as common medical instruments (stethoscope, tuning fork, pulse oximeter); a can of Tab (Dean Antonio Gotto’s favorite beverage); copies of the New York Times and Wall Street Journal dated 11/9/11; lab standards like gloves and a white coat; and the Ithaca-to-New York intercampus bus schedule. The objects were chosen by a committee chaired by Helen Appel; members included Robert Belfer, Joan Weill, Anita Gotto, Graduate School Dean David Hajjar, PhD, and student overseer Jeffrey Russ. “It’s quite an eclectic accumulation of things, and some of it may not be recognized by 2098,” said Gotto, noting that the year was chosen because it will mark both the bicentennial of the founding of the Medical College and the centennial of its renaming in honor of Joan and Sanford Weill. Toward the end of the November 9 dedication ceremony, Gotto and Appel sealed the capsule with rubber mallets—and the dean pointed out that organizers had taken pains to insure that it will be accessible eighty-seven years in the future. “There have been instances where people or institutions put away sealed time capsules and then can’t find them,” he said. “But we’ll surely be able to find it, because there will be a plaque on the wall to mark where it is.” Closing time: Pages signed by dignitaries at the dedication were put into the time capsule just before it was sealed. SPECIAL ISSUE 2011 33 34-39WCMspecial11nathan_WCM redesign 11_08 12/12/11 3:16 PM Page 34 CENTERS FOR DISEASE CONTROL AND PREVENTION Persistent pathogen: Mycobacterium tuberculosis Creative Solutions 34 WEILL CORNELL MEDICINE By Sharon Tregaskis 34-39WCMspecial11nathan_WCM redesign 11_08 12/12/11 3:17 PM Page 35 I n the summer of 1959, seven years after Selman Waksman won a Nobel Prize for his discovery of streptomycin to treat tuberculosis, thirteen-year-old Carl Nathan started a summer job as an assistant animal handler in the NYU lab of pathologist Lester Grant, MD, DPhil. While Grant investigated how inflammatory signals trigger white blood cells to adhere to the endothelial cells lining blood vessels, the teenager cleaned rabbit cages and cultivated a passion for scientific inquiry. Even as he commuted to Grant’s lab in lower Manhattan, Nathan fueled his curiosity by reading biographies of such nineteenthcentury scientists as Robert Koch, who won the 1905 Nobel for revealing Mycobacterium tuberculosis as the infectious agent behind tuberculosis, and Louis Pasteur, whose food-sterilizing treatment prevents transmission of a form of the disease that once sickened those who drank raw milk from Mycobacterium bovis-infected cattle. “I was fascinated by the history of medicine,” recalls Nathan, the R. A. Rees Pritchett Professor of Microbiology and chairman of Weill Cornell’s Department of Microbiology and Immunology. “I was impressed with how these giants created the experimental structure that defines modern medicine. For them, TB was an overwhelming concern.” More than half a century later, Nathan’s lab investigates the molecular machinery of the bacterium behind the disease in search of new strategies to foil its infective power. In the last seven years, he has also begun promoting new models of collaboration among scientists, nonprofits, and pharmaceutical companies—including pilot programs with GlaxoSmithKline, Lilly, and Sanofi-Aventis—to bring drugs to market that combat neglected infectious diseases like TB. Even in the years immediately following Waksman’s streptomycin discovery, tuberculosis remained an overwhelming force both in society and in medical practice. Everyone knew someone who had been touched by the disease. Grant—just one generation older than his apprentice— had lost both his mother and the aunt who subsequently raised him to the disease; during World War II, he was excused from military service because his own bout with TB destroyed one of his knees. Yet by the time Nathan was in high school, public health experts were confident that, armed with Waksman’s new antibiotic, physicians would fast vanquish a disease that had been a cultural touchstone and Microbiologist Carl Nathan, MD, is marshalling a myriad of weapons in the ongoing battle against TB the cause of one in four deaths in the U.S. and Western Europe during the nineteenth century—including those of Frédéric Chopin, Henry David Thoreau, and Elizabeth Barrett Browning. “The final chapter of the battle against tuberculosis appears to be at hand,” Waksman declared in his 1964 memoir, The Conquest of Tuberculosis. By then Nathan was an undergraduate at Harvard, studying East Asian history. When his mother was diagnosed with cancer, he resolved to expand upon his earlier training in immunology with Grant to find a cure for the disease. He received notice of his admission to Harvard Medical School on the day she died, cementing his course. “I was incredibly impressed with the power of the immune system to protect us,” he recalls. “I wanted to bring that to bear on metastatic cancer.” Nathan would go on to earn board certification in oncology, ascend to the chairmanship of the National Cancer Institute’s Tumor Immunology Committee at age thirty-three, and then direct his focus to the mechanisms by which host defense cells like macrophages battle cancer. In the process, Nathan became increasingly discouraged by the broad destruction wrought by chemotherapy and the lack of biochemical underpinnings to inform the development of more effective, less toxic treatments. “I was frustrated with the underdeveloped state of immunology in terms of our understanding of when cells kill, how they kill, and how their power to kill is regulated,” he says. Answering those SPECIAL ISSUE 2011 35 34-39WCMspecial11nathan_WCM redesign 11_08 12/12/11 3:17 PM Page 36 ‘There are layers of problems that have led major pharmaceutical companies to retreat from antibiotic development— but meanwhile the ability of microbes to build resistance has been picking up steam.’ 36 questions demanded a shift to even more basic research. “I became fascinated by host protective cells and their seek-and-destroy ability. To train them on combating cancer, I had to understand the rules and the tools of engagement.” But cancer—especially in humans—involves complex processes. So in the mid-Seventies, Nathan took an evolutionary step back, parsing instead the settings in which our immune function evolved: defense against infectious agents. After a decade of toggling between the worlds of oncology and infectious disease, Nathan had detailed some of the fundamental pathways that regulate the ability of white blood cells like microphages to kill pathogens, such as release of interferon-gamma from antigen-stimulated lymphocytes, and the molecular machinery they deploy in the process, such as production of nitric oxide. “That,” he says, “led me to the mechanisms organisms use to protect themselves.” B y then it was 1986 and Nathan had moved from Rockefeller University to join the Weill Cornell faculty as the Stanton Griffis Distinguished Professor of Medicine. HIV—a catastrophic viral assault on the immune system— was roiling New York City hospitals. The aftershock—bacterial tuberculosis—hit just a few years later. Its resurgence owed to a perfect storm of biological, medical, and cultural realities. Scientists anticipating a speedy conquest of TB had largely abandoned research on improving dated diagnostic techniques and treatment protocols. Likewise, public health officials had let informational campaigns fall by the wayside. To make matters worse, HIV was emerging as a diabolical complement to TB: among those unfortunate enough to be infected with both, pathogenic synergy intensifies the pace and devastation of each disease. Meanwhile, due to a confluence of regulatory, legal, and economic forces, antibiotic development by pharmaceutical companies had stalled in favor of drugs to treat chronic conditions such as asthma, mental illness, and heart disease. Increasingly, strains of Mtb were developing antibiotic resistance, yet no new drugs were being released. In 1993, the World Health Organization declared a global tuberculosis epidemic—a stark contrast to Waksman’s optimistic declaration during Nathan’s youth. Today, Mtb resides in one in three people worldwide and causes another infection every second. Four people die of tuberculosis every minute—and over the course of a year, Mtb leads to 1.8 million fatalities, making it the third leading cause of premature death and the leading cause of death from a curable infection. “How WEILL CORNELL MEDICINE did we fall so far short of what Waksman thought we were about to achieve?” Nathan mused in a 2009 commentary in Cell Host & Microbe marking World TB Day (observed every year on March 24). “How much will the twenty-first century resemble the nineteenth in our relationship with TB?” Nathan credits Lee Riley, MD, then a Weill Cornell assistant professor investigating the molecular pathways that Mtb uses to infect its host, with re-igniting his interest in the disease. It was 1990, and every weekday morning Riley took his young children to the bus stop. As the family waited at the corner of First Avenue and 63rd Street, Nathan would walk by en route from Grand Central Station to the Medical College. Riley made the most of their morning pleasantries. “I casually said maybe we could put together a grant proposal to work on TB and the role of nitric oxide,” says Riley, now a professor in the Division of Infectious Disease and Vaccinology at the University of California, Berkeley, School of Public Health. “The macrophages make nitric oxide, and I had this feeling there was some relationship in how TB interacts with these macrophages and the release of nitric oxide.” Riley’s suggestion prompted a series of conversations in Nathan’s office. “Lee would drop by with his micrographs and bar graphs and show me what he was working on,” Nathan recalls. “He convinced me that TB is a fascinating disease.” Think of Mtb as the tortoise of the bacterial world—slow and steady. When it’s dividing, it reproduces at a rate of about one division per day and, once resident in a human host, can remain latent for decades—encapsulated within the macrophages meant to evict pathogens from our bodies—before sparking an active infection and resuming its geometric spread to new hosts. Once active, the disease exacts its toll at a leisurely pace, with a constellation of easily misdiagnosed symptoms including weight loss, diminished energy, poor appetite, and a productive cough. Over the course of many months, the patient wastes away. In the era preceding the Industrial Revolution, the bacterium’s handiwork was often credited to vampirism; even today, definitive diagnosis can take weeks because of the bacterium’s plodding growth in a test tube and the insensitivity of the microscopy methods used to analyze sputum samples. Humans are Mtb’s only natural host; we transfer it via aerosolized droplets of saliva propelled into the air when an infected person coughs or sneezes. While relatively rare in the United States, the disease is rampant throughout Asia, Africa, and Eastern Europe. Worldwide, it strikes disproportionately among the poor, for whom the extended and expensive treatment 34-39WCMspecial11nathan_WCM redesign 11_08 12/12/11 3:17 PM Page 37 regimen—a cocktail of complementary drugs that must be taken for six to twenty-four months—can be impossible to sustain. Incomplete or inconsistent treatment only bolsters Mtb’s virulence, speeding the evolution of drugresistant strains and increasing the imperative for new antibiotics. By 1990, when he and Riley started talking, Nathan had published more than seventy-five articles on the genes and molecular signals that govern the immune response. In the intervening two decades, he has deployed those insights in a quest for clues to the biochemical processes Mtb uses to set up housekeeping within the macrophages, the tactics these cells use to combat active infection, and the enzymes the bacterium uses to resist our defenses. He has also grown increasingly concerned about the economic, legal, and scientific conditions that have converged to shift pharmaceutical research and development away from antibacterial agents, and not just those used to treat neglected diseases like tuberculosis that afflict vast numbers of people in developing countries. “There are layers of problems that have led major pharmaceutical companies to retreat from antibiotic development—but meanwhile the ability of microbes to build resistance has been picking up steam,” he says, “We’ve been emptying our anti-infective medicine chest and not refilling it.” To restock the cabinet, Nathan has become convinced that scientists, policymakers, nonprofits, and pharmaceutical companies have to work collaboratively to combat infectious diseases. It can take decades to progress from the basic biochemical insights gleaned by academic scientists through the layers of clinical trials sponsored by a drug company and regulated by federal law to yield a marketable drug that produces returns high enough to satisfy stockholders. It is not patent law itself but the application of patent protection that shapes the incentives that reward progress. To speed the development of new weapons against TB, Nathan advocates a more integrated approach that commends not only an optional alternative incentive system, but also new relationships between academics and pharmaceutical companies, as well as changes to the FDA’s clinical trial regulations. He promotes the creation of public-private partnerships and open-access sectors within pharmaceutical companies to facilitate the development of treatments with high social value but low commercial appeal. Nature published his first thoughts on the topic in 2004. In 2007, his commentary “Aligning Pharmaceutical Innovation with Medical Need” appeared in Nature Medicine, and in 2009, Cell Host & Microbe published his analysis of the par- JOHN ABBOTT Carl Nathan, MD SPECIAL ISSUE 2011 37 34-39WCMspecial11nathan_WCM redesign 11_08 12/12/11 3:17 PM Page 38 ticular challenges TB poses for pharmaceutical companies. In May 2011, Nathan laid out his vision for new collaborative approaches in another commentary in Cell Host & Microbe that described the array of emerging partnerships formed to seek promising compounds in the fight against pathogens, while urging readers to imagine further innovations. “Campaigns to discover antiinfectives were launched only if they could forecast a return on investment comparable to what could be expected from selling a product under monopoly prices to very large numbers of affluent or well-insured people with chronic diseases who, being helped but not cured, would use it indefinitely,” he writes in the article’s con- clusion. “It is no surprise that anti-infective drug discovery nearly came to a halt. Given that a prolonged halt will prove catastrophic, every aspect of this depiction needs to be rethought.” Nathan doesn’t just call for change from the bully pulpit of peer-reviewed journals—he’s been actively involved in multiple pilot programs launched by firms that share his concerns. “Pharmaceutical companies,” he says, “are using this neglected disease as the point of the spear to experiment with new ways of working with academics, other pharmaceutical companies, and the nonprofit sector.” Under a grant from the Bill & Melinda Gates Foundation, Nathan has partnered with GlaxoSmithKline’s Open Laboratory at Tres Cantos, Spain, a research and ABBOTT Sabine Ehrt, PhD 38 WEILL CORNELL MEDICINE 34-39WCMspecial11nathan_WCM redesign 11_08 12/12/11 3:17 PM Page 39 development campus that hosts visiting researchers from academia and biotech startups. The visitors work on their own projects with a team of GSK researchers and have access to GSK’s compound collection, a library of 700 patents, and the drug discovery know-how of the team. The only condition: any resulting commercialization must be on an affordable basis in the least developed and lowest-income countries. “TB drug discovery is at a crossroads,” says Nick Cammack, a senior vice president and head of GSK’s Medicines Development Campus for Diseases of the Developing World. “It needs new approaches to find the drugs we need. The field accepted that the old ways of doing things were just not bringing us exciting molecules; Carl is one of the first to try new approaches to find those molecules.” In addition to his research collaboration with the Open Lab—he has a postdoc assigned to the Tres Cantos campus—Nathan serves on the project’s board of governors, which reviews applications from scientists proposing research at Tres Cantos. He holds a similar post as a member of the scientific advisory committee for the nonprofit ventures launched by Lilly and was a member of the expert review group on TB research priorities for the World Health Organization’s Stop TB Partnership. “As a citizen, a parent, and a physician and scientist, I became concerned that this was a huge problem and felt a responsibility to solving at least the scientific issues,” he says. “I started thinking about how we can influence the outcome of the battle between organisms and host defense in ways that illustrate new approaches to finding anti-infectives. Along the way, I’ve become fascinated by the disconnect between academia and industry, and how walls of secrecy interfere with the communication of ideas, lead to redundancy, and slow industry from trying things that might help them overcome the roadblocks to discovery.” M icrobial geneticist Sabine Ehrt, PhD, was a postdoctoral fellow in Riley’s lab at Weill Cornell in the mid-Nineties and worked with him and Nathan to isolate a novel antioxidant gene from Mtb. On the Weill Cornell faculty since 1999, Ehrt has continued collaborating with Nathan, co-authoring more than a dozen papers on the metabolic processes that sustain Mtb. Currently, the two have a five-year grant from the NIH to investigate how intrabacterial pH influences Mtb’s persistence in the macrophages. With her additional collaborator Dirk Schnappinger, PhD, she has funding from the Bill & Melinda Gates Foundation to collaborate with pharmaceutical companies in the search for new TB drugs. “Dr. Nathan sets an example that collaborations between academia and industry can be productive and fruitful,” she says. Nathan also encourages the synergies that can emerge when academics come together. His team meets weekly with those of Ehrt, Schnappinger, and fellow Weill Cornell TB investigator Kyu Rhee, MD, PhD, as well as biochemist Aihao Ding, PhD, to form a forty-member consortium comprising specialists in immunology, microbiology, genetics, metabolomics, and biochemistry, among other fields. “A collaborative project is one thing, but joint lab meetings really propel the work forward,” says Ehrt. “Often you are stuck in your own little world and the more you’re willing to step out of it, the more fun and productive research becomes. Dr. Nathan is not shy about suggesting ideas and coming up with experiments that might be high risk, but he proposes solutions, has very broad knowledge, and knows the literature. He’s not restricted to tuberculosis or nitric oxide, and he applies that broad knowledge to his own research and to our group meetings.” With funding from a second Bill & Melinda Gates Foundation grant, Nathan’s lab is screening a library of tens of thousands of compounds supplied by a combination of academic and industrial collaborators, including GlaxoSmithKline, Sanofi-Aventis, Lilly, Beijing University, the Broad Institute, the University of Kansas, Boston University, and the Lankenau Institute. Instead of providing the ideal conditions to promote TB’s growth in a test tube, they’ve used insights from research by Nathan, Ehrt, Schnappinger, and others to create conditions that mimic the hostile environment of the human immune system. “It isn’t reasonable to target a bacterium only when it’s in the test tube under conditions where it doesn’t have a care in the world, with all the oxygen, sugar, nitrogen, vitamins, and minerals it wants,” he explains. “It’s not like that when a pathogen is competing in the body—that’s a tough place. The host is already doing quite a bit to fight the infection, and the pathogens that are most effective are the ones that can defend themselves.” Nathan says that his work offers multiple non-financial rewards. In addition to the joy he gets from solving intellectually engaging problems, his research has the potential to forge new methods for finding anti-infective compounds, generate insights into the basic biology of the competition between host and pathogen—and, most important, help the millions afflicted by TB. Ultimately, he hopes, “we should put TB on the list, with smallpox and polio, of diseases that can be eradicated by modern medicine.” ‘It isn’t reasonable to target a bacterium only when it’s in the test tube under conditions where it doesn’t have a care in the world, with all the oxygen, sugar, nitrogen, vitamins, and minerals it wants.’ • SPECIAL ISSUE 2011 39 40-47WCMspecial11notebook_WCM redesign 11_08 12/12/11 3:17 PM Page 40 Notebook News of Medical College and Graduate School Alumni PROVIDED Michael Alexiades, MD ’83 40 Dear fellow alumni: As the summer of 2011 drew to a close, the weather vacillated between extreme heat and torrential rain—but even a hurricane could not prevent your Alumni Association from welcoming the Class of 2015 at the White Coat Ceremony on August 23. All entering students were presented with coats and stethoscopes, generously provided by the Buster Foundation and several alumni donors. This annual event marks a rite of passage for the incoming medical students, whose interests, accomplishments, and talents will contribute significantly to the Weill Cornell community. We have also received word from many of our newest alumni about their adventures in the medical world. Their days have been punctuated by hard work and long hours in their internships and residencies, demonstrating their commitment to medicine. The Alumni Association has planned some new and innovative ways to keep our newest graduates engaged as they progress through their training. This year is a time of transition for the Medical College. As I’m sure you know, Laurie Glimcher, MD, has been appointed the new Stephen and Suzanne Weiss Dean of Weill Cornell Medical College and Provost for Medical Affairs at Cornell University. The search committee evaluated more than fifty excellent candidates before choosing Dr. Glimcher, the Irene Heinz Given Professor of Immunology at the Harvard School of Public Health and professor of medicine at Harvard Medical School. The Alumni Association is delighted to welcome her to the Cornell family, and we look forward to working with her in supporting the mission of the Medical College. We thank outgoing Dean Antonio Gotto, MD, wholeheartedly for his guidance, enthusiastic engagement of our alumni, and steadfast support of the Alumni Association. His fifteen years in office have ensured that Weill Cornell is able to compete with the finest institutions in the world. He will remain active as a vice president of Cornell University and co-chair of the Weill Cornell Board of Overseers. This fall was busy as we traveled to Boston, Houston, and Denver, visiting alumni and friends. These events are a wonderful chance to reconnect with fellow alumni and discuss all things Weill Cornell. Looking ahead, we are planning another regional event in San Francisco in early February and will keep you updated as the date and venue are established. Furthermore, planning for Reunion 2012 (October 19 and 20) is well under way. It promises to be a wonderful weekend filled with celebrations and stimulating lectures. I look forward to seeing the extended Weill Cornell family get together next fall. Finally, I would like to thank you, the alumni of Weill Cornell, for your constant support of the institution and its students. In particular, your generous support of scholarships has made a medical career possible for many students who otherwise could not afford it. Best and warmest wishes, Michael Alexiades, MD ’83 President, WCMC Alumni Association alexiadesm@hss.edu WEILL CORNELL MEDICINE 40-47WCMspecial11notebook_WCM redesign 11_08 12/12/11 3:17 PM Page 41 1940s Emanuel Wolinsky ’38, MD ’41: “I’m almost 94 and retired from Metro Health Hospital and Case Western Reserve Medical School in Cleveland, where I spent 44 years in infectious diseases. My wife, Marjorie, and I would love to hear from anyone in the Class of ’41.” Francis Greenspan ’40, MD ’43: “I finally retired after 60 years of teaching clinical research and clinical practice of thyroidology. It was great. I’ve moved into an excellent retirement center with my wife, Bonnie (married 65 years), and am very happy.” Herbert I. McCoy, MD ’45: “I’m hanging in there at 90-plus and engaged to be trip doctor for a scuba group in Fiji and the Solomon Islands next April.” Bob Frankenfeld ’45, MD ’47: “I finally retired two years ago after practicing internal medicine in Long Beach, CA, for 53 years. I was associate clinical professor of medicine at both UCLA and UC Irvine. Four of us attended our 60th Reunion in 2008: Ernie Gosline ’45, MD ’47, with wife Whit; Nelson Niles, MD ’47, with wife Sofie; Carol Brach Hyman ’44, MD ’47; and me. We were the oldest class there.” Ernest Gosline ’45, MD ’47: “The field of psychiatry still holds my attention, but health may soon force full retirement. I recently published a rather bold paper called ‘Algorithm of the Mind’ based on various psychoanalytic schools of theory. I stay in contact with Bob Harwick ’45, MD ’47, Bob Frankenfeld ’45, MD ’47, and John Clements ’45, MD ’47. The ‘Greatest Generation’ sails onward, but in a leaky ship.” Ludwig G. Laufer, MD ’48: “I retired from the practice of psychiatry, after 55 years, in November 2008 and now spend most of every day outside working around our property that is on a cliff on Long Island. On a clear day I can see downtown New Haven, CT. Lots of medical problems under control. My wife, Patricia, and I love the location—no street lights and deer on the property.” Rees Pritchett, MD ’48: “I gave up patient care in June 2010, but remain on the Medical College’s full-time staff. I do development work and serve on several committees.” For posterity: Rees Pritchett, MD ’48, the Louis and Gertrude Feil Professor of Clinical Medicine, signs a banner to be sealed in the time capsule at the dedication ceremony for the Belfer Research Building. JOHN ABBOTT Edmund T. Welch, MD ’49: “Not much has changed since my last note. I just passed my 86th birthday and am getting along well with a cardiac pacemaker. My life now is much more sedentary, with no more tennis. I still correspond by e-mail with Harold Evans, MD ’49, and would welcome hearing from other classmates, although our number now is greatly decreased. My e-mail address is etwjdw @ yahoo.com.” 1950s Robert C. Hafford, MD ’50: “My wife, Audrey, passed away last April.” Carol Remmer Angle, MD ’51: “I’m retired— riding horses and enjoying life in Charlottesville, VA. I live next door to my son, Fritz, an interventional radiologist at UVA.” Roy W. Menninger, MD ’51: “I’m still in private practice of psychiatry in Topeka, KS.” Anne Johnson Minkoff ’48, MD ’51: “I’m ‘aging in place’ in Great Neck, NY, with my husband of 53 years. We still enjoy visiting our Lake Winnipesaukee island spot in New Hampshire, which is now owned by our children, Ellen and Paul. And our two grandchildren (one just graduated from Pitzer College and the other will next May) are doing great. Their mother, our daughter, Ellen Pashall, is practicing psychiatry in Newton, MA. Our son, Paul, is an X-ray tech at a SPECIAL ISSUE 2011 41 40-47WCMspecial11notebook_WCM redesign 11_08 12/12/11 3:17 PM Page 42 Congratulations: Cornell President David Skorton greets Dean Antonio Gotto at the dais at the Belfer Research Building dedication. ABBOTT Queens hospital.” Patrick J. Mulrow, MD ’51: “What a wonderful life: 60 years a physician. What fond memories of those four exciting years as a medical student culminating in graduation and the diaspora. Our class pursued many different disciplines. I chose an academic career and enjoyed teaching, patient care, research, administration (20 years as chairman of medicine), and world travel lecturing and presenting papers at international conferences. When young students ask my advice, I urge them to become a physician. It’s worth the effort and expense. What a wonderful life.” Edward Swain, MD ’51: “I’ve been retired since 1999 from the private practice of psychiatry. Still physically and mentally active in my 85th year—at least on an ageappropriate level.” Robert Boyer, MD ’52: “I’m enjoying retirement, including gardening, golf, and painting. Recently had a visit from Charlie Malone, MD ’53. I also see Allan Levy, MD ’51, and Ron Allen, MD ’54, periodically. Looking forward to our 60th Reunion next year.” Robert Wagner, MD ’52: “Sue and I are still holding forth at the foot of the Bighorn Mountains in Buffalo, WY. We sure could use a visit from classmates.” Ginger Weeks, MD ’52: “I’m coping with the Golden Age problems: AF, lymphedema, venous stasis ulcers, mild CHF, hypertension, hyperuricemia, and having been overweight. In the last three months I’ve lost 40 pounds with diuresis (oral) and dietary control. All my clothes have had to be altered. I’m working six hours a week in 42 WEILL CORNELL MEDICINE addiction outpatient clinics and enjoying my friends, grandchildren, and bridge.” Richard H. James, MD ’53: “Ginny and I are fine for 84 and 85 years. Golf and tennis are going OK. We have four children, nine grandchildren, and two great-grandchildren. Still living in Keene, NH, in our own house.” Peter R. Mahrer, MD ’53: “I cannot get myself to completely retire. Still doing teaching rounds at LAC/USC Medical Center and tertiary care at Kaiser Foundation Hospital in L.A.” Allen W. Mead, MD ’53: “I survived multiple neck fractures following a fall at home and am married again, to Mary Dean from McLean, VA, a 32-year employee of the CIA.” Bernard A. Yablin ’48, MD ’53: “Proto magazine has asked permission to print part of my letter on discontinuing the practice of wearing stethoscopes around the neck and placing them in the uniform pocket instead.” William H. Gordon Jr., MD ’54: “I retired after 44 years with Kaiser Permanente in Fontana and Riverside, CA; started nuclear medicine at both hospitals. I live in Upland, CA, with wife Jean. I have four children: Stephen, a federal defense lawyer; William, a broker; Valerie, a nurse at L.A. Children’s Hospital; and Michele, a cosmetologist. I’m active in the Episcopal Church and Claremont University Club.” Ken Herd, MD ’54: “Last February, while presenting a poster at a Gordon Research Conference in Ventura, CA, supporting our hypothesis that a deficiency of Gunter Blobel’s signal peptidase accounted for the primary pathology in cystic fibrosis (more aptly called mucoviscidosis), I ran into the distinguished son of one of our classmates. I had studied this disease in 1956 with the pathologist Dorothy Andersen, who first described her findings in 1938. She was also the first to describe the elevated sweat chloride levels, in 1948, later tests for which became the diagnostic hallmark clinical finding for this condition. Dorothy cautioned that elevated sweat chloride did not readily explain the pathology and urged our attention to the cellular process of protein secretion then being worked out by George Palade at the Rockefeller Institute and later clinched by Gunter Blobel’s publication of the signal peptide hypothesis in the 1970s. Then working in the general field of pediatric rheumatology, I did not become aware of the importance of the existence of hydrophobic signal peptides at the amino terminus of all secreted proteins until the late 1980s and was at once drawn back to the problems of sticky secretions in mucoviscidosis. Back to Ventura: Dr. David Erle was listed as a speaker on something to do with respiratory mucins, great big proteins secreted into the We want to hear from you! Keep in touch with your classmates. Send your news to Chris Furst: cf33@cornell.edu or by mail: Weill Cornell Medicine 401 East State Street, Suite 301 Ithaca, NY 14850 40-47WCMspecial11notebook_WCM redesign 11_08 12/12/11 3:17 PM Page 43 pulmonary passages. He was at UCSF. I recalled that our classmate with the same last name (Henry Erle ’50, MD ’54) had two sons, both MDs, one named David and one named Steven (Steven Erle, MD ’86). Indeed it was the same David Erle. We planned to meet at the Ventura GRC, but circumstances prevented his attendance. Upon return from the West Coast, I charged off to NYC hoping to have a visit with Gunter regarding our hypothesis about the role of his enzyme in the cause of cystic fibrosis, but his recent convalescence from major chest surgery prevented it, so I had dinner with Henry and Joan in their home in Bellaire Towers and looked down on the old familiar East River and NYC. What a delightful evening. If you want to recall what Henry looked like when we all studied together, Google David Erle from UCSF and you will see that the photo is an incredible likeness. Incidentally, David’s work is now getting published in PNAS. He has already given me some helpful pointers on mucins and very likely could well advise about the isolation of respiratory mucins from patients with mucoviscidosis. But first I’ve got to get some support. Wish me luck. I tried to stay retired, but no success there. Regards to all.” Ronald Arky ’51, MD ’55: “I’m active as teacher, clinician, and mentor. I completed 50 years on the Harvard faculty in June. Caring for patients is still fun and gratifying.” Reginald H. Isele, MD ’55: “I’m enjoying retirement—important activities are quite restricted due to health problems.” Joseph E. Johnston, MD ’55: “I’m retired except for three nursing homes. Traveling a lot. Enjoying life. Fifty-seven years is long enough to practice medicine. Everything is beautiful.” Artemis Pazianos-Willis, MD ’55: “I spent three weeks in July cruising the Rhine and Mosel rivers, and ended up in Paris for four days. Wonderful trip. I have been retired for more than two years now and am keeping busy. I enjoy every minute.” Cedric J. Priebe, Jr., MD ’55: “I’m still working part-time for the Dept. of Surgery at Stony Brook University Hospital, doing quality and safety work. New e-mail address: cedric.priebe @ sbumed.org.” Sidney Goldstein ’52, MD ’56: “I still have an office at Henry Ford Hospital and show fellows and residents how to examine the heart. I’m medical editor of Cardiology News and am involved with numerous clinical trials.” Robert J. Hubsmith ’52, MD ’56: “At the hospital I continue to advise for insurance on adverse determinations re: admissions, length of stay, and payments. I’ve had an active role in the Cornell Alumni Association of Northern New Jersey as treasurer since the mid-1960s. I visit with classmates and attend reunions less frequently.” Ramon R. Joseph, MD ’56, is happily retired in Sun City West, AZ. He married Karen Moran in February 2009. He has given up clinical practice and is now doing pro bono work helping senior and disabled citizens negotiate the difficulties they encounter with Social Security and Medicare. He also enjoys his three children and six grandchildren. Donald P. Goldstein, MD ’57: “I’m still working full time in gynecology at Brigham and Women’s Hospital. Gave up major surgery in 2006. Now doing mostly ambulatory surgery and consults and running the New England Trophoblastic Disease Center, which I founded in 1965. Connie is very busy as a board member of the Boston Early Music Festival, which produces Baroque operas. We continue to live in our home of 43 years in Weston, MA. Two grandsons are in college and another is getting ready to go next year.” William H. Plauth Jr., MD ’57: “I’m very happy in Santa Fe. Pretty much staying right there and enjoying gardening, tennis, dog walks, and friends—in no particular order. Would love to see my classmates.” Robert A. Levine ’54, MD ’58: “I left SUNY Upstate Medical University to join Boston Medical Center as professor of medicine, Boston University School of Medicine, in the Section of Gastroenterology. I’m working in the Liver Clinic and participating in academic activities. Barbara and I moved to Needham, MA, where we have two sons and four grandsons in the same town and are closer to my son in New York City with two granddaughters. We have a condo in Ogunquit, ME, for summer weekends and vacations. I am publishing my 105th paper, in Hepatology. I play lots of tennis and bike ride, too.” Robert G. Merin, MD ’58: “We have just moved to a continuing care community: 3500 West Chester Pike, F103, Dunwoody Village, in Newtown Square, PA 19073. So far we are enjoying it, but it’s quite a change.” Edward E. Wallach, MD ’58: “Hello, everybody. I’m still working, but at a reduced pace. Clinical responsibilities and mentoring of students, house officers, jun- ior faculty, and fellows consume a lot of time. I’m also busy with clinical research and committee work. Johns Hopkins has been a fantastic part of my professional life; since leaving Penn I’ve been here for 27 years. Joanne and I have gotten together with John Queenan, MD ’58, and also spent a day at Albert Einstein with Irwin Merkatz ’55, MD ’58. Cornell was a wonderful start to my medical life and a memorable experience.” L. Davis Arbuckle, MD ’59: “My wife, Julie, died in September 2010 after a long illness.” Bruce H. Drukker, MD ’59, and his wife, Esther, have moved from Salem, SC, to Spring Lake, MI. All is well and now they’re much closer to family and old friends. They’re also getting ready to reacquaint themselves with “big snow.” James E. Shepard, MD ’59: “It was great to see former classmates at reunion last year. It has been interesting to read and see the various advances at the Medical Center. One delightful surprise was discovering the little Italian restaurant at York and 71st that has the best linguine con vongole I have ever tasted.” 1960s Kenneth R. Barasch, MD ’60: “I’m still practicing ophthalmology in New York City. No plans to retire. The 50th Reunion was wonderful. When we all get together, it seems as though we had seen everyone the day before.” Gene Sanders ’56, MD ’60: “I’ve retired to Florida and spend time writing for a variety of non-medical journals and magazines, especially philatelic. I was recently voted outstanding alumnus of Frederick (MD) High School, bringing back a multitude of fond memories.” Carl G. Becker, MD ’61: “We are well, still sailing on Lake Michigan, and enjoying Door County, WI. Our local politics are insane, but nature is quite grand here. Best to all.” Andy Hedberg, MD ’61: “We’re looking forward to seeing our classmates at our 50th Reunion celebration in October 2012.” Bill Chaffee, MD ’62, will be back for the 50th Reunion. William R. Hazzard ’58, MD ’62: “I’m retired at last. But what does that mean? For me, so far, it’s a matter of philosophy and choice. So that means refilling my plate with things that are most likely to be fulfilling SPECIAL ISSUE 2011 43 40-47WCMspecial11notebook_WCM redesign 11_08 12/12/11 3:17 PM Page 44 in Lakewood, WA, managing the produce from the garden, and in winter enjoys a small house atop the hill overlooking Banderas Bay near Puerto Vallarta. Her 90-year-old husband, Jack, is hard at work in Washington constructing a cruising boat in a 16-foot Poulsbo hull, while in Mexico he continues to refine his selfbuilt sailing trimaran. These boats are the fourth and fifth in his series of bluewater-sailboatsconstructed-by-Jack. “We are both fortunate in being well, ambulatory, and able to travel a bit, so we are planning a trip up the west coast of Vancouver Island in the fall and a cruise on the Mekong River with University of Washington alumni next February. We recently stopped by and enjoyed a visit in La Jolla, CA, with Libby Barrett Connor, MD ’60, my Unfurled: When the name of the roommate for two years in Olin research building was announced, Hall. Best wishes to all.” a new banner was raised at the Alfred Parisi, MD ’63: “I’m construction site. consulting for Unum on cardiac disability claims and teaching ABBOTT at Miriam Hospital, Brown University.” and I would do for free (since that will generRobert S. Ennis, MD ’67: “I’m retired ally be the case). And so far it’s all going well from my orthopaedic surgery practice, and as planned: teaching and mentoring as I but I continue to teach and do part-time wish while steadfastly resisting administraconsulting. Lorelie, my wife of 47 years, tive re-engagement. Let’s touch base at our and I are active in a number of philan50th next fall for updates.” thropic organizations. There are currently Anthony Saidy, MD ’62: “In July I spoke four generations of the Ennis family livat the San Francisco Jewish Film Festival ing in Weston, FL—lots of celebrations.” after a screening of Bobby Fischer Against the John L. Marquardt, MD ’67, and his World, in which I appear. I’ve been wife, Betty, are living at the Ocean Reef wrestling with Dr. M. Angell’s articles in Club in Key Largo, FL, and enjoying the the New York Review casting grave doubts beautiful weather in South Florida. “Our on psychopharmacologic practice (see six children are all married, and we are www.nybooks.com).” expecting our fifteenth grandchild. We Thomas H. Snider, MD ’62: “I’m spendhope to see you all at the 45th Reunion ing my summers in retirement near Aspen, in 2012.” CO. I love San Antonio, but not nearly George G. Telesh ’62, MD ’67: “We’re enough when the temperature is 100 moving right along in Daytona Beach— degrees. It takes a while for my mail to make getting older and developing old age it up to Aspen, but I hope this will not deter issues, but still working full time. Keep you from sending news and mail to my San plugging.” Antonio address. I sincerely desire to mainBurton C. West, MD ’67: “Katherine tain my membership in the WCMC Alumni and I continue to enjoy our family in Association. Thanks very much, and my best Knoxville (three adult children and their to all.” families) and visits from and to the other Muriel King Taylor ’58, MD ’62, is haptwo adult children and their families in pily and completely retired, painting waterNashville and Birmingham. I’m enjoying colors and Sumi-e for fun. In summer, she’s 44 WEILL CORNELL MEDICINE seeing hospital patients about every other week, despite hassles. Aren’t contract medicine and government medicine wonderful!” Lois J. Copeland ’64, MD ’68: “I attended the Ludwig Von Mises Institute meeting in Vienna in mid-September, hoping it would reach the heights of its meeting in Spain two years ago. Important information for these difficult times in historic places.” Jeffrey S. Borer, MD ’69: With the acquisition of Long Island College Hospital, its original home in 1860, SUNY Downstate Medical Center has enlarged its health-care system and with it, the responsibilities of Dr. Borer, professor and chairman of the Dept. of Medicine and chief of the Division of Cardiovascular Medicine. He views the merger with LICH as a great opportunity, both for enhanced clinical service and heightened academic activity. Steve Shaul, MD ’69: “I’m still practicing rheumatology in Yakima, WA.” 1970s Peter W. Blumencranz, MD ’70, wrote a chapter, “Molecular Analysis of Breast Sentinel Lymph Nodes,” in Surgical Oncology Clinics of North America, and co-authored two major ACOSOG studies, Z0010 and Z0011, published in JAMA on July 27, 2011, and February 9, 2011. He is the medical director of the Comprehensive Breast Care Center of Tampa Bay. Roy Nuzzo, MD ’70: “I’m still practicing pediatric orthopaedic and reconstructive surgery at Overlook Hospital in Summit, NJ, and at St. Joseph’s Medical Center in Paterson, with emphasis on resident education and research at the latter. My daughter, Aimee, son-in-law, Rob, and two grandchildren, Lily and Michael, are living close by. We’re grateful. Jo and I are considering taking up Can-Am riding (three-wheel motorized bikes) if we don’t lose our nerve.” Steve Rosenblatt, MD ’71: “I’m in fulltime practice of nephrology and active in the transplant program in San Antonio, TX. In the summertime my wife and I enjoy hiking in Colorado. I play golf and enjoy skiing. I’d like to have more time for travel to family, touring, and just free time. I have three children: Josh lives in Rockville, MD, and is a pilot and airplane broker for business jets. He’s married to Kelley and has two children. David lives in Austin, where he works as a film editor; he and his wife, Michelle, have one child and one on the way. Lauren is a graduate engineer from Georgia Tech and works in New York City 40-47WCMspecial11notebook_WCM redesign 11_08 12/12/11 3:18 PM Page 45 as a research coordinator; she’s applying to medical school. The things I remember most are some pretty rough basketball games in the gym during exam time and the end-of-year skits.” Albert H. Mangold, MD ’73: “My daughter, Karen, just became a pediatric emergency attending at Children’s Memorial in Chicago. Jean and I became grandparents for the first time when my son, Kurt, and his wife gave us a grandson, Charlie, in March.” Stuart Mushlin, MD ’73, has been named the master clinician in the Dept. of Medicine at Brigham and Women’s Hospital. He is the second master clinician in all departments. Dr. Mushlin practices internal medicine and is director of preliminary residency for the Dept. of Medicine. Richard Tosi, MD ’73: “Based on how I used to work, one could say I was semiretired right now. I can practice like this forever, as my internal medicine/pulmonary career still holds great interest and professional enjoyment. Life is now less pressured since we have paid off the college bills for the three aliens who claim to be our children. They hit us up for Cornell once, Penn once, and Columbia twice. Contact me at agt200 @ gmail.com.” Jeffrey S. Wasser, MD ’73: “I retired from the private practice of hematology and medical oncology in 2008 and spent the next two years establishing a new cancer program at a local community hospital. In May 2011 I joined the division of hematology and medical oncology at the University of Connecticut as an assistant professor and medical director of the clinical trials office.” Roger W. Geiss, MD ’75: “I’m professor and chair of pathology at the University of Illinois College of Medicine at Peoria. For the academic year 2010–11, I received the student award for Best Instructor in the Cardiovascular Course, as well as the Faculty Outstanding Service Award.” James Newman ’71, MD ’75, a specialist in rheumatology, was named the first senior vice president and executive director of the Christiana Care Value Institute and appointed as Christiana Care’s chief academic officer. He previously served as Christiana Care’s chief medical officer and chief patient safety officer. Dr. Newman received his residency training in internal medicine at the Hospital of the University of Pennsylvania from 1975 to 1978 and completed a postdoctoral fellowship in rheumatology at Yale University Medical Center in 1980. He joined Christiana Care’s medical staff that year. His faculty appointments include lecturer in internal medicine at Yale University Medical Center, 1979–80, and clinical associate in medicine, 1984–89, at the University of Pennsylvania School of Medicine. Since 1982, he has been clinical associate professor of medicine at Jefferson Medical College. Karen Toskos Robertson, MD ’75: “I’m still working and loving it after all these years.” Jeffrey Gold ’74, MD ’78: “My daughter Steph graduated summa from NYU. I was named chair of the Liaison Committee on Medical Education for a twoyear term and re-elected to the AMA Council on Medical Education and then to the executive committee, broadly serving American medical education. I continue in my role as chancellor and executive vice president at the University of Toledo.” 1980s Carolyn Grosvenor, MD ’80: “I am still a staff physician at the Albany VA. I’m also on the faculty at the SUNY Albany School of Public Health, where I teach Social and Behavioral Aspects of Public Health. I work with a local rescue mission and am developing a health education curriculum. My husband, Wayne (we’ve been married 35 years), took early retirement and is pursuing a music career in acoustic bass with a jazz quartet.” Sharon A. Strong, MD ’81: “I love working in home hospice. My husband, Phil Bossart, MD ’81, continues at the ER at the University of Utah. Our oldest son, Chris, 24, started medical school this fall at the University of Utah. Abby, 21, has been studying in Spain for her junior semester abroad; she traveled to Portugal, Italy, Croatia, Switzerland, and Ghana, and finishes up at Occidental College in 2012. Matt, 19, finished his first year at Dartmouth.” Douglas F. Buxton, MD ’82, is clinical professor of ophthalmology at New York Medical College and president of the Jorge N. Buxton Microsurgical Education Foundation. Walter “Ted” Donnelly, MD ’82: “Life is busy in the Midwest. Our oldest son, Kevin, who would have made a brilliant engineer, is applying to medical school. Now I need to convince his mother that the Upper East Side is not rampant with muggers. Middle son Ryan is a sophomore at Ohio State in biomedical engi- neering, and daughter Erin still wants to be a vet. Karen and I celebrated our 25th anniversary last fall. Tempus fugit.” Peter H. Judson, MD ’82, and his wife, Grace Makari-Judson, MD ’82, have a son, Timothy, entering Weill Cornell in the Class of 2015. Barnaby Starr, MD ’82: “I continue to run a general pediatric practice in Baltimore. Not a day goes by that I don’t think back fondly on my Medical College experience. The clinical skills and confidence gained there are useful every day.” Mary Nolan Hall, MD ’83: “I have been promoted to deputy chief academic officer and designated institutional officer at Carolinas Healthcare System, a large regional system and a designated academic medical center with 12 academic departments and a regional branch campus for the University of North Carolina School of Medicine.” Timothy Higgins, MD ’83: “I’m still enjoying Seattle and continue to provide pediatric and adult anesthesia. Hard to believe that my two kids—Matt and Katie— are now out of college. Give me a call if you’re in town.” Maureen Tierney, MD ’83, and her husband, John Brennan, moved with their sons from Massachusetts to the D.C. area nine years ago, where Maureen worked for the FDA in the Office of Infectious Diseases and John was a Congressional lawyer specializing in railroads. John’s knowledge got him recruited for a terrific position with Union Pacific Railroad. “So here we are in the true heartland—Omaha, NE—and the boys, John, 15, and Jim, 13, are at Creighton Prep. I am doing some consulting and also becoming more involved in the support and advocacy for those with Asperger’s syndrome. Visitors most welcome.” Scott Hayworth, MD ’84: “I’m busy in my role as CEO of the Mount Kisco Medical Group. We have 270 physicians in 22 locations. Finishing my stint as chair of the American Medical Group Association and on the ACOG board. My wife, Nan Hayworth, MD ’85, is busy commuting between Washington and the district. She is enjoying the challenges of being a member of Congress. The long hours of practicing medicine have prepared her well for her new job.” Larry Robinson, MD ’84: “I completed my MBA this May—a tremendous amount of work but overall a great experience. I’ve used this degree to become the managing director for the research unit in our practice, but am also attempting to create a senior executive position of surgical services SPECIAL ISSUE 2011 45 40-47WCMspecial11notebook_WCM redesign 11_08 12/12/11 4:03 PM Page 46 life is fun and busy. Personally, Juliet and I just celebrated our 20th wedding anniversary. Andrew, 15, is looking forward to being able to drive, and Melissa, 13, enjoyed surf camp last year. Andrew loves computers and cars (and likes golf a bit), while Melissa is an amazing artist, having won several competitions. Everyone is doing well. Hope all are well. Please visit if you’re in Tampa.” Theresa Rohr-Kirchgraber, MD ’88, was named executive director of the Indiana University National Center of Excellence in Women’s Health. She is associate professor of clinical medicine and pediatrics and a faculty member in the Indiana University School of Medicine’s Division of Adolescent Medicine. Dora Weinstein, MD ’89: “My best wishes to all my friends and colleagues.” ABBOTT Celebration on 69th: Carlyle Miller, MD ’75 (center), associate dean for student affairs and equal opportunity programs, at the Belfer Research Building dedication with medical students (from left) Matthew Sheehan, Asha Jamzadeh, Kartik Kesavabhotla, Melissa Rusli, and José Villa-Uribe delivery for a new four-hospital merger. I’ll let you know how it goes.” Michelle Goldstein-Dresner ’81, MD ’85: “I’m a staff anesthesiologist at a surgery center in Boca Raton, FL. My son, Shmuel, 20, is a junior at Princeton majoring in economics and is premed (go figure). Daughter Rebecca, 19, is a sophomore, also at Princeton, majoring in molecular biology.” Subhendu “Bob” Narayan, MD ’85: “I’m still practicing gastroenterology in a twenty-person GI group in Berkeley and Walnut Creek, CA. My wife is a child psychiatrist at Kaiser. My daughter is starting her sophomore year at Occidental College in Los Angeles; my son is starting his junior year in high school. Any WCMC grads out in Northern California?” Montgomery Douglas, MD ’86: “I am associate professor and chair, Dept. of Family and Community Medicine, and associate dean for diversity and inclusion at New York Medical College in Valhalla, NY.” Matthew J. Kates, MD ’86: “I just reached 20 years in practice and am a partner in ENT and Allergy Associates, a 125doctor specialty practice. My oldest starts high school this fall. A lot has changed since we left the Medical College!” Randy Jacobs, MD ’87: “I’ve been a staff physician with Kaiser of Colorado in the St. Joseph Hospital Emergency Dept. for 16 years. We are affiliated with the Denver 46 WEILL CORNELL MEDICINE Health Emergency Medicine Residency. I enjoy the challenge of teaching residents in our busy ED. Aside from work, I’ve really gotten into the Colorado lifestyle; I mountain bike all summer and ski all winter. Right after returning to Colorado, I got married to Jill. We have three boys—Zak, Reed, and Max—who keep us very busy. If anyone from the class is ever in Colorado, give me a shout.” Karl A. Illig, MD ’88: “After 23 years at the University of Rochester, I have relocated to the University of South Florida, in Tampa, as professor of surgery and director of the Division of Vascular Surgery; my e-mail (and all are welcome to contact me there) is killig @ health. usf.com. I’ll miss Paul Rubery, MD ’88 (spine surgery in Rochester), who I operated with on a weekly basis. Professionally my career continues to be a lot of fun. I was elected to the Vascular Surgery Board of the ABS, and as Jeff Gershenwald ’84, MD ’90, is also on the Surgical Oncology Board, we have two members of our class helping to run the show. I’m editing a 120-chapter textbook on thoracic outlet syndrome and run a yearly national meeting for medical students and surgical residents interested in vascular surgery. I’m past president of the Peripheral Vascular Surgery Society and serve on several SVS committees, so 1990s Julio Lopez-Andujar, MD ’91: “I’m a primary care internist and medical director of a private geriatric multi-specialty clinic of CAC Florida Medical Centers in the great weather of South Florida, where we provide comprehensive and holistic care. I have a great wife, Amelia, and two great children, Sofia, 11, and Julio, 15. I enjoy traveling, spending time with my family, and my small private practice science lab and library of more than 3,000 books. I study every subject you can imagine, from astronomy and particle physics to sociology, literature, and economics. That broad perspective has really helped me better understand and deal with the multiple dimensions of my patients’ sense of wellbeing. I like working with a great, motivated team of staff and physicians. I remember Dr. Daniel Alonso’s sincere dedication and support for us students. I hope to hear from Alfonso Torres ’86, MD ’90, Byron Simmons, MD ’92, and Daniel Jones ’86, MD ’90. Life is great and Weill Cornell was a good starting experience.” Thomas W. Shields, MD ’96: “I’m an attending emergency department physician at Forsyth Medical Center in WinstonSalem, NC.” 2000s Katie Hisert, MD-PhD ’06: “I’m in the second year of my pulmonary and critical care medicine fellowship at the University of Washington. In February I will return to the lab full time to study the interactions between the innate immune system in the lung with bacterial pathogens.” 40-47WCMspecial11notebook_WCM redesign 11_08 12/12/11 3:18 PM Page 47 In Memoriam ’41, ’44 MD—Morton A. Beer of Morristown, NJ, August 12, 2011; ob/gyn; chairman, Dept. of Ob/Gyn, Morristown Memorial Hospital; clinical assistant professor of ob/gyn, Robert Wood Johnson Medical School; veteran; active in civic, community, and professional affairs. ’46 MD—Thomas C. Hill of Salisbury, MD, June 4, 2011; practiced internal medicine; chief of staff, Peninsula Regional Medical Center; veteran; worked on medical research that led to the safe use of pilot ejection seats; active in community, professional, and religious affairs. ’48, ’50 MD—Leon I. Charash of Plainview, NY, September 14, 2011; pediatric neurologist; associate clinical professor of pediatrics, Weill Cornell Medical College; consultant in child neurology; veteran; chairman, medical advisory committee, Muscular Dystrophy Association; founded a cerebral palsy center in São Paulo, Brazil; appeared yearly on the Jerry Lewis Labor Day Telethon; veteran; active in professional and alumni affairs. ’44, ’50 MD—Robert H. Dickson of La Crescenta, CA, September 10, 2011; general family practitioner; physician at the maximum security Tehachapi State Prison; veteran; active in community and professional affairs. Phi Delta Theta. ’50 MD—Heinz F. Eichenwald of Dallas, TX, September 8, 2011; expert in pediatric infectious diseases; professor emeritus and department chairman, UT Southwestern; chief of staff, Children’s Medical Center Dallas; chief of pediatrics, Parkland Memorial Hospital; helped improve pediatric hospitals in Chile, Colombia, Haiti, and Vietnam; active in professional affairs. ’51 MD—Lyle R. Smith of Kingsport, TN, September 3, 2011; president of medical staff and executive committee member, Holston Valley Medical Center; taught medieval English history at East Tennessee State University’s Kingsport Allandale Center for Continuing Education; held a degree in theology from the University of the South; veteran; active in community, professional, and religious affairs. ’47, ’51 MD—James O. Wynn Jr. of Carrboro, NC, February 10, 2011; chief, Division of Endocrinology, University of Arkansas Medical Center; taught at Duke University Medical Center; in private practice in Durham, NC; chairman, Dept. of Medicine, Durham Regional Hospital. Sigma Phi. Wife, Patricia Stroup Wynn ’50. ’52 MD—Leston L. Havens of Cambridge, MA, July 29, 2011; professor emeritus of psychiatry, Harvard Medical School; principal psychiatrist and co-director of education, the Cambridge Hospital; author; editor; active in professional affairs. ’52 MD—Russell S. Hoxsie of Wilbraham, MA, July 30, 2011; private family physician; medical director, Martha’s Vineyard Hospital’s Windemere long-term health delivery services; medical examiner; emergency room physician; set up the first cardiac care unit on Martha’s Vineyard; pioneer in the diagnosis and treatment of Lyme disease; author; newspaper columnist; active in community and professional affairs. ’52 MD—Herbert S. Sacks of New Haven, CT, August 30, 2011; clinical professor of child and adolescent psychiatry, Yale School of Medicine; international medical consultant; past president, American Psychiatric Association; volunteer faculty member, Child Study Center; proponent of confidentiality of medical records; campaigned for group insurance coverage for outpatient psychiatric treatment and mental health parity in insurance coverage; supported the “Goldwater Rule,” barring psychiatrists from offering professional opinions about anyone they have not personally examined; author, Hurdles: The Admissions Dilemma in American Higher Education; veteran; active in civic, community, professional, and alumni affairs. ’53 MD—Kenneth C. Archibald of San Francisco, CA, August 24, 2011; specialist in rehabilitation, California Pacific Medical Center; professor, UCSF Medical Center and Temple University; helped create the Archibald/ Ehrenberg Rehabilitation Terrain Park; veteran; ski patrol member. ’49, ’53 MD—Catherine Friedrich Root of Brainard, NY, June 27, 2011. Delta Gamma. Husband, Harlan D. Root ’50, MD ’53. ’57 MD—Helen Carter Abel of Elizabeth, NJ, June 25, 2011; gynecologist; active in community affairs. Husband, Robert R. Abel, MD ’56. ’55, ’59 MD—G. Billie Lerner of Washington, PA, August 4, 2011; first woman to be chief resident at the Veterans Hospital in New York City. Husband, William C. Lerner ’55. ’60 MD—James W. Innes of Stamford, CT, formerly of Greenwich, CT, August 29, 2011; practiced gastroenterology and internal medicine; taught interns and residents at Greenwich Hospital and Yale New Haven; veteran; active in civic, community, and professional affairs. ’64 MD—John B. Morrison of Dix Hills, NY, September 19, 2011; co-chief, Division of Cardiology, North Shore University Hospital; associate professor of medicine, Weill Cornell and NYU; served on four NIH study sections; veteran; author; active in professional affairs. ’65 MD—Robert P. LaFiandra of Middlebury, VT, September 3, 2011; physician; served in the Public Health Service in Chile; master gardener; active in community affairs. SPECIAL ISSUE 2011 47 48-48WCMspecial11postdoc_WCM 12/12/11 3:18 PM Page 48 Post Doc Get Moving Weill Cornell student group teaches disadvantaged kids the pleasures of exercise and good nutrition I nner-city kids face a host of hurdles in adopting a healthy lifestyle. There’s the ubiquity of fast-food outlets; the dearth of markets selling fresh fruits and vegetables at affordable prices; the lack of safe, open spaces to play. Those and other factors are fueling what Maura Frank, MD ’88, calls a crisis in childhood obesity. “We know that obesity is likely to continue into adolescence and adulthood unless there are interventions,” says Frank, an assistant professor of pediatrics and the director of pediatric ambulatory care at Weill Cornell. “Because of its severe effects, this may be the first generation of children who live shorter lives than their parents.” Frank is a faculty adviser to one such intervention: MAChO, a Weill Cornell student group that aims to instill healthy habits in kids from disadvantaged neighborhoods. Founded in 2009 by Ghanaian-born medical student Nii Koney ’12, the group—whose acronym stands for Motivating Action through Community Health Outreach—offers year-long programs for kids aged eight through thirteen. “Younger kids may not know things that are second nature to us, like calories or what lean meat is,” says Diana Mosquera ’14, a Colombia native whose Spanish fluency has been handy in communicating with immigrant parents. “What I find gratifying is knowing that I’m helping kids learn these things early on. And it’s fun spending time with them—they’re really adorable.” Each session begins with the “MAChO Super Set”: a fast-paced series of jumping jacks, push-ups, crunches, and other calisthenics. Then there are lessons in healthy cooking—from veggie-topped mini-pizzas to whole-wheat pasta with broccoli and pesto—as well as ample chances to run and play. Sometimes, the kids take field trips to places like an Upstate New York farm, an urban greenmarket, the Sony Wonder Technology Lab, or the Tribeca Film Festival. The program’s message is positive: the pleasures of healthy living can rival the temptations of junk food and video games. “We don’t say, ‘You must never eat candy,’ ” Koney says. “It’s, ‘If you’re going to have candy, eat it in moderation; check the nutrition label, know how much you’re taking in and what that means for your body.’ We don’t say, ‘Never go to McDonald’s’; instead, it’s, ‘When you go to McDonalds, you don’t have to have the hamburger— choose the salad.’ We try to empower them to make good choices.” Originally, the group—first named Movement Against Childhood Obesity—recruited kids who were already overweight or obese, with BMIs above the 90th percentile. “But we moved away 48 WEILL CORNELL MEDICINE PROVIDED BY NII KONEY Physical fitness: At MAChO, children participate in activities like yoga to encourage healthy living. from that,” Koney says, “to keep the program from being stigmatized as the ‘fat-kids’ camp.’ ” Besides, he says, “Our vision is to have our participants help change things at home, in their schools, and in their communities—and any kid can do that.” Koney notes that MAChO is a true community effort, with backing from a veritable village of supporters. It was started with the help of Warria Esmond ’80, MD ’84, medical director of East Harlem’s Settlement Health, a key venue for participant recruitment; it has been funded by such sources as the Weill Cornell Alumni Association, the Student National Medical Association, and the Aetna Foundation; student volunteers have come not only from Weill Cornell but also Hunter College, Columbia, NYU, and Cornell University’s urban semester program; and it is currently expanding through partnership with the Boys Clubs of New York. And, says Koney, they hope to eventually expand to other medical schools. Involving parents is also essential to the program’s success, Frank stresses. “You can see tremendous change if you affect even small pieces of behavior—for example, decreasing the sugary beverages that children consume—but you have to get the whole family on board, or it’s tough to make it work,” she says. “Younger kids are still growing—so if you can slow the weight gain, you’ve pretty much solved the problem.” — Beth Saulnier c3-c3WCMspecial11_WCM redesign 11_08 12/12/11 4:02 PM Page c3 c4-c4WCMspecial11_WCM redesign 11_08 12/12/11 3:25 PM Page c4 Weill Cornell Medical College and Weill Cornell Graduate School of Medical Sciences 1300 York Avenue, Box 144 New York, NY 10065 PRSRT STD US Postage PAID Permit 302 Burl., VT. 05401