Background and Analysis ……………………………………………………………………………………………………………………………1 Program Description ……………………………………………………………………………………………………………………1-2 Contents
advertisement
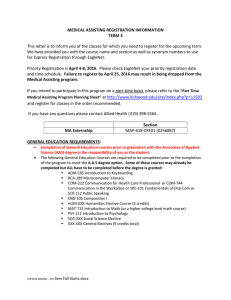
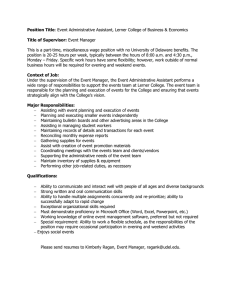
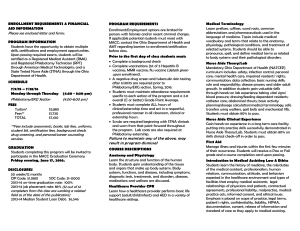
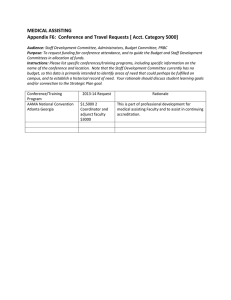
Medical Assisting Instructional Planning Report Spring 2014 Contents Background and Analysis ……………………………………………………………………………………………………………………………1 Program Description ……………………………………………………………………………………………………………………1-2 Relationships ………………………………………………………………………………………………………………………………….2 Accreditation ………………………………………………………………………………………………………………………………….2 College Relationships …………………………………………………………………………………………………………………..2-3 Learning Communities ……………………….. ………………………………………………………………………………………...3 Local/Regional/Statewide Relationships .…..……………………………………………………………………………………3 Community Relationships ……………………………………………………………………………………………………………….4 Cost ………………………………………………………………………………………………………………………………………………………….4-5 Student Learning Outcomes …………………………………………………………………………………………………………………… 5-6 Curriculum Review ………………………………………………………………………………………………………………………………………6 Student Success ……………………………………………………………………………………………………………………………………… 6-7 Results of Student Surveys …………………………………………………………………………………………………………………………..7 Results of Graduate Surveys ………………………………………………………………………………………………………………………..8 Results of Employer Surveys ………………………………………………………………………………………………………………………..8 Analysis of External Data Research …………………………………………………………………………………………………………8-10 Conclusions/New Directions …………………………………………………………………………………………………………………10-12 Program Planning Goals and Recommendations ………………………………………………………………………………… 12-13 List of Appendices ………………………………………………………………………………………………………………………………………13 Medical Assisting Instructional Planning Report Spring 2014 Background and Analysis Program Description Medical Assisting (MA) offers the following degree and certificates: A.S. Degree: Medical Assisting Certificate of Achievement: Medical Assisting Skills Certificates: Phlebotomy Technician Electronic Health Records The Medical Assisting Program is nationally accredited through the Commission on Accreditation of Allied Health Education Programs (CAAHEP) upon the recommendation of the Medical Assisting Education Review Board (MAERB). This accreditation ensures that a student graduating from the Medical Assisting Program can sit for the national exam to become a nationally Certified Medical Assistant. Cabrillo’s Medical Assisting Program is 1 of only 6 California Community Colleges that hold this national accreditation. The phlebotomy program is a state accredited program through the California Department of Health Services, Laboratory Field Services. A student completing this program is eligible to sit for the national exam and become a California State Certified Phlebotomy Technician I (CPT-I). MA has one full-time program chair/instructor, one full-time instructor, and five adjunct instructors. We have support staff including a 50% Program Specialist and a 40% Instructional Assistant. The Medical Assisting (MA) Program has been undergoing an enormous transformation as it works to meet the changing needs of a challenging healthcare field. In Fall 2010, the MA program was in jeopardy of losing their national accreditation because the program did not meet the thresholds of ≥ 60% of graduates being employed as medical assistants or in a related healthcare field and ≥ 70% of graduates passing the national exam. To try to resolve these issues, the MA Program Chair met with local healthcare employers on several occasions and solicited feedback about the MA program. The feedback given was that, even though our students excelled in MA skills, they lacked basic skills in English and math and soft skills. The MA Program Chair then began working closely with the Dean of CEED, Director of Workforce Development, and representatives from the Career Ladders Project to incorporate basic skills and soft skills into the current MA curriculum. In Spring 2012, we were awarded a $350,000 grant and the MA Program began the transformation of creating a learning community called the Accelerated Medical Assisting Program (AMAP), which has replaced our traditional MA program for students working towards a certificate or degree in Medical Assisting. As a result of the changes listed above our program is now meeting all of the accreditation thresholds. Our national exam pass rate went from 64% in 2010 to 91% in 2012. Our placement rate went from 64% in 2011 to 83% in 2012. The MA program continues to serve the needs of our non-AMAP students by offering courses and skills certificates for incumbent workers, students who are exploring occupations in healthcare, and students 1|Page from other allied health programs. For example, students on the waitlist in Nursing, Radiologic Technology, and Dental Hygiene take MA courses while they are on their respective waitlists. In addition the MA program offers a State accredited phlebotomy program. AMAP provides a new path to a career as a Certified Medical Assistant. Modeled after Cabrillo’s Nursing, Radiological Technology, and Dental Hygiene programs, all students take the same block of classes and move through the program together as one cohort. The courses provide a strong foundation in the essential skills employers have told us are needed to succeed in this career. The first semester includes courses that develop the necessary math and writing skills used in this profession. Each semester builds on the skills and knowledge developed in the previous semester, so that at the completion of the academic program students are positioned for success. AMAP is full time, Monday through Friday from 8:00 to 4:30. It is designed to result in a Medical Assisting Certificate of Achievement with completion of externship hours in four semesters. Students may also complete an Associate in Science degree. A new cohort begins twice a year, one during the Fall semester and one during the Spring semester. Students need to apply for the program and are accepted on a first come, first serve basis. We accepted 30-40 new students per semester. This is currently the only pathway for students pursuing a certificate or degree in Medical Assisting. Relationships Accreditation The Medical Assisting Program maintains a relationship with the Commission on Accreditation of Allied Health Education Programs (CAAHEP) and the Medical Assisting Education Review Board (MAERB). The phlebotomy program maintains a relationship with the California Department of Health Services, Laboratory Field Services. College Relationships The faculty and staff of the MA Program continue to work collaboratively with multiple programs on campus. We recently collaborated with the CABT, Math, and English programs to create contextualized courses for our medical assisting students. Our MA-70 Medical Terminology course is a pre-requisite for the Radiology Technology Program. Medical Assisting is a part of the Allied Health Department. The Director of Allied Health and the program chairs work collaboratively to implement new policies and procedures that affect all of the programs. Our recent efforts are focused on student success and the implementation of the ACE Foundation Course for all of our incoming students. The Accelerated Medical Assisting Program is an excellent fit for students affiliated with Extended Opportunity Programs and Services (EOPS/CARE) and Fast Track to Work (FTTW). Typically 1/3 of the MA cohort students come from these programs. We are currently working on building stronger relationships with both counseling and financial aid to help better serve the needs of our students. Both the MA program students and phlebotomy students are required to complete an externship. This externship is run through the Cooperative Work Experience Education (CWEE) program. Two MA faculty members serve as coordinators for these externships in which students are placed at local healthcare facilities. Both the MA program students and phlebotomy students have required health screening for their externships. Student Health Services (SHS) provides these screenings for our students. Student Health Services also allows 1- 2|Page 2 of our MA externs to be placed at their facility to complete their MA training. In addition, SHS hires MA graduates to work in their clinic. The MA program recently began partnering with the Academy for College Excellence (ACE) to help ensure student success in the program. Two faculty members from MA were trained as Master Mentors and currently teach the Foundation Course for our incoming cohort students. The Foundation Course is an intense 8-day presemester experience where students are taught the traits of a successful student, communication skills, professionalism, leadership skills, and working in teams. During this experience, students are able to bond with their classmates and their instructors. Since beginning to offer this to our incoming cohorts in Spring 2013 we have seen an improvement in professionalism of the students with a reduction in student behavioral issues and increase in student-to-student support. The MA program chair and students received the unique invitation to present at the April 2013 Cabrillo College Board meeting and the Cabrillo Foundation Annual luncheon. Both presentations exemplified effective student success strategies. A Board Member congratulated the program on the changes that have been made. The Accelerated Medical Assisting students are active participants in Cabrillo College events including the S4C Fourth Grade Experience, College and Career Night, Amgen Race, blood drive, teacher appreciation dinner, and student social events. Learning Communities In Spring 2012, AMAP became a learning community on Cabrillo College Aptos Campus. AMAP accepts students in the fall and spring semesters to begin the program. Students are required to be on campus Monday-Friday from 8:00-3:30 p.m. When not in classes, students complete their homework assignments with the support of peer study groups. Students who follow this model have found success in their college courses whereas numerous students reported they had not in the past. Local/Regional/Statewide Relationships Health Careers Partnership (HCP)- The Health Careers Partnership works county-wide to bring educators and employers together to address the healthcare educational needs of the community. The MA program chair attends annual meetings and actively participates in subcommittees. Bay Area Community College Consortium (BACCC) – The MA program chair is an active member of the BACCC and Medical Assisting Faculty Forum, which is a subcommittee of the BACCC. The BACCC works on a regional level to address the needs of employers and the Bay Area Community Colleges. The Medical Assisting Faculty Forum meets 2-3 times a year to discuss issues that affect the regional medical assisting programs. Topics thus far have included accreditation, curriculum, implementation of electronic health record courses and strategies for gaining and keeping externship sites. Areas of future focus will be on updating curriculum to include the enhancing roles of the medical assistant. Health Workforce Initiative (HWI) – The MA program chair worked collaboratively with other MA instructors and current medical assistants to update the state DACUM (Developing a Curriculum) and write curriculum for medical assisting. Career Ladders Project (CLP)- The Career Ladders Project works in partnership with California Community Colleges state-wide to provide educational and career advancement opportunities for Californians. The CLP fosters these opportunities through research, policy initiatives and strategic assistance to colleges and their workforce development partners. (http://www.careerladdersproject.org/). The MA program chair continues to work collaboratively with the CLP. Thus far we have sponsored two contextualized teaching and learning workshops presented by the CLP at Cabrillo College for faculty and staff of Cabrillo and the local high schools. The MA program chair was invited by the CLP to participate in a panel presentation about contextualized learning at the Student Success Conference in Fall 2012. 3|Page Community Relationships The MA program faculty and staff communicate regularly with members of its Community Advisory Committee (CAC) on programmatic matters to assess the needs of local employers. An annual Community Advisory Committee meeting is held each spring. We have a very close relationship with our local employers as their facilities also serve as externship sites for our students. The externship coordinators are in close contact with them throughout the semester via email, telephone calls, and site visits. Our goal is to increase the CAC meetings from one a year to two and to hold a separate meeting of just the employers once a year so that we may better serve their needs. Enrollments Academic Year Course Enrollment FTES Fall Spring Fall Spring 2008/09 1131 1167 91.3 2009/10 998 1026 2010/11 836 2011/12 2012/13 Section Fill Rate Fall Spring 95.7 99.5% 100.8% 83.8 88.2 96.4% 92.8% 954 76.3 89.9 89.2% 89.0% 788 794 70.8 71.2 84.9% 90.2% 729 786 66.1 73.6 82.3% 90.7% Enrollments dropped in 2008/09 in response to campus wide reductions due to the recession. The reduction of the FTES in 2011/12 is the result of switching over to a cohort model and only accepting a certain number of students into the Medical Assisting Program per semester based on labor market research and feedback from employer partners. We continue to get additional FTES from noncohort students, phlebotomy students, and students from other programs taking MA70 (Medical Terminology). Fill rates have remained high, though slightly below the college average. The 5-year average fill rate for MA was 92%. For the college over the same period of time it was 95%. Cost Program Income - FTES Academic Year Program College 2008/09 203 12,995 2009/10 182 2010/11 Base Expenditures Percent of Income Percent of Expense FTES/ Expense Ratio Program College 1.56% $348,338 $28,576,256 1.22% 1.3 12,283 1.48% $333,425 $26,987,796 1.24% 1.2 174 11,637 1.50% $280,304 $26,689,764 1.05% 1.4 2011/12 150 11,244 1.34% $288,825 $25,974,013 1.11% 1.2 2012/13 145 10,517 1.38% $276,821 $25,252,502 1.10% 1.1 Average 1.2 The MA program has been consistently efficient, generating on average 20% more revenue than it does expenses and 20% more WSCH/FTEF than the college average. 4|Page MA program Academic Year FTES Fall WSCH Spring Fall FTEF Spring Fall Spring WSCH/FTEF = Load Fall Spring 2008/09 91.3 95.7 2,843 2,995 4.1 4.1 702 733 2009/10 83.8 88.2 2,623 2,764 3.7 4.4 714 628 2010/11 76.3 89.9 2,393 2,808 3.6 4.6 665 616 2011/12 70.8 71.2 2,352 2,220 3.8 3.8 622 579 2012/13 66.1 73.6 2,123 2,303 3.9 3.9 551 590 Source: Datatel XFAS report [Faculty Assignment sheets.] MA to College Comparison College Academic Year WSCH/FTEF = Load Fall Spring Academic Year MA/College Load Ratio Fall Spring 2007/08 551 555 2007/08 1.5 1.4 2008/09 603 614 2008/09 1.2 1.3 2009/10 628 605 2009/10 1.1 0.9 2010/11 605 589 2010/11 1.1 1.2 2011/12 590 569 2011/12 1.3 1.2 Average 1.2 Source: Datatel XFAS report [Faculty Assignment Sheets.] Student Learning Outcomes SLOs had been written for courses and programs by the previous program chair. In Fall 2011, the current program chair began working with the SLO coordinator to devise a plan for assessing course and program SLOs. The MA faculty had never conducted SLO assessments so this process was talked about during the flex week program meeting in Spring 2012. At that time, course SLOs were looked at and discussions held amongst the faculty on the best ways to assess the course and program SLOs. It was determined at that time that the SLOs were going to be very difficult to assess because of the way they were written. It was also discovered that SLOs for courses in some cases were incorrect, i.e. not based on curriculum covered in that course, and that program SLOs were not written using the current format. Therefore, it was decided that all of the SLOs for courses and programs needed to be rewritten. The program chair continued working with the SLO coordinator to write assessable SLOs for all MA courses and programs. This was accomplished in Fall 2012. The MA program was selected to pilot the new CurricUNET SLO Assessment Module. Course SLO assessments were conducted by three MA faculty members in Fall 2013. The SLO coordinator then trained these three faculty members on inputting data into the CurricUNET SLO Assessment Module. In Spring 2014, the program chair trained the remaining MA faculty on how to use the Assessment Module. The three MA faculty members who participated in this training learned from their assessments that are SLOs are currently written in a way that they can be assessed and that there is room for improvement in instruction to ensure all students will master the course SLOs. The MA faculty is currently in the process of 5|Page assessing the remainder of the course SLOs. MA faculty will use the Assessment Module to input data by the end of this semester and discussions regarding results of the assessments will be held at the Fall 2014 flex week meeting. This process will be ongoing until all course and program SLOs have been assessed. During our work on the SLOs and our beginning assessment of them, we began having dialogue about teaching best practices in the MA program. The desire to seek guidance from colleagues and to share current teaching methods was brought about by first brainstorming about methods that could be used to assess SLOs. As faculty shared ideas, a richer conversation began about what was currently happening in the classrooms and how beneficial it would be to continue to share teaching methods with each other. The program chair and the full-time faculty member meet weekly to discuss students' progress, curriculum, and ongoing programmatic changes. All faculty are invited to attend this meeting but because of conflicting schedules, no adjunct faculty have been able to attend. We will continue to try to arrange meetings where more faculty can participate in the future. C u r r i c ul um R e v i ew All courses, certificates, and the A.S. degree were reviewed. Most courses were updated to reflect occupational changes and accreditation curriculum requirements. Several courses which have not been offered in the last two years were inactivated. The Medical Assisting Program reduced its certificate/degree offerings in Fall 2013 as a result of no demand for insurance specialists in the area. Based on employer feedback we have determined that there are very few jobs for students who are trained as administrative medical assistants only, particularly insurance specialists. Palo Alto Medical Foundation (PAMF) and Physicians Medical Group (PMG) have outsourced all of their billing and coding. Our employer partners have told us that they will only hire Medical Assisting students who have graduated with both administrative and clinical skills and who have taken the state or national test to become a Certified Medical Assistant. Therefore, we have decided to inactivate the Certificate of Achievement and Associate in Science degree in Medical Insurance Specialist. Student success continues to be the main focus of the Medical Assisting Program so further changes will be made in the courses required for the certificate of achievement, sequence of courses taken, and support given to incoming, current, and graduate students of the Medical Assisting Program. Student Success Medical Assisting Academic Year Course Success College Course Completion Course Success Course Completion Fall Spring Fall Spring Fall Spring Fall Spring 2008/09 70% 75% 89% 90% 69% 69% 86% 85% 2009/10 73% 77% 89% 87% 70% 71% 85% 85% 2010/11 77% 72% 89% 83% 71% 72% 86% 86% 2011/12 72% 69% 85% 86% 72% 73% 87% 87% 2012/13 73% 77% 89% 90% 72% 72% 88% 87% Average 74% 88% 71% 86% The Medical Assisting Program is slightly above the college totals for student success. With the implementation of the cohort model that began in Spring 2012, the goal is to continue to increase course and program success. We are currently looking at equity gaps to determine if this is a factor in course success 6|Page C r e d e nt i a l i n g E x a m O u t co m e s 2 0 1 3 A n n u a l R e p o rt M A E R B Total Year of Total Exam Number of Graduation Passers Graduates 2009 2010 2011 2012 Total 25 11 34 23 93 18 7 25 21 71 Accreditation Thresholds Established by MAERB Exam Pass Rate All Grads Over the last three years our national exam pass rate has gone from 63.64% to 91.3%. 72% 63.64% 73.53% 91.30% 76.34% 70% Results of Student Surveys In Fall 2013, the program chair requested that a new survey be taken to get feedback from students in our newly redesigned program which now includes cohort students participating in the Accelerated Medical Assisting Program and non-cohort students who enter the program the traditional way. Only classes that had a mix of students were surveyed. The survey results below reflect some dissatisfaction with the program and faculty because, under the grant, cohort students received perks such as scrubs and textbooks for the first semester, and guaranteed registration for all of their classes. The non-cohort students feel there is favoritism given to the cohort students. This survey was taken just a few weeks into the fall semester. Two new instructors were hired and were teaching two of the courses surveyed. Suggestions were made regarding revising faculty assignments and more faculty training. New faculty members are mentored by the program chair and full-time faculty member. As a result of the surveys, the program chair and faculty continue to work diligently to increase student satisfaction while in the medical assisting program. The surveys of our graduates and employers of our graduates show 100% satisfaction rate for the last 5 years. Refer to Tables E & F below. Students surveyed in the MA program are female (87%), male (13%), have a high school diploma or higher (96.5%), and are taking 12-15 units per semester (81.2%). Most respondents (80%) state that they would recommend MA classes to other students and the majority plan to take more MA classes at Cabrillo (87.1%). A majority (96.5%) of students responded that they have career plans within this field. These results suggest that MA classes are valuable to students who are strongly focused on career goals and see value in the employment preparation that MA courses offer. The majority of students surveyed feel that the course workload is appropriate (85.7%) and that the syllabi accurately reflect what is taught in class (89.3%). In response to the question, “What do you consider the major strengths of this program?” students most frequently mentioned excellence of instructors (35 times), the handson instructional methods used in the program (7) and great facilities and excellent lab equipment (5). In response to the question, “What are your suggestions for improving the program?” several responses included better enforcement of rules of the AMAP program regarding attendance, uniform, and behavioral issues (9) and suggestions were made regarding faculty assignments and training of new faculty. 7|Page 2 0 1 3 A n n u a l R e p o rt M A E R B G r a d u a t e S u rv e y R e s ul t s Number of Grads Returning Surveys Participation Percent Number of Surveys with Positive responses Cognitive Number of Surveys with Positive responses Psychomotor Number of Surveys with Positive responses - Affective Number of Surveys with Overall Positive Responses Percent Grad Survey Success Calendar Year Admitted Number of Graduates Number of Grad Surveys Sent 2008 34 34 22 65% 22 22 22 22 100% 2009 27 27 19 70% 19 19 19 19 100% 2010 27 27 23 85% 23 23 23 23 100% 2011 14 14 12 86% 12 12 12 12 100% 2012 6 6 6 100% 6 6 6 6 100% Total 108 108 82 76% 82 82 82 82 100% Accreditation Thresholds Established by MAERB 30% 80% 2 0 1 3 A n n u a l R e p o rt M A E R B E m pl o y e r S u r v ey R e s ul t s Admissi on Year Total Number of Positive Placeme nts Number of Grads Employ ed as MA or in Related Field Number of Grads Whose Employ ers Were Sent Surveys Numbe r of Grads Whose Employ er Return ed Surveys 2008 2009 2010 2011 2012 Total 21 21 20 9 5 76 10 13 17 4 3 47 8 8 12 3 2 33 8 8 12 3 2 33 Accreditation Thresholds Established by MAERB Participati on Percent Number of Surveys with Positive respons es Cognitiv e Number of Surveys with Positive responses Psychomo tor Number of Surveys with Positive respons es Affectiv e Number of Surveys with Overall Positive Respons es Percent Employ er Survey Success 80% 62% 71% 75% 80% 70% 8 8 12 3 2 33 8 8 12 3 2 33 8 8 12 3 2 33 8 8 12 3 2 33 100% 100% 100% 100% 100% 100% 30% 80% A n a l y s i s o f E x t e r n a l Da t a R e s e a r c h Medical Assistants are one of the fastest growing occupations in California. Employment growth is expected because of the increase in the number of group practices, clinics, and other healthcare facilities that need greater numbers of support personnel, particularly the flexible Medical Assistant who can handle both administrative and clinical duties. Because many healthcare employers prefer a trained staff, job prospects should be best for Medical Assistants with formal training or experience. 8|Page Projections of Employment In California, the number of Medical Assistants is expected to grow faster than average growth rate for all occupations. Jobs for Medical Assistants are expected to increase by 22.4 percent, or 18,100 jobs between 2010 and 2020. In Santa Cruz County, the number of Medical Assistants is expected to grow faster than average growth rate for all occupations. Jobs for Medical Assistants are expected to increase by 22.6 percent, or 140 jobs between 2010 and 2020. Estimated Employment and Projected Growth Medical Assistants Geographic Area Estimated Projected Numeric Percent (Estimated Year-Projected Year) Employment Employment Change Change California (2010-2020) Santa Cruz County (2010-2020) Additional Openings Due to Net Replacements 80,900 99,000 18,100 22.4 12,400 620 760 140 22.6 100 Source: EDD/LMID Projections of Employment by Occupation Annual Job Openings In California, an average of 1,810 new job openings per year are expected for Medical Assistants, plus an additional 1,240 job openings due to net replacement needs, resulting in a total of 3,050 job openings. In Santa Cruz County, an average of 14 new job openings per year is expected for Medical Assistants, plus an additional 10 job openings due to net replacement needs, resulting in a total of 24 job openings. Estimated Average Annual Job Openings Medical Assistants Geographic Area (Estimated YearProjected Year) California (2010-2020) Santa Cruz County (2010-2020) Jobs From Growth Jobs Due to Net Replacements Total Annual Job Openings 1,810 1,240 3,050 14 10 24 Source: EDD/LMID Projections of Employment by Occupation Wages The median wage in 2013 for Medical Assistants in California is $32,836 annually, or $15.79 hourly. The median wage for Medical Assistants in Santa Cruz County is $40,194 annually, or $19.32 hourly. The median is the point at which half of the workers earn more and half earn less. 9|Page Low (25th percentile) Median (50th percentile) High (75th percentile) California $26,434 $32,836 $39,575 Santa Cruz County $32,649 $40,194 $44,847 Annual Wages for 2013 Source: EDD/LMID Occupational Employment Statistics Survey, 2013 Wages do not reflect self-employment. Low (25th percentile) Median (50th percentile) High (75th percentile) California $12.71 $15.79 $19.03 Santa Cruz County $15.70 $19.32 $21.56 Hourly Wages for 2013 Source: EDD/LMID Occupational Employment Statistics Survey, 2013. Wages do not reflect selfemployment. Conclusions/New Directions The MA program graduated its first cohort in Fall 2013. While dramatic changes have been made, the process of redesign is far from complete. More work is necessary in the following areas: maintaining alignment between program learning outcomes and the changing role of the Medical Assistant; right-sizing the program for a dynamic labor market; retaining students to completion; ensuring that students have clinical experience; and staffing the program appropriately for the new design. Program Outcomes The requirements of the MA position are evolving at a faster pace as the Affordable Care Act is finally being implemented. It is imperative for the program to remain in close dialog with industry to keep abreast of employer’s changing expectations. Continue to convene the MA Advisory Committee once each year and continue to participate in the BACCC Medical Assisting marketplace to maintain alignment between the PLOs and the occupation’s requirements. Cost: $200, travel. Source: Perkins. Responsibility: faculty, CEED Dean. Timeline: ongoing, annual. Attend conferences and workshops and other professional development opportunities. Cost: $2000 conference fees and travel. Source: Perkins. Responsibility: faculty, CEED Dean. Timeline: ongoing, annual. Curriculum revisions will be necessary, including new course development. We do not know what those courses will be at this point, but once the need is identified it may be imperative for student success and employer satisfaction that we be able to respond quickly. There is a need to determine a way to be able to develop a course in one semester and offer it in the next. This may require advocacy with the COCCC and with the Statewide Senate. Responsibility: Curriculum Committee Chair, VPI, Faculty Senate President, Dean CEED. 10 | P a g e Right-sizing the Program for the Labor Market The labor market demand for Medical Assistants is also in flux as is the supply. There are many other educational institutions preparing people for this occupation (other colleges, ROP, adult schools, private schools) and it appears that the supply is substantially higher than the demand. On the other hand, employers are telling us that they are not able to find sufficiently well-prepared applicants. PAMF who employs 1400 MAs, recently reached out to the Bay Area Community College Consortium (hosted by Cabrillo) for assistance in meeting their need for well-prepared applicants. Some project that the demand for medical assistants will dramatically increase as healthcare reform increases and providers implement a medical care team that relies on medical assistants to deliver services that enable nurses and doctors to be more efficient with their time. The program will need to closely track demand for our graduates to determine the right size for our program. Continue to closely track Employment Outcomes Survey. Integrate accreditation reporting requirements with Survey to reduce duplication of effort, increase response rate. Share results of EOS with students and encourage participation in survey after they have graduated. Cost: no extra costs. Responsibility: Program Chair, PRO, CEED Dean. Timeline: integration - prior to carrying out EOS in late spring. Distribution to students - graduating class spring 2014, all classes fall 2014. Approach Health Improvement Partnership to request formal assistance in determining the right number of students to be graduating to serve Santa Cruz County employers’ needs. Also consult with Advisory Committee. Cost: no extra costs. Responsibility: Program Chair, Allied Health Director, Dean CEED. Timeline: Fall 2014 Continue to work towards building a stronger relationship with financial aid to better serve the needs of our students. Responsibility: Program Chair and Director of Enrollment Services. Retention to Completion Retention of students to the end of the program continues to be a challenge. Many of the students have enormous ground to cover between the start of the program and its completion. Retention rates for the cohorts have improved as the program has made curricular, pedagogical, and staffing adjustments. But there is room and a need for improvement. Areas to address this include improving students’ awareness of the program requirements and assisting them in making better choices about whether to enter the program, refining placement processes, improving the rate at which students acquire basic skills, improving resilience and selfefficacy, and improving economic supports. Improving Guidance to Students Before they Enroll We believe retention can be increased to some extent by assisting students to make better choices about whether to enter the program. We ask that the Counseling & Guidance department and PRO assist us in devising a strategy to measurably improve retention. Elements of this strategy may include changes to how counselors guide students, orientations or assessments, work with some of the referring agencies, and research into best practices. Cost: $500 research stipend for Counselor or faculty to research best practices. Source: Perkins. Responsibility: Chair C&G, PRO, MA Program Chair. Timeline: research summer 2014, design Fall 2014, implementation Spring 2015. Improving Acquisition of Basic Skills Students continue to struggle with the acquisition of basic skills in the MA program. One strategy under consideration is to require a higher level of skills for entry into the program. This would likely reduce the program’s accessibility to CalWORKs and WIA participants and other economically and academically disadvantaged students. Another strategy is to allow more students into the initial stages of the program. We have had sufficient success with contextualized instruction to believe that it is worthy of further development. Responsibility for developing and teaching these classes is unclear. Implementation of ACE Foundation Course: The ACE Foundation Course is designed to increase student success by helping students develop non-cognitive skills. It addresses traits of a successful student, communication and team-building skills, and identification of learning styles. AMAP is a learning community and the ACE Foundation Course helps ensure incoming students have bonded with each 11 | P a g e other and are acclimated to this type of supportive educational environment. With grant funding, the ACE Foundation course has been run as a separate course prior to the start of the following semesters: Spring 2013, Fall 2013, and Spring 2014. In these semesters we have seen greater retention than in the previous two semesters where similar curriculum was added into existing courses. Cost: Allocation of 3.25 TUs $5640.00 per semester. Staffing The realignment of the program around a cohort model and staffing changes required by years of budget reductions are requiring a redesign of how the program is staffed. There are certain critical elements of the curriculum, such as learning to give injections, that require more staff presence in order to ensure the health and safety of students. Adding additional staff in this capacity would be beneficial in providing additional safety measures for our students, increase our capability of maintaining accurate records for our accreditations, and be more support for our students which will help to increase student success. 70% IA position (increase from current 40% position) o Medical Assisting students are required to perform invasive procedures such as phlebotomy and injections on each other according to our accreditation standards. These lab classes have between 2530 students in them. The instructor is required to watch every single injection and every single blood draw. For safety reasons it is imperative to increase the current 40% IA position to a 70% position to enable the IA to be present in all clinical classes. Additional duties include, but are not limited to, proper disposal of sharps, inventory control, setting up and breaking down labs, and student support· As there is a need to maintain two separate accreditations (MA and phlebotomy) increasing this position would increase our capability of maintaining accurate records for these accreditations. Allocate 3 TUs for externship coordinator o Both Medical Assisting and Phlebotomy students are required to complete an externship of 180 hours or 120 hours respectively. We currently have a limited number of externship sites. Students will not graduate if they do not complete their externship. Currently some students’ graduation is being delayed by a semester because of the limited number of sites available. Allocating 3 TUs to the externship coordinator will ensure there is adequate time to acquire new sites, maintain current sites, place extern students in sites, and complete all of the necessary paperwork as mandated by our accreditation regarding externships. Additional Programmatic Costs (costs will vary depending on current market value) o Furniture/Equipment maintenance and replacement (e.g. beds, phlebotomy chairs, scales, autoclave, EKG machines, spirometer, stethoscopes, urinalysis machine, etc). o Repair broken equipment o Replace outdated equipment (EKG machine $3000-$5000; autoclave $6000). Anticipate need to replace equipment beginning in 2016. Equipment replacement schedule would be one piece of equipment per year at a cost of $3000-$6000. o Repair or replace broken lab furniture Program Planning Goals and Recommendations with costs 1. Staffing: Increase 40% IA position to 70% (10 mos). Cost: $36,694. 2. Staffing: Allocate 3 TUs for externship coordinator. Cost: $5205.00. 3. ACE Foundation Course implementation: 3.25 TUs (per semester). Cost $11,278. 4. Faculty professional development: Conference attendance/travel to regional meetings. Cost: $2200.00. 5. Curriculum changes based on employer need/accreditation requirements. Cost: $1735.00 per TU. 12 | P a g e 6. Improve guidance to students before they enroll. Cost: $500 stipend for research. 7. Furniture/equipment maintenance and replacement. Cost: $3000-$6000 per year. Program Planning Goals and Recommendations with no costs 1. Continued work on resizing the MA program for the labor market. 2. Annual Community Advisory Committee meetings. 3. Continued tracking of Employment Outcome Survey. 4. Improving guidance to students before they enroll. List of Appendices Occupational Program Assessment Analysis 2013-14 MA Catalog pages 13 | P a g e Occupational Program Assessment Analysis Use the form below to summarize the results of the department meeting in which you discussed the results of your program’s assessment process. Include this form in your Instructional Plan and incorporate the results into the narrative of your instructional plan. Department Medical Assistant Meeting Date 8/23/12 Number of Faculty in Attendance (% of full time and adjunct plus total) 8 (2 full-time, 6 adjunct) Number of Faculty sharing Assessment Results – if applicable (% of full time and adjunct plus total) 8 (2 full-time, 6 adjunct) SLO(s) Competency Measured MA70, MA185B, MA160, MA165, MA170B, MA172, MA173A, MA176, MA176L MA181, MA183C, MA184, MA130, MA130A, MA130AL, MA150, MA188 Certificate of Achievement/AS Medical Assistant Certificate of Achievement/AS Medical Insurance Specialist Skills certificate: Phlebotomy Technician Skills certificate: Electronic Health Records Assessment Tool (Briefly describe assessment tool) For the assessment of the course SLOs, Certificate of Achievement/AS in Medical Insurance Specialist and skills certificate in Electronic Health Record test questions, in class assignments and in class demonstrations were utilized. For assessment of the Certificate of Achievement/AS – Medical Assistant pass rate of the national exam was used. For assessment of the skills cert: Phlebotomy Technician pass rate of the national exam was used. Assessment Results (Summarize the overall results of your department including any It was unanimously decided that the current SLOs that we had for the courses and programs were not able to be assessed accurately; therefore, all course and program SLOs 14 | P a g e students needs and issues that emerged) were rewritten. Next Step in the Classroom o to Improve Student Learning (list all the items faculty felt would help them improve student learning) Next Step in the Department to Improve Student Learning (check all that the department felt would help them improve student learning) Priorities to Improve Student State goals or objectives of assignment/activity more explicitly o Revise content of assignment/activities o Revise the amount of writing, oral, visual, clinical or similar work o Revise activities leading up to assignment o Increase in-class discussions and activities o Increase student collaboration and/or peer review o Provide more frequent feedback on student progress o Increase guidance for students on assignments o Use methods of questions that encourage competency o State criteria for grading more explicitly o Increase interaction with students outside of class o Ask a colleague to critique assignment o Collect more data o Nothing; assessment indicates no improvement necessary X Other (please describe) : All course and program SLOs were rewritten. o Offer/encourage attendance at seminars, workshops or discussion groups about teaching methods o Consult teaching and learning experts about teaching methods o Encourage faculty to share activities that foster competency o Write collaborative grants to fund departmental projects to improve teaching o Prove articles/books on teaching about competency o Visit classrooms to provide feedback (mentoring) o Create bibliography of resource material o Have binder available for rubrics and results o Analyze course curriculum to determine that competency skills are taught, so that the department can build a progression of skills as students advance through courses o Nothing; assessments indicate no improvements necessary X Other (please describe) Assess newly revised course and program SLOs on a more regular basis and share feedback. Ensure faculty teaching the courses understand fully the SLOs and discuss ways to best assess them. 15 | P a g e Learning (List the top 3-6 things faculty felt would most improve student learning) Since SLOs needed revision, faculty discussed best teaching practices for all courses with the goal of implementing these in current courses. Faculty discussed the benefit of having more interactive in-class assignments and would begin to utilize these strategies. Implementation (List the departmental plans to implement these priorities) Timeline for Implementation (Make a timeline for implementation of your top priorities PC will ensure faculty for all courses understand SLOs and how to assess them. PC will ensure SLO assessment is discussed at faculty meetings during flex week . Once new SLOs have been approved through curriculum they will be reassessed beginning Fall 2013. Best teaching practices will be implemented immediately. Faculty will begin to create and implement more interactive in-class activities. 16 | P a g e Occupational Program Assessment Analysis Use the form below to summarize the results of the department meeting in which you discussed the results of your program’s assessment process. Include this form in your Instructional Plan and incorporate the results into the narrative of your instructional plan. Department Medical Assistant Meeting Date 4/24/13 Number of Faculty in Attendance (% of full time and adjunct plus total) 3 (1 full-time, 2 adjunct) Number of Faculty sharing Assessment Results – if applicable (% of full time and adjunct plus total) 2 adjunct SLO(s) Competency Measured MA180, MA186, MA189 Assessment Tool The SLOs for these courses are measured with in-class demonstrations by the students. (Briefly describe assessment tool) Assessment Results (Summarize the overall results of your department including any students needs and issues that emerged) Faculty felt that students were able to demonstrate proficiency of the student learning outcomes. Faculty assessed student proficiency of the SLOs over several course periods. 17 | P a g e Next Step in the Classroom to Improve Student Learning (list all the items faculty felt would help them improve student learning) Next Step in the Department to Improve Student Learning (check all that the department felt would help them improve student learning) o State goals or objectives of assignment/activity more explicitly o Revise content of assignment/activities o Revise the amount of writing, oral, visual, clinical or similar work o Revise activities leading up to assignment o Increase in-class discussions and activities o Increase student collaboration and/or peer review o Provide more frequent feedback on student progress o Increase guidance for students on assignments o Use methods of questions that encourage competency o State criteria for grading more explicitly o Increase interaction with students outside of class o Ask a colleague to critique assignment o Collect more data o Nothing; assessment indicates no improvement necessary X Other (please describe) Faculty felt the SLOs were appropriate and students were proficient in these areas. o Offer/encourage attendance at seminars, workshops or discussion groups about teaching methods o Consult teaching and learning experts about teaching methods o Encourage faculty to share activities that foster competency o Write collaborative grants to fund departmental projects to improve teaching o Prove articles/books on teaching about competency o Visit classrooms to provide feedback (mentoring) o Create bibliography of resource material o Have binder available for rubrics and results o Analyze course curriculum to determine that competency skills are taught, so that the department can build a progression of skills as students advance through courses X Nothing; assessments indicate no improvements necessary o Priorities to Improve Student Learning Other (please describe) (List the top 3-6 things faculty felt Since these courses involve coding and computer skills, the faculty felt repetition is the best way to improve student learning in these courses. Faculty felt continuing to have in-class activities is important to improve student learning. 18 | P a g e would most improve student learning) Implementation (List the departmental plans to implement these priorities) Timeline for Implementation (Make a timeline for implementation of your top priorities Faculty felt continuing to discuss teaching best practices with colleagues would be beneficial in improving student learning. PC will encourage open dialogue between the faculty regarding teaching best practices and SLO assessment. PC will ensure that SLO assessment is discussed during flex week during faculty meetings. Faculty will begin immediately implementing teaching best practices. Assessment of SLOs will continue during flex week Fall 2013. 19 | P a g e MEDICAL ASSISTING Health, Athletics, Wellness, and Kinesiology Division Ian Haslam, Division Dean Division Office, Room 1102 Pamela Sanborn, Program Chair (831) 479-6438 Aptos Counselor: (831) 479-6274 for appointment Watsonville Counselor: (831) 786-4734 Call (831) 479-6248 for more information http://www.cabrillo.edu/programs Medical Assisting A.S. Degree Program Description: The Cabrillo College Medical Assisting Program is accredited by the Commission on Accreditation of Allied Health Education Programs (www.caahep.org) upon the recommendation of the Medical Assisting Education Review Board (MAERB). Commission on Accreditation of Allied Health Education Programs (CAAHEP), 1361 Park Street, Clearwater, FL 33756, (727) 210-2350. The Medical Assistant is an integral part of the medical team; thus the job demands the same high caliber of ethics, attitude, confidentiality and performance that the public has come to expect of the medical profession. Opportunities are many and varied, depending upon such factors as personal ability, experience and education. Medical Assistants may become managers of clinics or group practices as well as assist in the physician's office, clinic or hospital. Security Screening: To comply with state and local regulations for health care providers, students participating in externships through the Cabrillo College Medical Assisting program are required to meet vaccination and drug testing requirements and provide documentation to the Student Health Services Center before being placed at an externship site. Students are also required to complete criminal background checks and may be required to undergo fingerprinting. Medical Assisting Certificate of Achievement and A.S. Degree: Students completing the requirements for the AS degree or Certificate of Achievement: Medical Assistant will: 1. Accurately & safely perform medical assisting tasks and procedures. 2. Perform receptionist and administrative medical facility duties. 3. Interact professionally and ethically with patients and medical facility personnel, working within the medical assistant scope of practice. A.S. General Education 21 Units Core Courses (32-32.5 units) MA 70 Medical Terminology. . . . . . . . . . . . . . . . . . . . . . . . . 3 MA 160 * Basic ICD-10-CM and CPT Coding . . . . . . . . . . . . 1 MA 165 *****Injection Short Course . . . . . . . . . . . . . . . . . . 1 MA 170B Medical Terminology-Structure and Function of the Body. . . . . . . . . . . . . . . . . . . . . . . . . 3 MA 172 Medical Office Procedures . . . . . . . . . . . . . . . . . . . . 4 20 | P a g e MA 173A Medical Law and Ethics . . . . . . . . . . . . . . . . . . . . . 1.5 MA 176 ** Introduction to Medical Assisting Procedures. . . 3 MA 176L ** Medical Assisting Lab . . . . . . . . . . . . . . . . . . . . . 1 MA 181 Medical Insurance. . . . . . . . . . . . . . . . . . . . . . . . . . . 3 MA 183C *****EKG Complete Skills . . . . . . . . . . . . . . . . . . . . 2 MA 184 Health Care Communication . . . . . . . . . . . . . . . . . . . 2 MA 185B *****Phlebotomy. . . . . . . . . . . . . . . . . . . . . . . . . . . 1 MA 199C *** Career Work Experience Education . . . . . . . . . . 3 CABT 31 Microsoft Word. . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3 CABT 110A **** Computer Keyboarding-Alphabet Keys . . . . . 0.5 and CABT 110B **** Computer Keyboarding-Numbers/Symbols . 0.5 Approved Electives (6.5-7 Units) Units CABT 111 Using Speech Recognition Software. . . . . . . . . . . . . 1 CABT 156 Writing for the Workplace. . . . . . . . . . . . . . . . . . . . . 3 CABT 102 10-Key Calculator . . . . . . . . . . . . . . . . . . . . . . . . . . . 1 COMM 2 Group Discussion . . . . . . . . . . . . . . . . . . . . . . . . . . . 3 COMM 6 Listening . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1 MA 100 Medical Assistant Essentials. . . . . . . . . . . . . . . . . . . 4 MA 150 Pharmacology for Medical Assistants. . . . . . . . . . . . 2 MA 180 ICD-10 Diagnostic and Procedural Coding . . . . . . . . 3 MA 186 CPT (Current Procedural Terminology) Coding . . . . 2 MA 188HP Human Pathophysiology. . . . . . . . . . . . . . . . . . . . . . 3 MA 189 Electronic Health Records . . . . . . . . . . . . . . . . . . . 1.5 MATH 190ALH Math for Allied Health Careers . . . . . . . . . . . . . . . . . 3 PSYCH 35ABC Death and Dying . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3 SPAN 1 Elementary Spanish I . . . . . . . . . . . . . . . . . . . . . . . . 5 SPAN 2 Elementary Spanish II. . . . . . . . . . . . . . . . . . . . . . . . 5 SPAN 3 Intermediate Spanish I . . . . . . . . . . . . . . . . . . . . . . . 5 SPAN 4 Intermediate Spanish II. . . . . . . . . . . . . . . . . . . . . . . 5 Total Units 60 *Students who have completed MA 180 and MA 186 are excused from this course and may substitute one unit from the Approved Electives list. **This course must be taken within one year of externship. ***All core classes must be completed before MA 199C can be taken. ****Students who enter the program with an ability to type 40 WPM should substitute CABT 110C to increase typing speed. *****MA 165, MA 185B, MA 183C must be taken in semester immediately preceding MA 199C (externship). Cabrillo College Catalog–2013-2014 addendum Medical Assisting Certificate of Achievement Core Courses (32-32.5 Units) Units MA 70 Medical Terminology. . . . . . . . . . . . . . . . . . . . . . . . . 3 MA 185B *****Phlebotomy. . . . . . . . . . . . . . . . . . . . . . . . . . . 1 MA 160 * Basic ICD-10-CM and CPT Coding . . . . . . . . . . . . 1 MA 165 *****Injection Short Course . . . . . . . . . . . . . . . . . . 1 MA 170B Medical Terminology-Structure and Function of the Body . . . . . . . . . . . . . . . . . . . . . 3 MA 172 Medical Office Procedures . . . . . . . . . . . . . . . . . . . . 4 21 | P a g e MA 173A Medical Law & Ethics . . . . . . . . . . . . . . . . . . . . . . 1.5 MA 176 ** Introduction to Medical Assisting Procedures. . . 3 MA 176L ** Medical Assisting Lab . . . . . . . . . . . . . . . . . . . . . 1 MA 181 Medical Insurance. . . . . . . . . . . . . . . . . . . . . . . . . . . 3 MA 183C *****EKG Complete Skills . . . . . . . . . . . . . . . . . . . . 2 MA 184 Health Care Communication . . . . . . . . . . . . . . . . . . . 2 MA 199C *** Career Work Experience Education . . . . . . . . . . 3 CABT 110A **** Computer Keyboarding-Alphabet Keys . . . . . 0.5 and CABT 110B **** Computer Keyboarding-Numbers/Symbols . 0.5 CABT 131 Microsoft Word. . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3 Other Required Courses (3 units) CABT 157 Business and Technical Writing . . . . . . . . . . . . . . . . 3 or ENGL 100 Elements of Writing . . . . . . . . . . . . . . . . . . . . . . . . . 3 or ENGL 1A/1AH/1AMC/1AMCH . . . . . . . . . . . . . . . . . . . . . . . . . . . . . . 3 Total Units 35.5 *Students who have completed MA 180 and MA 186 are excused from this course and may substitute one unit from the Approved Electives list. **This course must be taken within one year of externship. ***All core classes must be completed before MA 199C can be taken. ****Students who enter the program with an ability to type 40 WPM should substitute CABT 110C to increase typing speed. *****MA 165, MA 185B, MA 183C must be taken in semester immediately preceding MA 199C (externship). Electronic Health Records Skills Certificate Program Learning Outcomes: Students completing the requirements for the skills certificate Electronic Health Record will: 1. Correctly navigate an electronic health record system to record patient encounters, maintain health records and access patient information. Core Courses MA 70 Medical Terminology. . . . . . . . . . . . . . . . . . . . . . . . . 3 CABT 38 Introduction to Microsoft Office . . . . . . . . . . . . . . 3-4 CABT 101 Computer Proficiency . . . . . . . . . . . . . . . . . . . . . . . . 3 CABT 102 10-Key Calculator . . . . . . . . . . . . . . . . . . . . . . . . . . . 1 CABT 110A * Computer Keyboarding-Alphabet Keys . . . . . . . . 0.5 and CABT 110B * Computer Keyboarding-Numbers/Symbols . . . . 0.5 or CABT 110C Computer Keyboarding-Speed Development . . . . . 0.5 MA 173A Medical Law & Ethics . . . . . . . . . . . . . . . . . . . . . . 1.5 MA 189 Electronic Health Records . . . . . . . . . . . . . . . . . . . 1.5 Total Units 13.5-15 *Students who begin this skills certificate with an ability to type 40 WPM should substitute CABT 110C to increase typing speed.* Phlebotomy Technician Skills Certificate Program Learning Outcomes: 22 | P a g e Students completing the requirements for the skills certificate Phlebotomy Technician will: 1. Accurately and safely draw blood using capillary and venipuncture procedures. 2. Label, handle, and process blood and non-blood specimens to avoid pre-analytical sources of error and deliver to appropriate department. Required MA 130A * Phlebotomy . . . . . . . . . . . . . . . . . . . . . . . . . . . . 1.5 MA 130AL * Phlebotomy Lab. . . . . . . . . . . . . . . . . . . . . . . . . . . 1 MA 130B * Phlebotomy-Advanced . . . . . . . . . . . . . . . . . . . . 1.5 MA 199C * Career Work Experience Education . . . . . . . . . . . . 2 MA 70 Medical Terminology. . . . . . . . . . . . . . . . . . . . . . . . . 3 Total Units 9 *This course is required for California State Licensing, and must be taken within one year of MA 199C externship.) Medical Assisting Courses: MA 70 Medical Terminology 3 units; 3 hours Lecture Recommended Preparation: ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches allied health students fundamentals of medical word building with emphasis on prefixes, word roots, suffixes, combining forms, abbreviations, and lay terms. Transfer Credit: Transfers to CSU. MA 100 Medical Assistant Essentials 4 units; 3 hours Lecture, 3 hours Laboratory Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches essential principles, skills, and professionalism for success in the medical assistant profession. MA 110 Administrative Medical Assisting Procedures 3 units; 3 hours Lecture Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches medical assistant students administrative skills utilized in outpatient medical settings. MA 111 Introduction to Insurance and Medical Office Financial Management 3 units; 3 hours Lecture Prerequisite: MA 160 or MA 186 and MA 180. Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches medical assistant students basic financial management and insurance billing procedures utilized in outpatient medical settings. MA 120 Clinical Medical Assisting Procedures 6 units; 4 hours Lecture, 6 hours Laboratory 23 | P a g e Prerequisite: MA 70. Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches medical assistant students theory along with clinical skills utilized in outpatient medical settings. MA 130A Phlebotomy 1.5 units; 1.5 hours Lecture Prerequisite: MA 70. Corequisite: MA 130AL or current California phlebotomy certification. Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. California Certified basic phlebotomy course teaching proper collection of blood specimens, choice of proper equipment, venipuncture techniques, patient care, safety, tests, and quality assurance. This course is designed for all beginning students and for phlebotomists with less than 1,040 hours of experience. Students who wish to become California state certified phlebotomists must complete MA130A, MA130B and MA130AL, and a 120hour externship. Phlebotomists with less than 1,040 hours must take MA130A and B to become certified. Phlebotomists with more than 1,040 hours must take MA130B. All students must pass a national phlebotomy certification examination to become certified. May be offered in a Distance-Learning Format. MA 130AL Phlebotomy Lab 1 unit; 4 hours Laboratory Corequisite: MA 130A or current California phlebotomy certification. Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Provides the skills portion of the MA 130 series for beginning phlebotomy students working towards state certification. Students will perform approximately 35 venipunctures and 2 skin punctures, learning clinical and hospital procedures. A two-unit externship (MA 199C) is also required for those planning to become state certified phlebotomists. Students MUST bring a copy of verification of Hepatitis B vaccinations 1 and 2 to the first class. Student skills must demonstrate compliance to safety instructions or students may be dropped from course. New students who wish to become California state certified phlebotomists must complete MA 130A, MA 130B and MA 130AL, and a 120-hour externship. Phlebotomists with less than 1,040 hours must take MA 130A and B to become certified. Phlebotomists with more than 1,040 hours must take MA 130B. All students must pass a national phlebotomy examination to become certified. MA 130B Phlebotomy-Advanced 1.5 units; 1.5 hours Lecture Prerequisite: MA 130A or current California phlebotomy certification. MA 130AL. Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches phlebotomy equipment, techniques, patient care, safety, tests, advanced infection control and biohazards, quality assurance and communications. Advanced lecture required for state certification. Course designed for all students including phlebotomists with more than 1,040 hours of phlebotomy experience. All students must pass a national phlebotomy examination to become certified. May be offered in a DistanceLearning Format. MA 150 Pharmacology for Medical Assistants 2 units; 2 hours Lecture Prerequisite: MA 70. Recommended Preparation: Eligibility for ENGL 100 and READ 100; Eligibility for MATH 154. 24 | P a g e Repeatability: May be taken 1 time. Teaches medical assistant and allied health students drug therapy including the mechanisms of action, therapeutic effects, clinical indications, reactions, and interventions. MA 160 Basic ICD-10-CM and CPT Coding 1 unit; 1 hour Lecture Prerequisite: MA 70. Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches basic principles and conventions of the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) and Current Procedural Terminology (CPT) coding classification systems to students not majoring in billing or coding. MA 165 Injection Short Course 1 unit; 0.5 hour Lecture, 1.5 hours Laboratory Prerequisite: MA 70. Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches allied health students and current health care employees the correct procedures for administering intramuscular, intradermal and subcutaneous injections. MA 170B Medical Terminology-Structure & Function of the Body 3 units; 3 hours Lecture Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches medical assistant and allied health students terms of anatomy, physiology, diseases, diagnostic, operative, and x-ray procedures. MA 172 Medical Office Procedures 4 units; 4 hours Lecture Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches medical assistant students administrative skills and basic financial management utilized in outpatient medical settings. MA 173A Medical Law & Ethics 1.5 units; 1.5 hours Lecture Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches medical assistant and allied health students medical law, liability, and ethics. MA 176 Introduction to Medical Assisting Procedures 3 units; 3 hours Lecture Prerequisite: MA 70. Recommended Preparation: Eligibility for ENGL 100 and READ 100. Hybrid Requisite: Completion of or concurrent enrollment in MA 176L. Repeatability: May be taken 1 time. Teaches medical assistant students theory of clinical skills utilized in outpatient medical settings. 25 | P a g e MA 176L Medical Assisting Lab 1 unit; 3 hours Laboratory Recommended Preparation: Eligibility for ENGL 100 and READ 100. Hybrid Requisite: Completion of or concurrent enrollment in MA 176. Repeatability: May be taken 1 time. Teaches medical assistant students clinical skills utilized in outpatient clinical settings. MA 180 ICD-10 Diagnostic and Procedural Coding 3 units; 3 hours Lecture Prerequisite: MA 70 and MA 170B. Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches principles, functions, format, conventions, and guidelines of International Classification of Diseases 10th Revision Clinical Modification and Procedural Coding System (ICD-10-CM/PCS) for coding assignments as applicable to all levels of health care services for statistics and reimbursement. MA 181 Medical Insurance 3 units; 3 hours Lecture Prerequisite: MA 160 or MA 180 and MA 186. Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches theory and application of medical insurance billing and procedures as used in medical facilities. MA 183C EKG Complete Skills 2 units; 1 hour Lecture, 3 hours Laboratory Prerequisite: MA 70. Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches electrocardiography skills, holter and stress monitoring, and recognition of cardiac irregularities. MA 184 Health Care Communication 2 units; 2 hours Lecture Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches medical assistant and other allied health students skills of professional conduct and interaction for healthcare settings and job-related social settings. MA 185B Phlebotomy 1 unit; 0.5 hour Lecture, 1.5 hours Laboratory Prerequisite: MA 70. Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches health students and current healthcare employees phlebotomy. Course does not satisfy California State Phlebotomy licensing requirements. MA 186 CPT (Current Procedural Terminology) Coding 2 units; 2 hours Lecture Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches procedural coding for office and outpatient procedures. 26 | P a g e MA 188HP Human Pathophysiology 3 units; 3 hours Lecture Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches allied health students general principles of disease processes with emphasis on etiologies and physiological changes, diagnostic procedures, preventive measures, and current treatment. MA 189 Electronic Health Records 1.5 units; 1 hour Lecture, 1.5 hours Laboratory Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Teaches the use of electronic health records documenting patient encounter from scheduling to recording medical information. MA 190AZ Special Topics in Medical Assistant 0.5 - 5 units; 0.5 hour Lecture Recommended Preparation: Eligibility for ENGL 100 and READ 100. Repeatability: May be taken 1 time. Investigates special selected areas of interest in Medical Assistant not covered by regular catalog offerings. The special areas will be announced, described, and given their own titles and letter designations in the Schedule of Classes. 27 | P a g e May 7, 2014 MA Program Planning Goals and Recommendations 1. Description: Staffing: Increase IA position to 70%; (10 mos) Cost $36694 (general fund) 2. Staffing: Allocate 3 TUs for externship coordinator $5205 (general fund) 3. ACE Foundation Course implementation - 3.25 TUs per semester $1735x3.25 x2 $11278 (general fund) 4. Faculty Professional Development (conferences/travel expenses to meetings) $2200 (Perkins) 5. Curriculum changes based on employer needs/accreditation requirements $1735 per new TU required (general fund) 6. Improve guidance to students before they enroll $500 research stipend for counselor or faculty (Perkins) 7. Furniture/equipment maintenance and replacement estimate $3000-$6000 per year (general fund, possibly Perkins) 8. 9. 10. . . Cabrillo College 5/7/2014 10:48 AM May 7, 2014 MA Program Planning Goals and Recommendations Description: 1. Cost None Continued work on resizing the MA program for the labor market. 2. None Annual Community Advisory Committee meetings. 3. None Continued tracking of Employment Outcome Survey. 4. None Improving guidance to students before they enroll. 5. 6. 7. 8. 9. 10. . . Cabrillo College 5/7/2014 10:48 AM