An Uncommon Cause of Major Lower Gastrointestinal Bleeding Abigail Kopecky, MD
advertisement
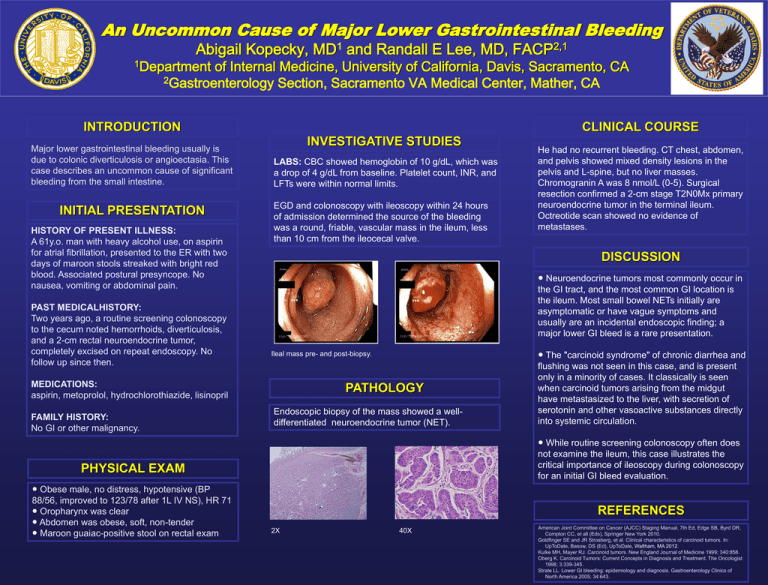
An Uncommon Cause of Major Lower Gastrointestinal Bleeding Abigail Kopecky, 1Department 1 MD and Randall E Lee, MD, 2,1 FACP of Internal Medicine, University of California, Davis, Sacramento, CA 2Gastroenterology Section, Sacramento VA Medical Center, Mather, CA INTRODUCTION Major lower gastrointestinal bleeding usually is due to colonic diverticulosis or angioectasia. This case describes an uncommon cause of significant bleeding from the small intestine. INITIAL PRESENTATION HISTORY OF PRESENT ILLNESS: A 61y.o. man with heavy alcohol use, on aspirin for atrial fibrillation, presented to the ER with two days of maroon stools streaked with bright red blood. Associated postural presyncope. No nausea, vomiting or abdominal pain. PAST MEDICALHISTORY: Two years ago, a routine screening colonoscopy to the cecum noted hemorrhoids, diverticulosis, and a 2-cm rectal neuroendocrine tumor, completely excised on repeat endoscopy. No follow up since then. CLINICAL COURSE INVESTIGATIVE STUDIES LABS: CBC showed hemoglobin of 10 g/dL, which was a drop of 4 g/dL from baseline. Platelet count, INR, and LFTs were within normal limits. EGD and colonoscopy with ileoscopy within 24 hours of admission determined the source of the bleeding was a round, friable, vascular mass in the ileum, less than 10 cm from the ileocecal valve. DISCUSSION ● Neuroendocrine tumors most commonly occur in the GI tract, and the most common GI location is the ileum. Most small bowel NETs initially are asymptomatic or have vague symptoms and usually are an incidental endoscopic finding; a major lower GI bleed is a rare presentation. Ileal mass pre- and post-biopsy. MEDICATIONS: aspirin, metoprolol, hydrochlorothiazide, lisinopril FAMILY HISTORY: No GI or other malignancy. PATHOLOGY Endoscopic biopsy of the mass showed a welldifferentiated neuroendocrine tumor (NET). ● The "carcinoid syndrome" of chronic diarrhea and flushing was not seen in this case, and is present only in a minority of cases. It classically is seen when carcinoid tumors arising from the midgut have metastasized to the liver, with secretion of serotonin and other vasoactive substances directly into systemic circulation. ● While routine screening colonoscopy often does not examine the ileum, this case illustrates the critical importance of ileoscopy during colonoscopy for an initial GI bleed evaluation. PHYSICAL EXAM ● Obese male, no distress, hypotensive (BP 88/56, improved to 123/78 after 1L IV NS), HR 71 ● Oropharynx was clear ● Abdomen was obese, soft, non-tender ● Maroon guaiac-positive stool on rectal exam He had no recurrent bleeding. CT chest, abdomen, and pelvis showed mixed density lesions in the pelvis and L-spine, but no liver masses. Chromogranin A was 8 nmol/L (0-5). Surgical resection confirmed a 2-cm stage T2N0Mx primary neuroendocrine tumor in the terminal ileum. Octreotide scan showed no evidence of metastases. REFERENCES 2X 40X American Joint Committee on Cancer (AJCC) Staging Manual, 7th Ed, Edge SB, Byrd DR, Compton CC, et all (Eds), Springer New York 2010. Goldfinger SE and JR Strosberg, et al. Clinical characteristics of carcinoid tumors. In: UpToDate, Basow, DS (Ed), UpToDate, Waltham, MA 2012. Kulke MH, Mayer RJ. Carcinoid tumors. New England Journal of Medicine 1999; 340:858. Oberg K. Carcinoid Tumors: Current Concepts in Diagnosis and Treatment. The Oncologist 1998; 3:339-345. Strate LL. Lower GI bleeding: epidemiology and diagnosis. Gastroenterology Clinics of North America 2005; 34:643.