Case Study 1: An Evidence Based Practice Review Report
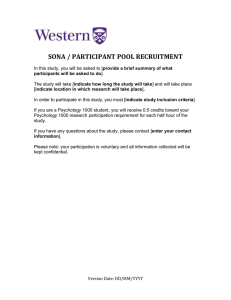
advertisement

Doctorate in Educational and Child Psychology Tamara Powell Case Study 1: An Evidence Based Practice Review Report Theme: Parent Interventions How effective is Parent Child Interaction Therapy (PCIT) at reducing symptom severity in young children with internalising disorders? 1. Summary Parent-Child Interaction Therapy (PCIT) is an empirically supported treatment designed to help parents manage problematic behaviour and build nurturing relationships with their child. Parents receive live coaching via a bug in the ear receiver from a therapist situated behind a one-way mirror throughout the course of treatment. Psychoeducational support that explains the treatment rational, nature of the disorder and effective parenting strategies is also interleaved into the various treatment modules. This literature review aimed to evaluate the effectiveness of PCIT and its neighbouring protocols in reducing symptom severity in young children with internalising disorders. A systematic literature search conducted over three databases revealed six studies, which were subsequently coded (adapted protocol from Kratochwill, 2003) and appraised using Harden and Gough’s (2012) ‘Weight of Evidence Framework.’ This review found moderate evidence for PCIT – Emotion Development (PCIT-ED) and preliminary evidence to support the effectiveness of Coaching Approach Behaviour Leading by Modeling (CALM) in reducing symptoms related to depression and anxiety. Traditional PCIT programmes, however, were found to be less effective in managing separation anxiety disorder (SAD) symptoms in children ages 3 to 8. Research that utilizes larger sample sizes and greater methodological rigour are warranted. 2. Introduction 2.1 Description of PCIT PCIT is an empirically validated psychotherapeutic intervention originally developed to treat young children (2-8 years) with disruptive behaviour problems. This intensive 8-14 week manual-based training programme is comprised of two Doctorate in Educational and Child Psychology Tamara Powell distinct phases: Child-Directed Interaction (CDI) and Parent-Directed Interaction (PDI). The former is focused on improving the parent child relationship and the latter in reducing disruptive behaviour. Both phases of treatment typically begin with a didactic training session that introduces key principles and skills and proceeded by individualised coaching sessions that provide parents live in vivo feedback. The CDI phase teaches parents PRIDE (Praise, Reflection, Imitation, Description, and Enthusiasm) coaching skills to elicit cooperative play behaviour, whereas the PDI phase focuses exclusively on firm, non-punitive disciplinary practices. During PDI, parents are trained to consistently praise desired behaviour (e.g., self-confidence, independence) and selectively ignore undesired behaviour (e.g., aggressive outbursts) through labelled praise and systematic ‘time-outs’. Daily homework is given throughout treatment and the programme is ceased once parents have mastered the CDI and PDI skills and their child’s internalising behaviour is brought within normal limits. PCIT can be administered by any mental health professional who has obtained at least a master’s degree in their field of work and undergone the required year-long training programme (Eyberg, 1999). In most cases, however, the programme is delivered by a clinical psychologist in a clinic-based setting. 2.2 Adaptations of PCIT 2.2.1 CALM CALM is an intensive 12 week intervention that treats young children with social phobia, generalized anxiety disorder (GAD), SAD and specific phobias. Similar to PCIT, CALM is a mastery based protocol that uses live, bug in the ear technology to coach parents in using positive attending and developmentally sensitive play skills (PRIDE). The programme begins with a teaching session and CDI phase of treatment which focuses on strengthening the parent-child relationship. Unlike PCIT however, the PDI phase is replaced by exposure sessions (brave behaviours module) that require parents to use directive parenting skills (Figure 1) to coach their child through increasingly difficult situations. Parents work alongside therapists to develop individualised fear hierarchies which children gradually achieve throughout the course of treatment. Doctorate in Educational and Child Psychology Tamara Powell Figure 1. Sequence of DADS steps (Puliafico, Comer & Albano, 2013). 2.2.2 PCIT-ED PCIT-ED is a developmentally lateral extension of PCIT for young children with early-onset depression. The programme includes three modules: CDI, PDI and the novel emotion development (ED) module. Throughout the ED module, children are encouraged to identify and label personal triggers as a way to consciously regulate precipitating stressors. Parents are also concurrently taught behavioural techniques to reinforce adaptive behaviour and strategies to manage their own negative affect. 2.3 Psychological Basis PCIT is built on the tenets of social learning theory (Bandura, 1977), operant conditioning (Skinner, 1938) and attachment theory (Bowlby, 1978). Although attachment theory forms part of the theoretical framework that guides PCIT, the intervention is primarily rooted in behaviourism and social learning theory (Allen, Timmer & Urquiza, 2014). The application of behavioural principles is arguably the most integral component of PCIT, as moment by moment functional analyses informs all treatment related decisions. Behavioural principles support the re-structuring of dysfunctional parent-child interactions, which according to social learning theory inadvertently develop in response to child behaviour problems. Coercive interactions between parent and child develop in a cyclical manner and are maintained through negative Doctorate in Educational and Child Psychology Tamara Powell reinforcement strategies (Stormont, 2002). Children’s maladaptive behaviour is therefore learned and preserved by parents (Patterson, Capaldi & Bank, 1991). With this in mind, PCIT attempts to specifically target critical, over-bearing parenting, found in anxious parents (Whaley, Pinto & Sigman, 1999) and inconsistent lowaccepting mothers in children with major depressive disorder (MDD; Gonzales, Pitts, Hill & Roosa, 2000). Consistent disciplinary practices in PDI that differentially reinforces adaptive behaviour is accordingly well suited for this population who exhibit dysfunctional, and often, reciprocal patterns of behaviour. Parent-child attachment style affects a child’s ability to effectively cope and regulate emotions during distressing or fearful situations (Cassidy & Kobak, 1988). That is, children who have parents that are sensitive and responsive to their needs (secure attachment) will come to consistently expect this treatment and view negative affect as a temporary state, which they will eventually master. The CDI phase of PCIT is thought to underpin changes in children’s internal working models, as parents are taught how to interpret their child’s cues and use positive parenting practices to facilitate warm and mutually responsive relationships (Timmer et al., 2011). 2.4 Rational Forty six percent of reception teachers now report that more than half of the pupils in their class were not ready for school (West, Denton, & Reaney, 2001). School readiness, defined as, emotional self-regulation, social competence, the absence of behaviour problems and parental involvement, plays a pivotal role in children’s future social and academic success (Ladd, Birch, & Buhs, 1999; Normandeau & Guay, 1998). Unfortunately, children with internalising disorders are at a heightened risk of exhibiting maladaptive emotional, social and behavioural difficulties that impede their ability to function productively within social and academic settings at school. The preschool period offers an early window of opportunity to offset potential long term and more intractable forms of psychopathology later in life. In fact, the neuroplasticity of the brain during this developmental period may serve to enhance robust treatment effects in this population (Luby, 2013). Early childhood interventions, such as PCIT, may also hold the potential to ameliorate long term Doctorate in Educational and Child Psychology Tamara Powell suffering, symptom impairment and reliance on psychotropic medication that carry risks and dangerous side effects for young children (Wagner, 2005). There is a growing body of evidence that highlights the importance of prevention and early intervention for childhood psychiatric disorders (DfES, 2001). In applied educational psychology practice, early interventions, including PCIT, can help reduce the number of permanent and fixed term exclusions and incidence of peer victimisation in schools. By building children’s resilience at a young age through secure early attachments and clear, firm and consistent disciplinary practices (DfE, 2015), students will also be more likely to establish healthy social relationships with peers and adults and consequently show higher levels of academic engagement and attainment. Psychosocial treatments for school aged children has been well-researched over the past 20 years, (Kendell, Furr, & Podell, 2010; Silverman, Pina & Viswesvaran, 2008), however, there is a paucity of work examining the treatment of anxiety and depression in early childhood. This may be due, in part, to the fact that empirically validated approaches to treating older children rely on higher cognitive capacities, such as thought monitoring, cognitive restructuring and mood identification, which have not yet developed in young children. PCIT circumvents this particular issue by focusing on reshaping the primary context within which development occurs (parent-child relationship), rather than working directly with children who lack the key metacognitive skills needed for treatment. Minor adjustments will likely be needed before PCIT can be implemented in the UK. Due to the intrusive nature of the intervention, it would be worthwhile to discuss with parents any personal boundaries that should be respected during treatment. Likewise, professionals should be mindful of their tone and directiveness when instructing parents, as it is imperative they feel like active agents in the problem solving process. 2.5 Review question How effective is PCIT and its various adaptations in reducing symptom severity in young children with internalising disorders? Doctorate in Educational and Child Psychology Tamara Powell 3. Critical Review of Evidence 3.1 Literature Search A comprehensive literature search was carried out between the dates of December 5th and 30th, 2014 to locate studies that were relevant to the research question. The literature search spanned three databases (PsycINFO, ERIC, MEDLINE) and used the search terms outlined in Table 1. The initial search, which was limited to the inclusion criteria summarised in Appendix 1, yielded 381 results (PsycINFO, n = 177; ERIC, n = 149; MEDLINE, n = 55). After removing 242 duplicates, the titles and abstracts of 127 studies were screened for eligibility, and a further 12 articles were examined through full text. On closer inspection, four papers were found to be review studies that did not report original empirical data and two focused on children with externalising behaviour problems (Appendix 2). Figure 2 depicts the entire screening process from the initial database searches to full article review and Table 2 identifies the six studies that were included in the final review. Table 1 Search Terms Applied Multifield Search Terms Parent child interaction therapy (abstract) and internal* (all fields) Parent child interaction therapy (abstract) and anxiety (all fields) PCIT (abstract) and anxiety (abstract) Parent child interaction therapy (abstract) and depression (all fields) PCIT (abstract) and depression (abstract) Parent child interaction therapy (abstract) and mood disorder* (all fields) Parent child interaction therapy (abstract) and inhibit* (all fields) Parent child interaction therapy (title) and internal* (all fields) Limits English language, peer reviewed, 2005current, human research English language, peer reviewed, 2005current, human research English language, peer reviewed, 2005current, human research English language, peer reviewed, 2005current, human research English language, peer reviewed, 2005current, human research English language, peer reviewed, 2005current, human research English language, peer reviewed, 2005current, human research English language, peer reviewed, 2005current, human research Doctorate in Educational and Child Psychology Multifield Search Terms Limits Parent child interaction therapy (title) and depression (all fields) Parent child interaction therapy (title) and mood disorder* (all fields) Parent child interaction therapy (title) and inhibit* (all fields) Parent child interaction therapy (title) and behavio*(title) PsycINFO n = 177 ERIC n = 149 Participants MEDLINE n = 55 TotalResearch n Design = 381 Control Group Tamara Powell English language, peer reviewed, 2005current, human research English language, peer reviewed, 2005current, human research English language, peer reviewed, 2005current, human research English language, peer reviewed, 2005current, human research Articles Identified Using Search Terms Papers Excluded by abstract: Inclusion criteria not met n = 127 Duplicates n = 242 Papers Full Text Reviewed Papers Excluded: Inclusion criteria 1b n = 4 Inclusion criteria 2b n = 2 Total Excluded n = 6 Included Papers n = 6 Figure 2. Application of inclusion and exclusion criteria. Doctorate in Educational and Child Psychology Tamara Powell Table 2 Studies Eligible for Review Included Studies Chase, R. M., & Eyberg, S. M. (2008). Clinical presentation and treatment outcome for children with comorbid externalizing and internalizing symptoms. Journal of Anxiety Disorders, 22(2), 273–82. Choate, M. L., Pincus, D. B., Eyberg, S. M., & Barlow, D. H. (2005). Parent-child interaction therapy for treatment of separation anxiety disorder in young children : A pilot study. Cognitive and Behavioral Practice,12(1),126–135. Comer, J. S., Puliafico, A. C., Aschenbrand, S. G., McKnight, K., Robin, J. A., Goldfine, M. E., & Albano, A. M. (2012). A pilot feasibility evaluation of the CALM program for anxiety disorders in early childhood. Journal of Anxiety Disorders, 26(1), 40–9. Lenze, S. N., Pautsch, J., & Luby, J. (2011). Parent-child interaction therapy emotion development: A novel treatment for depression in preschool children. Depression and Anxiety, 28(2), 153–9. Luby, J., Lenze, S., & Tillman, R. (2012). A novel early intervention for preschool depression: findings from a pilot randomized controlled trial. Journal of Child Psychology and Psychiatry and Allied Disciplines, 53(3), 313–22. 3.2 Evaluation Process This review is based on six papers that are delineated in Table 2. Included studies were critically evaluated using Harden and Gough’s (2012) ‘Weight of Evidence Framework’ (WoE; Table 3). This framework appraises studies on four dimensions: methodological quality, methodological relevance, relevance to the review question and overall assessment. Overall assessment, computed by averaging the WoE A, B and C, is particularly important because it provides a comprehensive measure that facilitates comparative inferences to be drawn (Table 4 and 5). Doctorate in Educational and Child Psychology Tamara Powell Table 3 Weight of Evidence Framework (Harden & Gough, 2012) Weight of Evidence A Methodological Quality The study’s methodological quality is judged against a generally accepted criteria. Weight of Evidence B - Methodological Relevance Weight of Evidence C- Relevance to the Review Question Review specific judgement about the appropriateness of the study design in answering the review question. Review specific judgment about the relevance of the type of evidence provided in relation to the review question. Weight of Evidence D Overall Assessment Averaged weight of evidence from sources A, B and C. Each study was coded using an adapted protocol from the Task Force on Evidence-Based Intervention in School Psychology (Kratochwill, 2003). An overall summary of each included paper and corresponding coding protocols can be found in Appendix 5 and 7, respectively. The weighting criteria and outcome scores for group and single based designs are also detailed in Appendix 3 and 4. Finally, Table 4 reports the results from WoE A, B, C and D for all six included studies. Table 4 Weighting of Evidence across the Four Scoring Dimensions Reviewed Study Chase & Eyberg (2008) Choate et al. (2005) Comer et al. (2012) Lenze et al. (2011) Luby et al. (2012) Pincus et al. (2008) WoE A WoE B Methodological Methodological Quality Relevance WoE C Relevance to the Review Question 1.8 1.0 1.0 0.8 1.0 1.0 1.2 1.0 3.0 1.8 1.0 2.0 1.8 3.0 3.0 1.0 1.0 1.0 WoE D Overall Assessment Low 1.3 Low 0.9 Med 1.7 Med 1.6 High 2.6 Low 1.0 Doctorate in Educational and Child Psychology Tamara Powell Table 5 Overall Weight of Evidence Overall Assessment Score (WoE D) High Medium Low Averaged Scores 2.5 or higher 1.5 to 2.4 1.4 or less 3.3 Critique and Appraisal of Studies 3.3.1 Participants A total of 131 children ages 3 to 8 years participated in the six reviewed studies. Children with depression were generally younger in age (preschool period), while children with anxiety related disorders spanned both the preschool and school age period. Gender was slightly skewed in favour of males (61%), and a much higher proportion of White children were included in four (Chase & Eyberg, 2008; Choate, Pincus, Eyberg & Barlow, 2005; Lenze, Pautsch, & Luby, 2011; Luby, Lenze & Tillman, 2012) out of the five studies that reported ethnicity and race. Families were also more likely to have high annual incomes (>60,000) and educational attainment (Lenze et al., 2011; Luby et al., 2012). With the exception of one study, all participants met criteria for a principle diagnosis of MDD (Egger & Angold, 2006) or a specific anxiety related disorder as judged by various DSM-IV screening measures (Appendix 5). Participants in Chase and Eyberg’s (2008) study displayed clinical levels of oppositional defiant disorder (ODD) and SAD, however, the primary diagnosis was not reported. Although participants were not concurrently receiving any other psychotherapies, several children in the PCIT-ED group were taking stable doses of psychotropic medication. Sample size varied across studies, as both group and single-based designs were included in the present review. In the group-based studies, stringent inclusion criterion and accessibility of low incidence populations impeded recruitment efforts. Consequently, only one (Chase & Eyberg, 2008) of the four papers employed a sufficiently large sample. Test sensitivities were therefore compromised in the remaining three papers (Lenze et al., 2011; Luby et al., 2012; Pincus, Santucci, Ehrenreich & Eyberg, 2005), which were all underpowered. Doctorate in Educational and Child Psychology Tamara Powell The level of parental involvement differed across papers. However, there was no evident group differences between single and co-parenting couples who participated in treatment. As seen in Table 4, overall WoE varied between low (Choate et al., 2005) and medium (Comer et al., 2012) ratings for studies that included both parents in all facets of treatment. Lastly, although the reviewed studies were carried out in an English speaking country (United States), there has been none to date conducted in the UK. Results should therefore be interpreted with caution, as cultural norms, legislation and educational systems differ between the two countries. 3.3.2 Research Design Two of the reviewed papers (Choate et al., 2005; Comer et al., 2012) used single-case experimental designs (SCED) to explore PCIT and CALM treatment effects. This design, however, was found to be poorly suited for the research question at hand. When examining methodological quality across both multiple baseline designs, it is apparent that symptom severity is ill-defined, and for this reason, measured at only 3 single time points across treatment. The inadequate amount of data is likely due to the fact that symptom severity, a broad concept that encompasses adverse changes in physical, emotional and social functioning (Kessler et al., 2002), is a very difficult operationalise, and therefore, overtly observe through time. Choate et al. (2005) consequently received an unclassified score of 0 for the quality of baseline and primary outcome measures, as there was an insufficient number of data points to judge the stability, overlap and trends in scores during the baseline and intervention time period. Comer et al. (2012) reported group averages for 9 participants at three different time points (baseline 1, baseline 2, and posttest) instead of showing three demonstrations of an experimental effect (Horner et al., 2005). The authors did not compute any statistical tests or provide sufficient data to allow independent calculations of significance. As such, the primary outcome rating could not be estimated using SCED or group experimental design (GED) guidelines, and it was in turn awarded no numerical ranking. Similar to Choate et al. (2005), this study also received an unclassified score of 0 for the quality of baseline because its short length precluded any conclusions regarding the level of the symptom severity in participants prior to treatment. Doctorate in Educational and Child Psychology Tamara Powell Within the GEDs, one randomised control trial study (RCT; Luby et al., 2012) offered the highest scores on all four weights of evidence. This strong weighting reflects the fact that Luby et al. (2012) employed an active comparison group, utilized multiple methods to assess symptom severity and randomly assigned participants to different experimental conditions. Two (Chase & Eyberg, 2008; Lenze et al., 2011) of the three remaining one-group pretest-posttest GEDs were also found to be methodologically sound (WoE A). In summary, GEDs methodology quality (WoE A) was found to be superior to SCEDs in measuring differences in symptom severity. Despite some efforts to increase experimental control through staggered start times (Choate et al., 2005; Comer et al., 2005), both SCED and GEDs received consistently low ratings on WoE B. Without a comparison group or within-participant control, one-group pretest posttest and multiple baseline designs face the inherent risk of having confounding variables influence participants’ symptom severity scores. 3.3.3. Intervention 3.3.3.1 PCIT Three studies (Chase & Eyberg, 2008; Choate et al., 2005; Pincus et al., 2008) examined the use of traditional PCIT in treating young children with SAD. The overall rating for each PCIT study was judged to be low and this ranking was shown to be largely consistent across WoE A, B and C. This low ranking can be attributed to a number of factors, including the lack of multi-sourced and multi-method data, poor methodological rigour and comparatively more participants with comorbid diagnoses. Further, children in Choate’s et al. (2005) study only participated in a total of 6 to 7 sessions, which is substantially shorter than the average 13-session length (Bell & Eyberg, 2002). Choate et al. (2005) and Pincus et al. (2008) also failed to stipulate whether neurological impairment, cognitive delay, psychotropic medication and family discord had been examined during the initial screening phase. Although, Chase and Eyberg’s (2008) study was appraised as being low on WoE B, C and D, it did show moderate evidence for methodological quality. A higher score on this dimension is probably due to longer treatment sessions (14 sessions), stringent inclusion criterion, high treatment fidelity, positive changes in diagnostic criteria and sufficiently large sample size. Doctorate in Educational and Child Psychology Tamara Powell 3.3.3.2 CALM Although the preliminary results of Comer’s et al. (2012) pilot study showed a moderate effect of treatment on children’s clinical outcome scores, the study failed to isolate the unique effects of the novel brave behaviour module (WoE A). There was, however, a high level of overall care taken to ensure positive outcomes, which included, a sufficiently long course of treatment (12 sessions), involvement of both parents and the administration of multiple assessment measures (WoE C). Such efforts resulted in a medium overall weight of evidence (WoE D). 3.3.3.3 PCIT-ED The strongest evidence in this review comes from Luby’s et al. (2012) RCT study examining the effects of PCIT-ED on preschool children with MDD. This study built on the previous work of Lenze et al. (2011) who examined PCIT-ED in a smaller sample of children using a one-group pretest posttest design. Both studies demonstrated a high fidelity to treatment, employed multiple assessment methods and offered clinically significant results (WoE A). 3.3.4 Measures Most studies (Choate et al., 2005; Comer et al., 2012; Pincus et al., 2008) utilised the Anxiety Disorder Interview Schedule – Child and Parent Version (ADISC/P) (Silverman & Albana, 1996) instrument to measure symptom severity in children with anxiety related disorders. The ADIS-C/P is a semi-structured diagnostic interview that uses the DSM-IV criteria to produce a clinician severity rating (CSR) score between 0 and 8 (> 4 indicates a clinical diagnosis). The inter-rater reliability for ADIS-C/P ranges between 0.65 and 0.88 (Silverman & Ollendick, 2005; Silverman, Saavedra & Pina, 2001), which is comparably higher than other more generic measures of SAD, such as the Diagnostic Interview Schedule for ChildrenParent Version (DISC-IV-P; retest reliability = 0.58; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000). Comer et al. (2012) also employed the Children’s Global Assessment Scale (CGAS; Shaffer et al., 1983) and Clinical Global Impression – Severity Scale (CGI-S) scores to measure the overall severity of child disturbance. However, the inter-rater reliability for CGAS is quite variable (0.62 to 0.99; Lavigne et al., 1995), and at present, reliability and validity for CGI-S has only been evaluated in samples of adults with dementia (Dahlke et al., 1992). Doctorate in Educational and Child Psychology Tamara Powell Preschool Age Psychiatric Assessment (PAPA Egger & Ascher, 1999), which assesses the intensity, frequencies, durations and first onsets of behaviour relevant to Axis 1 diagnoses on the DSM-IV, was the preferred diagnostic tool for preschoolers with MDD (Lenze et al., 2011; Luby et al., 2012). This is presumably because PAPA (test-retest reliability = 0.71; inter-rater reliability = 0.72) and other similar screening measures, such as Preschool Feelings Checklist (PFC; Cronbach’s alpha = 0.92; test-retest reliability = 0.82; Luby, Heffelfinger, Koenig-McNaught, Brown & Spitznagel, 2004) and Health and Behavior Questionnaire – Parent Version (HBQ-P; test-retest reliability = 0.88; Essex et al., 2002) show favourable psychometric properties. Aside from Comer’s et al. (2012) CALM study, there were no other anxiety related interventions that employed more than one measure to evaluate symptom severity in children. As a result, all traditional PCIT interventions scored low on WoE C and generally received low ratings (Chase & Eyberg, 2008; Choate et al., 2005) on the measurement item of WoE A. Notably poor reliability on Comer’s supplementary measures (CGAS and CGI-S) also effected this intervention’s (CALM) rating on WoE A (measurement). Interventions tailored for children with depression (PCIT-ED) that conversely used two (Lenze et al., 2011) or more (Luby et al., 2012) relevant outcome measures received medium (Lenze et al., 2011) to high (Luby et al., 2012) ratings on WoE C. Both PCIT-ED interventions were also awarded medium ratings on the measurement scale of WoE A, indicating such studies utilised sound evaluative tools. 3.3.5 Findings 3.3.5.1 Anxiety For the PCIT intervention, the results were mixed. Choate et al. (2005) and Chase and Eyberg (2008) found positive treatment effects, with high responder rates of 100% (3 out of 3) and 73% (11 out of 15), respectively. The majority of participants in Pincus et al. (2005) study, however, still met criteria for SAD at posttest (M = 4.2), and only marginal reductions (M = 1.6) were observed in participants CSR scores. Although this reduction resulted in a medium effect size, Doctorate in Educational and Child Psychology Tamara Powell there was no evidence to suggest PCIT made clinically relevant changes in participants’ symptom severity. Chase and Eyberg (2008) on the other hand, effectively demonstrated both statistical (large effect size) and clinical significance for most children with SAD and ODD in their sample. A large effect size was also found for all three participants in Choate’s et al. (2005) study. In Comer’s et al. (2012) intent to treat sample, there was an overall mean reduction of 2.8 (SD = 2.0) CSR points, which equated to a large effect size. Results indicate that children with SAD were the most responsive to treatment (75%), followed by social anxiety disorder (67%), GAD (50%) and specific phobia (0%). Large effect sizes and high response rates (e.g., improvement of 10 points on GCAS or scores lower than 3 on CGI-S) were similarly observed in the completers group for the CGAS (85.7%) and CGI-S (100%) measures. 3.3.5.2 Depression Positive changes in diagnostic profiles were reported in Lenze’s et al. (2011) study. Indeed, 5 out of the 7 participants (71%) showed subclinical levels of MDD at post-treatment and large effect sizes were noted for the PAPA MDD sum severity score and HBQ-P internalising symptom subscale. Luby et al. (2012) found a large effect size for PFC-S, however, the study reported a medium effect size for PAPA MDD and no effect for HBQ-P. Given the differences in sample size and design between the two studies, it’s more likely that the conservative estimates of PAPA MDD and HBQ-P provided by Luby et al. (2012) is closer to the population parameter. Table 6 provides an overview for the aforementioned effect sizes. Caution needs to be exercised, however, when interpreting these results. Importantly, the low overall weights of evidence for all traditional PCIT interventions (e.g., only covering the CDI and PDI modules) undermine the large (Choate et al., 2005) and medium effect sizes (Chase & Eyberg, 2008; Pincus et al., 2008) reported in the current review. Greater weight should instead be assigned to those interventions such as CALM (Comer et al., 2012) and PCIT-ED (Lenze et al., 2011; Luby et al., 2012) that received higher overall weights of evidence. Further, small sample sizes (Choate et al., 2005; Comer et al., 2012; Lenze et al., 2011; Luby et al., 2012; Pincus et al., 2008), which carry higher error rates and lower power may bias the obtained results. It should also be noted that effect sizes were calculated using different evaluative Doctorate in Educational and Child Psychology Tamara Powell frameworks (Becker, 1988; Morris, 2007). Comparative inferences, should therefore, be avoided between studies with and without a comparison group. Doctorate in Educational and Child Psychology Tamara Powell Table 6 Effect Size and Overall Quality Ratings Study Intervention & Programme Modules Design Outcomes Measure(s) Population Effect Size Descriptors Effect Size n Overall Weight of Evidence Chase & Eyberg (2008) PCIT – CDI and PDI GED – One group pretest posttest design Group x time interaction, with significant decreases in symptom severity in the SAD only group at posttest. Diagnostic Interview Schedule for Children was administered to child’s female caregiver. (DISC-IV-P) Anxiety Medium PPC SMD = 1.48 58 Low Choate et al. (2005) PCIT– CDI and PDI SCED – Multiple baseline design Clinical severity ratings for SAD decreased to subclinical levels at posttest and remained in the normative range at follow up. Anxiety Disorders Interview Schedule for DSM-IV – Child and Parent Versions. (ADISC/P) Anxiety Large Participant 1de Posttest: PP SMD = 1.29 Follow up: PP SMD = 1.29 3 Low Large Participant 2de Posttest PP SMD = 1.71 Follow up: PP SMD = 1.71 Large Participant 3de Posttest PP SMD = 1.29 Follow-up: PP SMD = 0.86 Doctorate in Educational and Child Psychology Study Comer et al. (2012) Intervention & Programme Modules Design Outcomes Measure(s) CALM – CDI and brave behaviour (exposure therapy) SCED – Multiple baseline design A diagnostic response was observed in 75% of SAD, 67% of social anxiety, 50% of GAD and 0% of specific phobia participants. Anxiety Disorders Interview Schedule for DSM-IV – Parent Version (ADISC-P) On average, global severity scores improved from “moderately” and “markedly” ill to “normal” “not at all ill” and “borderline ill.” Lenze et al. (2011) Tamara Powell PCIT-ED– CDI, PDI and Emotion Development GED – One group pretest posttest design Significant decline in depression severity scores following treatment. Effect Size n Overall Weight of Evidence Largea PP SMD = 1.26de 9 Medium Children’s Global Assessment Scale (CGAS) Largeb PP SMD = 1.64de 7 Clinical Global Impression Severity and Improvement Scales (CGI-S) Largeb PP SMD = 2.26de 7 Large PP SMD =1.19d 8 Large PP SMD =0.82d 8 Preschool Age Psychiatric Assessment (PAPA MDD) Health and Behavior Questionnaire – Internalising Symptoms Subscale (HBQ-P) Population Anxiety Depression Effect Size Descriptors Medium Doctorate in Educational and Child Psychology Study Luby et al. (2012) Pincus et al. (2008) Intervention & Programme Modules Design PCIT-ED – CDI, PDI and Emotion Development GED – Between subjects randomis ed pretest posttest design PCIT– CDI and PDI GED – One group pretest posttest design Outcomes Tamara Powell Measure(s) Effect Size Descriptors Effect Size Medium Preschool Feelings Checklist-Scale (PFC-S) Health and Behavior Questionnaire – Internalising Symptoms Subscale (HBQ-P) Significant decreases in symptom severity as measured by the PFC-S and HBQ-P in both experimental conditions. PAPA MDD conversely only found significant changes in the PCIT-ED group. Preschool Age Psychiatric Assessment (PAPA MDD) SAD symptomatology decreased after treatment, however, most scores remained in the clinical range. Anxiety Disorders Interview Schedule for DSM-IV – Child and Parent Versions (ADIS-C/P) Population Depression Anxiety n Overall Weight of Evidence PPC SMD = 0.50 42 High Large PPC SMD = 0.83 43 No effect PPC SMD = 0.00 40 Mediumc PP SMD = 0.73d 10 Low Notes: Effect size, referred to as Pretest-Posttest Standard Mean Difference (PP SMD; Becker, 1988), was calculated by dividing the difference in means by the pretest standard deviation score (Choate et al., 2005; Comer et al., 2012; Lenze et al., 2011; Pincus et al., 2008). In Chase and Eyberg (2008) and Luby’s et al. (2012) study, effect size (Pretest-Posttest-Control Standard Mean Difference; PPC SMD) was calculated by dividing the difference in means (pre and post treatment) by the pooled standard deviation (Hedge’s g; Morris, 2007). Doctorate in Educational and Child Psychology Tamara Powell a) To reduce potential sampling biases, statistical analyses was performed on the intent to treat sample. b) Data could not be obtained for the intent to treat sample, so effect size was computed using the completers sample. c) Standard deviation for measure was not reported, it was, therefore, computed using a sample of children with comparable demographics (Comer et al., 2012). d) Effect sizes were corrected in accordance to Hedges’ (1981) guidelines for small samples (e.g., groups with 10 or less participants; Becker, 1988). e) Choate et al. (2005) examined the impact of treatment on children’s symptomatology on an individual basis, whereas Comer et al. (2012) explored pre-post treatment differences using group means. To maintain consistency, the current review reported individual effect sizes at the two phases of treatment in Choate’s et al. (2005) study, and group level effect sizes between baseline and post-treatment for participants in Comer’s et al. (2012) SCED paper. Key: ODD- oppositional defiant disorder; SAD- separation anxiety disorder; ADHD- attention deficit hyperactive disorder; CD- conduct disorder; MDD- major depressive disorder; GAD- generalised anxiety disorder; OCD-obsessive compulsive disorder. Effect Size Descriptors (Cohen, 1988 Effect Size Descriptor Small Medium Large Cohen’s d 0.20 0.50 0.80 Doctorate in Educational and Child Psychology Tamara Powell 3.4 Conclusions Interventions that assign individual modules to problem specific behaviour were found to be stronger than treatment that targets symptomatology within a broader and widely applicable framework, such as traditional PCIT. For instance, in CALM children face personally relevant fears in a continually graded format during the brave behaviour module. The ED module in PCIT-ED similarly focuses on concurrently improving parent and child emotional competence through exercises that centre on emotional regulation and recognition. It is therefore not surprising that interventions, such as PCIT, that rely solely on Child-Directed Interaction (CDI) and Parent-Directed Interaction (PDI), consistently scored low on all weights of evidence. In fact, there were no detrimental effect found from removing the PDI module all together from treatment (Comer et al., 2012). This module may be more applicable to externalising disorders for which it was originally intended or better situated within designs that focus more extensively on the child’s underlying symptoms (e.g., PCITED). The first pilot study of CALM showed promising results in reducing symptom severity in children with a host of anxiety related disorders. However, a larger RCT study is required prior to drawing any conclusions with regard to treatment efficacy. A number of methodological constraints limit the extent to which results arising from this study and others within the PCIT tradition can be generalised to other children presenting similar issues. It is for these reasons, PCIT-ED is the only intervention that is being recommended for use in a clinical pre-school population with MDD. In practice, educational psychologists (EP) could work closely alongside other agencies, such as CAMHS, to deliver, support and maintain progress achieved through PCIT-ED. In schools, EPs could also liaise with staff to teach the behavioural approaches provided to parents in sessions to ensure consistency between the two settings. Finally, EPs may work in homes with parents to evaluate short and long term gains of the programme and to troubleshoot issues as they arise. 3.5 Limitations The findings from this review should be interpreted in light of its limitations. Firstly, the majority of reviewed studies lacked sufficient power to detect changes in Doctorate in Educational and Child Psychology Tamara Powell treatment because of inadequate sample sizes. Secondly, all studies primarily rely on parent reports, which carry many inherent biases. Although it was not appropriate or feasible to obtain supplementary self-report data because of the child’s age, observational data and teacher reports could have triangulated the obtained results. Thirdly, experimental control was low across multiple baseline and one-group pretest posttest study designs. Therefore, changes in symptom severity cannot be attributed to treatment alone, as regression to the mean, maturation and or expectancy effects could have influenced the outcome variable. Lastly, interventions took place in a contrived and highly controlled setting (university clinic) and despite some small scale efforts to generalise obtained results to the home environment (e.g., daily homework assignments) ecological validity was low. 3.6 Recommendations for Future Research Future research should examine the different dimensions of symptom severity in greater detail. Specifically with respect to what items on the DSM-IV criteria are the most and least resistant to treatment. An in depth analysis of symptoms and age should also be examined in tandem, as there is some preliminary evidence to suggest older children did not benefit from treatment to the same extent as younger children (Comer et al., 2012; Lenze et al., 2011; Luby et al., 2012). Higher response rates in children with SAD relative to other anxiety related disorders also signals a strong need for research to focus on underrepresented subpopulations that have not garnered much attention to date. Knowledge gained from this research can in turn guide more targeted treatment efforts for children who present different diagnostic profiles. As a final note, it would be remiss not to further examine the individual contributions of different programme components (e.g., CDI, PDI, ED, brave behaviours), which were largely neglected in the current review. Future work should evaluate which programme modules, and in which order and combination, have the greatest influence in improving both short term and long term symptomatology. Doctorate in Educational and Child Psychology Tamara Powell References Allen, B., Timmer, S. G., & Urquiza, A. J. (2014). Parent–child interaction therapy as an attachment-based intervention: Theoretical rationale and pilot data with adopted children. Children and Youth Services Review, 47, 334-341. American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author. Bandura, A. (1977). Social learning theory. Englewood Cliffs, NJ: Prentice Hall. Becker, B. J. (1988). Synthesizing standardized mean change measures. British Journal of Mathematical and Statistical Psychology, 41, 257-278. . Bell, S. K., & Eyberg, S. M. (2002). Parent-child interaction therapy: A dyadic intervention for the treatment of young children with conduct problems. Innovations in Clinical Practice: A Source Book, 20, 57-74. Bowlby, J. (1978). Attachment theory and its therapeutic implications. Adolescent Psychiatry, 6, 5-33. Brinkmeyer, M. Y., & Eyberg, S. M. (2003). Parent-child interaction therapy for oppositional children. In A. E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents (pp. 204-223). New York: The Guilford Press. Cassidy, J., & Kobak, R. R. (1988). Avoidance and its relation to other defensive processes. In J. Belsky, & T. Nezworski (Eds.), Clinical implications of attachment (pp. 300-323). Hillsdale, NJ: Erlbaum. Chase, R. M., & Eyberg, S. M. (2008). Clinical presentation and treatment outcome for children with comorbid externalizing and internalizing symptoms. Journal of Anxiety Disorders, 22(2), 273–82. Choate, M. L., Pincus, D. B., Eyberg, S. M., & Barlow, D. H. (2005). Parent-child interaction therapy for treatment of separation anxiety disorder in young children : A pilot study. Cognitive and Behavioral Practice,12(1),126–135. Cohen, J. (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Earlbaum Associates. Doctorate in Educational and Child Psychology Tamara Powell Comer, J. S., Puliafico, A. C., Aschenbrand, S. G., McKnight, K., Robin, J. A., Goldfine, M. E., & Albano, A. M. (2012). A pilot feasibility evaluation of the CALM program for anxiety disorders in early childhood. Journal of Anxiety Disorders, 26(1), 40–9. Dahlke, F., Lohaus, A. & Gutzmann, H. (1992). Reliability and clinical concepts underlying global judgments in dementia: Implications for clinical research. Psychopharmacological Bulletin, 28, 425–432. Department for Education and Skills (DfES). (2001). Promoting children’s mental health within early years and school settings. London: DfES. Department for Education. (2015). Mental health and behaviour in schools: Departmental advice for school staff. London: DfE. Egger, H., & Angold, A. (2006). Common emotional and behavioral disorders in preschool children: Presentation, nosology, and epidemiology. Journal of Child Psychology and Psychiatry, 47, 313–337. Essex, M. J., Boyce, W. T., Goldstein, L. H., Armstrong, J. M., Kraemer, H. C., & Kupfer, D. J. (2002). The confluence of mental, physical, social, and academic difficulties in middle childhood. II: Developing the macarthur health and behavior questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry, 41(5), 588–603. Eyberg, S. M. (2005). Tailoring and adapting parent–child interaction therapy to new populations. Education and Treatment of Children, 28(2),197–201. Eyberg, S. M., & Members of the Child Study Laboratory. (1999). Parent-child interaction therapy integrity checklists and session materials. Retrieved October 20, 2005, from University of Florida, PCIT Laboratory Website: http//www.pcit.org. Gallagher, N. (2003). Effects of parent-child interaction therapy on young children with disruptive behavior disorders. Bridges: Practice-Based Research Syntheses, 1(4), 1–17. Doctorate in Educational and Child Psychology Tamara Powell Gonzales, N. A., Pitts, S. C., Hill, N. E., & Roosa, M. W. (2000). A mediational model of the impact of interparental conflict on child adjustment in a multiethnic, lowincome sample. Journal of Family Psychology, 14, 365–379. Guyatt, G. H., Sackett, D. L., Sinclair, J. C., Hayward, R., Cook, D. J., Cook, R. J., Bass, E., Gerstein, H., Haynes, B., Holbrook, A., Jaeschke, R., Laupacls, A., Moyer, V., & Wilson, M. (1995). Users' guides to the medical literature: IX. A method for grading health care recommendations. Journal of the American Medical Association, 274(22), 1800-1804. Harden, A. & Gough, D., 2012. Quality and relevance appraisal. In D. Gough, S. Oliver & J. Thomas (Eds.), An introduction to systematic reviews (pp. 153178). London: Sage. Hedges, L. V. (1981). Distribution theory for Glass’s estimator of effect size and related estimators. Journal of Educational Statistics, 6,107–128. Hembree-Kigin, T. L., & McNeil, C. B. (1995). Parent-child interaction therapy. New York: Plenum Press. Herschell, A. D., Calzada, E. J., Eyberg, S. M., & McNeil, C. B. (2002). Clinical issues in parent-child interaction therapy. Cognitive and Behavioral Practice, 9, 16-27. Horner, R., Carr, E., Halle, J., Mcgee, G., Odom, S., & Wolery, M. (2005). The use of single-subject research to identify evidence-based practice in special education. Exceptional Children, 71(2), 165-179. Jacobson, N.S., Follette, W.C., & Revenstorf, D. (1984). Psychotherapy outcome research: Methods for reporting variability and evaluating clinical significance. Behavior Therapy, 15(4), 336-352. Kendall, P. C., Furr, J. M., & Podell, J. L. (2010). Child-focused treatment of anxiety. In J. R. Weisz A.E. Kazdin (Eds.), Evidence-based psychotherapies for children and adolescents second edition (pp. 45-60). New York, NY: Guilford Press. Kessler, R. C., Andrews, G., Colpe, L. J., Hiripi, E., Mroczek, D. K., Normand, S. L. T., Walters, E. E. & Zaslavsky, A. M. (2002). Short screening scales to Doctorate in Educational and Child Psychology Tamara Powell monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine, 32, 956-976. Kratochwill, T. R. (2003). Evidence-Based Practice: Promoting Evidence-Based Interventions in School Psychology. School Psychology Quarterly, 18(4), 389408. Ladd, G. W., Birch, S., & Buhs, E. (1999). Children’s social and scholastic lives in kindergarten: Related spheres of influence? Child Development, 70, 1373– 1400. Lavigne, J. V., Arend, R., Rosenbaum, D, Sinacore, J., Cincchetti, C., Binns, H. J., Kaufer Christoffel, K., Hayford, J. R., & McGuire, P. (1994), Interrater reliability of the DSM-III-R with preschool children. Journal of Abnormal Child Psychology, 22, 679-690. Lenze, S. N., Pautsch, J., & Luby, J. L. (2011). Parent-child interaction therapy emotion development: a novel treatment for depression in preschool children. Depression and Anxiety, 28(2), 153–9. Luby, J. L. (2013). Treatment of anxiety and depression in the preschool period. Journal of the American Academy of Child and Adolescent Psychiatry, 52(4), 346-358. Luby, J. L., Lenze, S. N., & Tillman, R. (2012). A novel early intervention for preschool depression: Findings from a pilot randomized controlled trial. Journal of Child Psychology and Psychiatry and Allied Disciplines, 53(3), 313– 22 Normandeau, S., & Guay, F. (1998). Preschool behavior and first-grade school achievement: The mediational role of cognitive self-control. Journal of Educational Psychology, 90, 111–121. Morris, S. B. (2007). Estimating effect sizes from the pretest-posttest-control group designs. Organizational Research Methods, 11, 364-386. Patterson, G. R., Capaldi, D., & Bank, L. (1991). An early starter model for predicting delinquency. Paper presented at the Earlscourt Conference on Childhood Aggression, Toronto, Canada, Jun 1988. Lawrence Erlbaum Associates, Inc. Doctorate in Educational and Child Psychology Tamara Powell Pincus, D. B., Santucci, L. C., Ehrenreich, J. T., & Eyberg, S. (2008). The implementation of modified parent-child interaction therapy for youth with separation anxiety disorder. Cognitive and Behavioural Practice, 15(2), 118125. Puliafico, A. C., Comer, J. S., & Albano, A. M. (2013). Coaching approach behavior and leading by modeling: Rationale, principles, and a session-by-session description of the CALM program for early childhood anxiety. Cognitive and Behavioral Practice, 20(4), 517-528. Shaffer, D., Fisher, P., Lucas, C.P., Dulcan, M. K., & Schwab-Stone, M. E. (2000). NIMH diagnostic interview schedule for children version IV (NIMH DISC-IV): Description, differences from previous versions, and reliability of some common diagnoses. Journal of American Academy Child Psychiatry, 39, 28– 38. Silverman, W. K., & Albano, A. M. (1996). The Anxiety Disorders Interview Schedule for DSM- IV-Child and Parent Versions. London: Oxford University Press. Silverman, W. K., & Nelles, W. B. (1988). The anxiety disorders interview schedule for children. Journal of the American Academy of Child and Adolescent Psychiatry, 7, 772-778. Silverman, W. K., & Ollendick, T. H. (2005). Evidence-based assessment of anxiety and its disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 34, 380–411. Silverman, W. K., Pina, A. A., & Viswesvaran, C. (2008). Evidence-based psychosocial treatments for phobic and anxiety disorders in children and adolescents. Journal of Clinical Child and Adolescent Psychology, 37, 105130. Silverman, W. K., Saavedra, L. M., & Pina, A. A. (2001). Test–retest reliability of anxiety symptoms and diagnoses with the anxiety disorders interview schedule for DSM-IV: Child and parent versions. Journal of the American Academy of Child and Adolescent Psychiatry, 40, 937–944. Doctorate in Educational and Child Psychology Tamara Powell Skinner, B. F. (1938). The behavior of organisms: An experimental analysis. New York: Appleton-Century. Stormont, M. (2002). Externalizing behavior problems in young children: Contributing factors and early intervention. Psychology in the Schools, 39, 127-138. Timmer, S. G., Ho, L. K. L., Urquiza, A. J., Zebell, N. M., Garcia, E. F., & Boys, D. (2011). The effectiveness of parent–child interaction therapy with depressive mothers: The changing relationship as the agent of individual change. Child Psychiatry and Human Development, 42,406–423. Wagner, K.D. (2005). Pharmacotherapy for major depression in children and adolescents. Progress in Neuro-Psychopharmacology and Biological Psychiatry, 29, 819–826. West, J., Denton, K., & Reaney, L. M. (2001). The kindergarten year: Findings from the early childhood longitudinal study, kindergarten class of 1998–1999 (Publication No. NCES2001-023). Washington, DC: Department of Education, National Center for Education Statistics. Whaley, S.E., Pinto, A., & Sigman, M. (1999). Characterizing interactions between anxious mothers and their children. Journal of Consulting and Clinical Psychology, 67, 826-836. Doctorate in Educational and Child Psychology Tamara Powell Appendix 1 Inclusion and Exclusion Criteria Inclusion Criteria 1. Publication Type a) Full length papers in a peer-reviewed journal. Exclusion Criteria Rational Material not in a peer reviewed journal (e.g., abstracts, book chapters, conference proceedings, dissertations). The peer review process ensures a higher level of methodological rigour. b) Studies containing primary empirical data. Studies that do not contain primary empirical data (e.g., literature reviews, metaanalysis and opinion papers). To ensure originality of findings. c) Studies written in English. Studies written in a language other than English. Translation services were not available. 2. Participants and Setting a) Children between the ages of 3 and 8 years. Infants younger than 3 years of age, and children older than 8 years of age. There is empirical evidence to support a clinical depression syndrome in children as young as 3 years of age (Egger & Angold, 2006; Luby et al., 2013). Similarly, various forms of childhood anxiety begin to emerge after 2.5 years of age (APA, 2000). This cohort of young children also require different types of treatment than older children with higher cognitive abilities. b) Children with internalising disorders, including anxiety and other mood disorders. -Children with major medical or neurological disease; pervasive developmental disorder; who have been adopted or subjected to and/or at risk of abuse. Participants exclusively presenting externalising behaviour problems in absence of any internalising disorders. -Family discord can place children at a heightened risk for an attachment disorder and cause socioemotional delays that could impact the efficacy of treatment. -Externalising behaviour problems are often present in children with internalising disorders, however, the former group represents a distinct population with different clinical needs. -Children with medical issues and/or developmental delays may have neurobiological differences from the target population. c) Children not undergoing concurrent intervention(s). Children engaged in more than one form of psychotherapy or on unstable doses of psychotropic medication. These confounding variables can influence the effect treatment has on symptom severity. Doctorate in Educational and Child Psychology Inclusion Criteria 3. Dependent Variables The study measures the efficacy of PCIT in relation to the child’s internalising symptoms. 4. Analysis The study reports means, standard deviations, test statistic(s) and/or data that allows for these measures to be computed. 5. Year of Publication Study was published after 2005. Exclusion Criteria The study does not measure the efficacy of PCIT in relation to the child’s internalising symptoms. Tamara Powell Rational Ensures papers directly relates to the research question at hand. The study does not report data that allows for means, standard deviations and/or test statistic(s) to be computed. These measures are required in the computation of effect size. Study was published prior to 2005. PCIT adaptions for internalising disorders were published in 2005 (Eyberg, 2005). Doctorate in Educational and Child Psychology Tamara Powell Appendix 2 Excluded Articles from PsycINFO, ERIC and MEDLINE 1 Studies Carpenter, A. L., Puliafico, A. C., Kurtz, S. M. S., Pincus, D. B., & Comer, J. S. (2014). Extending parent–child interaction therapy for early childhood internalizing problems: New advances for an overlooked population. Clinical Child and Family Psychology Review, 17(4), 340-356. Rational for Exclusion Criteria 1b – Paper does not report primary empirical data. 2 Kohlhoff, J., & Morgan, S. (2014). Parent-child Criteria 2b – interaction therapy for toddlers: A pilot study. Child & Participants have Family Behavior Therapy, 36(2), 121–139. been selected on the basis of externalising behaviour problems. 3 Pincus, D. B., Eyberg, S. M., & Choate, M. L. (2005). Adapting parent-child interaction therapy for young children with separation anxiety disorder, Education and Treatment of Children, 28(2), 163– 181. Criteria 1b – Paper does not report primary empirical data. 4 Puliafico, A. C., Comer, J. S., & Albano, A. M. (2013). Coaching approach behavior and leading by modeling: Rationale, principles, and a session-bysession description of the CALM program for early childhood anxiety. Cognitive and Behavioral Practice, 20(4), 517–528. Criteria 1b – Paper does not report primary empirical data. 5 Puliafico, A. C., Comer, J. S., & Pincus, D. B. (2012). Adapting parent-child interaction therapy to treat anxiety disorders in young children. Child and Adolescent Psychiatric Clinics of North America, 21(2), 607-619. Criteria 1b – Paper does not report primary empirical data. 6 Timmer, S. G., Ho, L. K. L., Urquiza, A. J., Zebell, N. M., Garcia, E. F., & Boys, D. (2011). The effectiveness of parent–child interaction therapy with depressive mothers: The changing relationship as the agent of individual change. Child Psychiatry and Human Development, 42(4), 406-423. Criteria 2b – Participants have been selected on the basis of externalising behaviour problems. Doctorate in Educational and Child Psychology Tamara Powell Appendix 3 Weighting of Studies 1. Weight of Evidence A: Methodological Quality A. Group Based Design: Randomised Control Studies and Quasi Experimental Designs Key Features Measurement High Rating (3) Instruments produce a reliability of 0.85 or higher and data is collected using multiple methods and from multiple sources for all primary outcomes. Medium Rating (2) Instruments produce a reliability of 0.70 or higher and data is collected either using multiple methods and/or from multiple sources for at least 75% of the primary outcomes. Low Rating (1) Instruments produce a reliability of 0.50 or higher for at least 50% of the primary outcomes. No Rating (0) Instruments produce reliability lower than 0.50 and/or data was not collected using multiple methods and/or from multiple sources. Comparison Group Inclusion of at least one “active” comparison group, group equivalency, counterbalanced change agents, equivalent mortality and low attrition at post-treatment. Inclusion of a “no intervention group” comparison group, as well as at least two of the following criteria: 1) Counterbalancing change agents 2) Group equivalence 3) Equivalent mortality with low attrition (Intent to Intervene must have been conducted in cases where this is not demonstrated). No efforts were made to ensure group equivalence. Primary Outcomes Appropriate units of analyses used, familywise/ experiment-wise error rate (if applicable) is controlled and there is a sufficiently large N. Also, significant outcomes must be shown for at least 75% of the total primary outcome measures for each key construct, with moderate effect sizes. Appropriate units of analyses used, familywise/ experimentwise error rate (if applicable) is controlled and there is a sufficiently large N. Also, significant outcomes must be shown for at least 50-75% of the total primary outcome measures for each key construct. At least one of the following: 1) Counterbalancing change agents 2) Group equivalence 3) Equivalent mortality with low attrition (Intent to Intervene must have been conducted in cases where this is not demonstrated). OR a comparison group for studies with no group equivalence procedures. Appropriate units of analyses used and familywise/ experimentwise error rate (if applicable) is controlled. Also, significant outcomes must be shown for at least 25-49% of the total primary outcome measures for any key construct. None of the outlined criteria were met. Doctorate in Educational and Child Psychology Tamara Powell Key Features Educational/ Clinical Significance High Rating (3) At least 3 of the 4 criteria is met at post-treatment or follow-up: 1) Categorical diagnosis data 2) Outcomes assessed by continuous variables 3) Subjective evaluation 4) Social comparison Medium Rating (2) At least 2 of the 4 criteria is met during post or follow-up: 1) Categorical diagnosis data 2) Outcomes assessed by continuous variables 3) Subjective evaluation 4) Social comparison Low Rating (1) At least 1 of the 4 criteria is met during post or follow-up: 1) Categorical diagnosis data 2) Outcomes assessed by continuous variables 3) Subjective evaluation 4) Social comparison No Rating (0) None of the outlined criteria were met. Identifiable Components Study shows strong evidence (score = 3) for significant primary outcomes, uses a design that isolates specific programme components and an analyses that demonstrates all components were necessary to produce change in the primary outcome variable. Study shows promising evidence (score = 2) for significant primary outcomes, uses a design that isolates specific programme components and an analyses that demonstrates at least 50% of the components were necessary to produce change in the primary outcome variable. Study shows weak evidence (score = 1) for significant primary outcomes, use a design that isolates specific programme components and an analyses that demonstrates at least 25% of the components were necessary to produce change in the primary outcomes. No evidence of which programme components were necessary to produce change. Implementation Fidelity At least 2 of the 3 criteria is met: 1) Ongoing supervision/consultation 2) Coding sessions 3) Audio/video tapes AND the use of a manual. If any adaptations are made they should be described in detail. At least 1 of the 3 criteria is met: 1) Ongoing supervision/consultation 2) Coding sessions 3) Audio/video tapes AND the use of a manual. At least 1 of the 3 criteria is met: 1) Ongoing supervision/consultation 2) Coding sessions 3) Audio/video tapes OR the use of a manual. No efforts were made to ensure implementation fidelity. Doctorate in Educational and Child Psychology Tamara Powell B. Single-Participant Design: Multiple Baseline Design Across Participants Key Features Measurement High Rating (3) For primary outcomes, instruments produce a reliability of 0.85 or higher, data is collected using multiple methods and from multiple sources and a case for the validity is made. Medium Rating (2) For primary outcomes, instruments produce a reliability of 0.85 or higher and data is collected using multiple methods and from multiple sources. Low Rating (1) For primary outcomes, instruments produce a reliability of 0.70 or higher. No Rating (0) Instruments produce reliability lower than 0.70 and/or data was not collected using multiple methods and/or from multiple sources. Overall Rating for Quality of Baseline At least 4 of the 5 criteria is met for each primary outcome: 1) Minimum of 3 baseline points 2) Stability of scores across baseline phase(s) 3) Baseline and intervention scores do not overlap 4) Behaviour problem(s) is evident 5) Dependent variable does not systematically increase or decrease At least 3 of the 5 criteria is met for each primary outcome: 1) Minimum of 3 baseline points 2) Stability of scores across baseline phase(s) 3) Baseline and intervention scores do not overlap 4) Behaviour problem(s) is evident 5) Dependent variable does not systematically increase or decrease At least 2 of the 5 criteria is met for each primary outcome: 1) Minimum of 3 baseline points 2) Stability of scores across baseline phase(s) 3) Baseline and intervention scores do not overlap 4) Behaviour problem(s) is evident 5) Dependent variable does not systematically increase or decrease No evidence or unknown/insufficient data reported. Visual analysis shows a large change in behaviour during the intervention stage, AND 3 of the 4 following criteria: 1) No-to-minimal overlap between the baseline and intervention phases 2) Clear trend reversal 3) Adequate phase length 4) Stable data Visual analysis shows a moderate to large change in behaviour during the intervention stage, AND 2 of the 4 following criteria: 1) No-to-minimal overlap between the baseline and intervention phases 2) Clear trend reversal 3) Adequate phase length 4) Stable data Visual analysis shows a moderate change in behaviour during the intervention stage, AND 1 of the 4 following criteria: 1) No-to-minimal overlap between the baseline and intervention phases 2) Clear trend reversal 3) Adequate phase length 4) Stable data No change in behaviour and either one or none of the listed criteria were met. Mean Rating Across Participants Overall Rating for Primary Outcomes; Mean Rating Across Participants Doctorate in Educational and Child Psychology Tamara Powell Key Features Educational/ Clinical Significance High Rating (3) At least 3 of the 4 criteria is met during post-treatment or follow-up: 1) Categorical diagnosis data 2) Outcomes assessed by continuous variables 3) Subjective evaluation 4) Social comparison Medium Rating (2) At least 2 of the 4 criteria is met during post- treatment or followup: 1) Categorical diagnosis data 2) Outcomes assessed by continuous variables 3) Subjective evaluation 4) Social comparison Low Rating (1) At least 1 of the 4 criteria is met during post- treatment or follow-up: 1) Categorical diagnosis data 2) Outcomes assessed by continuous variables 3) Subjective evaluation 4) Social comparison No Rating (0) None of the outlined criteria were met. Identifiable Components Study shows strong evidence (score = 3) for significant primary outcomes, uses a design that isolates specific programme components and an analyses that demonstrates all components were necessary to produce change in the primary outcome variable. Study shows promising evidence (score = 2) for significant primary outcomes, uses a design that isolates specific programme components and an analyses that demonstrates at least 50% of the components were necessary to produce change in the primary outcome variable. Study shows weak evidence (score = 1) for significant primary outcomes, use a design that isolates specific programme components and an analyses that demonstrates at least 25% of the components were necessary to produce change in the primary outcome variable. Components were not provided or none of the criteria was met. Overall Rating for Fidelity At least 2 of the 3 criteria is met: 1) Ongoing supervision/consultation 2) Coding sessions 3) Audio/video tapes AND the use of a manual. If any adaptations are made they should be described in detail. At least 1 of the 3 criteria is met: 1) Ongoing supervision/consultation 2) Coding sessions 3) Audio/video tapes AND the use of a manual. At least 1 of the 3 criteria is met: 1) Ongoing supervision/consultation 2) Coding sessions 3) Audio/video tapes OR the use of a manual. No efforts were made to ensure implementation fidelity. Mean Rating Across Participants Doctorate in Educational and Child Psychology Tamara Powell Overall Methodological Quality Score Overall methodological quality was computed by adding the weight of evidence from the aforementioned variables (e.g., assigning 3 for “high”, 2 for “medium”, 1 for “low” and 0 for “no evidence”) and dividing by a sum of six (or less in cases with no numerical rating). Averaged scores equate to the following ranking: Overall Methodological Quality (WoED) High Medium Low Averaged Scores 2.5 or higher 1.5 to 2.4 1.4 or less A. Group Based Design: Randomised Control Studies and Quasi Experimental Designs Study Chase & Eyberg (2008) Lenze et al. (2011) Luby et al. (2012) Pincus et al. (2008) Measures Comparison Group Primary Outcomes Educational/ Clinical Significance Identifiable Components Fidelity 1.0 NNR 3.0 2.0 0.0 3.0 2.0 NNR 1.0 3.0 0.0 3.0 2.0 2.0 1.0 2.0 0.0 3.0 2.0 NNR NNR 1.0 0.0 1.0 Overall Quality Med 1.8 Med 1.8 Med 1.7 Low 1.0 Doctorate in Educational and Child Psychology Tamara Powell A. Single-Participant Design: Multiple Baseline Design Across Participants Study Choate et al. (2005) Comer et al. (2012) Measures Quality of Baseline Primary Outcomes Educational/ Clinical Significance Identifiable Fidelity Components 1.0 0.0 0.0 2.0 0.0 2.0 1.0 0.0 NNR 2.0 0.0 3.0 Overall Quality Low 0.8 Low 1.2 Key: NNR- no numerical value 2. Weight of Evidence B: Methodological Relevance Weighting Description High Rating (3) GEDs: Random assignment of participants to a control or experimental group to establish group equivalence. Study also compares programme outcomes with an “active” comparison group pre and post treatment. SCEDs: High level of experimental control (more than three demonstrations of the experimental effect and controls for common threats to validity) and strong baseline data (minimum of five measurements). Medium Rating (2) Low Rating (1) GEDs: Non-randomised group design with a “no intervention” comparison group. SCEDs: Adequate experimental control (three demonstrations of the experimental effect and controls for common threats to validity) and baseline data (minimum of three measurements). GED: Quasi experimental designs with no control group. Data is obtained pre and post treatment across primary outcome variables. SCED: Weak experimental control (less than three demonstrations of the experimental effect and some between subject comparisons) and inadequate baseline data (less than three measurements). Doctorate in Educational and Child Psychology Tamara Powell Rational: Methodological relevance was weighted in relation to the guidelines for single case studies (Homer et al., 2005) and the hierarchies of evidence proposed by Guyatt et al. (1995). GED: Hierarchies of evidence (Guyatt et al., 1995) classify different study designs in relation to methodological rigour, which in turn guide the strength of recommendations for clinical practice. This framework is accordingly well suited for clinical decisions, such as, whether PCIT and its neighbouring protocols improve symptom severity in young children with anxiety and depression. SCED: According to Homer and colleagues (2005), threats to internal validity and experimental control are amongst the most important variables to consider when assessing SCED. A functional relationship between manipulations to the independent variable (PCIT) and changes in the dependent variable (symptom severity) can only be inferred once studies have collected an adequate amount of data across both the baseline and intervention time periods (within participant control). In line with Homer’s et al. (2005) recommendations, studies must demonstrate at least three experimental effects and three baseline points in order to achieve a medium rating. 3. Weight of Evidence C: Relevance to the Research Question Weighting High Rating (3) Medium Rating (2) Low Rating (1) Description Multiple methods (more than 2 measures) are used to assess symptom severity in a child population with a primary diagnoses of anxiety or depression. PCIT is administered by a trained therapist, and treatment is carried out for at least 12 sessions. Multiple methods (at least 2 measures) are used to assess symptom severity in children with a primary diagnosis of anxiety or depression. PCIT is administered by a trained therapist and treatment is carried out for at least 9 sessions. A single method is used to assess symptom severity in a sample of children with a comorbid diagnoses of anxiety or depression. PCIT is administered by a trained professional and treatment is carried out for less than 9 sessions. Doctorate in Educational and Child Psychology Tamara Powell Rational: Number of Assessment Measures: Kratochwill (2003) recommends using at least two measures to assess the primary outcome variable. Due to the young age of participants who may not to be registered in school or be able to voice their own opinions, only multimethod rather than multi-sourced data were considered. Further, symptom severity is a multidimensional construct that is difficult to measure. Thus, reliability and validity of findings are enhanced if several outcome measures are examined simultaneously. Diagnosis: Children presenting a principle diagnosis of anxiety or depression will show more severe symptomatology than children with a comorbid diagnosis. A number of confounding variables will also be introduced to the analyses if the child’s primary diagnoses falls outside the internalising domain. Programme Length: PCIT manual recommends that treatment be carried out for at least 9 sessions, with CDI lasting between 4 and 7 sessions and PDI 5 to 7 sessions (Hembree-Kigin & McNeil, 1995). Treatment Administrator: Therapists with clinical experience and expertise (graduate level) will be more adept in understanding the unique needs of clients relative to trained professionals will minimal or no clinical experience. Doctorate in Educational and Child Psychology Tamara Powell Appendix 4 Justification for Weights of Evidence Study Chase & Eyberg (2008) Methodological Quality (WoE A) 1.0 – Measures NNR – Comparison Group 3.0 – Primary Outcomes 2.0 – Edu/Clinical Significance 0.0 – Identifiable Components 3.0 – Fidelity 1.8 = Medium Methodological Relevance (WoE B) Quasi experimental design with no control group. Data was obtained pre and post treatment for primary outcome variable. Relevance of Evidence to the Review Question (WoE C) Overall Weight of Evidence (WoE D) DISC-IV-P was the only measure used to assess symptom severity. Participants had a comorbid diagnosis of ODD and SAD. 1.0 = Low 1.3 = Low Therapists’ credentials were not specified. Treatment lasted for 14 sessions. Choate et al. (2005) 1.0 – Measures 0.0 – Quality of Baseline 0.0 – Primary Outcomes 2.0 – Edu/Clinical Significance 0.0 – Identifiable Components 2.0 – Fidelity 0.8 = Low Weak experimental control (one data point at posttest and followup) and inadequate baseline data (single measurement). 1.0 = Low 1.0 = Low ADIS-C/P was the only measure used to assess symptom severity. Children’s primary diagnosis was SAD. Lead therapist was a professor with 2 years of training on PCIT. Treatment was carried out for 6 to 7 sessions. 1.0 = Low 0.9 = Low Doctorate in Educational and Child Psychology Study Comer et al. (2012) Methodological Quality (WoE A) 1.0 – Measures 0.0 – Quality of Baseline NNR – Primary Outcomes 2.0 – Edu/Clinical Significance 0.0 – Identifiable Components 3.0 – Fidelity 1.2 = Low Tamara Powell Methodological Relevance (WoE B) Relevance of Evidence to the Review Question (WoE C) Weak experimental control (group means reported at posstest only) and inadequate baseline data (two measurements). Symptom severity was assessed by: ADIS-C/P, CGAS and CGI. Subjects met diagnostic criteria for a principle anxiety disorder. 1.0 = Low CALM was administered by five Ph.D level therapists who had clinical experience working with children with anxiety related disorders. Overall Weight of Evidence (WoE D) 1.7 = Medium Treatment was conducted over 12 sessions. Lenze et al. (2011) 2.0 – Measures NNR – Comparison Group 1.0 – Primary Outcomes 3.0 – Edu/Clinical Significance 0.0 – Identifiable Components 3.0 – Fidelity 1.8 = Medium Quasi experimental design with no comparison group. Data was obtained pre and post treatment for primary outcome variable. 1.0 = Low 3.0 = High PAPA MDD severity score and HBQ-P internalising subscale were used to assess symptom severity. All children had an MDD principle diagnosis. Three graduate level therapists administered PCIT-ED. Treatment was completed over 14 sessions. 3.0 = Medium 1.6 = Medium Doctorate in Educational and Child Psychology Tamara Powell Study Methodological Quality (WoE A) Methodological Relevance (WoE B) Luby et al. (2012) 2.0– Measures 2.0 – Comparison Group 1.0 – Primary Outcomes 2.0 – Edu/Clinical Significance 0.0 – Identifiable Components 3.0 – Fidelity 1.7 = Medium Participants were randomly assigned to PCIT-ED (experimental group) or a didactic training (active control group) condition. Relevance of Evidence to the Review Question (WoE C) Overall Weight of Evidence (WoE D) PAPA MDD severity score, PFC-S and HBQ-P internalising subscale were used to assess symptom severity. All children had an MDD principle diagnosis. 3.0 = High 2.6 = High Five graduate level therapists administered treatment. Treatment was conducted over 12 weeks (14 sessions). Pincus et al. (2008) 2.0– Measures NNR – Comparison Group NNR – Primary Outcomes 1.0 – Edu/Clinical Significance 0.0 – Identifiable Components 1.0 – Fidelity 1.0 = Low Quasi experimental design with no comparison group. Data was obtained pre and post treatment for primary outcome variable. 3.0 = High ADIS-C/P was the only instrument used to assess symptom severity. Participants met diagnostic criteria for SAD. 1.0 = Low 1.0 = Low No information was provided on therapists’ credentials. Length of treatment was not reported. 1.0 = Low Doctorate in Educational and Child Psychology Tamara Powell Appendix 5 Summary of Reviewed Studies Study Aims Intervention PCIT To examine treatment effects of PCIT in children with comorbid SAD and ODD in relation to children with ODD only on measures of internalising and externalising symptomatology. Therapists adhered to the PCIT principles outlined in the Eyberg (1999) treatment manual for the CDI and PDI phases of treatment. Once proficiency was achieved in CDI, parents moved onto PDI which interleaved aspects of the initial CDI training. Treatment was completed when CDI and PDI skills were mastered and when parents reported their child’s behaviour to be within ½ SD of the normative mean for ECBI. Families participated in a mean of 14.05 sessions (SD = 7.2) over the span of 18.9 weeks (SD = 11.4). Design Chase & Eyberg (2008) Participants One group pretest posttest design Administrator n = 1 SAD severity scores are derived from the DISC-IV-P interview with the child’s female caregiver before and after treatment. Results are examined across time and group (SAD+ODD versus ODD only). Parents n = 1-2 per participant One lead therapist coached parents via a bug in the ear microphone. At least one caregiver was required to participant in the study, however, the sex of the parent and parent-child ratio was not reported. Children n = 64 Participants were part of a larger study examining maintenance of treatment following standard PCIT. To be included, participants required an ODD diagnosis and both the child and parent needed to demonstrate normative cognitive abilities, as assessed by the PPVT and WPT (minimum St. score of 75). Children with neurological impairments or in out of home placements were excluded. SAD+ODD group included 15 children, and the ODD only group 49 children between the ages of 3 and 6 years (M = 4.48; SD = 1.13; 22F, 42M). Children in the SAD+ODD group did not differ from the ODD group on any demographic variables. Measures (relevant to review) DISC-IV-P DISC-IV-P is a structured psychiatric diagnostic interview administered to parents to assess over 30 psychiatric diagnoses that occur in childhood and adolescents, including SAD and ODD. Diagnoses are based on the DSM-IV criteria and the interview is conducted by a trained graduate research assistant before and after treatment. Outcomes (relevant to review) Two way repeated measures ANOVA compared SAD symptoms in the SAD+ODD group to the ODD only group. Results showed a significant group x time interaction (F (1, 55) = 18.93, p < .001, Cohen’s d = 1.48), with a significant reduction in SAD symptoms for the SAD+ODD group between pre and post treatment (t (13) = 7.27, p <.001). The majority of participants (11 out of 15; 75%) diagnosed with SAD at pretreatment no longer met diagnostic criteria. Doctorate in Educational and Child Psychology Study Aims This pilot study aimed to describe the effects PCIT has on the treatment of SAD. SAD behaviours, clinical symptoms, and oppositional behaviour was examined. Intervention Design PCIT PCIT followed the standard procedures outlined by Herschell et al. (2002), which includes the CDI and PDI phases. Parents only proceeded onto the PDI phase once mastery was demonstrated in the CDI phase. The mastery criteria required parents to use no more than 3 questions, commands, or criticisms, and to use at least 10 behavioural descriptions, 10 reflections and 10 labelled praises. Parents received a teaching session during the PDI phase, followed by 2-3 sessions where they implemented the PDI procedures. The intervention terminated when parents demonstrated effective CDI and PDI skills, and when their child’s separation anxiety decreased to less than 2 incidents per week. Multiplebaseline experimental design PCIT ranged from 6 to 7 sessions for each family. Start times were staggered across the three families, with treatment beginning after 1, 2 and 4 weeks respectively. Due to logistical constraints, follow up interviews were conducted at 3 (2 families) and 6 months (1 family). Tamara Powell Choate et al. (2005) Participants Measures (relevant to review) Administrator n = 2 ADIS-C/P The lead therapist was a professor with 2 years of training on the administration of PCIT, and the co-therapist was a second year doctoral student. Semi-structured diagnostic interview designed to specifically assess child and adolescent anxiety and accompanying mood disorders, in accordance with the DSM-IV criteria. A CSR (ranging between 0 and 8) of 4 or greater indicates a clinical diagnosis of anxiety. Parents n = 6 Both parents participated in all facets of treatment. All three families had annual incomes that exceeded $75,000 and were of Caucasian decent. Children n = 3 All participants were recruited through the Child and Adolescent Fear and Anxiety Programme at the Centre for Anxiety and Related Disorders in Boston, Massachusetts. Children between the ages of 4 and 8 years, who were on stable doses of psychotropic medication, not at risk of harming themselves or others and whose primary diagnoses was SAD were invited to participate in the study. The sample included: 1) 5 year old male; principle diagnosis SAD and an additional provisional diagnoses of panic disorder 2) 8 year old female; principle diagnosis SAD and an additional diagnosis of ODD. 3) 7 year old male; principle diagnosis SAD ADIS-C/P is not standardised for children younger than 7 years (Silverman & Nelles, 1988), therefore the measure was not administered to the 5 year old participant. Outcomes (relevant to review) Descriptive statistics were carried out for the 3 participants at pretreatment, posttreatment and 3 or 6 month follow up time points. Sub clinical levels of SAD were found at post-treatment and maintained during the follow up period for all participants. Effect sizes at follow-up were 1.29, 1.71 and 0.86 for participant 1, 2 and 3, respectively. Doctorate in Educational and Child Psychology Study Aims Intervention CALM To investigate the preliminary feasibility and efficacy of a modified version of PCIT to treat youth with SAD, social anxiety disorder, GAD, and/or specific phobias. CALM follows the framework outlined in PCIT, including live and individualised coaching using unobtrusive measures. It also includes a CDI phase that focuses on strengthening the parent-child relationship. Unlike PCIT however, there are exposure sessions whereby parents teach children brave behaviours through increasingly challenging tasks. CALM is carried out for 12 sessions (4 devoted to CDI and 8 to brave behaviours) and the average completing time was 10.3 sessions (2 drop outs completed 4.5 sessions; completers took part in 12 sessions). Design Multiplebaseline experimental design The primary measure was administered across to two baseline assessments, then again at post-treatment. The length of time between Baseline 1 and Baseline 2 was randomly determined (ranged between 1 and 4 weeks) The ADIS-P (parent version) was completed by an IE who was blind to all treatment related data. Tamara Powell Comer et al. (2012) Participants Measures (relevant to review) Administrator n = 5 ADIS-C/P Five Ph.D level clinical psychologists with specialised knowledge in child anxiety disorders administered this manual-based adaptation of PCIT. Each therapist underwent 4 months of training on CALM, and received video-review supervision through the principle investigator. Semi-structured diagnostic interview designed to specifically assess child and adolescent anxiety and accompanying mood disorders, in accordance with the DSM-IV criteria. A CSR (ranging between 0 and 8) of 4 or greater indicates a clinical diagnosis of anxiety. Parents n = 17 With the exception of one participant, whose mother only took part, both parents completed the intervention with their child. Children n = 9 Children were recruited through community outreach efforts (e.g., mailings to paediatricians and media advertisements). Interested families were then screened to ensure they met the study inclusion criteria (child between the ages of 3 to 8 years; principle diagnosis is an anxiety disorder; English speaking). Participants were from racially and ethnically diverse backgrounds, ranging in age from 4 to 8 years (M = 5.4, SD = 1.3; 6F, 3M). At intake, 66% of children met criteria for a principle or co-principle diagnosis of SAD, 33% for a principle or co-principle diagnosis of social anxiety disorder and 11.1% for a principle diagnosis of specific phobia. CGAS CGI-S measures the overall severity of child disturbance (scores range between 0 and 100). CGI-S Illness severity is rated on a 7 point scale (1”normal” to 7 “amongst the most severely ill patients”). Outcomes (relevant to review) Descriptive statistics revealed no changes in outcome scores on the ADIS-P between baseline measures 1 and 2. Post-treatment scores however, showed an average CSR reduction of 2.8 (SD = 2.0), Cohen’s d = 1.26, amongst the intent to treat group (treated as the primary analysis). Overall, 66.7% of participants were found in the normative range following treatment. A mean improvement of 21.0 CGAS (SD = 11.0; Cohen’s d = 1.64) and 2.6 (SD = 1.0; Cohen’s d = 2.26) CGI-S severity points was observed between baseline and posttreatment. Doctorate in Educational and Child Psychology Study Aims Intervention PCIT-ED To report the preliminary findings from a novel adaptation of PCIT for preschool children with MDD. PCIT-ED covers three modules: CDI, PDI and the novel emotional development module. Treatment is conducted over 14 sessions, lasting approximately 18 weeks (+ 3.92). In contrast to standard PCIT, CDI and PDI is limited to 6 sessions and demonstrated proficiency is not required prior to proceeding onto the next module. The novel component includes one teaching session followed by seven coaching sessions, which are intended to help parents assist their child in managing and regulating intense emotion. Homework was assigned within each module to support gains made in sessions. Design One group pretest posttest design Pre-treatment assessments were conducted prior to the onset of treatment and post-treatment 2 weeks following the final 14th session. Tamara Powell Lenze et al. (2011) Participants Measures (relevant to review) Administrator n = 3 PAPA Three graduate level clinicians delivered the intervention. One co-therapist sat in every session and completed a treatment integrity checklist that was later reviewed alongside videotapes by the lead author. PAPA is a parent interview for diagnosing psychiatric disorders in preschool children ages 2 to 5 years. This measure assesses intensity, frequencies, durations, and first onsets of behaviour relevant to Axis 1 diagnoses on the DSM-IV. Parents = 9 Six mothers, one father and one couple completed treatment. Parental income ranged between $15,000 to more than $60, 000 per year. Children = 8 Participants were recruited through primary care, mental health and pre-school settings. Of the nine eligible participants, one refused entry and one dropped out due to child birth after 11 sessions. Children who did not meet a diagnostic criteria of MDD, with any neurological impairment, cognitive delays and or living with an adult other than their primary caregiver (> 6 months) were not permitted to participate. Final sample included seven Caucasian and one biracial child (4F, 4M). Five children were 5 years of age, one was 4 years of age and two were 3 years of age. HBQ-P HSQ-P is a parent questionnaire that provides information regarding the child’s level of mental health symptoms in the internalising and externalising domain. Outcomes (relevant to review) Wilcoxon Signed Rank tests showed significant differences between participants’ pre (M = 13.57, SD = 4.39) and posttest (M = 7.57, SD = 6.00) severity scores on the PAPA (S = 2.38, p <.01, Cohen’s d = 1.19). Overall, mean depression severity scores decreased by 44% and the majority of participants no longer meet diagnostic criteria for MDD (5 out of 7). Significant reductions in internalising symptoms was also reported on the HBQ-P (Cohen’s d = 0.82) Doctorate in Educational and Child Psychology Study Aims Intervention PCIT-ED To build on the previous work of Lenze et al. (2011) by adding more methodological rigour in the interpretations of PCIT-ED and its efficacy in a preschool POMDD population. PCIT-ED covers three modules: CDI, PDI and the novel emotional development module. Treatment is conducted over 14 sessions, lasting approximately 12 weeks. In contrast to standard PCIT, CDI and PDI is limited to 4 sessions each and demonstrated proficiency is not required prior to proceeding onto the next module. The novel component, which spans six sessions, directly teaches parents emotional competence and ways to apply this in practice to support their child’s emotional development. Psycho-educational control condition (DEPI) Parents are taught in groups of 2 to 6 concepts that are relevant to emotional and social development, in the absence of any individualised coaching or practice. Tamara Powell Luby et al. (2012) Design Between subjects randomised pretest posttest design Using simple random sampling, eligible participants were assigned to one of the intervention conditions. Therapists blind to the treatment condition and treatment process carried out the pre and post treatment assessments. Treatment commenced within 7 days of the initial assessment, and post-treatment measures were taken within 14 days following treatment (median 11 days). Participants Administrators n = 3 Five graduate level therapists (Master’s and Doctoral level) served as primary and co-therapist pairs. The treatment integrity checklist was filled out by each cotherapist, with results indicating a high degree of adherence (average 97%). Parents n = 1-2 per participant Both parents were encouraged to attend treatment sessions, however, mothers generally participated for most families. Children n = 43 Community paediatrician offices assisted with recruitment efforts for children between the ages of 3 to 7 years with MDD. Children with neurological impairments, cognitive or developmental delay, and or adopted after 6 months of age were excluded from the study. Higher dropout rates were observed in the control condition (ITT n = 18; completers n = 10) relative to the experimental condition (ITT n = 25, completers n = 19). Sample included children ages 3 -6 who were largely of Caucasian decent and from married families with high annual incomes and educational attainment (16F, 27M). Measures (relevant to review) PAPA PAPA is a parent interview for diagnosing psychiatric disorders in preschool children aged 2 to 5 years. This measure assesses intensity, frequencies, durations, and first onsets of behaviour relevant to Axis 1 diagnoses in the DSM-IV. PFC-S PFC-S is a 20 item checklist scale that assess depression severity in preschool children. Responses are recorded using a Likert scale, ranging from 0 (never) to 4 (most of the time). Outcomes (relevant to review) Paired sample t-tests Significant reductions in depression severity measured using the PAPA MDD was only observed in the PCIT-ED condition (Cohen’s d = 0.50). Significant declines in depression severity scores on the PFC-S and HBQ-P were found in in both the PCIT-ED (PFC-S Cohen’s d = 0.83; HBQ-P Cohen’s d = 0.0) and DEPI condition. Doctorate in Educational and Child Psychology Study Aims Intervention PCIT The shortcomings identified in this study assisted in the development of a modified version of PCIT (brave behaviour module). . Standard PCIT contained two phases: CDI and PDI (Brinkmeyer & Eyberg, 2003). CDI focuses on improving the quality of the parent-child relationship, while PDI aims to reduce disruptive behaviour in children. Each respective section begins with a teaching session followed by weekly coaching sessions that run for approximately 1 hour. Mastery needs to be displayed in CDI before proceeding onto the PDI phase (minimum of 3 sessions is required in each phase). Tamara Powell Design One group pretest posttest design Behavioural measures were recorded before and after treatment. Pincus et al. (2008) Participants Administrators n = not specified Parents n = 1 to 2 At least one parent or caregiver was required to accompany the child to treatment. Children n = 10 Ten children (4F, 6M) ages 4 to 8 years (M = 6.2 years) were recruited through the Child and Adolescent Fear and Treatment Anxiety Programme at the Centre for Anxiety and Related Disorders at Boston University. Inclusion criteria required children to have a principle diagnosis of SAD. Measures (relevant to review) ADIS-C/P Semi-structured diagnostic interview designed to specifically assess child and adolescent anxiety and accompanying mood disorders, in accordance with the DSM-IV criteria. A CSR (ranging between 0 and 8) of 4 or greater indicates a clinical diagnosis of anxiety. Outcomes (relevant to review) Descriptive statistics showed a reduction in SAD severity scores before (M = 5.8) and after (M = 4.2) PCIT (Cohen’s d = 0.73). However, there was no clinically relevant changes. Key: DISC-IV-P – diagnostic interview schedule for children; PCIT – parent-child interaction therapy; SAD – separation anxiety disorder; CDI – child directed interaction; PDI – parent directed interaction; PPVT – peabody picture vocabulary test; WPT – wonderlic personnel test; ADIS-C/P – anxiety disorders interview schedule for DSM-IV; child and parent versions; ODD – oppositional defiant disorder; CSR – clinical severity rating; CALM – coaching approach behaviour and leading and modelling; GAD – generalized anxiety disorder; M – mean; SD – standard deviation; CGAS – the children’s global assessment scale; CGI-S – clinical global impression-severity; IE- independent evaluator; ECBI – eyberg child behaviour inventory; PO-MDD – preschool onset major depressive disorder; PAPA – preschool age psychiatric assessment; HBQ-P; health behaviour questionnaire-parent version; MDD – major depressive disorder; DEPI- developmental education and parenting intervention; ITT – intent to treat sample; PFC-S – preschool feelings checklist scale; BDI – brave directed interactions. Doctorate in Educational and Child Psychology Tamara Powell Appendix 6 Effect Size and Overall Quality Ratings Study Outcomes Measure(s) Chase & Eyberg (2008) Group x time interaction, with significant decreases in symptom severity in the SAD only group at posttest. Diagnostic Interview Schedule for Children was administered to child’s female caregiver. (DISC-IV-P) Choate et al. (2005) Clinical severity ratings for SAD decreased to subclinical levels at posttest and remained in the normative range at follow up. Anxiety Disorders Interview Schedule for DSM-IV – Child and Parent Versions. (ADIS-C/P) Participants Effect Size Descriptors n Overall Weight of Evidence 58 Low Calculated from given data ODD + SAD Comorbid diagnoses: ADHD, CD, MDD Effect Size Medium PPC SMD = 1.48 Calculated from given data SAD + Panic Disorder Large Participant 1de Posttest: PP SMD = 1.29 Follow up: PP SMD = 1.29 3 Low SAD + ODD Large Participant 2de Posttest PP SMD = 1.71 Follow up: PP SMD = 1.71 3 SAD Large Participant 3de Posttest PP SMD = 1.29 Follow-up: PP SMD = 0.86 3 Doctorate in Educational and Child Psychology Study Outcomes Comer et A diagnostic response al. (2012) was observed in 75% of SAD, 67% of social anxiety, 50% of GAD and 0% of specific phobia participants. On average, global severity scores improved from “moderately” and “markedly” ill to “normal” “not at all ill” and “borderline ill.” Lenze et Significant decline in al. (2011) depression severity scores following treatment. Luby et Significant decreases in al. (2012) symptom severity as measured by the PFC-S and HBQ-P in both experimental conditions. PAPA MDD conversely only found significant changes in the PCIT-ED group. Tamara Powell Measure(s) Participants Anxiety Disorders Interview Schedule for DSM-IV – Parent Version (ADISC-P) SAD Social Anxiety Disorder GAD Specific Phobias Comorbidity: OCD, ODD & selective mutism Children’s Global Assessment Scale (CGAS) Clinical Global Impression Severity and Improvement Scales (CGI-S) Preschool Age Psychiatric Assessment (PAPA MDD) Health and Behavior Questionnaire – Internalising Symptoms Subscale (HBQ-P) Preschool Age Psychiatric Assessment (PAPA MDD) Preschool Feelings Checklist-Scale (PFC-S) Health and Behavior Questionnaire – Internalising Symptoms Subscale (HBQ-P) Effect Size Descriptors Effect Size n Overall Weight of Evidence Calculated from given data Largea PP SMD = 1.26de 9 PP SMD = 1.64de 7 PP SMD = 2.26de 7 Largeb Medium Largeb Calculated from given data MDD Large PP SMD =1.19d 8 Medium Large PP SMD =0.82d 8 Calculated from given data MDD Medium PPC SMD = 0.50 42 High Large PPC SMD = 0.83 43 No effect PPC SMD = 0.00 40 Doctorate in Educational and Child Psychology Tamara Powell Study Outcomes Measure(s) Pincus et al. (2008) SAD symptomatology decreased after treatment, however, most scores remained in the clinical range. Anxiety Disorders Interview Schedule for DSM-IV – Child and Parent Versions (ADIS-C/P) Participants Effect Size Descriptors Effect Size n Overall Weight of Evidence 10 Low Calculated from given data SAD Mediumc PP SMD = 0.73d Notes: Effect size, referred to as Pretest-Posttest Standard Mean Difference (PP SMD; Becker, 1988), was calculated by dividing the difference in means by the pre-test standard deviation score (Choate et al., 2005; Comer et al., 2012; Lenze et al., 2011; Pincus et al., 2008). In Chase and Eyberg (2008) and Luby’s et al. (2012) study, effect size (Pretest-Posttest-Control Standard Mean Difference; PPC SMD) was calculated by dividing the difference in means (pre and post treatment) by the pooled standard deviation (Hedge’s g; Morris, 2007). f) To reduce potential sampling biases, statistical analyses was performed on the intent to treat sample. g) Data could not be obtained for the intent to treat sample, so effect size was computed using the completers sample. h) Standard deviation for measure was not reported, it was, therefore, computed using a sample of children with comparable demographics (Comer et al., 2012). i) Effect sizes were corrected in accordance to Hedges’ (1981) guidelines for small samples (e.g., groups with 10 or less participants; Becker, 1988). j) Choate et al. (2005) examined the impact of treatment on children’s symptomatology on an individual basis, whereas Comer et al. (2012) explored pre-post treatment differences using group means. To maintain consistency, the current review reported individual effect sizes at the two phases of treatment in Choate’s et al. (2005) study, and group level effect sizes between baseline and post-treatment for participants in Comer’s et al. (2012) SCED paper. Key: ODD- oppositional defiant disorder; SAD- separation anxiety disorder; ADHD- attention deficit hyperactive disorder; CD- conduct disorder; MDD- major depressive disorder; GAD- generalised anxiety disorder; OCD-obsessive compulsive disorder. Effect Size Descriptor Small Medium Large Cohen’s d 0.20 0.50 0.80 52 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] Appendix 7 Coding Protocol: Group Based Design Domain: School-and community-based intervention programs for social and behavioural problems Academic intervention programmes Family and parent intervention programmes School-wide and classroom-based programmes Comprehensive and coordinated school health services Name of Coder: ____TP_____ Date: January 16th, 2015 Full name of Study in APA format: Chase, R. M., & Eyberg, S. M. (2008). Clinical presentation and treatment outcome for children with comorbid externalizing and internalizing symptoms. Journal of Anxiety Disorders, 22(2), 273–82. Intervention Name (description from study):Parent-Child Interaction Therapy (PCIT) Study ID Number (Unique Identifier): 1 Type of Publication: (Check one) Book/Monograph Journal article Book Chapter Other (specify): 53 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] A. General Characteristics Quasi-Experimental Designs Without Control Groups The One-Group Posttest-Only Design The One-Group Posttest-Only Design with Multiple Substantive Posttests The One-Group Pretest-Posttest Design The One-Group Pretest-Posttest Design Using a Double Pretest The One-Group Pretest-Posttest Design Using a Non-equivalent Dependent Variable The Removed-Treatment Design The Repeated-Treatment Design B. Statistical Treatment/ Data Analysis Yes No N/A B1. Appropriate unit of analysis B2. Familywise error rate controlled B3. Sufficiently large N B.3.1 Statistical Test: ANOVA B3. 2 Level: 2 ES: Large N required: 52 B4. Total size of sample (start of the study): 64 B5. Intervention group sample size: 58 (15 with and 49 without SAD) B6. Control group sample size: 0 C. Type of Programme C.1 Universal prevention programme C.2 Selective prevention programme C.3 Targeted prevention programme C.4 Intervention/Treatment C.5 Unknown D. Stage of the Programme D.1 Model/demonstration programmes D.2 Early stage programmes D.3 Established/institutionalised programmes D.4 Unknown 54 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] E. Concurrent or Historical Intervention Exposure E.1 Current exposure E.2 Prior Exposure E.3 Unknown II. Key Features for Coding Studies and Rating Levels of Evidence/Support (3 = Strong Evidence; 2 = Promising Evidence; 1 = Weak Evidence; 0 = No Evidence) A. Measurement A1. Use of outcome measure produces reliable sources for the majority of primary outcomes. A1.1Yes A1.2 No A1.3 Unknown/Unable to code A2. Multi-method A2.1 Yes A2.2 No A2.3 N/A A2.4 Unknown/Unable to code A3. Multi-source A3.1 Yes A3.2 No A3.3 N/A A3.4 Unknown/Unable to code A4. Validity of measures reported A4.1 Yes validated with specific target group A4.2 In part, validated for general population only A4.3 No A4.4 Unknown/Unable to code Rating for Measurement 3 2 1 0 55 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] B. Comparison Group No control group – all participants received the intervention B1. Type of Comparison Group B1.1 Typical contact B1.2 Typical contact (other) specify: B1.3 Attention placebo B1.4 Intervention elements placebo B1.5 Alternative intervention B1.6 Pharmacotherapy B1.7 No intervention B1.8 Wait list/ delayed intervention B1.9 Minimal contact B1.10 Unable to identify comparison group Rating for Comparison Group NNR- no control group 3 2 1 0 B2. Overall confidence rating in judgement of type of comparison group B2.1 Very low (little basis) B2.2 Low (guess) B2.3 Moderate (weak inference) B2.4 High (strong inference) B2.5 Very high (explicitly stated) B2.6 N/A B2.7 Unknown/unable to code B3. Counterbalancing of Change Agents B3.1 By change agent B3.2 Statistical B3.3 Other One lead therapist coached all parents who had children with ODD+SAD and ODD only. High adherence to programme standards were evidenced through treatment integrity checklist (M = 90%). B4. Group Equivalence Established B4.1 Random assignment B4.2 Post hoc matched set B4.3 Statistical matching B4.4 Post hoc test for group equivalence 56 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] Not Applicable – No control group B5. Equivalent Mortality B5.1 Low attrition (less than 20% for Post) B5.2 Low attrition (less than 30% for follow-up) B5.3 Intent to intervene analysis carried out Findings: Attrition rate was 36%, which is similar to other PCIT treatment programmes (Gallagher, 2003). ITT was not carried out, however, attrition rates were similar for children with and without SAD. C. Primary Outcomes Are Statistically Significant C.1 Evidence of appropriate statistical analysis for primary outcomes C1.1 Appropriate unit of analysis C1.2 Familywise/experimenterwise error rate controlled when applicable C1.3 Sufficiently large N C2. Percentage of primary outcomes that are statistically significant C2.1 Significant primary outcomes for at least 75% of the total primary measures for each key construct C2.2 Significant primary outcomes for between 50% and 74% of the total primary measures for each key construct C2.3 Significant primary outcomes for between 25% and 49% of the total primary measures for each key construct Rating for Primary Outcomes Statistically Significant 3 2 1 0 C3. Evidence of appropriate statistical analysis for primary outcomes Yes C3.1 Main effect analyses conducted C3.2 Moderator effect analyses conducted specify results: C3.3 Mediator analyses conducted, specify results: No 57 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] D. Educational/Clinical Significance Outcome Variable Pretest D1. Categorical Diagnosis Data Diagnostic information regarding inclusion into the DISC-IV-P; Diagnostic Interview study presented: Schedule for Children – Parent Edition Yes No Unknown D2. Outcomes Assessed via continuous Variables DISC-IV-P; Outcome Score Posttest Positive change in diagnostic criteria from pre to posttest: Positive change in diagnostic criteria from posttest to follow up: Yes No Unknown Positive change in the percentage of participants showing clinical improvement from pre to posttest: Yes No Unknown Positive change in the percentage of participants showing clinical improvement from posttest to follow up: Yes D3. Subjective Evaluation: The importance of behaviour change is evaluated by individuals in direct contact with the participant. Importance of behaviour change is evaluated: Yes No Unknown D4. Social Comparison: Behaviour of participant change Participant’s behaviour is is evaluated by individuals in compared to normative data: direct contact with the participant Yes No Unknown Follow-up No Unknown Importance of behaviour change from pre to posttest is evaluate positively by individuals in direct contact with the participant: Yes No Unknown Participant’s behaviour has improved from pre to posttest when compared to normative data: Yes No Unknown Yes No Unknown Importance of behaviour change from posttest to follow up is evaluate positively by individuals in direct contact with the participant: Yes No Unknown Participant’s behaviour has improved from posttest to follow up when compared to normative data: Yes No Unknown 58 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] Rating for Educational/Clinical Significance: 3 2 1 0 E. Identifiable Components E1. Evidence for primary outcomes: 3 2 1 0 Yes No E2. Design allows for analysis of identifiable components E3. Total number of components: 2 E4. Number of components linked to primary outcomes: 0 Additional criteria to code descriptively: Yes No E5. Clear documentation of essential components E6. Procedures for adapting the intervention are described in detail E7. Contextual features of the intervention are documented Rating of Identifiable Components 3 2 1 0 F. Implementation Fidelity F1. Evidence of Acceptable Adherence F1.1 Ongoing supervision/consultation F1.2 Coding intervention sessions/lessons or procedures F1.3 Audio/video tape implementation F1.3.1 Entire intervention F1.3.2 Part of intervention 59 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] F2. Manualization F2.1 Written material involving a detailed account of the exact procedures and the sequence in which they are to be used F2.2 Formal training session that includes a detailed account of the exact procedures and the sequence in which they are to be used F2.3 Written material involving an overview of broad principles and a description of the intervention phases F2.4 Formal or informal training session involving an overview of broad principles and a description of the intervention phases Yes No Unknown F3. Adaptation procedures are specified Rating for Implementation Fidelity 3 2 1 0 III. Other Descriptive or Supplemental Criteria to Consider A. External Validity Indicators Yes No A1. Sampling procedures described in detail Specify rationale for selection: Participants were part of a larger study Specify rationale for sample size: No rational provided Yes No A1.1 Inclusion/exclusion criteria specified A1.2 Inclusion/exclusion criteria similar to school practice A1.3 Specified criteria related to concern A2. Participant Characteristics Specified for Treatment and Control Group (see Appendix 5). A3. Details are provided regarding variables that: Yes No A3.1 Have differential relevance for intended outcomes Specify: SES, comorbid diagnoses A3.2 Have relevance to the inclusion criteria Specify: Scores on screening measure (DISC-IV-P) 60 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] A4. Receptivity/acceptance by target participant population No data on receptivity/acceptance reported Participants from Treatment Group Results (What person reported to have gained from participation in programme) General Rating Child/Student Parent/caregiver Teacher School Other Participants reported benefiting overall from the intervention Child/Student Parent/caregiver Teacher School Other Participants reported benefiting overall from the intervention Child/Student Parent/caregiver Teacher School Other Participants reported benefiting overall from the intervention Participants reported not benefiting overall from the intervention Participants reported not benefiting overall from the intervention Participants reported not benefiting overall from the intervention A5. Generalisation of Effects: A5.1 Generalisation over time Yes No A5.1.1 Evidence is provided regarding the sustainability of outcomes after intervention is terminated. Specify: A5.1.2 Procedures for maintaining outcomes are specified A5.2 Generalisation across settings Yes No A5.2.1 Evidence is provided regarding the extent to which outcomes are maintained in contexts that are different from the intervention context. Specify: A5.2.2 Documentation of the efforts to ensure application of intervention to other settings. Specify: Daily homework A5.2.3 Impact on implementers or context is sustained. Specify: 61 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] Unable to code A5.2.3 because there is insufficient information provided. A5.3 Generalisation across persons Yes No A5.3.1 Evidence is provided regarding the degree to which outcomes are manifested with participants who are different than the original group of participants for with the intervention was evaluated. Specify: B. Length of Intervention B1. Unknown/insufficient information provided B2. Information provided (if information provided, specify one of the following): B2.1. Weeks: 19 B2.2 Months: __ B2.3 Years: __ B2.4 Other: __ C. Intensity/dosage of Intervention C1. Unknown/insufficient information provided C2. Information provided (if information provided, specify one of the following): C2.1. Length of intervention session: unknown C2.2 Frequency of intervention sessions: 14 sessions D. Dosage Response D1. Unknown/insufficient information provided D2. Information provided (if information provided, answer D2.1): D2.1 Describe positive outcomes associated with higher dosage:_______ E. Programme Implementer E1. Research Staff E2. School Speciality Staff E3. Teachers E4. Educational Assistants E5. Parents E6. College Students E7. Peers E8. Others E9. Unknown/insufficient information provided 62 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] F. Characteristics of the Intervener F1. Highly similar to target population on key variables (e.g., race, gender, SES) F2. Somewhat similar to target participants on key variables F3. Different from target participants on key variables Unknown/insufficient information provided. G. Intervention Style or Orientation G1. Behavioural G2. Cognitive-behavioural G3. Experimental G4. Humanistic/Interpersonal G5. Psychodynamic/insight oriented G6. Other, specify: G7. Unknown/insufficient information provided H. Cost Analysis Data H1. Unknown/insufficient information provided H2. Information provided (if information provided, answer H2.1): H2.1 Estimated Cost of Implementation:______________________ I. Training and Support Resources I1. Simple orientation given to change agents I2. Training workshops conducted Parents received two training sessions that preceded the CDI and PDI phases. # of workshops provided: _2 (parents)_ Average length of training: _unknown_ Who conducted training: I2.1 Project Director I2.2 Graduate/project assistants 12.3 Other, specify: 12.4 Unknown I3. Ongoing technical support I4. Programme materials obtained I5. Special facilities I6. Other, specify: One way mirror and bug in the ear receiver required for this intervention. J. Feasibility J1. Level of difficulty in training intervention agents J1.1 High J1.2 Moderate 63 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] J1.3 Low J1.4 Unknown J2. Cost to train intervention agents (specify if known):_________ J3. Rating cost to train intervention agents: J3.1 High J3.2 Moderate J3.3 Low J3.4 Unknown Summary of Evidence for Group-Based Design Studies Indicator General Characteristics General Design Characteristics Statistical Treatment Type of Programme Stage of Programme Concurrent/Historical Intervention Exposure Key Features Measurement Comparison Group Primary Outcomes are Statistically Significant Educational/Clinical Significance Identifiable Components Implementation Fidelity Descriptive or Supplemental Criteria External Validity Indicators Length of Intervention Intensity/Dosage Dosage Response Programme Implementer Characteristics of the Intervener Intervention Style/Orientation Cost Analysis Data Provided Overall Evidence Rating NNR = No numerical rating or 03 Description of Evidence (Strong, Promising, Weak, No/limited evidence, or Descriptive Ratings NNR NNR NNR NNR One-group pretest-posttest design ANOVA Intervention/Treatment Established/Institutionalised NNR Unknown 1 NNR Weak Evidence No Control Group 3 2 0 3 NNR NNR NNR NNR NNR NNR NNR NNR Strong Evidence Promising Evidence No Evidence Strong Evidence Some Evidence 19 weeks 14 sessions Unknown Research Staff and Parents Unknown Behavioural/Psychodynamic Unknown 64 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] Training and Support Resources NNR Feasibility NNR Parents receive two training sessions; One-way mirror and bug in the ear receiver Unknown 65 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] Coding Protocol: Single-Participant Design Domain: School-and community-based intervention programs for social and behavioural problems Academic intervention programmes Family and parent intervention programmes School-wide and classroom-based programmes Comprehensive and coordinated school health services Name of Coder: ____TP_____ Date: January 16th, 2015 Full name of Study in APA format: Choate, M. L., Pincus, D. B., Eyberg, S. M., & Barlow, D. H. (2001). Parent-Child Interaction Therapy for Treatment of Separation Anxiety Disorder in Young Children : A Pilot Study, Cognitive and Behavioral Practice,12(1),126–135. Intervention Name (description from study):Parent-Child Interaction Therapy (PCIT). Study ID Number (Unique Identifier): 2 Type of Publication: (Check one) Book/Monograph Journal article Book Chapter Other (specify): 66 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] 1. General Characteristics A. General Design Characteriistics A1. Type of Single-Participant Design A1.1 Within-series design A1.1.1 Simple phase change A1.1.2 Complex phase change A1.2 Between-series design A1.2.1 Comparing two interventions A1.2.2 Comparing interventions with no interventions A1.3 Combined-series design A1.3.1 Multiple baseline across participants A1.3.2 Multiple baseline across behaviours A1.3.3 Multiple baseline across settings A1.3.4 Multiple probe design A1.4 Mixed design A1.4.1 Combined single-participant and group design A1.4.2 Combined single-participant design A1.4.2.1 Within-series design i. Simple phase change ii. Complex phase change A1.4.2.2 Between-series design i. Comparing two interventions ii. Comparing interventions with no interventions A1.4.2.3 Combined-series design i. Multiple baseline across participants ii. Multiple baseline across behaviours iii. Multiple baselines across settings iv. Multiple probe design A1.5 Other, Specify B. Other Design Characteristics (when randomisation is used) B1. Unit of assignment to conditions/groups B1.1 Individual B1.2 Classroom B1.3 School B1.4 Other, Specify B1.5 N/A (randomisation not used) B2.Type of assignment to conditions/groups B2.1 Random after matching, stratification, blocking B2.2 Random simple (includes systematic sampling) B2.3 Nonrandom, post hoc matching B2.4 Nonrandom, other B2.5 Other, Specify B2.6 Unknown/insufficient information provided 67 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] B2.5 N/A (randomisation not used) B3. Overall confidence of judgement on how participants were assigned to conditions/groups B3.1 Very low (little basis) B3.2 Low (guess) B3.3 Moderate (weak inference) B3.4 High (strong inference) B3.5 Very high (explicitly stated) B3.6 N/A (randomisation not used) B3.7 Unknown/unable to code B4. Equivalence of conditions/groups tested at pretest B4.1 Yes B4.2 No B4.3 Unknown/insufficient information provided B4.4 N/A (randomisation not used) B5. Total size of sample (start of the study): 3 B6. Intervention group sample size: 3 B7. Control group sample size: 0 C. Type of Programme C.1 Universal prevention programme C.2 Selective prevention programme C.3 Targeted prevention programme C.4 Intervention/Treatment C.5 Unknown D. Stage of the Programme D.1 Model/demonstration programmes D.2 Early stage programmes D.3 Established/institutionalised programmes D.4 Unknown E. Concurrent or Historical Intervention Exposure E.1 Current exposure E.2 Prior Exposure E.3 Unknown 68 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] II. Key Features for Coding Studies and Rating Levels of Evidence/Support (3 = Strong Evidence; 2 = Promising Evidence; 1 = Weak Evidence; 0 = No Evidence) A. Measurement A1. Use of outcome measures that produce reliable sources A1.1Yes A1.2 No A1.3 Unknown/Unable to code A2. Multi-method A2.1 Yes A2.2 No A2.3 N/A A2.4 Unknown/Unable to code A3. Multi-source A3.1 Yes A3.2 No A3.3 N/A A3.4 Unknown/Unable to code The outcome measure (ADIS-C/P) is not standardized for children younger than 7 years of age. It was therefore completed with the child and parent in only 2 out of the 3 families. A4. Validity of measures reported A4.1 Yes A4.2 No A4.3 Unknown/Unable to code Rating for Measurement 3 2 1 0 B. Quality of Baseline Participant 1 B1. Length: At least 3 data points during baseline B1.1 Yes B1.2 No B1.3 Unknown/insufficient information 69 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] B2. Stability: Variability in scores does not eliminate the detection of treatment effects B2.1 Yes B2.2 No B2.3 Unknown/insufficient information B3. Overlap: Extreme scores during baseline do not overlap with most scores during intervention phase B3.1 Yes B3.2 No B3.3 Unknown/insufficient information B4. Level: Behaviour is serious enough during baseline to warrant an intervention B2.1 Yes B2.2 No B2.3 Unknown/insufficient information B5. Trend: Behaviour is not systematically increasing or decreasing in the desired direction of intervention effects during baseline. B2.1 Yes B2.2 No B2.3 Unknown/insufficient information Rating for quality of baseline for participant 1 3 2 1 0 Participant 2 B1. Length: At least 3 data points during baseline B1.1 Yes B1.2 No B1.3 Unknown/insufficient information B2. Stability: Variability in scores does not eliminate the detection of treatment effects B2.1 Yes 70 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] B2.2 No B2.3 Unknown/insufficient information B3. Overlap: Extreme scores during baseline do not overlap with most scores during intervention phase B3.1 Yes B3.2 No B3.3 Unknown/insufficient information B4. Level: Behaviour is serious enough during baseline to warrant an intervention B2.1 Yes B2.2 No B2.3 Unknown/insufficient information B5. Trend: Behaviour is not systematically increasing or decreasing in the desired direction of intervention effects during baseline. B2.1 Yes B2.2 No B2.3 Unknown/insufficient information Rating for quality of baseline for participant 2 3 2 1 0 Participant 3 B1. Length: At least 3 data points during baseline B1.1 Yes B1.2 No B1.3 Unknown/insufficient information B2. Stability: Variability in scores does not eliminate the detection of treatment effects B2.1 Yes B2.2 No B2.3 Unknown/insufficient information 71 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] B3. Overlap: Extreme scores during baseline do not overlap with most scores during intervention phase B3.1 Yes B3.2 No B3.3 Unknown/insufficient information B4. Level: Behaviour is serious enough during baseline to warrant an intervention B2.1 Yes B2.2 No B2.3 Unknown/insufficient information B5. Trend: Behaviour is not systematically increasing or decreasing in the desired direction of intervention effects during baseline. B2.1 Yes B2.2 No B2.3 Unknown/insufficient information Rating for quality of baseline for participant 3 3 2 1 0 Average Quality of Baseline Rating Across Participants ∑ of X/N = 0+0+0/3 Overall Rating for Quality of Baseline 3 2 1 0 72 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] C. Visual Analysis Outcome #1:ADIS-C/P (Primary Outcome) Participant Participant 1 Participant 2 Visual Analysis C1.1 Changes in levels C1.1.1 large C1.1.2 moderate-to-large C1.1.3 moderate C1.1.4 no change C1.1.5 unknown/insufficient information C1.2 No to minimal score overlap C1.2.1 yes C1.2.2 no C1.2.3 unknown/insufficient information C1.3 Change in trend C1.3.1 yes C1.3.2 no C1.3.3 N/A (no trend present) C1.3.4 unknown/insufficient information C1.4 Adequate length C1.4.1 yes C1.4.2 no C1.4.3 unknown/insufficient information C1.5 Stable data C1.5.1 yes C1.5.2 no C1.5.3 unknown/insufficient information Rating for Visual Analysis for Participant 1: C1.1 Changes in levels C1.1.1 large C1.1.2 moderate-to-large C1.1.3 moderate C1.1.4 no change C1.1.5 unknown/insufficient information C1.2 No to minimal score overlap C1.2.1 yes C1.2.2 no C1.2.3 unknown/insufficient information C1.3 Change in trend C1.3.1 yes C1.3.2 no C1.3.3 N/A (no trend present) C1.3.4 unknown/insufficient information C1.4 Adequate length C1.4.1 yes C1.4.2 no C1.4.3 unknown/insufficient information C1.5 Stable data C1.5.1 yes C1.5.2 no C1.5.3 unknown/insufficient information 0 1 2 3 73 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] Participant 3 Rating for Visual Analysis for Participant 2: C1.1 Changes in levels C1.1.1 large C1.1.2 moderate-to-large C1.1.3 moderate C1.1.4 no change C1.1.5 unknown/insufficient information C1.2 No to minimal score overlap C1.2.1 yes C1.2.2 no C1.2.3 unknown/insufficient information C1.3 Change in trend C1.3.1 yes C1.3.2 no C1.3.3 N/A (no trend present) C1.3.4 unknown/insufficient information C1.4 Adequate length C1.4.1 yes C1.4.2 no C1.4.3 unknown/insufficient information C1.5 Stable data C1.5.1 yes C1.5.2 no C1.5.3 unknown/insufficient information 0 1 2 3 Rating for Visual Analysis for Participant 3: 0 1 2 3 Measures Support Primary Outcomes Average Rating for Measures Support Primary Outcomes Across Participants Using Score from Visual Analysis ∑ of X/N = 0+0+0/3 Overall Rating for Measures Support Primary Outcomes: 3 2 1 0 74 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] D. Educational/Clinical Significance Outcome Variable D1. Categorical Diagnosis Data ADIS-C/P; Dichotomous variable verifying the existence of anxiety (clinical severity score [CSR] of 4 or greater) Pretest Diagnostic information regarding inclusion into the study presented: Yes No Unknown D2. Outcomes Assessed via continuous Variables ADIS-C/P; Clinical Severity Score Posttest Positive change in diagnostic criteria from pre to posttest: Positive change in diagnostic criteria from posttest to follow up: Yes No Unknown Positive change in the percentage of participants showing clinical improvement from pre to posttest: Yes No Unknown Positive change in the percentage of participants showing clinical improvement from posttest to follow up: Yes D3. Subjective Evaluation: The importance of behaviour change is evaluated by individuals in direct contact with the participant. Importance of behaviour change is evaluated: Yes No Unknown D4. Social Comparison: Behaviour of participant change Participant’s behaviour is is evaluated by individuals in compared to normative data: direct contact with the participant Yes No Unknown Follow-up No Unknown Importance of behaviour change from pre to posttest is evaluate positively by individuals in direct contact with the participant: Yes No Unknown Participant’s behaviour has improved from pre to posttest when compared to normative data: Only on the PAPA MDD (not PFC-S) measure Yes No Unknown Yes No Unknown Importance of behaviour change from posttest to follow up is evaluate positively by individuals in direct contact with the participant: Yes No Unknown Participant’s behaviour has improved from posttest to follow up when compared to normative data: Yes No Unknown 75 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] Rating for Educational/Clinical Significance: 3 2 1 E. Identifiable Components E1. Evidence for primary outcomes: 3 2 1 0 Yes No E2. Design allows for analysis of identifiable components E3. Total number of components: 2 E4. Number of components linked to primary outcomes: 0 Additional criteria to code descriptively: Yes E5. Clear documentation of essential components E6. Procedures for adapting the intervention are described in detail E7. Contextual features of the intervention are documented Rating of Identifiable Components 3 2 1 0 F. Implementation Fidelity for Participants 1 to 3 F1. Evidence of Acceptable Adherence F1.1 Ongoing supervision/consultation F1.2 Coding intervention sessions/lessons or procedures F1.3 Audio/video tape implementation F1.3.1 Entire intervention F1.3.2 Part of intervention No 76 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] F2. Manualization F2.1 Written material involving a detailed account of the exact procedures and the sequence in which they are to be used F2.2 Formal training session that includes a detailed account of the exact procedures and the sequence in which they are to be used F2.3 Written material involving an overview of broad principles and a description of the intervention phases F2.4 Formal or informal training session involving an overview of broad principles and a description of the intervention phases Yes No Unknown F3. Adaptation procedures are specified Rating for Implementation Fidelity 3 2 1 0 III. Other Descriptive or Supplemental Criteria to Consider A. External Validity Indicators Yes No A1. Sampling procedures described in detail Specify rationale for selection: Within age limits with a SAD diagnosis Specify rationale for sample size: No rational provided Yes No A1.1 Inclusion/exclusion criteria specified A1.2 Inclusion/exclusion criteria similar to school practice A1.3 Specified criteria related to concern A2. Participant Characteristics Specified for Treatment and Control Group (see Appendix 5). A3. Details are provided regarding variables that: Yes A3.1 Have differential relevance for intended outcomes Specify: comorbid diagnoses A3.2 Have relevance to the inclusion criteria Specify: Scores on screening measure (ADIS-C/P) No 77 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] A4. Receptivity/acceptance by target participant population No data reported for receptivity/acceptance Participants from Treatment Group Results (What person reported to have gained from participation in programme) General Rating Child/Student Parent/caregiver Teacher School Other Participants reported benefiting overall from the intervention Child/Student Parent/caregiver Teacher School Other Participants reported benefiting overall from the intervention Child/Student Parent/caregiver Teacher School Other Participants reported benefiting overall from the intervention Participants reported not benefiting overall from the intervention Participants reported not benefiting overall from the intervention Participants reported not benefiting overall from the intervention A5. Generalisation of Effects: A5.1 Generalisation over time Yes No A5.1.1 Evidence is provided regarding the sustainability of outcomes after intervention is terminated. Specify: Follow-up 3-6 months after treatment A5.1.2 Procedures for maintaining outcomes are specified A5.2 Generalisation across settings Yes No A5.2.1 Evidence is provided regarding the extent to which outcomes are maintained in contexts that are different from the intervention context. Specify: A5.2.2 Documentation of the efforts to ensure application of intervention to other settings. Specify: Daily homework 78 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] A5.2.3 Impact on implementers or context is sustained. Specify: Unable to code A5.2.3 because there is insufficient information provided. A5.3 Generalisation across persons Yes A5.3.1 Evidence is provided regarding the degree to which outcomes are manifested with participants who are different than the original group of participants for with the intervention was evaluated. Specify: B. Length of Intervention B1. Unknown/insufficient information provided B2. Information provided (if information provided, specify one of the following): B2.1. Weeks: __ B2.2 Months: __ B2.3 Years: __ B2.4 Other: __ C. Intensity/dosage of Intervention C1. Unknown/insufficient information provided C2. Information provided (if information provided, specify one of the following): C2.1. Length of intervention session: unknown C2.2 Frequency of intervention sessions: 6 to 7 sessions D. Dosage Response D1. Unknown/insufficient information provided D2. Information provided (if information provided, answer D2.1): D2.1 Describe positive outcomes associated with higher dosage:_______ E. Programme Implementer E1. Research Staff E2. School Speciality Staff E3. Teachers E4. Educational Assistants E5. Parents E6. College Students E7. Peers E8. Others E9. Unknown/insufficient information provided No 79 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] F. Characteristics of the Intervener F1. Highly similar to target population on key variables (e.g., race, gender, SES) F2. Somewhat similar to target participants on key variables F3. Different from target participants on key variables Unknown/insufficient information provided G. Intervention Style or Orientation G1. Behavioural G2. Cognitive-behavioural G3. Experimental G4. Humanistic/Interpersonal G5. Psychodynamic/insight oriented G6. Other, specify: G7. Unknown/insufficient information provided H. Cost Analysis Data H1. Unknown/insufficient information provided H2. Information provided (if information provided, answer H2.1): H2.1 Estimated Cost of Implementation:______________________ I. Training and Support Resources I1. Simple orientation given to change agents I2. Training workshops conducted Length of training for lead and co-therapist was not specified. Parents received one teaching session during the PDI phase. # of workshops provided: _1(parents)__ Average length of training: ____ Who conducted training: I2.1 Project Director I2.2 Graduate/project assistants 12.3 Other, specify: 12.4 Unknown I3. Ongoing technical support I4. Programme materials obtained I5. Special facilities I6. Other, specify: One way mirror and bug in the ear receiver required for this intervention. 80 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] J. Feasibility J1. Level of difficulty in training intervention agents J1.1 High J1.2 Moderate J1.3 Low J1.4 Unknown J2. Cost to train intervention agents (specify if known):_________ J3. Rating cost to train intervention agents: J3.1 High J3.2 Moderate J3.3 Low J3.4 Unknown Summary of Evidence for Group-Based Design Studies Indicator General Characteristics General Design Characteristics Other design characteristics (when randomisation is used) Type of Programme Stage of Programme Concurrent/Historical Intervention Exposure Key Features Measurement Comparison Group Primary Outcomes are Statistically Significant Educational/Clinical Significance Identifiable Components Implementation Fidelity Descriptive or Supplemental Criteria External Validity Indicators Length of Intervention Intensity/Dosage Overall Evidence Rating NNR = No numerical rating or 03 NNR NNR NNR NNR Description of Evidence (Strong, Promising, Weak, No/limited evidence, or Descriptive Ratings Multiple baseline across participants Not applicable Intervention/Treatment Established/Institutionalised Unknown NNR 1 0 Weak Evidence No Evidence 0 2 0 2 No Evidence Promising Evidence No Evidence Promising Evidence NNR NNR NNR Some Evidence Unknown 6 to 7 sessions 81 [adapted from Task Force on Evidence-Based Interventions in School Psychology, American Psychology Association, Kratochwill, T.R. (2003)] Dosage Response Programme Implementer Characteristics of the Intervener Intervention Style/Orientation Cost Analysis Data Provided Training and Support Resources NNR NNR NNR NNR NNR NNR Feasibility NNR Unknown Research Staff and Parents Unknown Behavioural/Psychodynamic Unknown Parents receive one training session; One-way mirror and bug in the ear receiver Unknown