(i) Planning and consent for
advertisement

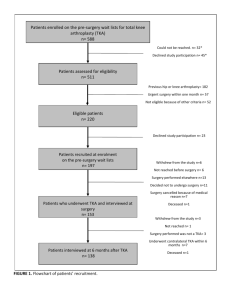
MINI-SYMPOSIUM: THE KNEE fracture.1e4 In this article we will discuss the important factors to consider in careful pre-operative planning in order to obtain successful surgical outcomes. We will then go on to discuss the principles of patient consent and describe how to obtain informed consent for TKA surgery. Knee joint arthroplasty is performed to reduce knee pain, improve function and to improve quality of life.5 In order to obtain the best surgical results the surgeon must perform an adequate pre-operative work up including appropriate patient selection, pre-operative medical assessment, clinical and radiological examination of the limb, selection of an appropriate prosthesis and adequate patient counselling about the operation. (i) Planning and consent for primary total knee replacement Donald J Davidson Susannah G Clarke Chinmay M Gupte Abstract Pre-operative clinical evaluation and assessment The aim of primary total knee replacement is to decrease pain, restore function and reduce disability. This is achieved by correct patient selection and adequate planning so that the appropriate prosthesis can be implanted in the appropriate manner. The technical goal of total knee arthroplasty is to implant a well-aligned prosthesis in a well-balanced knee, with linear patellar tracking and achieve infection-free healing. Weight bearing anteroposterior, lateral and patellofemoral joint radiographs are mandatory and standing long leg views help determine alignment. CT and MRI scans may be of value in assessing bone stock and ligamentous deficiency. If there is a lack of bone stock a stemmed prosthesis or augmentation wedges may be required, whilst a ligamentous deficiency may necessitate a stabilized or constrained prosthesis. The consent process for TKR commences at the outpatient consultation and must consider the reason for operation, alternative treatments, all common and serious risks and the rehabilitation protocol. There is an increasing use of multimedia tools (e.g. www.orthoconsent.com) in the consent process. History An adequate history is the key to patient selection. This should include a thorough assessment of pain (including rest pain and night pain) and disability (including walking distance, stair disability and leisure/occupational restriction). Previous treatments should be established including steroid injections (which increase the risk of infection), physiotherapy and operations such as arthroscopy or osteotomy. A past medical history of concomitant conditions such as diabetes, hypothyroidism, and immunosuppression may necessitate blood investigations prior to the procedure.6 A drug history should determine whether the patient is on warfarin, immunosuppressant therapy or diabetic medication. An allergy to nickel or metal may necessitate allergy testing as a non-cobalt chrome prosthesis (e.g. zirconium) may be required. The patient’s social history may determine post-operative rehabilitation and length of hospital stay, especially if they have little social support or live in a property with many stairs. With the growing volume of TKA surgery there has been a rise in multidisciplinary integrated peri-operative care pathways; these pathways aim to enhance the recovery of patients undergoing elective primary TKA by identifying and anticipating challenges likely to hamper the successful outcome of the operation.7 These pathways include thorough medical, nutritional and social circumstance assessment which, coupled with patient education, has been demonstrated to reduce pre-operative patient anxiety and improve post-operative outcome including shortened hospital stays, reduced morbidity and reduced mortality.7e9 These peri-operative clinics also permit patient information capture for joint registries and functional assessment scoring. Keywords consent; planning; pre-operative; primary total knee replacement; TKA Introduction With over 72 000 primary total knee replacements performed every year in the UK, primary total knee arthroplasty (TKA) is a common, but technically demanding surgical procedure that requires careful pre-, intra- and post-operative consideration. TKA surgery generally has excellent results with long prosthesis survival rates of 15e20 years and improved quality of life, but serious complications do occur in approximately 5% of cases due primarily to loosening, infection, instability, dislocation and Contraindications to primary total knee replacement The absolute contraindications to TKA include local or systemic infection, extensor mechanism discontinuity or severe dysfunction, recurvatum deformity secondary to muscular weakness and the presence of well-functioning knee arthrodesis.10 Relative contraindications include significant peripheral vascular disease, a Charcot joint and dermatitis within the operative field.10 Patients with pre-existing obesity and diabetes require special consideration prior to TKA. The prevalence of obesity is increasing and is linked to osteoarthritis, especially affecting the knee joint. Evidence shows that the outcome for morbidly obese (BMI >40) patients post primary TKA can be successful, but they suffer from higher rates of peri-operative complications and do Donald J Davidson MA (Cantab) MBBS MRCS Specialist Registrar, Trauma and Orthopaedics, Imperial College NHS Trust, St Mary’s Hospital, Paddington, London, UK. Conflict of interest: none. Susannah G Clarke MA (Cantab) MEng PhD Research Doctor, MSK Laboratory, Charing Cross Hospital Campus, Imperial College London, UK. Conflict of interest: none. Chinmay M Gupte MA (Oxon) BMBCh PhD FRCS (Tr&Orth) Consultant Orthopaedic Surgeon and Senior Lecturer, Imperial College NHS Trust, St Mary’s Hospital, Paddington, London, UK. Conflict of interest: none. ORTHOPAEDICS AND TRAUMA 27:6 345 Ó 2013 Elsevier Ltd. All rights reserved. MINI-SYMPOSIUM: THE KNEE not go on to lose weight after knee arthroplasty.11,12 Patients with Diabetes Mellitus have an increased risk of postoperative deep infection due to immune dysfunction and there is evidence to support the use of antibiotic impregnated bone cement in primary TKA to reduce this risk.13 may subsequently require the consideration of using a constrained TKA system. Inspection: joint angular deformity (especially varus or valgus) should be identified and then assessed clinically to determine if it is correctable. If it is not passively correctable, plans for soft tissue release during surgery should be made, or in severe cases, a constrained prosthesis should be available. It would also exclude a unicompartmental knee replacement even if only one knee compartment is affected.21 Femoral or tibial bowing should be noted and warrants further radiological assessment (a full length leg AP). Surgical scars should be noted and are evidence of previous surgery (e.g. high tibial osteotomy or trauma) which can impact upon the operative plan. The location of existing surgical scars affects where a new incision can be sited (the vascular supply to the skin anterior to the knee joint runs from medial to lateral). Ideally, a 7 cm skin bridge between incisions is advisable or the most lateral pre-existing vertical scar should be re-incised. If a transverse scar is evident the incision should be made perpendicular to this. If unsure, plastic surgical input is vital and consideration should be made to performing a sham incision prior to the definitive arthroplasty surgery. Clinical and radiological examination of the limb Thorough pre-operative planning permits the anticipation of many intra-operative challenges necessary to achieve accurate prosthetic seating, thus improving surgical technique. Suboptimal technique is a known risk factor for early prosthetic failure.14,15 The technical goals necessary to achieve a successful outcome in primary TKA surgery are16: Restoration of the neutral mechanical alignment of the limb The objective is to achieve a neutral mechanical alignment where the forces pass through the centre of the hip, knee and ankle joints. This permits equal load sharing across the prosthesis thus preventing excessive stress on either side leading to accelerated wear and early failure.17 Preservation (or restoration) of the joint line By the end of the procedure the joint line must be recreated at its original position taking into account any cartilaginous or bony erosion secondary to the arthritic process. Restoration of the joint line is important as it means peri-articular knee ligaments are correctly tensioned which is essential for prosthetic knee kinematics.18 Balancing of the peri-articular ligaments Over the course of the disease progression ligaments may become scarred and contracted or lax owing to a progressive articular angular deformity. It is long established that correct ligamentous balance is necessary to provide optimum function and wear of the prosthesis.19 Simplistically, ligaments on the concave side of the joint need releasing and those on the convex side tightening. Balancing must be achieved in both the coronal and sagittal planes. The goal in sagittal balancing is to achieve an equal flexion and extension gap, taking into account the two radii of curvature in the knee; the first at the patellofemoral articulation and the second at the weight bearing portion of the knee. Maintenance (or restoration) of linear patellar tracking and a normal Q angle Abnormal patellar tracking is the most common complication of TKA.20 The Q angle, the angle between the axis of extensor mechanism and the axis of the patellar tendon, is normally 11 þ/ 7 .20 An increased Q angle leads to lateral subluxation forces on the patella relative to the trochlear grove, which can lead to pain, mechanical symptoms, accelerated wear and even dislocation. Common intra-operative errors include internal rotation of the femoral or tibial prosthesis, medialization of the femoral component and placing the patellar prosthesis lateral on the patella. Joint range of motion: the pre-operative range of motion of the knee should be assessed and recorded, as there is a positive correlation between pre and post-operative movement range.22 Identification of a fixed flexion deformity will impact upon the surgical strategy possibly necessitating, depending on severity: the excision of the posterior osteophytes, posterior capsular release, posterior cruciate ligament (PCL) release and distal femoral resection (cadaveric studies demonstrate that a 2 mm distal femoral resection can give 10 of further extension).23,24 Assessment of ligaments: the integrity of the ligamentous structures of the knee must be assessed and further knee imaging may be warranted. An incompetent PCL is a contraindication to a cruciate retaining prosthesis and a competent anterior cruciate ligament (ACL) is essential if a unicompartmental knee replacement is to be considered. The integrity of the collateral ligaments is also essential for a non-constrained TKA design to be utilized and if there is any concern a constrained system should be available at the time of surgery. Radiological evaluation A detailed pre-operative radiographic assessment of the knee joint is essential to confirm the diagnosis, the severity of disease and to adequately plan TKA. The standard radiographic views include a standing anteroposterior (AP) of both knees, extension and flexion lateral of the affected knee and a tangential axial of the patellofemoral joint (typically a Merchant view but other alternatives include a skyline patellar view). Whilst a standing AP radiograph of the lower extremity (hip to ankle joint) is preferred, this is not routine in many orthopaedic centres, but is obligatory if there is: Obvious clinical deformity of the femoral or tibial shaft, Altered ipsilateral hip/femoral neck/shaft anatomy (e.g. from dysplasia, trauma, infection, previous operation), Extremes of height. Clinical assessment of the knee joint Crucial information necessary to pre-operatively plan TKA can be gathered in the clinic room. The affected knee, the ipsilateral hip and ankle, as well as the contralateral knee, should all be thoroughly examined. Gait assessment: evidence of a thrust gait is indicative of ligamentous laxity and warrants careful radiological assessment and ORTHOPAEDICS AND TRAUMA 27:6 346 Ó 2013 Elsevier Ltd. All rights reserved. MINI-SYMPOSIUM: THE KNEE The AP, lateral and Merchant radiographs will also demonstrate the presence of osteophytes, bony defects, loose bodies or deformities, which may require intervention during surgery. The position of osteophytes should be noted, as osteophyte excision is the first step in achieving ligamentous balance both in the coronal and sagittal planes. Pre-operative identification of the nature of the deformity allows the formulation of a sequential surgical plan to tighten the convex side and release the concave side of the joint until equilibrium is restored. The joint line can also be determined in the AP view which is important for balancing the flexion and extension gaps and the ligaments. If a varus thrust gait is evident and varus deformity is also present on weight bearing AP radiographs then a standing single leg AP radiograph is recommended to identify the presence of lateral ligament laxity. In this instance a constrained system should be made available at the time of surgery as instability problems are likely to be encountered during balancing and trialling.25 Radiographic evidence of previous surgery (e.g. high tibial osteotomy) will be apparent and intra-operative management must be considered pre-operatively. Supplementary radiographic views may be also indicated, including tunnel or Rosenberg views, which are useful to detect early joint space narrowing of the posterior weight bearing surfaces, osteochondritis dissecans in young patients, intra articular loose bodies and osteophytes projecting into the intercondylar notch. Additional imaging modalities can be indicated, including a CT and MRI, in the context of complex primary TKA post trauma or dysplasia, altered bone stock (Figure 1) and also for patient-matched instrumentation. The analysis of this radiographic survey gives valuable information for the formulation of an operative plan, namely the25: Determination of the femoral and tibial end cuts and cut angle, Position of the femoral canal entry point, Anticipation of ligamentous release, Identification of bone defects, joint subluxation or ligamentous laxity, Templating of prosthetic components. AP radiograph, to confirm and assess severity of knee pathology: the weight bearing AP radiograph (Figure 2) is used to confirm the involvement and severity of the arthritic process in the medial and lateral tibiofemoral joint compartments. When weight bearing, the radiographic joint space represents the thickness of the articular cartilage and is pathological if less than 3 mm.26 On review of the AP, in conjunction with the lateral and Merchant views, it is possible to confirm which of the joint compartments are affected and the decision to opt for either a primary TKA, unicompartmental arthroplasty, isolated patellofemoral arthroplasty or high tibial osteotomy can be considered. Lateral flexion and extension radiograph: the lateral radiographic (Figure 3) views have a role in disease confirmation and severity assessment. Additionally, in this view the suprapatellar region can also be evaluated for the presence of a joint effusion or loose bodies. Evidence of anterior tibial subluxation and/or posteromedial tibial wear on the lateral radiograph is indicative of an ACL injury and would be a contraindication to unicompartmental arthroplasty. If PCL insufficiency is suspected, a lateral kneeling Figure 1 This radiographic case study highlights the role of CT scanning in planning a left complex primary TKA (post gunshot wound). Images: (a), (b) and (d) are the pre-operative radiographs of the left knee; (c) is a sagittal image from the pre-operative planning CT scan demonstrating marked bone loss, leading to preoperative planning of a stemmed prosthesis and wedges if required at the time of surgery. However, after trialling, a standard prosthesis was implanted (e). ORTHOPAEDICS AND TRAUMA 27:6 347 Ó 2013 Elsevier Ltd. All rights reserved. MINI-SYMPOSIUM: THE KNEE intra-operatively, can cause loss of flexion and impingement pain. The patellar height can be described using the ratio of patellar tendon length to the greatest diagonal patellar length; a ratio greater than 1.2 is considered patella alta and less than 0.8 is considered patella baja.27 Tangential axial view of the patellofemoral joint: the Merchant view (Figure 4) is the most commonly used tangential axial view of the patellofemoral joint and, as already described, allows evaluation of the patellofemoral joint arthritis.28 The alignment of the patellofemoral joint can be assessed allowing the presence of pre-operative patellar subluxation to be identified and intraoperative lateral release to be considered.14 The role of the full length leg radiograph in achieving mechanical alignment: with the standing full length leg AP radiograph (Figure 5) it is possible to determine the anatomical and mechanical axes of the tibia and femur and determine where the bone cuts should be made to correct any malalignment. The femoral anatomic axis (Figure 6) is the line that bisects the intramedullary canal of the femur and typically exits the femur inferiorly through the intercondylar notch. The exit point determines the entry point for the intramedullary rod of the femoral jig used to prepare the femur during TKA. With femoral deformity the exit point of the axis can migrate away from the intercondylar notch in the coronal plane and this must be established preoperatively. The mechanical axis of the femur is the line connecting the centre of the femoral head to the point where the femoral anatomical axis intersects the intercondylar notch. The difference between these two axes determines the valgus cut angle (VCA) for the preparation of the distal femur. By setting the VCA on the femoral guide it is possible to make the distal femoral cut perpendicular to the femoral mechanical axis. The VCA is typically between 5 and 7 , decreasing with patient height. The anatomic axis of the tibia (the line bisecting the medullary canal) is, in the majority of patients, coincident with the tibial mechanical axis (the line from the centre of the proximal tibia to the centre of the ankle). Therefore, when the proximal tibial cut is made perpendicular to the anatomical axis it is also perpendicular to the mechanical axis thus permitting even loading through the tibial component. The proximal tibial cut can be made with reference to either an intramedullary or extramedullary tibial guide and they are equally efficacious.29 In the presence of a tibial bowing deformity (e.g. congenital or post trauma) the bowed tibia may not permit placement of the intramedullary guide; this must be established pre-operatively. Note that with tibial bowing the anatomical and mechanical axes can be disparate. The tibial joint line is typically 3 of varus compared with a perpendicular subtended from the mechanical axis (i.e. 87 ) (Figure 7). If not addressed, after the tibial cut there would be an unequal (unbalanced) trapezoidal flexion gap created due to the unparallel tibial and posterior femoral cut surfaces causing an increased lateral joint space. In order to equalize the flexion gap, the femoral component is placed in 3 of external rotation, thus compensating for the increase in lateral joint space. This has the additional benefit of improving patellar tracking by reducing the Q angle. The standing full length leg radiograph will also determine if there is varus or valgus alignment of the knees; this allows the Figure 2 AP radiographs of the knee joint (weight bearing and non-weight bearing). Note the partial loss of joint space in the medial tibiofemoral joint compartment which is complete in the weight bearing radiograph (on the right). stress radiograph will demonstrate this. Excessive fixed flexion both clinically and in the lateral view is evident in PCL tightness and prompts consideration of a PCL sacrificing prosthesis. The patellar height can be ascertained on the lateral radiograph. The presence of a patella baja which, if not addressed Figure 3 Lateral radiograph of the knee demonstrating reduced joint space, fixed flexion, osteophytes and subchondral sclerosis. ORTHOPAEDICS AND TRAUMA 27:6 348 Ó 2013 Elsevier Ltd. All rights reserved. MINI-SYMPOSIUM: THE KNEE surgery so that intra-operatively the correct implant sizes are available.31 It has been shown to be cost effective and presumed to shorten the surgical time.32 Various acetate and digital templating techniques have been investigated and the results are similar; the accuracy of predicting actual component size to within one size above or below is 90e95%.31 Templating based solely on patient characteristics (age, gender, height, weight and body mass index) has been shown to be more efficacious compared to all other radiographic templating techniques.31 Figure 4 Tangential axial view of the patellofemoral joint demonstrating bilateral loss of joint space and subchondral sclerosis. anticipation of the intra-operative ligament release for coronal balancing as described previously. Significant valgus deformity is associated with lateral femoral condyle hypoplasia which should be anticipated as, in this instance, posterior axis referencing would result in the placement of the femoral component in an internally rotated position. If severe extra-articular angular deformity (>10 in the coronal plane and >20 in the sagittal plane) is evident, simultaneous osteotomy and TKA should be planned, as in this instance attempted joint line restoration can result in complex imbalance of the collateral ligaments.30 Patient-matched technology: the advent of 3D printing as a cost effective method of manufacture has allowed the introduction of customized instrumentation for TKA. All major orthopaedic companies now offer a customized pre-operative planning and instrumentation service. Pre-operative planning is undertaken on CT or MRI scans; 3D models are constructed from the imaging data. The scan must include the ankle, knee and hip. To reduce radiation dose, specific protocols may be set up-to include only the required areas. From the 3D models, bony landmarks at the ankle, knee and hip are located and used to provide the mechanical axis reference frame for the lower leg. Default sizing and positioning of the total knee implants in accordance with manufacturer recommendations can be made with reference to the mechanical axes of the femur and tibia. Interactive planning software allows variation of implant position and orientation to accommodate each patient’s specific needs. The pre-operative plan is used to create custom instrumentation for the patient. The custom instrumentation is manufactured using one of a number of methods of rapid manufacture and will generally be made out of Nylon or a similar polymer. Depending on the manufacturer, the custom instrumentation will guide the initial tibial and femoral saw cuts, or will allow pin placement for use with re-usable metal cutting guides. The custom instrumentation is designed to provide a positive fit onto the patient’s exposed bone. A CT-based system will fit onto bone; an MRI-based system will fit onto the articular cartilage. Once designed, the custom instrumentation is manufactured, sterilized and sent to the operating theatre. This type of patient-matched technology is still in its infancy and there is not a wealth of supporting evidence to demonstrate superiority to conventional techniques. In contrast to planar radiographs, the use of 3D imaging allows a greater understanding of the case prior to surgery. Accurate placement of the instrumentation is essential to ensure correct implementation of the plan. Templating: pre-operative templating attempts to accurately determine the size of the femoral and tibial components prior to Choice of TKA prosthesis There are different designs of prostheses that can be used for primary TKA and they are categorized depending upon the level of mechanical constraint in the prosthesis. The most common primary TKA designs are divided into those which retain or sacrifice the PCL; the merits of one system over the other have been much debated.33 Beyond this are the constrained systems, either hinged (highly constrained) or non-hinged, which tend to be used for revision surgery but can also be used in the context of a complex primary TKA with ligamentous insufficiency or marked deformity. Figure 5 A standing full length leg AP radiograph the bilateral lower limbs. In this radiograph the mechanical axis of the limb (from the centre of the femoral head to the centre of the ankle joint; marked with a blue line) passes more medially through the knee joint in the left leg compared to the right. This patient had undergone a left medial meniscectomy 30 yrs earlier, leading to medial OA and varus malalignment. ORTHOPAEDICS AND TRAUMA 27:6 Cruciate retaining TKA: in the native knee, posterior glide and roll back of the tibiofemoral contact point during flexion is influenced 349 Ó 2013 Elsevier Ltd. All rights reserved. MINI-SYMPOSIUM: THE KNEE demonstrated paradoxical forward sliding with knee flexion.35 The advantages are that it is a bone preserving prosthesis, the joint line is consistently restored and post-operative proprioception is better as the PCL remains. The disadvantages are that it is harder to balance with severe deformities (Varus >10 and Valgus >15 ). PCL balance is critical for long-term wear but PCL recession is technically demanding and excessive recession can result in late PCL rupture which can cause instability of the knee.36 Cruciate sacrificing TKA: there are two types of cruciate sacrificing (CS) TKA; posterior stabilized (post and cam mechanism) and the anterior stabilized (extended anterior polyethylene lip). The posterior stabilized TKA is the most commonly used CS TKA and there are specific indications for its use including pre-existing patellectomy, inflammatory arthritis (as risk of subsequent PCL rupture) or pre-existing PCL rupture.37 The advantages of CS TKA include that it is technically easier to balance in the presence of severe deformities, as excision of the PCL increases the flexion gap by 5 mm which permits surgical access.34,38 Evidence suggests that using CS design increases post-operative knee flexion, although the difference is small (8 ) and not associated with improved function.34 There is less sliding wear debris created compared to the CR system, although wear analysis of retrieved posterior stabilized TKAs demonstrate the cam-post interface is an additional source of polyethylene debris.39 The disadvantages specific to the posterior stabilized system are that the femoral cam can jump over the tibial post if the flexion gap is too loose, scar tissue can form superior to the patella which can get caught in the cam mechanism as the knee moves into extension causing a patellar clunk. It also requires additional bone stock removal compared to the CR prosthesis to accommodate the post and cam mechanism. Figure 6 Diagram demonstrating the anatomical axis of the femur (solid red line), mechanical axis of the femur (solid blue line) and the coincident tibial mechanical and anatomical axes (dashed red and blue line). Additional TKA design decisions There are other decisions to be made pre-operatively in choosing the prosthetic design for the patient’s primary TKA. Mobile bearing TKA were developed in an attempt to decrease wear at by the PCL and is essential for deep flexion as it prevents posterior impingement.34 The advantage of the cruciate retaining (CR) TKA is that the PCL helps regulate flexion stability and PCL tension also regulates femoral roll back, although some studies have Figure 7 Left; native balanced knee with joint line in slight varus. Middle; proximal tibia is cut perpendicular to mechanical axis leaving wide lateral joint space. Right; flexion gap balanced by externally rotating femoral component 3 . ORTHOPAEDICS AND TRAUMA 27:6 350 Ó 2013 Elsevier Ltd. All rights reserved. MINI-SYMPOSIUM: THE KNEE dictated in the clinic letter), confirmed at pre-assessment and reconfirmed on admission for surgery.47 There is no UK statute setting out the general principles for consent, however case law has established that if a health professional intentionally or recklessly touches a patient without valid consent they are committing a crime of battery or a tort of trespass to the person or negligence.43,46 There is no set method established to obtain valid informed consent prior to any surgery. There are, however, generic guidance documents produced by the Department of Health and the GMC which aid clinicians who are seeking consent for medical procedures and operations. More specifically the British Orthopaedic Association (BOA) has endorsed a freely accessible website (www.orthoconsent.com) which gives orthopaedic surgeons access to a bank of pre-written procedure specific consent forms, including primary TKA, covering the procedure description, alternative procedures and the specific risks of surgery.45e47 the tibiofemoral articulation, the aim being to reduce wear by permitting the insert to slide on a smooth tibial base plate. Slight improvements in knee scores and pain have been noted, but no long-term differences have been observed and there is a dislocation rate (spin out) of the insert of 2.5%.40,41 The decision whether or not to resurface the patella during primary TKA has been debated. The results from the Knee Arthroplasty Trial, a multicentre randomized control trial, demonstrated at 5 years no benefit in resurfacing with regard to functional status, treatment cost, or quality of life, although there was a non-significantly higher re-operation rate in the nonresurfaced group compared to the resurfaced group over that time frame.42 The senior author (CG) prefers to resurface the patella in most patients. However, in the presence of patellofemoral joint wear of grade two or less, in a patient with no systemic disease (rheumatoid, hypothyroidism or diabetes) and with a well-tracking patella on trialling of the prostheses, the patella is left unresurfaced. The potential role of computer navigated surgery (CAS) should also be considered pre-operatively to aid the placement of prosthetic components. There are advantages to CAS including the calculation of soft tissue tension to perfectly balance the knee, the accurate restoration of the mechanical alignment, reducing blood loss and fat embolism, but there are also disadvantages including prolonged operation time, higher costs and lack of long-term evidence of benefit.2 A recent review of CAS demonstrates that it improves the alignment of the components, but there is no demonstrable improvement in outcomes; its role may be in complex primary and revision TKA.2 Specifics of consent Who should take consent? The responsibility for the taking of consent for TKA surgery falls on the operating surgeon. If it is not practical for the operating surgeon to take the consent, they can delegate this role to a suitably trained and qualified person with sufficient knowledge of the proposed operation and who understands the risks involved and the principles of consenting patients as outlined in the GMC guidance.45 If this role is delegated the operating surgeon is still responsible for ensuring that the patient has had sufficient time and information to make an informed decision and that the patient has given their informed consent before commencing the operation. Consent for primary TKA Principles and legal background The consenting process for a TKA, as for any procedure, is a dialogue between the patient and the surgeon culminating in the patient giving permission for the operation to be performed. In order to give consent the patient must have intellectual capacity, be acting voluntarily and be broadly aware of the nature and purpose of the treatment.43 The process of obtaining informed consent involves explaining the salient features of the procedure, describing any alternative therapies (including any conservative management), describing the risks of the procedure, answering any relevant questions and asking for the patient’s written permission to proceed to surgery.44,45 The decision to consent is not binding and the patient still has the autonomy to withdraw that consent at any point.46 Guidance from the General Medical Council (GMC) encourages orthopaedic surgeons to work in partnership with their patients and discuss with them, in a way they understand, their medical condition and the intended operation. Patient autonomy must be respected allowing the patient to make their own informed decision regarding their care.45 Consent can be written, verbal or implied, but for a significant operation, such as a TKA, written informed consent should be obtained.45,46 It is, however, worth bearing in mind that signed written consent can be invalid if the consenting process is inadequate.43 Obtaining informed consent is a continuous process; it is recommended that consent should be taken in clinic at the point the patient is placed on the operating list (preferably ORTHOPAEDICS AND TRAUMA 27:6 What should be discussed? In the process of obtaining informed consent for a primary TKA the surgeon must do the following: introduce themselves and describe their role in the management of the patient, inform the patient of their knee pathology and the likely disease progression, the management options including non-operative treatments, the potential risks and benefits of the procedure, explain to the patient their right to refuse the operation or seek a second opinion.45 If the procedure is being performed in the private medical sector, the cost of any procedure must also be discussed as should any potential conflict of interest which may impact patient care.45 This conversation should be tailored depending on the specific needs and concerns of each individual patient. The surgeon can augment this discussion with written or any other up-to-date multimedia material. Patients should also be consented for their data to be collected for the National Joint Registry database. Risks of surgery The risks of TKA surgery must be clearly and accurately explained in a way the patient understands in order to make an informed decision.45 The risks should be presented in a balanced fashion and include the side effects of having a TKA, the potential complications of surgery and the potential failure of the TKA to achieve the desired outcome.45 When assessing the risk of surgery the patient’s specific co-morbidities must be considered and the patient specific surgical risks should be explained.45 351 Ó 2013 Elsevier Ltd. All rights reserved. MINI-SYMPOSIUM: THE KNEE Complication rates (BOA consent form, literature and joint registries) Complication BOA consent form rate (%) Joint registry/literature rate (%) Pain 2e5% Dissatisfaction Bleeding necessitating transfusion Blood vessel damage Revision Knee stiffness e 2e5 <1 e 2e5 Prosthesis wear Infection Deep vein thrombosis Pulmonary embolism Myocardial infarction Death Nerve damage Bone damage (fracture) 2e5 1e2 2e5 <1 e <1 <1 <1 Altered wound healing Joint dislocation Leg length discrepancy <1 <1 <1 1 month: 44.4; 3 months: 22.6; 6 months: 18.4; 12 months: 13.1 14e19 15.1 0.08e0.17 6.6 1.3e5.3; necessitating manipulation under anaesthesia: 2 Necessitating revision: 7e15 1.6 Symptomatic 1.8; asymptomatic 38.1 0.7e0.81; fatal 0.15 0.4 0.5 Peroneal 0.3; overall 1.3 Supracondylar fracture: 0.3e2.5; patellar fracture: 0.05e21; tibial fracture: rare e 0.5 e Table 1 Conclusion Contrary to the widely held belief that the patient should only be informed of risks of >1%, patients must be informed of any serious adverse outcome from the operation, even if they occur infrequently, and they should also be informed of less serious frequently occurring risks. The GMC describe a serious adverse outcome as, “an outcome resulting in death, permanent or longterm physical disability or disfigurement, medium or long-term pain, or admission to hospital; or other outcomes with a longterm or permanent effect on a patient’s employment, social or personal life.” The table above lists the clinically significant complications of primary TKA surgery and compares the complication rates listed on the BOA validated consent forms with those published in the literature and from joint registry data.44 (Table 1) Primary TKA is a successful operation but one which requires careful pre-operative planning to achieve the best outcome. Adequate pre-operative planning for primary TKA includes appropriate patient selection for the operation, clinical and radiological evaluation of the limb, pre-operative medical assessment, selection of an appropriate TKA prosthesis and adequate patient counselling about the operation, which culminates in the patient providing written informed consent for surgery. A REFERENCES 1 National joint registry of England and Wales. 9th annual report, 2012. http://www.njrcentre.org.uk/NjrCentre/Portals/0/Documents/England/ Reports/9th_annual_report/NJR%209th%20Annual%20Report% 202012.pdf. Accessed August 27, 2013. 2 Desai AS, Dramis A, Kendoff D, Board TN. Critical review of the current practice for computer-assisted navigation in total knee replacement surgery: cost-effectiveness and clinical outcome. Curr Rev Musculoskelet Med 2011; 4: 11e5. 3 Ethgen O, Bruyere O, Richy F, Dardennes C, Reginster J-Y. Healthrelated quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J Bone Joint Surg Am 2004; 86-A: 963e74. 4 Harris WH, Sledge CB. Total hip and total knee replacement (2). N Engl J Med 1990; 323: 801e7. 5 Singh JA. Epidemiology of knee and hip arthroplasty: a systematic review. Open Orthop J 2011; 5: 80e5. 6 National Institute for Health and Care Excellence. Preoperative tests the use of routine preoperative tests for elective surgery, CG3. London: National Institute for Health and Care Excellence, 2003. Litigation relating to primary TKA With the growing litigious culture in orthopaedic surgery, especially lower limb arthroplasty, insufficiency in the consenting process is a common source of legal complaint.48 The volume and cost of litigation claims relating to TKA is rising significantly.49 By reviewing the National Health Service Litigation Authority database of claims made relating to TKA, it is clear that the litigation success rates are higher when involving technical errors, but a large number of claims brought (39%) related to poor patient reported outcome.50,51 The mismatch between patient expectation, informed consent and outcome is at the core of many claims and often centres on the fact that the patient feels they were not properly counselled regarding the risks and potential complications of the procedure.48,49 Errors, insufficiencies and omissions in the provision of information relating to forthcoming TKA surgery leads to confused patients and puts orthopaedic surgeons and health trusts at risk of litigation and must be remedied prior to surgery.47 ORTHOPAEDICS AND TRAUMA 27:6 352 Ó 2013 Elsevier Ltd. All rights reserved. MINI-SYMPOSIUM: THE KNEE 7 Ibrahim MS, Khan MA, Nizam I, Haddad FS. Peri-operative interventions producing better functional outcomes and enhanced recovery following total hip and knee arthroplasty: an evidence-based review. BMC Med 2013; 11: 37. 8 Cook JR, Warren M, Ganley KJ, Prefontaine P, Wylie JW. A comprehensive joint replacement program for total knee arthroplasty: a descriptive study. BMC Musculoskelet Disord 2008; 9: 154. 9 Kamal T, Conway RM, Littlejohn I, Ricketts D. The role of a multidisciplinary pre-assessment clinic in reducing mortality after complex orthopaedic surgery. Ann R Coll Surg Engl 2011; 93: 149e51. 10 Crockarell JR, Guyton JL. Part III e arthroplasty of ankle and knee. In: Canale, ed. Campbell’s operative orthopaedics. 10th edn. Mosb., 2003. 11 Winiarsky R, Barth P, Lotke P. Total knee arthroplasty in morbidly obese patients. J Bone Joint Surg Am 1998; 80: 1770e4. 12 Samson AJ, Mercer GE, Campbell DG. Total knee replacement in the morbidly obese: a literature review. ANZ J Surg 2010; 80: 595e9. 13 Chiu FY, Lin CF, Chen CM, Lo WH, Chaung TY. Cefuroxime-impregnated cement at primary total knee arthroplasty in diabetes mellitus. A prospective, randomised study. J Bone Joint Surg Br 2001; 83: 691e5. 14 Erdogan AO, Gokay NS, Gokce A. In: Kinov Plamen, ed. Preoperative planning of total knee replacement, arthroplasty e update. InTech, 2013 ISBN 978-953-51-0995-2. http://dx.doi.org/10.5772/55023. Available from: http://www.intechopen.com/books/arthroplastyupdate/preoperative-planning-of-total-knee-replacement. Accessed August 27, 2013. 15 Fitzgerald SJ, Trousdale RT. Why knees fail in 2011: patient, surgeon, or device? Orthopedics 2011; 34: e513e5. 16 Lotke PA, Ecker ML. Influence of positioning of prosthesis in total knee replacement. J Bone Joint Surg Am 1977; 59: 77e9. 17 Fang DM, Ritter MA, Davis KE. Coronal alignment in total knee arthroplasty: just how important is it? J Arthroplasty 2009; 24(Suppl 6): 39e43. 18 Ee G, Pang HN, Chong HC, Tan MH, Lo NN, Yeo SJ. Computer navigation is a useful intra-operative tool for joint line measurement in total knee arthroplasty. Knee 2013; 20: 256e62. 19 Insall JN, Binazzi R, Soudry M, Mestriner LA. Total knee arthroplasty. Clin Orthop Relat Res 1985; 192: 13e22. 20 Malo M, Vince KG. The unstable patella after total knee arthroplasty: etiology, prevention, and management. J Am Acad Orthop Surg 2003; 11: 364e71. 21 Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg Am 1989; 71: 145e50. 22 Menke W, Schmitz B, Salm S. Range of motion after total condylar knee arthroplasty. Arch Orthop Trauma Surg 1992; 111: 280e1. 23 Mihalko WM, Whiteside LA. Bone resection and ligament treatment for flexion contracture in knee arthroplasty. Clin Orthop Relat Res 2003; 406: 141e7. 24 Cross MB, Nam D, Plaskos C, et al. Recutting the distal femur to increase maximal knee extension during TKA causes coronal plane laxity in mid-flexion. Knee 2012; 19: 875e9. 25 McPherson EJ. Adult Reconstruction. In: Miller M, Thompson S, Hart J, eds. Review of orthopaedics. 6th edn. Elsevier Saunders, 2012. 26 Ahlb€ ack S. Osteoarthrosis of the knee. A radiographic investigation. Acta Radiol Diagn 1968;(suppl 277); 7e72. 27 Insall J, Salvati E. Patella position in the normal knee joint. Radiology 1971; 101: 101e4. ORTHOPAEDICS AND TRAUMA 27:6 28 Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am 1974; 56: 1391e6. 29 Blakeney WG, Khan RJK, Wall SJ. Computer-assisted techniques versus conventional guides for component alignment in total knee arthroplasty: a randomized controlled trial. J Bone Joint Surg Am 2011; 93: 1377e84. 30 Lonner JH, Siliski JM, Lotke PA. Simultaneous femoral osteotomy and total knee arthroplasty for treatment of osteoarthritis associated with severe extra-articular deformity. J Bone Joint Surg Am 2000; 82: 342e8. 31 Miller AG, Purtill JJ. Total knee arthroplasty component templating: a predictive model. J Arthroplasty 2012; 27: 1707e9. 32 Hsu AR, Gross CE, Bhatia S, Levine BR. Template-directed instrumentation in total knee arthroplasty: cost savings analysis. Orthopedics 2012; 35: e1596e600. 33 Wright G, Chitnavis J. Which design of TKR e does it matter? J Bone Joint Surg Br 2011. Available at: http://www.boneandjoint.org.uk/ sites/default/files/FocusOn_TKRdesign.pdf. Accessed 27 Aug 2013. 34 Jacobs WCH, Clement DJ, Wymenga AB. Retention versus removal of the posterior cruciate ligament in total knee replacement: a systematic literature review within the Cochrane framework. Acta Orthop 2005; 76: 757e68. 35 Delport HP, Banks SA, De Schepper J, Bellemans J. A kinematic comparison of fixed- and mobile-bearing knee replacements. J Bone Joint Surg Br 2006; 88: 1016e21. 36 Worland RL, Jessup DE, Johnson J. Posterior cruciate recession in total knee arthroplasty. J Arthroplasty 1997; 12: 70e3. 37 Paletta GA, Laskin RS. Total knee arthroplasty after a previous patellectomy. J Bone Joint Surg Am 1995; 77: 1708e12. 38 Mihalko WM, Krackow KA. Posterior cruciate ligament effects on the flexion space in total knee arthroplasty. Clin Orthop Relat Res 1999; 360: 243e50. 39 Puloski SK, McCalden RW, MacDonald SJ, Rorabeck CH, Bourne RB. Tibial post wear in posterior stabilized total knee arthroplasty. An unrecognized source of polyethylene debris. J Bone Joint Surg Br 2001; 83-A: 390e7. 40 Kim Y-H, Yoon S-H, Kim J-S. The long-term results of simultaneous fixed-bearing and mobile-bearing total knee replacements performed in the same patient. Acta Radiol Diagn 2007; 89: 1317e23. 41 Price AJ, Rees JL, Beard D, et al. A mobile-bearing total knee prosthesis compared with a fixed-bearing prosthesis. A multicentre single-blind randomised controlled trial. J Bone Joint Surg Br 2003; 85: 62e7. 42 Breeman S, Campbell M, Dakin H, et al. Patellar resurfacing in total knee replacement: five-year clinical and economic results of a large randomized controlled trial. J Bone Joint Surg Am 2011; 93: 1473e81. 43 Pattinson SD. Medical law and ethics. 3rd edn. Thompson Reuters (Professional) UK Limited, 2011. 44 Beresford-Cleary NJ, Beresford-Cleary N, Halliday J, et al. Consent process for elective total hip and knee arthroplasty. J Orthopaedic Surg (Hong Kong) 2011; 19: 274e8. 45 General Medical Council. Consent: patients and doctors making decisions together. London: General Medical Council, 2008. 46 Department of Health. Reference guide to consent for examination or treatment. 2nd edn. London: Department of Health, 2009. 353 Ó 2013 Elsevier Ltd. All rights reserved. MINI-SYMPOSIUM: THE KNEE 47 Atrey A, Leslie I, Carvell J, et al. Standardised consent forms on the website of the British Orthopaedic Association. J Bone Joint Surg Br 2008; 90: 422e3. 48 Khan IH, Jamil W, Lynn SM, Khan OH, Markland K, Giddins G. Analysis of NHSLA claims in orthopedic surgery. Orthopedics 2012; 35: e726e31. 49 McWilliams AB, Douglas SL, Redmond AC, et al. Litigation after hip and knee replacement in the National Health Service. Bone Jt J 2013; 95-B: 122e6. ORTHOPAEDICS AND TRAUMA 27:6 50 Atrey A, Gupte CM, Corbett SA. Review of successful litigation against English health trusts in the treatment of adults with orthopaedic pathology: clinical governance lessons learned. J Bone Joint Surg Am 2010; 92: e36. 51 Chen A, Khan Y, Akhtar K, Cobb JP, Gupte CM. Cost of adverse events in knee arthroplasty e a review of the National Health Service Litigation Authority database. In: Bask spring meeting March 2013; 12e13 [Leeds, UK]. 354 Ó 2013 Elsevier Ltd. All rights reserved.