Childbirth and Maternity From Cradle to Grave
advertisement
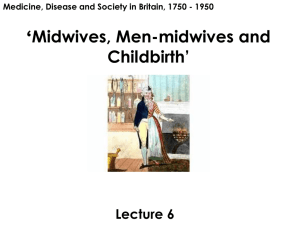
From Cradle to Grave Childbirth and Maternity Lecture Outline 1. Traditional’ childbirth – fear and ceremony (social childbirth) 2. Maternal mortality 3. Midwives - roles, training, characteristics and practice, qualification 4. Lying-in hospitals to hospitalisation 5. Changes in the 19th and 20th century– GP practice, registration of midwives 6. Medicalisation of child birth: hospitals, personnel and technology of childbirth Fear! • Death in childbirth (mothers and babies) • High stillbirth rate, high infant mortality, high maternal death rate. • Childbirth could be lengthy, painful, complicated. • impact of rickets, poor diet, instrumental births, childbirth fever, bad medical attendance. • While infant mortality fell from around 1900, maternal mortality high until 1930s/1940s. Maternal mortality • Causes: puerperal sepsis (post-partum fever) (40%), toxaemia (20%), haemorrhage (20%) • Deaths from puerperal sepsis and septic abortion rose between 1900-1934 • Maternal morality rate (MMR): – – – – 1900 - 42 per 10,000 births 1930 – 44 1940 – 26 1950 - 8.7 • How was fall explained? – Sulphonomides – reduced infection, mid-1930s. – War – blood transfusion and obstetric flying squad – Ergometrine 1942 reduced deaths from haemorrhage Alice Gregory (ed.), The Midwife: Her Book (London, 1923) ‘I have twice seen the desolation of a working man’s home when the mother is suddenly taken from her young children, and I never want to see it again. She went up to her room in good health perhaps twelve hours before, and she will never come down again until her body is carried to the grave.’ • 1920-29 - 25,000 women died in Britain from childbirth-related causes Poverty and pregnancy • Poor women’s pregnancies - money struggles and health problems. • Many continued to work hard throughout pregnancy. • General Lying-in Hospital early C20th - One patient ‘half-starved’ and another had ‘not had good food during her pregnancy’ (see Ellen Ross, Love and Toil). • Women’s Co-operative Guild letters. • Maud Pember Reeves 1912 - ‘motherhood is hanging over them like a curse’. Margaret Llewelyn Davies (ed.), Maternity. Letters from Working Women (London, 1915) ‘Three months before the baby came, I was practically an invalid…. Of course, I had chloroform; indeed I had it with all my seven children, except two, as I have always such long and terrible labours… I am never able to get up under three weeks after confinement, as I always start to flood directly I make any movement… to me [childbirth] is a time of horror from beginning to end’. Who became midwives? • Neighbours who occasionally helped, to women who delivered babies fairly regularly to those who worked ‘professionally’ as midwives. • Many ‘professional’ midwives scaled their fees according to what the patient could pay – often delivered for doctors • Many took on other roles – nursing and laying out the dead. • Many also helped in the household. • Mixture of abilities – some skilled and experienced, some not. • Most worked in women’s homes. Training • Until the late 19th century no formal training or qualification in midwifery in Britain (on continent midwifery training and schools were set up and midwives licensed by towns from early modern period). • Some midwives were trained by apprenticeship. • Skills were passed down from mother to daughter or other female relative. • Most training was practical, hands on – honed by practice and experience. • A few had more theoretical knowledge and book learning. Attributes and Tasks • Ideal midwife - kind, honest, gentle and not gossips. • Midwives were supposed to limit themselves to normal births and were not use medicines or instruments – to ‘wait on nature’. • They were not to be associated with birth control or abortion. • It was also important for them organize the birth and manage the lying-in. The social aspects of birth. A Women’s sphere? • Some midwives acted as a court witness in cases of infanticide, rape and abortion – also task to persuade mothers of illegitimate children to name father. ‘Traditional’ childbirth • Collective female culture (social rather than medical?) Midwife in charge. • Organised by women – but this changed in many households in 19th century as male doctors took over • Period of lying in for 1 month after the birth • Ended with churching ceremony – marking the return of the mother to public life – still practised in East End in early 20th century. Lying-in Hospitals to Maternity Hospitals • 18th century rise of lying-in hospitals – offered training to midwives and man-midwives. • Run as charities – poor women had limited access to care, concerns about population. Many in London. • Became dreaded sites of puerperal fever – feared by many. • 1848 Ignaz Semmelweis and infection control. • Poor Law also provided maternity care – of sorts – to pauper women • By 1920s and 1930s private nursing homes increasingly popular with middle and upper classes. Poor women also keen to have birth in hospital, though conditions often bad. Male obstetric practitioners 3 groups involved: • Man-midwife 18thC – increased in number (fashion and forceps) • Rise of GP, especially during 19thC – who took on more and more obstetric work • Rise of specialism of obstetrics (and gynaecology). New concerns about risks of childbirth (diseases of women). Though ostensibly worked with difficult cases also engaged themselves in normal obstetrics. Training and Registration Doctors: • 1840s midwifery added to the medical curriculum • 1850s diplomas awarded by medical schools • Licence in Midwifery (LM) acquired by many general practitioners – midwifery ‘a foothold’ of general practice Midwives: • 1862 King’s College Hospital introduces midwifery training for nurses, gradually training schemes introduced • Late 19th intense lobbying for registration and recognition of profession • 1902 Midwife Registration Act Medicalization of Childbirth? Why did male practice take hold? • Birth described as increasingly risky for mothers – made a medical matter with high levels of intervention – birth only ‘normal’ in retrospect. • A new spirit of medical enquiry, especially in the fields of anatomy and physiology, emphasis on formal training – new forms of ‘expertise’. • New technologies – forceps 18th century, anaesthesia (chloroform) 19th century. • The rise of the surgeon-apothecary as the family doctor . • Marketplace competition – midwifery lucrative. • Shift from home to hospital. • Changes in ‘culture’ of childbirth. Campaigns for training midwives • Female Medical Society and Midwives Association campaigned for proper training programmes l.C19th • Midwives Act 1902 – certification became a requirement. Managed largely by doctors. Central Midwives Board established. Unqualified midwives – bona fides – given a few years to acquire a licence. • 1905 Select Committee established a register of midwives, with a central body to approve training schools and admit qualified candidates. • 1936 Midwives Act local councils charged with providing adequate, salaried domiciliary service. Relief for midwives but most women then had to pay the local authority for midwifery care. • 1948 NHS introduces free midwifery services 1940s antenatal class Maternity Ward, The Royal Free Hospital, London (19133) Rise of hospital births • Hospital has become synonymous with ‘safe’ birth – provided justification for move to hospital but little evidence to show hospital safer. – 1900 most births at home with midwife. – 1930s birth at home with midwife or GP standard – 1950s trend towards hospital set in. – 1960 33% of women in England and Wales gave birth at home – 13% 1970 and by 1992 1 % • 1970 Peel Report declared hospital the proper place to give birth – around same time women began to assert their right to a home delivery. Ironic? Technology and birth • Hospital associated with more interventions – increased use of analgesics and anaesthesia in 20th century. • Pain relief also demanded by women. National Birthday Trust Fund set up in 1928 – aimed at ‘safer motherhood’ through better midwifery services and promoted anaesthesia in hospital and also pain relief at home. • After 1936 midwives allowed to use gas and air at home, but not chloroform. Counter movements • Grantly Dick-Read, obstetrician and pioneer of natural childbirth – Natural Childbirth (1933), Childbirth without Fear (1942). • National Childbirth Trust – more natural approaches. • Radical Midwives organisations. • Sheila Kitzinger – advocated an active role for women in birth, breathing techniques. • 1985 Wendy Savage Case. Twentieth century 3 factors that made the ‘medicalization’ of childbirth more apparent: 1. Men take over of childbirth – Female midwives lose autonomy. 2. Hospital deliveries increase – shift from home to hospital, especially after WWII. 3. Increasing intervention and use of technologies in childbirth – instruments and anesthetics. Changes • Fear of childbirth diminishes in the 1930s, as maternal mortality falls. 1948 free service. • Consumption of childbirth / the ‘good’ birth. • BUT still problems – overstretched services and many women give birth in poverty; impact of immigration; many mothers over 40 so ‘high risk’. Mother and child in maternity ward, 1962
![Letter to MPs re: maternal mental health report Dear [Name of MP] I](http://s3.studylib.net/store/data/006839335_1-7d7b3127aade7ad6d126565942ce75c1-300x300.png)