Document 12885870
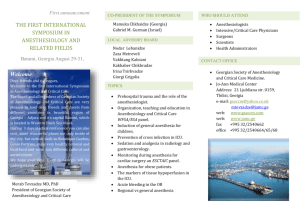
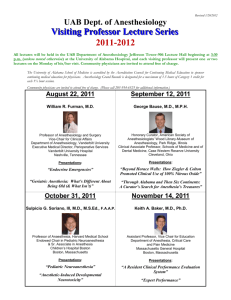
advertisement

Table of Contents Message from the Chair.............................................................2 RESEARCH Department Overview................................................................3 Research Overview..................................................................37 Department Leadership..............................................................4 Labs Focus on Translational Science.......................................38 Administrative Staff...................................................................5 Key Clinical Research Studies.................................................41 Endowed Lectureships & Awards..............................................6 Vanderbilt Lands Patient-centered Research Grant ................43 EDUCATION Putting the Power of Technology into Practice........................44 Office of Educational Affairs.....................................................8 Perioperative Clinical Research Institute (PCRI)....................46 Educational Courses and Conferences.....................................10 Vanderbilt Anesthesiology & Perioperative Informatics Research (VAPIR) Division.....................................................48 Simulation Provides Invaluable Lessons................................. 11 BH Robbins Scholars Excel.....................................................12 Department Plays Lead Role in $1 Million AMA Grant.........15 Center for Research & Innovation in Systems Safety (CRISS)...50 Selected Publications, 2012-2013............................................51 Achieving Balance...................................................................56 Vanderbilt International Anesthesia Continues to Expand.......16 New Faculty Reinforce International Outreach.......................19 CLINICAL CARE Clinical Overview....................................................................20 nagem ent Ma in ic Division of Pain Medicine.......................................................31 ed Division of Obstetric Anesthesiology......................................30 eM Division of Neurosurgical Anesthesiology..............................29 in Division of Multispecialty Adult Anesthesiology....................28 e Pa Anesthesia Technicians Provide Critical Support....................27 P e ri o p e r a ti v Certified Registered Nurse Anesthetists...................................26 y Division of Cardiothoracic Anesthesiology.............................25 d lt Anesthes i b io er log Division of Anesthesiology Critical Care Medicine................24 Va n Division of Ambulatory Anesthesiology..................................22 Established 1946 Division of Pediatric Anesthesiology.......................................33 Division of Pediatric Cardiac Anesthesiology.........................34 Vanderbilt Preoperative Evaluation Center (VPEC)................35 Veteran’s Affairs Anesthesiology Service................................36 1 Message from the Chair We are in a time of growth and transformation at the Vanderbilt University School of Medicine’s Department of Anesthesiology. The department is vibrant and strong, and we are well prepared to face the challenges that the changing healthcare economy will surely place before us. The department is excelling in all areas of our three-fold mission: • • • Practicing excellent perioperative medicine Providing top-notch education for our medical students, residents, and fellows Conducting cutting-edge basic, translational, and clinical research We have one of the largest clinical programs in the country, providing on-demand coverage for more than 90,000 adult and pediatric anesthetic encounters annually at more than 100 anesthetizing locations. We cover critical care, pain management, and all perioperative anesthesia needs. Vanderbilt University Hospital is the region’s only Level I Trauma Center. Additionally, we have an active high-risk obstetrics program, a busy Transplant Center, and the region’s largest pediatric referral hospital. Responding to demand for ambulatory procedures, we added off-site service locations by taking over anesthesia services at Vanderbilt Bone & Joint in 2011. Moreover, we expanded our regional anesthesia services, pulling increasingly complex procedures out of the inpatient OR and into the outpatient setting. We have consolidated our Pain Medicine services in order to provide consistent, comprehensive care for both acute and chronic pain. In 2013, the department also formed the new Division of Neurosurgical Anesthesiology, under the leadership of Lorri Lee, MD, a nationally renowned neuroanesthesiologist. Our commitment to patient safety was strengthened with the 2011 formation of the Center for Research and Innovation in Systems Safety (CRISS), which conducts basic and applied research in healthcare informatics, patient safety, and clinical quality and designs and evaluates informatics user interfaces, care processes, and medical technology across VUMC. This center has been awarded a twoyear, $750,000 grant from the Patient Centered Outcomes Research Institute (PCORI), one of the first grants awarded by the nonprofit institute established by the Patient Protection and Affordable Care Act of 2010. In 2011, we also formed the Vanderbilt Anesthesiology & Perioperative Informatics Research (VAPIR) Division to leverage our wealth of historical data, with the goal of generating valuable research and new evidence-based protocols to bring consistency and excellence to our patient care. To support clinicians in their pursuit of excellent patient care, we have redoubled our development of cutting-edge perioperative information systems. We continue to refine and deploy our internally-developed OR VigilanceTM and VigiVUTM applications. These applications provide increased transparency and situational awareness for clinicians by making data visible and pushing it – literally – to the clinician’s hand. We have used these applications to implement quality improvement projects that have brought rebates to the department from the Vanderbilt Self Insurance Trust. More importantly, the automated process monitoring and process control systems developed at Vanderbilt have contributed materially to improving patient outcomes by, for example, reducing wound 2 infection rates and 14-day readmission rates. We are international leaders in perioperative informatics, and as healthcare reforms promise increased accountability and efficiency, our sophisticated systems provide a unique competitive advantage. Our educational programs continue to excel. In the Warren S. Sandberg, MD, PhD 2013 National Chair, Department of Anesthesiology Residency Match, our Vanderbilt University School of Medicine department received 852 applications for 15 positions. After interviewing 111 outstanding medical students, the program successfully filled all 15 positions within the top 25 students on our Match list. Ten out of the 15 are AOA members, and the Mean USMLE Step 1 Score for the entire group is 245. We provide one-on-one faculty instruction and mentorship, and deep offerings in didactic education with grand rounds, case discussions, lectures, journal clubs, and visiting professorships from our top colleagues across the country. We nurture enterprising young researchers through the innovative BH Robbins Scholars Program, and we support seasoned research veterans who mentor developing researchers and generate significant extramural research funding. In 2012, the department’s investigators brought in more than $4.5 million in new extramural research funding from NIH and other sources. The department now boasts more than $8.5 million in active grants, and Vanderbilt Anesthesiology now places 12th among U.S. academic anesthesiology departments in NIH funding. The department also makes a major investment in protected academic time for its faculty, and the department’s Perioperative Clinical Research Institute provides complete support for clinical and informatics research activities. During the 2012-2013 academic year, our faculty produced more than 220 publications, including five books and 35 book chapters. At the 2013 Annual Meeting of the American Society of Anesthesiologists, department members contributed more than100 entries, including oral presentations, medically challenging cases, poster presentations, problem-based learning discussions, workshops, panel discussions, and refresher courses. The department’s researchers organized, led, or presented at more than a dozen national or international meetings in 2013. The Vanderbilt Department of Anesthesiology is excelling in patient care, providing superb education across the whole anesthesia curriculum, and advancing research and academic enquiry across all fronts. We proactively seek innovative ways to provide the best possible care for patients with the smartest use of our resources and technology. Through its successes, our department is positively influencing the future of our specialty as a whole. Department Overview The Vanderbilt Department of Anesthesiology was one of the first independent departments of anesthesiology in the United States, established on December 12, 1945. After observing that the battlefield-wounded of World War II were more likely to survive if they received immediate, skilled anesthesia care, Vanderbilt physicians advocated that anesthesiology be established as an autonomous department. At that time, few medical schools possessed an academic anesthesiology service of any type. This tradition of pioneering in our specialty continues today. Our exemplary faculty provide top-quality clinical services for a full spectrum of medical specialties. Vanderbilt Anesthesiology is recognized as an innovator in perioperative management, healthcare information technology, and scientific discovery. We also have high-caliber basic science and clinical research teams pursuing fundamental and translational knowledge to directly improve patient safety and care. Department Chairmen Dr. Warren S. Sandberg (2010-present) Dr. Michael S. Higgins (2004-2010) Vanderbilt Anesthesiology is also: • A national leader in developing and applying new technologies – often developed in-house by our own physicians and research personnel – to improve the effectiveness and safety of perioperative patient care. These include electronic medical record keeping, automated real-time decision support, and smart phone-based OR transparency software. • Well-represented on the editorial boards of major anesthesia journals. • Highly represented as educators at the Annual Meeting of the American Society of Anesthesiologists and at national anesthesiology, critical care, and pain medicine subspecialty conferences. • Home to a number of NIH-funded principal investigators and seven Board Examiners for the oral exams of the American Board of Anesthesiology. Dr. Jeffrey R. Balser (2001-2004) Dr. Charles Beattie (1994-2001) In addition to our department’s achievements, recent accolades for Vanderbilt’s medical program are many: • In 2012, Vanderbilt University Medical Center (VUMC) was recognized for the 13th consecutive year as one of the top 100 hospitals in the country in a study by Thomson Reuters Healthcare. • Becker’s Hospital Review named VUMC one of America’s 100 Best Hospitals in rankings released in March 2013. • Monroe Carell Jr. Children’s Hospital at Vanderbilt is included among the nation’s leaders in pediatric health care in U.S. News & World Report magazine’s Best Children’s Hospitals rankings. The hospital achieved rankings in 9 out of 10 pediatric specialty programs. • VUMC is one of the top medical schools for National Institutes of Health funding, receiving more than $286 million for research initiatives for fiscal year 2012. • For the ninth consecutive year, Vanderbilt University Medical Center was named one of the nation’s 100 “Most Wired” hospitals and health systems for its innovative efforts in medical technology, according to the 2013 Most Wired Survey and Benchmarking Study conducted by Hospitals and Health Networks magazine. • VUMC has been named the top hospital in Tennessee and the top health care provider in the Metro Nashville region according to U.S. News & World Report’s 2013-2014 Best Hospitals edition. • Vanderbilt University Hospital earned an “A” Hospital Safety Score in July 2013 from the Leapfrog Group, placing VUH among the safest hospitals in the nation. Dr. Bradley Edgerton Smith (1969-1993) Dr. Charles Bernard Pittinger (1962-1969) Dr. Benjamin Howard Robbins (1946-1961) 3 Department Leadership Vice-Chairs and Administrative Leadership Suanne Daves, MD Vice-Chair for Pediatric Anesthesiology Anesthesiologist in Chief, Monroe Carell Jr. Children’s Hospital at Vanderbilt Stephen Doherty Associate Director for Finance Edward Sherwood, MD, PhD Vice Chair for Research Matt Weinger, MD Vice-Chair for Faculty Affairs Curtis Baysinger, MD Division of Obstetric Anesthesiology James Berry, MD Division of Multispecialty Adult Anesthesiology Suanne Daves, MD Division of Pediatric Cardiac Anesthesiology Robert Deegan, MD Division of Cardiothoracic Anesthesiology Eric Delpire, PhD Basic Science Research Katherine Dobie, MD Division of Ambulatory Anesthesiology Marc Huntoon, MD Division of Pain Medicine 4 William Furman, MD Vice-Chair for Clinical Affairs Matthew McEvoy, MD Vice-Chair for Educational Affairs Division Chiefs Lorri Lee, MD Division of Neurosurgical Anesthesiology Lee Parmley, MD, JD Division of Anesthesiology Critical Care Medicine Ann Walia, MD Division of Veteran’s Affairs Anesthesiology CRNA Leadership Steve Blanks Chief CRNA Buffy Lupear Assistant Chief CRNA Administrative Staff The Vanderbilt Department of Anesthesiology’s administrative and research staff members provide critical support for every division of the department. From personnel who manage clinical scheduling and payroll, to staff members who provide research support and perform general administrative duties, each division of the department has assigned administrative staff members. There are approximately 54 administrative staff members and 20 research staff members. These individuals are vital to successfully achieving the department’s three-fold mission of practicing excellent perioperative medicine; provide exemplary education for our medical students, residents and fellows; and conducting cutting-edge basic, translational and clinical research. 5 Endowments Support Special Lectureships & Awards The Vanderbilt Department of Anesthesiology hosts several special lectureships throughout the year, as well as presenting distinct recognitions to department members who have provided exemplary service to both their patients and colleagues. Many of these are a direct result of philanthropic support from our alumni, as well as from current department members and other program supporters. Fortunately, such “seed” funding is within the reach of many private donors, whose gifts materially improve the academic life of the Vanderbilt Department of Anesthesiology. “We are very appreciative of our many donors who support our department,” said Chairman Warren Sandberg, MD, PhD. “Through these gifts we are able to establish and strengthen programs; support innovative research endeavors; and advance the education and continued betterment of our faculty, staff, and students.” Members of Dr. James Phythyon’s family attend the annual lecture named in his honor. Shown here is the family with guest lecturer Randall Wetzel, MD, Vice-Chair for Pediatric Anesthesiology Suanne Daves, MD, and Department Chairman Warren Sandberg, MD, PhD. Dr. James Phythyon Endowed Lectureship in Pediatric Anesthesiology For the past eight years, the Dr. James Phythyon Endowed Lectureship in Pediatric Anesthesiology has brought renowned experts in the field to Vanderbilt’s campus as visiting professors. At a special Grand Rounds lecture, these experts share their research findings and expertise with the department. During their visit, the speakers also meet with residents and fellows for small group teaching sessions and informal discussions. The lectureship was established by the family of Dr. James Phythyon, a founding member of VUMC’s Pediatric Anesthesia Division. Dr. Phythyon’s widow, Mrs. Marlin Sanders, and the couple’s daughters, Mary Neal Meador, Elizabeth Donner, and Sarah Miller, are strong supporters of the department. Each year, they attend the lecture and other events in honor of Dr. Phythyon. In 2013, Randall Wetzel, MD, Chairman of the Department of Anesthesiology Critical Care Medicine at Children’s Hospital in Los Angeles presented a well-received Grand Rounds lecture on “Meaningful Use of Complex Medical Data.” 6 Past Phythyon Lectureship speakers include: Peter Marhofer, MD, Director of Paediatric Anaesthesia and Professor, Anaesthesia and Intensive Care Medicine, at the Medical University of Vienna, Vienna, Austria; Dean Andropoulos, MD, MHCM, Chief of Anesthesiology at Texas Children’s Hospital; Shobha Malvia, MD, of The University of Michigan Health System; Philip Morgan, MD, of the University of Washington and Seattle Children’s Hospital; Francis X. McGowan Jr., MD, of the Children’s Hospital Boston; Peter Davis, MD, of the Children’s Hospital of Pittsburgh; and Myron Yaster, MD, of Johns Hopkins University School of Medicine. Left to right: Vice-Chair for Pediatric Anesthesiology Suanne Daves, MD, Sandidge Pediatric Pain Management Award winner Drew Franklin, MD, and Paula C. Sandidge, MD. Sandidge Pediatric Pain Management Endowed Fund Retired Vanderbilt anesthesiologist Paula C. Sandidge, MD, created The Sandidge Pediatric Pain Management Endowed Fund at Monroe Carell Jr. Children’s Hospital at Vanderbilt in 2010 to recognize and encourage progress in pain management for children. An anesthesiologist for 30 years, Dr. Sandidge recognized how lacking her early training had been in controlling pain for the youngest of patients when her grandson was born with a painful form of osteogenesis imperfecta. He lived just one day, but Sandidge realized then that pain control provided infants something irreplaceable: the opportunity to be held comfortably by the people who love them for the few precious moments they have. In 2013, Pediatric Anesthesiologist Drew Franklin, MD, received the Sandidge Pediatric Pain Management Award in recognition of his work with patients at the Pediatric Pain Management Clinic at Children’s Hospital. Dr. Franklin presented a Grand Rounds lecture entitled “A multidisciplinary approach to the management of refractory pediatric complex regional pain syndrome.” Past recipients of the Sandidge Pediatric Pain Management Award include Stephen Hays, MD, FAAP, associate professor of Anesthesiology & Pediatrics and director of Pediatric Pain Services; and Twila Luckett, BSN, RN-BC. Family members of David H. Chestnut, MD, along with Bradley E. Smith, MD (second from left) and Department Chair Warren Sandberg, MD, PhD (far right). Perinatology (SOAP), as well as the Society for Technology in Anesthesia (STA). He also represented the state of Tennessee on the ASA Board of Directors for many years. Winner of the 2013 Vuksanaj Award is Jenna Helmer Sobey, MD. Shown with her, left to right, are Vice-Chair for Educational Affairs Matt McEvoy, MD, past Vice-Chair for Educational Affairs John Algren, MD, and Vice-Chair for Pediatric Anesthesiology Suanne Daves, MD. Dila Vuksanaj Memorial Fund for Resident Education Pediatric anesthesiologist Dila Vuksanaj, MD, practiced at the Children’s Hospital for 13 years, dedicating herself to her patients and to the hundreds of trainees who looked to her as a role model, mentor, and friend. Following her death in 2009, her family, including her husband Jacques Heibig, MD, founded the Dila Vuksanaj Memorial Fund for Resident Education. The fund is used to present an annual award to the anesthesiology resident who demonstrates the best overall performance in pediatric anesthesiology. In 2013, Jenna Helmer Sobey, MD, was recognized for her outstanding work at Children’s Hospital. Past recipients include: Korie Vakay, MD; Justin Sandall, DO; and Elizabeth Lee, MD. Dr. Bradley E. Smith Endowed Lectureship on Medical Professionalism Throughout his more than four decades of practice and leadership, former Anesthesiology Department Chairman Bradley E. Smith, MD, defined what it means to be a true professional, and in 2009 a lectureship on medical professionalism was established in his name by then department chairman Michael Higgins, MD. The goal of the lectureship is to reflect on the characteristics, responsibilities, and rewards of professionalism as applied to the practice of anesthesiology. As chairman of the department for nearly 25 years, Dr. Smith was a national leader in the development of anesthesia subspecialties. He was a cofounder of the Society for Obstetric Anesthesia and David H. Chestnut, MD, was the guest speaker for the Smith Lectureship in 2013. Dr. Chestnut is the editor of Obstetric Anesthesia: Principles and Practice, which is regarded as the leading textbook in obstetric anesthesia. Dr. Chestnut is director of Medical Education at Gundersen Lutheran Health System in LaCrosse, Wisconsin. Past speakers for this special lectureship include: William D. Owens, MD, recipient of the American Society of Anesthesiologists Distinguished Service Award; Peter McDermott, MD, PhD, past president of the ASA; and Joseph Gerald “Jerry” Reves, MD, Dean of the College of Medicine at the Medical University of South Carolina (MUSC). Dr. Charles Beattie Endowed Lectureship Established in 2011 by the current chairman, this lectureship honors Charles Beattie, MD, the fourth chair of the department. “Dr. Beattie was many things to the many people who knew him,” said Dr. Sandberg. “He was at once a great humanist, a colorful character, and an early and forceful driver in the creation of what we now call ‘systems-based practice,’ the core competency which we exercise to create robust systems to assure that all patients receive consistent, safe, outstanding care in an environment that Charles Beattie, MD naturally performs well.” Dr. Beattie came to anesthesiology after first becoming a nuclear power engineer. This background surely informed and motivated his passions in anesthesiology. The lectureship is intended to bring innovators in anesthesiology from unique backgrounds and compelling world views to Vanderbilt as visiting professors. 7 Office of Educational Affairs The Office of Educational Affairs for the Vanderbilt Department of Anesthesiology supports and oversees the full continuum of education related to anesthesiology and perioperative medicine, which includes undergraduate medical education, graduate medical education for residents and fellows, and continuing education for faculty and advanced practice nurses. The extensive education and training programs offered by the Department of Anesthesiology integrate scientific and clinical advances with current clinical practice to prepare medical students, residents, fellows, nurses, and faculty for productive careers as clinicians, academicians, and scientists. A major factor in attracting residents, fellows, and faculty is the strength of the department’s subspecialties, as residents and fellows benefit from in-depth training in all subspecialty disciplines of clinical anesthesiology, critical care, and pain management. An additional draw is the Vanderbilt International Anesthesia (VIA) rotation, which provides a month-long global health experience to an average of eight residents and fellows each year. Trainees are also attracted by the department’s extensive research opportunities, in particular the BH Robbins Scholars program, which offers oneon-one mentorship and collaboration for young physician-scientists preparing for careers as academic anesthesiologists. “Vanderbilt offers a comprehensive clinical experience that spans the breadth of clinical anesthesia and perioperative medicine, and it does this in the context of one institution,” said Matt McEvoy, MD, Vice-Chair for Educational Affairs and Program Director. “We offer the full scope of training experiences, as well as opportunities for academic development in the fields of research, education, medical informatics, and leadership. Furthermore, we are leveraging our departmental and institutional resources to be a national leader in the new ACGME Milestones system and in the concept of the surgical home.” The Office of Educational Affairs including oversight of the Residency Program, is led by Dr. McEvoy and is supported by Associate Program Director Jane Easdown, MD; Associate Program Director Michael Pilla, MD; Director of Medical Student Education Amy Robertson, MD; and four administrative staff members. The department’s specific offerings to each learner group are outlined below. Medical Students Dr. Amy Robertson serves as the Director of Medical Student Education for the department and oversees a wide range of programs for medical students. The department’s faculty members contribute to Vanderbilt medical students’ education throughout the fouryear curriculum, beginning with Vanderbilt University School of Medicine’s (SOM) College Advisory system. Associate Program Director Michael Pilla, MD, serves in a leadership role as a SOM College Mentor in this system. Dr. Robertson was recently selected as one of 10 Portfolio Advisors for the SOM. Additionally, Dr. Jesse Ehrenfeld is a co-director of the Continuity Clinical Experience (CCX) for all medical students in Curriculum 2.0, a longitudinal clinical experience spanning all four years of medical school. Formal clinical courses provide numerous opportunities for clinical education in anesthesiology and perioperative medicine, including Introduction to Anesthesiology elective, Critical Care Skills Course, Perioperative Medicine “Immersion Course,” Critical Care elective, and Advanced Anesthesiology Clerkship for senior students. Many medical students also participate in research mentored by Anesthesiology faculty. 8 Additionally, informal, as well as formal, mentorship of medical students by faculty and residents has advanced the understanding and appreciation of the specialty. These efforts have led to an increase in Vanderbilt medical students planning careers in anesthesiology, from six graduates in the class of 2011 to 12 students in the class of 2012. Residents The department’s fully accredited residency program is highly sought after by the nation’s top medical students. Proof of this is in the numbers: in the 2013 National Residency Match, the department received 852 applications for 15 positions. After interviewing 111 outstanding medical students, the program successfully filled all 15 positions from the top 25 students on its rank list, including five of the top 10. The National Residency Matching Program Report continues to rank Vanderbilt’s program in the top quartile of all U.S. anesthesia residency programs for key quality indicators: number of positions offered, recruiting efficiency, AOA membership (67%), mean USMLE Step 1 score (245), and mean USMLE Step 2 score (256). It is the department’s goal to produce perioperative physicians who are prepared with all of the requisite cognitive, technical, and academic skills to be leaders in the future of our specialty in medicine as a whole. The department seeks applicants who desire this level of training and development during their residency and beyond. Vanderbilt Anesthesiology’s four year residency program currently enrolls 15 resident physicians per year. Our physician educators are nationally and internationally recognized as leaders in their fields, and the department successfully supports residents interested in academic anesthesiology so they can develop careers focused on advancing knowledge in the specialty. The department typically has 25-30 residents who present original research and overviews of challenging cases at national meetings every year, a clear indication that the department’s educational programs are creating physicianscholars who are prepared for both medical practice and scientific investigation. The department’s educational program for residents, as well as fellows, consists of a combination of comprehensive didactic conferences, mentored clinical training by subspecialists in every domain of anesthesiology, simulation training, and self-study. Simulation training features prominently in the cognitive, procedural, and teamwork aspects of anesthesia education, and Vanderbilt University School of Medicine’s Center for Experiential Learning and Assessment is a nationally renowned, on-campus resource for this training. The ACGME core competencies form a framework for the training program, and a major curricular revision is underway that is targeting the new ACGME Milestones system, as well as the recent changes to the ABA Certification process. On average, Vanderbilt Anesthesiology residents have scored at the 70th percentile on standardized examinations when compared with the national cohort. The goal of the curriculum revision will be to continue to achieve or exceed that level of academic achievement. Fellows Building from the department’s strength in subspecialties, six clinical fellowships, as well as a research fellowship, are offered to individuals seeking advanced, focused training. The following clinical fellowships are offered at Vanderbilt: The Office of Educational Affairs includes, front row, Associate Program Director Jane Easdown, MD; Associate Program Director Michael Pilla, MD; and Administrative Director Joyce Speer. Back row, Program Coordinator Marsha Moore; Vice Chair for Educational Affairs Matthew McEvoy, MD; and Program & Events Coordinator Deborah Nelson-Rouse. Not pictured: Director of Medical Student Education Amy Robertson, MD. • • • • • • Adult Cardiothoracic Anesthesiology* – 3 fellows Anesthesiology-Critical Care Medicine* – 8 fellows Obstetric Anesthesiology* – 1 fellow Pain Medicine* – 3 fellows Pediatric Anesthesiology* – 4 fellows Regional Anesthesiology** – 2 fellows *ACGME Accredited **ACGME Accreditation not offered Advanced Practice Nurses The Department of Anesthesiology has a unique partnership with the Vanderbilt University School of Nursing to offer an Acute Care Nurse Practitioner (ACNP) Intensivist track as part of the ACNP master’s degree program. The program combines the didactic training of the School of Nursing’s ACNP program with supplemental specialty lectures in critical care medicine. Students perform their clinical rotations in seven of the Vanderbilt and VA ICUs. Students also receive additional exposure to ICU medicine through twice monthly simulation sessions and weekly clinical case conferences taught jointly by members of both faculties. Additional partnership programs between the Anesthesiology Department and the School of Nursing are being planned. Vanderbilt University Medical Center, one of the largest employers of nurse practitioners in the country, and the Division of Anesthesiology Critical Care Medicine now have more than 35 Acute Care Nurse Practitioners on staff who provide highly skilled treatment in intensive care settings. Nurse Anesthetists More than 100 Certified Registered Nurse Anesthetists form a critical part of our department. Their continuing education is led by Steve Blanks and is supported with recurring education programs, including Grand Rounds and Morbidity, Mortality & Improvement Conferences. In addition, Vanderbilt is a primary clinical affiliate of the Middle Tennessee School of Anesthesia (MTSA) in Madison, Tennessee, and of the Union University Nurse Anesthesia program in Jackson, Tennessee. Student nurse anesthetists participate in approximately 7,000 anesthetics per year while on Vanderbilt rotations, and their on-campus training is coordinated by the Department of Anesthesiology. Continuing Medical Education The Office of Educational Affairs oversees a full calendar of continuing medical education opportunities for faculty, residents, fellows, nurse anesthetists, and nurse practitioners. Some examples are weekly Grand Rounds, which feature leading experts from throughout the world; Mortality, Morbidity & Improvement Conferences (MM& I), which focus on recent cases with the goal of improving patient care; Faculty Development Seminars, which provide targeted training for professional development; and Combined Integrative Health and Pain Medicine Quarterly Rounds, which focus on issues related to the management and treatment of pain. Awarding and Recognizing Excellence The department recognizes excellence in both its trainees and faculty members. Outstanding performance by residents is recognized through annual Clinical Excellence Awards, and exceptional performance in teaching is recognized through the annual presentation of Golden Apple Awards and the Volker I. Striepe Award for Outstanding Teaching. In addition to these local awards, our faculty members garner national and international recognition of their excellence in educational programs and research. Dr. Ehrenfeld is part of a team in the SOM that was recently awarded a $1 million grant from the AMA as a part of the Accelerating Change in Medical Education program. Dr. Mark Newton was celebrated in 2012 by the American Medical Association with the Dr. Nathan Davis International Award in Medicine, recognition of his 15 years of service at Kijabe Hospital as a leader of international anesthesia education in Kenya. Additionally, our faculty routinely are awarded research grants from the Foundation for Anesthesia Education and Research. 9 Educational Courses and Conferences The Vanderbilt Department of Anesthesiology provides a full calendar of educational opportunities for anesthesiologists and other medical professionals. Our medical education offerings include: For Medical Students Critical Care Skills Week: Weeklong, quarterly workshop for thirdyear medical students to prepare them to recognize and manage critical problems encountered in clinical practice. This training includes hands-on education using simulation at Vanderbilt’s Center for Experiential Learning and Assessment (CELA), as well as lectures by departmental faculty. Surgery Clerkship Selective: This rotation provides a hands-on, continually monitored and mentored experience. Students become an integral part of an anesthesia care team and participate in perioperative management of adult patients presenting for surgical, diagnostic, or therapeutic interventions. Students participate in preoperative assessment, risk stratification, anesthetic planning and conduct of anesthesia, airway management, and postoperative planning and care of patients. Introduction to Anesthesia: This rotation provides a hands-on, continually monitored and mentored experience. Students become an integral part of an anesthesia care team and participate in perioperative management of adult patients presenting for surgical, diagnostic, or therapeutic interventions. Students participate in preoperative assessment, risk stratification, anesthetic planning and conduct of anesthesia, airway management, and postoperative planning and care of patients. Perioperative Medicine Immersion Courses: This four-week course emphasizes perioperative medicine as a continuum of care with application of both basic science and clinical knowledge from a variety of rotation experiences. Basic science topics are applied to specific disease processes, clinical decision making, and perioperative outcomes. Emphasis is placed upon the importance of the collaboration of care with medical specialists and healthcare team members to achieve optimal patient outcomes. Senior Anesthesia Elective: This four-week elective for fourthyear medical students provides a multidisciplinary experience in Anesthesiology so that all students rotate through the following venues: Adult Anesthesia at VUH and/or VA; Cardiothoracic Anesthesia; Pediatric Anesthesia; OB Anesthesia; Neuro ICU/SICU/ BICU; and Acute Pain Service. In addition, students participate in departmental lectures for residents, Grand Rounds, and MM&I Conferences. For Interns Boot Camp: Workshops held during orientation, as well as periodically throughout the year, focusing on developing specialized skill sets essential to anesthesia and perioperative care. Intern Conferences: Introduction to Anesthesia Seminars; Matrix Seminars (QI training program); and practice-improvement discussions, organized using the Healthcare Matrix and Basics of Anesthesia lectures. For Residents ABA BASIC Exam Prep Series: Weekly conferences for CA-1 residents. The content of this didactic series maps directly to the ABA Content Outline for the new ABA BASIC Exam that starts in August 2014. Subspecialty Conferences: Conferences coordinated by individual divisions of the department, including Pediatric, Obstetric, Cardiothoracic, Neurosurgical Anesthesiology, Regional, Pain Medicine, Critical Care Medicine, and Multispecialty Adult Anesthesiology. Senior Seminars: Seminar series for senior residents focused on problem-based learning and preparation for Oral Exams. Professional Development Conferences: Resident conferences focused on elements of subspecialty selection, career paths, and business practices related to perioperative anesthesia. For All Journal Clubs: Informal meetings in which medical articles pertaining to the specialty are summarized and reviewed. Journal Clubs are held by department divisions, including Multispecialty, Pediatric, Cardiothoracic, Critical Care, and Pain Medicine. Academic Development Conferences: For fellows, residents, and faculty on topics related to educational theory and practical aspects of classroom and clinical teaching, mentorship, etc. Transesophageal Echocardiogram training offered by the Department of Anesthesiology includes real-time cardiac simulation. 10 Grand Rounds: Formal, weekly lectures featuring recognized experts in the fields of anesthesiology, perioperative medicine, or pain medicine. Mortality, Morbidity & Improvement Conferences: Monthly conferences focused on case studies with the goal of improving patient care. Each quarter, Perioperative M&M Conferences also include surgical specialties and nursing services to better facilitate the exploration of cases and the exchange of ideas. Special Courses Fundamentals of Critical Care Support (FCCS): Multidisciplinary, two-day comprehensive course addressing fundamental management principles for the first 24 hours of critical care. This course is sponsored by the Society of Critical Care Medicine, and is directed by members of the Anesthesiology Department’s Division of Anesthesiology Critical Care Medicine. Instructors for the FCCS course represent multiple specialties at Vanderbilt University Medical School. Maintenance of Certification in Anesthesiology (MOCA®) Simulation Courses: The department, in partnership with the Center for Experiential Learning and Assessment (CELA) at Vanderbilt, offers immersive patient simulation education for ABA Diplomates seeking to fulfill their Practice Performance Assessment and Improvement (PPAI) requirement for the American Board of Anesthesiologists’ (ABA) Maintenance of Certification in Anesthesiology (MOCA®) Program. This course fulfills the simulation education requirement of Part 4 of MOCA®. The VUMC simulation program has been endorsed by the ASA Committee on Simulation Education. Combined Integrative Health and Pain Medicine Quarterly Rounds: Quarterly day-long course for anesthesiology faculty, as well as integrative health services providers, including rehabilitation physicians, physical therapists, psychiatrists, and others involved in treatment and management of pain. Simulation Education Provides Invaluable Lessons Simulation education is a virtual approach to training physicians and other medical providers in the management of complex clinical cases and challenging situations, especially those they might not encounter on a regular basis in the clinical setting. The Vanderbilt University School of Medicine has a remarkable on-campus resource for medical simulation training, the Center for Experiential Learning and Assessment (CELA), and our Anesthesiology Department faculty are national leaders in providing simulation training in anesthesiology airway management, critical care, perioperative management, and transesophageal echocardiogram procedures. Arna Banerjee, MD, an assistant professor of anesthesiology in the Division of Anesthesiology Critical Care Medicine was named director of CELA in July 2013. endorsed by the American Society of Anesthesiologists (ASA) as one of about 30 centers in the nation officially approved to deliver certified educational programs. Anesthesiologists can receive Continuing Medical Education (CME) simulation training at CELA that qualifies for American Board of Anesthesiology Maintenance of Certification in Anesthesiology (MOCA®) credit. To achieve the ASA endorsement, the CELA program met strict criteria, including having strong leadership, and the necessary equipment, facilities, and personnel to provide consistent, effective training. CELA, which opened in 2007, is an 11,000-square-foot facility that is home to both the Program in Human Simulation and the Simulation Technologies Program. The center offers advanced simulation technologies, including computerized mannequins that can reproduce both routine and critical clinical situations. One floor of the facility includes flexible space that can serve as a six-bed emergency department, a four-bed intensive care unit, or a couple of operating rooms — all monitored by computer-controlled audio/video equipment. At Vanderbilt’s Center for Experiential Learning and Assessment (CELA), computerized In May 2009, the Vanderbilt Simulation mannequins, including obstetric and infant mannequins, are used to reproduce routine and critical Technologies Program, under the direction care clinical situations. of Matthew B. Weinger, MD, was 11 BH Robbins Scholars Excel with Publications, Lectures For young scholars, building critical academic research skills under the mentorship of established scientists makes them strong future investigators. With this goal, the Benjamin Howard Robbins Scholars Program began in 2007. The program is named in honor of the Vanderbilt Anesthesiology Department’s first chairman, a renowned physician-scientist. The BH Robbins Scholars program is multidisciplinary, encouraging and supporting mentorships and collaborations that extend far beyond the traditional boundaries of anesthesia. Benjamin Howard Robbins, MD, the Department of Anesthesiology’s first Chair and a noted physicianscientist. “This program provides a unique mentored research experience for young scholars that culminates in a two-year multidisciplinary fellowship, with at least one year devoted to research,” said Department Chair Warren Sandberg, MD, PhD. “Our Robbins Scholars benefit from one-on-one mentorship, a wealth of research and educational resources, protected research time, and a stipend during their residency and fellowship.” The BH Robbins Scholars program is co-directed by Jerod Patrick Henson, DO Denton, PhD, and Pratik Pandharipande, MD. Following is an update on current Scholars’ progress and achievements in the Patrick Henson, DO, is working past academic year. under the mentorship of Dr. Ed Sherwood, MD, PhD, and is actively enrolling patients in his study aimed at evaluating and measuring cellular expression of PD-1 and markers of immune tolerance in patients following severe burn injury. He has been active in many local teaching opportunities. Thomas Austin, MD, is in the second year of his two-year, $175,000 Foundation for Anesthesia Education and Research (FAER) Mentored Research Training Grant-Basic Science for his project, “Effect of Neuronal K-Cl Cotransporter KCC2 Activation on Pain Perception.” Dr. Austin is mentored by Eric Delpire, PhD. In the past year, Dr. Austin has presented at the Society for Pediatric Anesthesia, the American Society of Anesthesiologists, and the Association of University Anesthesiologists meetings, has authored three manuscripts, and is currently pursuing a master’s degree in statistics. Thomas Austin, MD, who is mentored by Eric Delpire, PhD, won the 2011 Association of University Anesthesiologists’ resident travel award as a result of his research. 12 Adam Kingeter, MD, is the most recent BH Robbins Scholar. He is interested in health resource utilization and is presently involved in a project evaluating cost of care in the ICU Christopher Hughes, MD, has published several original research manuscripts during his B.H. Robbins Fellowship, and he has presented his work at national meetings. Christopher Hughes, MD, is serving as the Vanderbilt site PI of an NIH-sponsored multicenter MENDS 2 study that evaluates the role of sedation paradigms on delirium and mortality in critically ill septic patients. He has successfully obtained Vanderbilt Institute for Clinical and Translational Research (VICTR) funding for two projects pertaining to the role of endothelial dysfunction in delirium. In the past academic year, Chris has presented the findings of his research at both national and international meetings and has published over 10 peer reviewed articles/book chapters, including manuscripts in The New England Journal of Medicine, Critical Care Medicine, and Anesthesiology. Dr. Hughes is mentored by Pratik Pandharipande, MD, MSCI, as well as Wes Ely, MD, MPH (Department of Medicine’s Division of Allergy, Pulmonary and Critical Care). Amanda Lorinc, MD, is a recent recipient of the Foundation for Anesthesia Education and Research (FAER) Research in Education Grant (REG) for her project, “Handover Tool Participatory Design and Educational Training Intervention to Improve Perioperative Neonatal Safety.” She is mentored by Matthew Weinger, MD. She is also working with Dan France, PhD, on projects related to improving neonatal outcomes via monitoring of non-routine events. Amanda has presented at the Society for Pediatric Anesthesia and has authored two manuscripts in this past year. Carrie Menser, MD, is researching the utilization of a pediatric pain service in the perioperative management of pediatric palliative care patients and evaluating perioperative complications in pediatric palliative care patients. She is also involved in projects related to delirium and withdrawal in pediatric patients, as well another project evaluating cry acoustics in neonates. She recently presented her research at the Society for Pediatric Anesthesia. Adam Kingeter, MD Amanda Lorinc, MD Carrie Menser, MD 13 Joseph Schlesinger, MD, at right, discusses his research with Vice-Chair for Clinical Affairs William Furman, MD. Joseph Schlesinger, MD, is examining multisensory perceptual training, and specifically improving unisensory pulse oximetry pitch perception and attention load processing. Dr. Schlesinger has received a VICTR grant for his research and is mentored by Mark Wallace, PhD, Director of the Vanderbilt Brain Institute. Dr. Schlesinger has presented his work at the American Society of Anesthesiologists, the Society for Neuroscience, the American Society of Critical Care Anesthesiologists, and the American Medical Association. His original research articles have been published in Anesthesiology and Anesthesia and Analgesia. Heidi Smith, MD, MSCI, won the award for best oral presentation at the 2013 Anesthesiology Department Research Symposium. Department Chair Warren Sandberg, MD, PhD, presented the award. 14 Heidi Smith MD, MSCI, has ongoing studies, in collaboration with pediatric psychiatry and critical care, that include validation of a delirium monitoring instrument for children under the age of five, an observational study evaluating executive dysfunction in critically ill children, an implementation study of delirium monitoring in critically ill children, and an epidemiological study evaluating the prevalence, risk factors, and outcomes associated with delirium in critically ill patients. Heidi is a recent recipient of a VICTR Heidi Smith, MD, MSCI grant. She has presented her work at regional and national meetings, including the American Society of Anesthesiologists, the Association of University Anesthesiologists, and the Society of Critical Care Medicine. She has numerous publications including research in Critical Care Medicine, Seminars in Respiratory and Critical Care Medicine, and Pediatric Clinics of North America. BH Robbins Scholars gathered at the 2013 Anesthesiology Department Research Symposium to present their research. Here, left to right, are Department Chair Warren Sandberg, MD, PhD; guest lecturer Cor Kalkman, MD; Joe Schlesinger, MD; BH Robbins Program Co-Director Pratik Pandharipande, MD, MSCI; Amanda Lorinc, MD; Carrie Menser, MD; Heidi Smith, MD, MSCI; Patrick Henson, DO; and Adam Kingeter, MD. Not pictured: Thomas Austin, MD; and Chris Hughes, MD. Department Plays Lead Role in $1 Million AMA Grant In June 2013, American Medical Association (AMA) selected Vanderbilt University School of Medicine (VUSM) to receive a $1 million grant as one of the nation’s 11 top medical schools transforming medical education. The grant, part of the AMA initiative Accelerating Change in Medical Education, makes Vanderbilt the recipient of $1 million over the next five years to take part in a consortium created to rapidly disseminate best practices in medical education across the country. Bonnie Miller, M.D., senior associate dean for Health Sciences Education, said the announcement is evidence the innovations brought about by VUSM’s new educational curriculum, Curriculum 2.0, are among the nation’s most advanced. For VUSM, Curriculum 2.0 represents the departure from a highly regarded, but traditional medical school curriculum to a complex, integrated, collaborative, and flexible course schedule that includes less traditional lecture-based learning and more clinical and case-based experience. “This is a validation that Curriculum 2.0 represents some of the most exciting and innovative ideas for medical education,” Miller said. “It is just what the AMA is looking for. Through this grant, the AMA hopes to disseminate best practices to medical educators throughout the nation. We believe this funding and collaboration will allow us to accelerate the changes we hope to bring about with Curriculum 2.0, and to rigorously evaluate the curriculum’s effectiveness.” Dr. Ehrenfeld will lead efforts related to the first goal, learning in which students are embedded in the health care workplace. This will be largely accomplished through the Clinical Continuity Experience (CCX) program in which students become team members at a single clinical site for the duration of their undergraduate medical education. Intentional learning activities are spread across a four-year curriculum, including seminar activities and clinical experiences. The mission of CCX is to create self-directed learners, integrate the patient care experience with medical knowledge, integrate systems knowledge with clinical care, and cultivate respectful professionals. Submissions for the AMA grant were quite competitive, with more than 80 percent of the nation’s medical schools providing proposals. Dr. Ehrenfeld and the grant coinvestigators will serve in the national consortium of medical schools established by the AMA grant, giving Vanderbilt an exciting opportunity to exchange best practice information with our colleagues. This initiative will likely change the face of medical education in our country. Jesse Ehrenfeld, MD, MPH, associate professor of Anesthesiology, Surgery, and Biomedical Informatics, is one of four Vanderbilt co-investigators for the grant. Dr. Miller authored Vanderbilt’s submission along with co-investigators Robert Dittus, MD, MPH, associate vice chancellor for Public Health and Health Care; Kim Lomis, MD, associate dean for Undergraduate Medical Education; and Anderson Spickard III, MD, MS, FACP, associate professor of Medicine and assistant professor of Biomedical Informatics. In brief, the grant has three primary goals: 1. To embed learning in the workplace throughout undergraduate medical education. 2. To create a competency-based assessment system that guides student learning with explicit, standardized expectations and provides accurate information for high stakes decisions independent of time in the educational program. 3. To develop a process for personalized learning plans guided by individual student strengths, needs, and interests, and facilitated by a comprehensive electronic portfolio that collects and displays assessment data and links to the curriculum management system and the electronic health record. Jesse Ehrenfeld, MD, MPH, associate professor of Anesthesiology, Surgery, and Biomedical Informatics, is one of four Vanderbilt co-investigators for the AMA grant. Bonnie Miller, MD, senior associate dean for Health Sciences Education, is author of the grant. 15 Vanderbilt International Anesthesia Continues to Expand When Mark Newton, MD, speaks of the urgent need to reach medically underserved populations throughout the world, his words of compassion are backed up by 15 years worth of action. Dr. Newton’s humanitarian efforts in healthcare were recognized in 2012 by the American Medical Association with the presentation of the Dr. Nathan Davis International Award in Medicine. Named for AMA’s founder, the award honors physicians whose influence reaches the international patient population and changes the future of their medical care. Dr. Newton, an associate clinical professor in the Department of Anesthesiology and a pediatric anesthesiologist at Monroe Carell Jr. Children’s Hospital at Vanderbilt, was instrumental in founding, and now directs, the Vanderbilt International Anesthesia (VIA) program. Established in 2007, VIA is the Vanderbilt Department of Anesthesiology’s global service, education, and research division which focuses on anesthesia and ICU issues in low resource countries. Dr. Newton also developed an anesthesia education and training program for indigenous anesthesia providers in Kenya. Dr. Newton divides his time between being a pediatric anesthesiologist at Vanderbilt and serving as chief anesthesiologist for Kijabe Hospital in Kenya. “Over the span of his career, Mark has contributed substantially, and at great personal sacrifice, to international anesthesia education and training in low income countries,” said Warren Sandberg, MD, PhD, Chairman of the Department of Anesthesiology. “Anesthetic morbidity and mortality are a leading cause of death among surgical patients in developing countries, largely due to lack of trained personnel. Mark embodies, in spirit and action, the true meaning of a physician servant, and his personal contribution to healthcare on an international level will have a perpetual, positive impact.” Working in partnership with the Vanderbilt Institute of Global Health (VIGH), VIA has sent residents, fellows, and faculty to areas including Haiti, Guatemala, Vietnam, Jamaica, and East Africa (Kenya) for the past five years in order to improve anesthesia provision in these areas. The faculty has provided education to anesthesia care providers in Jamaica and Vietnam through locally organized seminars. Pediatric anesthesiologists, fellows, and CRNAs also share their skills at a children’s hospital in Guatemala City through a partnership between the Monroe Carell Jr. Children’s Hospital at Vanderbilt and the Shalom Foundation. Each year some of the pediatric anesthesia fellows Mark Newton, MD, at far left, and Kelly McQueen, MD, at center, join a recent class of Kenyan Registered Nurse Anesthetists (KRNAs) in Kijabe, Kenya. 16 are able to practice pediatric anesthesia in Guatemala, alongside one of their Vanderbilt mentors who is a specialist in global anesthesia. Vanderbilt residents in their CA-3 year can participate in an ACGME-approved, one-month, international anesthesia rotation at Kijabe Hospital in Kenya. The program allows four to six residents annually an international opportunity, providing a unique educational experience unlike any other found in U.S. academic anesthesiology training programs. Each resident is exposed to a medical experience in a resource-poor setting where clinical skills must be sharpened to compensate for lack of technology and supplies. The residents also provide clinical training and give classroom lectures to local medical providers. The nurse anesthetist training program in Kenya continues to expand under Dr. Newton’s leadership, with now up to 20 students per class. After graduation, these students provide anesthetic care in remote areas of Africa. In addition, multiple critical care fellows from Vanderbilt have had critical care rotations in Kenya while managing complicated, critically ill patients in an environment with fewer resources. Each of these Vanderbilt Anesthesiology’s Jenna Helmer Sobey, MD, assists KRNA students as they provide anesthesia to a pediatric patient at Kijabe Hospital. Mark Newton, MD, has developed a close bond with the healthcare providers he helps train in Kenya. 17 rotations has been instrumental in preparing anesthesia care providers for a career that will include a global health focus. “We have successfully positioned our department to lead in global anesthesia development from our home base at Vanderbilt,” said Dr. Sandberg. “It is rewarding to know that our efforts have a definitive impact on the provision of safe, effective anesthesia in parts of the world where people often die due to the lack of basic medical care. Going overseas to both train and be trained is invaluable to our residents and fellows, and they typically come back from VIA missions changed doctors. They gain experiences there that cannot be learned from a textbook or from our clinical environments in the United States.” The capacity building projects that have been developed at Kijabe Hospital over the past 15 years revolve around training physicians and non-physicians for rural anesthesia care in Kenya, South Sudan and areas of the Horn of Africa. These programs have all been developed in coordination with the respective Ministries of Health and national(African) academic institutions. Partnerships between academic institutions in Africa (University of Nairobi, Department of Anesthesiology), AIC Kijabe Hospital, and Vanderbilt University have provided the foundation for strengthening of physician anesthesia training in East Africa. Kijabe Hospital is now hosting a resident per month for clinical and didactic education as part of its program from the University of Nairobi. In addition, the East Africa Pediatric Anesthesia Fellowship began in September Kenyan Registered Nurse Anesthetists perform an ultrasound-guided leg block. The students receive training in regional anesthesia techniques through the VIA Regional Anesthesia and Acute Pain Initiative. 18 2013 with the involvement of the World Federation of Societies of Anaesthesiologists (WFSA), many international pediatric anesthesia societies, and the University of Nairobi/Kijabe Hospital partnership. In his long-term position in East Africa, Dr. Newton has had the opportunity to assist in the development of these exciting physician anesthesia capacity building programs which are deeply embedded in the local academic fabric of each involved country. “These are exciting times for our department, and our leadership in global health continues to attract some of the brightest residents and fellows who want to have an impact on the world with their specialty training,” said Dr. Sandberg. Vanderbilt physicians Jenna Helmer Sobey, MD, at left, and Chris Sobey, MD, at right, assist KRNAs during a procedure. New Faculty Reinforce International Outreach To further strengthen VIA’s efforts in global outreach/research, grant writing, and in fundraising to support the initiative, Kelly McQueen, MD, MPH, was recruited by the Department of Anesthesiology in 2012 to serve in the role of Director of Vanderbilt Anesthesia Global Health and Development. Dr. McQueen has a career-long commitment to disaster response and humanitarian aid, and her continued work on advocating for surgery and anesthesia as a global health agenda has grown in the past year at Vanderbilt. Matt McEvoy, MD, vice-chair for Educational Affairs and program director, joined the Department of Anesthesiology faculty in April 2013 and is a strong supporter and advocate of the VIA experience for residents and fellows. Through Dr. McEvoy’s leadership, the VIA opportunity is actively promoted during recruitment of new medical students, residents, and fellows with special interest in global medical service. She is a founding member of the Alliance for Surgery and Anesthesia Presence (ASAP), an advocacy and action group that builds awareness regarding the urgent need for safe global surgery and anesthesia facilities. In August 2013, ASAP became the 6th Integrated Society of the International Society of Surgeons, and Dr. McQueen was elected as president of this new international society. She also continues to serve as chair of the American Society of Anesthesiologists’ Global Humanitarian Outreach Committee, as well as directs the Global Surgical Consortium, a non-profit organization dedicated to improving surgical infrastructure in low income countries through data collection and advocacy. “The Vanderbilt community is a collaborative and nurturing environment for Global Health across the disciplines, and I am thrilled to be part of the anesthesia faculty and VIA Team” said Dr. McQueen. Kelly McQueen, MD, lectures to healthcare providers at Kijabe Hospital in Kenya. Dr. McQueen, who joined Vanderbilt Anesthesiology in 2012, has more than two decades of experience in international medical outreach. 19 Clinical Overview Serving in one of the largest clinical programs in the nation, the Vanderbilt Department of Anesthesiology’s clinicians provide procedural, critical care, pain management, and all perioperative anesthesia services for more than 90,000 adult and pediatric patient encounters annually at more than 100 anesthetizing locations. Of these, more than 10,000 patients are seen annually in the Vanderbilt Interventional Pain Clinic, and approximately 20,000 Vanderbilt adult and pediatric patients receive an anesthetic during a radiologic, gastrointestinal, or other diagnostic or therapeutic procedure. The department’s faculty, residents, fellows, certified registered nurse anesthetists (CRNAs), and nurse practitioners provide care in our operating rooms, five adult intensive care units, and the pediatric and neonatal intensive care units, and perform approximately 4,000 anesthetics per year in the labor and delivery suite. The faculty, residents, fellows, nurse anesthetists, and nurse practitioners provide services in three hospitals (Vanderbilt University Hospital, Monroe Carell Jr. Children’s Hospital at Vanderbilt, and the Nashville Veterans Administration Hospital) and five outpatient facilities. Specialized clinicians provide the full range of anesthetic techniques and procedures in the operating rooms, procedural suites, intensive care units, and pain management clinics. All surgical specialties are represented, including adult and pediatric cardiac surgery, all types of solid-organ transplantation, robotic surgery, neurosurgery, and high-risk obstetrics. Vanderbilt’s trauma service, which includes the orthopedic trauma program, is among the busiest in the nation. Tracy Jackson, MD, a member of the Pain Medicine Division, examines needle placement during a fluoroscopically guided radio frequency stimulation procedure. The operating room staff practices anesthesia care according to the Anesthesia Care Team model. Anesthetics are provided by one of the department’s highly skilled trainees or CRNAs under the direction of one of the medical faculty. By means of this model, the highest quality care is delivered in a safe and effective manner using the unique skills of all team members. ClinicalClinical Staff Staff of the Department Anesthesiology of the Department ofofAnesthesiology 300 Residents CRNAs Faculty 250 200 150 100 50 0 20 FY06 FY07 FY08 FY09 FY10 FY11 FY12 FY13 Vanderbilt Department of Anesthesiology is also known for innovation in the use and development of new technologies to deliver and improve patient care and to improve our educational offerings. The faculty use advanced human patient simulators to teach basic anesthesia skills, critical event response techniques, and team management in the operating rooms and intensive care units. Vanderbilt is one of the few medical training centers with a 3-D TEE simulator to teach the essential skill of cardiac ultrasound. The medical information systems at Vanderbilt are second to none and support the delivery of safe and efficient patient care. Perioperative record keeping is highly automated and managed through an anesthesia information management system developed by the Department of Anesthesiology. This system both enhances effective patient care and supports the clinical research program. Highlighted on the following pages are the services provided by the Vanderbilt Department of Anesthesiology’s clinical divisions. Department of Anesthesiology Clinical Volumes Department of Anesthesiology Clinical Volumes 120,000 Pain Procedures Out of OR 100,000 OR 80,000 60,000 40,000 20,000 - FY06 FY07 FY08 FY09 FY10 FY11 FY12 FY13 21 Division of Ambulatory Anesthesiology Katherine Dobie, MD, performs an ultrasoundguided block at the Vanderbilt Bone & Joint Surgery Center. “At Vanderbilt, we remind ourselves every day that ambulatory anesthesiology is rapidly evolving as a subspecialty, and we are going to be a big part of that,” said Ambulatory Anesthesiology Division Chief Katherine Dobie, MD. With a diverse patient and case mix, we are continually looking for new practices to improve our safety and quality. Currently, we have one of the highest patient satisfaction ratings within the institution, with minimal complications and minimal hospital transfers. At 13,000 patients and nearly 4,000 regional anesthetics yearly, we are proud of this. Growth coupled with enthusiasm is something we feel fortunate to have in our Division.” National statistics indicate that more than 70 percent of all surgeries are now performed in an outpatient setting. Vanderbilt’s Division of Ambulatory Anesthesiology meets the local manifestation of this increased demand with growth, both in locations and in additional services. In March 2011, the Division of Ambulatory Anesthesiology began providing anesthesia services at Vanderbilt’s newest ambulatory surgery center, Vanderbilt Bone & Joint in Franklin. The three-room center specializes in orthopedic procedures, and the expansion extended VUMC’s regional anesthesia services, including an at-home peripheral nerve catheter program, to Williamson and neighboring counties. The new site also added more than 3,000 ambulatory cases per year, to total nearly 13,000 cases annually in all of our outpatient centers. As NSC is primarily an orthopedic/sports medicine center, the majority of training in peripheral regional anesthesia occurs there. Under the leadership of Randall Malchow, MD, NSC Medical Director, Vanderbilt residents receive training in the techniques of ultrasound-guided regional blockade and the placement of regional catheters for homebased post-operative pain management. “We are unique among resident training programs in that we take the residents out of the OR for an eight-hour didactic training session at the beginning of their regional rotation,” said Dobie. “Attending anesthesiologists do the blocks that The Division of Ambulatory Anesthesiology was formed in 2008 and provides services for Vanderbilt University Medical Center satellite locations that include Nashville Surgery Center (NSC), Vanderbilt Outpatient Surgery (VOS), Cool Springs Surgery Center (CSSC), and Vanderbilt Bone & Joint Surgery Center. Two of the four centers are joint ventures where both Vanderbilt and community surgeons work, allowing for a broad base of cases rarely seen in an academic practice, including those requiring GI, ophthalmologic, ENT, plastic surgery, pediatric, urologic, neurosurgical, spine, orthopedic, and dental procedures. Vanderbilt Bone & Joint Surgery Center in Franklin, Tennessee, is the newest ambulatory surgery center in Vanderbilt University Medical Center’s network of satellite locations. 22 day, and residents do not start performing clinical regional anesthesia until we know they have a strong knowledge base. With the large volume of regional cases, residents and fellows leave our rotations equipped not only with technical skill, but also with an understanding of application in a high-volume, fast-paced environment. We have been able to do this without compromising efficiency.” Successful implementation of an outpatient catheter program, pioneered by Dr. Malchow in 2008, has allowed the migration of complex shoulder and foot and ankle cases out of the inpatient setting into the more patient-friendly ambulatory setting. All regional blocks are documented in Dr. Malchow’s comprehensive database for future academic research, which now contains 9,500 cases. The volume of pain management procedures offered at Cool Springs has also increased with the addition of a satellite location of the Vanderbilt Interventional Pain Center. Dan Lonergan, MD, who completed a Pain Medicine Fellowship at Vanderbilt, performs interventional pain procedures at the Cool Springs location to serve Williamson County and adjacent counties. Outpatient GI endoscopies have been increasing in volume at CSSC, and pediatric volume has been exponentially increasing at every center, with the largest percentage being pediatric ENT cases from community surgeons. Under the leadership of Jane Brock, MD, Cool Springs Surgery Center was named Symbion’s “Surgery Center of the Year” for 2011 and 2012. Cool Springs Surgery Center is located on Mallory Lane in Franklin, Tennessee. “This is a national recognition that we have enjoyed two years in a row; Dr. Brock’s leadership amidst tremendous growth and change has been outstanding,” said Dobie. The Vanderbilt outpatient surgery center (VOS) is primarily an ENT center where complex ear, sinus, and voice cases are performed, along with routine tonsillectomies and adenoidectomies. The Division of Ambulatory Anesthesiology is led by Dr. Dobie and includes five fulltime faculty, 21 CRNAs, and two to three residents who rotate through the program monthly. Nashville Surgery Center is located on Patterson Street in Nashville, Tennessee. 23 Division of Anesthesiology Critical Care Medicine The Division of Anesthesiology Critical Care Medicine provides critical care services in the cardiovascular ICU, neurological ICU, surgical ICU, and burn ICU at Vanderbilt University Medical Center and at the surgical ICU at the Tennessee Valley Health Care System Nashville Veterans Administration Medical Center. To address growing demands of critical care services with the recent opening of the 11-story Critical Care Tower, the division has expanded to include 21 anesthesiology intensivists along with more than 35 acute care nurse practitioners (ACNPs) and physician assistants (PAs), making it one of the largest critical care divisions in the country. The division operates using a multidisciplinary, intensivist-led critical care team model that includes ACNPs and PAs; this paradigm is being replicated with increasing frequency across the nation. for five years. Fellows have a diverse clinical experience through our subspecialty ICUs and an innovative didactic program of lectures delivered by multispecialty faculty, problem-based learning discussions, simulations, workshops, journal clubs, and an interactive web-based learning portal. Faculty and fellows participate in teaching the Fundamentals in Critical Care Support (FCCS) and the Advanced Trauma Life Support (ATLS) courses. In addition, faculty from the division have taken leadership roles in medical student education through the development of Immersion Courses and Critical Care Skill programs as part of the redesigned curriculum of the Vanderbilt University School of Medicine. An ongoing alliance between the Critical Care Division and the School of Nursing also supports an ACNP Intensivist training program. The Division of Anesthesiology Critical Care Medicine strives to provide excellent patient care, promote education, and engage in scholarly activity. Faculty and fellows routinely participate in CME activities and workshops to maintain and acquire new skills to keep abreast of modern technology and the changing spectrum of caring for the critically ill. This includes proficiency in ultrasound, echocardiography, and management of patients with ventricular-assist devices or who are on ECMO. By encouraging research to identify better ways to care for perioperative and critically ill patients, the division takes a proactive approach to the ever-changing demands and regulations in healthcare and the changing milieu of critical care. Active research programs in the Division of Anesthesiology Critical Care Medicine encompass both clinical and translational research and focus on perioperative risk factors and mechanisms of cognitive impairment, kidney injury in cardiac and non-cardiac patients, sepsis and its monitoring, education and implementation science, health resource utilization, multisensory training, and quality improvement projects. Active grants in the division include an RO1, a K23 training grant, and a FAER Education grant, in addition to numerous smaller industry and Vanderbilt Institute for Clinical and Translational Research (VICTR) grants. Faculty have been involved in more than 20 peer reviewed manuscripts and textbook chapters in the past academic year alone. Division faculty, who are involved in the training and mentoring of critical care fellows and residents from many disciplines, also participate in educational activities at the local, regional, national, and international level. The Critical Care Anesthesia Fellowship itself has recently been expanded to eight ACGME-accredited fellowship positions per year, accepting fellows with both anesthesiology and surgical training, and the fellowship has received accreditation Division of Anesthesiology Critical Care Medicine: Front row, left to right: Jonathan Shoopman, MD; William Costello, MD; Justin Sandall, DO (Fellow); James Mykytenko, MD; Josh Squiers, ACNP; Ryan Henderson, ACNP; Stuart McGrane, MD; David Hall, MD; Chris Hughes, MD; Lisa Weavind, MD; Pratik Pandharipande, MD; Lindsay Trantum, ACNP; Patrick Henson, DO; Frederick “Josh” Billings, MD; Steve Widmar, ACNP. Second row, left to right: Sheena Weaver, MD; Tracy McGrane, MD; Anna Fong, ACNP; Nathan Ashby, MD; Meg Shiffrin, ACNP; Jayme Gibson, ACNP; Roy Neely, ACNP; Ryan Truesdale, ACNP; Lee Parmley, MD, JD; Laura Wilkinson, ACNP; Arna Banerjee, MD. Not pictured: Holly Brooks, ACNP; Justin Calabrace, ACNP; John Barwise, MD; Jodi Cressler, ACNP; Olga Dayts, ACNP; Edmund Donahue, PA; Jamie Gibson, ACNP; Elizabeth Heitman, PhD; Amanda Hill, ACNP; April Kapu, ACNP; Jason Kennedy, MD; Hannah Maloney, ACNP; Lauren Nevels, ACNP; Nahel Saied, MD; Chad Wagner, MD; Nora Azzazy, MD; Jeff Barton, PA, Debra Cirone, ACNP; Donald Crabtree, MD; Gregory Evans, MD; Ailish Garrett, ACNP; Irina Gault, MD; Molly Goidel, ACNP; Meredith Golden, PA; Emily Holcombe, ACNP; Katherine Jackowski, ACNP; Ariel Kappa, ACNP; Michelle Kearney, ACNP; Avinash Kumar, MD; Jean Anne Leininger, MD; Aimee Marlar, PA; Roy Neeley, MD; Monica Nevels, ACNP; Kellie O’Connell, ACNP; Andrea Primm, ACNP; Christina Riley, ACNP; Briana Rogers, ACNP; Emily Spring, PA; Melissa Wiley, ACNP; Laura Wilkinson, ACNP; Joey Williams, ACNP; Briana Witherspoon, ACNP. 24 Division of Cardiothoracic Anesthesiology The Division of Cardiothoracic Anesthesiology is led by Robert Deegan, MD, PhD, and includes ten faculty members and ten nurse anesthetists. Each month, three residents rotate through the service. The fellowship program, under the leadership of Annemarie Thompson, MD, expanded in 2013 to three fellows trained annually. The Division is a microcosm of the larger department within which it resides, supporting the tripartite missions of clinical excellence, academic pursuits in anesthesiology, and education. practice, and is performed on nearly all adult cardiac patients. The cardiothoracic anesthesiologists are also increasingly in demand to provide intra-procedure TEE in the electrophysiology suite to, for example, rule out thrombosis of the atrial appendage, to guide trans-septal puncture, and to look for evidence of cardiac tamponade. All studies are performed and interpreted by the cardiothoracic anesthesiologist, and cases are digitally archived for future study. Innovation, research, and education are all key components of the division, as is evidenced by its support of novel clinical environments in the hybrid cath lab/OR, the introduction of transesophageal echocardiography as an invaluable monitoring tool in intensive care units, many research initiatives, and a strong commitment to being a national leader in cardiothoracic anesthesia education. The Division Cardiothoracic Anesthesiology faculty conduct research in vascular system function, cardiopulmonary conditioning, renal failure, and perioperative inflammatory response. Extramural grant support comes from the American Heart Association and the National Institutes of Health. The division works alongside the surgeons and cardiologists of the Vanderbilt Heart and Vascular Institute to perform approximately 1,200 adult cardiac procedures a year. These include coronary artery bypass grafting (the majority of which are performed off-pump), valvular surgery, cardiac transplantation, adult congenital procedures, hybrid bypass procedures, aortic aneurysm and dissection repair, and ventricular assist device (VAD) insertions. The VAD program dramatically expanded in 2013 to a rate of about 80 per annum. The TAVR program (percutaneous aortic valve replacement for severe aortic stenosis in patients who are too high risk for open-heart surgery) began in 2011, and approximately 100 TAVRs are completed annually (Corevalve and Sapiens). The division also has significant external and internal education presence. Division faculty have hosted successful workshops in perioperative transesophageal echocardiography (TEE) and hemodynamic echo, drawing anesthesiology residents, fellows, faculty, and private practitioners from throughout the region. Cardiothoracic anesthesiologist Julian Bick, MD, received a $100,000 Research in Education Grant from the Foundation for Anesthesia Education and Research which is used to train CA-1 residents in TEE. A TEE simulator, which provides 3-D, computer-generated views of the heart as a probe is guided through a mannequin, is housed at Vanderbilt’s Center for Experiential Learning and Assessment (CELA). The division’s TEE training is conducted with the simulator as the centerpiece. In addition to cardiac surgery, the division works with thoracic surgeons to perform about 600 thoracic cases annually, including thoracotomy, mediastinoscopy, lung transplantation, and esophageal procedures. Anesthesia services are also provided for bronchoscopies, placement of internal cardiac defibrillators, valvuloplasty, electrophysiology procedures, and septal ablations, which together account for approximately 2,500 cases annually. A subset of the division’s faculty is also board-certified in intensive care medicine. These individuals rotate through the cardiovascular intensive care unit, under the direction of division faculty member Chad Wagner, MD. Intraoperative transesophageal echocardiography (TEE) is an integral part of the clinical Division of Cardiothoracic Anesthesiology: Front row, left to right: Julian Bick, MD; Annemarie Thompson, MD; Susan Eagle, MD; and Robert Deegan, MD, PhD. Back row, left to right: Chad Wagner, MD; Mias Pretorius, MD; Jason Kennedy, MD; and Frederick “Josh Billings,” MD. Not pictured: Jeremy Bennett, MD; Antonio Hernandez, MD; and Brigitte Messenger, MD. 25 Certified Registered Nurse Anesthetists More than 100 Certified Registered Nurse Anesthetists are a critical component of the anesthesia care team model used at Vanderbilt University Medical Center. The Vanderbilt Department of Anesthesiology embraces the anesthesia care team approach to patient care, involving anesthesiologists and residents, certified registered nurse anesthetists (CRNAs), student registered nurse anesthetists (SRNAs), and anesthesia technicians. The more than 115 CRNAs at Vanderbilt provide anesthesia for all types of surgical procedures, including cardiac, pediatrics, vascular, trauma, neurosurgery, plastics, radiologic, and special procedures. CRNAs administer general, regional, and monitored anesthesia care for scheduled and emergency surgical, obstetric, and diagnostic procedures. Key job responsibilities of the CRNA include preoperative patient evaluation, management of the patient through completion of the operative procedure, safe transport of the patient to the recovery area, and assurance of the appropriate postoperative care. Additionally, CRNAs provide instruction and education for student nurse anesthetists (SRNAs). They also support the residency educational mission by providing service coverage to allow residents to attend educational activities and participate in elective rotations. Thus, the CRNAs are essential to many core endeavors. In terms of personnel, the CRNA Division is the largest division within the Department of Anesthesiology. Vanderbilt is the primary clinical affiliate of the Middle Tennessee School of Anesthesia (MTSA) in Madison, Tennessee, which is the second largest nurse anesthesia program 26 in the country. Vanderbilt is also the primary clinical affiliate for the Union University Nurse Anesthesia program in Jackson, Tennessee. Student nurse anesthetists assist in approximately 7,000 anesthetics per year while on Vanderbilt rotations. SRNA coordinators are CRNAs Brad Koss and Andrew Philips. The CRNA Division mirrors the VUMC operating room pod organization, and the service specialist position within the CRNA structure improves communication with all pod members. The six service specialists are Neurosurgery Service Specialist Tammy Freehling; AOS/Ortho Service Specialist Kathy Mitchell; General Oncology/Urology Service Specialist Ken Donnell; Opthalmology/Otolaryngology/Oral Surgery/ Plastics Service Specialist Mark Haffey; Out-of-OR Service Specialist Ki Szmyd-Hogan; and Pediatric Cardiothoracic Service Specialist Lewis McCarver. In addition to SRNA training, the CRNA division has developed a strong program of Continuing Education Unit-eligible educational programs designed specifically for CRNAs. These programs are overseen by CRNA Educator Mike Leersnyder. Chief CRNA Steve Blanks and Assistant Chief CRNA Buffy Krauser-Lupear direct the CRNA Division. Five designated lead CRNAs are Brian Reid in Ambulatory; Paul Wilson in Obstetric/ Gynecology; Edith Newberry in Adult Cardiac; Amanda Dickert in Pediatrics; and John Butorac in Multispecialty Adult Anesthesia. Anesthesia Technicians Provide Critical Support Vanderbilt University Medical Center is staffed with 38 anesthesia technicians who contribute to safe, efficient anesthesia care by providing highly skilled assistance to anesthesiologists and nurse anesthetists at both on- and off-campus clinical locations. Anesthesia technician duties include equipment maintenance and servicing, running laboratory tests on blood samples, maintaining quality assurance records, and operating a variety of equipment used to monitor, evaluate, and manage the patient undergoing anesthesia. As the level of the anesthesia technician’s training, experience, and knowledge increases, the anesthesia technician provides closer intraoperative support to the anesthesia provider. The department offers structured classroom lectures to train technicians in a nondistracting clinical setting. The anesthesia technician, the certified anesthesia technician, and the certified anesthesia technologist cover areas related to the following adult and pediatric services: neurosurgery, plastics, urology, ophthalmology, vascular, trauma, cardiothoracic, general surgery, orthopedics, obstetrics/gynecology, and ENT. They also provide support for special procedures in the radiology department that include MRI, PET scan, radiation oncology, GI Lab, CT Scan, nuclear medicine, and the cardiac catheterization lab. Buffy Krauser-Lupear, Assistant Chief CRNA, oversees the Anesthesia Technician Program. Sue Christian, a certified anesthesia technologist and long-time member of the Vanderbilt team fills the Anesthesia Technician Manager/Educator position. The technical staff continues to evolve with greater emphasis being placed on teamwork and advancing clinical skills. Anesthesia technicians with specialized training operate autotransfusion equipment at Vanderbilt. Members of the anesthesia technician team at VUMC include, left to right, Ray Brazill and Mao Shinoda. 27 Division of Multispecialty Adult Anesthesiology The Division of Multispecialty Adult Anesthesiology is the department’s largest division, providing perioperative anesthetic care for more than 12,000 patients annually in 45 operating rooms and procedure suites for a wide variety of surgical services, including general surgery, orthopedics, urology, plastic surgery, ophthalmology, vascular surgery, otolaryngology, hepatobiliary surgery, liver and renal transplantation, and oral/maxillofacial surgery. MSA faculty and staff also provide 24-hour coverage for emergency and trauma surgery for the region. The division has 48 full- and part-time faculty members, most of whom have significant subspecialty training and expertise. An additional MSA activity is providing preoperative consultations. MSA Division faculty provide anesthesiology residents a wide variety of introductory and advanced clinical experiences and make many contributions to the educational programs for medical students, residents, and fellows. Additionally, MSA faculty teach and supervise residents from other specialties, as well as student registered nurse anesthetists who rotate in the MSA Division. Division faculty pursue a wide range of academic interests including regional anesthesia, airway management, information technology, perioperative cognitive dysfunction, echocardiography, and ultrasound imaging. The division’s members are also highly active in research, with numerous investigator-initiated clinical research projects currently in progress. MSA Division Chief James Berry, MD, believes the division’s multi-year research efforts to demonstrate the value of wireless monitoring of post-operative patients will ultimately lead to institution-wide adoption of the technology. By using wireless monitors that collect patients’ vital signs in post-op areas not typically monitored, nursing staff can be notified and medical staff would be able to respond immediately if abnormal readings are detected. Division of Multispecialty Adult Anesthesiology: Front row, left to right, Letha Mathews, MD; Amy Robertson, MD; Tekuila Carter, MD; Steve Hyman, MD; James Berry, MD; Clifford Bowens, MD; Michael Pilla, MD; Kofi Kla, MD; and Brian Rothman, MD. Second row, Michael Higgins, MD; Raj Gupta, MD; Jesse Ehrenfeld, MD, MPH; Chairman Warren Sandberg, MD; Marc Hayes, MD; Jason Lane, MD; James Blair, DO; and Edward Sherwood, MD, PhD. Not pictured: Brian Allen, MD; Eswara Botta, MD; Eric Briggs, MD; Jane Brock, MD; Susan Calderwood, MD; Chris Canlas, MD; Meera Chandrashekar; Katherine Dobie, MD; Jane Easdown, MD; Jean Fischer, MD; William Furman, MD; Stephen Harvey, MD; Loren Hemachandra, MD; Patrick Henson, MD; Shannon Hersey, MD; Doug Hester, MD; Scott Hoffman, MD; Kenneth Holroyd, MD; Lisa Jaeger, MD; Shannon Kilkelly, MD; Randall Malchow, MD; Jeffrey Martin, MD; Kelly McQueen, MD; Stephanie Rasmussen, MD; Staci Ridner, MD; Thomas Shultz, MD; Paul St. Jacques, MD; Jonathan Wanderer, MD; Matthew Weinger, MD; and Robert Wells, MD. 28 Division of Neurosurgical Anesthesiology For the third year in a row, Vanderbilt’s departments of Neurology and Neurological Surgery have ranked among the top of U.S. News & World Report’s “America’s Best Hospitals.” Neurosurgery and other neurologic services continue to expand at Vanderbilt University Medical Center, and faculty specializing in neurosurgical anesthesiology are providing increasingly complex anesthesia and sedation services. The Clinical Neurosciences Institute, a collaborative group established at Vanderbilt in 2011 by the departments of Neurology, Neurological Surgery, and Psychiatry to provide comprehensive patient care, continues to attract increasing numbers of referrals for service. The Vanderbilt Department of Neurological Surgery currently has the highest volume of deep brain stimulator implantation in North America. The Vanderbilt Brain Tumor Center provides comprehensive care for patients with brain tumors, and more than 400 major brain tumor operations are performed annually. More than 2,839 neurologic cases required anesthesia in fiscal year 2012. Because of these exciting changes in the Department of Neurological Surgery requiring increased demand for neurosurgical anesthesiology expertise, a separate division devoted to this subspecialty was created in September 2013. Anesthesiology Chair Warren Sandberg, MD, PhD, recruited Lorri Lee, MD, formerly a professor in the Department of Anesthesiology and Pain Medicine at the University of Washington, to head the division. Dr. Lee is nationally recognized for her work on outcomes and complications related to the perioperative management of neurosurgical procedures, primarily through the American Society of Anesthesiologists Closed Claims Project. She is also widely known for her efforts as a member of the Anesthesia Patient Safety Foundation Executive Committee and Newsletter coeditor. One of Dr. Lee’s primary goals is to make the division a national leader in neuroscience research through collaborative efforts with the departments of Neurological Surgery and Neurology, while maintaining the excellent clinical reputation that the division has earned. Current research in the department by Drs. Jesse Ehrenfeld, Letha Mathews, James Blair, and Koffi Kla and neurosurgeons in the Department of Neurological Surgery involve a series of clinical research projects aimed at improving patient outcomes and costeffectiveness. Paramount to the success of this newly created division is the collegial working relationship among team members. Dr. Letha Matthews, the newly appointed associate chief of the division, commented, “What excites me most is the successful collaboration that we have among the neurosurgical, anesthesia, and nursing teams. Our experienced and dedicated neuroanesthesia and neurointensivist faculty ensure that our quality of care is outstanding, resulting in one of the shortest average lengths-of-stay in the country following brain tumor surgery.” It is the patient that benefits most from the camaraderie of the clinical providers, as top quality care is consistent throughout the perioperative period. Four experienced certified registered nurse anesthetists led by Tammy Freehling, CRNA, are dedicated to neuroanesthesia services and are an integral part of the patient care Lorri Lee, MD Division Chief, Division of Neurosurgical Anesthesiology team. Avinash Kumar, MD, FCCP, and his neurointensivist team provide comprehensive intensive care management of critically ill neurosurgical patients in VUMC’s state of the art ICU. VUMC has six designated neurosurgical operating rooms where anesthesia services are provided for operations, including brain tumor, blood vessel malformation, aneurysms, stroke intervention, trauma, complex spinal procedures, functional neurosurgery, and chronic pain management. The Division of Neurosurgical Anesthesiology also provides specialized anesthesia services for “awake craniotomies” where patients are intermittently awake to facilitate speech and motor mapping during surgery to preserve the most vital areas of the brain. Anesthesia is also provided by the division in neurointerventional radiology suites, and at Monroe Carell Jr. Children’s Hospital at Vanderbilt. Like their surgical colleagues, neuroanesthesiologists face many unique challenges, including the length of procedures, which may last more than 16 hours in the OR, unusual patient positioning, and unexpected intraoperative events such as seizures or intracranial hemorrhage. “We are manipulating neurophysiology with drugs and other interventions during the procedure to facilitate surgery while we share the target organ with the neurosurgeons,” said Dr. Mathews. Residents on the neurosurgical anesthesia rotation find the ability to have an immediate impact on the operation exciting and gratifying, as do the faculty leading the training. Drs. Jane Easdown and Sheena Weaver have developed educational modules to illustrate these clinical concepts. Dr. Lee noted: “We all went to medical school to make a difference in patients’ lives, and neuroanesthesiology is one of the best fields to accomplish that goal every day.” 29 Division of Obstetric Anesthesiology Division of Obstetric Anesthesiology: Left to right, Sarah Starr, MD; Jill Boyle, MD; Ray Paschall, MD; Michael Richardson, MD; John Downing, MD; Curtis Baysinger, MD; Matthew Buck, MD; and Adrienne Rey, MD. The Division of Obstetric Anesthesiology provides dedicated, 24hour in-house obstetric care for approximately 4,000 deliveries at Vanderbilt University Medical Center annually, nearly half of which are considered high risk. The team also provides anesthesia services for approximately 2,500 gynecologic and other surgical procedures for primarily women in a suite of three operating rooms. In addition to offering the full complement of techniques for labor analgesia, the division provides consultation and critical care management services for high-risk obstetric patients, as well as specialized anesthesia care for fetal surgery. The resumption of in utero repair of myelomeningocele, a procedure pioneered at Vanderbilt University Medical Center in 1997, has brought an added dimension of specialized clinical service to the Division of Obstetric Anesthesiology. The results of a seven-year National Institutes of Health-funded trial, Management of Myelomeningocele Study (MOMS) demonstrated clear benefit for babies who undergo fetal surgery to treat spina bifida. These surgeries began again at VUMC in April 2011. The MOMS trial found fetal surgery significantly improved the child’s chances of being able to walk. There was no increased risk of death for the baby or the mother when the fetal surgery group was compared with a group that received surgery after birth. With patients being referred from across the nation, it is estimated that about 15 of these procedures will be performed at VUMC annually, with Obstetric Anesthesiologist Ray Paschall, MD, taking the lead in providing anesthetic care for these complex cases. Trainees in the Division of Obstetric Anesthesiology, including both residents (three each month) and fellows, receive extensive experience in the care of clinically challenging patients. In 2012, the Division of Obstetric Anesthesiology received ACGME 30 accreditation for their fellowship program. The Division is among the first 11 programs in the country that received approval from the ACGME/Resident Review Committee. The program received the full, three-year accreditation, and the first ACGME fellow completed his training in July 2013. The Division also has a number of on-going clinical research projects, including studies on various anesthetic techniques on patient outcomes. Research projects concerning transversus abdominis block for the relief of pain following Cesarean delivery, factors affecting the choice of pain relief during labor, and the effects of low-molecular-weight heparin on thromboelastographic measurements are ongoing. The Division has also recently resumed work examining the effects of obstetric and anesthetic drugs on both the maternal and fetal vasculature within the placenta using a dual-perfusion technique of isolated placenta tissue subunits. Research examining the transfer of drugs across the placenta from the maternal to fetal side is also planned, as well as work to understand the ion channel expression within in the vasculature of the placenta. The Division of Obstetric Anesthesiology is directed by Curtis Baysinger, MD, who will be stepping down from the position in early 2014. To then fill the role of division chief, the department has recruited one of the specialty’s top leaders, who has a longstanding reputation in innovative research, an impressive list of academic accomplishments, and a strong record in national leadership. The Division of Obstetric Anesthesiology includes six other faculty members, two CRNAs, and one administrative assistant. The division’s faculty members have all completed Obstetrical Anesthesia fellowship training and have extensive experience in obstetric care, regional anesthesia, and acute pain management. Division of Pain Medicine Chronic pain affects an estimated 100 million people in the United States – more than diabetes, heart disease, and cancer combined – according to the Institute of Medicine of the National Academies. In particular, the roles of select surgeries and cancer survival resulting in persistent chronic pain states are growing and are of interest to Anesthesiology. Because pain is complex and often involves physiological, psychological, emotional, and environmental factors, clinicians at Vanderbilt University Medical Center’s Pain Management Center utilize a multidisciplinary approach to pain care, offering thorough evaluations, consultations, and referrals to optimize available treatment modalities. “The Center is for all patients who have pain, regardless of cause and what has or hasn’t been done previously,” said Marc Huntoon, MD, Chief of the Division of Pain Medicine and Director of the Vanderbilt Pain Management Center. “It is the first stop for pain patients at Vanderbilt.” The Pain Management Center sees patients with all types of pain, including back, neck, abdominal, pelvic, nerve and joint pain, and chronic headache. During the first clinic visit, a patient’s medical history is thoroughly reviewed, and his or her condition is evaluated by Vanderbilt pain specialists to develop a teambased treatment plan. This team could include specialists from anesthesiology, psychology, psychiatry, neurology, neurosurgery, orthopedics, and rehabilitation. In partnership with the Vanderbilt Center for Integrative Health, the new EMPOWER program (Empowerment and Mindfulness Program for Outpatient Wellness, Education, and Rehabilitation) is being developed to offer those patients with recalcitrant pain syndromes new hope. The program focuses on education, functional improvement, and improvements in pain, anxiety, and other related issues. Pain Management Center physicians also work closely with a patient’s primary care providers to close the loop effectively and foster shared responsibility of patient health. “Providers at the primary care level often haven’t had the right resources for pain care,” Dr. Huntoon said. “At the Pain Management Center, we build relationships with primary care providers, get patients the care they need, and work on an ongoing basis with the providers. We see it as a very collaborative and supportive relationship.” The Vanderbilt Medical Group Pain Advisory Council, which first met in April 2010, began to envision a pain center, striving Division of Pain Medicine: Front row, left to right, Irina Phillips, MD; Meenal Patil, MD; Heather Jackson, NP; Tracy Jackson, MD; and Becca Ognibene, PT. Second row, left to right, Dan Lonergan, MD; Kurt Dittrich, MD; Marc Huntoon, MD; Chris Sobey, MD; and Amy Turner, RN. Not pictured: Natalie Strickland, MD; Brent Dilts, MD; John Corey, MD; and Janie Smith, MD. 31 to create an easy referral resource for both Vanderbilt physicians and outside providers that offered cutting-edge care based on the latest evidence. When Huntoon arrived at Vanderbilt in June 2011, he had much the same plan. “Many institutions try to achieve this to some extent but are unable to coordinate the multi-disciplinary vision,” Huntoon said. “The idea is that pain crosses many boundaries. No one specialty has the knowledge and capabilities to best serve all patients, but if we put our heads together, we can ensure optimal care.” The Pain Management Center and Interventional Pain Clinic are housed at Vanderbilt Health One Hundred Oaks, just off Interstate 65 in Tracy Jackson, MD, performs a fluoroscopically-guided block for a patient at the Vanderbilt Interventional Pain Nashville, Tennessee. The Interventional Pain Clinic’s Center. surgical service for patients with pain syndromes requiring the 7,000-square-foot space expertise of the Division of Pain Medicine faculty. The belief is includes state-of-the-art procedure rooms, exam rooms, recovery that patients admitted to Vanderbilt University hospitals should bays, and multidisciplinary rooms. In July 2011, a branch of have access to expert pain care, regardless of the reason for the Interventional Pain Center opened in the Cool Springs area admission. The Department of Anesthesiology’s interventional of Williamson County, under the direction of Vanderbilt Pain pain implantable device practice is also growing, and the CPS Medicine faculty member Dan Lonergan, MD. Services are also manages our own patients who are admitted for either device provided at the Cool Springs Surgery Center on Mallory Lane in trials or permanent implants. Providing targeted pain control for Franklin. both chronic and acute pain at the area of injury has produced better pain control, improved patient satisfaction, and the ability Monroe Carell Jr. Children’s Hospital at Vanderbilt is the site to reduce patients’ time in the hospital. of a unique Pediatric Pain Clinic, where Vanderbilt providers work with patients, their families, and their physicians to provide Expanding pain medicine education at Vanderbilt, from the the best pain management for the pediatric patient’s specific medical student level up, is a goal of Dr. Huntoon and the needs. The clinic sees two to three new patients every week, division. The Regional Anesthesia and Acute Pain Fellowship has and additional patients who live at a distance are monitored by already proven successful under the leadership of Lisa Jaeger, telephone. The Neonatal Intensive Care Unit at the Children’s MD, with two fellows in 2013-2014 learning advanced regional Hospital has its own specialized pain management program, and anesthesia and acute pain, developing into educators for residents, there is a regional anesthesia program to treat young patients as and growing to be scholars by developing research studies for well. publication. In addition, the division’s chronic pain fellowship The Comprehensive Pain Service (CPS) at VUMC also continues grew to include three fellows in 2012-2013. Both the acute and chronic pain fellowships are integral parts of the educational to grow as patients are benefitting in increasing numbers from continuum. Dr. Huntoon hopes to continue to incorporate pain epidural catheters, peripheral nerve blocks, and peripheral nerve medicine topics into the medical student curriculum and to catheters for pain management for complex shoulder and arm improve both resident and fellow initiatives in the specialty, surgery, knee arthroplasties, extensive ankle restorations, and making use of Vanderbilt’s advanced simulation technology, as repeated burn debridements. The CPS began in August 2012 as well as the anatomy lab setting. a new vision for in-hospital pain care that builds on the overall vision of the Pain Program. The new service continues to build capacity and capability to see consults from any medical and 32 Division of Pediatric Anesthesiology A much anticipated $30 million, 33-bed expansion at the Monroe Carell Jr. Children’s Hospital at Vanderbilt in 2012 has kept the Division of Pediatric Anesthesiology on their toes, finding ways to provide top-quality clinical services more efficiently, while keeping both young patients and their families happy. the nurse practitioners who work with the Division of Pediatric Anesthesiology in preoperatively preparing patients for anesthesia or sedation. Jill and her team work with Dr. Kilkelly in the scheduling and coordination of various care teams, as well as helping families navigate the process. In September 2013, Suanne Daves, MD, was named vice-chair for Pediatric Anesthesiology, a key leadership role for both the Department of Anesthesiology and the Monroe Carell Jr. Children’s Hospital at Vanderbilt. In 2012, Dr. Daves was named Anesthesiologist-in-Chief of the Children’s Hospital. Dr. Daves joined the Anesthesiology Department in December 2008 as an associate professor in the Division of Pediatric Cardiac Anesthesiology. She was then appointed chief of the Pediatric Cardiac Division in January 2009. Education and training of medical students, anesthesia residents, nurses, and associated healthcare personnel is a major faculty commitment. Several anesthesiology residents rotate on pediatric anesthesiology services each month and gain experience in the management of patients undergoing both routine and complex surgical procedures, as well as diagnostic and interventional procedures performed outside the operating room. The Pediatric Anesthesiology Fellowship Program offers a year of subspecialty training in pediatric anesthesia and perioperative care, including critical care and pain management. Knowing they were facing increasing demands on their resources with the hospital’s expansion, members of the Division of Pediatric Anesthesiology began examining their processes under a microscope, identifying areas for improvement. One example is their participation in an initiative to improve perioperative care processes. The initiative is led by a task force consisting of a surgeon, the nurse managers of the OR and the Holding/PACU areas, two business analysts, and Daniel Roke, MD, from Anesthesiology. The group initially focused on First Case Starts, examining the preoperative process thoroughly. Based on their recommendations, first case start times improved dramatically. The on-time first case start rate was 38% in April 2010 and is now above 70%, assuring that more patients and families have a timely start to their procedure. Modifications were also made in the areas of pediatric pain services and in pediatric radiation services to increase efficiency and serve more patients. With Stephen Hays, MD, and Drew Franklin, MD, both having dedicated clinical time to see patients, the number of patients seen in the pediatric pain clinic has tripled, and both internal and external referrals continue to increase. Peter Chin, MD, oversees anesthesiology services for pediatric radiology, and through finding better ways to manage patient flow, volume has increased and Saturday service for MRI procedures has been added. Areas of academic interest to the division’s faculty include quality improvement, airway management, pediatric pain management, regional anesthesia, ECMO, and perioperative care of cardiovascular patients. The Division of Pediatric Anesthesiology is an active member of Wake Up Safe, a quality improvement initiative of the Society for Pediatric Anesthesia. It is a Patient Safety Organization (PSO) composed of the leading children’s hospitals throughout the country. Through voluntary reporting from its member institutions, Wake Up Safe has developed the first-ever national registry of adverse perioperative events in pediatric patients. Its goal is to help define quality in pediatric anesthesia and develop strong quality improvement systems in an effort to help improve anesthetic care in children of all ages. The division provides perioperative care for more than 13,000 patients per year at Children’s Hospital, the region’s major pediatric referral center. The division’s 21 attendings, 22 CRNAs, and four fellows provide services for a variety of pediatric surgical procedures, including general surgery, ENT, neurosurgery, urology, and orthopedics. The division provides anesthesia services for procedures outside the operating room, including oncology, gastroenterology, and diagnostic and therapeutic radiologic procedures. Faculty also provide both acute and chronic pain management services. Jill Kilkelly, MD, an assistant professor in the division, spearheads a unique service at Children’s Hospital known as the CCoC (Complex Coordination of Care). Many children require frequent sedation or anesthesia for procedures or diagnostic testing. Frequent anesthetics create a tremendous burden for these patients and their families in terms of time away from school and work, as well as restrictions on eating and drinking before procedures. The goal of the CCoC is to provide a single, continuous anesthetic for multiple procedures or scans. While this sounds simple, the scheduling of multiple surgical and interventional services, often in different locations, is challenging. Jill Kinch, MSN, is the manager for Division of Pediatric Anesthesiology: Front row, left to right, Liz Hughes, MD; Kevin Saunders, MD; John Algren, MD; Stephen Hays, MD; and Kimberly Nesbitt, MD. Second row: Laura Zeigler, MD; Peter Chin, MBBS; Amanda Lorinc, MD; Jill Kilkelly, MD; and Thomas Romanelli, MD. Back row: Dan Roke, MD; Humphrey Lam, MD; Andrew Franklin, MD; Thomas Austin, MD; and Mark Newton, MD. Not pictured: Christopher Karsanac, MD; and Vikram Patel, MD. 33 Division of Pediatric Cardiac Anesthesiology As demand for pediatric cardiac anesthesia services at Monroe Carell Jr. Children’s Hospital at Vanderbilt continues to grow, the anesthesiologists providing those services are committed to ensuring that the quality and safety of patient care is continually improved as more patients are served. members, Gina Whitney, MD, and Suanne Daves, MD, are also board certified in Critical Care and are members of the Pediatric Cardiac Critical Care Division. They split their time between caring for pediatric cardiac patients in the operating room and in the cardiac critical care unit. In fact, one of the biggest accomplishments of the Division of Pediatric Cardiac Anesthesiology was to tackle the problem of unnecessary blood transfusions and wasted blood products during the treatment of critically ill children. The division’s effort reduced the number of transfusions by anesthesiologists in pediatric cardiac operating rooms by an average of 40%. And their success did not go unnoticed. The Pediatric Cardiac Anesthesiology Division was selected to be in the inaugural Vanderbilt Quality and Patient Safety Pioneer Program. Selection was based on proposed improvement goals, evidence of past improvement efforts, and leader participation. Through the Quality and Patient Safety Pioneer Program, the division’s members received training, as well as support, to design, implement, and test additional performance improvements. The group is tapping into valuable, archived patient data to guide their quality improvement plans. “The ability to continue care through the entire perioperative period has positively impacted the intraoperative management of our cardiac patients,” added Daves. “For example, the operative and critical care teams developed a ‘Hand-Over’ protocol that facilitates communication of intraoperative information to the ICU team. The second part of this process improvement project, ‘Hand-Over Part II,’ aims to standardize the physical presentation of the critically ill neonate between the ORs and ICUs.” “This is one of our initiatives, to use that data to improve patient care,” said Vice-Chair for Pediatric Anesthesiology Suanne Daves, MD. “We will be looking for outliers in areas like length of intubation and central line complications in order to make intelligent decisions to improve patient care.” Children with heart defects represent a complex group of patients who often require intensive surgical repairs to thrive or even survive into adulthood. The Division of Pediatric Cardiac Anesthesiology was formed in 2007 to support the growth of the program that cares for these patients at the Children’s Hospital. The division’s faculty members also provide intraoperative and catheterization laboratory anesthesia care. Two faculty Members of the Pediatric Cardiac Anesthesiology Division also team with surgeons for highly specialized procedures such as placement of Berlin Heart devices. The device is similar to other left ventricular devices (LVADs) used in adults, but is much smaller. The pediatric cardiac anesthesiologists work closely with nurse anesthetists trained in cardiac anesthesia care who have many years’ experience working with these unique patients. The division also trains pediatric and cardiothoracic clinical anesthesia fellows, as well as provides expert assistance and consultative services for children with congenital heart disease who are undergoing non-cardiac surgery/procedures. In the 2012-2013 academic year, several faculty members participated in the annual meetings of the Society of Cardiovascular Anesthesiologists, the Society for Pediatric Anesthesia, and the Congenital Cardiac Anesthesia Society, and the division’s members are actively involved in education and quality improvement at the national level. Division of Pediatric Cardiac Anesthesiology: Suanne Daves, MD; Scott Watkins, MD; Gina Whitney, MD; Brian Donahue, MD, PhD; and Alex Hughes, MD. 34 Vanderbilt Preoperative Evaluation Center (VPEC) Manager of Patient Care Services Russell Kunic, FNP-BC, front row right, and staff members at the Vanderbilt Perioperative Evaluation Center’s TVC location show off their 5-Star Award for Overall Quality of Care. The Vanderbilt Preoperative Evaluation Center (VPEC) continues to earn praise from the patients that come through its doors for evaluation before undergoing surgery at Vanderbilt University Medical Center. In 2013 – for the fifth year in a row – the service received a Professional Research Consultants, Inc. patient satisfaction award, the coveted 5-Star Award for Overall Quality of Care. This means the center scored at the 90th – 99th percentile based on 2012 calendar year results and as compared with similar centers nationwide. For the second time, both VPEC sites, the main Vanderbilt University Hospital location and the location at Vanderbilt Health at One Hundred Oaks, received the awards. “VPEC faculty and staff perform comprehensive patient assessments and consult with our patients’ primary care physicians, specialists, and surgeons,” said VPEC Clinic Manager Russell Kunic, FNP-BC. “We are able to make decisions regarding the need for preoperative testing to assess the patients’ overall risk for surgery. Once the patient report is completed at VPEC, it becomes part of the patient’s electronic medical record and is accessible by any Vanderbilt medical provider with Internet and security access.” To ensure that patients undergoing scheduled procedures are properly evaluated and that all necessary labs and other patient information are in hand, VPEC offers a free evaluation and consultation service. This better ensures patient safety and helps prevent surgical delays and cancellations. The inpatient arm of VPEC completed more than 1,500 preoperative assessments in 2012. Also in 2012, VPEC clinicians evaluated 20,027 patients in clinic, or approximately 60% of all on-campus adult surgical patients. VPEC’s main location at Vanderbilt University Hospital has 11 exam rooms and is conveniently located adjacent to outpatient lab and radiology on the first floor of The Vanderbilt Clinic. VPEC’s second location at the Vanderbilt Health at One Hundred Oaks campus has seven exam rooms and is also adjacent to outpatient lab and radiology services. Additionally, VPEC is expanding to reach patients at a distance through phone interviews and is building an infrastructure that will make it possible to evaluate patients with telemedicine and through other virtual processes. VPEC includes 25 total staff, including 13 nurse practitioners, one of the largest single groups of nurse practitioners at Vanderbilt. Serving as VPEC’s Medical Director and Associate Medical Director are Vanderbilt Anesthesiologists Jonathan P. Wanderer, MD, MPhil, and Michael Pilla, MD. 35 Veteran’s Affairs Anesthesiology Service The Veteran’s Affairs Anesthesiology Service provides perioperative patient care services for more than 9,000 anesthesia procedures annually at the Veterans Administration Medical Center in Nashville and the Alvin C. York campus in Murfreesboro, Tennessee. The service provides anesthesia care for the full range of surgical procedures, including cardiac and thoracic surgery; orthopedic procedures including joint replacements; as well as major vascular, neurosurgical, ENT, ophthalmic, urologic, plastic, bone marrow, and transplant surgeries. In addition, sedation services are provided in several out-of-OR sites, including electro-convulsive therapy, diagnostic and therapeutic radiology procedures, pulmonary procedures, cardiac catheterization, electrophysiologic studies, cardioversion, and transesophageal echocardiography and gastroenterology services. The service also provides primary coverage for the VA surgical intensive care unit, acute and chronic pain management, and emergency airway management. In addition to patient care, education is a prime mission for the VA Anesthesiology Service. In addition to training senior anesthesiology residents and fellows, the service also educates critical care and emergency room physicians and other allied personnel in airway management skills outside the operating room. This excellence in teaching is demonstrated by the fact that, each year since 2009, a VA faculty member has received either a Golden Apple Award (given by Anesthesiology Department residents for superior teaching) or the Volker Striepe award (given by residents for superior teaching and mentorship). “Even though 80% of our surgical patients are ASA3 and 4, our morbidity and mortality rate is lower than the national average,” said Veteran’s Affairs Anesthesiology Service Chief Ann Walia, MBBS. “We have 85% on-time first-case starts, and a DOS case cancellation rate of less than 1%. For the past five years we have achieved 100% compliance with all National Performance Measures. We have a great team here, and they work hard to provide excellent care to our veterans.” The Division, led by Ann Walia, MBBS, is staffed by 21 anesthesiologists, 15 certified registered nurse anesthetists, eight nurse practitioners, three residents, a critical care anesthesiology fellow, four health technicians, and four administrative staff members. Areas of academic interest in the division include airway management, ultrasound-guided regional anesthesia, ischemiareperfusion injury and coronary artery disease in liver transplant recipients, and anesthesia practice pattern variations in liver transplantation. These have resulted in several national and international presentations and publications. The Veteran’s Affairs Anesthesiology Service provides a full range of perioperative care to veterans at VA medical campuses in Nashville and Murfreesboro. 36 Research Overview Major translational research initiatives at Vanderbilt University are moving discoveries from the bench to the bedside, and our scientists are working to transform both health care and health care delivery. In federal fiscal year 2012, the Vanderbilt University School of Medicine ranked 13th among U.S. medical schools for National Institutes of Health (NIH) funding, and VUSM funding from all sources has more than doubled since 2001. In academic year 2011, faculty across all disciplines received more than $521 million in external funding for research. The Vanderbilt Department of Anesthesiology is a key contributor to the institution’s standing as it is consistently ranked one of the top extramurally funded anesthesia research programs in the nation. In 2012, the department’s investigators brought in more than $8.5 million in total extramural research funding. This includes more than $3.39 million in awarded NIH grants in federal fiscal year 2012, which placed Vanderbilt Anesthesiology 12th among U.S. academic anesthesiology departments in NIH funding. Edward Sherwood, MD, PhD, joined Vanderbilt’s Department of Anesthesiology faculty in July 2012 as Vice Chair for Research, and he oversees all of the department’s investigational endeavors. A distinguished translational physician-scientist, Dr. Sherwood previously served as Vice Chair for Research and Professor/James F. Arens Endowed Chair of the Department of Anesthesiology as well as Director of the MD-PhD Combined Degree Program at the University of Texas Medical Branch in Galveston, Texas. The vision of the Research Division is to improve upon the department’s currently successful program by fostering excellence, collaboration, and the development of young investigators. The Vanderbilt Department of Anesthesiology has a strong, multifaceted approach to research, including: • A strong Basic Science Research Division, under the leadership of Eric Delpire, Ph.D., focusing on ion channel physiology and pain mechanisms. • The Perioperative Clinical Research Institute (PCRI), which provides all support services needed for successful clinical research. Numerous investigator-initiated and industrysponsored clinical studies are being conducted with the support of PCRI. • Best-in-class anesthesia and perioperative information systems, with complete control of application development and a dedicated team of analysts devoted to making electronic data widely available to investigators and quality improvement teams. These systems are managed by Perioperative Informatics, an institutional entity directed by Brian Rothman, MD. • The Vanderbilt Anesthesiology & Perioperative Informatics Research (VAPIR) Division, which is actively leveraging historical and current clinical data, with the goal of generating research and new control algorithms to positively impact patient safety under the leadership of Jesse Ehrenfeld, MD. • Strong statistical support from statisticians within our faculty with expertise in experimental design and complex analyses of large datasets. • The Center for Research and Innovation in Systems Safety (CRISS), which serves as an institution-wide resource for basic and applied research in healthcare informatics, patient safety and clinical quality, and designs and evaluates informatics user interfaces, care processes, and medical technology across Vanderbilt University Medical Center. In addition to providing a solid research infrastructure, the Department of Anesthesiology places a strong emphasis on faculty and fellow career development in academic anesthesiology. Active mentoring programs pair young investigators with experienced scientists in both basic and clinical research. The department’s B.H. Robbins Scholars Program provides a mentored research experience that is initiated during residency and culminates in a two-year clinical & research fellowship. Scholars may request to participate in clinical or basic science fellowship training or pursue additional formal education (e.g., Masters of Science in Clinical Investigation, Master of Public Health, Master of Science in Statistics) offered at Vanderbilt during the latter part of the program. Read more about the Vanderbilt Department of Anesthesiology’s specific research strengths on the department’s web site under the Research heading: www. vandydreamteam.com. The Vanderbilt Department of Anesthesiology’s multi-faceted approach to scientific investigation includes well-established basic science research laboratories as well as many successful endeavors in clinical research. 37 Labs Focus on Translational Science Basic Science Research Division: First row, left to right, Research Vice Chairman Edward Sherwood, MD; Albena Kozekova; Kelen Taylor; Sreedatta Banerjee; Kristie Lee; Basic Science Research Chief Eric Delpire, PhD; and Svetlana Stepanovic, PhD. Second row, Melissa Chont; Kerri Rios; Kevin Currie, PhD; Yin Guo, Julia Bohannan, PhD, and Afeef Husni, PhD. Back row, Stephen Bruehl, PhD; Mark Jewell, MS; Franck Potet, PhD; Jose Ponce-Coria, PhD; Jerod Denton, PhD; and Rene Raphemot. Not pictured: Daniel Swale, PhD; Jingbin Wang; and Liming Luan. The major focus of the Basic Science Research Division is the study of the physiology, pharmacology, and cell biology of ion channels, transporters, and receptors. These membrane proteins are involved in functions as diverse as shaping the cardiac action potential, salt and water homeostasis in the kidney, hormone and neurotransmitter release, modulation of synaptic transmission, and the gating/processing of pain signals. Because the disruption of each of these physiological processes has a significant impact on human health, research in the Basic Science Research Division addresses the translational missions of the National Institutes of Health and of private biomedical research-oriented foundations. Currently, there are two major themes that cut across multiple laboratories: drug discovery and the study of pain mechanisms. Three laboratories within the Research Division are actively pursuing drug discovery for clinically relevant ion channel and transporter targets. This work is sponsored by the National Institutes of Health Molecular Libraries Probe Center Network. Work in the laboratory of Jerod Denton, PhD, is aimed at understanding the integrative physiology and therapeutic potential of inward rectifier potassium (Kir) channels. Dr. Denton’s group employs high-throughput screening, medicinal chemistry, ion channel electrophysiology, and molecular modeling to develop small-molecule Kir channel probes used to interrogate Kir channel structure, function, and physiology. The Denton lab recently developed the first small-molecule probes of the renal outer medullary potassium channel, ROMK (Kir1.1) (Lewis et al., Mol. Pharmacol., 76: 1094-1103, 2009; Bhave et al., Mol. Pharmacol., 79: 42-50, 2011), an emerging diuretic target for hypertension (Denton et al., 2013). They are also developing pharmacological probes of the astroglial Kir channel, Kir4.1, which may represent a novel target for hypertension and epilepsy. Dr. Denton’s team was recently awarded a Grand Challenges in Global Health grant from the Foundation for the National Institutes of Health to develop chemicals to induce “kidney” failure in the mosquito Anopheles gambiae to help 38 fight malaria. Other work in Dr. Denton’s lab is funded by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) and the National Institute of Neurological Disorders and Stroke (NINDS). The lab of Eric Delpire, PhD, studies the regulation of intracellular Cl- in central and sensory neurons, and the regulation of renal salt transport mechanisms. The lab devised a screen to identify potent and specific inhibitors of a transporter, KCC2, involved in modulating inhibitory neurotransmission. By pumping Cl- ions out of neurons, this K-Cl cotransporter maintains a low intracellular Cl- concentration, strengthening inhibitory GABA- and glycine-mediated inhibition. This cotransporter is therefore involved in preventing hyperexcitability and the development of epileptiform activity. After developing a fluorescence-based methodology to visualize the activity of KCC2, Dr. Delpire’s group screened a 250,000 compound library and identified multiple inhibitors and some putative activators of KCC2 (Delpire et al. Proc Natl. Acad. Sci. 106: 5383-5388, 2009). Synthesis and analysis of a number of chemical variants of the most promising chemical scaffold yielded more potent inhibitors whose properties are being further analyzed (Delpire et al. Bioorganic & Med. Chem. Lett. 22: 4532-4535, 2012). The Delpire group also uses computational modeling to study protein-protein interaction and to design drugs that interact with the regulatory domains of protein kinases which regulate the ion transporters. Another interest in the Basic Science Research Division is the study of pain and pain mechanisms. Leading the effort in translational work bridging the basic and clinical sciences is Stephen Bruehl, PhD, who studies endogenous pain modulatory systems, links between these systems and psychological factors, and mechanisms contributing to chronic pain and pain-associated cardiovascular co-morbidities. Work in his lab has identified painrelated alterations in interacting cardiovascular-pain modulatory systems that contribute to enhanced pain responsiveness (Bruehl et al., Pain 2010; 149: 57-63) and may elevate future risk for both chronic pain (Walker et al., Pain 2010; 150: 568-572) and hypertension (Chung et al., Pain 2008; 138: 87-97). Work in Dr. Bruehl’s lab also explores how endogenous opioid pain inhibitory systems are intertwined with brain mechanisms underlying regulation of negative affect (Bruehl et al., Psychosom Med, 2011 Sep;73(7):612-9) and how these opioid systems are altered by persistent pain (Bruehl et al., Pain 148:167-171, 2010). His current National Institute on Drug Abuse-funded project examines predictors of responsiveness to opioid analgesic medications and the role of individual differences in endogenous opioid function in those predictive effects (Bruehl et al., Pain 154:1856-1864, 2013). Dr. Bruehl is also collaborating with Dr. Denton to identify variants in genes encoding G protein-coupled Kir (GIRK) channels that may influence opioid modulation of pain pathways, including responsiveness to opioid analgesic medications (Bruehl et al., Pain 2013 Aug 27. doi:pii: S03043959(13)00475-2; epub ahead of print). Dr. Bruehl mentors B. H. Robbins scholar Carrie Menser, MD. The lab of Kevin Currie, PhD, investigates the regulation of voltage-gated calcium channels and neurotransmitter/hormone release. Members of the CaV2 calcium channel family are expressed on presynaptic nerve terminals of primary afferent nociceptors and play key roles in pain transmission. The Currie lab investigates how neuromodulators, inflammatory mediators, and drugs alter channel function and transmitter release (Jewell Rebecca Brindley, PhD, is a member of the Kevin Currie laboratory, where the team studies the regulation of voltage gated calcium channels and neurotransmitter/hormone release. Jerod Denton, PhD, at left, and Rene Raphemot work together in the Denton lab to study novel methods of mosquito control. et al, Mol Pharmacol 79, 987-996; 2011; Zamponi & Currie, Biochim Biophys Acta 1828, 1629-43; 2013). This includes dissecting the cellular mechanisms by which gabapentin acts (Todd et al, Anesthesiology 116: 1013-24; 2012). Gabapentin is commonly used to treat chronic neuropathic pain, but can also exert acute perioperative analgesic effects and blunt intraoperative hemodynamic perturbations. The sympatho-adrenal stress response, in particular release of adrenal catecholamines and neuropeptides, is another area of focus in the Currie lab. Current projects investigate how G protein coupled receptors (including opioid receptors) and the serotonin transporter, an important target for antidepressants, orchestrate precise control of catecholamine secretion. The Currie lab, in collaboration with the Baudenbacher lab in the Department of Biomedical Engineering, is also developing novel microfluidic devices for “lab-on-a-chip” analyses of neurosecretion (Ges et al, Biosensors & Bioelectronics 34, 30-36; 2012). The laboratory of Eric Delpire, PhD, is also involved in pain research including the examination of the role of ion cotransport mechanisms in the modulation of GABA and glycine neurotransmission in the terminals of primary afferent fibers and in spinal cord neurons. The presynaptic terminals of primary afferent fibers are loaded with Cl- anions through a secondary active transport mechanism (NKCC1) that pumps Cl- into the cell against its electrochemical gradient equilibrium potential. High Cl- allows depolarization of the terminals upon GABA release and presynaptic inhibition. On the postsynaptic side, a different transporter, KCC2, pumps Cl- out of the cell, strengthening GABA and glycine inhibition. Tom Austin, MD, a B.H. Robbins scholar in the Delpire laboratory, devised a method of implanting intrathecal catheters in mice for the delivery of novel compounds targeting the postsynaptic transporter. The study showed that inhibition of KCC2 shortened the response to heat-evoked nociceptive signals (Austin and Delpire, Anesth. Analg. 113(6): 1509-1515, 2011). Dr. Austin is supported by a Foundation for Anesthesia Education and Research (FAER) Mentored Research Training Grant. 39 In October 2012, Brad Grueter, PhD, and Carrie Grueter, PhD, joined the Department of Anesthesiology. The husband-wife team are doctoral graduates of the Department of Molecular Physiology and Biophysics at Vanderbilt University. The goal of the Grueter lab research program is to advance the current understanding of the nucleus accumbens (NAc), a brain region responsible for integrating information from diverse inputs and modifying complex motivated behaviors, including its involvement in adaptive responses to rewarding and aversive stimuli. Specifically, the lab strives to elucidate the molecular constituents in the NAc that are necessary and sufficient to drive complex motivated behaviors. As part of the mesolimbic dopamine system, the NAc integrates a complex mix of excitatory, inhibitory and modulatory inputs to optimize adaptive motivated behaviors. Dynamic alterations in synaptic transmission within this circuitry are strongly implicated in the development and expression of many neuropsychiatric disorders. Thus, two broad questions addressed are: 1.) How does in vivo experience such as cocaine exposure, pain, or high fat diet alter the neurocircuitry of the NAc? 2.) What are the synaptic mechanisms underlying the behavioral adaptations to in vivo experience? The approaches the Grueter lab incorporates allow the researchers to thoroughly characterize the synaptic circuitry of the NAc in basal and pathophysiological conditions using a combination of cutting edge techniques in electrophysiology, molecular biology, metabolic phenotyping, optogenetics and behavior. These studies will provide information on how the NAc circuits integrate environmental stimuli and allow for specific behavioral responses. This enhanced understanding of NAc function may provide a basis for a more individualized approach to the treatment of many psychiatric disorders. The lab of Edward Sherwood, MD, PhD, is studying several aspects of sepsis and the systemic inflammatory response syndrome. A major interest is to define mechanisms of sepsisinduced systemic inflammation and organ injury with emphasis on the roles of natural killer (NK) and T lymphocytes. Current studies are being performed to evaluate the mechanisms of NK and T cell activation and chemotaxis during sepsis with emphasis on the chemokine receptor CXCR3 and its ligands, CXCL9 and CXCL10. The Sherwood group showed that CXCR3 activation is crucial for NK cell trafficking during sepsis and that CXCR3 blockade will decrease inflammation and organ injury in experimental models of sepsis. The underlying goal is to further understand the contribution of CXCR3 activation in the pathogenesis of sepsis and develop clinically relevant interventions to block CXCR3 and improve outcome. In further studies, Dr. Sherwood’s lab group is evaluating the immunomodulatory properties of TLR4 agonists and their ability to modify the host response to systemic infection. The group showed that the TLR4 agonists lipopolysaccharide and monophosphoryl lipid A are potent immunomodulators that alter systemic cytokine production and enhance innate resistance to bacterial infections. The improved resistance to infection is caused by neutrophil expansion and enhanced neutrophil functions. The group is working to define the mechanisms by which TLR4 agonists promote the antimicrobial functions of neutrophils and develop TLR4 agonists as agents that can be used 40 Kerri Rios works in the laboratory of Eric Delpire, PhD, where the group identifies inhibitors of a transporter, KCC2. clinically to improve the resistance of critically ill patients to infection. Together, the members of Basic Science Division of the Department of Anesthesiology pursue a mutually complementary and collaborative program of research to create new knowledge leading to improved practice in anesthesiology. Moreover, the division provides critical mentorship to a new generation of anesthesia clinician scientists who will help bind the basic science and clinical missions of the department together even more effectively. Key Clinical Research Studies Key Clinical Research Studies Homeless Surgical Patients: Optimizing Care and Follow-Up Bret Alvis, MD: RIFL (Rigid and Flexing Laryngoscope) vs. Fiberoptic Bronchoscope: A Comparison of the Ease of Use During Intubation on Difficult Airways Impact of Attending Surgical Case Coverage on Perioperative Outcomes Curtis Baysinger, MD: Effects of Tadalafil (Cialis), a Long-acting PDE5 Inhibitor, on the Human Fetoplacental Microcirculation: A study Using the in Vitro, Dual-perfused, Single-isolated Cotyledon, Human Placental Model Impact of On-time OR Starts on Workflow Perceptions Multi-Center, Double-Randomized, Double-Blind, Placebo-Controlled Study to Evaluate the Analgesic Efficacy and Safety of Intravenous CR845 Dosed Preoperatively and Postoperatively in Patients Undergoing a Laparoscopic Hysterectomy Tyler Berutti, MD: Delirium in Critically Ill Children: Prevalence, Risk Factors and Outcomes. Impact of Diabetes Quality Improvement Protocol Impact of Sexual Orientation and Gender Identity on Health Outcomes Incidence and Impact of Hypoxemia During Surgery and Anesthesia Information Management Systems for Continuous Evaluation and Feedback Multicenter Performance Site (MPS) Normothermia and the Risk of Surgical Site Infection Frederic T. Billings, MD: The Effect of Short-term Atorvastatin Use on Acute Kidney Injury Following Cardiac Surgery Objective and Novel Approach to Resident Competency Measurement: Utilizing Data from Anesthesia James L. Blair, DO: Does Continuous Perioperative Dexmedetomidine Infusion Reduce Time to Discharge in Patients Undergoing Major Lumbar Fusion? A Double-Blind, Placebo-controlled Study Predictors of Post-Operative Deterioration Peri-anesthetic Imaging of Cognitive Decline (PAICOD) – A Prospective Pilot Study Clifford Bowens, MD: Comparison of Perineural Catheter Depth for the Continuous Popliteal Nerve Block using Ultrasound Guidance and Dermabond Stephen P Bruehl, PhD: Hypogonadism and Pain Christopher Canlas, MD: Perioperative Pulse Oximetry in Obstructive Sleep Apnea Patients in the Ambulatory Setting Elizabeth Card, RN: Prevalence of Delirium in the Post Anesthesia Care Unit Brent Dilts, MD: Ultrasound-guided Cervical Medial Branch Blocks for Diagnosing Cervical Facet Joint Pain Katherine Dobie, MD: Takeover of a Private ASC Practice by Academic Anesthesiologists: A Retrospective Before and After Study Over Two Years. Ultrasound-guided Isolation and Blockade of the Upper Trunk for Shoulder Surgery: Time to Replace the Traditional Interscalene Approach? Jesse M. Ehrenfeld, MD, MPH: Automatic Identification of Postoperative Events Using Advanced Informatics Tools Automatic Prediction of Perioperative Events Awareness and Prevention of Acute Lung Injury Central Line Placement Under Ultrasound: Are Routine Chest X-rays Warranted? Does Use of Non-depolarizing Neuromuscular Blocking Agents Predict Postoperative Respiratory Complications? Effects of Protease Inhibitors on Post-operative Pain Control Effect of a Novel Electronic Blood Ordering System on Patient Outcomes Perioperative Risk Stratification of Surgical Patients Prevalence of Red-Green Colorblind Healthcare Providers: Pilot Study Real-Time Evaluation of Perioperative Risk Scores Technology Diffusion and Uptake Into and Across Anesthesia Departments Understanding the Impact of Health Literacy and Perioperative Outcomes United States Critical Illness and Injury Trials Group (USCIITG) Informatics Working Group (IWG) Utility of the Surgical Apgar Score on Postoperative Outcomes in Pediatrics Using Natural Language Processing to Identify Lesbian, Gay, Bisexual, Transgender and Intersex (LGBTI) Patients Daniel France, MD: Efficiency Evaluation of Mobile Clinical Information System Andrew Franklin, MD: Open-label, Multicenter Study of the Safety of Twice Daily Oxycodone Hydrochloride Controlled-release Tablets in Opioid Experienced Children from Ages 6 to 16 Years Old, Inclusive, with Moderate to Severe Malignant and/or Nonmalignant Pain Requiring Opioid Analgesics Open-label, Extension Study to Assess the Long- Term Safety of Twice Daily Oxycodone Hydrochloride Controlled-release Tablets in Opioid Experienced Children Who Completed the OTR3001 Study Stephen R. Hays, MD: Multisite RCT Comparing Regional and General Anesthesia for Effects on Neurodevelopmental Outcome and Apnea in Infants Pediatric Anesthesia NeuroDevelopment Assessment Study (PANDAS) Randomized, Placebo Controlled, Multicenter Study of the Efficacy, Pharmacokinetics (PK) and Pharmacodynamics (PD) of Intravenous (IV) Acetaminophen for the Treatment of Acute Pain in Pediatric Patients Evaluation of Disparities in Care of Perioperative Patients Genomic Impact on Patient Response to Anesthesia 41 Multicenter Study of the Safety, Tolerability, Effectiveness, and Pharmacokinetics of Oxymorphone HCl Extended-Release Tablets in Pediatric Subjects Requiring an Around-the-Clock Opioid for an Extended Period of Time Open-Label, Non-Randomized, Multicenter, Ascending Dose by Age, Single-and Multiple-Dose Evaluation of the Effectiveness, Safety, and Tolerability of Oral Liquid Oxymorphone HCl Immediate-Release Oral Liquid for Acute Postoperative Pain in Pediatric Subjects Patrick Henson, DO: Study Evaluating the Expression of Effectors of Immune Tolerance and Associated Infectious Outcomes in Burn Patients Douglas Hester, MD: King Vision Video Laryngoscope vs. Glidescope Video Laryngoscope: A Comparative Study in Ambulatory Surgery Center Patients Marc Huntoon, MD: Controlled, Two-arm, Parallel Group, Randomized Withdrawal Study to Assess the Safety and Efficacy of Hydromorphone Hydrochloride Delivered by Intrathecal Administration Using a Programmable Implantable Pump Heidi Smith, MD: Pediatric Delirium: Validation of the Preschool Confusion Assessment Method for the Intensive Care Unit (psCAMICU) Assessing the Compliance and Reliability of a Unit-wide Rollout of a Nursing Delirium Screening Tool in a Pediatric Critical Care Unit. Paul St. Jacques, MD: King Vision Video Laryngoscope vs. the McGrath Video Laryngoscope: A Comparative Study Sarah Starr, MD: Initiation of a Nitrous Oxide Service: Implications for Patient Access to Obstetric Anesthesia Services Chad Edward Wagner, MD: Multicenter Retrospective hTEE Review Jeffrey Waldman, MD: Ischemic Kidney Injury During Liver Transplantation Surgery Steve A. Hyman, MD: Survey to Determine the Level of Honesty in Survey Participants When Asked About Personal Drug Usage Ann Walia, MD: Incidence of Coronary Artery Disease and Morbidity and Mortality in Patients with Coronary Artery Disease that Underwent Orthotopic Liver Transplantation Christopher Karsanac, MD: Tonsil and Adenoidectomy PACU Questionnaire QI Project Jonathan P. Wanderer, MD, MPhil: An External Validation of the Z-Score System for Normalizing Residency Evaluations Michael Leersnyder, CRNA: Congruence of Perceived Effective Clinical Teaching Characteristics Between Students and Preceptors of Nurse Anesthesia programs (Part I & II) Determinants of Variation in Anesthetic Drug Costs Lesley Lirette, MD: Comparing Efficiency in Delivering Regional Anesthesia in a Teaching Model Style Outpatient Surgery Center vs. A Non-trainee Outpatient Surgery Center External Validation of the Risk Quantification Index Daniel Lonergan, MD: Opioid Detoxification Outcomes in an Outpatient Chronic Pain Clinic Letha Mathews, MD: Radiographically Measured Neck Motion during Intubation with MILS by Two Different Video Laryngoscopes Matthew McEvoy, MD: Effect of a Cognitive Aid on Adherence to the American Society of Regional Anesthesia Guidelines for Management of Patients on Anticoagulation Evaluation of Electronic Screening Tools for Preoperative Assessment Factors Influencing Resident Case Preference Impact of GasChart Notifications on Anesthesia Provider Behavior Utilization of Perioperative Antiplatelet Drugs in Patients with Coronary Stents Understanding The Use of Electronic Pre-operative Notes through EMR Audit Logs Prediction of Airway Management Difficulty from Patient Photographs Perioperative Fluid Management and Outcomes Quantification of Variability in Anesthesia Residency Training Test of Automated Device for Code Recording Scott Watkins, MD: Improving Team Performance in Simulated Pediatric Emergencies Through Incorporation of Non-Technical Skills into an Electronic Decision Support Tool Effect of a Cognitive Aid on Adherence to Perioperative Guideline Thanh Nguyen, MD: Phase IV, Open-Label, Safety Study Evaluating the Use of Dexmedetomidine in Pediatric Subjects Undergoing Procedure-type Sedation What is the Prevalence of Vitamin D Deficiency Among Children Undergoing Posterior Spinal Fusion? Michael Pilla, MD: A Study of Belmont Rapid Infusion Devices Michael Richardson, MD: Quality Emergency Obstetric Care: Evaluation of the Obstetric Emergency Team (OBET) Response System Warren Sandberg, MD, PhD: Assessment of FAER’s Investment in the Career Development of Anesthesiologists Survey of Departmental Approaches to Meeting JC Ongoing Professional Practice Valuation and Focused Professional Practice Evaluation Requirements 42 Edward Sherwood, MD: The Introduction of Quantitative Neuromuscular Monitoring in the PACU: Impact on Residual Blockade and Postoperative Recovery Liza Weavind, MD: Phase III, Randomized, Double-Blind, PlaceboControlled, Adaptive Design Study of the Efficacy, Safety, and Tolerability of a Single Infusion of MK-3415 (Human Monoclonal Antibody to Clostridium difficile toxin A), MK-6072 (Human Monoclonal Antibody to Clostridium difficile toxin B), and MK-3415A (Human Monoclonal Antibodies to Clostridium difficile toxin A and toxin B) in Patients Receiving Antibiotic Therapy for Clostridium difficile Infection Vanderbilt Lands Patient-centered Research Grant Thanks to a federal grant received by Vanderbilt University Medical Center, researchers, patients and their families now have an active role and voice in research designed to improve the quality and safety of patient care. VUMC investigators were awarded a two-year, $750,000 grant from the Patient Centered Outcomes Research Institute (PCORI), one of the first grants awarded by the nonprofit institute established by the Patient Protection and Affordable Care Act of 2010 and the first such grant awarded in Tennessee. The PCORI’s mission is to help patients, providers and other healthcare stakeholders make informed care decisions by producing and promoting information resulting from research guided by patients, caregivers and the broader healthcare community. The Vanderbilt research will track both patients’/patient families’ and clinicians’ reports of “non-routine” events in four different clinical areas: elective pediatric cardiac surgery, outpatient pediatric oncology (chemotherapy administration), adult day surgery, and adult patients with acute coronary syndrome who are undergoing cardiac catheterization. A non-routine event is defined as any event that deviates from optimal or expected care for a specific patient in a specific clinical situation. A multidisciplinary team of nearly 30 Vanderbilt faculty/physicians and staff, including nurses, surgeons, anesthesiologists, oncologists, cardiologists, pediatricians, engineers, psychologists, anthropologists, statisticians and informatics personnel, are working together on the project. Select patients and patient family members who are members of Vanderbilt’s PatientFamily Advisory Council also are part of the research team. “I’m excited that Vanderbilt received one of these highly competitive grants,” said U.S. Representative Jim Cooper (D-Tenn.), a strong supporter of the mission of the PCORI. “This important research, done right here in Nashville, will help improve health care delivery and outcomes for patients and their families all over the country.” Matthew Weinger, MD, professor of Anesthesiology, Biomedical Informatics, and Medical Education, and director of the Center for Research and Innovation in Systems Safety (CRISS), is the study’s principal investigator. Dr. Weinger and his staff had previously developed a standardized process for capturing reports of non-routine events from clinicians, and the PCORI-funded study is building on this knowledge to also capture and understand what patients and their families consider non-routine events. Non-routine events in clinical settings have been shown to occur frequently and are typically due to multiple factors. In a previous study of 910 elective surgical cases representing a cross-section of anesthesia techniques, surgical procedures, and patient complexity, 39% of cases contained at least one non-routine event, and of those cases, 42% included more than one non-routine event. In another study, 107 intensive care unit nurses reported medication-related nonroutine events (incorrect medication or dosage) in 31 of 153 fourhour observation periods in three different hospitals. “This project is important because we will be able to determine what aspects of their interaction with the healthcare system patients and families feel reflect lower quality of care and safety,” said Weinger, who is also the Norman Ty Smith Chair in Patient Safety & Medical Simulation. “I believe we will also show that patients and their families will provide important new information about ways to change how we deliver care so that it is safer and better meets their needs. “A unique aspect of this research will be the involvement of patients in designing the studies and analyzing the results,” added Weinger. Only 50 pilot projects out of more than 1,000 applications were selected to receive this first round of PCORI funding. Awards approved include those for projects designed to develop a range of tools and techniques aimed at improving patient-centered care and decision-making; create new patient-centered care measures; and improve delivery of patient-centered counseling in health care settings. A federal grant awarded to VUMC researchers actively involves patients and patient families in a study hoped to improve the quality and safety of patient care. Members of the research team include Diane H. Buckberg, Jessica Pasley, principal investigator Matthew Weinger, MD of the Department of Anesthesiology, and Susan Morley. Buckberg, Pasley and Morley are Vanderbilt Patient-Family Advisory Council members. 43 Putting the Power of Technology into Practice The Vanderbilt Department of Anesthesiology has long been a national leader in the development and advancement of perioperative informatics, and there’s been an increased focus in recent years to further strengthen the informatics initiatives at Vanderbilt. “This department has always had a very strong commitment to informatics, and many notable accomplishments in the field,” said Department Chairman Dr. Warren Sandberg. “By bringing some key talent on board and by providing the faculty already here the dedicated time and necessary staff to expand and improve our informatics programs, we are looking forward to dramatically impacting our specialty, and patient care in total, through new research and technology.” A combination of world-class research, active software development, and utilization of the latest clinical applications allows the department to drive the use of technology within anesthesiology to improve patient safety and quality. Advances in both research and clinical care are being facilitated by several faculty members in the department, many of whom have additional faculty appointments in the Department of Biomedical Informatics. The two key groups affiliated with the department driving this effort are the Vanderbilt Anesthesiology & Perioperative Informatics Research (VAPIR) Division and Perioperative Informatics. Perioperative Informatics Patients at VUMC who are either diabetic or to whom glucose is being administered are closely monitored through use of a tool developed through a collaboration between the VAPIR Division and Perioperative Informatics. As seen in this pop-up, medical providers are notified about a patient’s glucose monitoring status at appropriate intervals. their awareness of patients who were at risk of having OSA so that the increased anesthetic and perioperative risks could be proactively mitigated as much as possible. This tool was also combined with new preoperative nursing screening questions to further help identify those patients with OSA to support postoperative evaluation and intervention by respiratory therapy before leaving the perioperative space. • Integrated Presence: Perioperative Informatics has partnered with Vanderbilt’s Informatics Center to pilot a new web-based version of Vigilance TM, Integrated Presence. Vigilance TM has delivered situational awareness in the perioperative environment since 2004. Integrated Presence was created to bring situational awareness to the bedside for every provider. Situational awareness is an understanding and awareness of what is happening around you, accomplished by the perception of environmental elements, comprehension of their meaning and prediction of a future state based on those elements and their meaning. Improving situational awareness is thought to improve patient safety and work efficiency while reducing costs and is especially effective when providers are responsible for more than one active care location. It is expected that the advantages realized in the perioperative space will be seen in the inpatient care environments across Vanderbilt in conjunction with a bedside monitoring initiative. • Phases of Care: The time patients spend in the Postoperative Anesthesia Care Unit (PACU) is dependent on the type of surgery performed, patient comorbidities, and the planned disposition. Significant enhancements to VPIMS’ postoperative nursing electronic documentation Perioperative Informatics, a group directed by Brian Rothman, MD, Medical Director of Perioperative Informatics, is a hospital entity that develops and manages the clinical applications used within the perioperative setting. The Vanderbilt Perioperative Information Management System (VPIMS) application suite developed and commercialized by Vanderbilt includes GasChartTM for electronic anesthesia documentation, VigilanceTM which improves clinicians’ situational awareness, the iOS-based situational awareness mobile application VigiVUTM, and PatientTrackerTM for electronic nursing documentation during each perioperative phase of care. “Our job is to solve known or previously unidentified issues related to workflow and system functionality while understanding how these two elements intersect,” said Rothman. “We are identifying unique solutions that improve patient safety, operating room efficiency, the quality and character of the data collected, staff workflow, and that decrease cognitive workload on our staff through a combination of creative software design and development, with a particular focus on user interface.” Following are a few recent Perioperative Informatics successes. • 44 Electronic Obstructive Sleep Apnea (OSA) Screening: Identifying our obstructive sleep apnea (OSA) patients in 2013 has been more important than ever with OSA now seen as a growing, silent epidemic. Armed with the STOP-Bang screening tool that has been used manually at other institutions, the Perioperative Informatics team used existing data from their electronic preoperative evaluation tool, along with new data introduced through module enhancements, to create a complete electronic OSA screening tool in six weeks. The result was an automated STOP-Bang score delivered to providers, heightening An innovative hand hygiene monitoring application was developed internally at Vanderbilt. module now support postoperative nursing’s ideal workflow. The accumulation of discrete, contemporaneous data related to patient location, phase of care, and planned disposition paves the way for improved PACU efficiency, patient care, and throughput. This data will soon be externalized to VUMC’s bed management team to aid in efforts to improve patient throughput throughout the institution. • Documentation Compliance: The VPIMS anesthesia documentation module, GasChartTM, effectively collects a large amount of data for compliance and billing purposes. However, in response to recent changes in compliance regulations, the Perioperative Informatics team has further improved the documentation processes. Implementation of a forced function now ensures that attendings document what emergency surgery is planned and the indication that qualifies it as an emergency. In addition, the development team has implemented case checks to ensure that minute-by-minute, in-room provider times are accurate and reasonable. These changes have resulted in improved documentation quality and significant time savings for Vanderbilt’s billing staff. Over the next year, the development team will improve documenting lines and monitors and regional anesthesia procedures while reducing ambiguity, which will further improve the clinical documentation quality. On a much larger scale, Perioperative Informatics is working toward data “interoperability” by providing patient information collected through VPIMS in a useful form to the institution. Exchanging data with the Core Data institutional information database and Star are examples of how the group is opening doors to exchange information throughout the continuum of patient care. Hand hygiene observations are quickly and accurately recorded to track compliance with this critical patient safety measure. “The interoperability with the institution is essential,” said Rothman. “Because we have such a large volume of Vanderbilt patients passing through our area, we see it as our vital mission to communicate data we collect to other care providers across the institution. Likewise, the availability of important care information when a patient receives care in the perioperative space is equally vital. We don’t focus on inbound or outbound data. We focus on bi-directional communication with all systems. That is our goal in the years to come.” Taken together, the informatics effort in the Department of Anesthesiology seeks to close the loop, ensuring that patients are fully protected from harm and that beneficial interventions are always executed. Because Vanderbilt “owns” its information systems, both literally and figuratively, rapid cycle processes of hypothesis generation, pilot demonstration and full scale implementation of quality improvement projects are uniquely supported. An improved electronic nursing assessment now includes automated process monitoring for alcohol and abuse screenings. 45 Perioperative Clinical Research Institute (PCRI) Members of the Perioperative Clinical Research Institute: Front row, left to right, Emily Brink, RN, BSN; Kelen Taylor; Jennifer Morse; Sue Walsh, RN; Donna Nelson, RN, CAPA; and Kristie Lee. Second row, Edward Sherwood, MD, PhD; Damon Michaels, CCRP; Elizabeth Card, RN, CPAN, CCRP; Misty Hale; Christine Goldsberry; William Hardeman, CCRP; and Cleo Carter. Not pictured: James Berry, MD; Kiersten Card, Brian Donahue, MD, PhD; and Patricia Hendricks, RN. Navigating through countless regulations, mastering the nuances of grant writing, and properly managing finances in order to conduct clinical research is enough to fray the nerves of any fledgling investigator. To keep the process running smoothly, from initial concept to published research, the Department of Anesthesiology’s Perioperative Clinical Research Institute provides a full range of support services, including regulatory management, data management, contracts management, biostatistics, bioinformatics, and financial oversight. The group also trains new investigators so they can grow to the point of having their own funded research that leads to major publications. “We are here to facilitate the research process for our investigators,” said Clinical Trials Manager Damon Michaels. “We assist with compliance with federal, state, and local regulations and other details so the investigators can focus on their science. The end goal is stronger research, with an eye toward publication in leading journals.” Clinical research within the department includes both industrysponsored and investigator-initiated clinical projects and focuses on the advancement of medical practice in the fields of perioperative care, chronic pain, and medical devices. Most of the department’s investigators are practicing physicians who use their clinical expertise to develop research protocols that seek to answer clinically significant questions. The PCRI oversees more than 85 active clinical trials, with many more studies in development. PCRI is directed by Vice Chair for Research Edward Sherwood, MD, PhD, and Clinical Trials Manager Damon Michaels. The team consists of highly trained and broadly experienced research professionals, including five research nurse specialists, one research assistant, two clinical trials associates, and one research analyst. “It has been exciting to see the growth in clinical research since PCRI was founded in 2007,” said Michaels. “When I started, the department was mainly focused on basic science research. We added industry-funded studies to help new investigators 46 learn about the research process. As they’ve progressed in their research careers, our investigators have started developing their own complex questions that will improve the quality of patient care for years to come.” PCRI Supported Nursing Research The Perioperative Clinical Research Institute includes five research nurse specialists who are all practicing registered nurses with specialized training in conducting clinical research. The research nurse specialists provide support for clinical investigators, assisting in the design of clinical research and ensuring the integrity and quality of clinical research trials. Over the past two years, the nurses’ role has expanded to the point that they are now presenting their own research at national conferences and have published in the academic press. “These individuals support our ongoing investigations, and their contributions are invaluable,” said Michaels. “They are often the critical contact point ‘in the trenches,’ and are able to make sure nothing falls through the cracks or lags for any reason. They have been growing professionally so that they are more responsible, and are now pursuing their own research.” The role of the research nurse practitioner is also being developed within the Department of Anesthesiology to expand the responsibility that nurses have traditionally played in support of clinical trials. This role will allow nurses with advanced degrees and appropriate licensure to have increased responsibilities in research. Unlike other NPs who primarily work in a clinical role, the research NP will focus primarily on research. The department envisions utilizing research nurse practitioners as subinvestigators working closely with their principal investigators. They will also be PIs on their own research studies and will apply for grants, obtain their own extramural funding, and participate in the dissemination of research findings. Steve Klintworth, RN The clinical research nurses in PCRI are: Elizabeth Card, RN, CPAN, CCRP A practicing registered nurse since 1990, Elizabeth’s nursing background includes ICU, CVICU, PACU, holding room, pediatrics, transplant, and vascular case management. She has served as a sub-investigator or key study personnel in more than 45 clinical research studies at Vanderbilt involving drugs, devices, observational, or survey studies. Her research includes two ongoing studies on delirium Elizabeth Card, RN, CPAN, CCRP or cognitive impairment. Presently, Elizabeth serves as president for the Tennessee Society for PeriAnesthesia Nurses (TSPAN) and as Middle Tennessee Society for PeriAnesthesia Nurses (MTSPAN) Education Chair. In 2012, Elizabeth won the Vivien Thomas Award for Excellence in Clinical Research, an annual award presented by the Vanderbilt University Medical Center’s Office of Research. A practicing registered nurse since 1986, Steve’s nursing background includes critical care in MICU and SICU, general surgery, and nursing supervision. He’s been a sub-investigator or key study personnel in more than 25 clinical research studies at Vanderbilt involving drugs and devices. Steve’s current focus is on chronic pain research. Steve Klintworth, RN Donna Nelson, RN, CAPA Mary Hamilton Chestnut, FNP Mary Hamilton Chestnut, NP Mary Hamilton joined the Anesthesiology Department in November 2012. She is involved with several perioperative clinical research projects at Vanderbilt, primarily in the area of pediatrics, including studies on liquid oxymorphone for acute postoperative pain and on the safety of oxycodone CR tablets in opioid-experienced children. Donna Nelson, RN, CAPA A practicing registered nurse since 1980, Donna’s nursing background includes PACU, holding room, pediatrics, and labor & delivery. She has served as a sub-investigator or key study personnel in more than 15 clinical research studies at Vanderbilt involving drugs, devices, observational, or survey studies. She is working on an ongoing study on delirium or cognitive impairment. Patricia Hendricks, RN Patricia Hendricks, RN A practicing registered nurse since 1978, Patty’s nursing background includes ICU, PACU/holding room, cancer pain and symptom management therapies, and home health care. She has served as a sub-investigator or key study personnel in more than 15 clinical research studies at Vanderbilt involving drugs, devices, observational, or survey studies. Patty works exclusively with Josh Billings, MD, on a study focusing on acute kidney injury and delirium following cardiac bypass surgery. 47 Vanderbilt Anesthesiology & Perioperative Informatics Research (VAPIR) Division The Vanderbilt Anesthesiology & Perioperative Informatics Research (VAPIR) Division, led by Jesse M. Ehrenfeld, MD, MPH, focuses on utilization of information technology within the perioperative environment to improve patient safety and the quality of care delivered. The multidisciplinary group, which has grown from three full-time research support staff in 2010 to eight in 2013, manages more than seventy active clinical research projects and has taken the lead on developing methodologies for evaluating the impact of technology and information management systems within the operating room. Milestones Achieved Major achievements have included successful competition for a grant from the Anesthesia Patient Safety Foundation (APSF), a complete redesign of the Perioperative Data Warehouse (the elevenyear historical archive of data from the Vanderbilt Perioperative Information Management System), and recruitment of five new full-time employees. Realization of these steps was an important milestone for the group, as demand for perioperative data continues to grow in support of the Anesthesiology Department’s research mission. Additionally, VAPIR has supported a number of important operational initiatives, such as the development, launch and maintenance of the Perioperative Dashboard Project, which provides a real-time overview of a series of OR management and cost metrics to front-line managers and clinicians. “We have successfully positioned the VAPIR group to lead informatics research at Vanderbilt,” said Department Chairman Warren Sandberg, MD, PhD. “It is rewarding to know that our efforts in informatics research will ensure that the decisions made by researchers based on the information we are able to provide them will help ensure the safety and quality of patient care is never compromised.” Novel Collaborations, Here and Abroad The work accomplished by VAPIR has led to recognition of Vanderbilt as home to one of the premier anesthesia informatics research programs in the world, and this has resulted in many fruitful partnerships and collaborations. “We are appreciative for the opportunities for our group to partner not only with collaborators at Vanderbilt, but also with colleagues performing research across the nation and the world,” said Dr. Ehrenfeld. “Through these collaborations, we have been able to establish and strengthen our group’s mission to promote patient safety and quality of care, both here and abroad.” One such collaboration is with the National Institutes of Healthsponsored U.S. Critical Illness and Injury Trials Group, in which Vanderbilt is co-leading an effort to bring together de-identified, high-resolution intensive care unit data from a consortium of medical centers. This unprecedented effort is allowing researchers across the country to quickly and efficiently answer important questions about how to best care for critically ill patients. One example project centers around determining what post-surgical blood pressure is ideal to prevent the development of acute renal failure after surgery. Innovations in Quality and Delivery of Care Discoveries made by researchers in the VAPIR group have led not just to the creation of new knowledge, but in many cases have resulted in the direct improvement of care and operative outcomes of Vanderbilt patients — and thousands of patients undergoing surgery and anesthesia worldwide. Three projects are highlighted below. Better Care for Diabetic Patients Vanderbilt is leading a multicenter effort to understand the impact of providing real-time clinical decision support for the management of glucose during surgery. Preliminary results from the study have demonstrated an improvement in a variety of outcomes and, most notably, a reduction in post-surgical readmission rates in diabetic patients at Vanderbilt. Cost Containment of Anesthesia VAPIR Division Research Director Jesse Ehrenfeld, MD, MPH, discusses ongoing clinical research projects with Database Administrator Michaelene Johnson. 48 This two-phase study is geared toward providing a mechanism to decrease the average cost of anesthesia for surgery. The first phase, which was completed in 2012, consisted of the creation and verification of an accurate system to tabulate and display anesthesia-related costs for operative cases. This has allowed VAPIR to understand the magnitude of and factors leading to significant cost variability. The second phase of the study will test several ways of sharing this information with providers and assess methods to actively manage anesthesia and surgical costs. Preventing Post-Operative Deterioration While the morbidity and mortality attributed to anesthesia is low, there continues to be a high post-operative complication rate. Supported by a grant from the Anesthesia Patient Safety Foundation (APSF), VAPIR members have set out to identify characteristics that may be predictive of adverse events in the immediate post-operative setting (i.e., within 72 hours of surgery). To date, VAPIR researchers have identified a cohort of 35,090 adult patients who had a surgical procedure and were admitted to the hospital after surgery. Of these patients, 689 had an unanticipated transfer to the ICU within 72 hours. The team is now modeling the differences between patients who experienced these unexpected transfers and those who did not. Ultimately, the plan is to automate a predictive model in order to provide real-time model output to clinicians in the OR. Teaching the Next Generation Consistent with the department’s educational mission, VAPIR is actively engaged in the education and training of students, residents, and fellows through a variety of mechanisms including seminars, journal clubs, and a successful summer research training program. During the 2012-2013 academic year, VAPIR provided mentorship and research opportunities for more than 20 students – including undergraduate, medical, and graduate students – who joined VAPIR from Vanderbilt and seven other academic institutions. VAPIR continues to attract renowned experts in the fields of biomedical informatics and clinical research to Vanderbilt’s campus as visiting scholars. At the monthly Anesthesia Informatics Research Seminar, which is open to the entire Vanderbilt University community, these specialists share their research findings and expertise. Vanderbilt Anesthesiology and Perioperative Informatics Research (VAPIR) Division, by the Numbers VAPIR Research Protocols Approved Research Protocols..................................................................................................................................................................... 49 Pending Research Protocols.......................................................................................................................................................................... 4 Total Research Protocols............................................................................................................................................................................. 53 Active VAPIR Projects Clinical Research & Quality Improvement Projects................................................................................................................................... 70 Technical Team Projects............................................................................................................................................................................. 36 Grant Applications Applications Submitted............................................................................................................................................................................... 15 Applications Funded..................................................................................................................................................................................... 2 Manuscripts Papers Under Review.................................................................................................................................................................................. 20 Papers Accepted.......................................................................................................................................................................................... 18 Total Papers................................................................................................................................................................................................. 38 Abstracts & Podium Presentations at Scientific Meetings National Meetings....................................................................................................................................................................................... 71 International Meetings.................................................................................................................................................................................. 8 Total Original Research Presentations........................................................................................................................................................ 79 Collaborations Vanderbilt Departments.............................................................................................................................................................................. 15 Departments at other U.S. Institutions.......................................................................................................................................................... 9 International Departments............................................................................................................................................................................. 5 49 Center for Research and Innovation in Systems Safety (CRISS) Vanderbilt University School of Medicine’s Center for Research and Innovation in Systems Safety (CRISS), directed by Matthew B. Weinger, MD, is an institution-wide resource for human factors, usability and systems engineering and design located within the Department of Anesthesiology. CRISS is an integral part of Vanderbilt’s Institute for Medicine and Public Health (IMPH), led by Robert Dittus, MD. To fulfill its mission of enhancing healthcare quality and safety, CRISS conducts basic and applied research in healthcare informatics, patient safety and clinical quality; designs, assesses and improves care processes, medical technology and electronic health record (EHR) user interfaces; and utilizes state-of-the-art simulation facilities to test and analyze medical equipment and procedures. Current research includes an Agency for Healthcare Research and Quality (AHRQ)-funded multicenter study to develop and deploy standardized simulation scenarios to assess the performance of board-certified physicians. In July 2012, CRISS was the recipient of one of only 50 pilot grants (out of 1,400 applicants) from the Patient Centered Outcomes Research Institute (PCORI). In this project, the group is analyzing the occurrence of non-routine events reported concurrently by patients and their clinicians in four different domains – pediatric cardiac surgery, pediatric oncology, adult cardiac catheterization, and adult ambulatory surgery. CRISS is also actively involved in two federal contracts to conduct informatics research: a National Institute of Standards and Technology (NIST)-funded project to define best practices for the design of Electronic Medical Records (EMRs), and an AHRQ-funded project to study the relationship between workflow and Electronic Health Record (EHR) use in ambulatory settings. Finally, CRISS researcher Richard Holden, PhD, received a federal career development award (KL2) through the Vanderbilt Institute for Clinical and Translational Research to design a home-based software tool for patients with congestive heart failure to manage their symptoms and therapy. Previously, in an AHRQ-funded study, CRISS members showed that a simulation-based training intervention enhanced the quality of handovers and communication between anesthesia providers and PACU nurses. In another VA-funded study of 1,000 surgical cases, CRISS investigators found that OR teams’ workload ratings were strongly associated with reported intraoperative events; the relationship of workload and reported events to 30day morbidity and mortality is being analyzed. For a National Heart, Lung, and Blood Institute (NHLBI) R21 grant, Dan France, PhD, modeled the factors affecting the ability of patients presenting to the emergency department with acute coronary syndrome to receive evidence-based care. In a study funded by the Anesthesia Patient Safety Foundation, Anne Miller, PhD, and her colleagues implemented and evaluated goal-directed care protocols in the cardiovascular ICU. CRISS involvement with Vanderbilt University Medical Center operational initiatives in quality improvement range from participating in the review and analysis of most serious clinical events at VUMC, to re-engineering blood transfusion processes, improving clinician handovers, and enhancing compliance with perioperative timeouts and checklists. 50 CRISS faculty and staff are integrally involved in user interface design and evaluation on numerous applications for VUMC’s Informatics, including the next-generation EHR, SmartVU™, which will be a platform independent, web-browser compliant, highly usable application that is being designed to model clinicians’ mental models of care and their workflow. SmartVU™ includes application modules for patient intake, clinical note writing, medication and order management, results tracking, patient education/communication, and clinician communication. SmartVU™ includes state-of-the-art clinical decision support. CRISS is also helping to design several perioperative informatics (i.e., VPIMS) modules including the new preoperative application, PREP. Finally, CRISS is assisting Vanderbilt Informatics in obtaining Meaningful Use certification from the federal government for its clinical applications. CRISS faculty members include Director Matthew B. Weinger, MD, MS; Arna Banerjee, MD; Daniel France, PhD, MPH; Richard Holden, PhD; Kevin Johnson, MD; Amanda Lorinc, MD; Anne Miller, PhD; Laurie Lovett Novak, PhD, MHSA; Jason Slagle, PhD; Matt Shotwell, PhD; Theodore Speroff, PhD; Scott Watkins, MD; Jonathan Wanderer, MD; Kim Unertl, PhD; and Gina Whitney, MD. CRISS staff include: Russ Beebe; Christine Buchanan; Eva Cassedy; Krys Dworski; Christine Goldsberry; Jeff Hottle; Andrew Kline; Eric Porterfield, MS; and Christopher Simpson, MS. CRISS staff worked with members of Perioperative Informatics to develop a Universal Protocol/Time Out (UP/TO) at VUMC which increases patient safety by prompting clinicians – though easily followed visual check lists – to confirm important patient data. Selected Publications, 2012-2013 Original Research Agarwal H, Hardison D, Saville B, Donahue B, Lamb F, Bichell D, Harris Z. Residual lesions in postoperative pediatric cardiac surgery patients receiving extracorporeal membrane oxygenation support. J Thorac Cardiovasc Surg. 2013 Apr 15. pii: S00225223(13)00324-3. Agarwal H, Saville B, Slayton J, Donahue B, Daves S, Christian K, Bichell D, Harris Z. Standardized postoperative handover process improves outcomes in the intensive care unit: a model for operational sustainability and improved team performance*. Crit Care Med. 2012 Jul;40(7):2109-15. Alamanda V, Delisca G, Mathis S, Archer K, Ehrenfeld J, Miller M, Homlar K, Halpern J, Schwartz H, Holt G. The financial burden of reexcising incompletely excised soft tissue sarcomas: a cost analysis. Ann Surg Oncol. 2013 Apr [Epub]. Ares G, Haque M, Delpire E, Ortiz P. Hyperphosphorylation of Na-K-2Cl cotransporter in thick ascending limbs of Dahl salt-sensitive rats. Hypertension. 2012 Dec;60(6):1464-70. Backman E, Triant V, Ehrenfeld J, Lu Z, Arpino P, Losina E, Gandhi R. Safety of midazolam for sedation of HIV-positive patients undergoing colonoscopy. HIV Med. 2013 Jan [Epub]. Balaguer J, Yu C, Byrne J, Ball S, Petracek M, Brown N, Pretorius M. Contribution of endogenous bradykinin to fibrinolysis, inflammation and blood product transfusion following cardiac surgery: A randomized clinical trial. Clin Pharmacol Ther. 2013 Apr;93(4):326-34. Bateman B, Mhyre J, Ehrenfeld J, Kheterpal S, Abbey K, Argalious M, Berman M, St. Jacques P, Levy W, Loeb R, Paganelli W, Smith K, Wethington K, Wax D, Pace N, Tremper K, Sandberg W. The risk and outcomes of epidural hematomas after perioperative and obstetric epidural catheterization: a report from the Multicenter Perioperative Outcomes Group Research Consortium. Anesth Analg. 2013 Jun;116(6):1380-5. Billings F, Balaguer J, Yu C, Wright P, Petracek, M, Byrne J, Brown, N, Pretorius M. Comparative effects of angiotensin receptor blockade and ACE inhibition on the fibrinolytic and inflammatory responses to cardiopulmonary bypass. Clin Pharmacol Ther. 2012 Jun;91(6):1065-73. Billings F IV, Pretorius M, Schildcrout J, Mercaldo N, Byrne J, Ikizler T, Brown N. Obesity and oxidative stress predict AKI after cardiac surgery. J Am Soc Nephrol. 2012 Jul; 23(7):1221-8. Bruehl S, Apkarian A, Ballantyne J, Berger A, Borsook D, Chen W, Farrar J, Haythornthwaite J, Horn S, Iadarola M, Inturrisi C, Lao L, Mackey S, Mao J, Sawczuk A, Uhl G, Witter J, Woolf C, Zubieta J, Lin Y. Personalized medicine and opioid analgesic prescribing for chronic pain: opportunities and challenges. J Pain. 2013 Feb;14(2):103-13. Bruehl S, Burns J, Gupta R, Buvanendran A, Chont M, Kinner E, Schuster E, Passik S, France C. Endogenous opioid function mediates the association between laboratoryevoked pain sensitivity and morphine analgesic responses. Pain. 2013 Jun [Epub]. Bruehl S, Liu X, Burns J, Chont M, Jamison R. Associations between daily chronic pain intensity, daily anger expression, and trait anger expressiveness: an ecological momentary assessment study Pain. 2012 Dec;153(12):2352-8. Brummel N, Jackson J, Girard T, Pandharipande P, Schiro E, Work B, Pun B, Boehm L, Gill T, Ely E. A Combined Early Cognitive and Physical Rehabilitation Program for People Who Are Critically Ill: The Activity and Cognitive Therapy in the Intensive Care Unit (ACT-ICU) Trial. Phys Ther. 2012 Dec;92(12):1580-92. Burkle F, Nickerson J, von Schreeb J, Redmond A, McQueen K, Norton I, Roy N. Emergency surgery data and documentation reporting forms for sudden-onset humanitarian crises, natural disasters and the existing burden of surgical disease. Prehosp Disaster Med. 2012 Sep;1-6. Burns J, Bruehl S, Chont M. Anger regulation style, anger arousal and acute pain sensitivity: evidence for an endogenous opioid “triggering” model. J Behav Med. 2013 Apr [Epub]. Carpenter L, Baysinger C. Maintaining perioperative normothermia in the patient undergoing cesarean delivery. Obstet Gynecol Surv. 2012 Sept; 67(7):436-446. Chao T, Burdic M, Ganjawalla K, Derbew M, Keshian C, Meara J, McQueen K. Survey of surgery and anesthesia infrastructure in Ethiopia. World J Surg. 2012 Nov;36(11):2545-53. Collins S, Starr S, Bishop J, Baysinger C. Nitrous oxide for labor analgesia: expanding analgesic options for women in the United States. Rev Obstet Gynecol. 2012 Oct;5(3):131-134. Delpire E, Baranczak A, Waterson A, Kim K, Kett N, Morrison R, Scott Daniels J, David Weaver C, Lindsley C. Further optimization of the K-Cl cotransporter KCC2 antagonist ML077: Development of a highly selective and more potent in vitro probe. Bioorg Med Chem Lett. 2012 Jul;22(14):4532-5. Ding J, Ponce-Coria J, Delpire E. A trafficking-deficient mutant of KCC3 reveals dominant-negative effects on K-Cl cotransport function. PloS One. 2013 Apr;8(4):e61112. Douglas S, Cartmill R, Brown R, Hoonakker P, Slagle J, Schultz Van Roy K, Walker J, Weinger M, Wetterneck T, Carayon P. The work of adult and pediatric intensive care unit nurses. Nurs Res. 2013 Jan-Feb;62(1):50-8. Downing J, Baysinger C, Johnson R, Paschall R. Review: potential druggable targets for the treatment of early onset preeclampsia. Pregnancy Hypertens. 2013 May [Epub]. doi: 10.1016/j.preghy.2013.4.120. Epstein R, Dexter F, Rothman B. Communication latencies of wireless devices suitable for time-critical messaging to anesthesia providers. Anesth Analg. 2013 Apr;116(4):911-8. Epstein R, St Jacques P, Stockin M, Rothman B, Ehrenfeld J, Denny J. Automated identification of drug and food allergies entered using non-standard terminology. J Am Med Inform Assoc. 2013 Jun [Epub]. Fletcher K, Visotcky A, Slagle J, Tarima S, Weinger M, Schapira M. The composition of intern work while on call. J Gen Intern Med. 2012 Nov;27(11):1432-7. Franklin A, Hays S. Successful Management of a Thoracic Cerebrospinal Fluid Cutaneous Fistula in a Two Year-Old Child Using a Thoracic Epidural Blood Patch. J Clin Anesth. 2013 Jun;25(4). Franklin A, Lorinc A, Donahue B. Malignant Hyperthermia-Like Manifestations in a Two-Month Old Child with Holt-Oram Syndrome Undergoing Cardiac Surgery. J Cardiothorac Vasc Anesth. 2013 Mar [Epub]. Gagnon K, Delpire E. Molecular physiology of SPAK and OSR1: two Ste20-related protein kinases regulating ion transport. Physiological Rev. 2012 Oct;92(4):15771617. Gagnon K, Delpire E. Physiology of SLC12 transporters: lessons from inherited human genetic mutations and genetically engineered mouse knockouts. Am J Physiol Cell Physiol. 2013 Apr;304(8):C693-714. Garcia A, Bonnaig J, Yoneda Z, Richards J, Ehrenfeld J, Obremskey W, Jahangir A, Sethi M. Patient variables which may predict length of stay and hospital costs in elderly patients with hip fracture. J Orthop Trauma. 2012 Nov;26(11):620-3. Garg S, Kumar A. Successful echocardiography-guided management of refractory postoperative hypotension after alfieri repair of the mitral valve. J Cardiothorac Vasc Anesth. 2013 Jun;27(3):e21-2. Girard T, Ware L, Bernard G, Pandharipande P, Thompson J, Shintani A, Jackson J, Dittus R, Ely E. Associations of markers of inflammation and coagulation with delirium during critical illness. Intensive Care Med. 2012 Dec;38(12):1965-73. Gonzalez-Villalobos R, Janjoulia T, Fletcher N, Giani J, Nguyen M, Riquier-Brison A, Seth D, Fuchs S, Eladari D, Picard N, Bachmann S, Delpire E, Peti-Peterdi J, Navar L, Bernstein K, McDonough A. The absence of intrarenal ACE protects against hypertension. J Clin Invest. 2013 May;123(5):2011-23. Grimm P, Taneja T, Liu J, Coleman R, Chen Y, Delpire E, Wade J, Welling P. SPAK isoforms and OSR1 regulate sodium-chloride co-transporters in a nephron-specific manner. J Bio Chem. 2012 Nov;387(45):37673-37690. Grosse-Sundrup M, Henneman J, Sandberg W, Bateman B, Uribe J, Nguyen N, Ehrenfeld J, Martinez E, Kurth T, Eikermann M. Intermediate acting non-depolarizing neuromuscular blocking agents and risk of postoperative respiratory complications: prospective propensity score matched cohort study. BMJ. 2012 Oct 15.345:e6329. Grueter B, Robison A, Neve R, Nestler E, Malenka R. ∆FosB differentially modulates nucleus accumbens direct and indirect pathway function. Proc Natl Acad Sci U S A. 2013 Jan;110(5):1923-8. Gupta R. Using an electronic clinical decision support system to reduce the risk of epidural hematoma. Am J Ther. 2012 Oct [Epub]. Gupta R, Lane J, Allen B, Shi Y, Schildcrout J. Improving needle visualization by novice residents during an in-plane ultrasound nerve block simulation using an in-plane multiangle needle guide. Pain Med. 2013 Jun [epub]. Haas J, Winter H, Lim E, Kirby A, Blumenstiel B, DeFelice M, Gabriel S, Jalas C, Branski D, Grueter C, Toporovski M, Walther T, Daly M, Farese R Jr. DGAT1 mutation is linked to a congenital diarrheal disorder. J Clin Invest. 2012 Dec;122(12):4680-4. Hain P, Gay J, Berutti T, Whitney G, Wang W, Saville B. Preventability of early readmissions at a children’s hospital. Pediatrics. 2013 Jan;131(1):e171-81. Harden R, Oaklander A, Burton A, Perez R, Richardson K, Swan M, Barthel J, Costa B, Graciosa J, Bruehl S; Reflex Sympathetic Dystrophy Syndrome Association. Complex regional pain syndrome: practical diagnostic and treatment guidelines, 4th edition. Pain Med. 2013 Feb;14(2):180-229. 51 Harden R, Wallach G, Gagnon C, Zereshki A, Mukai A, Saracoglu M, Kuroda M, Graciosa J, Bruehl S. The osteoarthritis knee model: psychophysical characteristics and putative outcomes. J Pain. 2013 Mar;14(3):281-9. Kynes J, Schildcrout J, Hickson G, Pichert J, Han X, Ehrenfeld J, Westlake M, Catron T, St. Jacques P. An analysis of risk factors for patient complaints about ambulatory anesthesiology care. Anesth Analg. 2013 Jun;116(6):1325-32. Hata J, Togashi K, Kumar A, Hodges L, Kaiser E, Tessmann P, Faust C, Sessler D. Effect of the Pressure-Volume Curve (PVC) for PEEP Titration on Clinical Outcomes in Acute Lung Injury and the Acute Respiratory Distress Syndrome: A Systematic Review. J Intensive Care Med. 2013 Jun [Epub]. Lane J, Sandberg W, Rothman B. Development and implementation of an integrated mobile situational awareness iPhone application VigiVU™ at an academic medical center. Int J Comput Assist Radiol Surg. 2012 Sep;7(5):721-35. Hays S, Deshpande J. Newly postulated neurodevelopmental risks of pediatric anesthesia: theories that could rock our world. J Urol. 2013 Apr;189(4):1222-8. Helwani M, Saied N. Intraoperative plateau pressure measurement using modern anesthesia machine ventilators. Can J Anaesth. 2013 Apr;60(4):404-6. Helwani M, Saied N, Asaad B, Rasmussen S, Fingerman M. The current role of ultrasound use in teaching regional anesthesia: a survey of residency programs in the United States. Pain Med. 2012 Oct;13(10):1342-6. Hernandez A, Cogdill R, Hinojosa-Laborde C, Restrepo M. Comparison of silicone spray versus water soluble lubricating jelly for the aid in bronchoscopic examination. Journal of Anesthesiology & Clinical Science. 2013 Jun; 2(7). DOI:10.7243/20499752-2-7. Hester D, McGrane S, Higgins M. Respiratory parameters as a surrogate marker for duration of intubation: potential application of automated vital sign collection. J Clin Monit Comput. 2013 Apr [Epub]. Hill J, Ashit P, Del Corral G, Sexton, K, Ehrenfeld J, Guillamondegui O, Shack R. Preoperative anemia predicts free flap failure and thrombosis in microvascular reconstruction. Ann Plast Surg. 2012 Oct;69(4):364-7. Hollenbeck R, Wells Q, Pollock J, Kelley M, Wagner C, Cash M, Scott C, Burns K, Jones I, Fredi J, McPherson J. Implementation of a standardized pathway for the treatment of cardiac arrest patients using therapeutic hypothermia: “CODE ICE”. Crit Pathw Cardiol. 2012 Sep;11(3):91-8. Hughes C, Brummel N, Vasilevskis E, Girard T, Pandharipande P. Future directions of delirium research and management. Best Pract Res Clin Anaesthesiol. 2012 Sep;26(3):395-405. Hughes C, McGrane S, Pandharipande P. Sedation in the intensive care setting. Clin Pharmacol. 2012;4:53-63. Hughes C, Morandi A, Girard T, Riedel B, Thompson J, Shintani A, Pun B, Ely E, Pandharipande P. Association between Endothelial Dysfunction and Acute Brain Dysfunction during Critical Illness. Anesthesiology. 2013 Mar;118(3):631-9. Hughes C, Patel M, Pandharipande P. Pathophysiology of acute brain dysfunction: what’s the cause of all this confusion?. Curr Opin Crit Care. 2012 Oct;18(5):518-26. Ivakine E, Acton B, Mahadevan V, Ormond J, Tang M, Pressey J, Huang M, Ng D, Delpire E, Salter M, Woodin M, McInnes R. Neto2 is a KCC2 interacting protein required for neuronal Cl- regulation in hippocampal neurons. Proc Natl Acad Sci USA. 2013 Feb;110(9):3561-6. Jackson T, Lonergan D, Todd R, Martin P. Intentional intrathecal opioid detoxification in 3 patients: characterization of the intrathecal opioid withdrawal syndrome. Pain Pract. 2013 Apr;13(4):297-309. Kaufmann K, Romaine I, Days E, Pascual C, Malik A, Yang L, Zou B, Du Y, Sliwoski G, Morrison R, Denton J, Niswender C, Daniels J, Sulikowski G, Xie X, Lindsley C, Weaver C. ML297 (VU0456810), the first potent and selective activator of the GIRK potassium channel, displays antiepileptic properties in mice. ACS Chem Neurosci. 2013 Jun [Epub]. Kent M, Hackworth R, Riffenburgh R, Kaesberg J, Asseff D, Lujan E, Corey J. A comparison of ultrasound-guided and landmark-based approaches to saphenous nerve blockade: a prospective, controlled, blinded, crossover trial. Anesth Analg. 2013 Apr [Epub]. Knowlton L, Chackungal S, Dahn B, Lebrun D, Nickerson J, McQueen K. Liberian surgical and anesthesia infrastructure: a survey of county hospitals. World J Surg. 2013 Apr;37(4):721-9. Krupka D, Sandberg W, Weeks W. The impact on hospitals of reducing surgical complications suggests many will need shared savings programs with payers. Health Aff (Millwood). 2012 Nov;31(11):2571-8. Kumar A, Hata J, Bayman E, Krishnan S. Implementing a Hybrid Web-Based Curriculum for an Elective Medical Student Clerkship in a Busy Surgical ICU: Effect on Test and Satisfaction Scores. Journal of Surgical Education. 2013 Jan. Kumar A, Schweiger H. Intraoperative Use of a Chest Physiotherapy System During Whole Lung Lavage for Pulmonary Alveolar Proteinosis. Therapeutic Advances in Respiratory Disease. 2012 Aug;6(4):239-42. Kumar A, Suneja M. Hetastarch-Induced Osmotic Nephrosis. Anesthesiology. 2012 Sep;117(3):647. 52 Lebrun D, Dhar D, Sarkar M, Imran T, Kazi S, McQueen K. Measuring global surgical disparities: a survey of surgical and anesthesia infrastructure in Bangladesh. World J Surg. 2013 Jan;37(1):24-31. Lebrun D, Saavedra-Pozo I, Agreda-Flores F, Burdic M, Notrica M, McQueen K. Surgical and anesthesia capacity in Bolivian public hospitals: results from a national hospital survey. World J Surg. 2012 Nov;36(11):2559-66. Levin S, Harley E, Fackler J, Lehmann C, Custer J, France D, Zeger S. Real-time forecasting of pediatric intensive care unit length of stay using computerized provider orders. Crit Care Med. 2012 Nov;40(11):3058-64. Li F, Sexton K, Hocking K, Osgood M, Eagle S, Cheung-Flynn J, Brophy C, Komalavilas P. Intimal thickness associated with endothelial dysfunction in human vein grafts. J Surg Res. 2013 Mar;180(1):e55-62. Likis F, Andrews J, Collins M, Lewis R, Seerogy, J, Starr S, Walden R, McPheeters M. Nitrous Oxide for the Management of Labor Pain [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US). 2012 Aug (Comparative Effectiveness Reviews, No. 67). Logan D, Williams S, Carullo V, Claar R, Bruehl S, Berde C. Children and adolescents with complex regional pain syndrome: more psychologically distressed than other children in pain?. Pain Res Manag. 2013 Mar-Apr; 18(2):87-93. Lonergan D, Ehrenfeld J. Advancement of information technology in outpatient and perioperative settings to support patient care and translational research. Pain Management. 2012 Sept;2(5):445-449. DOI 10.2217/pmt.12.43. Lucas O, Hilaire C, Delpire E, Scamps F. KCC3-dependent chloride extrusion in adult sensory neurons. Mol Cell Neurosci. 2012 Jul;50(3-4):211-20. Maltais S, Costello W, Billings F IV, Bick J, Byrne J, Ahmad R, Wagner C. Episodic monoplane transesophageal echocardiography impacts postoperative management of the cardiac surgery patient. J Cardiothorac Vasc Anesth. 2013 Feb [Epub]. Mandell M, Pomfret E, Steadman R, Hirose R, Reich D, Schumann R, Walia A. Director of anesthesiology for liver transplantation: existing practices and recommendations by the United Network for Organ Sharing. Liver Transpl. 2013 Apr;19(4):425-30. Mao S, Garzon-Muvdi T, Di Fulvio M, Chen Y, Delpire E, Alvarez F, Alvarez-Leefmans F. Molecular and functional expression of cation-chloride cotransporters in dorsal root ganglion neurons during postnatal maturation. J Neurophysiol. 2012 Aug;108(3):83452. Marczak E, Marzec J, Zeldin D, Kleeberger S, Brown N, Pretorius M, Lee C. Polymorphisms in the transcription factor NRF2 and forearm vasodilator responses in humans. Pharmacogenet Genomics. 2012 Aug;22(8):620-8. McClain C, Hughes J, Andrews J, Blackburn J, Sephel S, France D, Viele M, Goodnough L, Young P. Blood ordering from the operating room: Turnaround time as a quality indicator. Transfusion. 2013 Jan;53(1):41-8. McGrane S, Agarwal A, Pandharipande P. Acute visual loss in ICU. In: Kellum J, Fortenberry J, Fuchs B, Shaw A, eds Decision Support System in Critical Care Medicine. Wilmington, DE: Decision Support in Medicine, LLC; 2013. Available at: http://www.decisionsupportinmedicine.com. McGrane S, Maziad J, Netterville J, Saied N. Therapeutic hypothermia after exsanguination. Anesth Analg. 2012 Aug;115(2):343-5. McPherson J, Wagner C, Boehm L, Hall J, Johnson D, Miller L, Burns K, Thompson J, Shintani A, Ely E, Pandharipande P. Delirium in the cardiovascular ICU: exploring modifiable risk factors. Crit Care Med. 2013 Feb;41:405-413. McQueen K, Malviya S, Gathuya Z, Tyler D, Davidson A. International advocacy for education and safety. Paediatr Anaesth. 2012 Oct;22(10):962-8. Mirzakhani H, Nozari A, Ehrenfeld J, Peterfreund R, Szabo M, Walsh J, Jiang Y, Sandberg W, Rosow C, Wang J. Case report: profound hypotension after anesthetic induction with propofol in patients treated with rifampin. Anesth Analg. 2013 May [Epub]. Moore D, Yoneda Z, Powell M, Howard D, Jahangir A, Archer K, Ehrenfeld J, Obremskey W, Sethi M. Gunshot victims at a major level I trauma center: a study of 343,866 emergency department visits. J Emerg Med. 2013 Mar;44(3):585-91. Morandi A, Pandharipande P, Jackson J, Bellelli G, Trabucchi M, Ely E. Understanding terminology of delirium and long-term cognitive impairment in critically ill patients. Best Pract Res Clin Anaesthesiol. 2012 Sep;26(3):267-76. Nguyen M, Lee D, Delpire E, McDonough A. Differential regulation of Na+ transporters along nephron during AngII-dependent hypertension: distal stimulation counteracted by proximal inhibition. Am J Physiol Renal Physiol. 2013 May [Epub]. Sen P, Yang Y, Navarro C, et al. incl. Hays S. Novel FOXF1 Mutations in Sporadic and Familial Cases of Alveolar Capillary Dysplasia with Misaligned Pulmonary Veins Imply a Role for its DNA Binding Domain. Hum Mutat. 2013 Jun;34(6):801-11. Nguyen M, Yang L, Fletcher N, Lee D, Kocinsky H, Bachmann S, Delpire E, McDonough A. Effects of K+-deficient diets with and without NaCl supplementation on Na+, K+, and H2O transporters’ abundance along the nephron. Am J Renal Physiol. 2012 Jul;303(1):F92-104. Seymour C, Pandharipande P, Koestner T, Hudson L, Thompson J, Shintani A, Ely E, Girard T. Diurnal sedative changes during intensive care: Impact on liberation from mechanical ventilation and delirium*. Crit Care Med. 2012 Oct;40(10):2788-2796. Olsen R, Bruehl S, Nielsen C, Rosseland L, Eggen A, Stubhaug A. Hypertension prevalence and diminished blood pressure-related hypoalgesia in individuals reporting chronic pain in a general population: the Tromsø study. Pain. 2013 Feb;154(2):257-62. Patel M, McKenna J, Alvarez J, Sugiura A, Jenkins J, Guillamondegui O, Pandharipande P. Decreasing adrenergic or sympathetic hyperactivity after severe traumatic brain injury using propranolol and clonidine (DASH After TBI Study): study protocol for a randomized controlled trial. Trials. 2012 Sep;13(1):177. Patel P, Fassl J, Thompson A, Augoustides JG. Transcatheter aortic valve replacement-part 3: the central role of perioperative transesophageal echocardiography. J Cardiothorac Vasc Anesth. 2012 Aug;26(4):698-710. Ponce-Coria J, Gagnon K, Delpire E. Calcium binding protein 39 facilitates molecular interaction between Ste20p proline alanine-rich kinase (SPAK) and oxidative stress response 1 (OSR1) monomers. Am J Cell Physiol. 2012 Dec;303(11):C1198-205. Poon S, Zuckerman S, Mainthia R, Hagan S, Lockney D, Zotov A, Holt G, Bennett M, Anders S, France D. Methodology and bias in assessing compliance with a surgical safety checklist. Jt Comm J Qual Patient Saf. 2013 Feb;39(2):77-82. Potet F, Lorinc A, Chaigne S, Hopkins C, Venkataraman R, Stepanovic S, Lewis L, Days E, Sidorov V, Engers D, Zou B, Afshartous D, George A Jr, Campbell C, Balser J, Li M, Baudenbacher F, Lindsley C, Weaver C, Kupershmidt S. Identification and characterization of a compound that protects cardiac tissue from human Ether-àgo-go-related gene (hERG)-related drug-induced arrhythmias. J Biol Chem 2012. Nov;287(47):39613-25. Pretorius M, Murray K, Yu C, Byrne J, Billings F, Petracek M, Greelish J, Hoff S, Ball S, Mishra V, Meisch, C, DeMatteo A, Body S, Brown N. Angiotensin-converting enzyme inhibition or mineralocorticoid receptor blockade do not affect prevalence of atrial fibrillation in patients undergoing cardiac surgery. Crit Care Med. 2012 Oct;40(10):2805-12. Raphemot R, Rouhier M, Hopkins C, Gogliotti R, Lovell K, Hine R, Ghosalkar D, Longo A, Beyenbach K, Denton J, Piermarini P. Eliciting renal failure in mosquitoes with a small-molecule inhibitor of inward-rectifying potassium channels. PLoS One. 2013 May;8(5):e64905. Raphemot R, Weaver C, Denton J. High-throughput screening for small-molecule modulators of inward rectifier potassium channels. J Vis Exp. 2013 Jan 27;(71). pii: 4209. Rasmussen S, Saied N, Bowens C Jr, Mercaldo N, Schildcrout J, Malchow R. Duration of upper and lower extremity peripheral nerve blockade is prolonged with dexamethasone when added to ropivacaine: a retrospective database analysis. Pain Med. 2013 June [Epub]. Robertson A, Eagle S. Transesophageal echocardiography during orthotopic liver transplantation: maximizing information without the distraction. J Cardiothorac Vasc Anesth. 2013 Apr 30. pii: S1053-0770(12)00582-4. Rothman B, Dexter F, Epstein R. Communication latencies of apple push notification messages relevant for delivery of time-critical information to anesthesia providers. Anesth Analg. 2013 Jun [Epub]. Rothman B, Leonard J, Vigoda M. Future of electronic health records: implications for decision support. Mt Sinai J Med. 2012 Nov-Dec;79(6):757-68. Saied N, Chopra A, Agarwal B. Parenteral erythromycin for potential use to empty retained gastric contents encountered during upper gastrointestinal endoscopic procedures. Open Journal of Gastroenterology. 2012 Aug;2(3):119-123. DOI: 10.4236/ ojgas.2012.23025. Saied N, Helwani M. Successful lumbar epidural catheter placement through a lower back lipoma. Saudi J Anaesth. 2013 Jan;7(1):83-5. Sandberg E, Sharma R, Sandberg W. Deficits in retention for verbally presented medical information. Anesthesiology. 2012 Oct;117(4):772-9. Saritas T, Borschewski A, McCormick J, Paliege A, Dathe C, Uchida S, Terker A, Himmerkus N, Bleich M, Demaretz S, Laghmani K, Delpire E, Ellison D, Bachmann S, Mutig K. SPAK differentially mediates vasopressin effects on sodium cotransporters. J Am Soc Nephrol. 2013 Feb;24(3):407-18. Schewnk E, Mraovic B, Maxwell R, Kim G, Ehrenfeld J, Epstein R. Root causes of intraoperative hypoglycemia: a case series. J Clin Anesth. 2012 Dec;24(8):625-30. Shanmugasundararaj S, Das J, Sandberg W, Zhou X, Wang D, Messing R, Bruzik K, Stehle T, Miller K. Structural and functional characterization of an anesthetic binding site in the second cysteine-rich domain of protein kinase Cδ*. Biophys J. 2012 Dec 5;103(11):2331-40. Sherman A, Bruehl S, Smith C, Walker L. Individual and additive effects of mothers’ and fathers’ chronic pain on health outcomes in young adults with a childhood history of functional abdominal pain. J Pediatr Psychol. 2013 May;38(4):365-75. Shillcutt S, Bick J. Echo didactics: a comparison of basic transthoracic and transesophageal echocardiography views in the perioperative setting. Anesth Analg. 2013 Jun; 116:1231-1236. Shimazu T, Hirschey M, Newman J, He W, Shirakawa K, Le Moan N, Grueter C, Lim H, Saunders L, Stevens R, Newgard C, Farese R Jr, de Cabo R, Ulrich S, Akassoglou K, Verdin E. Suppression of oxidative stress by β-hydroxybutyrate, an endogenous histone deacetylase inhibitor. Science. 2013 Jan;339(6116):211-4. Sigakis M, Bittner A, Wanderer J. Validation of a risk stratification index and risk quantification index for predicting patient outcomes: in-hospital mortality, 30-day mortality, 1-year mortality and length of stay. Anesthesiology. 2013 Sep;119(3):525540. Smith H, Berruti T, Strohler B, Brink E, Fuchs C, Ely E, Pandharipande P. Pediatric critical care perceptions on analgesia, sedation, and delirium. Semin Respir Crit Care Med. 2013 Apr;34(2):244-61. Smith H, Brink E, Fuchs C, Pandharipande P. Pediatric delirium: monitoring and management in the pediatric intensive care unit. Pediatr Clin North Am. 2013 Jun;60(3):741-60. Solis C, Leon P, Sanchez N, Burdic M, Johnson L, Warren H, Iddriss A, McQueen K. Nicaraguan surgical and anesthesia infrastructure: survey of ministry of health hospitals. World J Surg. 2013 Jun [Epub]. Squiers J, King J; Wagner C, Ashby N, Parmley C. ACNP Intensivist: A new ICU care delivery model and its supporting educational program. Journal of the American Academy of Nurse Practitioners. 2012 Sep; 25(3): 119-125. DOI: 10.1111/j.17457599.2012.789.x. Sun Y, Shieh C, Delpire E, Shen M. K+-Cl- cotransport mediates the bactericidal activity of neutrophils by regulating NADPH oxidase activation. J Physiol. 2012 Jul;590(Pt 14):3231-43. Tiwari V, Dexter F, Rothman B, Ehrenfeld J, Epstein R. Explanation for the nearconstant mean time remaining in surgical cases exceeding their estimated duration, necessary for appropriate display on electronic white boards. Anesth Analg. 2013 Jun [Epub]. Vasilevskis E, Han J, Hughes C, Ely E. Epidemiology and risk factors for delirium across hospital settings. Best Pract Res Clin Anaesthesiol. 2012 Sept;26(3):277-287. Wagner C, Fredi J, McPherson J, Parmley C. Integration of Cardiology and Cardiac Surgery in the Cardiovascular Intensive Unit: Formation of a Multidisciplinary Approach on the Path to Building a High-Reliability Organization. ICU Director. 2013 Mar;4(2). DOI: 10.1177/1944451612472505. Walker L, Sherman A, Bruehl S, Garber J, Smith C. Functional abdominal pain patient subtypes in childhood predict functional gastrointestinal disorders with chronic pain and psychiatric comorbidities in adolescence and adulthood. Pain. 2012 Sept; 153(9):17981806. Waller C, Vandenberg B, Hasan D, Kumar A. Stress Cardiomyopathy with an “Inverse” Takotsubo Pattern in a Patient with Acute Aneurysmal Subarachnoid Hemorrhage. Echocardiography. 2013 Jun [Epub]. Walters J, Lonergan D, Todd R, Jackson T. Idiopathic peripheral neuropathy responsive to sympathetic nerve blockade and oral clonidine. Case Rep Anesthesiol. 2012;2012:407539. Wanderer J, Anderson-Dam J, Levine W, Bittner E. Development and validation of an intraoperative predictive model for unplanned postoperative intensive care. Anesthesiology. 2013 Sep;119(3):516-524. Wanderer J, Charnin J, Driscoll W, Bailin M, Baker K. Decision support using anesthesia information management system records and accreditation council for graduate medical education case logs for resident operating room assignments. Anesth Analg. 2013 Aug;117(2):494-9. 53 Wanderer J, Ehrenfeld J. Clinical decision support for perioperative information management systems. Semin Cardiothorac Vasc Anesth. 2013 May [Epub]. Wanderer J, Ehrenfeld J, Sandberg W, Rathmell J. Infographics in Anesthesiology: A Volatile Tale of Two Institutions. Anesthesiology. 2012 Oct. Wanderer J, Leffert L, Mhyre J, Kuklina E, Callaghan W, Bateman B. Epidemiology of obstetric-related ICU admissions in Maryland: 1999-2008. Crit Care Med. 2013 Aug;41(8):1844-1852. Wanderer J, Rao A, Rothwell S, Ehrenfeld J. Comparing two anesthesia information management system user interfaces: a usability evaluation. Can J Anaesth. 2012 Nov;59(11):1023-31. Watkins S, McNew B, Donahue B. Risks of noncardiac operations and other procedures in children with complex congenital heart disease. Ann Thorac Surg. 2013 Jan;95(1):204-11. Watson P, Pandharipande P, Gehlbach B, Thompson J, Shintani A, Dittus B, Bernard G, Malow B, Ely E. Atypical Sleep in Ventilated Patients: Empirical Electroencephalography Findings and the Path Toward Revised ICU Sleep Scoring Criteria. Crit Care Med. 2013 Jun [Epub]. Bowens C, Ehrenfeld J. Perioperative Optimization in Orthopedic Trauma. In: Sethi M, Jahangir A, Obremskey W, eds. Orthopedic Traumatology: An Evidence-Based Approach. New York, NY: Springer 2012: 431-444. Bruehl S. Pain and hypertension. In: Giamberardino M, Jensen T, eds. Pain Comorbidities: Understanding and Treating the Complex Patient. Seattle, WA: IASP Press; 2012. Dittrich K. Anesthesia Techniques. In: Urman R, Ehrenfeld J, eds. Pocket Anesthesia. 2nd ed. Philadelphia, PA: Lippincott, Williams, & Wilkins; 2012. Eagle S, Thompson A. Congenital heart disease in the adult presenting for non-cardiac surgery. In: ASA Refresher Courses in Anesthesiology. Hagarstown, MD: Lippincott Williams & Wilkins 2013:40. Easdown L, Banerjee A, Weinger M. Simulation for assessing human responses to critical events. In: Lee J, Kirlik A, eds. The Oxford Handbook of Cognitive Engineering. New York, NY: Oxford University Press; 2013: 336-351. Weavind L, Saied N, Hall J, Pandaharipande P. Care bundles in the adult ICU: is it evidence-based medicine? Curr Aesthesiol Rep. 2013 Mar; 3(2): 79-88. DOI 10.1007/ s40140-013-0017-6. Ehrenfeld J, Calderwood S. Pre-Operative Evaluation. In: Urman R, Ehrenfeld J, eds. Pocket Anesthesia. 2nd ed. Philadelphia, PA: Lippincott, Williams, & Wilkins; 2012: 1-1. Whitney G, Daves S, Hughes A, Watkins S, Woods M, Kreger M, Marincola P, Chocron I, Donahue B. Implementation of a transfusion algorithm to reduce blood product utilization in pediatric cardiac surgery. Paediatr Anaesth. 2013 Mar [Epub]. Ehrenfeld J, Urman R. Ethical Issues & Event Disclosure. In: Urman R, Ehrenfeld J, eds. Pocket Anesthesia. 2nd ed. Philadelphia, PA: Lippincott, Williams, & Wilkins; 2012: 33-1. Wray C, Scovotti J, Tobis J, Niemann C, Planinsic R, Walia A, Findlay J, Wagener G, Cywinski J, Markovic D, Hughes C, Humar A, Olmos A, Sierra-Anderson R, Busuttil R, Steadman R. Liver Transplantation outcome in patients with angiographically proven coronary artery disease: a multi-institutional study. Am J Transplant. 2013 Jan;13(1):184-91. Hernandez A. Commentary on sedation and delirium in the ICU. In: Cohn S, Brower S, eds. Surgery: Evidence-Based Practice. Shelton, CT: PMPH-USA; 2012. Xu P, Grueter B, Britt J, McDaniel L, Huntington P, Hodge R, Tran S, Mason B, Lee C, Vong L, Lowell B, Malenka R, Lutter M, Pieper A. Double deletion of melanocortin 4 receptors and SAPAP3 corrects compulsive behavior and obesity in mice. Proc Natl Acad Sci U S A. 2012 Jun;110(26):10759-64. Zamponi G, Currie K. Regulation of Ca(V)2 calcium channels by G protein coupled receptors. Biochimica Biophysica Acta. 2012 Oct [Epub]. Zuckerman S, France D, Green C, Leming-Lee S, Anders S, Mocco J. Surgical debriefing: a reliable roadmap to completing the patient safety cycle. Neurosurg Focus. 2012 Nov;33(5):E4. Books Ehrenwerth J, Eisenkraft J, Berry J, eds. Anesthesia Equipment: Principles and Applications. 2nd ed. Philadelphia, PA: Elsevier 2013. Matthews K, Urman R, Ehrenfeld J, eds. Anesthesiology: A Comprehensive Review for the Written Boards and Recertification. New York, NY: Oxford University Press; 2013. Urman R, Ehrenfeld J, eds. Morgan and Mikhail’s Clinical Anesthesiology Flashcards. New York, NY: McGraw-Hill Professional; 2013. Urman R, Ehrenfeld J, eds. Physicians’ Pathways to Non-Traditional Careers and Leadership Opportunities. 2012 ed. New York, NY: Springer; 2012. Urman R, Ehrenfeld J, eds. Pocket Anesthesia. 2nd ed. Philadelphia, PA: Lippincott, Williams, & Wilkins; 2012. Book Chapters Banerjee A. Crush injury and crush syndrome. In: Kellum J, Fortenberry J, Fuchs Banerjee A. Crush injury and crush syndrome. In: Kellum J, Fortenberry J, Fuchs B, Shaw A, eds. Decision Support System in Critical Care Medicine. Wilmington, DE: Decision Support in Medicine, LLC; 2013. Available at: http://www. decisionsupportinmedicine.com. Banerjee A, Pandharipande P. Delirium. In: Bope E, Rakel R, Kellerman R, eds. Conn’s Current Therapy 2013. Philadelphia, PA: Saunders/Elsevier; 2013: 932-935. Baysinger C. Antepartum and postpartum hemorrhage - prediction and management. In: Kellum J, Fortenberry J, Fuchs B, Shaw A, eds. Decision Support System in Critical Care Medicine. Wilmington, DE: Decision Support in Medicine, LLC; 2013. Available at: http://www.decisionsupportinmedicine.com. Beauchamp R, Higgins M. Perioperative Patient Safety. In: Townsend C, Beauchamp R, Evers B, Mattox K, eds. Sabiston Textbook of Surgery. 19th Ed. Philadelphia, PA: Elsevier Saunders 2012: 201-210. Berry J. Tactical First Aid (TFA). TacMedicine. Nashville, TN 2013: 48. 54 Berry J, Harvey S. Laryngoscopic orotracheal and nasotracheal intubation. In: Hagberg C, ed. Benumof and Hagberg’s Airway Management. 3rd ed. Philadelphia, PA: Elsevier 2012: 346-358. Hernandez A. Management of acute myocardial infarction and cardiogenic shock. In: Cohn S, Brower S, eds. Surgery: Evidence-Based Practice. Shelton, CT: PMPH-USA; 2012: 901-906. Howson S, Barwise J, Parmley C. Cardiovascular Therapy. In: Newfield P, Cottrell J, eds. Handbook of Neuroanesthesia. Philadelphia, PA: Lippincott Williams & Wilkins; 2012 Oct: 372-384. Hughes C, Pandharipande P. Altered mental status: delirium and coma. SCCM Adult Multiprofessional Self-Assessment Review Book on Neurologic Critical Care. 2012. Hughes C, Pandharipande P. New paradigms in sedation of the critically ill patient. In: Stevens R, Sharshar T, Ely E, eds. Brain Disorders in Critical Illness. United Kingdom: Cambridge University Press 2013. Hughes C, Weavind L, Pandharipande P. Sedation, paralysis, and pain management of the critically ill obese patient. In: Solh A, ed. Critical Care Management of the Obese Patient. Hoboken, NJ: Wiley-Blackwell 2012. Huntoon M. Emerging Imaging Tools for Interventional Pain. In: Deer T, Leong M, Buvanedran A, Gordin V, Kim P, Panchal S, Ray A, eds. Comprehensive Treatment of Chronic Pain by Medical,Interventional, and Integrative Approaches: The American Academy of Pain Medicine Textbook on Patient Management. New York, NY: Springer 2013: 575-580. Hyman S. Preventing Physician Burnout. In: Urman R, Ehrenfeld J, eds. Physicians’ Pathways to Non-Traditional Careers and Leadership Opportunities. New York, NY: Springer Press; 2012: 35-43. Mehta P, Zaleski K, Foege R, Peeters-Asdourian C, Jackson T, Meenal P. Acute and Chronic Pain. In: Matthews K, Urman R, Ehrenfeld J, eds. Anesthesiology: A Comprehensive Review for the Written Boards and Recertification. New York, NY: Oxford University Press; 2013 Mar. Neeley R. Acute altered mental status. In: Kellum J, Fortenberry J, Fuchs B, Shaw A, eds. Decision Support System in Critical Care Medicine. Wilmington, DE: Decision Support in Medicine, LLC; 2013. Available at: http://www.decisionsupportmedicine. com. Neeley R. Transcranial Doppler Sonography. In: Ehrenfeld J, Cannesson M, eds. Monitoring Technologies in Acute Care Environments. New York, NY: Springer; 2013. Pandharipande P, Banerjee A. Sedation and delirium. In: Parsons P, Wiener-Kronish P, eds. Critical Care Secrets. 5th ed. Philadelphia, PA: Saunders/Elsevier; 2012: 512-520. Parmley C. Legal Issues in Anesthesiology. In: Longnecker D, Brown D, Newman M, Zapol W, eds Anesthesiology. 2nd ed. New York, NY: McGraw-Hill Professional; 2012. Rothman B, Berry J. Monitoring ventilation. In: Ehrenwerth J, Eisenkraft J, Berry J, eds. Anesthesia Equipment: Principles and Applications. 2nd ed. Philadelphia, PA: Elsevier 2013. St Jacques P, Berry J. Perioperative informatics. In: Ehrenwerth J, Eisenkraft J, Berry J, eds. Anesthesia Equipment: Principles and Applications. 2nd ed. Philadelphia, PA: Elsevier 2013. Steele S, Holroyd K, Fadem T. Creating Ethical, High-Value Industry-Academic Partnerships. In: Alving B, Dai K, Chan S, eds. Translational Medicine - What, Why and How: An International Perspective. Basel, Switzerland: Karger Publishers 2013: 82-88. Terhune K, Pandharipande P. Delirium in the ICU. In: Le Roux P, Levine J, Kofke W, eds Monitoring in Neurocritical Care. Philadelphia, PA: Sauders; 2013 Mar. Urman R, Ehrenfeld J. Pharmacology: Antibiotics and Herbal Medications. In: Urman R, Ehrenfeld J, eds. Pocket Anesthesia. 2nd ed. Philadelphia, PA: Lippincott, Williams, & Wilkins; 2012: 2-44-49. Wagner C, Ashby N, Kennedy J. Intensive Care. In: Matthews K, Urman R, Ehrenfeld J, eds. Anesthesiology: A Comprehensive Review for the Written Boards and Recertification. New York, NY: Oxford University Press; 2013 Mar: 591-611. Walia A, Schumann R. Practice Patterns of Liver Transplant Anesthesiology. In: Wagener G, ed Liver Anesthesiology and Critical Care Medicine. New York, NY: Springer; 2012 Jan;111-130. Weinger M, Berry J. Vigilance, alarms, and integrated monitoring systems. In: Ehrenwerth J, Eisenkraft J, Berry J, eds. Anesthesia Equipment: Principles and Applications. 2nd ed. Philadelphia, PA: Elsevier 2013. Weinger M, Berry J, Loeb B. Ergonomics of the anesthesia workspace. In: Ehrenwerth J, Eisenkraft J, Berry J, eds. Anesthesia Equipment: Principles and Applications. 2nd ed. Philadelphia, PA: Elsevier 2013. Case Reports Austin T, Botta E, Sripada R. Monoplegia Following Vascular Transposition. Clin Anesth. 2013 Mar;25(2):162-4. Austin T, Franklin A. Outpatient Rehabilitation of Pediatric Complex Regional Pain Syndrome. J Clin Anesth. 2013 Mar [Epub]. Bowens C, Dobie K, Devin C, Corey J. An approach to neuraxial anesthesia for the severely scoliotic spine. Br J Anaesth. 2013 May [Epub]. Card E, Nelson D, Jeskey M, Miller A, Michaels D, Hardeman W, Hale M, Morse J, St Jacques P, Berry J. Early detection of a blood transfusion reaction utilizing a wireless remote monitoring device. Medsurg Nurs. 2012 Sep-Oct; 21(5):299-302, 308. Franklin A, Austin T. The Use of a Continuous Brachial Plexus Catheter to Facilitate Inpatient Rehabilitation in a Pediatric Patient with Refractory Upper Extremity Complex Regional Pain Syndrome. Pain Practice 2013 Feb;13(2):109-13. Tsoulfas G, Elias N, Sandberg W, Ko D, Kawai T, Cosimi A, Tsitsopoulos P, Agorastou P, Hertl M. Liver transplantation results in complete neurologic recovery from malignant hypertension secondary to fulminant hepatic failure: a case report. Ann Transplant. 2012 Jan-Mar;17(1):117-21. Editorials Baysinger, C. Committee Reports: Economics and Governmental Affaris Committee: Local Action is Needed Now. SOAP Newsletter. 2012 Summer. Baysinger, C. Editorial Comment on: McDonald S, Fernando R, Ashpole K, Columb M. Maternal cardiac output changes after crystalloid or colloid coload following spinal anesthesia for elective cesarean delivery: a randomized controlled trial. Anesth Analg. 2011 Oct;113(4) Obstetric Anesthesia Digest. 2012 Dec;32(4):240-240. Baysinger, C. Editorial Comment on: Murphy J, Togioka B. Aspiration in early pregnancy: risk factors revisited. J Clin Anesth 2011;23:435-6. Obstetric Anesthesia Digest. 2012 Sep;32(3):169-169. Baysigner C. Editorial Comment on: Wolfson A, Lee A, Wong R, Arheart K, Penning D. Bilateral multi-injection iliohypogastric-ilioinguinal nerve block in conjunction with neuraxial morphine is superior to neuraxial morphine alone for postcesarean analgesia. J Clin Obstetric Anesthesi Digest. 2013; 33(2). Newsletter Articles Brockway E, Westman A, Robertson A. PreAnesthetic Assessment of the Patient with Cirrhosis-Related Pulmonary Complications. Anesthesiology News. 2012 Apr;28-32. Baysinger C. Nitrous oxide for labor analgesia. SOAP Newsletter. 2012 Summer. Easdown J. Great Books on Education. SEA Newsletter. 2012 Fall;31(2). Easdown J. Resources for Scholarly Curriculum Development. SEA Newsletter. 2013 Spring;32(1). McQueen K. Awarding Outstanding Humanitarianism: The 2nd Annual Nicholas M. Greene, M.D. Award. ASA Newsletter. 2012 Dec;76(12):24. McQueen K. Central America Lifebox Initative. ASA Newsletter. 2013 Mar;77(3):50. McQueen K. Evolving Expectations of Providing Anesthesia in Humanitarian Settings. ASA Newsletter. 2013 Jan;77(1):26-28. Nesbitt K. Juvenile Diabetes: An Update. SPA News. 2013 Mar;26(1). Nesbitt K. Pediatric Anesthesiology 2013 Meeting Reviews - Sunday, March 17 Session I. SPA News. 2013 July;26(2). Rothman B. Cloud Computing: What is the ‘Cloud?’. ASA Newsletter. 2012 Aug;76(8):24-26. Starr S, Baysinger C. Inhaled nitrous oxide for labor: utilizing a blender device to provide patient-controlled analgesia. Sensor Online. 2013 Jan;24: 6-9. Letters Ehrenfeld J. Which is the original and which is the modified rapid sequence induction and intubation? Let history be the judge!---author’s reply. Anesth Analg. 2013 Jan;116(1):265. Huntoon M. A humble farmer-on fertile ground. Reg Anesth Pain Med . 2013 JanFeb;38(1):1-2. Krupka D, Sandberg W. The correct business case for the Michigan Keystone Patient Safety Program in ICUs. Am J Med Qual. 2012 Mar-Apr;27(2):175. Huntoon M. Case reports, cover updates, statistics, and targeted intrathecal infusions. Reg Anesth Pain Med. 2013 Mar-Apr;38(2):89-90. McPherson J, Boehm L, Wagner C, Ely E, Pandharipande P. The authors reply. Crit Care Med. 2013 Jun;41(6):e101-2. Richardson M, Litman R. In utero myelomeningocele repair: baby steps and giant leaps for fetal surgery. Anesthesiology. 2013 May;118(5):1016-1018. Richardson M, Ikeda A, Isono S, Litman R. In Reply (Facemask ventilation and neuromuscular blockade in anesthetized patients). Anesthesiology. 2013 Apr;118(4):994-996. Richardson M, Litman R. Ventilation before paralysis: crossing the rubicon, slowly. Anesthesiology. 2012 Sep;117(3):1-3. Thompson A, Mahajan A. Perioperative Management of Cardiovascular Implantable Electronic Devices (CIEDs): What every anesthesiologist needs to know. Anesth Analg. 2013 Feb;116:276-277. Watkins S. A simulation-based trial of surgical-crisis checklists. N Engl J Med. 2013 Apr 11;368(15):1459. Wilson J, Bick J, Thompson A. Another use for transesophageal echocardiography during aortic valve bypass surgery. J Cardiothorac Vasc Anesth. 2012 Oct. Editorial Reviews Poems Baysinger C. Commentary on: Abdallah F, Halpern S, Margarido C. Transversus abdominis plane block for postoperative analgesia after Caesarean delivery performed under spinal anaesthesia? A systematic review and meta-analysis. Br J Anaesth. 2012 Nov;109(5):679-87. Faculty of 1000 Reviews. 2013 April. http://f1000.com/ prime/717954821. Harvey S. Family Quartet. Able Muse. 2012 Winter;14. Baysinger C. Commentary on: Bauchat J, McCarthy R, Koski T, Cambic C, Lee A, Wong C. Prior lumbar discectomy surgery does not alter the efficacy of neuraxial labor analgesia. Anesth Analg. 2012 Aug;115(2):348-53. Faculty of 1000 Reviews. 2012 Nov. Baysinger C. Commentary on: Dean G, Jacobs A, Goldstein R, Gevirtz C, Paul M. The safety of deep sedation without intubation for abortion in the outpatient setting. J Clin Anesth. 2011 Sep;23(6):437-42. Faculty of 100 Reveiws. 2012 July. http://f1000. com/717949613. Baysinger C. Commentary on: Srofenyoh E, Ivester T, Engmann C, Olufolabi A, Bookman L, Owen M. Advancing obstetric and neonatal care in a regional hospital in Ghana via continuous quality improvement. Int J Gynaecol Obstet. 2012 Jan;116(1):1721. Obstetric Anesthesia Digest. 2013; 33(1). Harvey S. Deposition in New York. Anesthesiology. 2012 Aug;117(2): 422. doi: 10.1097/ALN.0b013e3182531b88. Harvey S. From Auschwitz with love. Pharos Alpha Omega Alpha Honor Med Soc. 2012 Summer;75(3):25. Harvey S. Poet’s Plight. Chest. 2012;142(5):1352. doi:10.1378/chest.11-3087. Harvey S. The Meditation Garden. JAMA. 2012;308(11):1072. doi:10.1001/ jama.2012.9881. Harvey S. University Clinic. Chest. 2012;142(5):1352. doi:10.1378/chest.1103137 Hester D. First case with Adèle and Aegis. Anesthesiology. 2012 Sep;117(3):669. Hester D. Can’t Stop the Clock. Tabula Rasa. 2013 Jun; VII. 55 Achieving Balance The Vanderbilt Department of Anesthesiology is a dynamic group, providing the very best in patient care, presenting challenging educational programs for our trainees, and leading our specialty in investigational research. But productivity and career satisfaction isn’t all about work. We know how to take that same energy and have a great time. 56 We gather regularly for family-friendly events, events to welcome new residents, fundraisers for our Vanderbilt International Anesthesia program, and other fun activities throughout the year. Here are just a few images from our events.