CARCINO EMBRYONIC ANTIGEN ... CARCINO EMBRYONIC ANTIGEN LABSC00009
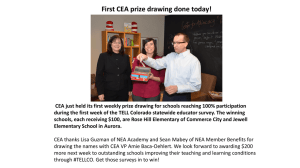
advertisement

CHANGE CARCINO EMBRYONIC ANTIGEN CARCINO EMBRYONIC ANTIGEN EFFECTIVE 08/26/2014 LABSC00009 Effective August 26, 2014, the clinical laboratory will switch methodologies for the Carcino Embyronic Antigen (CEA) assay. The switch will be from the Siemens ADVIA Centaur Chemiluminescent Immunoassay to the Abbott ARCHITECT i1000 Chemiluminescent Microparticle Immunoassay (CMIA). The comparison studies between the ARCHITECT and the Centaur methods showed some significant differences, with the ARCHITECT method recovering higher overall. However, the differences between methods seem to vary between patients, with some patient sample comparisons showing similar results, but other patients with larger differences. The Deming regression statistics for the two studies (n=40 for each) were: Study 1: ARCHITECT CEA ng/mL = 1.59 x Centaur CEA – 0.04 r = 0.96 Study 2: ARCHITECT CEA ng/mL = 1.58 x Centaur CEA – 0.34 r = 0.96 In order to provide some baselining of results, once we begin reporting results using the new Architect method, we will also provide the Centaur result in a comment attached to the CEA result. We will baseline patients with values >5.0 ng/mL and with a previous Centaur result for a 3-month period. Sample Requirements: Collect: SST (gold top) or plain red top serum, 4 mL. Patient Preparation: NA Storage/Transport: Deliver at room temperature to the laboratory for processing. If sample cannot be delivered to the laboratory within 24 hours of collection, centrifuge sample and transport separated serum refrigerated at 2-8°C. Stability: Separated serum can be refrigerated at 2-8°C for up to 7 days, or frozen at -20°C for longer storage. Minimum volume: 0.5 mL serum; (absolute minimum – only pipetable once – 0.3 mL serum) Unacceptable Conditions: Samples other than serum or samples not held at correct temperature. Reference Interval: 0 – 5.0 ng/mL Additional Information: The assay should not be used as a cancer screening test. Patients with confirmed carcinoma frequently have a pretreatment CEA level in the same range as healthy individuals. Elevation in circulating CEA levels may be observed in smokers, as well as, patients with nonmalignant disease. For these reasons, a serum CEA level, regardless of value, should not be interpreted as absolute evidence of the presence or absence of malignant disease. The CEA level should be used in conjunction with information available from clinical evaluation and other diagnostic procedures. LIS mnemonic: CEA www.testmenu.com/ucdavis Expected Values The manufacturer’s study of 1,141 specimens showed the following distribution of CEA values as tested by the Architect analyzer. In this study, 93.5% of healthy subjects (n=308) had CEA values of 5.0 ng/mL or less. The distribution table below for malignant disease is derived primarily from patients representing both active (clinical evidence of disease progression) and inactive (no clinical evidence of disease progression) disease states. Distribution of Architect CEA Values in Percent (%) >3 - 5 >5 – 10 Number of 0 – 3 ng/mL ng/mL ng/mL Subjects Healthy Subjects Smokers 74.2 18.2 6.9 159 Non-smokers 83.2 11.4 5.4 149 Total 78.6 14.9 6.2 308 Nonmalignant Disease Ulcerative Colitis 72.0 20.0 4.0 50 Rectal Polyps 83.3 10.3 5.1 78 Pulmonary 81.7 20.0 13.3 60 Cirrhosis 47.3 30.0 15.5 110 Hepatitis 70.0 18.7 11.7 60 Renal 60.0 15.0 15.0 20 Malignant Disease Colorectal 24.0 10.7 10.7 150 Gastric 62.2 5.4 10.8 37 Pulmonary 47.3 19.1 9.1 110 Mammary 62.4 11.1 10.3 117 Ovarian 78.0 7.3 2.4 41 >10 ng/mL 0.8 0.0 0.3 4.0 1.3 5.0 7.3 1.7 10.0 54.7 21.6 24.5 16.2 12.2 Routine Testing: T & TH, dayshift in the Special Chemistry section at the Clinical Lab’s STC location. If you have questions or need additional information please contact Laboratory Client Services at (916) 734-7373 or email pathologyclientservices@ucdmc.ucdavis.edu. LIS mnemonic: CEA www.testmenu.com/ucdavis