Hold The Heparin Nicholas Wettersten, MD; Ezra Amsterdam, MD Introduction
advertisement
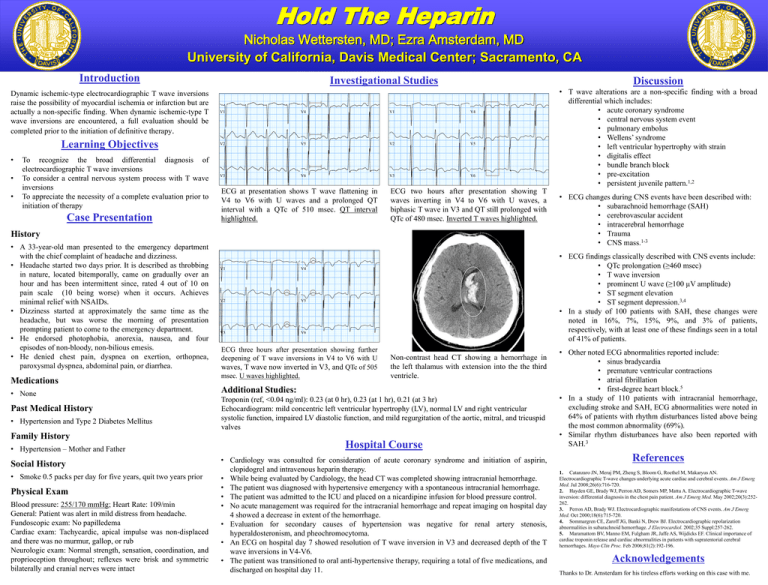
Hold The Heparin MORALES, LAURO ID:1662868 18-JUL-1978 (33 yr) Male Hispanic Vent. rate PR interval QRS duration QT/QTc P-R-T axes Room:6673 Loc:0 94 190 96 408/510 57 33 Nicholas Wettersten, MD; Ezra Amsterdam, MD University of California, Davis Medical Center; Sacramento, CA 19-AUG-2011 MORALES, 11:38:35 LAURO BPM ms ms ms 90 Normal sinus18-JUL-1978 rhythm (33 yr) Vent. rate Hispanic PR interval Nonspecific Male ST and T wave abnormality QRS duration Prolonged QT Room:6673 QT/QTc Abnormal ECG Loc:0 P-R-T axes Confirmed by BOMMER MD, WILLIAM (3) on 8/22/2011 11:43:51 AM Technician: AZ Test ind:DIZZY Technician:STAFF ER Test ind:Hypertension, unspecified Introduction DIAGNOSIS: ID:1662868 Referred by: SHARON WILSON DIAGNOSIS: DIAGNOSIS: 78 162 94 410/467 56 27 UCD MED 19-AUG-2011 CENTER 13:38:26 BPM ms ms ms 176 UCD MED CENTER Normal sinus rhythm Left ventricular hypertrophy with repolarization abnormality Abnormal ECG Confirmed by VENUGOPAL MD, SANDHYA (53) on 8/21/2011 10:42:16 AM Investigational Studies Electronically Signed by: WILLIAM BOMMER Referred MD by: SHARON WILSON Electronically Signed by: SANDHYA VENUGOPAL MD Dynamic ischemic-type electrocardiographic T wave inversions raise the possibility of myocardial ischemia or infarction but are I aVR actually a non-specific finding. When dynamic ischemic-type T wave inversions are encountered, a full evaluation should be completed prior to the initiation of definitive therapy. V1 I V4 aVR V1 V4 Learning Objectives V2 II V5 aVL V2 V5 II • • • aVL To recognize the broad differential diagnosis of electrocardiographic T wave inversions V6 aVF V3 V6 To considerIIIa central nervous systemaVFprocess with T wave V3 III ID:1662868 19-AUG-2011 14:20:18 UCD MED CENTER inversionsMORALES, LAURO ECG at presentation shows T wave flattening in ECG two hours after presentation showing T 18-JUL-1978 (33necessity yr) Vent. rate 78 BPMpriorNormal sinus rhythm To appreciate the of a complete evaluation to Male Hispanic PR interval 154 ms ST & T waveV4 abnormality, consider inferior ischemia to V6 with U waves and a prolonged QT waves inverting in V4 to V6 with U waves, a QRS duration 100 ms ST & T wave abnormality, consider anterolateral ischemia initiation Room:6673 ofV1therapy V1 QT/QTc 432/492 ms Prolonged QTinterval with a QTc of 510 msec. QT interval biphasic T wave in V3 and QT still prolonged with Loc:0 History P-R-T axes Case Presentation 69 68 176 Abnormal ECG Confirmed by BOMMER MD, WILLIAM (3) on 8/22/2011 11:40:04 AM highlighted. Technician:STAFF ER Test ind:WILSON II II Referred by: SHARON WILSON DIAGNOSIS: • A 33-year-old man presented to the emergency department with the chief complaint of headache and dizziness. • Headache started two days prior. It is described as throbbing I aVR V5 in nature, located bitemporally, came on gradually over an 10mm/mV 150Hz 7.1.1 12SL 239 CID: 74 hour and 25mm/s has been intermittent since, rated 4 out of 10 on pain scale (10 being worse) when it occurs. Achieves II aVL minimal relief with NSAIDs. • Dizziness started at approximately the same time as the headache, but was worse the morning of presentation prompting patient to come to the emergency department. III aVF • He endorsed photophobia, anorexia, nausea, and four episodes of non-bloody, non-bilious emesis. • He denied chest pain, dyspnea on exertion, orthopnea, V1 paroxysmal dyspnea, abdominal pain, or diarrhea. Medications • None QTc of 480 msec. Inverted T waves highlighted. V1 Electronically Signed by: WILLIAM BOMMER MD V4 V5 25mm/s 10mm/mV EID:3150Hz EDT: 11:43 7.1.1 22-AUG-2011 12SL 239ORDER: CID: 72629467 139 ACCOUNT: 020020589634 Page 1 of 1 V2 V5 V3 V6 ECG three hours after presentation showing further deepening of T wave inversions in V4 to V6 with U waves, T wave now inverted in V3, and QTc of 505 msec. U waves highlighted. Past Medical History • Hypertension and Type 2 Diabetes Mellitus V5 Family History 25mm/s 10mm/mV 150Hz 7.1.1 12SL 239 CID: 139 • Hypertension – Mother and Father Social History • Smoke 0.5 packs per day for five years, quit two years prior Physical Exam Blood pressure: 255/170 mmHg; Heart Rate: 109/min General: Patient was alert in mild distress from headache. Fundoscopic exam: No papilledema Cardiac exam: Tachycardic, apical impulse was non-displaced and there was no murmur, gallop, or rub Neurologic exam: Normal strength, sensation, coordination, and proprioception throughout; reflexes were brisk and symmetric bilaterally and cranial nerves were intact • T wave alterations are a non-specific finding with a broad differential which includes: • acute coronary syndrome • central nervous system event • pulmonary embolus • Wellens’ syndrome • left ventricular hypertrophy with strain • digitalis effect • bundle branch block • pre-excitation • persistent juvenile pattern.1,2 • ECG changes during CNS events have been described with: • subarachnoid hemorrhage (SAH) • cerebrovascular accident • intracerebral hemorrhage • Trauma • CNS mass.1-3 • ECG findings classically described with CNS events include: • QTc prolongation (≥460 msec) • T wave inversion EID:53 EDT: 10:42 21-AUG-2011 ORDER: 72635768 ACCOUNT: 020020589634 • prominent U wave (≥100 µV amplitude) Page 1 of 1 • ST segment elevation • ST segment depression.3,4 • In a study of 100 patients with SAH, these changes were noted in 16%, 7%, 15%, 9%, and 3% of patients, respectively, with at least one of these findings seen in a total of 41% of patients. Non-contrast head CT showing a hemorrhage in the left thalamus with extension into the the third ventricle. Additional Studies: II Discussion Troponin (ref, <0.04 ng/ml): 0.23 (at 0 hr), 0.23 (at 1 hr), 0.21 (at 3 hr) Echocardiogram: mild concentric left ventricular hypertrophy (LV), normal LV and right ventricular systolic function, impaired LV diastolic function, and mild regurgitation of the aortic, mitral, and tricuspid valves EID:3 EDT: 11:40 22-AUG-2011 ORDER: 72632910 ACCOUNT: 020020589634 Page 1 of 1 Hospital Course • Cardiology was consulted for consideration of acute coronary syndrome and initiation of aspirin, clopidogrel and intravenous heparin therapy. • While being evaluated by Cardiology, the head CT was completed showing intracranial hemorrhage. • The patient was diagnosed with hypertensive emergency with a spontaneous intracranial hemorrhage. • The patient was admitted to the ICU and placed on a nicardipine infusion for blood pressure control. • No acute management was required for the intracranial hemorrhage and repeat imaging on hospital day 4 showed a decrease in extent of the hemorrhage. • Evaluation for secondary causes of hypertension was negative for renal artery stenosis, hyperaldosteronism, and pheochromocytoma. • An ECG on hospital day 7 showed resolution of T wave inversion in V3 and decreased depth of the T wave inversions in V4-V6. • The patient was transitioned to oral anti-hypertensive therapy, requiring a total of five medications, and discharged on hospital day 11. • Other noted ECG abnormalities reported include: • sinus bradycardia • premature ventricular contractions • atrial fibrillation • first-degree heart block.5 • In a study of 110 patients with intracranial hemorrhage, excluding stroke and SAH, ECG abnormalities were noted in 64% of patients with rhythm disturbances listed above being the most common abnormality (69%). • Similar rhythm disturbances have also been reported with SAH.3 References 1. Catanzaro JN, Meraj PM, Zheng S, Bloom G, Roethel M, Makaryus AN. Electrocardiographic T-wave changes underlying acute cardiac and cerebral events. Am J Emerg Med. Jul 2008;26(6):716-720. 2. Hayden GE, Brady WJ, Perron AD, Somers MP, Mattu A. Electrocardiographic T-wave inversion: differential diagnosis in the chest pain patient. Am J Emerg Med. May 2002;20(3):252262. 3. Perron AD, Brady WJ. Electrocardiographic manifestations of CNS events. Am J Emerg Med. Oct 2000;18(6):715-720. 4. Sommargren CE, Zaroff JG, Banki N, Drew BJ. Electrocardiographic repolarization abnormalities in subarachnoid hemorrhage. J Electrocardiol. 2002;35 Suppl:257-262. 5. Maramattom BV, Manno EM, Fulgham JR, Jaffe AS, Wijdicks EF. Clinical importance of cardiac troponin release and cardiac abnormalities in patients with supratentorial cerebral hemorrhages. Mayo Clin Proc. Feb 2006;81(2):192-196. Acknowledgements Thanks to Dr. Amsterdam for his tireless efforts working on this case with me.