1 STIMULATION IN SELECTED PATIENTS WITH GILLES DE LA TOURETTE SYNDROME
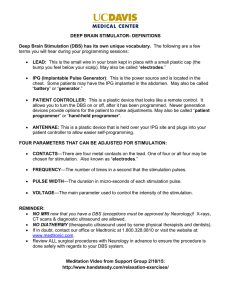
advertisement

1 1. TITLE PAGE 1.1. Title : DOUBLE BLIND ASSESSMENT OF PALLIDAL DEEP BRAIN STIMULATION IN SELECTED PATIENTS WITH GILLES DE LA TOURETTE SYNDROME Short title: Pallidal Stimulation for Gilles de la Tourette Syndrome 1.2 Investigators Dr Hugh Rickards Dr Hardev Pall Professor Marwan Hariz Mrs. Rosalind Mitchell Dr Patricia Limousin Professor Marjan Jahanshahi Professor Eileen Joyce Professor Mary Robertson Dr Ian Mitchell Mr Ludvic Zrinzo 1.3 Protocol details Version 9 February 2008 2 2. CONTENTS PAGE 1.1. Title : 1.2 Investigators 1.3 Protocol details 2. CONTENTS PAGE 3. LIST OF ABBREVIATIONS AND DEFINITIONS 4. SUMMARY 5. BACKGROUND 6. TRIAL OBJECTIVE AND PURPOSE 7. STUDY DESIGN 8. SUBJECT SELECTION 9. SUBJECT RECRUITMENT 10. TRIAL INTERVENTIONS 10.1 General information 10.2 Use within the trial 11. RANDOMISATION 12. BLINDING & OTHER MEASURES TAKEN TO AVOID BIAS. 13. DATA 13.1 Data to be collected 13.2 Data handling and record keeping 14. STATISTICAL CONSIDERATION 15. COMPLIANCE AND WITHDRAWAL 15.1 Subject compliance 15.2 Withdrawal / drop our of subject 16. INTERIM ANALYSIS AND DATA MONITORING 17. ETHICAL CONSIDERATIONS 18. FINANCING AND INSURANCE 19. REPORTING AND DISSEMINATION REFERENCES APPENDIX 3 3. LIST OF ABBREVIATIONS AND DEFINITIONS DBS GTS MRI YGTSS GPi YBOCS TS-QoL Deep brain stimulation Gilles de la Tourette syndrome Magnetic Resonance Imaging Yale Global Tics Severity Scale Globus pallidus internum Yale Brown Obsessive Compulsive Scale Tourette Syndrome Quality of Life Scale LFP EEG NART WASI CVLT RMF Local field potential Electro-encephalogram National Adult Reading Test Wechsler Adult Scale for Intelligence California Verbal Learning Test Recognition Memory for Faces 4 4. SUMMARY Aims and rationale To investigate whether deep brain stimulation (DBS) of the globus pallidus internum (GPi) can alleviate tics in Gilles de la Tourette syndrome (GTS) and whether this treatment has any influence on social, psychological and behavioral disability and quality of life. The rationale is that GPi DBS is efficient in alleviating other movement disorders such as dystonia and dyskinesias, and there are few well documented case reports in Tourette syndrome showing promising results. Interventions/measures Up to 20 participants will be recruited into this study. They will be recruited from the Tourette Clinic at The National Hospital for Neurology and Neurosurgery at Queen Square, London and the Tourette syndrome clinic at the Queen Elizabeth Psychiatric Hospital in Birmingham. The study will include a 6 months period with doubleblinded assessments with stimulation on vs. off in a cross-over design. Primary and secondary objectives The primary objective is to study the effect of DBS in the GPi on the frequency and severity of Tics assessed with validated scales. Secondary objectives are to evaluate the impact of DBS on neuropsychiatric and cognitive parameters and quality of life. Brief description of methods Patients will undergo tests using validated scales prior to surgery. Surgery will be performed in a similar fashion to that for dystonia, a routine indication in the 2 participating sites. Stereotactic implantation of DBS electrodes in the GPi is performed under general anesthesia. Programming of stimulation will be optimized by clinicians over the first 6 weeks. Patients will be randomly assigned to either ON or OFF stimulation for the next 3 month period. Blinded assessment will be conducted at the end of this period followed by a crossover in the stimulation condition in each patient for an additional 3 months. After final blinded assessment, patients will be offered the opportunity of participating in an “open label" extension study. 5 5. BACKGROUND Gilles de la Tourette’s syndrome (GTS) is a chronic disabling disorder characterized by multiple motor and vocal/phonic tics. Co-morbid symptoms and disorders are common including Obsessive-compulsive disorder, attention deficit hyperactivity disorder and depression. When severe, GTS may cause considerable social impairment. A substantial proportion of patients with GTS improve markedly when they reach adulthood, but the prevalence, and potentially disabling nature, of adult GTS is probably under recognized. There is good evidence to indicate a significant genetic component although the underlying gene(s) remain unknown. Treatment is directed towards symptom relief and relies largely on the pharmacological modification of the dopaminergic system. Standard treatments include behaviour therapies and a variety of neurotransmitter modulators which, in the majority of patients, are successful in bringing about an improvement of symptoms. However, a number of patients fail to respond and continue to suffer. Additionally, pharmacological treatment of tics may come at the price of marked side effects and is not always helpful (Leckman, 2002; Robertson, 2000). Alternative treatments for tics need to be explored, particularly in those who are severely affected, resistant to conventional treatments and suffering a markedly reduced quality of life. Deep brain stimulation has proven a valuable, and safe, additional treatment in patients with other movement disorders such as Parkinson’s disease or dystonia. Several case reports suggest that DBS may be helpful in severe GTS. Thus there is a need for a systematic evaluation of this treatment in GTS. In the past, neurosurgical procedures for GTS have been used including limbic leucotomy, frontal lobotomy, anterior cingulotomy, thalamic and infrathalamic lesions (for review see Temel and Visser-Vandewalle, 2004). However, the results have often been unsatisfactory partly due to side effects caused by the lesioning procedure. At the National Hospital for Neurology and Neurosurgery, limbic leucotomy has been used in two patients with success but less for the movements and more for the associated self-mutilative and obsessive compulsive behaviours (Robertson et al., 1990). In their review Temel and Visser-Vandewalle (2004) point out that thalamic lesions as performed by Hassler and Dieckmann (1970) showed the best results with respect to reduction of tics in Tourette’s patients. Hassler and Dieckmann (1970) reported the results of three TS patients where they carried out numerous coagulations bilateral in the intralaminar, medial thalamic nuclei and the nucleus ventro-oralis internus resulting in an improvement in tics of 70%-100%. Targeting the basal ganglia and the thalamus in Tourette’s syndrome is matched by results in animal studies on the role of these structures in the occurrence of stereotypy and tics (for example Graybiel and Canales, 2001; Mink, 2001). Abnormalities of the basal ganglia and related thalamo-cortical circuits in Tourette’s patients have been described in various neuropathological and imaging studies (Moriarty et al., 1997; Stern et al., 2000) suggesting their fundamental pathophysiological importance in GTS. Correspondingly, defective dopamine transmission has been revealed in patients with GTS (Heinz et al., 1998; Singer et al., 2002). It is hypothesised that an abnormal spontaneous activation of discrete sets of striatal neurones (possible dopaminedependent effects) inhibit Gpi and substantia nigra reticulate (SNr) neurons that would normally be active to suppress unwanted movements. This would result in a defective suppression of competing motor pattern generation and behavioural 6 programs at the level of the basal ganglia and disinhibition of thalamo-cortical circuits leading to the stereotypic features in GTS (Graybiel et al., 1994; Mink, 2001). Deep brain stimulation (DBS), a safe and reversible neurosurgical approach, has been established recently in the treatment of other movement disorders such as Parkinson’s disease and dystonia (Limousin et al., 1995; Coubes et al., 2001). Here, among other motor symptoms, hyperkinesias have been successfully treated by high frequency stimulation of the globus pallidus internum (Gpi) (Coubes et al., 2000; Follett, 2004). Thalamic DBS (ventral intermediate thalamic nucleus) has been used successfully in patients with myoclonus−dystonia (Trottenberg et al., 2001) and essential tremor (Lyons and Pahwa, 2004) without occurrence of severe side effects. The centromedian nucleus of the thalamus has been used as a target in functional neurosurgery in epilepsy and pain with beneficial effects (Velasco et al., 1995; Hariz and Bergenheim, 1995). Furthermore, 17 patients with cervical dystonia have been treated by unilateral lesioning of the ventro-oralis internus (Voi) nucleus of the thalamus (von Essen et al., 1980). With this background, a number of patients have been reported in the literature as having undergone DBS for GTS. Visser-Vandewalle (2003) reports on three patients where bilateral DBS electrodes were implanted at a strategic point allowing stimulation of either the centromedian nucleus, the substantia periventricularis and/or the ventro-oralis internus. The selection of the thalamus as a target for DBS has been based on the lesion studies by Hassler and Dieckmann (1970) and justified by the involvement of the ventral and medial thalamic nuclei in the basal ganglia-cortical circuits and additional neuronal projections from the midline and intralaminar nuclei to the striatum (overview in Visser-Vandewalle et al., 2003). The inhibition of these targets during high frequency stimulation is likely to influence activity levels in motor and limbic basal ganglia circuits. In this study, all three male patients presented with intractable GTS without co-morbidity except for associated behavioural problems. A significant reduction in frequency and severity of tics was revealed after one week of continuous DBS (about 50%-80%) and long-term follow-up showed an improvement in tics of about 70%90% and a reduction in compulsive and self-injurious behaviour (Visser-Vandewalle et al., 2003). None of the patients showed severe side effects of DBS but all patients reported a feeling of “reduced energy”. Neuropsychological assessment has not been reported in detail but at least one patient showed decreased reaction time and word fluency during DBS (Visser-Vandewalle et al., 2003). Similarly, active DBS contacts have not been related to the neuroanatomical target structures in this study. Interestingly, different active contacts have been used across patients and stimulation frequency is remarkably less in one patient when compared to parameter settings used in PD or dystonia. Unfortunately, the results of surgery have not been uniformly or comprehensively analyzed in all patients. The largest series of DBS targeting specific thalamic nuclei reports an improvement in all 18 patients (Servello et al). However these findings are not supported by a well designed randomized trial of 5 patients. Another patient reported is a 36 year old woman with severe GTS who has been operated simultaneously in the centromedian-parafascicular complex of the thalamus and the anteromedial part of the Gpi (Houeto et al., 2005). Thalamic as well as pallidal high frequency stimulation lead to significant improvement in severity and frequency of tics by about 70% but no add-on effect has been described during 7 simultaneous stimulation at both targets (Houeto et al., 2005). In this patient, thalamic stimulation resulted in amelioration of depression and mood stabilization, not observed during Gpi-DBS (Houeto et al., 2005). A small number of patients have undergone GPi DBS with promising results. These preliminary results suggest that DBS of the thalamus or the pallidum holds promise for the treatment of intractable GTS using its advantage as a reversible and adjustable method. A number of factors point towards the GPi as an attractive target for DBS in Tourette syndrome. Information flow in neural circuits can be influenced at a number of sites. It is well known from the movement disorder literature that bilateral surgery is better tolerated on the pallidum than in the thalamus. Additionally, the pallidal target can be easily visualized on MRI allowing uniformity of targeting across patients. Targeting of thalamic sub nuclei does not enjoy this important practical advantage Currently, systematic studies with an interdisciplinary team are needed to refine patient selection and stimulation parameter settings as well as to gain further insights into the beneficial effects of this new approach on the various aspects of GTS (motor symptoms and associated behavioural disorders). 7. TRIAL OBJECTIVE AND PURPOSE The trial is non-commercial, there is a clinical and research element. The primary objective of this trial is to establish if deep brain stimulation of the internal pallidum is effective to improve tics in GDS. For this purpose, GPi DBS will be compared to off-DBS condition in double blind. The secondary objectives are assessing the effect of GPi DBS on quality of life, cognitive and behavioral functions. 8. STUDY DESIGN The primary end point will be the clinical rating score for tics, at the end of 3 month period on-DBS versus 3 months off-DBS in a randomised order, with double blind assessment. The Yale Global Tic Severity Scale, clinician rated and patient rated scales will both be used. Rush video assessment scale, a clinician rated video score from a 12 minute video sequence will be obtained in a standardized way and assessed by an independent rater. All the video sequences will be assessed blindly. We have chosen a cross-over design since this will allow each patient to be his own control, in a small group of patients it seems the most appropriate way to have a control group. We anticipate that any carry over effect will be diluted in the 3 months period. This is a phase II study. This treatment, if effective is a life long treatment. In addition to the 6 months period in double blind it is important to follow this improvement over time and make sure it is maintained. For this reason, we intend to proceed to an open label extension study after completion of the cross-over period. 8 A randomised cross-over study of DBS in Severe Tourette syndrome. Surgery Randomisation. Stimulator on. Stimulator off. O.L.E. t-2 mo t-1 mo t + 6 wks Stimulator off. Stimulator on. t=0 t + 18 weeks = Assessment Visit Schedule for DBS in Tourette syndrome trial. t=30 weeks 9 Visit 1. Screening t-2 months Visit 2. Visit 3. Consent Surgery t-1 month t=0 Visit 4. Baseline t + 6 wks Visit 5. Visit 6. Crossover End t + 18 wks t + 30 wks Screening Psychiatric examination Neurological Examination Trial Consent Surgical Consent Surgery YGTSS Video rating DCI Y-BOCS NPI BDI STAI TS-QoL MOVES NART WASI CVLT RMF Fluency Trail making test Stroop test Paced serial addition letter cancellation Corsi blocks Adverse effects Key. DCI = Diagnostic confidence index YGTSS = Yale Global Tic Severity Scale Y-BOCS = Yale-Brown obsessive Compulsive Scale NPI = Neuropsychiatric Inventory BDI = Beck Depression inventory II STAI = Spielberger State Trait Anxiety Inventory TS-Qol = Tourette syndrome Quality of Life Scale MOVES = Movement Disorder self-report scale NART = National Adult Reading Test WASI = Wechsler Adult Scale for Intelligence CVLT = California Verbal Learning Test RMF = Recognition Memory for Faces Primary outcome measure. The primary outcome measure will be the change in YGTSS between start and end of “stimulator on” phase compared with change in YGTSS between the start and end of “stimulator off” phase, when compared within patients. 10 Secondary end point will include: Assessment of quality of life: TS-QoL, disease specific scale administered at visits 2,4,5 and 6. Assessment of depression and anxiety: Beck Depression Inventory and Spielberger State-trait Anxiety index administered at visits 2,4,5, and 6. Assessment of behaviour: Neuropsychiatric Inventory, a career rated instrument administered at visits 2,4,5, and 6 Obsessive Compulsive rating scale: YBOCS- clinician rating administered at visits 2,4,5, and 6. Cognitive function o Measures of intellectual ability (NART, WASI) o Verbal and non-verbal memory (CVLT, RMF) o Tests of executive function and attention: phonemic and semantic word fluency, Trail Making Test, Stroop, paced serial addition test, letter cancellation test, Corsi blocks These tests will be administered by a neuropsychologist at visits 2,4,5 and 6 Adverse effects from surgery. 9. SUBJECT SELECTION Two centres will be involved. Patients will be selected from the specialist Tourette clinics at the NHNN and in Birmingham. These clinics have assessed around 3000 patients between them. Patients will be selected by the clinician running the clinic. The inclusion criteria are - Adults with stable Tourette syndrome. In most cases this means being over 25 years of age but there may be rare exceptions to this - Chronic and severe Tourette syndrome with a Yale Global Tourette Severity Scale of at least 35/50for at least 12 months - Resistant to adequate trials of conventional medical and psychological treatment - Stable medical treatment for a year - Compliant with treatment plans The exclusion criteria are Tics attributable to another neurological diagnosis Treatment with anticoagulants or antiaggregants that cannot be stopped for 2 weeks before and 2 weeks after surgery - Coagulation problems - Other disease compromising life expectancy - Other medical or psychiatric conditions which increase the risk of a failed procedure - Patient likely to benefit significantly from psychological intervention - Psychosocial risk factors which increase the risk of the procedure or may compromise post-operative care - Patient unwilling to co-operate with post-op assessment and care. We intend to recruit 20 patients. - 10. SUBJECT RECRUITMENT Patients will be recruited in the relevant clinics (see above). Clinicians responsible for the clinics will identify patients that could potentially benefit from this operation. 11 Patients will be given verbal information and an information sheet. Patients interested in taking these further will be screened for exclusion criteria. The consent for the study will be obtained by two senior clinicians at both sites. Surgical consent will be obtained separately by the neurosurgeon (Prof.Hariz, Mr. Zrinzo or Mrs. Mitchell) 11. TRIAL INTERVENTIONS 11.1 General information Deep brain stimulation (DBS) is regularly used for the treatment of Parkinson’s disease. Over recent years new applications such as dystonia have been developed. A few papers have reported in a small number of patients improvement of tics in patients with Tourette syndrome. The use of DBS is recommended by NICE for dystonia and tremor. Risk and benefits DBS implies a surgical procedure to implant electrodes in the brain. It has been used for more than 15 years to treat tremor and Parkinson’s and for more than 10 years to treat Dystonia. It is approved by NICE and is considered a very safe surgical treatment in terms of severe morbidity, with a very low risk of hemorrhage, stroke, paralysis etc. (less than 1%). 11.2 Use within the trial The DBS procedure will be done the same way it is routinely done for dystonia and for Parkinson’s disease (pallidal procedures). It will be done in general anesthesia, electrode will be implanted in the posteroventral internal pallidum under MRI guidance, using the Leksell stereotactic system. Postoperative MRI will be to verify good placement of the electrodes. Thus, the surgery itself is identical to the one used routinely to treat dystonia and parkinsonian dyskinesias. 12. RANDOMISATION The protocol includes a 6 months randomized blinded period. Patients will be randomized to either “stimulation on first” or “stimulator off first” The clinician responsible for the programming of the stimulator will be informed of this via a sealed envelope and program the patient accordingly. The patients, the clinicians and psychologists involved in rating will not be aware of the condition. 12 13. BLINDING & OTHER MEASURES TAKEN TO AVOID BIAS. - All the clinical scores done after 3 month on-stimulation and 3 month offstimulation will be double-blind, the patient and the clinician directly involved in the scoring will not be aware of the condition of stimulation. - The video assessments of tics done at all time points will be assessed by 2 investigators who will be blinded of the timing of the recording and the stimulation condition. - The clinician doing the programming will spend the same time adjusting the stimulator of the patient at the start of the on or off-stimulation period. The electrical parameters will be selected in a way that does not induce any side-effect perceived by the patient. 14. DATA 14.1 Data to be collected Data will be collected before surgery, at baseline and at the end of each block Data include validated scales of the patients’ symptoms and quality of life to measure changes within patients comparing “stimulator on” to “stimulator off” settings Measures of cognitive functions will also be recorded to evaluate any eventual side effect from the operation on those functions. 14.2 Data handling and record keeping Data will be collected on paper; they will be stored in a locked cabinet. Later on data will be coded and entered on computers protected by password. Records will be kept securely for 10 years after the end of the study. The rule of Data Protection Act 1998 will be followed. 15. STATISTICAL CONSIDERATION To assess clinical outcome repeated measure ANOVA will be used to compare the conditions “before surgery”, “stimulation on” and “stimulation off” for each patient. This is a pilot study since until now only case reports have been published in this area. The decision on the sample size has been based on practical considerations and not formal calculation. The results of this study could be used for the sample size of a multicenter trial if the results are favorable to design such a trial. 16. COMPLIANCE AND WITHDRAWAL 16.1 Subject compliance The stimulator works automatically and the patients will not be able to alter the setting programmed by the physicians. 16.2 Withdrawal / drop our of subject If a patient withdraws from the study before surgery he will be replaced. 17. INTERIM ANALYSIS AND DATA MONITORING A data monitoring committee will be convened to perform interim analysis if required. A separate safety committee will be convened to provide independent advice about safety and adverse events during the trial. 18. ETHICAL CONSIDERATIONS Information sheet and informed consent forms are included in the appendix. 13 Only patients over 20 and able to give informed consent will be included. Patients will be able to withdraw from the study. 19. FINANCING AND INSURANCE Standard NHS Indemnity arrangements apply for providing indemnity and/or compensation in the event of a claim by, or on behalf of participants for negligent harm. No compensation arrangements for non-negligent harm are available under NHS indemnity for providing indemnity and/or compensation in the event of a claim by, or on behalf of participants 20. REPORTING AND DISSEMINATION Results will be reported in meeting and submitted to journals after agreements of all investigators. REFERENCES 1. Coubes P, Roubertie A, Vayssiere N, Hemm S, Echenne B. Treatment of DYT1−generalised dystonia by stimulation of the internal globus pallidus. Lancet 2000; 355(9222):2220−2221. 2. Follett KA. Comparison of pallidal and subthalamic deep brain stimulation for the treatment of levodopa−induced dyskinesias. Neurosurg Focus 2004; 17(1):E3. 3. Graybiel AM, Aosaki T, Flaherty AW, Kimura M. The basal ganglia and adaptive motor control. Science 1994; 265(5180):1826−1831. 4. Graybiel AM, Canales JJ. The neurobiology of repetitive behaviors: clues to the neurobiology of Tourette syndrome. Adv Neurol 2001; 85:123−131. 5. Hariz MI, Bergenheim AT. Thalamic stereotaxis for chronic pain: ablative lesion or stimulation? Stereotact FunctNeurosurg. 1995;64:47−55. 6. Hassler R, Dieckmann G. [Stereotaxic treatment of tics and inarticulate cries or coprolalia considered as motor obsessional phenomena in Gilles de la Tourette's disease]. Rev Neurol (Paris) 1970; 123(2):89−100. 7. Heinz A, Knable MB, Wolf SS, Jones DW, Gorey JG, Hyde TM et al. Tourette's syndrome: [I−123]beta−CIT SPECT correlates of vocal tic severity. Neurology 1998; 51(4):1069−1074. 8. Houeto JL, Karachi C, Mallet L, Pillon B, Yelnik J, Mesnage V et al. Tourette's disorder and deep brain stimulation. J Neurol Neurosurg Psy 2005; in press. 9. Limousin P, Pollak P, Benazzouz A, Hoffmann D, Le Bas JF, Broussolle E et al. Effect of parkinsonian signs and symptoms of bilateral subthalamic nucleus stimulation. Lancet 1995; 345(8942):91−95. 10. Lyons KE, Pahwa R. Deep brain stimulation and essential tremor. J Clin Neurophysiol 2004; 21(1): 2−5. 11. Mink JW. Basal ganglia dysfunction in Tourette's syndrome: a new hypothesis. Pediatr Neurol 2001; 25(3):190−198. 12. Moriarty J, Varma AR, Stevens J, Fish M, Trimble MR, Robertson MM. A volumetric MRI study of Gilles de la Tourette's syndrome. Neurology 1997; 49(2):410−415. 14 13. Robertson M, Doran M, Trimble M, Lees AJ. The treatment of Gilles de la Tourette syndrome by limbic leucotomy. J Neurol Neurosurg Psychiatry. 1990; 53(8):691−4 14. Singer HS, Szymanski S, Giuliano J, Yokoi F, Dogan AS, Brasic JR et al. Elevated intrasynaptic dopamine release in Tourette's syndrome measured by PET. Am J Psychiatry 2002; 159(8):1329−1336. 15. Stern E, Silbersweig DA, Chee KY, Holmes A, Robertson MM, Trimble M et al. A functional neuroanatomy of tics in Tourette syndrome. Arch Gen Psychiatry 2000; 57(8):741−748. 16. Temel Y, Visser−Vandewalle V. Surgery in Tourette syndrome. Mov Disord 2004; 19(1):3−14. 17. Trottenberg T, Meissner W, Kabus C, Arnold G, Funk T, Einhaupl KM et al. Neurostimulation of the ventral intermediate thalamic nucleus in inherited myoclonus−dystonia syndrome. Mov Disord 2001; 16(4):769−771. 18. Velasco F, Velasco M, Velasco AL, Jimenez F, Marquez I, Rise M. Electrical stimulation of the centromedian thalamic nucleus in control of seizures: long−term studies. Epilepsia 1995; 36(1):63−71. 19. Visser−Vandewalle V, Temel Y, Boon P, Vreeling F, Colle H, Hoogland G et al. Chronic bilateral thalamic stimulation: a new therapeutic approach in intractable Tourette syndrome. Report of three cases. J Neurosurg 2003; 99(6):1094−1100. 20. Von Essen C, Augustinsson LE, Lindqvist G. VOI thalamotomy in spasmodic torticollis. Appl Neurophysiol 1980; 43(3−5):159−163. 21. Orth M, Amann B, Robertson MM, Rothwell JC.Excitability of motor cortex inhibitory circuits in Tourette syndrome before and after single dose nicotine. Brain. 2005;128:1292-300 APPENDIX - Patient information sheet Patient consent form Ethics form