BOARD OF DIRECTORS MEETING IN PUBLIC 27 March 2014
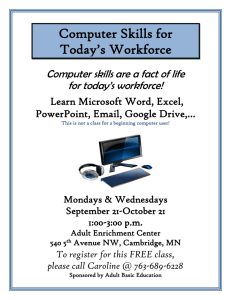
advertisement

BOARD OF DIRECTORS MEETING IN PUBLIC 27 March 2014 PAPERS Board of Directors’ Meeting Part I in Public 27 March 2014 09.00 The Education Centre, Birmingham Children’s Hospital AGENDA Item No. 14.43 14.44 14.45 14.46 14.47 14.48 14.49 14.50 14.51 14.52 Item Apologies for absence Declarations of interest Minutes of public Board meeting 27 February, 2014 Outcome Note Note Approve Matters arising from public Board meeting 27 February Note 2014 Chairman’s Report Note Chief Executive’s Report Note Strategy Our Nursing Workforce. Note & Michelle McLoughlin, Chief Nurse Approve Next Generation Project Note & Sarah-Jane Marsh, Chief Executive Approve Monitor Operational Plan 2014/15 – 2015/16 Note & David Melbourne Chief Finance Officer & Deputy Chief Approve Executive and Matthew Boazman, Director of Strategy and Planning 10.45 Break 10 mins Quality & Resources Quality Report 2013-14 – Local Indicators Vin Diwakar, Note & Chief Medical Officer Approve Time Allocated time 09.00 09.00 05 mins Report type Verbal Verbal Enclosure 01 Verbal 09.05 09.10 05 mins 20 mins Verbal Verbal 09.30 30 mins Enclosure 02 10.00 30 mins Presentation 10.30 15 mins Enclosure 03 10.55 20 mins Enclosure 04 14.53 Quality Report - Vin Diwakar, Chief Medical Officer and Note & Michelle McLoughlin, Chief Nurse Approve 11.15 10 mins Enclosure 05 14.54 Performance Report - David Melbourne Chief Finance Officer & Deputy Chief Executive Resources Report - David Melbourne Chief Finance Officer & Deputy Chief Executive, Phil Foster, Director of Finance & Procurement and Theresa Nelson, Chief Officer for Workforce Development. 11.25 10 mins Enclosure 06 11.35 10 mins Enclosure 07 11.45 05 mins None 14.55 Note & Approve Note & Approve Any other business 14.56 Questions from members of the public Part II of this meeting of the Board of Directors will be held in private, as the information to be discussed is exempt from public disclosure under the Freedom of Information Act 2000. Next meeting of the Board of Directors: 30 April 2014, Education Centre, BCH UNCONFIRMED Item 14.45 Enc 01 BOARD OF DIRECTORS MEETING Minutes of the meeting held in public on 27 February 2014 at 09.00 in the Education Centre, Birmingham Children’s Hospital Present Attending Ref. 14.29 14.30 14.31 14.32 14.33 Keith Lester Sarah-Jane Marsh Tim Atack Vin Diwakar Judy Green Jon Glasby Colin Horwath Michelle McLoughlin David Melbourne Theresa Nelson Roger Pearce Elaine Simpson KL SJM TA VDi JAG JG CH MM DM TN RP ES Interim Chairman Chief Executive Officer Chief Operating Officer Chief Medical Officer Non-Executive Director Non-Executive Director Non-Executive Director Chief Nursing Officer Deputy CEO and Chief Finance Officer Chief Officer for Workforce Development Non Executive Director Non Executive Director Deborah Bannister Matthew Boazman Christine Braddock Claire Burden Simon Crooks Phil Foster DB MB CB CBN SC PF Interim Company Secretary Director of Strategy and Planning Chairman elect Deputy Chief Operating Officer Executive Office Manager (minutes) Director of Finance and Procurement Item Apologies There were no apologies for absence. Declarations of Interest None Minutes of the Board meeting held in public on 30 January 2014 The minutes were agreed as an accurate record. Matters arising from the Board meeting held in public on 30 January 2014 There were no matters arising not covered by the agenda. Chairman’s Report Judy Green This would be the last meeting that JAG would attend pending her retirement at the end of this month. The Board joined with KL in expressing their thanks and appreciation for the dedicated service and time given by JAG to the Trust over the last eight years Governors DB was now redrafting the Trust constitution to incorporate changes arising from the Health & Social Care Act 2012 but also to consider options as to the number and breakdown of Governor Page 1 of 8 Action UNCONFIRMED Item 14.45 Ref. Enc 01 Item particularly following the demise of PCT’s, leaving a number of partner governor vacancies. In addition a KPMG questionnaire had been circulated to governors seeking details as to how effective they thought their role was. SJM expressed the importance of encouraging greater involvement from all governors, not just the more outspoken members, as staff governors in particular have a lot to give. In addition the Trust membership needs to be reviewed - how to arrest the decline and increase membership was important, together with improved engagement. TN referred to the four staff governors and suggested staff should be encouraged to engage and become more involved with their representatives. The Board noted the verbal report 14.34 Chief Executive’s Report SJM reported verbally as follows: The outcome of a Trauma Peer Review carried out at the Trust had been extremely positive. The reviewers felt they had learnt a lot from the Trust that they could go on to share as best practice. The only suggestion made was to be wary of complacency and to continue to strive to improve. A Deanery visit focussing on neuro and orthopaedic surgical training had also received excellent feedback. An impressive cultural change in respect of junior doctors had been noted as well as improved communication. Again the only concern had been the danger of losing momentum. The staff survey results had just been received and were now being analysed. They would be considered initially by the Quality Committee before being presented to Board. All five engagement indicators had improved. Key messages and concerns were related to levels of stress and long hours. It was hoped that the forthcoming Intent to listen sessions would hopefully provide the opportunity to discuss these concerns in more detail. SJM was hosting ‘tea parties’ recognising excellent team performance, the latest one had been in the KIDS service. SJM and MM had enjoyed an excellent session with the Trust’s YPAG, who had been asked to describe what constituted excellent care. Compassion was seen as the core requirement, but the ability to “remove worry” was also seen as a vital element. A presentation from YPAG was expected at the March Board meeting.. NHS Change Day is Monday 3rd March. Over 80 members of staff had joined SJM in pledging to support the power of storytelling, which in turn was attracting media coverage. Page 2 of 8 Action UNCONFIRMED Item 14.45 Ref. Enc 01 Item SJM was attending the NHS EXPO event in Manchester to join a discussion on care data. The Board noted the verbal report STRATEGY 14.35 Fundraising strategy – Review and Update LM presented a review of the Trust’s fundraising strategy and emphasised the importance of the Trust establishing a strategy that was fully integrated with the Trusts long term plans. Fundraising is often the most visible part of the organisation and therefore cannot work in isolation. This was specifically important with the decision to pursue the new hospital project. A number of core objectives were highlighted, the principal one being to raise £10 million per annum by 2017/18. Whilst significant growth was noted in recent years, LM stated that there were key building blocks that must be put in place now to establish key networks/partnerships that will be essential in the future. To achieve this, the reliance on public fundraising via one large local capital appeal had to change in favour of supporting the hospital as whole and having a variety of projects on offer. Individuals, corporates and trusts are all looking for something different and we need to get more sophisticated by having the right proposition for each market. Another key objective was the need to invest in new technology to ensure prospective donors were being approached in the most effective way and the new database will strengthen the strategic overview functions. Furthermore LM wished to highlight that in order to deliver the fundraising strategy it was vital that the brand awareness of the Hospital was strengthened, which in turn would benefit long term fundraising strategies. The importance of promoting the Trust from a local, regional provider towards more of a Midlands and national profile would certainly enhance donations. In summary LM outlined critical areas to achieve planned growth. Firstly, a core proposition for individuals must be created, explaining why they should support the charity ahead of others, which will grow our individual giving income streams and in turn create more sustainable funding. A portfolio of fundraising projects must also be created. Over the next three years we plan to grow major gift and trust fundraising income by 300% and currently we don’t have a future pipeline. LM asked all to consider what process could be put in place to ensure we’re not missing opportunities. In addition, LM stated that current reviews and discussions in regards to fundraising systems were taking place to ensure that our operations were centralised and fit for Page 3 of 8 Action UNCONFIRMED Item 14.45 Ref. Enc 01 Item purpose to cope with predicted future volumes. LM highlighted the growing competitiveness of the fundraising market and emphasised the need to embrace a culture of fundraising within the hospital. It’s important for all staff to be able to articulate why fundraising approaches are being made and secondly to explain where their donations were going and for what reason. Discussion followed on the how the fundraising strategy was perceived; DM indicated that the philanthropy team at Barclays Wealth had suggested our targets were not ambitious enough, whilst JG added that there was still a wide spread misconception that the NHS still relied on central funding and didn’t need charitable support. To counter this MB suggested the fundraising message could be strengthened by emphasising the need and cost of medical research. VDi referred to the strong market penetration Great Ormond Street Hospital had achieved. SJM explained that this was due to the huge marketing machine their fundraising team enjoyed, but at the same time this highlighted the need for BCH to move away from being seen as a local provider, positioning in the fundraising market was vital. CH agreed and added that it was important to raise the BCH brand awareness. CB stressed the importance of promoting the fundraising brand in the culture of BCH – job specifications should have the message and importance embedded within them. Secondly would our ambitions be restricted by the proposed figure of £10m and whether we should have a silent target? The message would also benefit from including details of how fundraising had benefited the Trust – lives saved, the impact on patients. MM asked how going forward we would work in partnership with BCH Charities and emphasised the importance of working with them. The Board accepted the report and agreed to the outline proposals recommended. 14.36 Developing our Transformation – the EQUIP work stream CBN introduced a presentation on the Trust’s proposed Enabling Quality Improvement Programme (EQuIP). The EQuIP has been designed to oversee the planned transformation of services provided by the Trust. The transformation programme will provide dedicated project management support directly into front line services. The primary aim of the transformation programme is to deduce waste whilst maintaining and where possible improving quality in order to generate capacity to work differently. What individual services chose to do with any realised capacity from transformation is for each Directorate to determine. The transformation programme will be accountable to Senior Leadership Team (SLT). The transformation programme will be developed through two forums, a clinical and patient forum. Page 4 of 8 Action UNCONFIRMED Item 14.45 Ref. Enc 01 Item Operational initiatives will be reviewed and prioritised by the clinical and patient forums in order that the transformation programme concentrates it's efforts to areas of greatest need. In the year 1 four work streams have been identified; Theatre/Surgical, Outpatients, Pre admission and Drug management. It will be the role of the clinical and patient forums to prioritise initiates within these work streams. The transformation programme will be fully supported by a Programme Management Office (PMO). The PMO will ensure that all transformation work streams are sufficiently worked up in terms of milestones, actions, risks and outcomes. The PMO is an essential component of delivering the transformation agenda. To pump prime the transformation programme CBN shared that there is a business case for the Board to consider proposing a fixed term partnership with an engineering redesign company, Newton Europe (“Newton”). Newton offer expert skills in process engineering and their support would accelerate the redesign of services within the surgical and outpatients work streams. A piece of preliminary work completed by Newton identified a number of areas that the transformation programme could focus on to improve patient flow. Newton worked alongside our clinicians and our clinicians impressed by the Newton team analysis and their approach; feedback was consistently that Newton colleagues listened and adapted their models accordingly. TA emphasised the importance of this and the wider engagement with clinicians. Initial discussions had already taken place and feedback was encouraging. VDi supported the approach but emphasised the importance of clinicians been part of the operation. The Board stressed the importance of communication in this process: the approach and development of the transformation had to be done in partnership and not in isolation. SJM agreed – all projects had to fit together to avoid mixed or confusing messages to staff. CB expressed a degree of confusion. She felt the message was not clear enough and would be difficult to promote and ensure engagement. In conclusion the first clinicians meeting had taken place and the first patient’s forum would be held in April. The next steps would be Board approval to appoint Newton who would enable the operational change process and for the Board to invest in a PMO to manage the transformation. The Board accepted the report and agreed to the outline proposals recommended QUALITY & RESOURCES 14.37 Quality Report VD introduced the report containing a range of issues that had been reviewed and investigated during the month. Items of note included; Page 5 of 8 Action UNCONFIRMED Item 14.45 Ref. Enc 01 Item There were no serious untoward incidents in January 2014 and no Never Events since last April. An analysis of SIRIs showed no evidence that they occurred in particular ethnic groups or at specific times of the day or days of the week The crude number of deaths per 1000 patients, PICU and cardiac and liver transplant mortality run charts, plus reviews of individual deaths showed no evidence of systematic care failing . However, the trust's Hospital Standardised Mortality Ratio (HSMR) remained high. This had been looked at internally and it was felt that the current ratio calculation was not appropriately risk adjusted as it was predominately adult based and did not reflect paediatric diseases. VD said that the safety team were considering how to develop a more appropriate measure with the other children's hospitals, and how to introduce external review into the mortality process. SJM also asked whether deaths could be graded on 1-4 scale of preventability as had been done in the two previous mortality annual reports? VD said this would be done, but there would be a delay between the death and the report since the grading was done after speciality review and the trustwide mortality group. The current board report containing individual details of every death only relates an initial review by a senior nurse and senior doctor. In the updated list of current inquests, the background to item 4 was explained, based on a delay in administering antibiotics to a septic child on intensive care. The trust's own investigation had focused on systems but the trust solicitors had commissioned an expert opinion which focused more on the actions of individuals. This was being dealt with. MM reported. The patient feedback App was now attracting media interest. Safeguarding level 2 training was not good enough; the need to increase the figure was being reviewed, possibly by on-line training. The Safe Kids Audit tool was being looked at by Salford who were impressed with its function. The Board noted the report. 14.38 Performance Report DM presented the report, which had earlier been reviewed by the Finance & Resources Committee. The following key issues were highlighted and discussed; Diagnostic waiting list – MRI The original forecast which predicted the back-log of existing operations would be cleared by May now, due to a spike in February, suggested the trajectory would not be cleared until June. It was clear that the Trust didn’t have the capacity to manage unexpected increases in demand. Page 6 of 8 Action UNCONFIRMED Item 14.45 Ref. Enc 01 Item The service would benefit from the return, after maternity of a radiologist. In addition a range of measures were being examined to try and improve the position, including Saturday and Sunday working. Cancelled Operations In January 15 patients had their operation cancelled on the day due to hospital reasons. This was lower than previous months and the current average. However there were a further 39 patients who had their operation cancelled the day before and 4 patients who breached the 29 day standard in January. It was noted that the PWC report on this matter would be presented to the F&R Committee in March. Emergency Department Continues to perform well, meeting the 4 hour target in January. 18 Weeks The standard was met in January with performance at 90.3% against the 90% standard. The Board noted the report. 14.39 Resources Report A strong performance in January had led to the Trust being £2,113k above target. The forecast year end surplus of £8m was inflated by the unexpected receipt in the last two weeks of £2.1m for the CAHM’s service. This was unexpected, but presented a problem on how to explain the receipt at the year end. CIP performance had deteriorated against plan and now stood at 28% below planned schemes. The Trust had benefitted from a strong cash balance with reduced capital spend due to delays in the electrical infrastructure work and the cancer centre. TN reported. Sickness levels had reduced by 0.2%, dropping below 3.5% for the first time since September. The Trust was continuing to engage with staff on the impact of stress to help reduce the problem. Staff appraisal rates remained static at 83%, continuing to fall short of the 90% target. The Board noted the report Page 7 of 8 Action UNCONFIRMED Item 14.45 Enc 01 Ref. 14.40 Item Foundation Trust finances PF introduced a presentation centred on the NHS Quarter 3 Foundation Trust performance. From this it was clear that the Acute services remained the most challenged, particularly small/medium sized Trusts, with 18 of the 59 Trusts falling in this category facing financial difficulties. As a specialist Trust, BCH remained in line with average financial indicators for this sector. Specialist Trusts were the best performing sector. Overall the Midlands remained the most financially challenged area, with 14 of 38 Trusts in deficit and a further 14 of 37 non Foundation Trusts forecasting a deficit. The Board noted the presentation OTHER 14.41 Questions from the Public There were no questions from members of the public. Next Board Meeting: 27 March 2014, The Education Centre, BCH Page 8 of 8 Action Board of Directors Public Meeting 27 March 2014 “The Nursing Workforce at Birmingham Children’s Hospital” Item 14.49 Enc 02 Strategic Objective/ Enabler Report Title Sponsoring Director Author(s) Previously considered by Nursing Workforce – The story so far Michelle McLoughlin Michelle McLoughlin Andrew Gralton Quality Committee (20 March 2014) Finance & Resources Committee (25 March 2014) Situation It is essential that we have the right people, with the Right skills in the Right place at the Right time to enable us to provide the best care we can for the children, young people and their families who use our services. Background The dynamic nature of our services requires us to review and alter our clinical nurse workforce regularly to ensure we meet the care needs of the children and young people that require our services. To ensure consistency, changes are based on formal workforce reviews (skill mix) established within the trust and based on national standards and then daily amendments that meet immediate need. There is now a greater scrutiny on how the NHS provides care and a number of recent reports have been commissioned which reinforce this: Compassion in Practice (NHS England 2012) Report of the Mid Staffordshire NHS Public Inquiry (2013) Review into the quality of care provide by 14 hospitals trusts in England: overview report Prof Sir Bruce Keogh (NHS England 2013) A promise to learn, a commitment to act: improving safety of patients in England, (DoH 2013) The Cavendish review: an independent review into healthcare assistants and support workers (DoH 2013) Each has highlighted the importance of having a safe nursing staffing establishment in place. The NHS Quality Board have recently published: “How to ensure the right people, with the right skills, are in the right place at the right time”(DoH 2013) which takes the key element from all of the above reports and identifies a number of expectations regarding nursing staffing which will be used by our external partners (Care Quality Commission, Monitor, NHS Trust Development Authority, NHS England) to demonstrate safe and effective care. The Francis Inquiry and the government’s response has highlighted the need for safe staffing whilst the National Quality Board report on staffing emphasised the accountability of Board for ensuring staffing levels are in place. In a recent roundtable discussion itemised in a HSJ article (Feb 2014) it was noted that the key was to being able to demonstrate that systems and processes are in place 24/7, 365 days a year and that ultimately there had to be a focus on professional assurance. The round table discussion identified that there should be a warning against tick box exercises and whilst staffing may be an indicator of safety, organisations needed to be mindful not to fixate on them and make the process an industry out of collecting and measuring data. Further key points were around ensuring rosters were aligned to demand and pertinent to particular areas and that it is not just about reported numbers but getting out and seeing how staffing is delivered and very importantly listening to what our staff are telling us. Assessment Birmingham Children’s Hospital has an established process of managed nursing workforce reviews. These have been based on the foundations of setting the nursing establishments to deliver the staffing levels at the planning stage. It is essential that robust processes are in place to manage daily issues and then monitor for compliance and impact upon our nursing workforce and the quality of care they deliver. The nursing workforce reviews previously delivered at Birmingham Children’s Hospital meet all of the expectations currently recommended in the ‘Right People, Right Place, Right Time paper it is: Evidence based, Takes into account three key factors, workforce, activity and resources Produced from the ward team up Has multi-disciplinary involvement. Our process at BCH of ensuring safe staffing is based on:- 1. Skill mix foundation: National and International evidence, professional judgement, validation with activity and available resources. 2. Daily Management: The delivery of safe, compassionate care to children and young people in hospital is a 24 hours a day, seven days a week challenge. To ensure this is achieved the nursing management team has developed a robust process for the escalation of any issues both in and out of hours which ensures that safety is maintained with risk mitigation. We are currently reviewing this process to identify good practice and formalise current actions. 3. Monitoring: The review of ward/department use of staffing has been part of our process for some time, we have an electronic solution to staff rostering and are now working to triangulate this ongoing review with nursing care quality indicators, patient experience and safety data and would like to further enhance this by an electronic nursing dashboard. Future Work:As part of our next phase of working we are developing a Nursing Rota policy which will provide guidance on the expectations of the wards to use the workforce allocated in the reviews. We are producing a formal Escalation Policy which will build upon the established work of the Hospital Operations Centre and will formalise the complex decisions that Ward Mangers, Lead Nurses and the Heads of Nursing make on an on-going basis to ensure that the wards are safely staffed. We next plan to work with colleagues in the Workforce Directorate to utilise the forthcoming data from the Staff Friends and Family Test to ensure that our staffs views are part of this process. Our current assessment following a workshop attended by the Chief Nurse’s Nursing Leadership Team is that we are in a strong position to meet and deliver the 10 Expectations (as identified in “How to ensure the right people, with the right skills, are in the right place at the right time”(DoH 2013) however we need to explore how we formalise some of our operational practices so that we capture the complex and dynamic nature of nurse staffing and that we achieve the requirement of increased reporting detailed within the 10 Expectations. For example, operationally within the trust there is constant monitoring and management of skills and competencies and patient acuity from a ward to the Directorate and Hospital Operations Centre. This process engages all level of staff from ward to Head of Nursing, incorporating patient’s needs, acuity and staffing. While this process is very successful at meeting the needs of the patients we do not currently record emerging issues, the actions taken or the outcome achieved. It is evident that the majority of data required to be presented to the Board and public is already available within the current reporting systems. The aim of this next phase of work will be to collate all the current and new data into a single report. Engagement within the wider workforce within the organisation is being coordinated within each work-stream and at the most effective time. There is a pilot in April when all staffing numbers will be visible on the entrance to some wards. There will be monthly updates to the Board as part of the Workforce report in the Resources report. The Board will receive 6 monthly updates with the detailed information on nursing workforce. Recommendations The Board is asked to note the work already undertaken so far and the schedule for reports to the board. Key Risks Risk Description Controls Risk Description: Controls: There is requirement to reports staffing numbers to our commissioners immediately. This data needs to be accurate and understandable. We need to clearly explain why the data received from our Trust will be different that that received adult providers. Data produced about nursing workforce should be validated before it is presented our external Partners. Assurances Current practice standardised We currently have no real time Acuity system While risk mitigation occurs on an ongoing basis there is currently little record of this for example our need to produce an Escalation Policy or that there is not a real time Acuity system policy Key Impacts Strategic Objectives CQC Registration (state outcome) NHS Constitution Every child and young person cared for by Birmingham Children’s Hospital will be provided with safe, high quality care and a fantastic patient and family experience. The CQC is currently developing a new approach to monitoring, inspecting and rating providers, staffing capacity and capability will be central to this new approach Other Compliance (e.g. NHSLA, Information Governance, Monitor) Equality, diversity & human rights Trusts Contacts Others Monitor will expect that NHS Foundation Trusts have the right people, in the right place at the Right Time and will act where the CQC identifies deficiencies in staffing levels The need to have the Right people, in the Right place at the Right time must be developed in tandem with the Trust’s Equality and Inclusion agenda to better match the our workforce with the local population and our service users It is clearly defined that commissioners will actively seek assurance that the right people, are in the right place at the right time within providers with whom they contract. The Nursing Workforce at BCH: The story so far February 2014 Michelle McLoughlin, Chief Nurse Andrew Gralton, Head of Nursing Workforce Context The Francis Inquiry and the government response to it have highlighted the need for safer staffing. HSJ February 2014 identified that there can be no hotter topic in the NHS at the moment than getting the ‘right staff in place’. Five key papers have been produced in the last 18months setting out a road map to better care within the NHS • • • • • Compassion in Practice (NHS England 2012) Report of the Mid Staffordshire NHS Public Inquiry (2013) Review into the quality of care provide by 14 hospitals trusts in England: overview report Prof Sir Bruce Keogh (NHS England 2013) A promise to learn, a commitment to act: improving safety of patients in England, (DoH 2013) The Cavendish review: an independent review into healthcare assistants and support workers (DoH 2013) ‘Right People, Right Place, Right Time – A Guide to nursing and care staffing capacity and capability. (NHS England 2013) Context • There is evidence which suggests that there are better patient outcomes when people, in the right place at the right time. • There is no single ratio or formula that can calculate the answer to such a complex question, as how well is this ward staffed? • We need to be more open and transparent to our patients and the public about how wards are staffed. • It is thought that at this time staffing levels will not be mandated although there is much debate about this. Right People, Right Place, Right Time – A Guide to nursing and care staffing capacity and capability (2013). The paper contains 10 Expectations which are:1. Boards take full responsibility for the quality of care provided to patients, and as a key determinant of quality, take full and collective responsibility for nursing, midwifery and care staffing capacity and capability. 2. Processes are in place to enable staffing establishments to be met on a shift to shift basis. 3. Evidence –based tools are used to inform nursing, midwifery and care staffing capacity and capability 4. Clinical and managerial leaders foster a culture of professionalism and responsiveness, where staff feel able to raise concerns. 5. A multi-professional approach is taken when setting nursing, midwifery and care staff establishments 6. Nurses, midwives and care staff have sufficient time to fulfil responsibilities that are additional to their direct caring duties. 7. Boards receive monthly updates on workforce information, and staffing capacity and capability is discussed at a public Board meeting at least every 6 months on the basis of a full nursing establishment review. 8. NHS provides clearly displayed information about nurses and care staff on each ward, clinical setting, department or service on each shift. 9. Providers of NHS services take an active role in securing staff in line with their workforce requirements. 10. Commissioners actively seek assurance that the right people, with the right skills, are in the right place at the right time within the providers with whom they contract. BCH - Our story so far The key elements to understanding our nursing workforce • • • • Workforce Foundations Ongoing Monitoring Future State Planning Describing Workforce foundations On going monitoring Planning for future systems and processes Identifying out future aspirations Our Workforce Foundations; The Workforce Planning Reviews • • Professional judgement: Every Lead Nurse, Ward Manager, HoN External proposed challenges & advice Environmental factors e.g. Location re pt journey Layout of the ward (cubicles visibility) Uplift for: AL, Sickness, Non clinical time and Study (range 26.5-28%) Maternity Leave excluded • Each workforce review at BCH has been based on the best evidence available: We have developed tools when they have not existed – TMR & TMRG Model. Triangulated to ensure the outcomes are valid Output of the Workforce Reviews An establishment, that is the number of nurses for each ward was identified, the nurse to patient ratio and a subsequent skill mix expected per ward was defined. This is known as the staffing Plan . • Department Ward 1 Ward 2 Ward 5 Ward 7 Ward 8 Ward 9 Ward 10 Ward 11 Ward 12 Ward 15 Burns Emergency Dept Medical Day Care Medical HDU Neonatal Surgical PAU PICU Surgical Day Care Theatres Ashfield Heathlands Irwin Trust overview – January 2014 Clinical WTE est 21.2 33.8 28.7 21.6 39.2 36.8 33.5 34.2 33.4 64.8 24.3 57.8 11.5 18 35.5 33.7 258.2 16.5 157.3 28.5 23.8 26.5 • Beds Nurse to bed Skill mix % 12 20 15 12 13 19 18 16 16 28 7 N/A 14 6 16 19 28 18 N/A 8 14 12 1.8 1.7 1.6 1.9 3.0 1.9 1.9 2.1 2.0 2.3 3.5 0.8 * 3.0 2.2 1.8 9.2 0.9* 3.6 1.7 2.2 82 85 78 86 87 78 83 87 83 86 88 78 84 94 85 82 90 73 77 66 63 65 Ward level example Ward 8 Day/Shift ** Early Late Night Mon 6 (5/1) 7 (6/1) 5 (4/1) Tue 7 (6/1) 7 (6/1) 5 (4/1) Wed 6(5/1) 7 (6/1) 5 (4/1) Thurs 6 (5/1) 8 (7/1) 5 (4/1) Fri 7 (6/1) 7 (6/1) 5 (4/1) Sat 6 (5/1) 5 (5/0) 4 (4/0) Sun 5 (5/0) 6(5/1) 5 (4/1) Total staff (RN/CSW) ** No one day has the same requirement i.e. Thursday afternoon, ward round day Monitoring Our Nursing Workforce: Daily Escalation of Staffing Issues REVIEW PROCESS • 24 hour service; staffing issues can occur at any time. • In hours escalation from ward nurse in charge, to Lead Nurse to Head of Nursing; issues raised at bed meetings by Lead Nurses for shared resolution • Out of hours, ward nurse in charge escalates to clinical coordinator • Actions taken in/out hours to resolve or mitigate staff shortfalls • Actions include moving staff from other areas, staff rostering reviewed, bank staff requested, study leave cancelled. Just looking at the nursing numbers is not the solution its about assurance of real time assessments (HSJ Feb 2014) IN DAY TIMELINE – 8.30 Surgical bed meeting to review staffing numbers/acuity/admissions – 9.30 Hospital bed meeting; Lead Nurses representing all areas. Hospital Safety Check covering Staffing/Acuity/Risk/Flow – 13.45 Bed meeting as above. Repeat Hospital Safety Check – 16.00 Additional bed meeting if required – 19.00 Clinical coordinator and On call Senior Manager review. Hospital Safety Check Monitoring Our Nursing workforce: Right Skills , Right Numbers, Right Place • • • • • • • Establishment is a starting point The right skills at the right time need to be achieved. The Rotas policy & procedural guide established roles, rules and articulated expectations. The implementation of an electronic rota system, providing a monitoring system recording our actions and allows for trend analysis. Workforce reports are already produced (resources report). It is crucial that there is not just one data source. Listening to staff is always the key. Monitoring: Our Every Day Management of the Nursing Workforce Current State • Each day each ward/department assesses their workforce: • In relation to the: • Number of patients • Acuity of patients • Speciality • This is done at ward, Directorate level and hospital level and involves nurse of all levels Future State • Developing from a practice into a process solution: – Establishing a data set – Recording our actions Need an IT – Producing a highlight report solution – Reporting via the Dashboards Planning our Response to the 10 Expectations • Working groups have been established to undertake the gap analysis for each of the Expectations. • We have a detailed gap analysis against the 10 Expectations from the Right People , Right Place, Right Time. • Action plans have been prioritised against the gap analysis. Future priority areas:• The formalisation of the current daily nursing escalation process – Established practices to formalise the process. • The development of a Ward level Nursing Dashboard so that we can publicly display our daily nursing numbers at ward level – First trial April 2014. Future State : Providing Assurance to the Board Assurance: – A monthly report of compliance with the staffing plans to enhance current workforce information in resources report to the Board. – A 6 monthly update to the Board regarding nursing workforce establishment. Monthly Board Assurance Framework Monthly Workforce Resources Report BOARD ASSURANCE FRAMEWORK JANUARY 2014 Item 14.20 Risk No. Enc 02 Current Risk Score & movement Strategic Risk 1.0 Failure to change the culture of the workforce may prevent the Trust from meeting its strategic ambitions. 4x5=20 3x4=12 2.0 Failure to match our service demands to specialist workforce requirements will reduce capacity and quality of services and impact on the achievement of our strategic objectives. 4x5=20 3x4=12 3.0 The service experience for the patients we treat and their families is poor impacting on both clinical outcomes and Trust reputation. 3x5=15 2x4=8 4.0 Failure to have long term plan for the physical estate on Steelhouse Lane will frustrate the ambitions of the organisation to further develop its reputation and services. 4x5=20 3x5=15 5.0 Inability to provide the physical capacity over the medium term on Steelhouse Lane will mean failure to deliver demand and generate the resources for a new hospital. 4x5=20 3x4 = 12 6.0 An inability to innovate in the way in which we provide care reduces access to and quality of our services. 4x5=20 3x4=12 7.0 Unnecessary harm is caused to our patients 4x4=16 3x4=12 8.0 The Trust’s IT infrastructure is inadequate for future business needs. 4x4=16 3x3=9 9.0 Failure to work collaboratively across the city/region. 3x4=12 3x3=9 10. Failure to capitalise on growth and innovation opportunities 3x4=12 3x3=9 11. Failure to manage the resources available to the Trust in an effective manner. 4x4=16 3x3=9 12. Failure to manage timely access to patients who require surgery so the Trust meets its 18 weeks target 4x4=16 3x3=9 Board of Directors Public Session 27th March 2014 Item:14.51 Report Title Sponsoring Director Author(s) Previously considered by Enc. 03 Monitor Operational Plan for BCH 2014-2016 Matthew Boazman, Director of Strategy & Planning Matthew Boazman, Director of Strategy & Planning (Lead Author) Chief Officer’s Finance & Resources Situation The Trust is required to submit its organisational plans to Monitor on an annual basis as part of the Annual Planning Review (APR) process. New planning guidance has been recently issued by Monitor which outlines the changes to the planning cycle for 2014/15 onwards. The attached document covers the operational planning (2014-2016) requirements set out by Monitor as part of this planning framework. Background The planning framework for 2014/15 has changed significantly from previous years in order to address some of the gaps identified by Monitor following their review of organisational submissions for 2013/14. Some of the key changes are summarised briefly below: Increased strategic focus Requirement for robust engagement across Local Health Economy (LHE) Requirement to self-assess organisational viability Supported by long term financial projections and modelling The requirement to ensure there is a robust engagement process with key local stakeholders is particularly prominent within the planning framework- this includes ensuring that there is a strong alignment between provider and commissioner planning assumptions compared to previous years. In order to develop a robust strategic plan Monitor considers it essential that organisations can demonstrate the minimum following steps within their planning cycle: - Put in place a robust planning process and, in particular, ensure sufficient and appropriate engagement with the key stakeholders within the Local Health Economy (LHE) Assess the risks to sustainability of high quality services in conjunction with LHE stakeholders by drawing on accurate inputs that have been analysed and presented correctly Assess the options available to address the identified sustainability risks in conjunction with the LHE stakeholders and make choices on which option(s) are most appropriate Define a vision for sustainability and develop the key initiatives which underpin this, where appropriate, in conjunction with LHE stakeholders Set out a plan for delivery including financial projections which are internally consistent and based on credible assumptions Assessment In order to comply with the planning guidance BCH must submit two separate planning documents which will cover the key operational and strategic challenges: A two-year operational plan for 2014-2016 - Submission by 4th April 2014 Review by Monitor April-May 2014 Assess FT understanding of the challenges it faces Assess engagement and alignment with key stakeholders Evaluate the congruence of commissioner and provider activity and revenue assumptions Assess the level of planned capacity available compared to the predicted demand Review robustness of Cost Improvement Plans and efficiency programmes A five-year Strategic and Sustainability Review Plan - Submission by 30th June 2014 Review by Monitor July-September 2014 Assess the robustness of the strategic planning process A review of the FT plans for securing its long term clinical and financial sustainability An assessment of the strategic options that the FT believes are available to ensure the sustainability of high quality services for patients Assess engagement and alignment with key stakeholders Evaluate the congruence of commissioner and provider activity and revenue assumptions over the five year period Completed gap analysis against the best practice self-assessment framework The FT Board is required to complete a self-assessment of its longer term sustainability (Declaration of Sustainability) and outline the key points to support its conclusions Recommendations The attached document is the two year operational plan covering the period 2014-2016. The content included is aligned to the planning guidance set out by Monitor and covers the specific sections Monitor expects to be detailed within the submission. As part of the submission process the Board of Directors is required to review and support the plan and the final version must be formally signed off by the Chair, CEO and CFO for submission on 4 th April 2014. Key Impacts Strategic Objectives NHS Constitution Other Compliance (e.g. NHSLA, Information Governance, Monitor) Equality, diversity & human rights The operational plan links with all of the strategic objectives None The operational plan is a core component of the Monitor annual planning and compliance requirements None Operational Plan Document for 2014-16 Birmingham Children’s Hospital NHS Foundation Trust DRAFT : VERSION 7 1 Operational Plan Guidance – Annual Plan Review 2014-15 The cover sheet and following pages constitute operational plan submission which forms part of Monitor’s 2014/15 Annual Plan Review The operational plan commentary must cover the two year period for 2014/15 and 2015/16. Guidance and detailed requirements on the completion of this section of the template are outlined in section 4 of the APR guidance. Timescales for the two-stage APR process are set out below. These timescales are aligned to those of NHS England and the NHS Trust Development Authority which will enable strategic and operational plans to be aligned within each unit of planning before they are submitted. Monitor expects that a good two year operational plan commentary should cover (but not necessarily be limited to) the following areas, in separate sections: 1. Executive summary 2. Operational plan a. The short term challenge b. Quality plans c. Operational requirements and capacity d. Productivity, efficiency and CIPs e. Financial plan 3. Appendices (including commercial or other confidential matters) Please note that this guidance is not prescriptive and foundation trusts should make their own judgement about the content of each section. The expected delivery timetable is as follows: Expected that contracts signed by this date 28 February 2014 Submission of operational plans to Monitor 4 April 2014 Monitor review of operational plans April- May 2014 Operational plan feedback date May 2014 Submission of strategic plans to Monitor 30 June 2014 (Years one and two of the five year financial plan will be fixed per the final plan submitted on 4 April 2014) Monitor review of strategic plans July-September 2014 Strategic plan feedback date October 2014 2 Operational Plan for y/e March 2015 and 2016 This document completed by (and Monitor queries to be directed to): Name Matthew Boazman Job Title Director of Strategy and Planning e-mail address Matthew.boazman@bch.nhs.uk Tel. no. for contact 0121 333 8533 Date 04/04/2014 Approved on behalf of the Board of Directors by: Name (Chair) Keith Lester Signature Approved on behalf of the Board of Directors by: Name (Chief Executive) Sarah-Jane Marsh Signature Approved on behalf of the Board of Directors by: Name (Finance Director) David Melbourne Signature 3 1. Executive Summary Birmingham Children‟s Hospital NHS Foundation Trust provides children‟s health services for young patients from Birmingham, the West Midlands and beyond, with over 240,000 patient visits every year. We are one of the UK‟s four standalone children‟s hospitals, one of 33 providers of specialised children‟s services, and one of the UK‟s 246 trusts providing hospital paediatric services to the local population. We provide 11+ national services, 30+ services to children and young people in the West Midlands, and general and emergency services to the south and central population of Birmingham. We are characterised by a unique co-location of all the services, specialist expertise and diagnostic and treatment resources that a sick child needs. The population is characterised by diseases which have one or more of the following features: rarity, complexity, co-morbidity, unresponsiveness to conventional therapy, age or acuity. Our hospital is home to: 54 specialties 11 Nationally Commissioned Services 150,000 outpatient visits a year 50,000 Emergency Department patients a year 44,000 inpatient admissions each year 244,000 patient visits per year 360 beds across 16 wards at Steelhouse Lane and 4 Child and Adolescent Mental Health Services (CAMHS) wards at Parkview in Moseley 14 theatres 61 parent and family accommodation rooms – the largest facility in Europe KIDS regional emergency transport service Wellcome Clinical Research Facility 31 bedded PICU £239m annual income 3,500 staff The issues we are facing with increasing high demand for our services means we have to continue to grow our capacity at a rapid pace, not just by building new facilities, but also by organising ourselves differently to improve our patient pathways. We need to redesign our workforce to use our skilled professionals in new ways and invest in technology to enable change. If we look ahead to the next five years, our local population is expected to grow significantly, and we will see thousands more children every year, with even more complex conditions. Our analysis tells us our current 150 year old hospital will simply not be able to cope with this demand, so we have been developing options for a new hospital, either at our current Steelhouse lane site or at Edgbaston within the City. The development of Birmingham‟s first purpose-built children‟s hospital is an exciting and important step in our future strategy, but we fully recognise that 2022, the very earliest it could be built by, is too long to wait, and it is essential that we invest in our future now, to be able to cope with our current demand projections. For that reason, we are launching our Next Generation project in April 2014 and this will form a key element of both our operational and strategic plan for the next ten years up until 2024. 4 2. Our Vision The Trust‟s strategy is based on our mission, which is “to provide outstanding care and treatment to all children and young people who choose and need to use our services, and to share and spread new knowledge and practice, so we are always at the forefront of what is possible.” This is supported by a clear set of strategic goals and our vision of being the leading provider of healthcare to children and young people in the UK, whatever their condition and wherever they need our expertise. Our Mission To provide outstanding care and treatment to all children and young people who choose and need to use our services, and to share and spread new knowledge and practice, so we are always at the forefront of what is possible. Our Vision To be the leading provider of healthcare to children and young people in the UK, whatever their condition and wherever they need our expertise Our Strategic Goals Figure 1 The Trust Vision for 2014-2016 3. The Trust Priorities 2014-2016 As part of the business planning process in 2013 the Trust agreed a set of three year operational priorities covering the period 2013-2016. These have been reviewed at the end of year one to take into account progress to date and to reflect any key changes to our priority areas and the refreshed priorities for 2014-2016 are outlined in figure 2. 5 Figure 2 Our Priorities for 2014-2016 We will strengthen Birmingham Children’s Hospital’s position as a provider of Specialised and Highly Specialised services, so that we become the leading provider of healthcare in the UK •To develop and promote our strategy for rare diseases •To be more ambitious in our delivery of specialised mental health services, ensuring children and young people receive the best care in the best environment Every child and young person requiring access to care at Birmingham Children’s Hospital will be admitted in a timely way, with no unnecessary waiting along their pathway •To ensure that no child or young person has their appointment or operation cancelled, unless there is unforeseen urgent clinical priority. •To provide high quality consistent emergency medical and surgical care by improving the patient journey and removing all unnecessary delays. Every member of staff working at Birmingham Children’s Hospital will be a champion for children and young people. We will continue to develop Birmingham Children’s Hospital as a provider of outstanding local services: ‘a hospital without walls’, working in close partnership with other organisations •To further develop our position as an advocate and provider of public health advice, improve the lives of our patients, and all children and young people across Birmingham •To further strengthen the voice of children and young people in how our services are run and how we promote healthy lifestyles •To improve the quality of end of life care •To improve the life chances for young people with a learning disability by developing a range of employment opportunities •To continue to develop, with our partners, a Birmingham Children’s Network, that enables high quality, high value health care for children and young people across Birmingham •To work with primary care partners to examine how we might come together to best provide first line care for children and young people •To examine, with partners, how we best provide community mental health services for children and young people, given the budget reductions expected from commissioners Every child and young person cared for by Birmingham Children’s Hospital will be provided with safe, high quality care and a fantastic patient experience Every member of staff working at Birmingham Children’s Hospital will be looking for, and delivering better ways of providing care, at better value •To further develop our approaches to gaining feedback from staff, children, young people and families to ensure that their voice is heard at every level of the organisation •To further innovate our systems to promote and enhance patient safety and reduce avoidable harm. •To introduce technology to improve the service safety, quality and experience •To build an organisation of high performing teams, focussing on quality 6 •To review whether we have the right people, with the right skills, undertaking key roles to ensure we can provide high quality services within the resources available •To support and develop innovation in the delivery of care by redesigning a range of of clinical pathways •To explore how we can work with partners, to improve our commercial offer in order to further support our NHS services 4. Operational Plan 4.1. Our Short-Term Strategic Analysis- Summary Over the past year the Trust has undertaken a detailed strategic analysis to support the development of our organisational strategy which has considered: The specialist nature of the hospital and responding to the increasing centralisation of complex services into a few national centres as part of the emerging NHS England strategy. Developing the local Birmingham and West Midlands acute paediatric service offer, working closely with other local paediatric providers such as Heart of England NHS Foundation Trust and Sandwell & West Birmingham Hospitals NHS Trust in partnership with the local commissioners to identify how local paediatric services are best delivered. Extending clinical networks into the community and secondary care across the West Midlands. Providing a complete service for children and young people with mental health problems from specialist community to complex inpatient care. Developing and promoting our strategy for research and rare diseases in line with the UK National Strategy. Improving the quality of our end of life care. Championing the health and well-being of children and young people in Birmingham, across the West Midlands and nationally. The need to address capacity issues in our estate in both the short and long term Some of the key challenges that we are facing and that have influenced the development of our strategy in both the short and medium term are briefly outlined in figure 3. These will be explored in greater detail within the strategic plan that will be submitted to Monitor in June 2014. Within the context of this operational planning document the specific elements that are driving our short-term capacity model and the associated operational challenges will be considered in greater detail. Demographics Clinical Evolution and Technology National Designations BCH Patient and Family Expectations Policy and Finance The changing face of secondary care Workforce Figure 3 Key Strategic Issues for BCH 7 Patient & family expectations: - for children and young people coming into hospital can be a frightening and disorientating experience. Currently much of the hospital is based on old-fashioned Nightingale wards that offer poor privacy and space for our patients. Upgrading to more single rooms will offer greater dignity and privacy and also allow parents to sleep next to their children. Workforce: - healthcare is primarily a service-based industry, delivered by people. The Trust‟s aim is to attract and retain the best and brightest people in what is becoming an increasingly competitive labour market. The number of available senior doctors and nurses is gradually decreasing and we will be competing for a diminishing pool of healthcare workers with other children‟s health care providers both within the UK and internationally. This is explored in more detail in the people strategy. Clinical service evolution and technology: - our current estate, due to ad-hoc expansion, does not provide ideal clinical adjacencies, leading to inefficiencies for staff. In addition the core of the estate is based on Victorian buildings and does not have the capacity to accommodate large-scale cutting edge technology such as inter-operative MRI. Many of the Trust‟s national and international competitors are investing heavily in new infrastructure (Manchester, Liverpool, Sheffield and Great Ormond Street) and in order to achieve our service ambitions BCH will need to respond. 4.2. Understanding our Demand In order to develop the operational plan for 2014-2016 it is important that we fully understand our future demand and capacity requirements. As part of our operational planning we have therefore modelled through the expected demand for the next two years based on a range of indicators that are outlined in figure 4 below. These will all have an impact on the future capacity requirements across BCH, both in terms of workforce and estate, and have helped to form the basis of both our longer term strategic modelling and our two year operational plan modelling. The factors that will have an influence between 2014-2016 will be explored further within this operational planning document, whilst the longer term factors will be covered further in the strategic planning document. Figure 4 Factors Influencing Future Service Demand 8 4.2.1. Demographic & Population Changes The birth rate in the West Midlands is currently rising, and combined with the effect of migration, urban centres including Birmingham are experiencing very rapid rises in the number of children and young people living within them. This has a direct impact on the number of children and young people requiring treatment, and using our services. Birmingham Children‟s Hospital serves a local, regional and national population, and has developed an adapted demographic trend model, that adjusts for local authority specific population projections derived from ONS data. This enables BCH to recognise the differential impact of local population changes on secondary care services, and national changes on the specialist paediatric care market. It gives both a short and long term forecast on likely activity change, which then underpins forecasting in relation to other factors influencing place and volume of care within services for children and young people. BCH‟s active model is based on 2013 data, with forward projections to 2021 by year, and a long term forecast to 2030. It shows a 7.1% increase in total hospital activity by 2021 from 2013 baseline, rising to a total increase of 8.5% by 2025. The most significant rise in volume is in the 0-4 age group, although the largest proportional rise is in 5-9 year olds. The model also predicts a shift in length of stay, with increasing number of admissions in ages that historically have shorter lengths of stay. Based on demographic change, we expect to see a 4.7% rise in demand for bed days due to the majority of growth in ages with slightly shorter average lengths of stay. Figure 5 Demographic Changes for West Midlands 2013-2030 (ONS Data) Outside of London, the West Midlands is also the most ethnically diverse region in England and Wales. The ethnic diversity of the population has a significant impact on activity profiles due to rises in case-mix complexity and birth rates, leading to an increase in demand and rising complications from consanguineous relationships. Understanding the age profile and demographic of the West Midlands population and the expected shifts over the next few years is critical for ensuring that we are able to accurately model expected demand by service area. All of our services have a relatively unique age profile, in terms of peak activity levels and linking this to the known population changes enables us to predict more accurately the demand and variation at a specialty level rather than population based level. 9 An example of the methodology that has been used is outlined in figures 6 and 7 below, which illustrates the significant impact that this can have at a specialty level and point of delivery (theatres, outpatients, inpatient beds) for BCH. This has informed our operational planning and specialty level activity modelling for 2014-2016 and beyond. Figure 6 Admission Profile by Specialty 2012-2021 Figure 7 Bed Day Requirement 2012-2021 Overall we see that demographic change alone will increase activity by an additional 1,500 bed days by 2015, with the largest growth in paediatrics, paediatric surgery and clinical haematology and blood/marrow transplantation. As part of the original Strategic Outline Case, developed initially in 2012, we also combined the demographic changes with intelligence gathered from our clinical leads regarding service changes, clinical practice and emerging trends. This generated the high level activity modelling for 2020, outlined in figure 8 below, and we are due to revisit this as part of phase 1 of the Next Generation project. 10 Figure 8 Predicted Activity Levels 2010-2020 (BCH Strategy Unit Modelling) 4.2.2. Market Assessment In addition to understanding demographic changes it is important to also consider changes linked to market share and competition from other providers. A full market analysis of key competitors for Birmingham Children‟s Hospital has been undertaken as part of the strategic planning process and will be outlined in detail within the June submission as per the guidance. It is important to also consider whether or not there are likely to be any major market shifts within the lifetime of this operational planning document- 2014 to 2016. We have evaluated whether there is likely to be any key changes to the paediatric market within the next two years based on our strategic assessment and this is briefly summarised below for both the secondary care and specialised services market. The Market for Secondary Paediatric Care- It is possible to evaluate the current strength of BCH in the secondary care market by analysing market share data. Over the last few years BCH has continued to increase its overall market share within the West Midlands region for the provision of paediatric care (figure 9). The data set covers all locally commissioned activity for 0-18 year olds- it is not possible to evaluate share for the 0-16 age group although it is clear BCH would occupy a higher market share percentage in as their presence is diluted by the inclusion of patients aged 16-18 in this analysis. The increased share illustrates the relatively low risk from other competitors within the secondary care paediatric market. This, coupled with our intelligence developed through the Children‟s Health Network, local commissioners and the Royal College of Paediatrics supports the view that secondary care provision of paediatrics is reducing amongst some providers, with activity shifting to specialist centres, such as BCH, potentially as a result of the difficulty of maintaining expertise and clinically viable rotas. Figure 9 Percentage Change in Provider Activity 2006-2011 (HED Data) 11 Specialised Services & The Emerging NHS England Strategy- In terms of the regional specialised services market BCH is effectively the monopoly provider for the majority of commissioned services with no other immediate regional competitor. Competition for the specialist paediatric market is therefore primarily at a national level and continues to be influenced by service designations and direct competition with specialist nationalist providers. BCH remains in a strong position with regard to the number of nationally commissioned services provided (figure 10) and there is no indication that market share will decrease over the period 2014-2016. 19 Number of Nationally Commissioned Services 12 11 9 9 9 7 7 6 5 Figure 10 Number of Nationally Commissioned Services (Adult and Paediatric) BCH is well placed in terms of the maximising the potential opportunities that may arise from the emerging NHS England strategy for specialised services. The strategy proposes that specialised services are provided in centres of excellence and that the number of nationally commissioned providers reduces significantly from the current number. This aligns well with the strategy that we have developed and the expansion of our estate, as part of the Next Generation project, gives us the flexibility to expand our market share as a result as the model is implemented. Figure 11: Developing Model for Specialist Service Provision 12 4.2.3. National & Local Commissioning Priorities It is critical that our plans are congruent with both national and local commissioning priorities and seek to address some of the challenges that will be faced across our Local Health Economy (LHE) during the next two years. Having an affordable and realistic financial offer from local, regional and national commissioning bodies continues to be important for maintaining and growing market share. Within our LHE we have engaged through the local Joint Clinical Commissioning Group and have presented both the long term strategic challenges and shorter term activity projections to our commissioning partners to ensure that they are supportive of our operational planning assumptions. The commissioning architecture of the NHS has changed significantly during 2013 as a result of changing national policy. As we are now coming towards the end of the first year under this new architecture the impact and risks identified last year have been reviewed and updated based on experience during the year. These are outlined below. - National service specifications Provider led networks Funding for high cost drugs and devices and new treatments Impact Risk/Opportunity Mitigation/Action National service specifications are now in place for all prescribed services, where previously there have been none. Compliance exercise highlighted a small number of specifications where the Trust was non-compliant; there is a risk that there will need to be significant investment if specifications are not changed. Actions identified for all specifications where there are gaps There are approximately 60 service specifications that are applicable to the Trust. Opportunity to increase market share for services that are able to demonstrate full compliance Move to provider led networks for some specialised services. As a specialist trust this will mean that BCH will be acting as the lead for the network and so commissioning services from other providers e.g. Cystic Fibrosis where a shared arrangement with BCH as the host st has been in place from 1 April 2013. Trust is accountable for the performance of all members of the network and if standards are not met the Trust would be responsible for improvement. Consolidates position as specialist provider. Increases the opportunity to improve standards and care across network and drive innovation. 13 Issues have been raised directly with commissioners and through clinicians that sit on the Clinical Reference Groups. Derogations currently in place but not yet received clear feedback on the future impact, the issues raised are not unique to BCH. For Cystic Fibrosis work stream an internal project group has been established which considers: Contracts and finance Quality standards In addition a wider stakeholder group is in place which will look at the development of the network. BCH is heavily engaged in a range of national networks and is also leading on the development of regional network models for surgery High cost drugs, devices and innovative treatments not on the approved list which previously would have been funded through Individual Funding Requests (IFR) Delays in treatment or treatment not authorized. Financial risk if drugs are authorized for use and funding not secured. Internal process strengthened to identify new drugs and treatments as well as process for individual funding requests. Internal group established for BCH staff who are members of Clinical Reference Groups Figure 12 Commissioning Changes & Implications 2014/15 Under the new commissioning arrangements approximately 75% of services are now prescribed services and commissioned directly by NHS England. The local area team have highlighted that there is a deficit predicted across their portfolio for 2014/15. Contract negotiations for 2014/15 are based on forecast outturn for 2013/14 with no growth included. Given the demographics for the region there is an expectation that there will continue to an increase in demand, this is acknowledged by commissioners but not within contract baselines. There is limited opportunity for new developments except where these can deliver QIPP. 4.2.4. Service Reviews and Reconfigurations In addition to the changing commissioning architecture across the NHS outlined above there are also a range of commissioner led initiatives that have also been considered as part of our operational planning. - Review of paediatric critical care QIPP and demand management initiatives Decommissioning proposals Any Qualified Provider tenders Impact Risk/Opportunity Mitigation/Action Opportunity to improve capacity across the region and therefore improve flow within BCH BCH are fully engaged in the review. Provides stability in 2014/15 but does not provide any support in reducing demand on services. BCH has identified a small number of areas where QIPP could be achieved for commissioners. We will continue to share ideas where possible. Critical care review NHS England commissioners are to carry out a review of critical care provision across the region - will include intensive care and high dependency care provision QIPP and demand management Commissioners have not identified any areas where they plan to implement demand management plans or to apply QIPP as part of the 2014/15 contract. 14 Decommissioning Commissioners have indicated that they will be decommissioning the current community CAMHS. This will be subject to competitive tendering in 2014/15 with the new contract going live from October 2015. Impact on morale of the workforce and risk of staff leaving. . Financial risk associated with tender process for BCH. Inability to redesign service for 18 months. Regular communication with staff is in place to keep them informed. Management team within the service is working to continue to make improvements where appropriate. Current outcome measures are positive and will continue to be monitored. Any Qualified Provider Limited impact for the Trust. A 0-25 year old mental health service is being tendered for Birmingham which will include the current CAMHS. Loss of contract, new provider operating in Birmingham for CAMHS. Delivery of the new service would mean a partnership with another provider so that the full range could be delivered. This is being explored. Significant resource will be needed to deliver the bid. Loss of the contract for community services may impact on our ability to continue to provide Tier 4 services. National congenital heart review. Launched a year ago following the end of Safe & Sustainable review. Examines the organisation of children‟s and adults congenital heart services across England. Further development of BCH as a larger specialist centre. The timetable for implementation of the new standards led approach is at the earliest during the 2015/16 financial year. Trust has representation on both the clinical group management group supporting this change. Assumed no impact other than natural demand increases in our modelling. Figure 13 Service Reviews 2014/15 and Impact Assessment 4.2.5. Children and Adolescent Mental Health Services (CAMHs) During the planning period covered by this plan commissioners are undertaking a market testing exercise on our community CAMHs. The Trust is commissioned to provide these services for children and young people up to the age of 16. Birmingham & Solihull Mental Health Foundation Trust is commissioned to provide the services for ages 18 plus. The commissioning strategy is to market test the whole 0-25 service and they have indicated that the successful bidder will be characterised by a single lead provider. The tender process is expected to be completed by April 2015 with full transition by September 2015. 15 The Trust has consistently cross subsidised community CAMHs from other service lines and commissioners had proposed a further funding reduction of £1.4 million per annum from April 2014. We have been able to secure transition funding of £2.1million to cover an annual funding gap of £1.4million over the period until September 2015. We are currently working with other partners in developing our intent to bid. Our financial plans assume a downside financial scenario – (the specific details of which are of a commercial nature). 4.2.6. Regional Reconfiguration and the Potential Impact on BCH 2014-2016 As part of our operational planning for 2014-2016 we have considered three potential sector reconfigurations that may have an impact on BCH during that time frame. - Worcester Acute Hospitals Mid-Staffordshire NHS Trust The George Eliot Hospital Worcester Acute Hospital Reconfiguration- one of the major potential service reconfigurations within our Local Health Economy relates to the reorganisation of Worcester Acute Hospital NHS Trust. The Future of Acute Hospital Services in Worcestershire Report of the Independent Clinical Review Panel was published in January 2014. The suggested changes that affect paediatrics are: Paediatric inpatient beds should be closed at the Alexandra Hospital (AH). A networked “emergency centre” should be developed at AH. The emergency department at AH will be adult only. A 24 hour Urgent Care Centre (UCC) and a minor injury unit should be developed at AH, both of which will treat children. A paediatric assessment unit (PAU) should be developed at AH and will be open until 10pm. PAU will accept referrals from the UCC and GPs. Consultant led maternity services at AH should be moved to Worcester Royal Hospital. Figure 14 Outline of Proposed Worcester Reconfiguration The current proposals are going out to public consultation with implementation being completed in 2015/16 at the earliest. It is therefore possible that the proposed model for Worcestershire will not be 16 implemented during the two years covered by this operational plan. However, it is necessary to consider what the implications might be if the new model was to be implemented, particularly whether it will lead to an increase in paediatric attendances. Some of the key issues that we have considered are: • • • The potential increase in A&E attendances Increase in the number of emergency admissions at BCH, which may increase even further after 10pm when the paediatric assessment unit at AH closes. Some mothers will choose to go to Birmingham Women‟s rather than Worcester Royal Hospital for maternity care, potentially linked to easier public transport. Therefore there may be increased transfers from Birmingham Women‟s Hospital NICU to BCH. The impact of travel time has been considered in further detail by looking at the main post codes areas where our activity comes from in terms of paediatric activity across Worcestershire- the two highest concentrations are unsurprisingly focused around Bromsgrove and Redditch. Using this data it is possible to review the likely travel time associated with road and public transport as this was highlighted as one of the key factors within the review document for determining patient, and parent, behaviour and has also been highlighted by the King‟s Fund as one of the key determinants in patient behaviour. The data (figure 15) illustrates the potential impact public transport may have on choice. At this stage we have therefore assumed that there will be some shift in activity that might come to BCH within the next two years as a result of the WAH reconfiguration. Figure 15 Travel Times for Bromsgrove & Redditch Residents Mid-Staffordshire NHS Trust- pending the implementation of the Trust Special Administrators (TSA) recommendations, paediatric flows through Mid Staffordshire will alter significantly. Historically, Mid Staffordshire has treated approximately 9,000 Finished Consultant Episodes (FCE) for paediatrics, largely focussed around short stay admissions. It undertakes around 1000 paediatric surgical procedures per year, but these are largely non-complex. The trust does not have a paediatric surgery department. Our flow assessment aligns with the TSA report that the majority of this activity will now be undertaken through University Hospital North Staffordshire and hospital providers in the Black Country with minimal impact on demand at BCH. We continue to monitor the outcomes of the review around consultant led obstetric services on the Stafford site, as this is also likely to impact on future paediatric service models North of Birmingham. George Eliot- there is some potential for paediatric services at George Eliot hospital to be reconfigured, as part of the hospital‟s future model review. The new service model includes a PAU at George Eliot, with onward referral to University Hospitals Coventry and Warwick (UHCW) Trust. The needs assessment identified activity of 1676 inpatient admissions, but estimated only 12 per week would require transfer for inpatient care, for which UHCW is developing additional capacity. Our flow analysis again suggests that any further changes would have minimal impact on our inpatient and surgical services. We have identified a geographical sector that would potentially use Birmingham Children‟s Hospital if no services were to be available at George Eliot, but population density is low in these areas, and any impact would be shared with UHCW. We do not therefore envisage there being any major impact as a result during 2014-2016. 17 4.3. Dealing with Demand- operational capacity for 2014-2016 As outlined in section 4.2 above there are a range of factors that will influence, and in the majority of cases increase, the likely demand on our services between 2014-2016. These will continue to present us with real challenges in terms of service demand, particularly across some of our more specialised clinical services, such as PICU and cardiac surgery. 4.3.1. Next Generation Project The issues we are facing with increasing high demand for our services means we have to continue to grow our capacity at a rapid pace, not just by building new facilities, but also by organising ourselves differently to improve our patient pathways. We need to redesign our workforce to use our skilled professionals in new ways and invest in technology to enable change. For that reason, we are launching our Next Generation project in April 2014. This project has two phases; - Phase 1- today until 2022 Phase 2- our new hospital from 2022 and beyond Planning for these will overlap, but they are part of the same ambition for children and young people. Next Generation must not be seen as purely a buildings project as both of these phases are about more than just bricks and mortar, and have four key components: 1. 2. 3. 4. Patient pathways – How can we make them the very best they can be? People – What teams and skills do we need to invest in to make these pathways a reality? Technology – How can technology act as a catalyst to radical new ways of delivering care? Facilities – How can our buildings help us to increase capacity, and improve the environment? Patient Pathways Better patient pathways improve patient care and help us maximise our capacity The paths that our patients take to get to us, the way they are looked after while they're here, and how 18 this continues when they've gone home, is what makes their experience of care what it is. We know that in general, our children, young people and families want to get better and get home as soon as they can, and we work hard to make that happen. One of our most recent improvement projects has been to our emergency care pathway. By creating our Paediatric Assessment Unit, and Hospital at Home team, we have been able to better manage the flow of patients into hospital beds, allowing us to care for those most in need, more quickly. Building on this we will now focus on our current „hot spot‟ pathways – outpatients and surgical flows. Working with frontline staff that struggle on a daily basis to get patients in and treated, we will determine what improvements can be made to be more efficient, and through this we know we will be able to see patients more quickly, with fewer delays. This programme of work will form the basis of our EQUIP work stream (Enabling Quality Improvement). People The best teams deliver the best results Like many hospitals around the country we continue to face staffing challenges due to national shortages of specialist doctors, nurses and other healthcare professionals. This is why it is more important than ever to look at how we can work differently and ensure we have the right skills, at the right level, rather than be fixated on old fashioned workforce models that we could never recruit to anyway. Training also plays a critical role in the success of our people, and amongst our ongoing training programmes, a key area of focus will be equipping managers with the skills and knowledge to support staff to deliver better services. Our Team Maker Programme is the cornerstone of this. We also need to be realistic given the fact that we, and the NHS as a whole, face the biggest financial challenge in our history and as a result it has never been more important to make every penny work hard for us. Sometimes this is about getting the basics right and we hear about great common sense ideas all the time that just need to happen. Through a Trust wide campaign we will support people to make better use of our funding, so we can reinvest more into patient care. The Trust‟s People Strategy sets out our commitment and plans for developing and supporting every member of staff to be the best they can be. Technology Taking the hassle out of healthcare Technology will play a critical role in delivering our Next Generation project. We have a clear vision and strategy for how we will use technology to enhance the quality of care we provide for children and their families, and at the same time improve our working lives. Our goal is to go paperless, and to do this in the next few years through Paediatric Electronic Patient Record (PEPR) programme. PEPR will be a place which will: Bring together integrated information to support clinicians in running their services- for example clinic lists, ward lists, operation lists, inpatient lists, activity data Bring together information to improve decision making and clinical care – for example demographic details, tests, scans, medicines, correspondence within a single electronic patient record Help us communicate better with children and families by providing direct access to information about care, and let them provide feedback directly to clinicians. Help us communicate better with other healthcare professionals – general practitioners and also other professionals who ask our advice, and from whom we ask advice. 19 Facilities Great buildings support great care Our hospital is old, cramped and restrictive, and we must look at how our existing buildings can be remodelled and where new buildings could be built on site, to keep us going through to 2022. Our Board has committed £35 million to developing our site, on top of the £9 million already allocated to Parkview. The project team will develop our business case for approval by the end of 2014, with building work due to be completed by early 2016. In December 2012 the Board reviewed the initial Strategic Outline Case (SOC) for the development of a new children‟s hospital facility in Birmingham. This was based on analysis that indicated in order to meet demand over the medium and longer term and maintain and improve market share new facilities would be required. In approving the case the Board recognised: Whilst there were two options that were feasible – develop at the back of the current city centre site or move to Edgbaston co-located with UHB, with a new joint facility with BWH, the latter was the favoured option. This would require service reconfiguration and close working between Birmingham Women‟s Hospital NHS Foundation Trust and University Hospitals Birmingham NHS Foundation Trust. Assuming the development of a new hospital in 2022 investment was required over the medium term to meet demand requirements. Our modelling has indicated that the Trust would require four new theatres, additional beds and associated patient and carer facilities (e.g. Parent accommodation). We have worked with our partners since January 2013 to develop a solution in the City Centre that will provide a legacy facility if the main hospital site is to move. Up until 2022 this will be mainly utilised by BCH, post 2022 it will be shared by BCH and UHB providing a specialist facility and addressing some of the access issues that were raised by commissioners during the development of the SOC. The Trust has appointed a range of professional advisors to support the development of this legacy solution and we would expect a business case to be submitted to the Trust board in the autumn of 2014 with a value of £35million. We would expect a start on site at the end of the period covered by this plan and capital expenditure associated with the demolition of the multi-storey car park on site on which the new clinical block will be located. We are currently exploring the funding options for this new facility – starting with a strong cash position and £4million collected via fundraising for the children‟s oncology element of the new facility. We would expect the majority of the capital to come from these internally generated resources but may consider a loan from the Foundation Trust Funding Facility for a small element. Our June 2014 submission will include full details of the financing of this facility. 4.3.2. The Better Care Fund In addition to the Next Generation project we are also actively engaged within our local health economy with the Better Care Fund (BCF), which presents us with a unique opportunity to strengthen integrated working across the region. The BCF plan requires local areas to formulate a joint plan for integrated health and social care and to set out how their single pooled BCF budget will be implemented to facilitate closer working between health and social care services. Work undertaken through the development of the BCF plan for Birmingham has resulted in a shared commitment to develop a viable health and social care system which more appropriately responds to the needs of individuals who are vulnerable. The programme focuses upon an aspiration to maximise the opportunities for providing quality care including mental health in a variety of community based settings, with a focus on preventative and 20 proactive care, only admitting to a hospital bed when it is the right thing to do so. This means avoiding non-qualified admissions and discharging people from acute care at the optimum time into more appropriate alternatives. There is a system wide piece of work to model the implications of this shift using a 7 day maximum length of stay for an unplanned spell within a typical acute district general hospital setting. This along with information about the type of services required enables an informed assessment of the type and volume of community alternatives needed. We are a member organisation within the Birmingham Integration partnership board and therefore influential in developing the delivery plans. As an organisation we are supportive of these plans and they are in line with our own strategy. 5. Key Performance Risks There are two specific areas that have been highlighted within our operational plan for 2014-2016 in terms of key operational performance risks and these are outlined below: 5.1. Diagnostic Waits The Trust has failed to meet the 6 week diagnostic wait target for MRIs since January 2013. There are a number of factors which have contributed to this. - Increased demand for diagnostic imaging Increased proportion of requests requiring general anaesthetic Lack of capacity in the workforce These factors have led to a backlog and the service has been unable to flex to meet spikes in demand that have been seen during some weeks of the year. A number of actions have been taken and are planned which aim to bring performance back in line with targets and to ensure that the service is sustainable. This includes actions to reduce demand as well as increase capacity: - Approval for recruitment of additional radiologists and radiographers Use of mobile scanners Increase in GA sessions Improved use of tools for modelling and forecasting demand and capacity Figure 16 Performance Trajectory Diagnostic Waits Based on current assumptions it is forecast that the target will be met from June 2014. BCH has 21 commissioned an independent clinically lead review from the transformation team at the Royal College of Radiologists to assess the actions taken and working practices to identify any further improvements that can be made. 5.2. Cancelled Operations The level of cancelled operations, both on the day and the day before, continues to be a concern to the organisation. The single biggest reason for cancellations continues to be access to a PICU bed. There are also issues around ward beds and theatre capacity. Significant work has been completed in 2013/14 to address some of the issues this has included reviewing the surgical pathway processes. In addition an external review was carried out by PWC to consider the actions taken and any further actions. A number of actions have been taken and are planned in 2014/15: Increased capacity through use of other facilities plus internal capital works; Increased anaesthetic capacity; Transformation programme to include focus on theatre scheduling and booking; Implementation of pre assessment service; This will remain a priority for 2014/15 in particular focusing on a reduction in the number of children who are cancelled more than once and those cancellations which are due to administration errors or equipment failure. 6. The BCH Clinical and Quality strategy (2014-2016) One of our strategic objectives is that “Every child and young person cared for by BCH will be provided with safe, high quality care and a fantastic patient experience.” In order to deliver against this objective we have developed our clinical and quality strategy which has a key focus on ensuring that we further innovate our systems to promote and enhance patient safety and reduce avoidable harm. Some of the key projects and highlights of our quality strategy planned for 2014-2016 are outlined below: - Implement and embed the Safer Clinical Systems Handover Project Trust wide. Pilot and review the use of the Safety Case approach as a method for embedding quality review of service delivery across the organisation. Support the development of the national Paediatric Safety Thermometer building upon the SCAN work Re-launch the Sepsis Care Pathway. Implement SHINE 12 – „Listening to You‟ – a tool to measure parental concerns and standardise the format for handing over care between a parent and a nurse. Improving situational awareness by introducing the proven „huddle‟ model to improve communication and address underlying cultural causes for safety failures. 6.1. Developing the Strategy As we continue to make technical advances in the clinical care we deliver, so we must advance in our approach to patient safety. To achieve this we need to shift away from the traditional definition of safety as being the absence of harm. Instead, we need to consider safety as the ability to succeed under varying conditions, so that the number of intended and acceptable outcome is as high as possible. In so doing, we can learn from what goes right with the clinical care we deliver. This affirmative action will foster greater transparency and an enhanced safety culture within our organization. 22 The emphasis of our patient safety strategy is therefore focused on people and relationships for 20142016: our engagement and empowerment of children, young persons and carers, the growth and development of our staff, and design of our clinical systems to support our staff in delivering high quality care. The following sections will outline the key themes that we will focus on as part of our patient safety strategy for 2014-2016 and also summarise the key priority areas within each theme. Theme One: Ensuring that things go right- a proactive approach to safety We will look at what goes right as well as what goes wrong with the clinical care we deliver. We will learn from what succeeds as well as what fails, recognising that things go well because people make sensible adjustments according to the demands of the situation. - - Favourable Event Reporting – We will develop and implement a system of reporting for well managed events with positive outcomes to mirror and compliment the incident reporting system. This is to ensure that we are able to learn from what has gone right as well as what has gone wrong. We will design a model of a successful investigation based on a review of investigations and their relative successes in improving outcomes. When something has gone wrong, we will look for everyday performance adjustments that people usually make and the reasons for them. - - Through Root Cause Analysis investigations we will look to identify both performance adjustments which are appropriate and necessary and inform the qualities of a resilient team but also those performance adjustments which are necessary to mitigate risk inherent in our systems. We will look in detail at every monthly Clinical Risk & Quality Assurance Committee at a minimum of at least one significant risk by applying risk methodologies which not only take account of past harm and likelihood of harm but consider potential „harm loops‟ prevented by the performance adjustments and inherent resilience of our staff. We will look at what happens regularly and focus on events based on how often they happen and not just how serious they are. - We will include a monthly aggregated analysis of Patient Experience Feedback sources to include, SIRIs, the Patient Experience Feedback database, Complaints and PALS contacts within the Quality Report to Board. We will allow clinical teams time to reflect, to learn and to communicate to enable consolidation of experiences and understanding of situations of clinical care provision. - The “Closing the Gap in Patient Safety: Redirecting the clinical gaze to reduce harm and drive cultural change through better communication in children‟s wards” project aims to introduce the proven „huddle‟ model to improve communication and address underlying cultural causes for current safety failures. Specifically, the project aims reduce avoidable error and harm to over 4,000 acutely sick children by 2016, to involve as many parents and patients better in their care and to evaluate the cultural change, allowing the learning to be applied beyond paediatric wards. 23 Theme Two: Building workforce capability in quality improvement and patient safety science We will deliver training in Quality Improvement and Patient Safety Science for our workforce. - We will build a patient safety and quality improvement faculty and develop a Foundation in Improvement Science module including the following elements: o Mapping, Measures, Modify, Model, Maintain We will coach clinical frontline teams to enable them to implement patient safety and quality improvement initiatives. We will implement a Coaching Scheme that will seek to: - Identify existing resources and develop an informed coaching support network Develop a mechanism for access to the coaching support network in relation to patient safety and quality improvement initiatives Build on existing resources to widen and strengthen the network We will continue to develop the UK “Making it Safer Together” (MiST) Group with our peers, sharing outcomes and data with the group. Theme Three: Design Human Factors into our clinical systems We will use Human Factors Science to make our clinical systems safer for patients, more reliable and resilient and to improve the well-being of our workforce. - Patient Safety is one of the foundations of EQuIP. The Programme will ensure, through the clinical forum that Human Factors Science is included within all service redesign projects. Theme Four: Continual Learning – better use of patient safety and quality information We will re-balance our safety measures to enable us to ensure care will be safe in the future. - We will work with our paediatric partners to develop a true paediatric risk adjusted Standardised Mortality Ratio which could be used internationally. We will measure whether we are responding and improving from our understanding of our safety information. - We will conduct an annual safety culture survey and use this to inform priorities for pro-active risk reduction. Theme Five: Transparency of our quality and patient safety information We will use safety cases to explicitly state the safety and vulnerability of our clinical systems. - We will use safety case methodology to assess the safety of surgical pathways and challenge and test the effectiveness of our risk controls. We will actively engage in sharing of our patient safety data with our staff, users of our services, other NHS organisations and the wider public. - We will circulate the Monthly Quality Report to all staff We will provide summaries for front-line staff which disseminates learning from SIRI Investigations 24 - We will provide dedicated Patent Safety Intranet resources for staff We will develop the shared reporting and interrogation of risk data for wider staff groups via the Vesper reporting platform We will actively engage patients and carers in quality improvement and re-design of our clinical systems. - The Young Persons Advisory Group will provide a patient forum to approve and monitor the progress of EQuIP projects. 7. Quality & Safety Governance Birmingham Children‟s Hospital is continually striving to improve the quality of the services it provides, in terms of safety, patient experience and clinical effectiveness. Quality continues to be at the heart of our strategic objectives which ensures a constant focus on quality at all levels of the Trust, including meetings of the Board and its committees. The committee structure is designed to support the Board to focus on the right things. 7.1. Quality Report A monthly Quality Report is produced and reviewed at the Trust Board, Quality Committee, Clinical Risk & Quality Committee and the Senior Leadership Team meetings. The report includes information on serious incidents, complaints, mortality data, cardiac arrest, respiratory arrest, other acute life threatening events, infection control data, safety thermometer and range of patient experience indicators. Information on Never Events and other safety information is reported by exception, including the progress of key projects related to the Safety Strategy such as the Safer Clinical Handover Project and the Sepsis Care Pathway. The report contains detailed monthly updates looking at mortality data, a summary of which is provided below, and is supplemented by a mortality case review. The case review includes a summary of all deaths in the previous month and whether or not any potential care management issues have been identified. 7.2. Mortality data In addition to the review of individual deaths, mortality data is presented to both the Quality Committee and The Trust Board using a range of performance indicators in order to provide the appropriate level of interrogation and assurance. Indicators reviewed include: • Absolute number of deaths per time period. • Number of deaths per time period per 1000 admissions. • Standardised mortality ratio • Cumulative sum (CUSUM) charts 7.3. Internal Assurance and the Board Assurance Framework The Board Assurance Framework (BAF) provides a structure and process to enable the Board to understand and focus on the risks to achieving the organisation‟s strategic objectives and to assist the Board in discharging its responsibility for internal control. The BAF is presented to the Board for review at each monthly Board meeting. The content of and process surrounding the BAF were reviewed by the Internal Auditor in 2012/13. The review gave significant assurance, but a number of 25 recommendations were made for improvement, and these have been implemented. This included a Board workshop to reassess the Trust‟s risks, which took place in February 2013. The outcome of this workshop has led to further development of the BAF and a review of the goals we must achieve to meet our strategic objectives. A further review is being undertaken for the 2014/15 period, the current high level BAF is presented below (figure 17) and shows the assessed level of strategic risks up to the February 2014 Trust Board. Figure 17 Summary Board Assurance Framework 8. The BCH Participation & Patient Experience Strategy (2014-2016) We want our patients and families to feel that they will be cared for, will feel safe and will feel confident in their treatment. In making this a reality for all of our children, young people and families it is essential that we work in partnership to ensure their opinions are heard, feedback is acted on and lessons are learned. The Participation & Patient experience Strategy will ensure that we engage and involve children, young people and families in the planning, provision and evaluation of all aspects of our services as outlined in section 242 of the NHS Act. In order to ensure children and young people are placed at the forefront of the care they receive and are key stakeholders in influencing the quality and delivery of their health service we maintain a „toolkit‟ approach and currently gather a wide range of information from different sources including, including feedback cards, e mail, ward walkabouts, verbal feedback; all collated on the Patient experience Database (PED), the Friends and family Questionnaire, Patient Opinion and more qualitative feedback from patient experience and participation projects such as patient stories, quality walkabouts, patient shadowing and mystery shopper experience. In the last year we have moved to a more real time data collection and responsiveness. This has been enhanced by a new communications tool – the feedback app- and is also increasingly being supported by the use of social media including Facebook and Twitter. The feedback app has provided an opportunity for parents, children and young people to let us know about their experience, both positive and negative, in real time and has enabled staff to respond directly in real time too. 26 The objectives that have been developed as part of the Participation and Patient Experience Strategy for 2014-16 are outlined in figure 18 below. Objective Measure Secondary Measure Build on existing work to further develop robust systems and processes for gaining both qualitative and quantitative feedback from CYP and families. - CQUIN target for 2014/15 met Volunteers will begin to undertake regular surveys Continue with Tea @3 initiative and evaluate Switch over to Vesper reporting services for both PED and Friends & Family Pilot drop in sessions on wards incorporate child & family information Enhanced use of social media - Quarterly trend analysis available triangulating PALS/complaints & PE data - - - Develop more robust analysis and triangulation of complaints and PALS with PE to inform improvement - - - - - - To lead a Trust-wide 'campaign' style approach to make improvements in identified themes or services - The Trust Board will play an active leadership role in advocating improvements in the patient experience - Develop a minimum data set and dashboard for teams and departments to drive improvements - - - CQUIN target for 2015/16 met Develop a library of short films of patient experience Adapt friend and Family in line with anticipated National Paediatric roll out in march 2015 Undertake paediatric survey – currently under review between Picker Institute and NHS England Recruit and train young inspectors to undertake You’re welcome assessments Standardised process in place for measuring satisfaction of complaint handling and outcome Annual directorate plans are developed to address identified common themes Evidence of recommendations from Clwyd and NHSLA Areas for improvement will have been identified Training and education needs will have been identified - Annual Trust strategic objective will be influenced by patient feedback ‘Intelligent’ use of patient stories at Board meetings Patient Experience will provide a focus and influence both the quality and safety senior walkabouts. - Patient stories and patient experience will form a regular part of every board meeting; with evidence of the learning that has come from them in strategic decision making. The role of patient and parent/ carer governor will be strengthened New PE key performance indicators will be developed - 27 - Every service in the trust will be using PE to identify opportunities for improvement and will implement at least one patient experience improvement project annually Develop systems and processes to provide feedback to children, young people & families and other stakeholders both at service / department and corporate level. - - Every ward/ departmental will have an agreed minimum data set display in place. The display will have both parent and be CYP focussed. - There will be a clear and comprehensive presence of patient feedback in all public and clinical areas of the organisation. Figure 18 BCH Patient Experience & Participation Objectives 2014-16 9. Learning from Francis, Berwick & Keogh The impact of these key national reviews has been reported and considered at Trust Board and across a wide range of operational and clinical forums and the Francis review formed the basis of our annual InTent staff engagement event in September 2013. For each of the reviews we have considered the overall implications and assessed the position of BCH against the key recommendations. This has informed the developed our both our quality strategy and the patient experience strategy outlined above. The assessment of BCH and the challenges presented to us are summarised in this section for each of the reviews. 28 9.1. The Berwick Report 29 9.2. BCH Assessment against Berwick Recommendations BCH has undertaken an assessment against the key recommendations developed within the Berwick report in order to assess and map our current priority areas against the key recommendations and this is summarised below. 30 9.3. The Keogh Review 31 9.4. BCH Assessment against Keogh Review We have also undertaken an assessment of our position in relation to the Keogh review and the key recommendations in order to establish whether our strategy and priority areas for 2014-2016 are appropriately aligned. 32 10. The BCH People Strategy 2014-2016 As one of the UK‟s leading paediatric centres we go to great lengths to target, teach, nurture and develop the skills of our present and future workforce, to enable access to training and education and to foster life-long learning. Our aim is to ensure that all staff are appropriately equipped and qualified for the work they do and continue to learn and develop in their time with us. We continually examine our practice and look at ways to innovate and improve the service we all deliver so that our children, young people and families receive a first-class service. To support this we have developed our People Strategy which is a key enabler for supporting the delivery of the overall Trust strategy. In developing our People Strategy we have considered a range of national, regional and local factors. 10.1. National Factors The workforce supply chain is crucial and our intelligence tells us there will be less speciality doctors available in the future but an increase in the numbers of GPs in training. As a Trust we need to ensure we are exploiting this and providing a good training environment for medical staff. Nationally there is a predicted 6% downward shift in the availability of junior medical staff. This will have a significant impact in some of our clinical specialties and how we respond to this is critical to meeting our service demands and providing an excellent education experience. Some initiatives we have developed include the extension of nurse led services such as the development and integration of Advanced Nurse Practitioners and clinical site practitioners in order to cover many tasks traditionally covered by junior doctors. We have also appointed 4 Physician Associates and 5 international doctors through the MTI scheme and in partnership with a neighbouring trust The nursing workforce needs to grow significantly, nationally and regionally, and the predicted supply will not meet this demand. We therefore need to create alternative roles to support the gaps in qualified nursing staff. We are bringing in cohorts of Clinical Support staff and have developed a robust programme and career framework for these staff. We are also looking at advanced practice in other health care staff such as Pharmacy and we now have more people who can prescribe which supports the junior doctor workforce. The national decisions around Pay will no impact on retention so we need to work to reduce this risk and build resilience into structures. The requirement to grow seven day services will be a priority for the next couple of years and we have commenced this in areas such as our support services directorate. The premium rates will make this prohibitive in many cases so we must work with staff to develop a more flexible approach 10.2. Regional Factors With changes in regional demographics it is predicted that Birmingham will become the second plural city by 2024. Cultural competency in our workforce will be crucial to delivering quality care that meets the individual needs of the communities we serve. The LETB & LETC structures have also developed significantly over the last year and have improved the workforce planning process and education commissioning approval process so that there is regional ownership of these key decisions. 33 We have good relationships with education providers and are developing a proposal for joint appointments to improve the quality of evidence based practice in curricular development 10.3. Achievements so Far Our people strategy is a three year programme of work covering 2013-2016. We have already made some significant progress during our first year across some of our core themes Developing our People Significant improvement in junior doctors induction Improved education QA processes & highly commended deanery feedback Development of the Youth Academy, traineeships and apprenticeship programme New Intern programme- 25 completed or current interns New leadership programme established Launch of the Team Maker programme A full review of Education and Learning functions completed Caring for our People Best ever response rate to the National Staff Survey - 22% increase 3% increase in overall staff engagement scores Positive NICE audit on wellbeing services A range of new wellbeing initiatives launched for staff Managing our People Innovative workforce design solutions developed eg. Appointment of 4 Physician Associate & 5 International doctors. Through the „Future Fit‟ workforce project we have identified a number of productivity opportunities which are being implemented with identified savings of £500k All junior rotas monitored and deemed fully compliant Workforce planning process embedded into business planning and improved information available to support more effective education commissioning Improved recruitment processes- average appointment time reduced from 12 to 9 weeks Development of a robust assurance framework for all regulatory standards 10.4. Challenges for 2014-2016 With the launch of the Next Generation project there are a number of workforce priorities that we will continue to focus on as we refresh the People strategy, these are: 1. Developing a mechanism that supports leaders to be compassionate and effective people managers 2. Providing Organisational Development initiatives that continue to develop our culture and improve staff involvement in the delivery of our services 3. Ensuring that we have a sufficient and appropriately skilled workforce supply 4. Developing a culture that supports staff to raise concerns 5. Ensuring that the pay bill is maintained within the reducing financial envelope 6. Leading the development of new health care roles that can support the delivery of new models of care as part of the Next Generation project As we move forward the challenges presented as a result of the financial pressures facing the NHS, coupled with the need to deal with increased demand on our services, means that we also have to look at changing the profile of our workforce in order to be able to deliver sustainable service models. This is particularly challenging across some of our more specialised clinical areas such as PICU and 34 Oncology were we experience high attrition rates in our junior nursing workforce. As part of the operational planning for 2014-2016 we have undertaken a detailed workforce profiling in order to understand these workforce changes across our key staff groups. This has enabled us to model and predict the required skill mix shift across each key area using the business planning data provided by our front line clinical teams and intelligence regarding the future labour market. An example of this approach is shown in figure 19 for our nursing staff and this methodology has been used across all other key areas. Figure 19: Workforce Scenario Modelling 2015-2019 10.5. Education & Training The provision of high quality education and training is a fundamental part of our core business. We have hundreds of health care professionals in training throughout the year and their experience is critical to service delivery and our reputation as a teaching trust. As we move forward over the next few years the need to develop and train new roles in response to the workforce challenges we face means that the provision of high quality education and training becomes even more essential. As a result we have undertaken a comprehensive review of our education and training provision during 2013 and developed our future strategy for 2014-2016. Within the strategy we have developed a systematic process for redesigning roles around changing patient pathways; our challenge over the next 2 years is to build this capability across the organisation. Pilot work, to test our workforce redesign methodologies, has commenced, initially on our surgical pathways. Once these have been evaluated and refined they will be more broadly utilised. A college leadership team will be established and this will be made up of clinical leaders and educationalists and they will jointly deliver the education strategy to ensure education and learning fully supports workforce transformation. In summary our new approach to workforce development will see: - Education coming under a single umbrella to support skills- rather than profession- based approaches to workforce development facilitating new models of care delivery 35 - Focus on structured career frameworks to build resilience in supply chains across workforce groups New education quality dashboard aligned to regulatory and national education outcomes New process to identify investment priorities for education and training aligned to delivering workforce transformation at scale (figures 20 & 21) Figure 20 Developing a Portfolio Model for Education & Training 36 Figure 21: Our Approach to Commissioning and Providing Education 2014-2016 11. Our Financial Plan 2014-2016 The Trust is forecasting to end 2013/14 with a surplus of £8m. This is £3.4m above its plan in year but on a normalised basis the surplus is circa £6m. The Trust continues to perform strongly financially having reported a Financial Risk Rating of 4 for Quarter 1 and 2 respectively and a Continuity of Service Risk Rating of 4 in Quarter 3 with Quarter 4 expected to deliver the same. Despite the strong historical performance of the organisation it is clear that the financial issues facing the NHS as we move forward into 2014/15 are significant and these will present a tougher challenge to BCH than in previous years. The forward look Income & Expenditure position indicates this and shows a reducing surplus over the lifetime of this operational plan. (Figure 22). Income and Expenditure [I&E] Income from activities Other income Operating expenses EBITDA Interest receivable Depreciation Impairment PDC dividend Interest paid Net Surplus / (deficit) Forecast Mar-14 £m 216.46 23.19 -222.89 16.77 0.13 -4.91 -0.69 -2.68 -0.49 8.13 Plan Mar-15 £m 218.42 18.27 -224.58 12.12 0.13 -4.62 0.00 -2.94 -0.45 4.23 Plan Mar-16 £m 215.79 18.52 -221.79 12.52 0.09 -5.29 0.00 -2.86 -0.45 4.01 Figure 22 Forward Look I&E Forecast 2014-2016 37 The challenge for the Trust is to maintain these levels of surpluses to enable medium term investment in the estate as well as build up the longer term investment potential for a new hospital. In developing the financial plan we have been conscious of balancing the need for future investment with the need to ensure efficiency requirements remain at manageable levels. The key investments for the Trust have been identified within the Estates section of this plan. The impact of these can be seen within the Statement of Financial Position (figure 23). Statement of Financial Position Non-Current Assets Current Assets excluding Cash Cash Assets, Total Liabilities, Current Net Current Assets (Liabilities) Liabilities, Non Current Total Assets Employed Taxpayers' Equity: Public Dividend Capital Retained Earnings (Accumulated Losses) Revaluation Reserve Total Taxpayers Equity Forecast Mar-14 £m 102.15 17.37 42.85 162.37 -30.24 29.98 -6.34 125.79 Plan Mar-15 £m 112.86 24.29 35.93 173.08 -29.70 23.26 -6.09 137.28 Plan Mar-16 £m 134.33 42.08 18.14 194.56 -28.92 6.23 -6.54 159.10 86.22 26.80 12.77 125.79 86.22 31.03 12.77 130.02 86.22 35.03 12.77 134.02 Figure 23 Statement of Financial Position 2014-2016 As the constituent parts of the Medium Term Clinical Strategy are developed the impact of the increasing non-current asset base can be seen on the Trust‟s cash balance which reaches its lowest point in 2015/16. The cashflow movements highlight the investment programme (figure 24). Cashflow Opening Balance Movements: Surplus/(Deficit) from operations Increase/(decrease in working capital Property, plant and equipment Net cash inflow/(outflow) from financing Net cash outflow/inflow Closing Balance Forecast Mar-14 £m 36.17 Plan Mar-15 £m 42.85 Plan Mar-16 £m 35.93 15.70 3.74 -10.22 -2.55 6.68 42.85 9.82 -0.89 -13.03 -2.81 -6.92 35.93 9.97 -0.77 -24.22 -2.77 -17.79 18.14 Figure 24 Cashflow Profile 2014-2016 The revenue impact associated with increasing the Trust‟s infrastructure is also highlighted in the I&E position as clinical income rises significantly over the period despite tariff reductions being forecast. The aims of the Trust‟s financial strategy remain to: - Improve the quality of service that reduce variation, waste and harm; Provide the resource to deliver world class patient centred care; Provide the funding for a productive, motivated and professional workforce; Provide better value for money; and Deliver affordable, world class health services for children and young people. The strategy will be delivered through the following six components: 1. Using a mixed funding strategy for major new infrastructure investment; 38 2. 3. 4. 5. 6. Developing a clear financial framework – to monitor financial stability and investment; Delivering the necessary efficiency savings through traditional and transformational routes; Improving financial literacy across the organisation; Developing NHS and non-NHS business opportunities; and Recognise charitable funds as a core component of the funding mix. The key risks to achieving the Trust‟s financial strategy are outlined below and these will be picked up in the Trust‟s downside scenario. Ability to finance the Medium Term Estates Strategy; CIP delivery; Funding Reductions o Move to Education Placement rates and then to Education Reference Costs o Future uncertainty over the paediatric top-up, with the NHS England and Monitor review of funding specialised services ongoing o Loss of Community CAMHs funding and further public sector funding reductions; Cost of Clinical Negligence Scheme for Trusts contributions; Cost of maintaining the retained estate; External commissioning environment changes; and Reforming the Trust‟s Workforce. 11.1. Income The 2014/15 income included in the financial plan is based on provisionally agreed contracts with commissioners and anticipated contractual positions. At the time of writing the position with the Trust‟s 2 main Commissioners is as follows: NHS England – agreement of contractual value - £158.8m. This accounts for 73% of the Trust‟s clinical income portfolio; and Birmingham South Central CCG and Associates – basis of contract agreed. Commissioning- contracts have largely been based on out-turn activity with the major development being the agreed income associated with the further expansion of PICU to 31 beds in a full year from 2015/16. Agreements with NHS England for 2014/15 have seen the Trust fall into line with contracting conditions imposed throughout England. This has seen funding reductions for Chemotherapy and Major Trauma. During the course of the Trust‟s business planning process we undertook a clinically led „bottom-up‟ approach with individual specialties engaged in modelling their activity projections. This provided the basis for our corporate assumptions recognising that due to capacity constraints the realisation of these will not be possible until the mid-term of the 5 year planning period once the Trust‟s proposed estate development has been completed. CAMHs- a key risk in the Trust‟s future financial plan is the long-term future of the Community CAMHs service. The Birmingham Cross-City, Birmingham South Central and Sandwell and West Birmingham CCGs are currently tendering a Community Mental Health Service for under 25 year-olds across Birmingham. A key part of this is the Trust‟s CAMHs Community service for which the Trust presently receives £9.6m, of which £8.2m is recurrently funded. Commissioners have provided 18 months (£2.1m) of non-recurrent funding for the part of this service which was previously financed by Birmingham City Council. The full-year funding (£1.4m) is not part of the existing financial envelope of 39 the services being tendered. A decision on the successful applicant is due by February 2015 with mobilisation of the new service by 1 October 2015. The operational plan assumes that the Trust will be successful in being awarded the Community CAMHs contract. The key drivers of income in the Trust‟s plans are: - Tariff; Growth; CQUIN; PICU growth; and New drug charges. Tariff-we have assumed a tariff reduction in 2015/16 based on the planning assumptions included in Monitor‟s “Guidance for the Annual Planning Review 2014/15”. Specifically for the Trust we have not assumed any changes to the two-tiered system of funding for the Paediatric Top-Up. Other key changes to the tariff that have impacted upon the Trust are: Further local adjustments to CF year of care tariffs; and Unbundled diagnostics. Growth- We have assumed limited growth throughout the course of the plan although given historical activity levels this may be a prudent approach. This in part is down to the existing capacity constraints. The medium-term plan will build in more of the specialty by specialty assessments of growth. Any predicted growth levels will not trigger contractual clauses that will impact upon the Trust‟s ability to cover its costs in delivering this additional activity. CQUIN- The national 2.5% CQUIN level means that the Trust has the opportunity to receive circa £4.5m through this route. The Trust‟s plans assume that the majority of this is recovered and is putting in specific resource to ensure that this is achieved. The Trust was successful in receiving 100% of CQUIN monies in 2012/13 and remains on course for a similar outcome in 2013/14. PICU- The Trust is on an agreed PICU bed development path which has seen incremental increases in the number of beds commissioned. Although physical bed capacity is available the Trust does not expect to be operating at its 31 bed capacity until 2015/16. The agreed level of funded PICU beds in 2014/15 remains 29.5 with performance variations adjusted for at a 50% marginal rate. New Drug Charges- The specialist nature of the Trust‟s mandatory services has seen a consistent increase in the income levels generated through non-pbr other activities. The majority of these rises are deemed “pass-through” items ie the Trust incurs the cost and invoices Commissioners the equivalent amount to ensure cost neutrality. Although no further growth has been built in from the Trust‟s perspective an increasing percentage of items of this nature applies downward pressure to the EBITDA and I&E Surplus Margins. The Trust remains committed to working with our health economy to reduce the overall cost burden of this area of the contracting portfolio. This builds on from the successful opening of the Trust‟s Outpatient Pharmacy subsidiary, the Medicine Chest, in January 2013. Away from Clinical Income the Trust‟s levels of Education and R&D income are reducing. The level of CLRN funding reduced further in 2013/14 but the Trust is now expecting a flat funding profile going forward. 40 The transition towards tariff based education income commenced in 2013/14 with NMET and SIFTS moving to a placement methodology and this has advanced further in 2014/15 with the full impact of those changes being incurred plus the first year of MADEL changes. The combined cumulative loss for the Trust over the duration of this planning period is £0.5m in 2013/14, £1.0m in 2014/15 rising to £1.3m in 2015/16. The Trust will be pushing for local flexibility support from HEEWM as this funding methodology is punitive for specialist hospitals. Looking further forward, the Trust has been actively supporting the DH on the Education Reference Cost project so will be well placed for future collection exercises. 11.2. Costs The cost base of the Trust is predicated on delivering the same levels of activity in 2014/15 as 2013/14 whilst delivering efficiencies sufficient enough to remove the impact of pay and price inflationary pressures and any significant one-off costs. The plan for 2014/15 retains a forward look given the expected “cliff-face” of increased costs in 2015/16 so part of the financial planning approach has been to smooth out the transition between the 2 years. Inflationary pressures are once again based on the planning assumptions outlined in Monitor‟s “Guidance for the Annual Planning Review 2014/15”. The Trust has assumed 1% national pay growth in each of the future years plus localised impacts of Agenda for Change and Consultant Contract seniority. The assumptions are as follows: Pay Drugs Clinical Supplies Other Costs 2014/15 1.50% 3.00% 3.00% 3.00% 2015/16 1.50% 3.00% 3.00% 3.00% Figure 25 Cost Assumptions 2014-2016 The financial plan for 2014/15 has built in non-recurrent funding to facilitate the extensive transformation programme that the Trust will be undertaking. In addition to this the Trust has sought to pump prime developments during 2013/14 which will enable the minimisation of costs and the maximisation of savings during 2014/15. From 2015/16 the Trust will see increasing financial pressures on 2 fronts: - Changes to employers‟ pension contributions - Changes to the charging methodology for CNST The latter is more specific to the Trust as the current charging methodology provides with the Trust with a 30%, equivalent to £1m, rebate as allowed upon reaching NHSLA Level 3. The worst case scenario is that the Trust will lose the full benefit of this. Although the new methodology has not yet been communicated some of the contributory factors are known and it is likely that the Trust‟s contributions will increase in 2015/16. 11.3. Local Cost Pressures As in all previous financial years there are a number of localised cost pressures being experienced by the Trust. A cost pressure reserve has been set aside to fund those pressures that are deemed a clinical priority. In 2014/15 these include supporting the IT infrastructure to allow the implementation of the Trust‟s IT strategy, Infection Control, Nurse Staffing and ERA. 41 Work is progressing to identify the impact of seven day services at the Trust. Following on from “NHS Services Seven Days a Week – Summary of Initial Findings” the Trust has been using the HFMA template to assess this impact. As with a number of other organisations seven day services have incrementally been developed at the Trust although the overall financial plan assumes any further expansion will be cost neutral. As per previous years the Trust has built flexibility, albeit at a lower level than 2013/14, into the I&E position by way of a contingency reserve. Non-utilisation of this will deliver a higher in-year surplus as per the experience of 2013/14. 11.4. Capital Expenditure The Board approved the financial strategy in March 2012. This indicated that given the cost of capital and the continuing global banking and sovereign debt crisis, traditional bank and bond funding alone, that have underpinned funding mechanisms such as the Private Finance Initiative, will not be affordable. This means that if the Trust is to develop an infrastructure to compete successfully over the longer term in local, regional and national paediatric markets it has to develop a financing plan that is affordable and sustainable through using a range and combination of sources. The 2014/15 capital programme has been developed in this context and will have to work within the resource envelope set out in the Trust financial strategy. The Trust‟s Capital Programme has been derived via the following process: Specialty and Corporate Department Business Plans outlining capital requirements for the medium term; Identification of trust-wide capital requirements that fell outside of specific specialty plans; and Prioritisation process through nominated Executive. The single largest element of the capital programme over the duration of the operational plan will be the planning and initial works on the new clinical block on the Steelhouse Lane site. The £35m set aside for developing the site will be spread over 2014/15-2016/17 and will be linked to the Trust‟s fundraising strategy. Prior to this the Trust has a number of short-term plans which will deal with immediate capacity issues, which are a combination of revenue and capital schemes. The capital associated with the immediate operational plan was contained within the 5 year Capex Forecast submitted to Monitor in January 2014. Capital Expenditure New Build Maintenance - Routine Non-Backlog - locally Funded Maintenance - Backlog - Locally funded Maintenance - Backlog - DH Funded Equipment Information Technology Other Gross Capital Expenditure Including IFRS Impact & Asset transfers Disposals and Transfers Grants and Donations Net Capex against Health Budget incl IFRS impact Plan Plan Mar-15 Mar-16 £m £m 4,775 19,901 500 500 1,500 1,500 0 0 2,250 2,500 5,397 1,578 910 790 15,332 26,769 0 0 (2,300) (2,550) 13,032 24,219 Figure 26 Forecast Capital Expenditure 2014-2016 42 Outside of the new clinical block development the other key aspects of the programme are: - Phase One of the CAMHs Tier IV development (2014/15) and agreeing Phase Two of the development (2015/16); - Continued implementation of the IT Strategy (assisted by funds received from the Safer Hospitals, Safer Wards Technology Fund - Wave One and charitable monies for the development of an e-prescribing system); - CT scanner and Gamma Camera projects concluded; - Adding additional physical capacity at the Steelhouse Lane site; - Backlog estates maintenance programme; and - Replacement medical equipment programme including replacing one of the Trust‟s 3 MRI scanners in 2015/16. Other schemes that have been approved include: - Patient experience projects; - Minor building projects; and - Front of house development. Further strategic capital schemes have not been included in the figures above as they are yet to be approved at Finance and Resources Committee and Board of Director level. Business cases will be expected to be received during the year for these and may include a buying-out the existing arrangement with Riverside Housing. 11.5. Liquidity The Trust enters the operational planning period with a strong liquidity position. The cash balance retained with Government Banking Services at 31 March is anticipated to be in the region of £43m. This is an increase of £6.7m on 2012/13. The planned annual surpluses of £4m will enhance this further. However, the planned investment in the estate over the operational planning period will see this reduce to £18m by March 2016. The Programme Board set up to progress the Estates Strategy will develop a funding approach for the medium and long-terms. This may alter the current funding approach which is to finance the Clinical Build through a combination of internally generated funds and fundraised monies. 11.6. Risk Ratings The Risk Ratings associated with the baseline operational plan are outlined in figure 27. Continuity of Services Risk Rating Forecast Mar-14 £m Plan Mar-15 £m Plan Mar-16 £m Metric: Liquidity Days 36.8 42.0 31.7 Liquidity Metric 4 4 4 Capital Servicing Capacity 5.0 2.9 3.0 Capital Servicing Metric 4 4 4 Overall Rating 4 4 4 Figure 27 Forecast Continuity of Service Risk Ratings 2014-2016 The liquidity days declines over the duration of the operational plan as the capital programme 43 intensifies whilst the Capital Servicing metric reduces from its high point in 2013/14 as the I&E surplus and associated EBITDA levels reduce by over £3.5m. Sensitivity of Risk Ratings- the resilience of the Trust‟s Risk Rating varies by CoSRR metric. In the operational period £18m less cash could be accommodated without the Liquidity Metric reducing to a 4. However, a reduction in the Trust‟s EBITDA margin of £1.4m would cause the Capital Servicing Metric to reduce to a 3. This would still give the Trust an overall CoSRR of 4. For the Capital Servicing metric to reduce to 2 and therefore result in the overall CoSRR reducing to a 3 the EBITDA position would have to reduce by £4.25m which would lead to the Trust‟s planned surplus being fully eradicated. This is the equivalent of CIP delivery falling 50% short of plan whilst all flexibility is also used up. 11.7. CIP Governance As part of the operational planning for 2014-2016 there has been a significant shift towards developing a more transformational approach to the delivery of Cost Improvement Programmes (CIP). The historical performance of NHS Trusts across the FTN sector and the past performance of BCH against annual CIP targets is an important factor for moving towards a more transformational approach. The historic CIP performance for The Trust is illustrated below in figure 28. Plan £k Actual £k Shortfall £k % Delivered 2010/11 5,559 5,313 -246 -4% 2011/12 9,488 9,212 -276 -3% 2012/13 10,730 8,118 -2,612 -24% 2013/14 8,436 5,358 -3,078 -36% Figure 28 Historic CIP deliver BCH 2010-2014 This shows a deteriorating level of achievement over the past 2 years due to an increasing overreliance on traditional CIP programmes and cost-cutting rather than the development of a more sustainable and transformational programme of service improvement and redesign. This approach and the need to change is put into further context when we consider the scale of the future CIP programme that will have to be delivered over the next ten years based on our analysis of future I&E (figure 29). Figure 29 Predicted I&E Modelling BCH 2014-2024 Building on the Trust‟s forecast outturn position we have tracked Monitor‟s assumptions around the level of efficiency required on an annual basis, but also assumed levels of inflation and key financial 44 pressures. At the end of the Monitor ten year planning period the Trust will have had to bridge a financial gap of £46million, equivalent to 19.7% of current costs simply to break-even. In addition if the Trust is to invest in the current site and build up the financial reserves to afford a new hospital the £46million increases to over £76 million. In generating the financial plan an overall CIP target of £9.07m is required in 2014/15. This incorporates legacy CIPs carried forward from 2013/14 and if achieved alongside the Directorate rebasing process will ensure balanced financial positions across the Trust. The difference in approach for 2014/15 and 2015/16 is to have a two-tier programme eg for 2014/15: Hospital wide schemes account for £4.24m; Directorate specific schemes account for £4.83m of which £3.86m must be cost reducing or non-clinical income generating. This will have a more traditional CIP focus and have been worked up by Directorates since the launch of the business planning process in late 2013. For these schemes it is seen as a vital shift in emphasis away from clinical income generating schemes to ones of cost and cash releasing. The hospital wide schemes will be based on 5 themes and form part of the Next Generation project phase 1. - Transformation; Workforce; IT Strategy; Back to Basics; and Commercial and R&D. 11.8. Transformation The options for supporting our programme of transformation in terms of the way in which we provide services have been examined in detail. After undertaking a detailed analysis the most effective method was to appoint external experts supported by a small internal team. The external support provides us with a new set of skills and tools and working alongside our internal team will ensure the skills are embedded across the organisation. We have chosen Newton to be our partner in developing this work and this is based on an initial diagnostic of four potential areas- two of these, theatres and outpatients, will form the basis of our work going forward. In each area our early work shows the potential to deliver additional capacity through examining how we organise the processes and flow through each service area. Freeing up this capacity will reduce the need for significant premium time working and will help in meeting the increased demand for services outlined above. Our estimates of the financial benefits associated with this work are £3million per annum. The Newton team will begin work in late March 2014 and will be on site for between seven and nine months. However, these are only two of four areas that our transformation team will be examining in 2014/15, the other two areas being drugs spend and usage and pre-assessment of patients. 11.9. Workforce In 2013/14 the Trust set aside £1.25million to examine new ways of working. The purpose of this funding was to address the need to change our skill mix, fill hard to recruit areas and also meet the efficiency challenge that we face. The latter is driven by simple economics in that we can‟t address continued efficiency requirements without reducing labour costs that represent 65% of our cost 45 structure. The £1.25million invested last year was in recognition that this would take longer than a year and the results had to be substitution of new roles rather than additionally and would need to release cash. The funding was predominantly non-recurrent so a failure to secure these changes would add cost pressures back into the Trust‟s finances. The second element of the workforce was looking at a range of terms of condition issues – at a basic level ensuring that we work to these but then based on a piece of work undertaken by KPMG looking at whether it is possible to develop some alternatives. Changes to national terms and conditions have delivered some savings in 2013/14 but widening these to local agreements will be necessary in future years. 11.10. Information Technology The Board of Directors agreed the IT strategy in 2013. The financial impact of implementing this has been assessed and will form a key strand of the overall CIP programme between 2014-2016. The work undertaken in developing and costing the strategy was crucial in the successful bid submitted to the national technology fund to secure additional funding. The estimated benefit in 2014/15 is £0.48million. Achieving this will not be easy and will require some difficult decisions to be made around the scale, scope and role of staff currently undertaking clinical administration. 11.11 Back to basics This is a wide-ranging piece of work that covers areas from non-pay procurement savings through to tightening of authorisation controls and further financial training of all staff. In terms of procurement we are going to rationalise the procurement catalogue with the target being to reduce non-pay inflation next year to zero (set by the national procurement strategy). This will save approximately £0.6million. Other aspects of the Back to Basics workstream include: Avoiding contractual penalties for missing quality targets/indicators; Ensuring 100% achievement of CQUIN targets at minimal enabling cost; and Avoiding readmission income losses. The overall back to basics campaign will be extended to other areas during 2014-2016. 11.12. Commercial and R&D This workstream will examine how we might leverage our position as a specialist paediatric provider both in terms of improved research and development income (and contribution) and other commercial opportunities. The most obvious component is private patients and this will be looked at as part of the site development plans. Capacity constraints realistically mean that any growth in this area is limited before that point. In 2014/15 the trust-wide targets are broken down as follows: Technology workstream Workforce Future Fit New Ways of Working Theatres and Outpatients Transformation Back To Basics – Procurement Reduction in contract penalties Drug spend reduction TOTAL HOSPITAL WIDE SCHEMES 2014/15 £m £0.48 £0.57 £0.20 £0.96 £0.60 £0.93 £0.50 £4.24 Figure 30: Summary of Trust Wide CIP Programmes by Theme 46 Following the external review by KPMG the Trust will also be strengthening its Project Management Office (PMO) function during 2014/15. This will be in place by July 2014 and will work in conjunction with the transformation team. 11.13. Management of CIPs The long-term financial plan sets out the level of cash releasing efficiencies required over the medium term. The average level of efficiency is similar to that of peer organisations which gives some assurance that the levels required are in line with the broad assessment across the sector. The Finance & Resources Committee receives regular financial reports that reflect on progress against the CIP plan and also test the feasibility of future plans. The achievement of long-term efficiency savings is recognised as one of the core strategic risks on the Board Assurance Framework, which is reviewed on a regular basis by the Board and also reviewed in more depth at the Audit Committee. Directorate CIP delivery is reviewed monthly against targets and corrective action and support, where necessary, agreed to ensure recovery. Monthly Resources reports, produced for the Board of Directors and Finance and Resources Committee, will include a KPI of CIP against target and the detail behind this. As part of the management processes for delivering CIP programmes in 2014-2016 there are a range of key principles around which they are organised: - Each scheme has a specific PID, managerial and clinical lead Clinical engagement is central to the design and delivery of many of the schemes Each scheme is risk assessed through a quality impact assessment, which is signed off by a local clinical leader as well as the Chief Medical Officer and Chief Nursing Officer. Each scheme is risk assessed for delivery with key dependencies identified Schemes are tested against the Trust's strategic objectives. *****END OF DOCUMENT***** 47