Health Information Exchange Case Study Northern California Health Information Network
advertisement

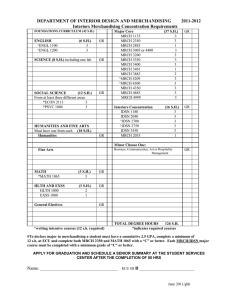
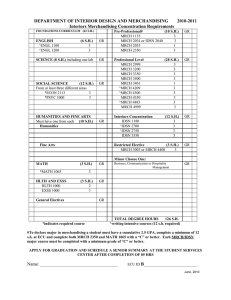
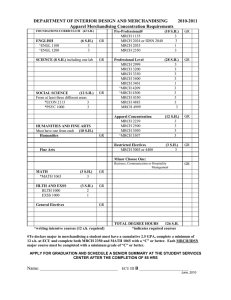
Health Information Exchange Case Study Northern California Health Information Network January 30, 2014 Katherine K. Kim Danielle Gordon San Francisco State University, Health Equity Institute Prepared for California Health eQuality University of California Davis Institute for Population Health Improvement http://www.ucdmc.ucdavis.edu/iphi/programs/cheq/ Copyright © 2013 The California Health and Human Services Agency (CHHS). All rights reserved. This publication/product was made possible by Award Number 90HT0029 from Office of the National Coordinator for Health Information Technology (ONC), U.S. Department of Health and Human Services. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of ONC or the State of California Contents Introduction ..................................................................................................................................... 2 Methods .......................................................................................................................................... 2 Description of North Coast Health Information Network (NCHIN) ................................................. 2 NCHIN’s Project Goals and Plans ..................................................................................................... 3 Results ............................................................................................................................................. 4 Participants .................................................................................................................................. 4 Technology .................................................................................................................................. 7 Lessons learned ............................................................................................................................... 9 Sustainability ............................................................................................................................... 9 Practice Workflow ..................................................................................................................... 10 Working with EHR Vendors ....................................................................................................... 10 Interface Implementation ......................................................................................................... 11 Relationship Building ................................................................................................................. 11 Conclusion ..................................................................................................................................... 12 About the Partners ........................................................................................................................ 13 1|Page Introduction Callifornia Health eQuality (CHeQ), a program of the Institute for Population Health Improvement at UC Davis, engaged San Francisco State University’s Health Equity Institute to develop a case study on one of its HIE Acceleration awardees, the North Coast Health Information Network (NCHIN). This report summarizes NCHIN’s grant goals, the progress made towards those goals, and lessons learned along the way. We hope that this information will be of assistance to other organizations who are seeking to launch or sustain their HIE efforts. Methods Two team members reviewed documentation provided by CHeQ including grant proposals, progress reports, and presentations. CHeQ also made introductions to the grantee’s staff. SFSU team conducted in-person interviews with three leadership and staff members, a board member and medical provider, and had one telephone interview with another community medical provider. Interviews were audiotaped and transcribed for analysis. The research was conducted from June to December 2013. The protocol was approved by San Francisco State University Institutional Review Board prior to conducting research. Description of North Coast Health Information Network (NCHIN) The North Coast Health Information Network (NCHIN) began as a project of the HumboldtDel Norte IPA and Foundation (HDN) in Eureka, CA. It serves as a data information hub, receiving health data from labs and hospitals, and routing it to local primary and specialist medical providers in Humboldt and Del Norte Counties. Prior to forming NCHIN, HDN initiated the North Coast Referral Network, aimed at facilitating the electronic transfer of patient clinical data between referring and specialist physicians. Based on the success of this project, and the commitment of the community to health information exchange, a decision was made to pursue the formation of a health information organization (HIO). NCHIN’s mission statement is to…“provide secure and appropriate sharing of electronic health and clinical data among diverse organizations facilitating access and retrieval of data for health care purposes, and to use that, individual, aggregated and comparative clinical data to improve health outcomes for clinicians and citizens of Humboldt County and Northern California.” NCHIN was incorporated as a separate legal entity in 2010. NCHIN is a “virtual” organization, and utilizes the employees and physical offices of the HDN. There are four permanent employees who provide services to the Medical Foundation, the IPA and to NCHIN, designating hours as needed to each entities’ projects. It is the recipient of four grants from California Health eQuality (one originating from its predecessor funding agency, Cal eConnect): an HIE Expansion Grant in 2011, an Interface Grant in 2012, an Immunization Interface Grant in 2013 and a grant to participate in CHeQ’s 2|Page California Trust Framework Pilot in 2013 . The receipt of the Expansion Grant corresponded with the initial foray into health information exchange (HIE) for NCHIN, and marks the start of their work in this area. NCHIN also received funds to participate in the Western States Consortium project, now called National Association for Trusted Exchange (NATE). In this case study we focus on NCHIN’s work related to the Expansion Grant and Interface Grant only. NCHIN’s Project Goals and Plans NCHIN’s goals in the Expansion and Interface Grants were to lower barriers to community provider’s ability to meet Meaningful Use requirements by completing the following: 1. Create a conduit for our region to send and receive electronic lab data between practice offices and lab facilities at the local hospitals. 2. Add 5 new HL7 laboratory interfaces for additional EHRs to route results from local hospitals to primary care practices and public health. 3. Build an interface to deliver documents and reports from hospitals and public health. 4. Add functionality to the existing IRIS referral system to exchange standard Continuity of Care Document (CCD) formatted referrals with specialists. 5. Transmit referral data electronically from IRIS to participating practices with EHRs. 6. Extract demographics data from EHRs on a real-time basis to keep the demographic data in IRIS synchronous with that stored in the EHRs. 7. Continue to provide existing data exchange services such as IRIS to non-EHR-enabled offices. Table 1 below summarizes the originally planned activities by category of data as outlined in the initial project proposal and describes the goals and methods for development. Table 1. Technology Development Plan Data Category Laboratory Data Goals Planned development methods 1. Create a hub and spoke system 1. EHR vendor will build 3 with NCHIN at the hub and interfaces practice offices, tele-health visiting 2. NCHIN will build systems to specialist centers, specialist offices, accept lab data from 2 existing county public health, and local hospital interfaces and route it chronic care and other state-wide to practices. registries being the spokes. 3. NCHIN will create a channel with Public Health to receive lab results Demographic 1. EHRs will forward demographic 1. EHR vendors will build 3 of the Data data to IRIS on a regular basis. process and message channels. 2. Establish real-time exchanges of 2. NCHIN will build the other 2. HL7 demographic data between EHRs and IRIS Referrals 1. Create a channel for Referral 1. EHR vendors will build 4 of the Status messages to be routed to process and message channels. 3|Page Data Category CCD Goals Planned development methods the referring provider’s EHR. 1. Provide an HITSP C32 CCD Component to the specialist provider at the time of referral. 2. Archive a copy of the CCD in the NCHIN repository. 2. NCHIN will build the other 1. 1. EHR vendors will build 3 systems to send the CCDs to NCHIN. 2. NCHIN will build the other 2. 3. NCHIN will build a web portal to provide access to archived CCDs to vetted ER providers. Results Participants The intended exchange participants included hospital labs, IPAs, community and Indian Health clinics, physician practices, and public health. NCHIN exceeded their goals for interfaces as well as the number of participating organizations. As of May 2013, they completed implementation of: 5 active inbound lab feeds 10 inbound document sources, 13 outbound feeds to individual practices Bi-directional feed for the internet-based referral system. Dictated document interfaces ADT outbound and ADT inbound from 1 of the local hospitals Processed 1.3 million data transactions from March to May, 2013 There was little community interest in building a CCD repository and this deliverable was cancelled. Figure 1 shows of the hub and spoke organization of NCHIN as of April, 2013. On the left, in boxes, are the data sources, organized by provider. On the right are the various practices that draw data through the NCHIN network. The chart is color coded to indicate the origin of each interface providing data to a provider site. 4|Page Figure 1. NHCIN Hub and Spoke Data Flows Table 2 below shows the interface, source, destination and status of each interface as of Dec. 2013 at the completion of the grant. Table 2. Interface Development Interface Dictated documents Source Entity Mad River Community Hospital (MRCH) St Josephs Health System (SJHS) MRCH Dictated documents MRCH Dictated documents MRCH Dictated documents MRCH Dictated documents SJHS A/D/T messages A/D/T messages 5|Page Destination Entity/EHR Current Status NCHIN LIVE NCHIN Development NCHIN United Indian Health Services/NextGen Open Door Community Health Centers/EPIC Redwood Family Practice/eClinicalWorks NCHIN LIVE LIVE Testing LIVE LIVE Interface Source Entity Dictated documents SJHS/MRCH Dictated documents SJHS/MRCH Dictated documents MRCH IRIS Interface demographics IRIS Interface demographics IRIS Interface – demographics IRIS Interface referral status messages IRIS Interface referral status messages IRIS Interface referral status messages Destination Entity/EHR Fortuna Family Medical Group/eHealthLine Eureka Family Practice/Practice Partner United Indian Health Service/NextGen United Indian Health Services IRIS (UIHS) Humboldt Medical Group IRIS (HMG) Fortuna Family Medical Group IRIS (FFMG) Current Status LIVE LIVE Cancelled due to funding issues LIVE LIVE LIVE IRIS United Indian Health Services/NextGen LIVE IRIS Fortuna Family Medical Group/eHealthLine LIVE IRIS Humboldt Medical Group/Practice Partner LIVE Laboratory results Eureka Internal Medicine (EIM) NCHIN LIVE Laboratory results SJHS/MRCH/EIM Laboratory results SJHS Laboratory results SJHS/MRCH/EIM Laboratory results MRCH Laboratory results SJHS/MRCH/EIM Laboratory results Humboldt County Department of Health and NCHIN Human Services (PH) Laboratory results SJHS/MRCH/EIM Laboratory results SJHS/MRCH/EIM Laboratory results SJHS/MRCH/EIM Laboratory results SJHS/MRCH/EIM 6|Page North Coast Surgical Specialists/Allscripts Pro NCHIN Eva Teresa Marshall, MD/Synamed NCHIN Humboldt Medical Group/Practice Partner Margaret Grossman, MD/Athena Fortuna Family Medical Group/eHealthLine Redwood Family Practice/eClinicalWorks Eureka OB-GYN/Prime Clinical LIVE LIVE LIVE LIVE LIVE LIVE Cancelled due to lack of provider interest (no cost interface) LIVE LIVE LIVE Interface Laboratory results Single normalized multi-source feed Laboratory results Single normalized multi-source feed Laboratory results Laboratory results Source Entity SJHS/MRCH/EIM PH PH Development LIVE Laboratory results SJHS/MRCH/EIM Laboratory results MRCH/PH Immunization Data UIHS A/D/T LIVE Cancelled due to funding issues SJHS/MRCH/PH Dictated documents Eureka Family Practice/Practice Partner Current Status SJHS/MRCH/EIM/ United Indian Health PH Service/NextGen Laboratory results Laboratory results Destination Entity/EHR St Josephs Health System Eureka Pediatrics Eureka Internal Medicine/AllScripts Enterprise McKinleyville Family Practice HSU Health Center/Orchard LIS California Immunization Registry (CAIR) SJHS/MRCH/EIM/ Redwood Pediatrics/Intergy Public Health SJHS/MRCH Redwood Pediatrics/Intergy Redwood NCHIN Pediatrics LIVE LIVE LIVE Development LIVE LIVE LIVE Technology NCHIN uses Mirth Connect as their core technology for HIE. They have implemented VPN tunnels, web-based security certificates, or an SFTP file drop system to transmit data, depending on the capabilities of the sites involved. They have also implemented DIRECT standard to push data to participants with NCHIN acting as the health information service provider (HISP). In addition, they support HL7 interfaces as shown in Table 2. To maintain provider data, NCHIN has a dedicated web portal for participating practices to access and update their provider data. Changes made to the provider directory are automatically emailed to the IT department and the NCHIN internal database updates Mirth. 7|Page Figure 1 shows NCHIN’s overall technical schema. 8|Page Lessons learned The NCHIN team learned many lessons through the grant-funded activities related to startup and ongoing management of the HIO, working with partners, and technology issues. Sustainability NCHIN’s HIO business model includes charging data suppliers a set fee per transaction, and data recipients a set fee per provider. At the time of the interviews for this report, participants in the HIO were reviewing a revised Participation Agreement that outlined this payment structure. It remains to be seen whether customers will accept the pricing model. Indications from the interviews conducted for this report seem to point toward this being an acceptable model. NCHIN is structured in a unique way to leverage existing staff and physical resources. By contracting existing staff from the IPA, as needed, it has been possible to maintain a highly experienced, skilled, permanent workforce, even as grant funding for the HIE ebbs and flows. This has allowed NCHIN to develop additional marketable services, which in turn contributes to the sustainability of the organization. NCHIN also made a key decision to assign one administrator to development of revenue generating products/services and sustainability. At the time of this report, NCHIN was providing a full package of IT support to three local medical practices. “[We] know more about people’s EHRs; we know more about their systems, their IT infrastructure than they do and we needed to learn that to do this work, to build the interfaces. And so we’re easily the most skilled IT shop in town by far…And so practices don’t have to get their systems from somebody, their EHR from somebody, their HIE from somebody, their, you know HEDIS measure aggregation from somebody. You know my goal is to have all of that be provided from here.” In an effort to develop sustainability for the organization, NCHIN also offers a bundle of IT services to community providers including workflow consulting, hardware and software consulting, selection, installation and maintenance. In the future, they are considering adding disaster data recovery as an additional fee-based service. For example, from their experience as a meaningful use adoption service provider, they created a “Practice Liaison” position that provides services such as workflow consulting. This service is offered for a fee to practices needing support around integrating new workflow systems to become aligned with meaningful use requirements. “…as practices have come along they’re finally starting to hear that you can’t put an electronic record system on top of a broken paper workflow…And so you really need to step back and look at that all over again. So we can teach them process mapping and quality improvement and PDSA [plan-do-study-act] cycles...” 9|Page As both a free community service and a marketing strategy, NCHIN offers educational sessions on topics pertinent to Meaningful Use and HIE. By recognizing the need for expert training on the technology and regulations, NCHIN has built its relationships and credibility among community providers. One internal medicine provider said, “And they sort of distilled things down to okay, these are the bullet points, these are the changes you’re going to need to make to go to upgrade to Meaningful Use stage 2. And you know and then we’re going to rely on their help in order to do that to qualify.” Practice Workflow For a practice to engage in HIE, they must first have enabled an electronic health record, and successfully transitioned their staff and workflow systems to the new technology. NCHIN staff identified multiple barriers to the adoption of EHR technology, including financial, cultural, conflicting priorities, and workflow. “They need to know how resistant people are to change their existing workflows; how the present EHRs how poor they are, how bad they really are. They need to understand that a lot of the barriers to using health information are cultural barriers around how clinicians deal with the world; they’re not really around providing information or not providing information.” As discussed in the Sustainability section above, NCHIN is addressing this challenge by providing workflow and meaningful use consultations to their HIE clients. Working with EHR Vendors One of the major challenges NCHIN reports is that often EHR vendors are uninterested in building desired interfaces. They reported multiple occasions when their work plan was delayed due to an inability to get the project on the vendor’s calendar. NCHIN was able to put centralized resources toward the relationships with vendors, keeping on top of the issues and communicating regularly, until resolution was reached. This is a commonly reported issue and one which individual provider offices would have even greater difficulty managing on their own. “In some cases we found that the EHR vendors were impacted by the need for all of these interfaces. And they didn’t have staff that were capable. And so we felt a couple times that our job here was to train EHR vendor staff to build interfaces. We have one EHR vendor that never built an interface. We were their first.” “The Iris interfaces were really difficult because we found that a lot of the EMR vendors do not want to write referral interfaces for referrals…They just said no, no, we don’t do referral interfaces. It was really amazing. So we ended up writing 3 or 4 of them.” 10 | P a g e Interface Implementation NCHIN developer staff report that much of the job of implementation requires relationship building with staff on both the sending and receiving ends of the interface. There is much work that goes in to standing up a new interface, and at times it is difficult for the practices to spare personnel for those tasks. One of the more challenging is to organize the individuals involved in testing a new interface. Project management and communication are key skills for implementers. “To make a lab interface work with the [hospital system] it takes an active person in the lab who usually is a med tech, somebody who actually knows how their system works and they have to generate test messages; those test messages them in their system go to their data center… and then they go across an interface to their interface company. And then the interface company if you will massages them in some particular way and sends them to us. And then we send them on to the practice. And each of these steps there is often some sort of programming responsibility and then there’s some sort of testing responsibility at the end of it. So you need somebody in the lab, you need somebody on the interface company’s side, you need us and then you need someone in the practice and you need the practice vendor. So you’ve gotta get 5 people working on this for it to really work. And I think that nothing could be harder really on some days. And so those people have to be scheduled; those people have to have the time to work on it.” Relationship Building NCHIN staff expressed that in some ways they are at the mercy of the administrative decisions that are made at the medical practices and hospitals. They reported several circumstances in which it was necessary to change or even cancel planned projects because the partners’ priorities had shifted. “St. Joe has a relationship with us to do all of their exchange but they could make a political decision that they want to do exchange another way and that decision would be made in Orange [system headquarters]. And they would just drop off our map…So having large multi-county, multi-state organizations work with local community HIEs the power is so disproportionate.” NCHIN administrators and staff are acutely aware that the ability to mitigate this risk and to continue progress toward full HIE in their community rests on the organization’s capacity to build relationships with the various stakeholders. They have been successful because they have built those relationships and strive to be responsive to the needs of those partners. 11 | P a g e “Again it’s relationships, talking to people. And you know the hospital hasn’t spent any money to get its results into all of these practices so you’d think that they’d like that. And so I think that you know our strongest tool there is to do good work.” “I think existing relationships are usually the most important part of it …we’re not interested in being an HIE, we’re interested in having an HIE here in the community for our clinicians, our providers. And so we had relationships with practically everybody that we built an interface for. And that is part of the overall organizational theory and I guess goals is for all of our projects they all have the same aim to make it work in Humboldt County. Now we’ll have some of the same techniques, you know relationships and being in the practices and having some idea about workflow. So all of that you know it’s true for the quality projects is true for the HIE projects; it’s true for utilization management.” They also acknowledge that some of their greatest barriers come about due to a lack of relationship with the other entity. They believe that excellent communication and responsiveness can help mitigate the inevitable challenges that come up in technology projects. For example, in building interfaces for practices the following barrier was described: “But I never hear him say, ‘Boy that was hard code to put together you know I really struggled with that.’ He doesn’t say that at all, he says, ‘I can’t get them to return my phone calls.’” Conclusion NCHIN provides a very interesting case study. Their strategy of leveraging human and physical resources of an existing IPA to initiate a new organization, was successful. This strategy reduced the hurdles of a startup, allowed efficient use of funds, and jump started the pulling together of existing relationships within the community to accomplish HIE. This approach put the organization in a strong position to meet the current and future HIE needs of their community. Although a small team, the staff and leadership of the HIO seem well suited to their roles. In addition, as a team, they were adept at business planning, project management, technical development, and operations which are important functions that an HIO must fulfill. Through the interviews conducted for this case study, several lessons learned were identified that may be useful to other HIOs. The fact of shifting priorities for current and potential participants is a universal reality for HIOs working toward interoperability. This theme is significant, since it can have a real financial impact on an HIO. Also the need to be strategic and proactively work to ensure that planned projects proceed is valuable to recognize. The experience around workflow changes is similarly important, because if a medical practice is unable to implement adequate changes to their workflow systems, they will not 12 | P a g e reap the benefits of HIE, and may become discouraged from pursuing electronic data exchange at all. The critical importance of building relationships with all stakeholders in the HIE development and implementation process, and of being perseverant is extremely valuable to underscore. It is important for all organizations involved in HIE to expect that resources are needed for project management to coordinate the data providers, data receivers, and EHR developers, for any given interface. While HIE implementation is largely technology focused, it is the human factors involved that can contribute the most to the success of the projects and ongoing benefit HIE can provide to provider practices and their patients. About the Partners About California Health eQuality (CHeQ) California Health eQuality (CHeQ) is a program of the UC Davis Institute for Population Health Improvement that administers statewide health information exchange (HIE) projects for California. Funded by the California Health and Human Services Agency, under the auspices of the Office of the National Coordinator for Health IT State HIE Cooperative Agreement, CHeQ is promoting coordinated and integrated care through health information exchange. Programs including a trusted exchange environment, improved public health capacity for electronic reporting, HIE acceleration funding opportunities, and the monitoring of HIE adoption lay a foundation for improved quality of care for all Californians. Please visit CHeQ at http://www.ucdmc.ucdavis.edu/iphi/programs/cheq/. About Institute for Population Health Improvement (IPHI) The UC Davis Institute for Population Health Improvement (IPHI) is working to align the many determinants of health to promote and sustain the well-being of both individuals and their communities. Established in 2011, the institute is leading an array of initiatives, from improving health-care quality and health information exchange to advancing surveillance and prevention programs for heart disease and cancer. About Health Equity Institute at San Francisco State University The Health Equity Institute of SFSU seeks to foster innovation and community engagement towards a vision of a truly healthy society. The mission of the Health Equity Institute (HEI) is to create an intellectual environment that encourages diversity of perspectives, challenges conventional approaches, and produces innovative action-oriented research in the biomedical and behavioral sciences in order to improve health, eliminate health disparities, and establish equity in health. San Francisco State University (SFSU) is a public university affiliated with the California State University system. Located in San Francisco, it offers 118 different Bachelor's degrees, 94 Master's degrees, and 5 Doctoral degrees. 13 | P a g e