BOARD OF DIRECTORS MEETING IN PUBLIC 31 July 2014
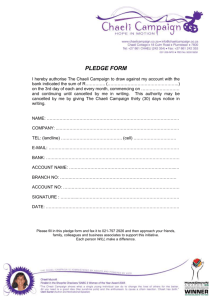
advertisement

BOARD OF DIRECTORS MEETING IN PUBLIC 31 July 2014 PAPERS Board of Directors’ Meeting In Public 31 July 2014 The Education Centre, Birmingham Children’s Hospital AGENDA Item Outcome Time Item No. 14.176 Apologies for absence Note 14.177 Declarations of interest Note Verbal 14.178 Minutes of public Board meeting 26 June 2014 Approve Enclosure 01 14.179 Matters arising from public Board meeting 26 June 2014 Note Verbal 14.180 Chairman’s Report Note 10:55 10 mins Verbal 14.181 Chief Executive’s Report Note 11.05 10 mins Verbal Note 11.15 15 mins Presentation Note 11.30 15 mins Presentation Quality Report - Vin Diwakar, Chief Medical Officer and Note Michelle McLoughlin, Chief Nursing Officer *Performance Report - David Melbourne, Deputy Chief Note Executive & Chief Finance Officer *Resources Report - David Melbourne Deputy Chief Note Executive & Chief Finance Officer and Theresa Nelson, Chief Officer for Workforce Development. AOB 11.45 15 mins Enclosure 02 Questions from members of the public 12:00 10:50 Allocated time 05 mins Report type Verbal Strategy 14.182 14.183 Critical Care Summit Feedback, Vin Diwakar, Chief Medical Officer Aspire @ BCH, Theresa Nelson, Director of Workforce Quality & Resources 14.184 14.185 14.186 14.187 Enclosure 03 Enclosure 04 05 mins LUNCH 12.05 - 12.30 *For note, unless item becomes unstarred at the commencement of the meeting Next meeting of the Board of Directors: 30 September 2014, Education Centre None UNCONFIRMED Item 14.141, Enc 1 BOARD OF DIRECTORS MEETING Minutes of the meeting held in public on 26 June 2014 at 09.00 in the Education Centre, Birmingham Children’s Hospital Present Attending Ref. 14.139 14.140 14.141 14.142 Christine Braddock Sarah-Jane Marsh Vin Diwakar Jon Glasby Colin Horwath Keith Lester Michelle McLoughlin David Melbourne Theresa Nelson Roger Peace Elaine Simpson Judith Smith CB SJM VD JG CH KL MM DM TN RP ES JS Chairman Chief Executive Officer Chief Medical Officer Non-Executive Director Non-Executive Director Non-Executive Director Chief Nursing Officer Deputy CEO and Chief Finance Officer Chief Officer for Workforce Development Non-Executive Director Non-Executive Director Non-Executive Director Deborah Bannister Claire Burden Simon Crooks DB CBN SC Interim Company Secretary Deputy Chief Operating Officer Executive Office Manager (minutes) Item Action Apologies for absence Apologies for absence were received from Tim Atack and Matthew Boazman. Declarations of interest There were no declarations of interest. Minutes of the Board meeting held in public on 26 June 2014 The minutes of the meeting held in public on 29 May 2014 were agreed as an accurate record. Matters arising from the Board meeting held in public on 30 April 2014 CB referred to minute 14.118 and the action on her behalf to meet with YPAG. She had meet with Iona Clayton and agreed to attend the upcoming YPAG conference. She would report back CB to the next meeting. 14.143 Chairman’s Report CB reported verbally as follows: • She had attended a series of meetings with Elisabeth Buggins and Jackie Smith to discuss and progress the new hospital development. The intent to pursue the development remained positive. In the future, she would be attending monthly chairs Page 1 of 5 UNCONFIRMED Item 14.141, Enc 1 Ref. Item meetings with the chairs of the Birmingham Women’s Hospital and University Hospital Birmingham and will keep the board apprised of developments. • An invite from Aston University to discuss their new medical school had been received. However, it was felt that this needed to be considered carefully and that a dialogue should be opened first with Birmingham University to talk about the development in light of our existing connections. • Since taking her the role of Chair, CB reported that she had received countless invitations to attend a variety of hospital and other events. CB confirmed she was having to think carefully about which to accept. Whilst it would be lovely to attend everything, this would impact on the time she had available to concentrate on core issues. As a result, she would be seeking assistance from other Non-Executive Directors to attend these events on her behalf. • We are due to start our Monitor Well Led Board Self Assessment process. Further detail will be provided at the session around objectives, work planning and timescales. • CB stated that going forward she would like to utilise the whole day that is allocated for board, for board business from the Autumn. Where the board agenda results in the meeting finishing at lunchtime, it will be important to use the afternoon for board development. It may also be sensible for the NEDs to schedule in regular NED meetings that day. CB will consider how the time can be best utilised over the summer, and report back at September board. The Board noted the verbal report 14.144 Chief Executive’s Report SJM reported verbally as follows: • The care provided to critically ill children has been subject to an intense two day external review. A number of areas were visited including theatres, ED, wards, PICU and the operations centre. The result was very positive. The assessors were very impressed. Of note, they stated that since their last visit in 2006, they felt there had been a massive cultural change resulting in a big improvement in the service provided. • A review of the Trust’s Safeguarding processes had been carried out by the CCG. The feedback was very positive. The assessors had specifically commented on the passion that staff had for keeping children safe. • A new, exciting partnership bid for the CAMHS tender was announced last week. The Trust had created a core partnership with Worcestershire Health and Care NHS Trust and the Priory Group. Other partners involved include Beacon UK, the Children’s Society and Birmingham Metropolitan College. CB felt this was a strong, stimulating bid and would probably be different to any other bids that the commissioners received. Page 2 of 5 Action CB UNCONFIRMED Item 14.141, Enc 1 Ref. Item JG emphasised the values and cultures of the partnership were just as important as the technical design and development. It would be important to show how the cultures of the organisation would be brought together for the benefit of the patients. Action A strong marketing and communication campaign was behind the bid. DM advised that the PQQ had been submitted and, assuming we were successful, the tender had to be submitted by the second week of September. • Matthew Boazman and Dr Bruce Morland are currently in the USA with representatives from Marketing Birmingham, University Hospital Birmingham and Birmingham University promoting Birmingham Health Partners, with the aim of attracting commercial investment and developing new partners / networks. • The Trust AGM will be held on 16th July 2014, during the Next Generation week. A new interactive format was planned for this year with Chief Officers providing short video presentations, together with a Governors stand. CB and SJM will discuss the invitation of external stakeholders to the AGM. CB/SJM • The Urgent Care Service across Birmingham was being reviewed by local commissioners, with a view to redesigning it. The trust would be involved in the planning, particularly the impact on children and young children. • SJM, JS and JG had attended the NHS Confederation Conference earlier in the month where Simon Stevens, the new CEO of NHS England, had given his first major speech to NHS leaders. This had been full of content and intellectual thought. Initial points were the transfer of some specialised services to CCG commissioning. He felt too many services were categorised as specialist services. Genomics Medicine Centres would be going out to tender in the autumn. JS felt the speech was directed to try and encourage local providers to plan and work out solutions for services. In addition, Simon Stevens appeared very thoughtful on the issues of primary care, community care and smaller hospitals. JG agreed about the intellectual aspect of the speech, but feedback he had picked up mentioned the lack of emotional engagement. The Board noted the verbal report. STRATEGY 14.145 Patient Safety Strategy VD introduced the Trust’s Patient Safety Strategy. Clinical risk and quality assurance remained important within each directorate. The issues relating to the capacity of the hospital and workload pressures on staff were the main risks to providing safer high quality care. The purpose of the strategy was to recognise this and to build the ability of staff to recognise when a safety issue was potentially apparent. Page 3 of 5 UNCONFIRMED Item 14.141, Enc 1 Ref. Item Five key principles would therefore oversee the strategy; • • • • • A proactive approach to safety including a redesign of incident investigation to encourage staff and patient career engagement Building workforce capability in quality improvement and patient safety awareness Design human factors into our clinical systems, i.e. what went wrong and how can we learn from it. Improvements included the implementation of a sepsis 6 programme to ensure 75% of patients received antibiotics within three hours of diagnosis, and the introduction of the medication safety audit to counter drug errors. Continual learning to include better use of patient safety and quality information, including mortality review process and redesigning the mortally recording form. Transparency of patient safety and quality information; the Trust App was very proactive, provided a real time review and was seen as a clear leader in its field. NHS England had devised and was promoting a ‘Sign up to Safety’ campaign encouraging organisations and individuals to support five pledges to strengthen patient safety. We will be signing up. KL expressed concern over the timings WI in the strategy, and the expected timeframe to achieve specific targets. A lack of an action plan to meet target dates could lead observers to assume this was an unsafe hospital. CB agreed. The strategy lacked a stepping stone approach saying what had to be achieved and by when. Furthermore CB was concerned as to where this development sat within the overall development of hospital plans. The presentation needed to show how this strand and its cost fit into the new development plans. CB commented that the intention and strategy is absolutely right, however there are “missing chunks” in the way it is presented. TN mentioned that aligning this with other strategies is critical, in order to develop the right culture for staff to feel confident about raising safety concerns. CBN reassured the Board that the clinical panel are using the safety case strategy as an integral part of the redesign programme, so each time we redesign a service the safety case principles are used. ES asked how progress in implementing the strategy would be monitored. She questioned what processes would be utilised and would it come up to the Board at any point going forward. VD explained that there would be a progress report four times a year, though the Clinical Risk and Quality Assurance Committee. After discussion, it was agreed that the Quality Committee should take the lead in this. The Board received the report. Page 4 of 5 Action UNCONFIRMED Item 14.141, Enc 1 Ref. 14.146 Item QUALITY & RESOURCES Action Quality Report JG raised a proposal from the Committee to organise a refresher training session on how to analyse mortality data, in order to understand the information and to ask the right questions. It was agreed that a time would be found on a scheduled Board meeting date to hold the VD training session. The Board noted the report. 14.147 Performance Report RP raised two items, namely diagnostic waiting times and cancelled operations. Diagnostic waiting times were now coming to the attention of commissioners. Our original target of bringing the MRI waiting list down to zero by the end of June was no longer possible. This had been due in large part to over reliance on a mobile scanner which, due to the patient mix, had not been possible to utilise as intended. CB asked if we could focus on capacity issues in relation to cancelled operations – can we look at mobile theatres? KL expressed his concern that whilst the position relating to both diagnostic waiting lists and cancelled operations had not got any worse, we seemed unable to resolve the problem. What assurance could the executive team give the Board that positive action was in hand. DM advised that an independent diagnostic review had been conducted by the Royal College of Radiologists, and their report was expected on 10th July. We are also assessed by the clinical team that no patients are put at risk by waiting an extra one to two weeks. In addition there were clear guidelines that prevented certain children being scanned via a mobile scanner due to clinical imaging issues. DM assured the Board that all steps were being undertaken to manage and resolve this issue, and we are sighted on the clinical risk and safety of all patients. The Board noted the report 14.148 Resources Report The Resources Report was received and noted. OTHER 14.149 Questions from the Public There were no questions from members of the public. Next Board Meeting: 31 July 2014, The Education Centre, BCH Page 5 of 5 CRAQA Item 14.184 Enc 02 Report Title Sponsoring Directors Contributors Previously considered by 23rd July 2014 Quality Report Dr Vin Diwakar, Chief Medical Officer & Michelle McLoughlin, Chief Nursing Officer Governance Services, Corporate Nursing, Education, Infection Prevention and Control, PICU & Cardiac Services Clinical Risk & Quality Assurance Committee, SLT Situation The enclosed report provides an update on key clinical safety and quality topics. A new development this month has been to concentrate on an identified key existing or emergent theme. This month the focus is on: The risk to patient safety and quality of care resulting from cancelled operations. Background The report is collated from a number of information sources and provides assurance that key risks are being escalated and monitored until sufficient action has been taken to address the concerns. The report includes information on key risks, serious incidents, mortality data, cardiac arrest, respiratory arrest, other acute life threatening events, infection control data, Safety Thermometer data, Net Promoter Question results, and data from the PED database. Information on Never Events and other safety information is included by exception. The report now aligns information against Trust priorities and measures. Assessment Achievements Information suggests that BCH continues to provide high quality, safe healthcare with a good experience for our patients: • 546 positive comments • Zero new Never Events for 15 months • Over 78% of Patient Experience Feedback is positive • Net promoter scores: Parent /carer 89 Children & Young People 87 • Successful bid for funding from the Health Foundation’s Safer Clinical Systems programme. Demonstrating the safety of the surgical system and the application of the safety case Opportunities for Improvement • 4 new SIRIs • 20 new complaints • 153 new Need to Improve comments Theme for discussion: Cancelled Operations Concerns about high levels of cancelled operations led the Clinical Risk and Quality Committee to examine this issue in detail. • • • There are 9 ongoing or recently concluded formal complaints related to cancelled operations There were 20 PALS Contacts during Quarter 1 related to Cancelled Operations The number of cancelled operations flagged as nationally reportable in June 2014 is 54 and is above average. Total hospital cancellations at 261 are high compared to May (169) and we remain above our strategic goal of a reduction on 12/13 levels. There were seven breaches of the 28 day standard in June. In March 2014, Clinical Risk & Quality Assurance Committee received a detailed risk assessment considering the impact of cancelled operations on patient safety. The risk assessment also considered the global service delivery risk to the organisation. The risk assessment used central cancelled operations data but also specifically drew on relevant reported incident data, formal complaints and PALS contacts. Due to the control strategies we have in place the risk to patient safety was considered to be low. The vast majority of cancellations resulted in no harm with a low level of minor temporary harm also recorded. However, the poor experience of patients is an ongoing concern. One the main causes of cancellation is the lack of availability of a Paediatric Intensive Care bed due to more urgent or long term patients. A Critical Care Summit took place in July, attended by over 40 clinicians, senior nurses, parents, and commissioners. The meeting examined the root causes of problems with PICU availability and suggested 50 possible actions which the trust could take. The recommendations will be assessed and worked up from September 2014. Recommendations • Review the enclosed report and confirm that risks to quality, safety and patient experience are being well managed in the trust Risk Description Failure to correctly identify the greatest risks to the quality of care and safety of our patients. Key Risks Controls • Directorate Governance systems • Board Assurance Framework • Risk Register • Safety Strategy • Safety Dashboard Key Impacts Strategic Objective Strategic Priorities CQC Registration NHS Constitution Other Compliance Equality, diversity & human rights Assurances • • • • Monthly Board Safety Report Mortality Review Monitoring of incident trends Monitoring of complaints trends Every child and young person cared for by Birmingham Children’s Hospital will be provided with safe, high quality care, and a fantastic patient and family experience 3. Further develop our approaches to gaining feedback from staff, children, young people and families to ensure that their voice is heard at every level of the organisation. 4. Further innovate our systems to promote and enhance patient safety and reduce avoidable harm. Standard 16 - Assessing & monitoring the quality of service provision could be affected by a failure to manage risks highlighted by the report. Risks to compliance with other standards may be highlighted by the reports. Patient Rights • Quality of Care and Environment • Treatments, Drugs • Respect • Consent and Confidentiality • Informed Choices • Complaint and Redress The report supports compliance with NHSLA and Monitor requirements Right to life Quality Report: Safety & Patient Experience July 2014 Vin Diwakar, Chief Medical Officer Michelle McLoughlin, Chief Nurse Theme for discussion: Cancelled Operations 1 Cancelled Operations Formal Complaints Waiting, delays & cancellations 30 25 There were 20 PALS Contacts during Quarter 1 related to Cancelled Operations 20 15 10 5 0 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 1011 1112 1112 1112 1112 1213 1213 1213 1213 1314 1314 1314 1314 1415 There are 9 ongoing or recently concluded formal complaints related to cancelled operations Delays to theatre list. Eventually cancelled as the surgeon ran out of time. Planned fundoplication and gastrostomy. Only the latter went ahead, which Mum feels was to save time. Planned surgery using Bone Morphogenic Protein was cancelled with inadequate explanation. 10 9 8 7 6 5 4 3 2 1 0 Cardiac surgery had been Cancelled and rearranged 3 times. Planned removal of K-wires did not go ahead as the bed had not been booked. Concern that surgical bed had been cancelled, due to bed availability Parents unhappy that they were told that the procedure had been cancelled 5 minuets prior to their allocated time slot. Patient arrived at hospital for surgery under the Plastics Team. 3 hours later family were informed that the surgery had been cancelled several weeks ago and attempts to contact the family by telephone were unsuccessful. Given a date for surgery in May, but it was cancelled due to lack of beds. Reassured that child would be prioritised and not cancelled again. Given a date in June cancelled the evening before due to lack of beds. 2 Cancelled Operations On The Day - National Definition 2012/13 80 2013/14 2014/15 Avge 66 70 54 60 50 40 28 30 20 10 Apr May Jun Jul Cancellation by Specialty April – June 14 16.0% 14.0% 12.0% 10.0% 8.0% 6.0% 4.0% 2.0% 0.0% Aug Sep Oct Nov Dec Jan Feb Mar Reason for cancellation April – June 14 30.0% 25.0% 20.0% 15.0% 10.0% 5.0% 0.0% 3 A patient’s story I’m a single mum with 3 children. I am separated from my children’s father so live on my own in Hampshire with XX and my other two children, aged 12 and 9. This is our cancelled operation story…… 1st operation planned for 18th with TCI on 17th. Chosen because of the school holidays. 15th : Mum was called at home by Consultant’s secretary to cancel the operation due to no PICU bed. No alternative date was given and mum was told she was on call and likely to be asked to come in next week. Mum not given a named person to contact Mum had not heard anything so called the secretary back approximately a week later and was told there may be a bed this or next week. Mum was told she would get a call by Monday. On Thursday, mum was called at 11am and was asked if she could come to hospital before 6pm that same day for surgery on Friday. Mum arranged childcare and XX came to hospital where he was prepared for theatre, a cannula was inserted, IV fluids were started and he was starved. Told XX would be going to theatre 1011am in the morning. I found the situation stressful but fully understood why XX was cancelled and that there were other children that needed surgery sooner On Wednesday XX was prepared for theatres again (starved etc). The nurse looking after M told mum that PICU was full again so the operation was cancelled. The ward manager spoke to mum about the cancellations and the liaison team was informed. Monday came and mum was told the operation would not take place today, but perhaps on Tuesday or Wednesday. Mum and XX went to Ronald McDonald house. He still had his cannula in and was asked to come back twice a day to have the cannula flushed and checked. “I wish they had taken the cannula out and we felt isolated in RM house with no TV in the bedroom and no Wi Fi” In the morning, mum was told the operation was cancelled due to no PICU beds. Mum was told that surgery would definitely not happen over the weekend, possibly on Monday. This has caused a financial burden on us, especially driving back and forth between hospital and home. Although I get some money back for petrol, it does not cover the full cost and the financial worries of living at BCH including food and expenses. The Liaison nurses are helping me with this. On Thursday Consultant apologised to mum and said that the operation would not be until next Wednesday or Thursday, but could not guarantee this. Mum was given the choice to go home or stay. She chose to go home because of child care arrangements. On Sunday, mum was called at home by the ward nurse and told XX was 1st on the list in the morning and was asked to come back to BCH by 6pm for surgery on Monday morning. Child care was arranged. XX went to surgery on Monday morning. What are the causes of cancellations and where in the process do they occur? Hospital Cancellations Operation not necessary 14% Patient not suitable for OP 11% Unfit with acute illness 6% Lack of theatre time 6% Surgeon Unavailable 4% Anaesthetist unavailable 2% Bed Shortage 26% No ITU bed 8% Emergency Admission 16% Admin error 2% A third of cancellations due to patient-specific factors. A third due to bed shortage. An third in response to emergencies. and problems on the day (none assigned to transplant in this quarter) Risk Controls Risk that reduced bed availability leads to increased cancellations Day prior to admission review of bed situation to identify whether cancellations could be made the day before, this is then reviewed with the Consultants to identify clinical priority. Daily 8.30 Ward Manager Bed Meeting – this has been in place for the past 6 months and is where TCIs for the day and discharges are discussed. Any patients that need to be cancelled on the day are discussed with the Clinician regarding clinical priority or to understand any co-morbidities, eg learning difficulties or pre-op preparations. Any on the day cancellations are prioritised to be re-admitted within 28 days. This is monitored on a daily basis and a report shared weekly with COO. Risk that reduced PIC bed availability leads to increased cancellations of cardiac patients Consultant surgeon of the week has clinical oversight of all patients waiting for operations. They review and prioritise taking into account any new tertiary referrals received which are predominantly new born/neonates The surgical team use the PICU electronic bed booking system and adjust the booking sequencing according to clinical prioritisation. The consultant surgeon will also discuss cases on a daily basis with the PIC Consultant of the day. The PICU team advise on likely patient movement weekly and there is a daily assessment of likely discharges at 4pm. The team review what is on the electronic bed booking system and discuss with the booking in clinician if there is any capacity mismatch. Parents are advised about the reliance on a PIC bed. Theatre capacity is available every day to ensure access to elective and emergency demand and to ensure emergency demand does not displace elective demand. During times of high demand or low PIC we discuss with the wider PIC community, deploy additional retrieval teams to support transfers to non specialist centres and back transfers and finally to other specialist centres and will refer cardiac cases Out of Region. In this situation it's escalated to Executive level and Commissioners are notified. Risk that inefficient use of Theatre time leads to increased cancellations Reviews of all lists to ensure they are not over booked. Queries are checked with the clinical team and then operation booked may be readjusted on ORMIS. The list is locked down 2 weeks prior to the operation. Pre operation checklist to check surgeon anaesthetist staffing and kit required. Any queries checked with the management team and set out in the weekly scheduling action log sent to all service managers with a responsible officer identified to complete required tasks. On the day of operation the theatre coordinator reallocates staff if required. Lists are staggered if any issues present on the day. The WHO checklist may identify last minute issues and no operation will proceed if any aspect is deemed as not being safe such as missing or damaged instrumentation where no other replacement can be secured quickly. We report lost, missing and damaged items sent to BBraun as per the pan Birmingham non conformity SOP. Items that are missing identified at team brief are fast tracked over from BBraun as they are able. 6 Harm Caused There were 607 cancellations affecting 528 patients • • • • 1 cardiac patient was cancelled 6 times, 5 times due to lack of PIC beds, once due to emergency/trauma. They were the subject of one incident during this time; this was unrelated to the cancellation and caused no harm . 1 cardiac patient was cancelled 4 times due to lack of PIC beds, They were not subject to an incident or PALS/Complaints contact. 8 patients were cancelled 3 times, 1 haematology patient was cancelled 3 times, due to their unsuitability for treatment. Of these ‘cancelled 3 times’ patients 5 were cancelled due to unsuitability for treatment 53 patients had a procedure cancelled twice. 464 patients had a procedure cancelled once. • 12 of these had an associated PALS contact, • 3 had an associated complaint, • 18 were subject of an incident report relevant to the cancellation, • 2 were subject of an incident and families complained • 1 incident had an impact of 3 (moderate, temporary harm) • 5 incidents had an impact of 2 (Minor harm) Risk Scores Patient Safety risk score = 8, Moderate Likelihood = 2: 5% of cancellations led to an incident report being completed. Severity = 4: The median harm score associated with those reports was 2. However, since this risk potentially affects patients across the Trust a consequence modifier of +2 is added to the score. Service Delivery risk score = 20; High Likelihood = 5: In Q1 2014/15 there were 368 surgical cancellations. Each day saw a cancellation. Severity = 4: Within the risk matrix Service/ Business Interruption descriptors, ‘Loss/ interruption > 8 hours‘ is scored at 2. However, since this is a service critical to the Trust a consequence modifier (+2 is added to the score) New Events & Concerns There have been no new Never Events since 15/4/13 There have been 4 new SIRIs 14/15:22 Failure to identify NAI before discharge resulting in a patient being put at risk of further injury. 14/15:21 Severe tissue injury to buttock. This is believed to be a chemical burn caused by the patient’s faeces. The patient is a very complex cardiac patient and had been suffering with gut motility problems. Documentation records that the patient was promptly cleaned after each episode of diarrhoea. 14/15:19 Loss of power in the feet following spinal surgery. There may have been a delay identifying the loss of function and therefore instigating treatment. The patient is currently expected to recover full functionality. 14/15:15 Unexpected death of a patient with Epidermolysis Bullosa. The patient had been admitted with possible sepsis and was treated for this. They had clinically improved and were due to be discharged the following day, but unexpectedly passed away during the night. There have been 20 new Formal Complaints Need to Improve Comments Complaints Q1 waiting delays and cancellation June 2014 staff attitude Quality of Treatment Communication 2 29 26 28 20 PALS Q1 2014/15 9 84 67 14 17 50 45 40 35 30 25 20 15 10 5 0 Waiting, delays & cancellations Quality of Treatment Other Staff Attitude Communication Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 Q2 Q3 Q4 Q1 1011 1112 1112 1112 1112 1213 1213 1213 1213 1314 1314 1314 1314 1415 New Formal Complaints 25 20 15 10 5 Jun-14 Apr-14 May-14 Feb-14 Mar-14 Jan-14 Dec-13 Nov-13 Oct-13 Sep-13 Aug-13 Jul-13 Jun-13 May-13 Apr-13 Feb-13 Mar-13 Jan-13 Dec-12 Nov-12 Oct-12 Sep-12 Aug-12 Jul-12 Jun-12 May-12 0 Mother raised several Mother has raised concerns concerns in relation to the stating that Consultant co-ordination of her son's Paediatric Urologist failed to care between specialties, diagnose undescended testis including cancellation of on two occasions. surgery due to bed availability Dad raised concerns following the letter sent to his family in relation to the confidentiality breach, where a handover sheet had been found outside the Trust. Mother is unhappy with the treatment and diagnosis that their child received. Following PM results, the family were told their child had a rhabdoid tumour. A follow up letter mentioned that if the Consultant knew it was a rhabdoid tumour, they would have chosen a different treatment. The family have numerous questions. Mother states that an Orthoptist continued described her child as uncooperative during an assessment, and she disagrees. Parents have raised concerns about the delay in being consulted by a member of the Paediatric Surgeon team on admission. Mother has raised concerns regarding the quality of care received from a Consultant Nephrologist. Mother feels that the Consultant has not listened to her, disagrees with the diagnoses given and wishes for it to be removed from her child's records. Mother of patient unhappy with repeated cancellations of operation and delays to treatment. Mum had visited her GP, as her son had painful, swollen testicles, and was told he had a trapped nerve and needed surgery immediately. Surgery took place the next day. The Consultant surgeon subsequently informed the family that their son's ‘testicles had disappeared’, and if the operation had been performed immediately this could have been prevented. Foster carer states that as staff had failed to read the patient‘s medical records, they were Patient arrived at hospital for surgery under the Plastics unprepared for the admission and the procedure was cancelled. Team. 3 hours later family were informed that the surgery Following incidents reported to the Accommodation Manager involving the communal kitchen and had been cancelled several weeks ago and attempts to bathroom areas a family have been asked to leave hospital accommodation. he family believe that contact the family by telephone were unsuccessful. they have not been listened to, misunderstood and the situation not dealt with appropriately. Family are concerned that the operation for their child's undescended testicle was not performed correctly. Dad wrote in to complain that his son should not have been sectioned under the Mental Health Act. Parents have raised concerns surrounding the quality of nursing care received on MDC. Concerns that the management during admittance to Surgical Day Care was poor resulting in the proposed morning slot being rescheduled to an afternoon slot. Mother felt that her daughter's rights were not respected. Other patients were seen before her and that no-one explained what was happening. She also felt that her daughter's privacy was not respected. Dad has raise concerns about his daughter's Cardiac surgery has been cancelled and rescheduled on 3 occasions. Family state that they informed that they had been referred to the wrong specialty after a wait of several months. The child was internally referred but that referral was subsequently refused and the child referred back with further delays. Mother states that she was spoken to 9 rudely by Consultant Anaesthetist. Closed SIRIs There were 3 closed SIRIs in June Summary 14/05:02 Delays processing referrals from other organisations have resulted in delays in outpatient appointments. One of the patients involved had symptoms which indicated a brain tumour. That patient was reviewed urgently and does not have a brain tumour. None of the patients involved have suffered from harm. Key Actions The root cause of this incident was described as variation across the specialties with how referral letters are handled. •The Call centre processes will undergo redesign. •The General paediatrics workflow will undergo redesign. •A key component of the Call Centre redesign will be to identify more effective ways of monitoring workflow. 13/14:87 A patient was transferred to BCH from a DGH for line insertion. The patient was known to BCH because of his underlying skin condition. The patient unexpectedly suffered a cardiac arrest and passed away. The patient’s death was considered unavoidable and solely due to the severity of his condition. However, some recommendations were made to improve processes, including: •We will raise awareness at BCH about the significance of very high lactate levels even when the rest of a patient’s blood markers are normal. 13/14:83 A PICU handover sheet was found off-site in a public location by a member of BCH staff. This sheet contained patient confidential information. There have been 2 subsequent incidents with very similar circumstances. While we continue to work towards an electronic handover solution we will develop the handover sheet to include a watermark and so that it is printed on a specific colour which will act as visual cues to prompt staff about the importance of keeping these documents safe. Posters have been displayed across the Trust reminding staff about the importance of document security. Specific guidance has been added to the Information Governance Policy in relation to the practice of taking handover sheets off site. This guidance has been publicised across the entire organisation via a joint letter from the Chief Nurse and Chief Medical Officer. 10 There were 12 Closed Complaints in June Summary Key Actions Father wants to know why child was not referred to Respiratory care earlier. •Explanations provided at a follow up meeting with father. Requested pressure cubicle for child and wants transferred to PAU and accommodation. Mother is unhappy that cardiac surgery is now to be conducted at the QEH • Consultant to work closely with the relevant service manager on complex cases to ensure and would like to know why the surgery was cancelled. communications are clear and delivered in a timely fashion. •Tracking of correspondence to be used on Heartsuite for out of region patients. •Review of transitional care arrangements. Mother unhappy with change of medications and no follow up. •Apology given and case discussed with the epilepsy team. inconsistent advice from Doctors. Epilepsy nurse not returning phone call. Father has requested a written response as to why his child suffered blood loss resulting in a further urgent procedure taking place. Concerns with the quality of medical and nursing care received within the Emergency Department and GP Referral Unit. Mother has raised concerns surrounding a communication she has found within her son's medical records. Referring to her as ‘difficult’. Parents raised concerns in relation to care given on Ward 2. In particular, infection control and barrier nursing. Father has raised concerns regarding a lack of communication from a Consultant Neurologist. Mother has raised concerns about the quality of medical care received from a Consultant Gastroenterologist. •No recommendations were made as the post operative bleed is a recognised complication of a tonsillectomy. •Review the option to have a system of "Open Access" for patients that may need to return to the hospital on successive days. •Further training in relation to he Trust Infection Control Policy. •Case to be used as part of our ongoing training for all medical secretaries within BCH •The revised nursing assessment chart now has infection control status box. •The storage of oxygen mask on Ward 2 has been discussed with the ward manager and these are now stored in a more accessible place. •Addressed via a letter from the Consultant. None. Concerns that notes were not available prior to a clinic appointment. Apology given. Father questioned why a full skeletal x ray and head scan were performed after being admitted with a wheezy chest. Claims to not have been informed of Hospital staff meeting with Social Services. Mother was unhappy with treatment and transition of care for her child. •The importance of clear communication has been shared with those concerned None 11 Patient Experience Database (PED) The top 5 positive comments continue to reflect satisfaction with Jun-14 Directorate Total Total Positive Need to Improve %+ve CAMHS 92 46 46 50 Clincial Support Services 109 67 42 61.47 Medical 118 87 31 73.73 Specialised Services 279 257 22 92.11 Surgery 100 88 12 88 Trust 699 546 153 78.11 Adult 416 86 82.87 Young Person 130 67 65.99 nursing care, the overall experience of children, young people and families, care by Allied health Professionals and overall quality of care. This is consistent with the feedback from the Friends & Family questionnaire and the patient experience APP The need to improve comments are relatively small in number with the highest concerns again relating to waiting and delays - the comments relate to a number of areas but predominantly were about ED and OPD waiting times, and waiting to go to theatre. The last few months we have seen a reduction in the overall number of comments entered on to the PED. This is primarily due to a move in emphasis from the yellow feedback cards – where the majority of comments were previously received to the friends and family questionnaires. You said… We did.… We could improve on waiting times in out-patients We have started a project into the flow of patients through the out-patient department and also addressing the booking of patients into clinics. This project aims to review the times at which appointments are made in clinics that don't run well and reschedule them, to fit a more realistic pattern which will hopefully result in much improved waiting times “The wait time is ridiculous.” “The appt was 10.00am and still not seen at 12.15. Just make one appt at a time instead of booking 4 at a time.” Friends and family questionnaire Jun-14 Directorate Target (20%) Total Total Positive Need to Improve Medical 77 56 48 8 85.71 Specialised Services 29 26 23 2 88.46 Surgery 94 275 235 34 85.45 Trust 88 357 306 44 85.71 Adult 88 357 281 39 78.71 Young Person 42 30 25 5 7 Target responses achieved across parent/ carer inpatient areas Net promoter scores: Parent /carer 89 Children & Young People 87 %+ve ED Directorate Target (15%) Total Total Positive Need to Improve Medical 313 38 33 3 86.84 Trust 313 38 33 3 86.84 Adult 313 38 28 3 73.68 Young Person 129 5 5 0 13.16 All detractor comments have been discussed with the relevant individual ward managers for response and action. Positive Jun-14 Needs to Improve %+ve Room for improvement in both young people and ED responses In order to improve children and young people responses in ED we have introduced more child-friendly forms The issue of noise at night has been raised with ward managers and we will monitor the issue as it continues to be raised through all feedback methods. Feedback App & Social Media During June we received 35 app comments Responding to feedback Finalist “The fire alarm was terrible, too loud, went on way too long, and if it wasn't in that part of the building, why did it go off in the first place. When we were seen the service was brilliant, but the fire alarm was a huge let down.” A new piece of work with the estates and fire team means that the fire alarm will very soon be 'zoned'. this will result in the alarm only sounding in the areas nearest to the trigger location. This will result in less disruption to our patients and their families, hopefully allowing our service users to have a better experience when with us. Social Media The past year has seen an increase of the use of social media by staff. Social media and the app can support our ambition to be open and transparent and encourage frank conversations as well as a great opportunity to interact directly with children, young people and parents. The app and social media provide an opportunity for parents, children and young people to let us know about their experience, both positive and not so good, in real time and for staff to respond directly in real time too. Facebook and Twitter: In June 2014 we received almost 140 comments via the BCH facebook page and twitter account @Bham_Childrens All were positive except 1 twitter comment. The issue was addressed the same day by the Lead Nurse. 14 The Application of Safety Cases BCH have been successful in a bid for funding from the Health Foundation’s Safer Clinical Systems programme. The project involves Demonstrating the safety of the surgical system and the application of the safety case A Safety Case is a structured argument, supported by evidence, intended to justify that a system is acceptably safe. Safety cases are often used in highly regulated industries such as the nuclear industry to demonstrate that systems and processes are safe, prior to their implementation. Until recently their use in healthcare has been limited to the use of medical devices. The overall aim of the project is to provide hazard and risk analysis and sense checking around the level of safety of the complex surgical clinical care pathway at BCH. We intend to use a safety case approach to achieve this aim and explore the feasibility of using the safety case methodology across a complex clinical pathway. We see safety cases as a potentially powerful tool underpinning and aligning themes, helping us to consider safety as the ability to succeed under varying conditions, rather than the absence of harm. In theory, this will allow us to engineer resilience into our systems by identifying those aspects of the system requiring redesign. Patient Safety Study The Collaboration for Leadership in Applied Health Research and Care - West Midlands (CLAHRC- WM) have agreed to work with BCH on a research project designed with the intention to produce insights for developing the capacity needed to translate evidence into practice for quality improvement, specifically in the domain of patient safety. The research will study the use and flow of patient safety evidence at BCH and will consider the challenge in assimilating evidence derived from the frontline of clinical service delivery through the clinical governance infrastructure. The initial focus of research will develop insight across about the corporate management and governance of risk evidence. This research will be undertaken through non-participatory observation and interviews. Tracer studies will be used to follow the processes and practices associated with evidence ‘flows’ at middle levels of the hospital. Specific studies will be identified through insights developed in phase one. The safety case method is still new and relatively untested in a health context, particularly in its application to an existing system. 15 Monitoring Infection control June 2014 Infection No. MRSA Bloodstream Infections (BSI) 0 MSSA BSI (pre 48 hour) 2 MSSA BSI (post 48 hour) 2 E. Coli bacteraemia (pre 48 hour) 4 E. Coli bacteraemia (post 48 hour) 1 Glycopeptide-resistant enterococci 0 C. Difficile 0 MSSA pre 48 Hours 2011/12 MSSA pre 48 Hours 2013/14 MSSA pre 48 Hours 2012/13 MSSA pre 48 Hours 2014/15 5 4 3 2 1 0 MSSA post 48 hours 2011/12 MSSA post 48 hours 2013/14 4.5 4 3.5 3 2.5 2 1.5 1 0.5 0 April May June 5 4 3 2 1 0 E-Coli - pre 48 hours 2011/12 E-Coli - pre 48 hours 2013/14 E-Coli - pre 48 hours 2012/13 E-Coli - pre 48 hours 2014/15 July Aug Sept MSSA post 48 hours 2012/13 MSSA post 48 hours 2014/15 Oct Nov Dec Jan Feb March E-Coli - post 48 hours 2011/12 E-Coli - post 48 hours 2012/13 E-Coli - post 48 hours 2013/14 E-Coli - post 48 hours 2014/15 5 4 3 2 1 0 16 Respiratory Arrests, ALTEs and Unplanned Admissions to PICU Explanation of Data Unplanned admissions to PICU are a measure of how well we are monitoring patients on the wards. Good monitoring on the wards means that we will pick up deteriorating patients more quickly, allowing us to admit them to PICU when required. A combination of high levels of unplanned admissions and low levels of cardiac arrests, respiratory arrests and acute life threatening events (ALTEs) means that we are monitoring and escalating clinical deterioration in a timely manner. Details of Cardiac Arrests In June there were 4 cardiac arrests outside PICU. 2 out of hospital ED and 2 on the wards. None have been classified as predictable or preventable. Number of Emergency Events No of Cardiac Arrests (ex PIC) No of Respiratory Arrests No of Cardiac Arrests (PICU) No of ALTEs 19 18 17 16 15 14 13 12 11 10 9 8 7 6 5 4 3 2 1 0 17 Safeguarding Key Figures Child Protection Training Level 1 99.1% Level 2 87.4.% Level 3 86.1.% There has been 0 Safeguarding SIRI There has been 0 new Safeguarding Complaint There has been 1 “Position of Trust’ case There have been no new recommendations from Serious Case Reviews 100% of BSCB Meetings attended by BCH Executive lead or representative 90% of cases which require peer review /clinical supervision have had this There has been 0 child deaths related to suspected physical abuse/neglect Safeguarding CQUINS: We have had discussions with our Commissioners and agreed some Safeguarding CQUINS for 2014. An agreed Qualitative Audit Proforma will be used to capture key aspects of a child’s journey through the safeguarding process. This will be done via the following groups: •Burns Child Protection Peer Review •General Paediatric Child Protection Peer Review •Emergency Department Child Protection Clinical Supervision Sessions •Safeguarding Operations Group. A Child’s Journey through the Safeguarding Process: A 15 month old baby was admitted following an unexplained fracture to her left arm. There were some issues of delayed presentation. The baby was in a shared care arrangement between parents. The Child Protection process was commenced in ED: •A timely referral was made to Social Care. •A Child Protection medical examination was completed and the child was admitted to PAU. •The Child Protection Nurse met with the family to explain the process. •The Health Visitor and GP were informed and Police involved. •A Strategy Meeting was held at BCH under CP procedures. •A Section 47 Enquiry opened. •A Social Worker met the family to agree a safe discharge plan before the baby was discharged to the care of grandmother. Mother’s Feedback: The process was stressful, however, good explanations, support and information were received from all professionals involved. Mother was happy with the process and clearly understood the need for the investigation. She stated that there was nothing in the process that could have been better. All professionals involved recognised the need to safeguard and promote the baby’s welfare and safety. Mortality Past Harm Mortality data is presented in a number of ways, and an overall picture can only be gained by using a number of indicators. These are: •Absolute number of deaths per time period. •Number of deaths per time period per 1000 admissions. •Standardised mortality ratio (See next slide) •Cumulative sum (CUSUM) charts. •Review of individual deaths. Inpatient deaths per 1000 admissions This is a simple calculation to overcome any variations in admission numbers over time (e.g. the hospital may have more admissions in the winter months) or between hospitals of different sizes. Data can be compared between organisations by this method as it allows for different admission numbers but it is limited as a tool for comparison as there is no modification for case mix. The graph on the right shows the number of inpatient deaths per 1000 inpatient admissions at BCH since June 2012. Please note that the data does not include deaths which occurred in the Emergency Department. Absolute Number of Deaths The simplest way to represent mortality is as an absolute number of deaths in a particular time period; however it does not take into consideration either the number of admissions to the hospital or the case mix of patients. It is useful only as a sense guide to other data as it has not been modified in any way. Data cannot be compared between organisations in this format. 16 Deaths Deaths per 1000 Admissions 14 12 10 8 6 4 2 0 19 Standardised Mortality Ratio (SMR) In order to account for differences in case mix for different organisations the idea of standardised mortality ratios has been developed. This attempts to account for differences in patients, such as diagnosis, age and pre-existing medical problems, and allows for comparisons between hospitals. A standardised mortality ratio (SMR) is the ratio of the actual number of deaths in a hospital within a given time period, to the number that might be expected if the hospital had the same death rates as a larger reference population (e.g. all English Hospitals). The SMR scores can be presented in a number of ways. Run Chart This shows how the standardised mortality rate of a hospital changes over time. If there are a small number of deaths in each time period then the month to month variation can be quite wide (as is the case with BCH where there are on average 4-12 deaths a month). 20 Bar chart presenting data comparing a number of hospitals: This shows the position of an individual hospital in comparison with its peer group. It is easy to understand but does not give much information about whether our outcomes are unusual. The graph presented below shows 6 months’ worth of data rather than 12 as previously presented. Our SMR has fallen from 161.77 to 152.83 Movement in last month Funnel plot This shows the standardised mortality ratio on the Y axis, and the number of expected deaths on the X axis. Control limits can be applied, so that it is possible to see how likely that the variation from a score of 100 is by chance only. In the example below an amber dot occurs if there is between a 0.3% (1 in 330) and 5% (1 in 20) likelihood that the score is different from 100 by chance and a red dot if there is less than a 0.3% likelihood that the score is different from 100 by chance. Such warnings should be investigated as to cause. The funnel plot below is presented using 6 months’ worth of data. We are in the red section of the funnel plot. 21 Deaths in the Paediatric Intensive Care Unit (PICU) CUSUM Charts Another way of representing outcome data is by cumulative sum charts. These can be used where there is a score available to give a risk of mortality for each individual patient. Currently this method is in use at BCH for intensive care. The charts use data from all patients, not just deaths, so are more powerful than SMR in detecting problems. For BCH, the PICU CUSUM is a good reflection of overall hospital mortality as over 70% of deaths at the hospital occur on PICU. There is no evidence of systemic care failures which could have contributed to deaths on PICU. 22 Deaths in Cardiac Services CUSUM Chart One of the Trust’s highest risk specialties is Cardiac Services. The nature of the activity means that proportionally more of our mortality is related to that specialty than others. The team carefully monitors clinical outcomes to ensure that that we are providing high quality care. The CUSUM chart is a graphical representation of the outcome data for the specific procedures which are nationally monitored (70-80% of our patients fall into this group). In addition, the team also monitors overall mortality for all surgical patients. In 2000-2005, the overall mortality rates (30 days postoperatively) was 4.8%. In the period October 2010 – September 2012 this had dropped to 3.3%. An upward movement in the chart means that the outcome for a specific patient was better than expected. A large increase means that the outcome was significantly better A downward movement means that the outcome for a specific patient was worse than expected, again the size of the decrease is a measure of how much worse the outcome was than expected Overall our outcomes are better than expected. However, please note that the baseline will be reset on a regular basis, so we do not expect to move further and further from the x-axis 23 Item . Board of Directors Public Meeting Thursday 31st July 2014 Enc 03 Strategic Objective/ Enabler Every child and young person requiring access to care at BCH will be admitted in a timely way, with no unnecessary waiting along their pathway Report Title Performance – June 2014 Performance Report Sponsoring Director Deputy Chief Executive Author(s) Head of Health Informatics, Performance Manager Previously considered by Finance and Resource Committee Situation This report provides the June update on this month’s Trust Performance supporting improving our patient experience. The report highlights where performance is not being met and any concerns or improvements. The attachments provide: • Further details on our current and comparative performance Background There are five areas to highlight: Access to services 1. Diagnostic waits including MRI The trajectory for zero MRI breaches by August as reported last month now looks unachievable with latest forecasts being 32 breaches in July and 30 in August. Breaches amount to 7% of the total MRI waiting list. All of these are for non-GA. Additional MRI capacity via a mobile scanner was put in place for June, and whilst this has helped it has not had as significant an impact as was first envisaged as a number of the patients booked for it were not suitable for the mobile scanner. It became apparent that the quality of images was not acceptable eg in some complex cases to meet the clinical need, hence reducing the number of patients who could use the facility. This impacted upon the June figures in particular. This and an increased demand have meant we still are forecasting breaches. Regarding demand, additions to the MRI Waiting List were very high in the last week of June, at 171 the count was the highest in the last 18 months, and above the upper confidence interval (see the SPC chart on slide 8) The mobile scanner is booked again for July. The waiting list has been assessed to make sure the capacity can be filled with suitable patients. A further booking for September is planned. In order to further increase capacity, negotiations are currently being undertaken with Aston University to make use of their 3T Scanner. Of the 32 predicted breaches for July, 16 could potentially use the scanner at Aston. The aim is to get this capacity in place for the last week in July. The size of the MRI waiting list has remained steady in June, despite the increased capacity provided by the mobile scanner. This is due to the increased demand referred to above (15 20% increase in additions.) Looking at all diagnostic wait breaches, there were 27 patients at the end of June who had been waiting over 6 weeks for a diagnostic test, (23 for MRI and 4 for CT). The total breaches amount to 3.1% of all diagnostic waits and this is above the 1% NHS standard. Regarding MRI breaches alone, the 23 breaches equate to 7% of the waiting list. Forward look Recruitment for additional radiographers and radiologists has been successful and a number of experienced staff have been appointed. This will provide more sustainable capacity from October 2014, with increased utilisation of the scanner. The independent review commissioned with a specialist from the Royal College of Radiologists transformation team is complete and initial findings are as expected. A final report is due soon which will provide some guidance on how the team works and what actions can be taken to improve the performance. As reported above, negotiations are on-going with Aston University, to use their top-of-therange 3T MRI scanner, which will increase routine capacity. The second CT scanner is now fully operational. 2. 18 weeks waiting time The 18-week standard was met in June with performance for admitted patients at 90.6% against the 90% standard. 90 admitted patients and 46 non-admitted patients were not treated within 18 weeks due to insufficient capacity (136 patients compared to 91 last month – an increase of 49%). The performance for incomplete pathways increased slightly to 92.9% against the 92% standard. The chart on page 6 shows than increasing numbers are waiting over 14 weeks, and will receive a TCI late in their pathway. This makes it difficult to meet the target and so this trend is a concern as more breaches are likely. The number of patients waiting over 30 weeks is 116 (a decrease from 140 last month), 9 of these had their clock stopped. There were three patients waiting over 52 weeks, all of whom had patient related pauses which reduces the wait to below 52 weeks, (with 2 of these below 18 weeks.) The overall waiting list size showed a small increase which was as expected due to the high levels of cancellations in June. Looking forward, based on current assumptions and forecasts meeting the standard in July will be a challenge and the 18 week waiting time continues to be a risk for the organisation. Demand for elective services is increasing, with referrals growing including from outside of the main Birmingham catchment area. The outpatient list size has increased significantly; by 36% from start of April due in part to this rising demand. There have also been some administrative delays in creating appointments and adding referrals to the list which have had an impact here. If the additional outpatients also need inpatient treatment it will put further pressure on the RTT targets. Regarding the outpatient referrals from outside Birmingham, there has been a 16% increase in these in Q1 2014/15 when compared with 13/14 average. The Contracting Team at BCH are intending therefore to raise this with our lead CCG in order to further emphasise the issue of demand management across associate commissioners. Nationally there is increased scrutiny on RTT and weekly reporting is now required to Monitor and Commissioners on our backlog of RTT patients who are awaiting a clock stop. It has been announced that funding will be made available to support organisations to meet the targets, although It is not necessarily the case that this amounts to additional moneys above tariff. Specialities are putting recovery plans in place, and these plans will be submitted to commissioners. CAMHS achieved 98.9% for 18 weeks. However the average wait time has increased to 5 weeks due to data catch up. 3. Emergency The Trust continues to perform well against the 4 hour standard and met the target in June. The 95th percentile performance was 3.93 hours. This was despite continued high levels of demand. The following Emergency Department (ED) standards were not met: • The local ED triage objective (all within 15 minutes), the 95 percentile performance • being 33 minutes (previous month was 32). Median time to be seen was 64 minutes (target is 60 minutes). This report does not normally report patients deflected from ED as we don’t normally have any of these. However this month 4 patients were transferred. This is as a result of a series of measures to create capacity in ED on the morning of 11th June, to ensure we could provide a safe emergency service. The other measures included additional consultant support in ED and the wards, cancellation of operations, delays in tertiary admissions and diverting ambulances (except trauma & life threatening cases) to HEFT. The parents of the transferred children agreed to the transfer and this was to the most appropriate DGH for them (based on where they lived). The KIDS team supported the transfers. Utilisation of resources 4. Cancelled operations In June there were 54 patients or 2.58% of all operations were cancelled on the day due to hospital reasons. This is more than previous months (at 28) and June 2013. In addition there were a further 207 patients that had their operation cancelled by the hospital before the day of the operation. Similar to last month, the total number is above the upper confidence level and any previous months. There were seven breaches of the 28 day standard in June. The target is zero except that it is recognised that there may be breaches due to no PICU capacity. 2 of the breaches were due to no ward beds, 3 due to no ICU beds and 2 due to emergency cases. Directorates continue to review how they are managing this target given the relatively small numbers in the context of the total activity each month. Of the total of 607 cancellations year to date 158 (26%) were due to no ward bed being available, 100 (16.5%) were due to emergencies and only 50 (8.2%) were due to no PICU bed. This compares to 24% of all cancellations being due to no PICU beds for 2013/14 and 14% being due to ward beds. The Surgical Directorate had 393 (65%) of the cancellations with plastics having 88 (14%), Paediatric surgery having 73 (12%) and ENT having 69 (11.4%). 33 patients had an operation cancelled more than once by the hospital, with total cancellations for these patients totalling 80 operations. Work continues to understand the drivers for the cancellations and bed capacity issues, to minimise the level of cancellations. One factor is that the classification of cancellations that are the responsibility of the hospital changed in April 2014 so that more are being counted as such. For example ‘patient not suitable for op’ now maps to hospital cancelled. In total this has added 30% to the total number. 5. Long stayers and delayed discharges Our ability to deliver elective activity has been impacted by the high level of emergencies. Another factor is the increase in the length of stay. The charts on page 17 of the report show the profile of those in inpatient beds. The overall number of children staying more than seven days is increasing, in particular since the last quarter of 2013/14. There is also an increase in those staying over 30 and 90 days. Some of these will link to the delayed discharges referred to below whilst others still need treatment in hospital reflecting the complexity. Paediatrics is the specialty which has experienced the biggest growth in these longer staying patients. Prior to Winter 2013 there were on average 15 Paediatrics patients who had been in the hospital more than 7 days at any one time. During Winter this increased to 30, but rather than come down since then the number increase so that for May 14 and first half of June it was closer to 35. The second half of June has at last shown some reduction in the numbers of long stayers for Paediatrics however, with numbers in the low to mid 20s. In June there were 4 children (compared to 7 last month and 9 the month before), who were fit for discharge but waiting for other reasons. One has waited for over a year. This is the lowest number for some months. The reasons are for housing and social care reasons. The total number of bed days relating to these delays is 916 days. In addition there were seven CAMHS patients with delayed discharges (of 817 days). Six were waiting for placements and/or funding whilst the seventh was waiting on agreement of funding. These delayed discharges have been escalated to commissioners. Update on other areas of performance Tertiary referrals and Home Referrals There were seven West Midlands and one out of region patient who couldn’t get a bed in June. In the longer term, there has been a significant drop in refusals since December 2010 with the numbers fluctuating between 0 and 6 each month, although for June the number of refusals was 8, higher than normal due to the high demand within the emergency department. Twenty nine, of which twenty five were West Midlands patients that were admitted had to wait over 24 hours before a BCH bed was provided. This was despite continued high levels referrals and demand for beds. When a referral is received the specialty consultant is asked to identify the time period in which the child should be admitted. This is under 12 hours, 12 – 24 hours or 48 hours. When comparing actual time to admission against recommended time for admission, 81% of requests were met compared to 87% last month. The decrease is due to demand for beds from the high Emergency Department attendances. 92% of patients who were assessed as needing a bed within 12 hours were admitted within the timeframe, again lower than last month’s 99%. Internal Audit completed their review of this indicator for data quality and have provided significant assurance. Recommendations and an action plan for their implementation have been agreed. PICU (Paediatric Intensive Care Unit) referrals The West Midlands (WM) PICU service is provided by BCH, University Hospitals of North Staffordshire NHS (UHNS) Trust and the KIDS (Kids Intensive care Decision Support) service run by BCH. Twelve West Midlands (WM) patients and ten non WM patients could not be supported due to hospital reasons. This is higher than last month due to the increased ED demand already mentioned. CAMHS referrals The CAMHS Tier-4 (Child & Adolescent Mental Health Service) West Midlands service is provided by BCH and other providers (some private) with BCH providing the assessment of all requests. Due to capacity and urgency, Twelve patients could not be supported by BCH CAMHS in June; lower than last month (at 17). There continues to be significant capacity pressures across the West Midlands and nationally for Tier 4 beds. Internally the ERA service has now extended to 7 days a week and this has had a positive impact providing a more rapid response where needed and ensuring young people receive support whilst waiting. Assessment Continued increases in elective demand have led to an increase in inpatient and outpatient waiting lists and the waiting times for MRI. The demand is not just from Birmingham, there is growth from across the West Midlands. Reductions in beds and limited access to services in other parts of the local NHS are playing a part. The additional demand is putting us at risk of not meeting our access targets. Emergency demand is up in ED, and although short stay emergency admissions are down, longer stay patients for example in paediatrics have been creating pressures on beds. There has been a resultant impact on cancelled operations. Plans to reduce delays are noted below. PICU Capacity: • • We expect a delay to increase beds from 28 to 31 beds. This is predominantly due to staffing issues in nursing. Therefore there will continue to be an impact on performance. Commissioners have been informed that a 31 beds position is unlikely until quarter four of 2014/15. Recent interruptions in the supply of medical trainees are having a short term impact on capacity but a range of actions have been put in place to mitigate this risk. Theatre Capacity: • • • Weekend working, including lists on Sundays and additional capacity at the Birmingham Treatment Centre have been in place for some months now. A Theatre Working Group is in place with a focus on improving staffing levels to maintain and increase theatre capacity. A project is underway to look at how we ensure all elective patients undergo pre- • • • • admission which will help to reduce the risk of cancellation. Business case for extending capacity through use of the Plaster room approved, and is expected to become operational in October 2014. Newton currently reviewing the flow management through theatres. Their scheduling tool is planned to go live in early August In August, there is an intention to expand the use of the laser theatre to support more emergency lists to stop them overrunning into elective lists. Are considering the use of a mobile theatre and ward to increase capacity, alongside other proposals stemming from the work being done with commissioners around Operational Resilience Diagnostic waits - MRI capacity: • • • • • • • A medium term capacity plan for Imaging is being produced which includes new ways of working. New consultants are now in place and more expected to start in September 2014. Additional lists for GA were agreed both in week and on Saturdays for January and May, with discussion over this continuing in future months. Mobile scanner was used in May and June and has been booked for July Extended working hours agreed with radiographer workforce. New roster agreed with radiologists. Investigating use of Aston University Scanner, (which will provide more routine additional capacity). The Medium Term Clinical Estates Strategy is being developed to identify future demand and solutions to meet demand. Recommendations The Board is asked to note the performance and plans for further improvement. Key Risks Risk Description Controls Assurances Escalating demand for our Discussions with Maintaining scrutiny on services, potential risk of commissioners to be held performance against various failing access targets about demand management RTT targets Bids against operational resilience moneys Insufficient capacity in place Appropriate escalation to meet service demands systems in place Validation of waiting lists stepped up Daily, weekly and monthly reporting in place. Specialty recovery plans and Revised capacity plans being plans for additional capacity produced. being put in place as part of response to ‘Operational Resilience’ Capacity plans being renewed and developed. This includes modelling capacity/demand between now and 2020 (new hospital) Key Impacts Strategic Objectives CQC Registration outcome) NHS Constitution This reports covers progress against meeting the strategic objectives linked to supporting improving our patient experience. (state 4: Care and welfare Yes – treatment within 18-weeks is a requirement within the NHS Constitution. Other Compliance (e.g. Many of the indicators are local or national standards NHSLA, Information monitored by the Department of Health, Monitor and our Commissioners. Governance, Monitor) Equality, diversity & human The report considers any particular impact on patients with learning disabilities, and on different ethnic groups. rights Trust contracts Non-delivery of NHS standards can result in financial penalties Other Meeting the strategic objectives raises the profile of Trust locally, regionally and nationally Operational Performance Report Month 3 2014/15 Performance for June 2014 David Melbourne Paul Franklin Pragati Raithatha Deputy Chief Executive Officer and Chief Finance Officer Head of Health Informatics Performance Manager 1 Operational Performance Indicators How our patients access care ED - time in ED 18 weeks performance (incomplete) PICU – non WM patients supported ED – time to seen 18 weeks performance (admitted) PICU – non WM patients not supported ED – Time to triage (all) 18 weeks performance - CAMHS PICU – WM patients not supported ED – time to triage (ambulance) Long waiters - patients not treated within 18 weeks due to insufficient capacity MRI waits over 6 weeks ED – Left without being seen Long waiters - patients not treated within 30 weeks In region Tertiary referrals sent elsewhere ED – Unplanned readmissions Long Waiters - patients waiting over 52 weeks Tertiary patients waiting over 24 hours for a BCH bed Patient Deflectors 18 weeks performance (non admitted) CAMHS Patients that requested a T4 bed and were not admitted Utilisation of our facilities Cancelled operations – national definitions Cancelled operations – breaches of 28 day standard Cancelled operations – all hospital cancellations Cancelled operations - equipment failures or admin errors Long stay patients and patients with delays after being declared fit for discharge Cancelled operations - patients cancelled more than twice 2 Operational Performance Report Month 3 2014/15 Performance for June 2014 How our patients access care 3 Emergency Department 95th % time in A&E: 3.93hrs 95th % time to triage (all): 33 minutes Median time to be seen: 64 minutes 95th % time to triage (ambulance): 13 minutes 4 Patients Deflected Left without being seen: 2.17% ED re-attenders for related condition 2.44% ED overall position: June has been extremely busy for ED. Despite this, we continue to see ambulance patients within target and have met the four hour wait target for 15 consecutive months and only small numbers of our patients are leaving the Dept. without being seen. It is also pleasing that re-attenders have reduced compared to the previous month. However three targets have not been met. The target of all patients (not just ambulance patients) having an initial assessment within 15 minutes is routinely not met, but the target on seeing patients within 60 minutes of arrival was also not met this month by one minute. This report does not normally report on the final missed target (patients deflected from ED) as there are none. However this month 4 patients were transferred. This is reported by the relevant Operational colleagues as being part of a series of measures to create capacity in ED on the morning of 11th June, to ensure we could provide a safe emergency service. The other measures included additional consultant support in ED and the wards, cancellation of operations, delays in tertiary admissions and diverting ambulances (except trauma & life threatening cases) to HEFT. The parents of the transferred children agreed to the transfer and this was to the most appropriate DGH for them (based on where they lived). The KIDS team supported the transfers. Total Time Spent in A&E Standard ≤ 4 hours (95th Percentile) % Patients Who Left ED Without Being Seen Standard < 5% Time to be Seen Standard ≤60 minutes (Median) 90 4.70 7.0 6.0 4.50 5.0 4.30 4.0 80 70 60 50 4.10 3.0 2.0 3.90 1.0 3.70 0.0 A M J J A S O N D 2012-13 2013-14 2014-15 Target J F M 40 30 20 10 3.50 0 A M J J A S O N D J F M A M J J A S O N D J 2012-13 2013-14 2012-13 2013-14 2014-15 Target 2014-15 Target F M 4 18 week waits Admitted Non admitted Incomplete • 90.6% • 95.6% • 92.9% 18 weeks overall position: all targets were met in June 2014. The admitted performance level has decreased compared last month’s figure of 91.3%. The incomplete pathways remain just above target. 116 patients were waiting over 30 weeks and also the number of patients receiving TCIs late in their pathway remain relatively high, so the pressure on waiting times is likely to continue going forward. It is anticipated that meeting the targets in July 2014 will be challenging. 136 patients were not treated within 18 weeks due to insufficient capacity. Increase in non admitted clock stops from 4 to 46 is mainly due to additional cardiology clinics to clear waiting patients. 18 weeks admitted performance 94.0% 93.0% Patients not treated within 18 weeks due to insufficient capacity 14 10 11 3 patients were waiting over 52 weeks (All 3 patients had patient related pauses which reduces their wait to below 52 weeks) Admitted Non admitted 112 90 87 90 Jun-14 M 97 May-14 F Target 118 Jan-14 J Nov-13 D 4 1 75 Oct-13 N 2014/15 61 56 62 128 118 73 Sep-13 O 105 Aug-13 S 2 8 Jul-13 A 2013/14 Apr-13 J Mar-13 J 2012/13 4 54 41 25 29 Feb-13 M 42 Jan-13 A 83 Dec-12 86.0% 3 Nov-12 8 0 Jun-13 2 14 87.0% 3 May-13 88.0% 46 4 Mar-14 7 89.0% 12 8 Dec-13 90.0% Apr-14 14 91.0% Feb-14 92.0% The 3 patients waiting over 52 weeks had patient related pauses, which reduces the wait to below 52 weeks, (with 2 of these below 18 weeks). 5 18 week waits Fig 1 - % still waiting for clock stop (incomplete) under 18 weeks Fig 2 - 18 Weeks: Current problem, future problem 600 100.0% 500 98.0% 400 96.0% 94.0% 300 92.0% 200 90.0% 100 88.0% M 2012/13 J J A 2013/14 S O N D 2014/15 J F M Target 0 02.06.13 16.06.13 30.06.13 14.07.13 28.07.13 25.08.13 08.09.13 22.09.13 06.10.13 20.10.13 03.11.13 17.11.13 01.12.13 15.12.13 05.01.14 19.01.14 02.02.14 16.02.14 01.03.14 16.03.14 30.03.14 13.04.14 27.04.14 11.05.14 01.06.14 22.06.14 A Performance for patients still waiting for their initial treatment (either admitted or non admitted pathway) has increased slightly since last month to 92.9% being within 18 weeks (Fig 1.) Regarding patients waiting for an admission (Fig. 2), the green line, (which is the total of the red and blue lines) illustrates the overall potential problems we have in managing our 18 weeks admitted demand; this showed a large increase in December 13 and has steadily decreased until March, but is now higher than December 2013 levels. The blue line illustrates patients with a date to come in who are already over 18 weeks or whose TCI date is over 18. The red line illustrates patients who are waiting 14 plus weeks and do not have a TCI date yet. Both these are increasing and therefore the challenge of meeting 18 weeks for our admitted patients continues to grow. 6 Whole Inpatient waiting list and long waits Whole Waiting List Size (not just RTT patients) 116 RTT patients either still waiting or whose clock stopped after 30 weeks 8000 7000 All Patients Still Waiting or Whose Clock Stopped Over 30 Weeks 160 6000 Specialty break down of the 107 patients still waiting over 30 weeks 140 5000 120 4000 100 3000 80 2000 60 40 20 Inpatients Surg/Cardiac Inpatient Outpatients The overall waiting list for surgical and cardiac stands at 2111, with the total inpatient list standing at 3554. The Cardiac/Surgical list was reducing since the new calendar year but has increased slightly in the last 3 months. The outpatient list size has increased significantly (36%) from start of April due to a mix of rising demand, short term reduction in capacity and admin errors. Specialities are putting recovery plans in place. 73 94 109 116 99 107 At end of June, there are still 116 patients waiting over 30 weeks (either still waiting or who had their clock stopped in the month). Of the 116 patients 9 had their clock stopped over 30 weeks and 107 are still waiting. Jun-14 May-14 Apr-14 Mar-14 Feb-14 Jan-14 Dec-13 Nov-13 Oct-13 Sep-13 Aug-13 0 Jul-13 03/06/2014 03/05/2014 03/04/2014 03/03/2014 03/02/2014 03/01/2014 03/12/2013 03/11/2013 03/10/2013 03/09/2013 03/08/2013 03/07/2013 03/06/2013 0 54 49 54 57 61 Jun-13 1000 140 140 Cleft Lip & Palate Surgery Paediatric Burns Care Paediatric Cardiac Surgery Paediatric Cardiology Paediatric Dermatology Paediatric Ear Nose and Throat Paediatric Neurosurgery Paediatric Ophthalmology Paediatric Plastic Surgery Paediatric Surgery Paediatric Thoracic Surgery Paediatric Trauma and Orthopaedics Paediatric Urology Paediatrics Grand Total 1 2 2 16 1 24 4 1 25 10 1 15 4 1 107 7 Diagnostic waiting lists Diagnostic waits overall position: we continue to fail to meet our key target for MRI. However June breaches are much lower than previous months. Demand continues to be high. The charts below illustrate that demand for diagnostic test continues to be high and the waiting list is showing a slight decrease. There is a switch in the make up of the list towards non GA. MRI Waiting list Number of patients waiting over 6 weeks for MRI (actual and forecast) 123 107 101 106 88 101 500 Aug-14 32 30 Jul-14 Jun-14 May-… Apr-14 Mar-… Feb-14 Jan-14 Dec-13 Nov-13 Oct-13 Sep-13 Aug-13 Jul-13 Jun-13 May-… 23 NON GA WL 1000 0 71 45 51 GA WL 2012-03-… 2012-04-… 2012-05-… 2012-07-… 2012-08-… 2012-09-… 2012-10-… 2012-11-… 2012-12-… 2013-01-… 2013-03-… 2013-04-… 2013-05-… 2013-06-… 2013-07-… 2013-08-… 2013-09-… 2013-11-… 2013-12-… 2014-01-… 2014-02-… 2014-03-… 28/04/20… 29/05/20… 2014-06-… 97 Patients 139 133 115 Total WL 1500 The MRI service continues to be under significant pressure, but actions to manage the position are starting to show results, with 27 patients breaching the 6 week target in June 2014 (23 for MRI and 4 for CT scan.) The forecast position for July is 32 breaches. A nil breach position is now expected to be reached in September, as whilst the capacity is there, it cannot all be utilised as some patients are not suitable for treatment on the mobile facility. However other options such as the use of a scanner at Aston University are being investigated which should reduce the predicted breach position. The SPC chart (right) on total waiting list additions shows that levels of additions remain high. The most recent complete week is well above the upper confidence interval of the SPC chart. Demand is a continuing factor in the achievement of this target. 8 Access to CAMHS Community CAMHS Breakdown of Waiting Time to Assessment CAMHS 18 Weeks Performance A:- 0-4 wks 105 100% 100 95 90 80% 364 708 60% 952 40% 85 20% 80 B:- 4-8 wks C:- 8-13 wks D:- >13 wks 382 361 36 237 1059 755 852 870 766 1465 1117 873 2010/2011 2011/2012 2012/2013 1210 0 76 50 390 0% 75 Apr May Jun Jul 2012/13 Aug Sep Oct 2013/14 Nov Dec Jan 2014/15 Feb Mar 2014/2015 CAMHS are now assessing more of their patients within four weeks (76% so far in 2014/15 compared with 52% in 2013/14.) Data catch-up exercise in the department shows that the average wait is now 5 weeks from 4 weeks in 2013/14, and 8 in 2012/13. The overall level of assessments has reduced over time following the introduction of improved protocols for the management and assessment of referrals. Target CAMHS continue to achieve their 18 week target with 98.9% of patients seen within target in June. CAMHS Patients that requested a T4 bed and were not admitted (month trend) 18 2013/2014 CAMHS Tier 4 Gateway Referrals The no has reduced to 12 16 Total No Referrals 14 GA Completed Referred to SCT 40 12 30 10 20 8 6 10 4 0 2 0 Apr May Jun Jul Aug 2012/13 Sep Oct 2013/14 Nov Dec 2014/15 Jan Feb Mar Tier 4 referrals (in blue) and gateway assessments (the red line) are decreasing since the start of this year and patients not able to access a bed and are referred to the Specialised Commissioning Team has 9 decreased in June to 12 (from 17 in May). Urgent Tertiary and Home Referrals 179 referrals for specialist beds, 150 admitted 7 in region patients unable to get a bed 1 out of region patients unable to get a bed 21 patients no longer required a BCH bed 25 in region patients waited over 24 hours to get a BCH bed 4 out of region waited over 24 hours to get a BCH bed Overall position: Tertiary and home urgent referrals in June at 179 is lower than past three months. 8 patients were unable to get a bed and 29 patients waited over 24 hours (further detail for these 2 indictors about in and out of region is provided above). 81.3% of requests were met within the required clinical timescale. Activity levels The level of urgent referrals is lower this month than for the past three months. Urgent Tertiary and Home Referrals 250 200 150 100 50 0 175 186 199 175 170 188 191 172 182 Home Waiting time vs. clinical target time Clinicians can request the patient to be admitted in up to 48 hours, dependent on their assessment. The graph shows the timescales requested for admittance and time of decision to admit. Overall 81.3% of requests were met in June (compared to 87.5% in May). This percentage has reduced since May due to the high admissions during this month via the Emergency department, resulting in less beds and delaying of tertiary patients 197 177 188 Tertiary 181 225 173 163 169 209 217 Total Performance vs clinical target time for patients provided a bed - home and tertiary referrals - June 14 80 70 60 50 40 30 20 10 0 100% 92% 81% 80% 57% 60% 40% 20% 0% within 12 hours Met 12-24 hours Up to 48 hours Target Time Not met % patients meeting tgt time 10 Urgent Tertiary and Home Referrals Referrals Sent Elsewhere Referrals Waiting over 24 Hours 8 referrals were sent elsewhere in June 14. Referrals sent elsewhere for 14/15 is now 50% of the entire 13/14 financial year total, indicating that the management of these urgent referrals has been challenging. The number of children waiting over 24 hours for a bed after a tertiary referral is close to the average. Referrals were lower this month. 81.3% of referrals were managed within the clinical target time, which is lower than last month (87.5%), due to high Emergency Department demand. Tertiary and Home Urgent Referrals Sent Elsewhere Paediatrics Trend - Tertiary and Home Referrals Waiting Over 24 Hours for a Bed T&O 50 Plastic 45 Surgery 40 35 Resp Med 30 Neurology 25 Nephrology 20 Medical Oncology 15 ENT 10 5 Clin Haem 0 Jun-14 lower ci Apr-14 Avge Feb-14 Over 24 Hr Waits Dec-13 20 Oct-13 15 Aug-13 YTD 14/15 10 Jun-13 5 Apr-13 0 Feb-13 Hepatology Dec-12 Oct-12 Cardiology upper ci Tot 13/14 11 PICU Demand and KIDS Service 10 non West Midlands patients could not be supported 12 West Midlands patients could not be supported 4 additional non West Midlands patients were supported PICU demand overall: Referrals are higher than previous month. 22 patients could not be supported within the local network and had to be taken out of region, due to the exceptionally high demand for beds. Year on Year Comparison of Total Referrals to KIDS 300 There were 128 referrals to KIDS in June 2014. 22% of referrals were avoided , 37% were admitted to BCH, 24% were referred to other WM hospitals and 17% went out of the region. 200 100 Referrals to KIDS Service Taken Out of Region 0 (Leics or Other Non WM Provider) Apr May Jun Jul Aug 2012/13 Sep Oct 2013/14 Nov Dec Jan 2014/15 Outcome of Referrals to KIDS - Trend Feb Mar 30 25 20 70% 15 60% 10 50% 5 40% 0 Total Avge Jun-14 Apr-14 Feb-14 Dec-13 Oct-13 BCH Out of Region The red line shows that BCH took fewer referrals in the first part of Winter 2013, but is now able to return to a more normal level, albeit with a relatively low level in June 14. With avoided admissions also low in June 14, out of Region admissions ended up being the highest in recent months Aug-13 Avoided Admission UHNS and Other WM Jun-13 0% Apr-13 10% Feb-13 20% Dec-12 Oct-12 30% For the winter periods patients are more likely to be taken out of Region. However in recent months due to high demand for beds, more patients have been taken out of region. 12 Operational Performance Report Month 3 2014/15 Performance for June 2014 Utilisation of our facilities 13 Cancelled operations trends Cancelled operations overall position: the number of cancelled operations flagged as nationally reportable in June 2014 is 54 and is above average. Total hospital cancellations at 261 are high compared to previous month (169) and we remain above our strategic goal of a reduction on 12/13 levels. There were seven breaches of the 28 day standard in June. There were 54 nationally reportable* cancelled operations in June 14, which is above the average. * Cancelled by hospital for non medical reasons on the day of admission or after admission Nationally Reportable Cancellations by Reason Total Hospital Cancelled Operations at 261 are well above the upper confidence interval in June 14. Total ICU/HDU beds unavailable 11 Bed shortage 30 Emergency/Trauma 7 Staff unavailable 1 Lack of theatre time 5 Total 54 There were 7 breaches of the 28 day standard in June 2014. 3 T&O, 2 Surgery, 1 Cardiac Surgery and 1 Plastics. Reasons are the same as last month - bed shortages, accommodating more urgent patients and general high levels of demand. 14 All Hospital cancelled operations year to date by specialty All Hospital cancelled operations year to date by reason The hospital has cancelled 607 operations so far in 2014/15. The Surgical Directorate have the most cancellations (393 – 65%) with Paediatric Surgery and Plastics being the largest single specialties. The biggest reason for the cancellations is due to bed shortages. This month 65 cancellations were due to bed shortages. 15 Multiple cancellations In June 2014 33 patients had an operation cancelled who had previously had an operation cancelled at least once in the same specialty in the previous 12 months. These 33 patients had 80 cancellations between them in total in the previous 12 months in the relevant specialty. Strategic objective: Year to date hospital cancelled operations are running 351% higher than the equivalent year to date figure for 2013/14. (Target 10% reduction) Classification changes account for this in part. Strategic Objective – patients cancelled more than twice (Hospital Cancellations Only) Eight patients had an operation cancelled in June 2014 for the third or more time (NB cancellations have to be in the same specialty and in the previous 12 months to be counted) Strategic objective: In June 2015, 10 operations were cancelled due to admin error, and 7 due to equipment failure or unavailability (Target is zero) 16 Fit For Discharge Days Long Stay Patients CAMHS - Long Stay Patients at end of June - Fit for Discharge Days Figure 1 illustrates the trend in various cohorts of long stay patients. There is an increasing number of these patients in the hospital, as can be seen by the trend lines illustrating the numbers over 7, 30 and 90 days at any particular point in time. As we have more of these patients and they stay for longer, there is an impact on the number of beds available to manage the hospital’s elective flow for example. Patient 7 Patient 6 Patient 5 Patient 4 Patient 3 Patient 2 Patient 1 0 100 200 300 400 500 The area with a particular increase is Paediatrics emergency patients Before fit for discharge Trend in Long Stay Patients After fit for discharge 7 CAMHS patients were fit for discharge at end of June. 2 were waiting for adult placements and funding to be available, 4 were waiting placements and one was waiting for agreement of funding. In total these seven cases have been fit for discharge for 817 days. 140 120 Long Stay patients at end of June - days fit for discharge 100 80 Patient 3 60 Patient 1 0 100 200 300 400 500 600 40 Before fit for discharge 20 04/07/2013 17/07/2013 30/07/2013 12/08/2013 25/08/2013 07/09/2013 20/09/2013 03/10/2013 16/10/2013 29/10/2013 11/11/2013 24/11/2013 07/12/2013 20/12/2013 02/01/2014 15/01/2014 28/01/2014 10/02/2014 23/02/2014 08/03/2014 21/03/2014 03/04/2014 16/04/2014 29/04/2014 12/05/2014 25/05/2014 07/06/2014 20/06/2014 0 Sum of GT7 Sum of GT30 Sum of GT90 After fit for discharge 4 patients were waiting for discharge at end of June, the lowest number for some months. Three patients were waiting for a care package (with one of these also waiting for housing and one having social issues). The fourth patient is waiting for housing (which won’t be available until September 2014). In total these 4 patients have been fit for discharge for 916 days. Assuming an average length of stay (excluding day cases) of 4 days, another 229 patients could have been seen at the hospital if these patients had been discharged, as they became fit . 17 Board of Directors Public Meeting Thursday 31 July 2014 Enc 04 Strategic Objective/ Enabler Every child and young person requiring access to care at BCH will be admitted in a timely way, with no unnecessary waiting along their pathway Report Title Resources report period 1st April 2014 – 30th June 2014 Sponsoring Director Chief Finance Officer Author(s) Director of Finance and Procurement, Chief Officer for Workforce, Head of Informatics Previously considered by Finance and Resource Committee Situation This report is to communicate the various aspects of Trust performance in the financial year to date, period ending 30 June 2014, and to identify any key risks that are evident within the organisation. The contents of this report will form the basis of the Trust’s Quarter 1 (Q1) Return to Monitor. The Trust is also required to report its predicted status for Governance and Mandatory Services. Background The Trust is required to comply with the finance related legal issues contained within our Terms of Authorisation as well as other key financial targets. This includes: • • Not breaching the Private Patient Cap (a legal requirement); Performing at plan for Monitor’s Continuity of Service Risk Rating leading to an overall CoSRR of 4; • Minimising triggering the additional financial indicators; and the • Risk Assessment Framework, which may result in formal discussions with Monitor. Delivery against these targets is driven by: • • The volume and mix of demand experienced by the Trust; and How the Trust uses its most valuable resource, its staff, in responding to that demand. The report explores each of these areas in turn and the impact on the financial position and performance. Assessment Monitor Declarations The key ongoing governance issue which impacts upon the Trust’s Monitor Governance rating is the performance against the 18 week target for admitted patients. Performance in month was 90.6% ie just above the 90% threshold. This and the continuing level of performance of the other metrics enable the Trust to forecast a Green Governance rating. From a financial perspective the ratings will be a 4 under the Continuity of Service Risk Rating. Under the old Compliance Framework a FRR of 4 would also have been reported. These remain strong performances. The Trust will soon be undertaking its Q1 and 2014/15 5 Year Plan Conference Call with Monitor and this will help formulate feedback on both these submissions. Activity Activity performance in the year to date against plan and compared to 2013/14 is as follows: Activity Type Against Plan Against 2013/14 Emergency Department +6.9% +6.9% Emergency/Non-Elective -5.3% -11.7% Planned Care +1.1% +2.6% Outpatients +1.8% +2.8% From a financial perspective income has underperformed by a further £0.8m in the month. The level of cancelled operations and the causes of these cancellations as reported in the Performance Report are instrumental in this. Workforce Demand remains high and this has brought into sharp focus the short to medium term capacity issues faced by the Trust. Sickness levels decreased in the month and stood at 3.3%. The cumulative rate remained static at 3.6% meaning both measures remain above the Trust’s 3% target. The combined substantive and bank staff level decreased in June by 16wte. Bank use dropped by 15wte whilst substantive staffing reduced by 1wte. Compared to June 2013 substantive wte have increased by 5% whilst Bank Staff has decreased by 13%. Engaging with staff, especially during periods of pressure, is important and appraisals are one indication of how well this is working in the Trust. The reported appraisal rate has dropped below 77% in the last month and remains short of the 90% target. Finance The end of the first quarter sees the Trust continuing to perform slightly below plan. An in-year surplus of £1.8m sounds strong. However, it falls short of the plan submitted to Monitor, is well below the levels reported in the final 6 months of 2013/14 and we have to be mindful that the plan we set was at the lower-end of expectations. Controlling the costs of care that we provide remains central to our financial success as downward pressure continues on the tariffs we are paid. Our savings levels are below target in June although we have started the year more strongly than in 2013/14. The key areas of shortfall are within trust-wide schemes (contract penalties and drugs) and it is vital that all trust-wide schemes are delivered given that these constitute 50% of the plan this year. We have to secure the level of savings that we anticipate this financial year to ensure affordability of the Next Generation project and having plans exceeding 100% of our target is a positive move to achieving this. A detailed review of CIP performance will be undertaken at the July Performance Board. The key issue financially in Quarter One has been the impact of cancelled operations on clinical income, which is £1.9m under target. This is clearly unsustainable. Our cash balances have once again dropped below plan. The June plan was the highest ever cash balance planned for the Trust and due to a delay in receiving payment for some 2013/14 year-end invoices we have fallen short of this. The Capital Programme was ratified by the Finance and Resource Committee in July. Quarter Two will now see higher levels of expenditure being incurred. Recommendations The Board review, discuss and approve the Resources Report. The Board of Directors is asked to approve a forecast Governance (Green) and Continuity of Service Risk Rating (“4”) for inclusion in the Monitor Q1 Return, which must be submitted by July 31. Key Impacts Strategic Objectives Staff and finance are key enablers to meeting the Trust’s strategic objectives. CQC Registration (state outcome) N/A NHS Constitution NHS Constitution has a pledge regarding 18-week waits. Other Compliance (e.g. NHSLA, Information Governance, Monitor) Monitor metrics are considered in the report. Equality, diversity & human rights N/A Trust contracts N/A Other N/A Resources Report July 2014 Phil Foster Theresa Nelson Paul Franklin Director of Finance and Procurement Chief Officer for Workforce Head of Informatics 1 Reporting on resources use 1. Summary 2. Monitor Assessments and Declarations 3. Volume and mix of activity 4. The impact on our workforce 5. Financial Performance Summary 2 Summary. June 2014 The end of the first quarter sees the Trust continuing to perform slightly below plan. The year to date surplus of £1.8m is a strong position but it does fall short of the plan submitted to Monitor and is also below the run rate reported in the second half of 2013/14. Achievement of the Trust’s planned £4.4m surplus is expected. However, the plan was widely accepted as being a downside case which makes the continued underperformance a worrying scenario. The operational difficulties at the Trust with regards to PICU and acute bed capacity, with increasing numbers of long stay patients, are leading to high levels of total cancelled operations. This is having a direct impact on clinical income, which is 3.4% below plan. Should this continue it will become financially unsustainable for the Trust. Controlling the costs of care that we provide remains central to our financial success as downward pressure continues on the tariffs we are paid. Our savings levels are below target in June although we have started the year more strongly than in 2013/14. It is crucial that the trust-wide schemes are delivered but these too are being impacted by the operational difficulties being experienced. We have to secure the level of savings that we anticipate this financial year to ensure affordability of the Next Generation project and having plans exceeding 100% of our target is a positive move to achieving this. Bank usage in June was 13% lower than the equivalent period last year although substantive staffing levels are 4.8% higher. Appraisal rates have reduced further and are now under 78%. In-month sickness reduced by 0.45% to 3.33%. This is its lowest level since September 2013. Year to date sickness has remained static at 3.56%. Our cash balances although remaining strong have dropped below plan. Cash received during June has not included significant year-end contracting debts, the largest of which is £1.25m with NHS England. The Capital Programme has been formally ratified by the Finance and Resource Committee with prioritised schemes now identified. 3 2. Monitor Assessments and Declarations 4 Our month 2 regulatory position remains strong. Quarter 4 - 2013/14 The predicted ratings for Quarter 4 reported to the Board in April 2014 have now been confirmed by Monitor. Monitor Quarter 4 2013/14 (Confirmed) Finance risk rating - Continuity of Service Risk Rating Governance risk rating Finance risk rating - Compliance Framework Plan Actual G (4) G (4) G G G(4) G(4) Month 3 Monitor Quarter 1 2014/15 (Predicted) Based on this performance the predicted measureable Month 3 performance is Green. The Continuity of Service Risk Rating for June is a 4 (the highest level). Finance risk rating - Continuity of Service Risk Rating Governance risk rating Finance risk rating - Compliance Framework Plan Actual G (4) G (4) G G G(4) G(4) For information under the old Compliance Framework regime a FRR of 4 would have been reported in Month 3. The above will result in the Trust achieving its planned Risk Ratings for 2014/15. 5 3. Volume and Mix of Activity 6 Emergency activity profile ED attendances Emergency Department (ED) attendances are slightly lower than the previous month but have increased by 6.9% YTD compared with last year. There was a 7.9% increase on the June 2013 figure. Activity is also 6.9% above plan in 14/15 so far. 6000 5000 4000 3000 2000 1000 0 A M J 2011/12 J A S 2012/13 O N D J F M 2013/14 2014/15 2014/15 Emergency department activity against plan 5000 4500 4000 3500 3000 2500 2000 1500 1000 500 0 J J A S 2014/15 actual O N D J F M 2014/15 plan 2000 1500 1000 500 0 A M Despite the additional ED demand, emergency FCE activity in month has decreased by 5.0% compared with June 2013 and shows a decrease of 11.7% in YTD figures compared to the same period last year. Emergency FCE activity is 5.3% behind plan YTD, with June activity levels being 6.8% lower than planned. A M Emergency /Non Elective FCEs The main reason for this change is the large reduction in the number of zero day length of stay patients being admitted from the ED Department and assigned to the A&E specialty as an admission – these are 20% down on plan. ENT, Trauma and Oncology show 10% + increases versus plan. J 2011/12 J A S O N 2012/13 D J F M 2013/14 2014/15 2014/15 Emergency/non elective FCEs activity against plan 1800 1600 1400 1200 1000 800 600 400 200 0 A M J J A 2014/15 actual S O N D J F M 2014/15 plan 7 Planned activity profile All elective FCEs 2014/15 All Elective FCE activity against plan (incl Reg Day Admissions) 3000 3000 2500 2500 2000 2000 1500 1500 1000 1000 500 500 0 0 A M J 2011/12 J A 2012/13 S O N 2013/14 D J F 2014/15 M A M J J A 2014/15 actual S O N D J F M 2014/15 plan Elective activity in June was 2.6% higher than in June 2013 and YTD activity also shows a 2.6% increase over 2013/14. Elective activity is now 1.1% above plan YTD, however activity was 1.7% below plan in June 2014. Although the overall variation against plan is quite small at this stage of the higher volume specialties Paediatric Surgery is showing an 11% increase, and Medical Oncology a 17% increase 8 Outpatient activity profile New OP attendance Outpatient Procedures 4000 3500 3000 2500 2000 1500 1000 500 0 June 2014 saw a 5.2% increase for new attendances and 5.0% increase for follow up patients when compared with June 2013. YTD activity shows that new attendances have decreased by 1.0% and follow ups YTD have increased by 4.2% when compared to 2013/14. A M J J 2011/12 A S 2012/13 O N D J 2013/14 F M 2014/15 Follow up OP attendance 10000 9000 8000 7000 6000 5000 4000 3000 2000 1000 0 Outpatient procedures performed in June are 46.7% higher than for June 13 and 38.1% higher than for same period in 2013/14. There has been in increase in the level of diagnostic coding in outpatients which may be impacting here. Against plan, all outpatient activity was 0.7% below plan in June 2014 and overall 1.8% ahead of plan YTD. A M 2011/12 J J A 2012/13 S O N 2013/14 D J F M 2014/15 For new attendances against plan the largest areas of growth are Orthopaedics (10%), and Cardiology (26%). For follow ups the biggest areas of growth are Paediatric Surgery (28%) and Oncology (23%). For procedures Cardiology and ENT are both over plan significantly for both activity and income. 1200 1000 800 600 400 200 0 A M 2011/12 J J A 2012/13 S O N D 2013/14 J F M 2014/15 2014/15 outpatient activity against plan (excl AHP CNS and Phone) 16000 14000 12000 10000 8000 6000 4000 2000 0 excludes AHP, CNS and phone attendances Activity A M J J A S O N D J F M 2014/15 actual 2014/15 plan 9 4. Workforce 10 Workforce Report Summary June 2014 Sickness Summary – In month sickness has decreased to 3.33%, which is higher than this time last year. Long term sickness (%) has decreased slightly to 2.21%, these staff are being supported through our processes. Short term sickness has decreased slightly to 1.09% during May 2014. The top 3 reasons for sickness during May are Anxiety/Stress (760.58 WTE days lost), Musculoskeletal (656.55 WTE days lost) and Gastrointestinal (282.85 WTE days lost). There is some evidence to suggest that gastrointestinal absences are linked to stress related absences (e.g. IBS exacerbated by stress). The majority of stress sickness absence episodes are due to personal circumstances, for example bereavements, change in family circumstances, financial pressures and carer responsibilities. However where work related factors are identified, these are addressed by way of individual stress risk assessments, OH referrals, signposting to the Trust’s support mechanisms and regular 1:1s with managers as appropriate. Bank/Agency Usage – There has been a slight decrease of 14.82WTE during June 2014 to 160.91 WTE, compared to May. Admin usage has decreased slightly by 0.36 WTE, however it continues to be high in the Medical Secretary profession (17.22 WTE) and also in Health Records (12.61 WTE). Top 3 Clinical departments using bank are: • PICU (20.75 WTE) to cover vacancies and maternity leave. Advertised vacancies June 14 (30.4WTE). 6 WTE awaiting clearances • Theatres (12.86 WTE) to cover vacancies. No jobs advertised in June. 1WTE awaiting clearance. • PAU (6.98 WTE) – Increased usage due to sickness, covering maternity and specialist skills required. PDR Summary - PDR % remains below 80%. This has been highlighted as a priority and Directorates are identifying hotspot areas, sending out email reminders to managers and supplying their DMT’s with monthly figures. Turnover Summary -12 month Turnover % for the Trust has decreased for the 12 month period ending June 2014 but remains above the Trust KPI (9%) at 10.89%. All Directorates with the exception of Surgery have a 12 month turnover % above the Trust 9% KPI target. 11 Workforce Dashboard Trust Target CSS Medical Specialised Surgical CAMHS Corporate Trust (Previous Month) Trust (Current Month) <3.00% 3.58% 4.65% 3.63% 3.02% 2.98% 2.84% 3.56% 3.56% ▬ <3.00% 3.47% 4.48% 2.36% 3.21% 3.48% 3.00% 3.78% 3.33% ▼ 85 111 88 70 38 59 449 451 ▲ LT Sickness % 2.23% 3.16% 1.45% 2.02% 1.94% 2.42% 2.39% 2.21% ▼ ST Sickness % 1.24% 1.33% 0.92% 1.19% 1.54% 0.58% 1.39% 1.09% ▼ £44,909.07 £75,483.39 £38,451.87 £29,108.14 £27,917.18 £31,479.14 £275,233.77 £247,348.79 £102,453.57 £154,056.12 £86,667.23 £58,839.97 £51,196.88 £69,368.79 £275,233.77 £522,582.56 546.29 901.37 558.82 439.66 312.07 502.40 3580.90 3260.61 ▼ 81.25% 84.11% 80.04% 79.57% 68.40% 66.43% 78.75% 77.44% ▼ Starters FTE 4.00 5.40 7.00 4.80 1.40 9.49 44.83 32.09 ▼ Leavers FTE 3.40 6.20 12.60 0.80 3.00 4.67 35.85 30.67 ▼ 9.20% 10.63% 12.31% 8.42% 12.45% 12.07% 11.10% 10.89% ▼ ▬ Indicator Sickness % (YTD) Sickness % (Month) Episodes Cost of sickness Cost of sickness YTD FTE days lost sickness PDR's % Rolling Turnover % 90% <9% Trend In Month Turnover % Headcount WTE in post 0.71% 0.90% 0.96% 0.21% 0.81% 0.36% 0.69% 0.69% 579 511.28 715 652.26 830 761.97 469 431.95 316 283.87 575 532.46 3483 3174.96 3484 3173.79 Active Recruitment 3 18 12 11 12 21 58 77 ▲ 5.73 38.33 40.35 23.53 9.10 43.87 175.73 160.91 ▼ 3.63% 4.68% 3.64% 4.42% 4.25% 1.77% 3.57% 3.70% ▲ 5 17 14 9 5 4 61 54 ▼ 2 n/a Bank Usage Maternity Leave % Staff in Difficulty Org Change Please note that sickness is still one month behind so we are currently reporting on Mays data Current months WTE may be slightly lower due to new starters from the 2nd induction still being inputted onto ESR. Employee Relations - On going or started during reporting month Consultant Appraisals % is now a rolling 12 month figure Turnover % is based on permanent staff leavers only 0 0 1 0 0 1 2 12 Sickness Absence BCH Monthly Sickness % Long and Short Term Sickness % 4.00% 3.50% 3.00% 100% 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 2.50% 2.00% 13/14 1.50% 14/15 1.00% Trust Target 0.50% 0.00% 2.21% 2.23% 1.09% 1.24% 3.16% 1.45% 2.02% 1.94% 1.19% 1.54% 2.42% Long Term Sickness BCH Trust Sickness 1.33% 0.92% 284 Dir 1 284 Dir 2 284 Dir 3 284 Dir 4 284 Dir 5 Clinical Medical Specialised Surgical CAMHS Support Directorate Services Directorate Services Services Short Term Sickness 0.58% 284 Dir 6 Corporate BCH Sickness Comparison 13/14 April May June 2.85% 3.13% 3.78% 3.33% July 3.39% August 3.58% 3.22% September October November December January February March 3.36% 3.74% 3.65% 3.43% 3.73% 3.76% 3.77% 14/15 BCH Sickness Absence - May 2014 BCH Total Clinical Support Services Medical Directorate Specialised Services Surgical Directorate CAMHS Services Corporate Number of Episodes Monthly Sickness % Cumulative 12 Month Sickness % 451 3.33% 3.56% 85 3.47% 3.58% 111 4.48% 4.55% 88 2.36% 3.63% 70 3.21% 3.02% 38 3.48% 2.98% 59 3.00% 2.84% With the exception of CAMHS all other Directorates have seen a decrease in their sickness % between April and May which has helped the Trust sickness % decrease from 3.78% to 3.33% The Medical Directorate continues to have LTS cases, 4 due to employee relations cases and the remaining due to MSK and long term health conditions. Sickness Management interventions continue to be managed tightly. • Sickness continues to be high on Ward 2, Complex Care and Haem/Onc . • Review meetings with all dept/ward managers scheduled for July and each quarter thereafter. . PICU has seen a reduction in their sickness absence figures. In March 2014, the absence was 4.7%, April 14 was 3.2% and May 14 has reduced further to 2.8% (Trust target is 3%). In February 2014, there were 11 long term sick cases which has reduced to 3 in May 2014. CAMHS – There has been an increase in sickness from 2.77% in April to 3.52% in May. This is due to an increase in LTS cases due to work related injury and employee relations cases. 13 Sickness Absence/Stress Audits A management of stress audit process has been developed in order to assess compliance with the requirements set out in the management of stress policy and reduce stress related sickness. There were 10 hotspot areas identified based on workforce KPI areas and have piloted a sickness absence/stress audit. PICU was identified as the pilot area by triangulating high sickness absence, high numbers of staff reporting stress, PDR rates and number of leavers etc. This data has been reviewed at SWC and will continue to be monitored through this group Stress Risk Assessments (SRA) (staff members off sick with stress related issues – Jan to May 14) Compliant – Manager completed a stress risk assessment within required timeframe Non Compliant - Manager didn't complete a stress risk assessment or within the required timeframe Total Stress Risk Assessments requested This Audit did not include the 19 staff members with less than 5 days off work with Stress Total number of staff off sick with stress Stress Risk Assessments (staff members who are have not taken time off sick with stress related issues) Number of SRA completed for staff who have said they are stressed but have not gone off sick Figures 52 40 92 19 111 Figures 30 •68 of the 92 cases audited were due to work-related stress. • 27 of the 52 individual stress risk assessments also had completed action plans to manage/minimise stress which is an improvement on the previous audit Jan – Dec 2013. •There were 30 stress risk assessments completed for staff who said they are stressed but who have not gone off sick. This figure indicates that managers are now identifying staff members stress at an early stage, which means that proactive signposting or support interventions can be put in place. Case Study: PICU There has been significant engagement from the PICU Senior team for the audit and the majority of the actions identified are now in place. The department has already begun to see a reduction in their sickness absence figures. In March 2014, the absence was 4.7%, April 14 was 3.2% and May 14 has reduced further to 2.8% (Trust target is 3%). In February 2014, there were 11 long term sick cases which has reduced to 3 in May 2014. Actions to improve management of stress •Currently reviewing the Management of Stress Policy •Feedback results of the audit to Directorates •Improve the information available on the management of stress via the Intranet. •Include an additional section within ESR training which explains the importance of, and how to record stress. •Promote the importance of undertaking individual stress risk assessments. •For the next audit undertake a review of persistent non-compliance with the Management of Stress Policy and target/support those areas. •Use local survey data to help determine where issues may exist •Use national survey to identify hotspot areas and targeted support •Development of e-resilience training and also training for managers •Listening sessions to help understand specific group issues •Commissioned the Big White Wall as additional staff support •Re tendered for staff psychological support contract for improved provision •Developing clinical supervision and professional support frameworks 14 Bank/Agency Usage Feb 14 Mar 14 Apr 14 May 14 June 14 CSS 8.29 8.20 8.88 4.66 6.01 5.73 Medical 41.03 39.80 57.04 39.14 42.61 38.33 Specialised 47.33 48.30 57.12 44.95 47.57 40.35 Surgical 17.62 19.60 27.99 26.57 26.80 23.53 CAMHS 9.27 7.80 9.01 9.07 8.65 9.10 Corporate 40.46 35.54 43.91 46.05 44.09 43.87 Total 163.99 159.24 204.00 170.44 175.73 160.91 * The latest month is an indicative figure and about 95% accurate. The previous month figure will be updated each month Trust Bank/Agency Usage (WTE) Yearly Comparison 250 200 WTE Jan 14 150 100 50 0 Top 3 reasons for Bank/Agency usage 1. Vacancy – 115.68 WTE 2. Sickness – 17.39 WTE 3. Specialist Skills Required – 10.22 WTE 2013/14 2014/15 Admin bank and agency usage = 76.61 WTE. This is a decrease of 0.36 WTE (May ’s usage was 76.97 WTE). Bank/Agency Usage - June 14 Top 3 reasons for Admin usage are Vacancy, Backlog and Sickness. Directorate Admin bank and agency is as follows: Priority 7 13.01 CSS - 2.90 WTE - Labs, Radiology and Surgical Day Care Medical - 8.88 WTE - Primarily Medical Secretary Areas (6.01WTE) 47.67 Specialised - 4.46 WTE – Cardiac Service, PICU and Theatres 39.32 Surgical - 18.63 WTE - Primarily Medical Secretary Areas (11.21 WTE) CAMHS – 4.49 WTE - Primarily East Locality (3.72 WTE) A&C Reg Non Reg Corporate – 38.28 WTE – Primarily in Health Records (12.61 WTE) 15 BCH Nursing Staffing: • • • • NHS choices reported 1st submission with 100% score for BCH A new separate web section on our Web page for Safer Staffing reports: http://www.bch.nhs.uk/story/safe-staffing First Month of Patient/Staffing acuity data collected Revised methodology for calculating trust-wide total used. Nursing Workforce Summary Monthly Ave: Annual Mat Leave Sickness Leave Bank 6.0% 12.4% 5.8% 4.6% 2.3% 81.1% 4.5% 15.2% 5.9% 3.5% 4.0% 79.9% 2.9% 14.15 6.55 3.0% 6.4% Act vs. Plan Acuity Apr-14* 95.9% TBC 81.5% May-14** 99.7% TBC Jun-14** 98.2% 92.4% *April data collected prior to DH guidance ** May & June data presented using new agreed format Skill Mix Vacancy Nursing Workforce Jun 2014 Nursing Workforce Dashboard: Ward Patient/Staffing Acuity Level Nursing Staffing Actual vs Planned Registered Care Staff Registered Care Staff Day Day Night Night Actual vs Planned % Actual vs Planned % Actual vs Planned % Actual vs Planned % Ward 11 120.6% 96.0% 96.8% 98.1% 97.8% 92.4% 93.5% 91.9% 95.4% 92.4% 102.7% 90.0% 115.3% 97.9% 88.9% 100.1% 106.1% 99.1% 135.2% 91.7% 107.7% 85.2% 108.4% N/A 89.8% 177.4% 90.8% 105.4% 98.3% 92.9% 101.7% 93.4% 102.2% 130.3% 100.9% 100.0% 98.0% 97.5% 100.0% 95.3% 116.7% 93.7% N/A 97.5% 90.2% 156.6% 110.6% N/A 143.3% 93.3% 100.0% 96.7% 93.3% N/A 126.7% N/A 125.0% N/A 100.0% 100.0% Ward 12 101.1% 93.5% 94.2% N/A 98.5% PICU MDC* 92.0% 122.1% 95.6% 85.6% 92.4% N/A 121.6% N/A 92.8% 116.1% SDC* 120.6% 187.9% N/A N/A 132.2% Ashfield 107.7% 92.1% 125.9% 91.5% 98.0% 112.9% 118.2% 90.2% 103.5% 95.6% 104.7% 98.4% May-14 Burns Neonatal Surgical Ward 1 Ward 5 Ward 9 Ward 10 ED PAU MHDU Ward 2 Ward 7 Ward 15 ODC* Ward 8 Heathlands Irwin Overall trust Average: National Submission reported Average 96.17% 95.59% * Excluded from National Upload 102.83% 102.59% 97.54% 97.54% 114.29% 114.29% Unplanned: Actual & Response Planned Resources Total Registerd Unfilled Vacancy Mat Leave Skill Leave% Roster% WTE % Mix% No of Green shifts No of Amber shifts No of Red shifts 3 1 2 9 7 4 9 5 9 22 0 13 TBC 5 4 9 11 0 2 TBC TBC TBC 0 0 0 0 0 0 0 0 0 0 0 1 TBC 0 0 0 3 0 0 TBC TBC TBC 77 83 82.7 71 81.4 80.3 81.6 80.7 85.3 82 100 88 64.6 88.5 86.5 9.6 4 3.5 8.2 10.1 3.7 5.4 6.6 9.1 7.6 1.9 18.2 26.5 15.8 4.6 0.8 -0.91 0.8 -0.2 -2 -0.3 8.7 -2 0.4 -2.4 -3 6.1 2.58 4.2 -0.3 12.7 11.9 9.2 12.5 14.4 18.1 15.3 12.8 15.7 12.7 19.2 16.6 10.3 9.8 17.2 88.6 89.2 88.8 8.2 21.1 32.9 1.2 22.41 -0.3 105.4% 95.3% 111.7% 87 89 88 81 83 86 81 85 81 68 90 76 TBC 85 86 81 76 60 58 TBC TBC TBC 72.7 73.8 53.7 58 40.1 19.8 19.2 15.7 98.2% 1441 115 4 79.9 13.3 Actual vs Planned % 112.2% 97.7% 99.2% 115.5% 97.7% 97.2% 94.1% 95.5% 97.5% 95.5% 130.1% 91.8% 112.0% 97.9% 90.0% 98.0% No of Times Raised to HoN Sickness Bank Fill % Bank Used 3.8 6.7 10.6 4.2 7.8 10.1 7.3 10 12.5 6.7 0 7 11.7 13.4 0 1.4 6.7 0.3 2.2 2.8 3 3.6 2.3 5.9 0.7 0.7 2.3 1.3 4.1 3.4 26.1 88.6 57.9 35.5 57.1 64.7 71.3 39.7 62.2 54.8 0.25 27.1 82.4 60 51.4 2.6% 3.8% 2.2% 3.8% 5.2% 2.6% 9.3% 5.7% 20.2% 22.4% 1.6% 4.5% 6.7% 5.9% 2.2% 9.7 15.5 19.1 1.8 4.9 5.1 8 1.9 4.6 49.1 43 100 4.8% 11.8% 1.9% TBC TBC TBC TBC TBC TBC TBC TBC TBC TBC TBC TBC TBC TBC TBC TBC TBC TBC -5.7 -0.6 -5.2 1.1 10.3 21.2 10.5 14.6 7.2 6 0 7 6 0.4 2.7 1.7 76.9 74.6 40 82.9 7.4% 8.9% 0.4% 7.7% TBC TBC TBC TBC 1.2 14.1 6.5 3 56.6 6.4% Nursing, Midwifery and Care Staff Staffing June 2014 Submission to NHS England Hospital Site Details Main 2 Specialties on each ward Registered midwives/nurses Care Staff Registered midwives/nurses Care Staff Ward name Site code *The Site code is automatically populated when a Site name is selected RQ301 RQ301 RQ301 RQ301 RQ301 RQ301 RQ301 RQ301 RQ301 RQ301 RQ301 RQ301 RQ301 RQ301 RQ301 RQ301 Hospital Site name BIRMINGHAM CHILDREN'S HOSPITAL BIRMINGHAM CHILDREN'S HOSPITAL BIRMINGHAM CHILDREN'S HOSPITAL BIRMINGHAM CHILDREN'S HOSPITAL BIRMINGHAM CHILDREN'S HOSPITAL BIRMINGHAM CHILDREN'S HOSPITAL BIRMINGHAM CHILDREN'S HOSPITAL BIRMINGHAM CHILDREN'S HOSPITAL BIRMINGHAM CHILDREN'S HOSPITAL BIRMINGHAM CHILDREN'S HOSPITAL BIRMINGHAM CHILDREN'S HOSPITAL BIRMINGHAM CHILDREN'S HOSPITAL BIRMINGHAM CHILDREN'S HOSPITAL BIRMINGHAM CHILDREN'S HOSPITAL BIRMINGHAM CHILDREN'S HOSPITAL BIRMINGHAM CHILDREN'S HOSPITAL Specialty 1 171 - PAEDIATRIC SURGERY 171 - PAEDIATRIC Neonatal Surgical SURGERY 171 - PAEDIATRIC Ward 1 SURGERY 171 - PAEDIATRIC Ward 5 SURGERY 171 - PAEDIATRIC Ward 9 SURGERY 171 - PAEDIATRIC Ward 10 SURGERY Burns ED 420 - PAEDIATRICS PAU 420 - PAEDIATRICS MHDU 420 - PAEDIATRICS Ward 2 420 - PAEDIATRICS Ward 7 420 - PAEDIATRICS Ward 15 420 - PAEDIATRICS Ward 8 420 - PAEDIATRICS Ward 11 Ward 12 PICU RQ301 BIRMINGHAM CHILDREN'S HOSPITAL Ashfield RQ301 BIRMINGHAM CHILDREN'S HOSPITAL Heathlands RQ301 BIRMINGHAM CHILDREN'S HOSPITAL Irwin 321 - PAEDIATRIC CARDIOLOGY 321 - PAEDIATRIC CARDIOLOGY 420 - PAEDIATRICS 711- CHILD and ADOLESCENT PSYCHIATRY 711- CHILD and ADOLESCENT PSYCHIATRY 711- CHILD and ADOLESCENT PSYCHIATRY Specialty 2 160 - PLASTIC SURGERY 171 - PAEDIATRIC SURGERY 361 - NEPHROLOGY 100 - GENERAL SURGERY 100 - GENERAL SURGERY 150 - NEUROSURGERY 180 - ACCIDENT & EMERGENCY 300 - GENERAL MEDICINE 300 - GENERAL MEDICINE 300 - GENERAL MEDICINE 192 - CRITICAL CARE MEDICINE 303 - CLINICAL HAEMATOLOGY 171 - PAEDIATRIC SURGERY 170 - CARDIOTHORACIC SURGERY 170 - CARDIOTHORACIC SURGERY 192 - CRITICAL CARE MEDICINE 711- CHILD and ADOLESCENT PSYCHIATRY 711- CHILD and ADOLESCENT PSYCHIATRY 711- CHILD and ADOLESCENT PSYCHIATRY Total monthly planned staff hours Total monthly actual staff hours Total monthly planned staff hours Total monthly actual staff hours Total monthly planned staff hours Total monthly actual staff hours Total monthly planned staff hours Total monthly actual staff hours Average fill rate Average fill rate registered registered Average fill rate Average fill rate care staff (%) care staff (%) nurses/midwives nurses/midwives (%) (%) 1170 1414 1950 1872 1170 1132 1924 1888 2022 1977 1833 1701 2730 2553 1950 1792 1170 1116 2145 1982 1365 1402 3673 3307 1898 1859 2360 2127 2022 2039 12285 11300 410 376 273 637 501 442 890 390 0 582 397 722 299 390 390 585 410 891 410 1463 271 990 861 990 459 1320 476 1221 810 2228 370 1320 0 990 526 1650 704 990 655 2915 294 1320 363 1683 365 1320 560 10153 906 1366 1012 1290 1343 1221 2184 1298 990 1573 1155 2731 1265 1518 1243 9381 99 517 0 231 330 286 330 330 0 330 0 44 187 132 0 407 155 120.8%100.1%101.7%156.6% 572 96.0% 109.2% 93.4% 110.6% 0 96.8% 99.1% 102.2% #DIV/0! 331 98.1% 135.2%130.3%143.3% 308 97.8% 91.7% 101.7% 93.3% 286 92.8% 107.7%100.0%100.0% 319 93.5% 91.0% 98.0% 96.7% 308 91.9% 94.8% 98.3% 93.3% 0 95.4% #DIV/0! 100.0% #DIV/0! 418 92.4% 90.3% 95.3% 126.7% 319 102.7%177.4%116.7% #DIV/0! 55 90.0% 90.8% 93.7% 125.0% 187 97.9% 98.3% 95.8% 100.0% 132 90.1% 92.9% 90.2% 100.0% 22 100.9% 93.5% 94.2% #DIV/0! 495 92.0% 95.6% 92.4% 121.6% 1348 1429 819 749 935 1106 385 368 1006 916 923 894 792 721 528 534 897 1130 806 910 847 877 517 509 106.0% 91.5% 118.2% 95.6% 91.0% 96.8% 91.0% 101.2% 125.9%112.9%103.5% 98.4% PDR - AFC Staff Staff Group - Table 1 Jan-14 Feb-14 Mar-14 Apr-14 May-14 Jun-14 Add Prof Scientific & Technical 86.43% 83.50% 87.25% 87.11% 84.10% 79.59% 88.89% 89.49% 87.54% 85.67% 77.42% 80.46% Admin & Clerical 77.96% 77.22% 77.38% 77.36% 74.18% 72.21% AHP's 87.76% 87.96% 89.09% 87.39% 78.76% 77.31% Estates & Anciliary 89.92% 90.40% 88.19% 85.39% 72.30% 70.00% Specialised Services Healthcare Scientists 83.78% 83.04% 76.00% 75.61% 76.42% 80.49% Surgical Directorate Nursing 87.50% 85.76% 85.47% 82.73% 81.80% 79.61% CAMHS Services Additional Clinical Services Table 1 shows via staff group the Appraisal compliance. Compared to last months report Additional Clinical Services and Healthcare Scientists are the only staff groups to see an increase in their PDR rate. Corporate PDR % (Hot spot areas) The below departments are showing red on the workforce dashboard and have a PDR rate less than 75% Bereavement Services – 33.3% Chaplaincy – 50% Child Protection – 33.3% Clinical Coding – 42.86% Contracting – 50% Corporate Nursing – 55.86% Domestics – 50% Executive Team (Including Exec Assistants) – 25% ICT Projects – 50% Facilities – 60% Finance – 54.55% Governance – 66.67% Human Resources – 61.11% Operations Management – 33.3% Porters – 66.67% Procurement – 25% Research & Development – 50% Trust Bank Management – 30% Table 2 BCH Clinical Support Services Medical Directorate Corporate Jan Feb Mar Apr May June 85.23% 84.68% 83.66% 82.22% 78.75% 77.44% 87.23% 88.21% 87.47% 86.68% 80.36% 81.25% 87.34% 88.49% 86.36% 83.55% 82.35% 84.11% 81.79% 81.47% 82.15% 81.87% 80.72% 80.04% 91.09% 87.13% 87.88% 85.91% 83.86% 79.58% 92.86% 90.25% 84.62% 86.40% 80.09% 68.40% 76.80% 76.17% 75.29% 72.15% 66.35% 66.43% This table shows the PDR %. Each months totals is for PDR’s that have taken place and recorded on ESR during the last 12 months, so for June the PDR period is July 13 to June 14. Plans to target PDR % CAMHS The CAMHS SLT will discuss and agree actions to address this issue and this will be monitored on a monthly basis. In addition monthly reports are going to be distributed to managers highlighting those that have expired and are due in next 3 months. An administrator is now covering for a LTS sick case and part of the role is to input PDR’s. Corporate HR will continue to email Corporate HODs and copying in chief officers requesting that appraisals are undertaken and also request a trajectory for them to be 100% compliant. 19 DBS Update One of the pre-employment checks undertaken for new starters is a DBS (Disclosure and Barring Scheme) check. As good practice the Trust re-checks all its staff who’s DBS check has expired after 3 years of employment with the Trust. The last phase of re-checking DBS’s involved 202 members of staff which are 100% complete. The next phase of re-checks is for approximately 2200 employees whose DBS’s are due to expire throughout 2014. This is high as in 2011 there was a significant push on DBS checks. Due to the volume of staff involved re-checking will be phased throughout the remainder of the year but prioritised with the safe guarding team. Directorate HC of staff required to complete BDS check HC completed % Completed CSS 27 27 100% Medical 49 49 100% Specialised 53 52 98.10% Surgical 24 24 100% CAMHS 22 22 100% Corporate 28 28 100% Total 203 202 99.50% 20 Staff in Difficulty Staff in Difficulty Cases (January 14 to June 14) 70 Number of Cases 60 61 53 54 50 40 37 35 38 30 20 10 0 January February The number of cases has decreased since last months report due to cases being ended or employees leaving the Trust, however a large proportion of the staff in difficulty cases are due to conduct issues. Managers are becoming more effective at dealing with inappropriate behaviour and measuring against the Trust values. Managers are identifying and managing staff in difficulty more effectively. This is supported by the HR team through the roll out of the master classes. March April May June Breakdown of Cases June 14 Total 54 cases 26% Disciplinary 42% Grievance Harassment 15% Performance 17% 21 Staff Friends and Family Test Understanding how staff feel about working at BCH has a direct link to measuring quality of care. This is why NHS England have launched Staff Friends and Family Test in April 2014 and all NHS Organisations must implement the test over 3 quarters with a break in Q3 for the national staff survey to be undertaken. The SFFT results will be submitted via UNIFY 2 to NHS England once approval has been given by the Chief Officer for Workforce Development. There are two questions related to the SFFT: • How likely are you to recommend Birmingham Children’s Hospital to friends and family if they needed care or treatment? How likely are you to recommend Birmingham Children’s Hospital to friends and family as a place to work? • Total number of staff responses: 477 approximately 14% of our workforce I would recommend this organisation as a place to work. If a friend or relative needed treatment I would be happy with the standard of care provided by this organisation. Staff Response Staff Response 80% 1% Yearly Comparison 2% 2% 0% 70% 12% 70% 50% 74% 60% 40% 50% 30% 40% 30% 20% 20% 10% 96% 0% Yes Neither likely or unlikely No Don't know 90% 80% 60% 13% Yearly Comparison 100% 2012 2013 10% 0% 2014 2012 2013 2014 ‘Significant improvement in both measures’ 22 Mandatory Training Update Mandatory training compliance is currently 81.82%. This represents a 3.31% increase compared to the average for mandatory training taken at the end of Dec 2013 which is 13.1% below the Trust KPI of 95% . The table below identifies the compliance statistics for all mandatory topics between Jan 2014 and July 2014 (source: Vesper 7/7/14). Notable improvements are in BLS, Blood Sampling, Blood Admin, Child Protection L2, Conflict Resolution, Healthcare Records and Manual Handling Practical. The pressure in the hospital is having and impact of releasing people to attend Mandatory Training. Education and Learning have seen lower engagement in face to face training as reported in June 2014. A review of the last 3 mandatory updates suggests 41% attendance with a 15% DNA rate . Bookings numbers for the next mandatory training date on 25th July are currently at 16% which supports suggestions that the release of staff to face to face training is still challenging for departments. Moodle however has seen a big increase in engagement with activity for mandatory refreshers increasing from 737 completions in May 14 to 1007 in June 14. This rise is partially due to the introduction of CP L2 online learning which has supported the big improvement in CP L2 compliance. As stated in the previous report, Education and Learning are going to pilot the use of “Training Boards” in areas as another option for staff to access training which may help in the challenge of releasing staff to face to face training and provide an alternative update method. Issues and Risks • • • • • Completed Actions: • • • • • Exclusion rules (Bloods and CP completed) Ongoing development of Ed Reporting systems – 21 day Education Reporting response working well. Review training plans and course content with Trainers – M&H currently planning changes using Moodle for Induction and mandatory refresher training. “Email Checker” – developed to correct email anomalies and gaps to ensure reminders reach staff – to be made available (Comms/Ed Reporting to sort) CP L2 – on induction D2 now and SfH online update in place Staff engagement low on face to face training DNA rates result in underutilised training places Exclusions need reviewing for some topics Top 3 staff groups with low compliance – Nursing, Medical and Additional Clinical Services Email reminders – not received by some due to incorrect email address or no email address on ESR Future Plans: • • • • • • Continue exclusion rule amends across all mandatory topics Booking reminder service pilot – work in progress Monthly Directorate reports to be introduced eTechnologist Intern starting Sep 15th Training Boards - pilot scheme to be planned Explore Refresher training to be assessment based avoiding repetition of training where competency can be demonstrated with the assessment 23 5. Financial Performance 24 Financial Performance Summary FINANCIAL PERFORMANCE REPORT Monitor Risk Assessment Framework Criteria Financial Performance Plan Actual Status Direction of Travel Capital Service Capacity 4 4 Liquidity 4 4 k seeks assurance regarding w hether the Trust is a going concern. Issue Plan £'000 Actual £'000 Variance £'000 Income and Expenditure 1,933 1,769 -164 Cash Balance 50,734 48,403 -2,331 Capital Programme 1,568 1,965 397 CIP 1,645 1,345 -300 Status Direction of Travel Incom e and Expenditure (Monitor assesses financial risk on a scale from 1 (high risk) to 4 (no evident concerns) The Trust is reporting a below plan position in Month 3. The key cause of this is a shortfall in clinical Foundation Trust Requirements income. Bed pressures and subsequent cancelled operations are the prime causes of this. Issue Measure Plan Actual Private Patient Cap Not to exceed 49% 0.4% 0.1% Status Direction of Travel Cash Balance At the end of June the cash balance w as 4.6% below plan. Capital Program m e The Trust is performing ahead of plan in Month 3 due to levels of expenditure being incurred on schemes carried forw ard from the previous financial year happening in a shorter timeframe. CIP Performance in June w as 18% below plan. This is a result of 2 trust-w ide schemes. 25 Income and Expenditure against Plan The Trust’s I&E position has deteriorated slightly in June with an overall deficit against plan of £0.16m now being reported. Headlines are: • The Trust is reporting a significant deficit against Clinical Income; • The key issues are the continued financial impact of cancelled operations, long stay patients and the associated causes of these. This has impacted upon the Trust’s elective activity performance most notably within Surgery and Cardiac Surgery; • Pressures are being felt in Directorates due to the impact of the clinical income performance (this is being particularly felt in Specialised Services and Surgery) and the phasing of trust-wide CIP targets; • At this stage of the year the Trust remains confident that the planned surplus of £4.377m will still be achieved. 2013/14 I&E to June 2014 Income from activities Other Income Operating Expenses EBITDA Interest Receivable Depreciation Profit/(Loss) on Asset Disposal Impairment PDC Dividend Interest Paid Net Surplus/(Deficit) Brackets indicate adverse variance Clinical Support Services Medical Directorate Specialised Services Surgical Directorate CAMHs Corporate Total Operational Budgets Bad Debts Donated Assets Operating Leases Teaching & Research Reserves and Provisions Total Other Budgets Total Budgets Annual Revised YTD Plan Plan per Annual Plan per LTFM LTFM £'000 £'000 £'000 217,995 216,904 55,568 19,666 22,218 4,687 -225,841 -227,341 -56,460 11,820 11,782 3,794 243 247 61 -4,624 -4,559 -1,156 0 0 0 0 0 0 -2,762 -2,762 -690 -300 -326 -75 4,377 4,381 1,933 Revised YTD Plan £'000 55,617 5,517 -57,351 3,783 62 -1,140 0 0 -690 -82 1,933 June Income Variance Pay Variance Non-Pay Variance Total Variance 88 10 -57 7 -8 297 337 -76 -135 -138 -413 94 -78 -746 -42 -47 -904 -62 -18 -420 -1,494 0 -30 -172 -1,100 -468 68 -202 -1,903 0 -0 -22 285 3,295 3,558 1,655 -0 -22 285 284 621 0 0 -746 3,295 3,273 1,779 YTD Actual £'000 53,766 6,138 -56,317 3,587 40 -1,157 0 0 -631 -70 1,769 Variance £'000 -1,851 621 1,034 -196 -22 -17 0 0 59 11 -164 May Variance £000 In-month Movement £000 -60 -208 -653 -285 38 -333 -1,502 0 -0 -20 190 2,167 2,337 835 31 36 -447 -183 30 132 -401 0 -0 -2 95 1,129 1,221 820 26 Profitability against Target The EBITDA (Earnings Before Interest, Taxation, Depreciation and Amortisation) Margin remains below target (6.0% compared with 6.3%), although this is an improvement on the gap experienced in Month 2 (6.9% actual compared with 7.4% plan). In monetary terms EBITDA was also below the YTD Monitor Plan, with little inmonth movement. EBITDA Margin 8.0% 7.5% 6.8% 7.0% 6.5% 6.0% Actual 6.0% 5.8% 5.5% Plan for Year 5.0% 4.5% 4.0% Apr May Jun The I&E Surplus Margin also continues below plan (3.0% compared with 3.2%) which is reflecting the EBITDA margin. This too is an improved performance compared with Month 2. With the plan of both metrics due to reduce, on average, through the remainder of the year it is expected that the variance between planned and actual %s will shorten over time. Jul Aug Sep Oct Nov Dec Jan Feb Mar I&E Surplus Margin 5.0% 4.5% 4.0% 3.5% 3.0% 2.5% 2.0% 1.5% 1.0% 0.5% 0.0% 3.9% 2.7% 3.0% Actual Plan for Year Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar 27 CIP This is the third CIP report for the new year. The overall target reflects the following: • Directorate targets; • Trust-wide scheme targets; and • Residual balance of the underlying legacy position from 2013/14. Headlines from Month 3 are as follows: • Overall schemes identified exceed the annual target – this is an improved position compared to 2013/14; • The majority of schemes have been risk assessed within Directorates; • Quality Impact Assessment review process has commenced with a further progress undertaken at 30 June; • Corporate is the area which is furthest from target for overall schemes. The gap has been reduced following work during June although formalised PIDs await completion which is leading to a potential under-reporting of achievement; • The June performance although under plan is potentially a prudent position as work continues on the evidencing of savings in some key areas; • The shortfall on the trust-wide schemes is within Contract Penalties (where pressures are evident for Diagnostics and 18 weeks) and Drugs (where schemes have been developed but await implementation); • Delivery against schemes in the year to date for Clinical Directorates is on target; • Phasing throughout the year remains back-ended; • A more detailed review of CIP performance will be presented at the July Performance Board. Directorate CAMHS Corporate CSS Medicine SSD Surgery Trustwide Totals Annual Target In Year Identified £389,526 £723,251 £666,136 £1,324,237 £1,390,984 £725,583 £4,240,000 £9,459,716 £388,640 £532,571 £634,116 £1,649,825 £1,420,330 £740,282 £4,240,000 £9,605,764 YTD Plan YTD Actual YTD Variance % Plan To Date % Annual Target £47,397 £116,666 £125,156 £389,869 £330,991 £109,208 £525,500 £1,644,787 £47,397 £67,315 £156,705 £355,320 £312,213 £148,318 £257,302 £1,344,571 -£0 -£49,351 £31,549 -£34,549 -£18,778 £39,110 -£268,198 -£300,217 100% 58% 125% 91% 94% 136% 49% 82% 12% 9% 24% 27% 22% 20% 6% 14% 28 Cash and Capital 2014/15 Plan Mar-16 Jan-16 Feb-16 Dec-15 Oct-15 Nov-15 Sep-15 Jul-15 Aug-15 Jun-15 Apr-15 May-15 Mar-15 Jan-15 Feb-15 Dec-14 Oct-14 Actual Nov-14 Sep-14 Jul-14 Aug-14 Jun-14 Apr-14 The Capital performance in June was £0.4m ahead of plan. With the core 2014/15 Capital Programme now agreed at July’s Finance and Resource Committee expenditure will start to increase in line with the plan. The spend to date relates to schemes carried forward from 2013/14. The impact of these at Month 3 is higher than anticipated although over the course of the year this will have a neutral impact upon cashflow. May-14 Although cash is below target the Trust’s Liquidity remains significantly above the Continuity of Service threshold of 4. 2014/15 Cash Position and Rolling Forecast 55,000 50,000 45,000 40,000 35,000 30,000 £k 25,000 20,000 15,000 10,000 5,000 0 Mar-14 Cash is now 4.6% below plan at Month 3. This equates to £2.3m and is primarily a result of increasing debtor balances as some year-end contracting invoices remain outstanding. Rolling Forecast 2014/15 Cumulative Capital Expenditure against Plan and Monitor Margins 16,000 14,000 12,000 10,000 £k 8,000 6,000 4,000 2,000 Apr May 14/15 Actual Jun Jul Aug 14/15 85% Sep Oct 14/15 115% Nov Dec Jan Feb Mar 14/15 Plan - Original 29 Debtors and Creditors Debtors over 90 days have increased in June in both percentage and actual terms. The overall level of debt is such that the top 5 debts reported below account for over 20% of our overall debt. Although major legacy debts have now all been cleared a wide range of other medium-high value debts remain. The single highest-value aged debt, relating to 2013/14 year-end settlements with NHS England was paid in early July with the other debts being actively chased. % Debtors and Creditors over 90 days 30% 25% 20% 15% 10% 5% 0% Apr May Jun Jul Aug Debtors>90 days % The Creditors position over 90 days has improved in the month with the payment of the largest single outstanding creditor. Of the 17% over 90 days still outstanding 7% relates to disputed charges associated with CF Year of Care tariff. This is subject to ongoing negotiations. Top 5 Debts Over 90 Days Old Customer NHS England NHS Sandwell and West Bham CCG Sep Oct Nov Dec Creditors>90 days % 30th June 2014 Age (Days) 107 Value (£k) 1,284 93 285 Health and Social Care Board NHS Bham South and Central CCG 101 Jan Feb Mar Target 31st May 2014 Age (Days) Value (£k) 102 171 106 145 170 University Hospitals Birmingham Private Patient - MK 1063 139 1033 139 Slater & Gordon (UK) LLP 265 136 235 136 NHS Birmingham Cross City CCG 188 57 158 2,013 57 649 30 Financial summary. June 2014 The Monitor Financial Risk rating is 4 per plan, with liquidity remaining strong. This 4 is per the Compliance Framework and the Continuity of Service Risk Rating (CoSRR). The I&E position is below the Monitor plan and the revised plan at £1.769m. The EBITDA and Income Surplus margins are 0.3% and 0.2% below plan, respectively. Clinical Income performance in June was below the Monitor plan and this was the key cause of the shortfall against the I&E plan. CIP at a Directorate level has started the year more strongly than previous years. This will remain the primary focus throughout the year. However, trust-wide schemes have fallen behind schedule resulting in 82% of the YTD plan being achieved as at 30 June. Cash balances are slightly below plan in June. The causes of the shortfall are known and being acted upon. Capital in month 3 performed ahead of plan. The Forecast position for the Trust remains to achieve the planned surplus of £4.377m, excluding any further benefit of donated asset income. 31