Who, What, When, Where, Why, and How? Antimicrobial Prophylaxis
advertisement
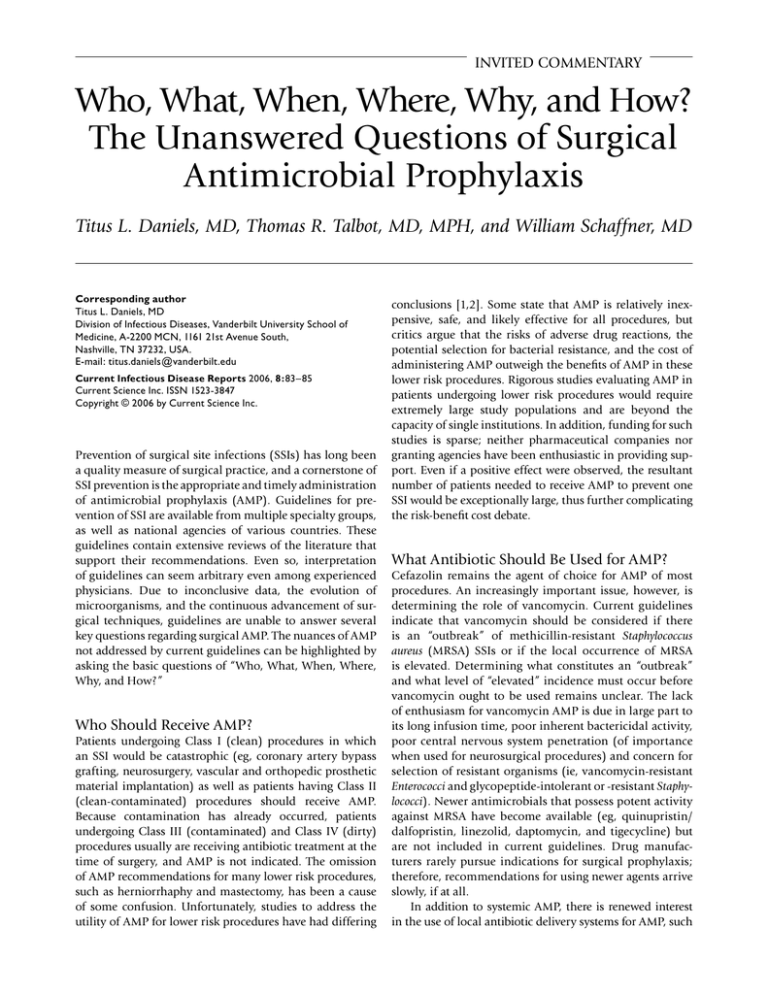
INVITED COMMENTARY Who, What, When, Where, Why, and How? The Unanswered Questions of Surgical Antimicrobial Prophylaxis Titus L. Daniels, MD, Thomas R. Talbot, MD, MPH, and William Schaffner, MD Corresponding author Titus L. Daniels, MD Division of Infectious Diseases, Vanderbilt University School of Medicine, A-2200 MCN, 1161 21st Avenue South, Nashville, TN 37232, USA. E-mail: titus.daniels@vanderbilt.edu Current Infectious Disease Reports 2006, 8:83 – 85 Current Science Inc. ISSN 1523-3847 Copyright © 2006 by Current Science Inc. Prevention of surgical site infections (SSIs) has long been a quality measure of surgical practice, and a cornerstone of SSI prevention is the appropriate and timely administration of antimicrobial prophylaxis (AMP). Guidelines for prevention of SSI are available from multiple specialty groups, as well as national agencies of various countries. These guidelines contain extensive reviews of the literature that support their recommendations. Even so, interpretation of guidelines can seem arbitrary even among experienced physicians. Due to inconclusive data, the evolution of microorganisms, and the continuous advancement of surgical techniques, guidelines are unable to answer several key questions regarding surgical AMP. The nuances of AMP not addressed by current guidelines can be highlighted by asking the basic questions of “Who, What, When, Where, Why, and How?” Who Should Receive AMP? Patients undergoing Class I (clean) procedures in which an SSI would be catastrophic (eg, coronary artery bypass grafting, neurosurgery, vascular and orthopedic prosthetic material implantation) as well as patients having Class II (clean-contaminated) procedures should receive AMP. Because contamination has already occurred, patients undergoing Class III (contaminated) and Class IV (dirty) procedures usually are receiving antibiotic treatment at the time of surgery, and AMP is not indicated. The omission of AMP recommendations for many lower risk procedures, such as herniorrhaphy and mastectomy, has been a cause of some confusion. Unfortunately, studies to address the utility of AMP for lower risk procedures have had differing conclusions [1,2]. Some state that AMP is relatively inexpensive, safe, and likely effective for all procedures, but critics argue that the risks of adverse drug reactions, the potential selection for bacterial resistance, and the cost of administering AMP outweigh the benefits of AMP in these lower risk procedures. Rigorous studies evaluating AMP in patients undergoing lower risk procedures would require extremely large study populations and are beyond the capacity of single institutions. In addition, funding for such studies is sparse; neither pharmaceutical companies nor granting agencies have been enthusiastic in providing support. Even if a positive effect were observed, the resultant number of patients needed to receive AMP to prevent one SSI would be exceptionally large, thus further complicating the risk-benefit cost debate. What Antibiotic Should Be Used for AMP? Cefazolin remains the agent of choice for AMP of most procedures. An increasingly important issue, however, is determining the role of vancomycin. Current guidelines indicate that vancomycin should be considered if there is an “outbreak” of methicillin-resistant Staphylococcus aureus (MRSA) SSIs or if the local occurrence of MRSA is elevated. Determining what constitutes an “outbreak” and what level of “elevated” incidence must occur before vancomycin ought to be used remains unclear. The lack of enthusiasm for vancomycin AMP is due in large part to its long infusion time, poor inherent bactericidal activity, poor central nervous system penetration (of importance when used for neurosurgical procedures) and concern for selection of resistant organisms (ie, vancomycin-resistant Enterococci and glycopeptide-intolerant or -resistant Staphylococci). Newer antimicrobials that possess potent activity against MRSA have become available (eg, quinupristin/ dalfopristin, linezolid, daptomycin, and tigecycline) but are not included in current guidelines. Drug manufacturers rarely pursue indications for surgical prophylaxis; therefore, recommendations for using newer agents arrive slowly, if at all. In addition to systemic AMP, there is renewed interest in the use of local antibiotic delivery systems for AMP, such 84 Invited Commentary as antibiotic-impregnated sutures, dressings, cement, beads, and irrigant solutions. Local delivery of high concentrations of antimicrobial agents to prevent SSIs seems logical; however, key questions remain. What concentration of antibiotic is optimal, and what duration of antibiotic exposure is necessary for the agent to be effective? Does local antibiotic therapy add any benefit to optimal systemic prophylaxis or could it replace systemic AMP altogether? Studies with SSI as an outcome to evaluate local antibiotic delivery methods are rare and generally evaluate the treatment of infections, not prophylaxis. Investigators have used different methods of preparing some local agents (eg, orthopedic cement) which result in varying concentrations of the locally delivered antimicrobial agent, compounding the difficulties encountered when comparing the effectiveness of local delivery systems. The impact of local antimicrobial delivery methods on the selection for antibiotic-resistant organisms is also unclear. Further, removal of a local delivery system may prove difficult in the event of a local or systemic adverse reaction to the antibiotic. Finally, local delivery modalities are often expensive and may de-emphasize the proven roles of strict adherence to antiseptic techniques and appropriate administration of AMP. Rigorous clinical trials to evaluate the effectiveness of local delivery methods must be completed before their routine use can be recommended. When Should AMP Be Administered? Recommendations state that the antibiotic infusion should begin within 60 minutes before incision in order to reach target tissue antibiotic concentrations but is there a “point-of-no-return” prior to incision when administration of antibiotic does not result in adequate tissue concentrations at the time of incision (eg, will a dose given 5 minutes before incision yield adequate tissue concentrations of AMP at the time of incision?). Some argue that it is critical to have adequate tissue concentrations of the drug at the time of incision whereas others believe that it is more important to have the highest antibiotic concentrations during and at the end of the procedure. Both arguments have theoretical merit; however, evidence to fully substantiate or refute either is lacking. Until more evidence is available, it is best to ensure adequate serum and tissue concentrations of the antibiotic at the time of incision, throughout the procedure, and for a short time after the operation is complete. Intraoperative redosing may be necessary to provide adequate concentrations of AMP throughout the procedure. Typically recommended after an interval equivalent to two half-lives of the AMP agent, redosing depends on the duration of surgery and the specific agent used. Further complicating the issue of redosing is the use of AMP in select populations. For example, it has been shown that morbidly obese patients undergoing gastric bypass surgery had rapidly declining tissue concentrations of cefazolin during the surgical procedure and suboptimal tissue levels well before the indicated redosing time [3]. Continuous infusion of cefazolin for AMP has also been proposed [4] to ensure adequate antibiotic levels throughout the procedure, though additional studies are needed before this practice can be recommended. Where Should AMP Be Administered and How Can Delivery Be Improved? These issues become difficult when considering the complexity of modern health care systems. Designing facility-specific processes to improve adherence to AMP is essential for effective SSI prevention. A variety of options are available for assisting providers in adhering to surgical AMP administration. Computer-aided systems for reminding providers to administer and/or redose AMP have been successful in increasing the appropriate redosing of AMP [5,6]. A preprinted checklist that accompanies the patient as they travel through the preoperative process and surgery can serve to remind clinicians to perform the essential tasks necessary to optimize AMP administration. Using a multidisciplinary approach, institutions must consider their unique facility characteristics to guide an AMP delivery process that best meets the needs of each system. The most important principles are to develop a system to improve AMP adherence and to ensure its use. Why Is AMP Important? SSIs are estimated to occur in up to 5% of all surgical procedures [7] causing substantial morbidity and mortality, are associated with prolonged hospitalizations, and lead to increased health care costs. Surgical AMP is a critical measure that has been proven effective in preventing SSI in multiple studies. With the national movement to provide patients with facility-specific nosocomial infection data, adherence to surgical AMP recommendations has been proposed as a publicly-reported process measure. The universal applicability of the basic tenets of surgical AMP and AMP’s proven benefits makes AMP adherence for major surgical procedures a rational quality metric for public reporting. Clinicians are entering a new era of SSI prevention. Novel methods of surgical AMP are available, but their effect on SSI prevention is unknown. Current AMP methods have a proven role in reducing SSIs, but several key questions remain in our understanding of surgical AMP. More effective strategies are welcomed, but one must first ensure that current processes have been optimized before venturing into unproven modalities. Funding such studies is a major hurdle but might be overcome if the evaluation of surgical AMP is also included as a component of studies evaluating surgical procedures. Furthermore, investigations into new surgical procedures should also address the question of surgical AMP as prevention of SSIs is a critical Invited Commentary element of any new surgical procedure. Current surgical AMP guidelines provide an important foundation for the prevention of SSIs. However, investigations to advance our knowledge of surgical AMP are urgently needed, lest an era of reliance on “the traditions of surgical AMP” be entered and evidence-based practice be forlorn. 3. 4. 5. References 6. 2. 7. 1. Sanchez-Manuel FJ, Seco-Gil JL: Antibiotic prophylaxis for hernia repair. Cochrane Database Syst Rev 2004, 4:CD003769. Mahatharadol V: A reevaluation of antibiotic prophylaxis in laparoscopic cholecystectomy: a randomized controlled trial. J Med Assoc Thai 2001, 84:105–108. 85 Edmiston CE, Krepel C, Kelly H, et al.: Perioperative antibiotic prophylaxis in the gastric bypass patient: do we achieve therapeutic levels? Surgery 2004, 136:738–747. Waltrip T, Lewis R, Young V, et al.: A pilot study to determine the feasibility of continuous cefazolin infusion. Surg Infect (Larchmt) 2002, 3:5–9. St Jacques P, Sanders N, Patel N, et al.: Improving timely surgical antibiotic prophylaxis redosing administration using computerized record prompts. Surg Infect (Larchmt) 2005, 6:215–221. Larsen RA, Evans RS, Burke JP, et al.: Improved perioperative antibiotic use and reduced surgical wound infections through use of computer decision analysis. Infect Control Hosp Epidemiol 1989, 10:316–320. Mangram AJ, Horan TC, Pearson ML, et al.: Guideline for prevention of surgical site infection, 1999. Hospital Infection Control Practices Advisory Committee. Infect Control Hosp Epidemiol 1999, 20:250–280.