2011 Medical School Annual Return (MSAR)
advertisement
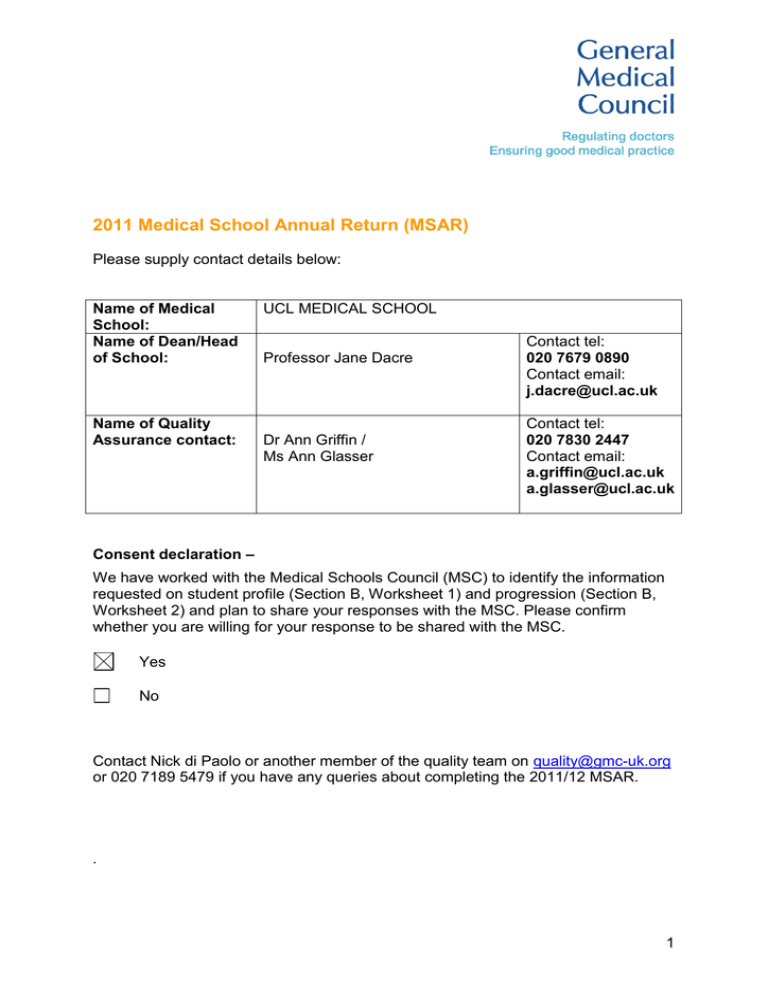
2011 Medical School Annual Return (MSAR) Please supply contact details below: Name of Medical School: Name of Dean/Head of School: Name of Quality Assurance contact: UCL MEDICAL SCHOOL Professor Jane Dacre Dr Ann Griffin / Ms Ann Glasser Contact tel: 020 7679 0890 Contact email: j.dacre@ucl.ac.uk Contact tel: 020 7830 2447 Contact email: a.griffin@ucl.ac.uk a.glasser@ucl.ac.uk Consent declaration – We have worked with the Medical Schools Council (MSC) to identify the information requested on student profile (Section B, Worksheet 1) and progression (Section B, Worksheet 2) and plan to share your responses with the MSC. Please confirm whether you are willing for your response to be shared with the MSC. Yes No Contact Nick di Paolo or another member of the quality team on quality@gmc-uk.org or 020 7189 5479 if you have any queries about completing the 2011/12 MSAR. . 1 MSAR 2011/12 – Section A For reference, please refer to the UCLMS Glossary QABME 2011 (Doc. 14) Domain 2 - Quality assurance, review and evaluation 1. How are you quality assuring clinical placements for your students? UCL Medical School has robust mechanisms to ensure it quality assures and enhances the student experience at UCL. The Quality Assurance Office co-ordinates the evaluation activities across the Medical School. In order to give our students the opportunity to provide feedback on their learning experience we employ a range of strategies which are complementary and fit for purpose given the complexity of the programme. Overall, the students feel they are represented in most discussions relating to the quality of the course. Partly driven by the sheer size of the faculty and the complexity of the clinical course we use an on-line system for gathering feedback through student evaluation questions. A number of research projects over the last few years, which have used qualitative methods to study the student experience, have provided particularly helpful insights into specific aspects of curricular change, for the new curriculum and students raising concerns. Student evaluation questionnaires - All modules and all NHS sites (including each of the 200+ GP practices) are evaluated via the on-line Student Evaluating Questionnaire (SEQ) system using the Opinio6 software. August 2010 saw the introduction of an upgraded version of Opinio©, which has enhanced reporting and drill down facilities and improved security. In 2010-11 we received over 15,000 individual responses of combined numerical data and free text. The SEQs have core questions and an overall satisfaction score which permits comparison of modules and sites. SEQ data is used in planning and preparation of NHS QA/SIFT site visits. Most module management groups (MMGs) refer to SEQ data in reviewing modules and in writing annual reports, e.g. the Annual Monitoring Report for College and the Annual SIFT Report for the Strategic Health Authority. Summary reports are also produced and reviewed during periodic Undergraduate Teaching Committees to evaluate the ‘health’ and delivery of modules. All elected student reps have full access to aid them in their role. In addition we have a text “no-show” system to alert us of unplanned cancellations and have a specific website for students wishing to raise concerns; permitting a more timely and proactive approach to quality assurance. http://www.ucl.ac.uk/medicalschool/quality/raising_student_concerns Standards for trusts: clinical teaching standards and provision of IT services for students – see IT Standards 2011-12 (Doc. 1) this year we have revised the standards for both clinical teachers and IT services required on clinical placements. Site visits – We have visited our central and district general hospitals on a regular basis, but our visiting procedures are currently under review and we are piloting a trust self-assessment return so that we can better reflect the external progress in quality assuring medical schools. (See http://www.ucl.ac.uk/medicalschool/quality/site-visits) Student representatives and student-staff consultative committees – student representatives are an integral part of the QA process. They undergo UCL and specific training by the QAU. They are invited to all significant committees and meetings. SSCCs are termly. Medical School Quality Management and Enhancement committee (mQMEC) – a termly meeting where key QA issues are discussed and disseminated. Primary care placements are quality assured by the Department of Primary Care & Population Health. Quality of clinical placements in general practice is continually monitored by course leads. The Department’s Primary Care Education Committee meets once each quarter to review evaluation reports. Monitoring of all community placements takes place mainly through the Medical School’s well-established, web-based evaluation system for collecting student feedback (Opinio). Individual reports are sent or emailed directly to teachers concerned and any problems are discussed with course leads. We also monitor the quality of teaching in GP Practice by means of practice visits and peer review of teaching. All courses and quality matters are also reviewed each term at Divisional Undergraduate Teaching Committee, MBBS Module Management Groups and Staff-Student Consultative Committees. Primary and secondary care teaching has standards for best practice (see Q2). 2 2. How are you quality assuring student assistantships for your students? Principles of design and evaluation of Hospital-based assistantships: The new Final Year was planned to make the most of the learning opportunities across the sites. Site leads and tutors have co-constructed the new course and this in turn has greatly facilitated our approach to evaluations and quality improvement. Specifically this has been done by the following: Design and development of assistantships has been done in collaboration with a team of Final Year DGH and GP tutors, recognising the need for maximum local flexibility to achieve common goals Team includes MBBS Sub Dean (Assessment) and Director of the North Central Foundation School Assistantships were grounded in a patient-centred, hands-on apprenticeship model, explicitly increasing direct responsibility for patients and working to an F1 doctor Risk and patient safety issues were anticipated (as far as possible) and managed Documentation about expectation and aim for clinical tutors, clinical supervisors and students was widely disseminated Documentation Standards for Clinical Teachers 2011-12 (Doc.2) Factsheets - downloadable individual documents outlining: Student Assistantships (Doc. 3) Curriculum for Safe Prescribing (Doc. 4) Supervision, Support & Assessment (including flow chart for formative feedback & completion of grade forms) (Doc. 5) Implications for Supervising Junior Doctors (Doc. 6) Syllabus Document 2011-12 (with focus on safety, presentations, problems and situations) – forms MBBS final exam blueprint (Doc. 7) Record of Completed Procedures (list sourced from TDs 2009) - DGH (Doc. 8) and GP (Doc. 9) Evaluation and quality improvement – cycle approach We have quarterly Final Year Curriculum team meetings to review progress and areas for developments. We had two additional meetings just to discuss our focus on prescribing and to link with pharmacists. Student experience: Student Evaluation Questionnaires (SEQs) and student representatives We have continued UCL’s tradition of using SEQs as the basis of student feedback. As the Final Year blocks were extended to 16 weeks, we added an SEQ at 4 weeks as an “early warning” mechanism and identified some issues with allocation of supervision and access to IT. Student reps proved invaluable in identifying “exceptions” such as an absent placement lead at one site and persisting issues with the allocation of students to F1 doctors at another. 3 DGH site visits: The cycle of visits - before starting assistantships, within 3 months of starting and after one year. All sites are visited by Sub Dean Final Year +/- Deputy Lead and each site was encouraged to develop local mechanisms to achieve the goals of the new Final Year and assistantships. These were informal and developmental visits. Student feedback was discussed in detail and innovations noted and shared. End of year action plan for each DGH: At the end of academic year 2010-11, all DGH tutors were sent an “end of year report”, highlighting their strengths and a list of actions (if any) for improvement. Ongoing cycle: The process of team meeting, input from the Foundation School, visits and data collection from SEQs, student reps is now undergoing its second cycle. GP assistantships: All students now undertake a GP Assistantship in their final year. Quality assurance for this programme is undertaken using the same mechanisms described for community based teaching. This course has a dedicated management team who carefully assess practices before allocating any students and closely monitor student feedback. Any concerns arising with individual practices are responded to promptly. All GPs involved in supervising the Final Year GP Assistantship are invited to an annual Year 5 GP Workshop and our annual conference for all UCL GP Tutors. Domain 3 - Equality, diversity and opportunity 3. How are you meeting your equality and diversity requirements set out in Domain 3 of Tomorrow’s Doctors 2009, specifically in relation to your duties under the Equality Act 2010? Criteria no. 4. 57: We adhere to UCL’s policy on equality of opportunity (ref: http://www.ucl.ac.uk/academic-manual/part-1/equalities-and-diversity) 58: Regular training course are available for staff on equality and diversity issues. 59: Reasonable adjustments are made for all students with both permanent and temporary disabilities. The main mechanism for this is through student support cards, which allow students to gain a degree of control over the request for reasonable adjustment. For details see A-Z Policies & Regulations for Student Support (Doc. 10). 60: Data about equality and diversity issues are routinely collected by UCL. 61: Changes to policy and practise are made through established administrative mechanisms. 62: See policies. 63-70: These criteria are all met through the above mechanisms. Do you have problems meeting your data requirements? We don’t have any problems accessing the required data. 4 5. What reasonable adjustments did you make in the last academic year and how did you make them? Please only provide examples of any adjustments that the school didn’t make in previous years. The bulk of reasonable adjustments made in the last academic year were for student assessments and were based on information received from UCL disabilities office. Over 50 reasonable adjustments were made for written papers, the majority being for dyslexia. 20 reasonable adjustments were made for OSCEs, the majority being for visual impairment. In addition, 10-12 new student support cards were issued for students with both permanent and temporary disabilities. The mechanism for issuing these cards is through the student support tutor team. 6. If any requests were refused, please briefly outline the reason for refusal. Please also include cases where student progression was refused on the grounds that a student would be unable to meet the outcomes required for graduation. Only two requests were refused, both Final Year students. A student with OCD was allowed 10 minutes extra per hour for written papers and had their OSCEs scheduled for afternoons on the grounds that the students found it had to “get going” in the mornings. However, the student also requested at least one day recovery time between the two OSCEs and this was felt to be unreasonable. The student appealed to UCL’s grievance panel that insufficient allowance had been made for her condition, but the appeal was turned down. A student with SLE also requested both central placements for the OSCEs and a day for recovery between the two OSCEs. Both requests were turned down and the student was happy with the explanation for this decision. Domain 4 - Student selection 7. If the selection tools or how and when tools are used in the selection process have changed since the last academic year please can you explain these changes in the box below We have not made any significant changes since last year to the selection tools used. 8. If the School has a specific approach to admissions that is aimed at students from backgrounds where participation in higher education and medicine is low please indicate how this differs from the standard admissions route (please tick all that apply) (please see 10f of the guidance document for further information). NB: Please only include information that relates to the selection process, not activity that precedes this. Standard Adjusted admission grade route only requirements for low participation groups Guaranteed interviews for low participation groups Extended degree / foundation year for low participation groups Ring fenced Other places for low participation groups 5 9. If ‘other’, please provide a brief explanation. N/A 10. When completing the Student Profile and Progression Data forms in section B please give a brief description of the nature of what you are returning for the following fields: a. Widening Participation (e.g. students from low participation groups or students who were admitted via a specific widening access route) We do not offer a specific widening access route, but contextual data for all applicants is considered, where available, as part of the overall assessment of UCAS applications. b. UK Transfer (e.g. students from X medical school as part of an established arrangement) The majority of our transfer students are taken under an established arrangement with Oxbridge (MOCAG) in order for their students to come to UCL and complete their clinical training. There are also a small number of students who have transferred into UCL from other UK medical schools in order to undertake their clinical training at UCL. c. International Transfer N/A 11. For the 2011/12 intake, please state how many of the applications received can be identified as from low participation groups and, where possible please indicate which alternative route and or adjustment was applied. The majority of information relating to low participation groups and contextual data associated with applications is analysed centrally by UCL and is not available to the Medical School at this time. 12. And of these, how many were accepted; again where please indicate which alternative route or adjustment was applied? See answer to Q11. However we do know that approximately 60-65% of our accepted students are from state schools, which reflects the proportion applying. 13. Please describe below the steps the school is taking to mitigate the impact of financial factors on initiatives aimed at widening participation (see guidance document 10h for background information). This will be handled centrally by UCL rather than by the Medical School. Information regarding the bursary plans UCL is formulating can be found online at: http://www.ucl.ac.uk/prospective-students/undergraduate-study/tabs/fees-and-costs/2012site 6 Domain 5 - Design and delivery of curriculum including assessment Assessment Systems Curricula Processes 14. Please use the below table to update us on any changes that have taken place within the school regarding processes, curricula and assessment systems in the previous EAR. Changes The Medical School’s organisational structure at UCL has recently changed to become a discrete division within the newly-formed Faculty of Medical Sciences. For the first time, this new structure combines the academic management of the MBBS (formerly through the Division of Medical Education) and the administrative structures (formerly Medical Student Administration). X We are launching a new curriculum in 2012/13 in all years and therefore we are currently reviewing all structures, documents and processes concerning the curriculum and assessment. X Please find attached 1) New Curriculum Document (Doc. 11) – draft curriculum management structures (awaiting approval) and 2) MBBS Programme Specification 2011-12 (Doc. 12) - overall outcomes and overview of the new MBBS. The teaching and learning strategy and programme specification are currently being reviewed to reflect the new management structures and to reflect the vision and planned delivery of the new curriculum. These documents will be finalised via the appropriate committees in January 2012. X We have introduced SBA paper to Year 2 and blueprinted both Year 1 and 2 assessments more closely to the curriculum. In Year 3, we have introduced an on-line, formative SBA in February. In Year 4, we are improving blueprinting of all of the assessments Domain 6 - Support and development of students, teachers and the local faculty 15. What trends, if any, has the School identified in student professionalism and fitness to practise concerns and cases? We assess professionalism and fitness to practise both in-course and during assessments. The majority of concerns raised during assessments are related to poor attitude or communication skills. The majority of concerns raised during the course are related to poor attendance. We have noted an increase in FtP cases over the last 5 years, partly as a result of greater number of students entering Medical School with CRB declarations or with ongoing health problems. 7 16. Are you informed about the fitness to practice of Foundation Year 1 doctors and if so, who informs you? Yes, the Dean of the relevant Foundation School informs us (most commonly NCTFS for our students). 17. Do you hold fitness to practise hearings for Foundation Year 1 doctors? Yes, rarely. 8 Additional questions 18. In the 2010/11 EAR you gave details of the training hours of your training programmes. If anything has changed please can you update the table below: Programme length No changes Year / Phase No changes Theoretical training (hours) No changes Practical training (hours) No changes 19. If your School has used the GMC supplementary guidance please can you give examples on how it has been used to improve school policy and processes? e.g. for Public Patient Involvement Clinical placements for medical students: The supplementary advice on clinical placements was used to help review our assistantships – it came too late to contribute to the introduction of the new Final Year programme but reassured us that we were exceeding expectations. The examples of good practice embedded within the text were useful as were the specific statements regarding indemnity. Assessment in undergraduate medical education: We are restructuring our Years 1 and 2 assessments in line with this guidance. This year, we have reduced the number of essay questions and next year they are going to be replaced altogether. Last year we stopped doing any vivas. Also we are currently looking into how to provide students with better feedback from their assessments. We hope to be able to provide them with details of their score compared to their peers. Finally we are trying to develop an online training session for assessors. This will include practice stations to mark, and a detailed description of their role. All new assessors will need to have completed this before being allowed to assess. Patient and public involvement in undergraduate medical education: The supplementary advice on PPI is a very thorough document and provided an excellent bibliography for our own PPI Project (see question 43b) although again the final version came a little late for us. It revealed that very little work has been done on the lay perspective of PPI in medical education especially regarding input into quality assurance and governance. The examples in the annex were very rich but a bit indigestible – might have benefited from some editing and a clearer index for easier reference. UCL Medical School has been working with GMC to look at how guidance might be operationalised. 9 20. Please tell us about any risks or challenges related to the implementation of Tomorrow’s Doctors 2009. The first row is an example Domain / Standard What is the risk / challenge and what action is taking place (if applicable)? Domain 3 TD 60 Risk: The school does not collect its own equality and diversity data and relies on the University to highlight issues as and when they arise. Action: We have developed an information sharing agreement that means the school receives equality and diversity data at the start of the new academic year. Domain 2 TD43 Challenge: Obtaining data from other education providers, evaluation data from patients and employers, as well as obtaining patient feedback on interaction with medical students, and evidence of change effected because of evaluation. Involving patients in meaningful ways in curriculum planning and review is difficult Action: Last year we had two important pilots: the PPI Beacon Project and the Preparedness for Practice study at Basildon (B&TUHNFT). We intend to reflect upon these pieces of work with a view to building more comprehensive systems for the routine capture of data from other stakeholders. Domain 5 TD 91 Challenge: Curriculum map Domain 6 TD 122 Challenge: Human resources, in terms of creating an integrated curriculum and increasing the number of small group work opportunities and personal tutors. There is a limit to the SIFT monies; traditionally curricula were designed in a less integrated fashion (i.e. about placements in the latter years), so as we create a very integrated course we run out of SIFT monies to pay clinicians to become heavily involved in Years 1 and 2. The fix of HEFCEt income at faculty level as part of the UCL management of the deficit, together with the long anticipated changes to SIFT, mean that it is hard to get people to take on new, time- consuming activities with no obvious increase of income Action: After much investigation and research, UCL Medical School has decided that curriculum mapping is going to be best sited within its virtual learning environment, rather than on a bespoke piece of software. This is ongoing and its progress closely linked to the new curriculum project. Action: Increasing individualised support for students in a climate of financial stringency is always going to be an issue. Mechanisms are being developed to ensure greater financial transparency and support for high quality education. These innovations have included the educational quality levy and innovation fund. We also maintain a risk register as part of the implementation project; it is mainly linked to finance issues. 21. Please identify any innovations the School is piloting or potential good practice that it would like to report, particularly successes or effective actions taken in implementing Tomorrow’s Doctors 2009 to potentially share with other schools Domain Example of Good Practice Quality assurance This year we have developed a system for students to report concerns to us. This has involved collaboration with the student body, welfare, quality and administrative teams: http://www.ucl.ac.uk/medicalschool/quality/raising_student_concerns We have developed and are piloting a self-assessment exercise for trusts. This will be helpful in identifying good practice as well as to 10 set a trust developmental plan for the subsequent year and permit the QAU to target their visits to areas of need. We have developed a set of standards for clinical teachers and reviewed and updated the information we provide about involving patients in medical education Teaching/learning/assessment Medical Education Conference and seminar series Extended patient projects and Patient Pathways E learning Formative feedback in Years 1 and 2 and case of the month – a case based on line exercise for Final Year students which has tutor input and feedback Lecture-casting and e-portfolio project being piloted Standards for IT and WiFi access on clinical placements Project: Patient and Public Involvement in assistantship design/evaluation Patient involvement As part of a larger project looking at PPI in the Medical School, patients, advocates and PPI representatives were asked about consent for involvement in assistantships and/or particular procedures, and about providing feedback to students. There was widespread endorsement from patients about being involved in students’ education - in real settings and with real patients – including permitting students to undertake procedures, providing that the students gained clear consent, supervision and guidance was provided. Patients are happy to give more direct advice and feedback to students they have had contact with but are a little wary of potentially hurtful or prejudiced comments. Our participants had less of an appetite for direct involvement in curriculum design and evaluation. 22. Throughout this return we have asked for examples of good practice and examples of how schools have used GMC guidance to improve their practices and processes. We would like to conduct case studies on successes, if you would like your school to be considered as case study please check the following box: Deadline: Thursday 1 December 2011 for: Section A (Word) – MSAR qualitative questions Section B (Excel) – Up to five worksheets If you have any queries about any aspect of the MSAR, please contact Nick di Paolo or another member of the quality team in the first instance at quality@gmc-uk.org, 020 7189 5479. 11