Theories and Techniques of Behaviour Language Therapy Interventions
advertisement

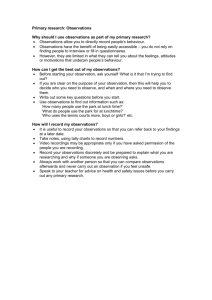
Theories and Techniques of Behaviour Change and their Application to Speech and Language Therapy Interventions Dr. Caroline Wood UCL Centre for Behaviour Change The UCL Centre for Behaviour Change CBC Team CBC Associates CBC Volunteers Key aims: • To increase the quality and quantity of research in behaviour change at UCL • Build communities to facilitate the engagement of policymakers, practitioners and researchers with expertise in behaviour change (e.g. project input and collaborative work) • Host cross-disciplinary events addressing social, practical and methodological issues • Provide teaching and training in principles and practice of behaviour change But first: Some important definitions… What do we mean by ‘behaviour’? Agreed across disciplines of psychology, sociology, anthropology and economics – “Anything a person does in response to internal or external events – Actions may be • overt (motor or verbal) and directly measurable, or • covert (activities not viewable but involving voluntary muscles) and indirectly measurable; – behaviours are physical events that occur in the body and are controlled by the brain” Hobbs, Campbell, Hildon, & Michie, 2011 What is a ‘behaviour intervention’? “An action or set of activities to get individuals to behave differently from how they would act without such an action” It can change … how people behave how often they perform a behaviour how long they act for over what time period • Considerable recent interest and investment into developing and evaluating health behaviour change interventions (HBCIs) • Increasing evidence for the effectiveness of HBCIs • Rise in wide use and implementation of these interventions in areas beyond research: Health services, public health practices and areas of social policy (Craig et al. 2008) Intervening at different levels… smoking cessation, increasing physical activity, medication adherence service delivery (medical procedures and techniques) adherence to guidelines, complying with policy “Can language therapy strategies and resources developed for spoken language bring observable change to Deaf adults’ therapeutic skills?” Joanna Hoskin, Bencie Woll & Ros Herman “Investigating the impact of a structured online environment (‘Better Conversations with Aphasia’) for Speech and Language Therapists (SLTs) to develop their skills in delivering conversation therapy” Suzanne Beeke, Firle Beckley, Wendy Best et al. “Improving transitions across SLT services in Greater Glasgow and Clyde for adults with longterm speech, language, swallowing or communication (SLSC) needs: a qualitative study of SLTs’ and service users’ views” Elspeth McCartney & Margaret Muir Intervention design: Where to start? MRC Guidance1 for developing and evaluating complex interventions: Tendency to use the ISLAGIATT2 principle of intervention design… 1. 2. Craig et al, 2009 BMJ Martin Eccles, Emeritus Professor of Clinical Effectiveness So how can we do better? Use an integrative theoretical framework • i.e. a framework that integrates a wide range of theories Take a systematic approach to intervention design • Start by understanding your target behaviour in context • Make a behavioural diagnosis • Design an intervention based on the behavioural diagnosis Understand the problem Make a diagnosis Prescribe treatment The key questions: 1. What exactly do we want the person to do? 2. What will it take to get them to do it? 3. How do we get them to do it? 4. How do we roll out the intervention? The key questions: 1. What exactly do we want the person to do? 2. What will it take to get them to do it? 3. How do we get them to do it? 4. How do we roll out the intervention? Specifying the target behaviour: When do they need to do it? Who needs to do what differently to achieve the desired change? Where do they need to do it? How often do they need to do it? With whom do they need to do it? In what context do they need to do it? Target behaviour should be specific: e.g. ‘Eat xxx fewer calories per day for xx days’ is more specific than ‘eat less’ A worked example… Proposed intervention: Target behaviour = Increasing participation in parent-toddler language promotion programme Target population = Parents The key questions: 1. What exactly do we want the person to do? 2. What will it take to get them to do it? 3. How do we get them to do it? 4. How do we roll out the intervention? The COM-B: A simple model to understand behaviour… Psychological or physical ability to enact the behaviour Reflective and automatic mechanisms that activate or inhibit behaviour Physical and social environment that enables the behaviour Michie et al (2011) Implementation Science, 6, 42 The Behaviour Change Wheel …result of synthesising 19 frameworks to classify interventions (health, environment, culture change and social marketing) Michie et al (2011) Implementation Science, 6, 42 Proposed intervention: Target behaviour = Increasing participation in parent-toddler language promotion programme Target population = Parents Behavioural diagnosis: “I don’t have time” “We don’t have a car to get to the sessions” Results of behavioural diagnosis: Physical opportunity …needs to shift in order for the behaviour to occur The key questions: 1. What exactly do we want the person to do? 2. What will it take to get them to do it? 3. How do we get them to do it? 4. How do we roll out the intervention? Select intervention functions… Inner ring: • 9 intervention functions (what purpose does the intervention serve?) Refer to Michie et al. (2011) or to BCW guide (Michie et al. 2014) Appropriate intervention functions include: Restrictions Environmental restructuring Enablement Training Changing the physical or social context E.g. “Sending a text-message several days before the next session to remind parents to book travel arrangements” We selected: Environmental restructuring Changing the physical or social context • How could we operationalise ‘environmental restructuring?’ • Likely to consist of more than one behaviour change technique Without knowing the ‘active ingredients’ in an intervention: X We can’t easily replicate X We can’t assess effectiveness Behaviour Change Technique Taxonomy v1 (BCTTv1): Points to consider… • • Shared language for specifying the ‘active ingredients’ of behaviour change interventions Why choose BCT X over BCT Y? – look at the evidence for the effectiveness in • situations 93 distinct BCTs with labels, definitions and examples similar populations and to yours Michie et al (2013) Annals of Behavioral Med, 46(1) • Is this BCT appropriate for the population and setting of my intervention? Environmental restructuring • Can I afford to use this BCT? Is it going to be acceptable to my population? Can it be - Refer to Michie et al. (2011) or BCW guide (Michie et al. 2014) delivered in my intervention? This intervention function translates into the following BCTs: E.g. • Prompts / cues • Adding objects to the environment • Remove access to the reward The key questions: 1. What exactly do we want the person to do? 2. What will it take to get them to do it? 3. How do we get them to do it? 4. How do we roll out the intervention? Outer ring: • 7 policy categories Select appropriate policy categories: • Refer to Michie et al. (2011) • Or to BCW guide Michie et al (2011) Implementation Science, 6, 42 Appropriate policy categories include: Environmental / social planning Guidelines Fiscal measures Regulation Legislation Creating documents that recommend or mandate practice. E.g. “The programme handbook was amended to include advice for practitioners on how to conduct sessions at parent/toddler’s home” Our intervention: Target behaviour = Increasing participation in parent-toddler language promotion programme Target population = Parents Behavioural diagnosis: “Parents unlikely attend programme sessions due to transport not being available”: Physical opportunity Select intervention functions and BCTs: Physical opportunity maps onto Environmental restructuring. “Parents were sent a text message 2 days (BCT = Prompts/cues) before the session to remind them to book travel arrangements” Select policy categories: ER maps onto Guidelines. “Advice for practitioners on how to conduct home sessions added to programme handbook” Your toolbox: • Start by understanding the behaviour – Behavioural analysis and diagnosis using COM-B • Systematically select appropriate intervention functions and policy categories to bring about change – Design the intervention (‘prescribed treatment’) using BCW based on the behavioural diagnosis • Specify active ingredients in the intervention – Using BCT Taxonomy @UCLBehaveChange behaviourchange@ucl.ac.uk Dr Caroline Wood caroline.wood@ucl.ac.uk Do you work in behaviour change? We want to hear from you! Go to our website: www.ucl.ac.uk/behaviour-change •Answer a short questionnaire •You will be added to our database of expertise •Linked in with other academics and opportunities to be contacted for your expert input/collaboration Theories & Techniques of Behaviour Change: Applications to Conversation Therapy for Aphasia Fiona Johnson UCL Division of Psychology & Language Sciences Guys & St Thomas’s Community Services Supervised by: Dr Suzanne Beeke, Professor Wendy Best Aims for today • Discuss role of behaviour change theory in SLT intervention research • Describe applications of behaviour change theory & techniques in my own research • Highlight benefits and challenges to using a behaviour change approach in SLT Background to research Better Conversations with Aphasia project Own interests in implementation MRC guidelines for developing & evaluating complex interventions (2008) Behaviour change research Why look at theories of behaviour change? • Need for theory to explain: – What works? – Why hasn’t it worked? – How can I adapt it without compromising effectiveness? • Expanding remit of SLTs e.g. Social & community participation focus to intervention Better Conversations with Aphasia Raising Awareness of Conversation • Session 1: Conversation & Agrammatism • Session 2: Turn-taking & Conversational Sequences • Session 3: Repair Barriers & Facilitators in Conversation • Session 4: Strategies for PWA • Session 5: Strategies for CP • Session 6: Topic Consolidating Strategy Use • Session 7: Practicing strategies in conversation • Session 8: Reviewing & Moving forward Key features of therapy • PWA & CP present for all sessions • Therapy targets Barrier & Facilitator behaviours in conversation • Materials include handouts and couples own videoed conversations • Strategies practiced via coached conversation, and homework activities Gaps in current knowledge... BCA outcome measurement is focussed on: • Decrease in barrier behaviours • Increase in facilitative behaviours Assumed theory of change appears to be: • Raised awareness about ones own conversational behaviours will lead to changes in behaviour But... • Knowing what to do ≠ Doing it (Barnes, Dunning & Rehfeldt 2011; Berkhof, van Rijssen, Schellart, Anema & Van der Beek 2011; Kennedy, Regehr Rosenfield, Roberts, Lingard 2004; Webb & Sheeran 2006) So... • Existing accounts of how conversation therapy works do not adequately explain how intended outcomes are produced What works in conversation therapy for aphasia & how? My research aims: • Describe factors that promote or constrain the use of targeted behaviour (i.e. the aspects of Capability, Opportunity & Motivation that determine conversational behaviour) • Identify mechanisms that support conversational behaviour change (i.e. Changes to Capability, Opportunity & Motivation that enable change to conversational behaviour) • Identify potentially active ingredients within Better Conversations with Aphasia (i.e. Therapy’s BCTs) Identifying behaviour change techniques present in the BCA therapy programme • Taxonomy of Behaviour Change Techniques v1 (Michie et al 2013) • Coding of BCA’s 8 session plans + all therapy handouts used with participants • Coding of two raters compared to establish: – Behaviour change techniques agreed to be present – Overall reliability of applying taxonomy Coding Better Conversations with Aphasia Extract from BCA A practice conversation with SLT: Video the task. • PWA to put their chosen strategies into practice as needed • SLT to coach as necessary After the task - discuss ease of strategy use (SLT to facilitate this discussion by replaying parts of the task if it has been video recorded). BCT 23 Behavioural practice/ rehearsal BCT 15 Prompts/cues BCT 8 Feedback on behaviour Findings: • 16 reliably identified Behaviour Change Techniques • Identification of potential new techniques • Mapping techniques to mechanisms of change = emerging theory of change for BCA Findings: Overall Reliability of Using BCT Taxonomy with Better Conversations with Aphasia • Two different measures of IRR carried out – Cohen’s Kappa (adjusts for chance agreement) – Percentage Agreement (better reflection of range of decision making) Cohen’s kappa 0.477 = ‘moderate’ agreement Percentage Agreement 79.8% 80% is threshold for satisfactory agreement What issues compromised IRR? • Different judgements re: – Intended meaning of therapy descriptions – Whether activities had a clear target behaviour • Differing levels of confidence in coding: – More subjective concepts e.g. BCT 85 Salience of Consequences – ‘Unfamiliar’ concepts e.g. BCT 68 Action Planning Some Reflections Challenges • Establishing consistency/ confidence with new terminology & concepts • Conversation Therapy – jointly produced action vs. individual behaviour Limitations • Behaviour change does not account for other intended outcomes of therapy e.g. Increased acceptance of aphasia, well being, QoL Questions • Communicative Behaviour Change = minute adjustments in fast flowing context • ?transferability of health behaviour research • Behaviour change for people with neurological impairments • ?transferability of research into non-impaired populations Conclusions Behaviour change theory & tools • Offer a framework for investigating and describing SLT interventions directed at activity & participation • Enable a systematic analysis of: – The influences on communicative behaviour – Possible mechanisms for changing behaviour – Techniques involved in changing behaviour • Provide a basis for building theories of change in some SLT interventions • Generate new insights with direct applications to clinical practice Thank you! Any Comments? Questions? fiona.johnson1@nhs.net fiona.johnson.09@ucl.ac.uk @msfionajohnson