Phenotypic knockout of VEGF-R2 and Tie-2 with angiogenesis in vivo
advertisement

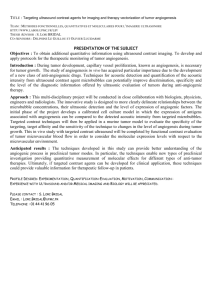
Phenotypic knockout of VEGF-R2 and Tie-2 with an intradiabody reduces tumor growth and angiogenesis in vivo Nina Jendreyko*†, Mikhail Popkov*, Christoph Rader‡, and Carlos F. Barbas III*§ *Department of Molecular Biology and The Skaggs Institute for Chemical Biology, The Scripps Research Institute, 10550 North Torrey Pines Road, La Jolla, CA 92037; and ‡Experimental Transplantation and Immunology Branch, Center for Cancer Research, National Cancer Institute, National Institutes of Health, Bethesda, MD 20892 Communicated by Richard A. Lerner, The Scripps Research Institute, La Jolla, CA, April 18, 2005 (received for review March 21, 2005) intrabody 兩 protein engineering 兩 therapeutic 兩 gene transfer 兩 combination therapy A ngiogenesis, the generation of new blood vessels, plays a key role in tumor growth and metastasis. Recent data suggest that agents that block endothelial cell proliferation and, thus, tumor angiogenesis are promising for cancer therapy (1). Tumor growth requires the establishment and remodeling of the vascular system, involving paracrine and autocrine signaling between various growth factors and endothelial receptors (2). The interaction between VEGF and their endothelial receptors, especially VEGF receptor 2 (VEGF-R2), activates receptorassociated kinase activity and initiates signaling pathways leading to tumor angiogenesis (3, 4). In addition to the VEGF-R2 pathway, endothelial cells also require the expression of proteins, such as angiopoietin (Ang)-1 and Ang-2 and their receptor Tie-2, for blood vessel stabilization and sprouting (5, 6). The VEGF-R2 and Tie-2 receptor pathways are currently believed to be the primary modulators of tumor angiogenesis (7). From a therapeutic perspective, the VEGF兾VEGF-R2 complex and the Tie-2兾Ang2 complex, both formed on the surface of proliferating endothelial cells, are attractive targets for antiangiogenic agents. Interference with the VEGF兾VEGF receptor system by means of retroviral expression of dominant-negative VEGF receptor variants (8), VEGF-neutralizing antibodies (9, 10), or recombinant VEGF-neutralizing receptor variants (11, 12), or interference with the Tie-2 receptor pathway by means of soluble dominant-negative receptors (13, 14), intrabodies (15), www.pnas.org兾cgi兾doi兾10.1073兾pnas.0503168102 or oligonucleotide-based strategies including RNA aptamers and RNA interference (16), resulted in reduced tumor growth and tumor vascularization. Several studies suggest that the VEGF receptor pathway and the Tie-2 pathway are independent mediators of in vivo angiogenesis, leading to the hypothesis that simultaneous interference with both pathways should result in additive effects on tumor growth (14, 17). To date, no studies have reported the effect of simultaneous VEGF-R2兾Tie-2 antagonism in vivo. A key feature of antibodies is their ability to bind almost any molecule with high specificity and affinity, providing powerful tools for diagnostic and therapeutic applications. Single-chain antibody fragments, termed ‘‘intrabodies,’’ have the potential for intracellular applications and have been exploited by a number of laboratories (18–20). Intrabodies present an alternative to methods of gene inactivation that target genomic DNA or messenger RNA, such as antisense oligonucleotides (21), zincfinger proteins (22), targeted gene disruption, or the relatively new approach of RNA interference (23). Unlike technologies that target nucleic acids, intrabodies operate at the posttranslational level and can be directed to relevant subcellular compartments and precise epitopes on target proteins (19, 24), potentially blocking only one of several possible functions of an expressed protein. We recently demonstrated inhibition of tumor growth and tumor-induced angiogenesis by Tie-2 receptor down-regulation by means of single-chain antibody fragment (scFv) intrabody expression (15). The results indicated that blocking Tie-2 activation alone was not sufficient to completely halt tumor angiogenesis, presumably because the VEGF pathway is also critical for the development of angiogenesis. Bispecific and tetravalent antibody fragments should improve and expand the inhibitory potential of single-chain, monospecific intrabodies by increasing affinity for antigen and more efficiently inhibiting protein function or intracellular trafficking. Recently, we reported the development and in vitro characterization of a human reactive tetravalent endoplasmic reticulum (ER)targeted intradiabody for the simultaneous surface depletion of two endothelial transmembrane receptors, VEGF-R2 and Tie-2 (17). Because tumor progression is a process involving multiple stages and pathways with built-in redundancies, a potent antitumor strategy should inhibit multiple independent targets. This study was performed to test whether a simultaneous phenotypic knockout of VEGF-R2 and Tie-2 is more powerful in antitumor and antiangiogenic therapy than a phenotypic knockout of Abbreviations: Ang, angiopoietin; ER, endoplasmic reticulum; HUVEC, human umbilical vein-derived endothelial cells; moi, multiplicity of infection; scFv, single-chain antibody fragment; VEGF-R2, VEGF receptor 2. †Present address: Humboldt University, Charité Department of Pediatrics, Augustenburger Platz 1, 13353 Berlin, Germany. §To whom correspondence should be addressed: E-mail: carlos@scripps.edu. © 2005 by The National Academy of Sciences of the USA PNAS 兩 June 7, 2005 兩 vol. 102 兩 no. 23 兩 8293– 8298 MEDICAL SCIENCES The endothelial cell receptor-tyrosine kinases, VEGF receptor 2 (VEGF-R2) and Tie-2, and their ligands, vascular endothelial growth factor (VEGF) and angiopoietins 1 and 2, respectively, play key roles in tumor angiogenesis. Several studies suggest that the VEGF receptor pathway and the Tie-2 pathway are independent and essential mediators of angiogenesis, leading to the hypothesis that simultaneous interference with both pathways should result in additive effects on tumor growth. In this study, a human melanoma xenograft model (M21) was used to analyze the effects of simultaneous intradiabody depletion of vascular endothelial growth receptor-R2 and Tie-2 on tumor angiogenesis and tumor xenograft growth. The intradiabodies were expressed from recombinant adenovirus delivered through subtumoral injection. Blockade of both VEGF-R2 and Tie-2 pathways simultaneously or the VEGF receptor pathway alone resulted in a significant inhibition of tumor growth and tumor angiogenesis (92.2% and 74.4%, respectively). In addition, immunohistochemical staining of intradiabodytreated tumors demonstrated a decreased number of tumor-associated blood vessels versus control treatment. Previous studies with intrabodies had demonstrated that the Tie-2 receptor pathway was essential for tumor growth. The simultaneous blockade of the VEGF and Tie-2 pathways resulted in effective inhibition of tumor growth and demonstrated the potential of simultaneous targeting of multiple pathways as a therapeutic strategy. VEGF-R2 alone. Because VEGF-R2 has attracted so much attention as a target for antiangiogenic therapy, we choose to compare the knockout of VEGF-R2 to the double knockout of VEGF-R2 and Tie-2. To accomplish this comparison, ERtargeted bispecific ( VEGF-R2兾Tie-2) and monospecific (VEGF-R2) tetravalent intradiabodies were generated, and a replication-deficient adenoviral vector was used for local delivery in a melanoma xenograft mouse model. Our results indicate that the simultaneous targeting of the VEGF receptor pathway and the Tie-2 pathway results in a greater antitumor and antiangiogenic effect in vivo than targeting VEGF-R2 alone and that the intradiabody approach is an efficient means of blocking two receptors. Materials and Methods Cell Culture. Human umbilical vein-derived endothelial cells (HUVEC) were maintained in endothelium growth medium supplemented with 2% bovine brain extract (BioWhittaker). Human embryonic kidney 293 cells (American Type Culture Collection) were cultured in DMEM supplemented with 10% FBS (HyClone) and 1% antibiotics. Human melanoma cell line M21 (obtained from Donald Morton, John Wayne Cancer Center, Santa Monica, CA) was maintained in RPMI medium 1640, containing 10% FCS and 1% antibiotics. Mouse endothelial cell line MS1 (American Type Culture Collection) was maintained in DMEM supplemented with 4 mM L-glutamine兾 1.5 g/liter sodium bicarbonate兾4.5 g/liter glucose兾1 mM sodium pyruvate兾10% FCS兾1% antibiotics. Immortalized human microvasculuture endothelial cells (HMEC-1) were obtained from Centers for Diseases Control兾Emory University (25). Cells were maintained in endothelial basal medium (BioWhittaker), supplemented with 10 ng/ml epidermal growth factor兾1 g兾ml hydrocortisone兾10% FCS兾1% antibiotics. All cells were cultured at 37°C in 5% CO2. asymmetric SfiI sites, and binding activity of the expressed scFv was confirmed by ELISA. Cloning of Diabodies. The scFv VR05 and 2S08b or VR05 and VR05 genes were linked through the second and third heavy chain constant domains of human IgG1 to generate bispecific and monospecific diabodies, respectively. Construct VRO5-CH2CH3-2SO8b: scFv VR05 was PCR-amplified by using primers extompseq and VEGF-R2-B (5⬘-GCC AGA CCC ACC GCC TCT AGA TGA GGA GAT GGT GAC CAG-3⬘). CH2-CH3 was amplified by using CH2-F (17) and CH3-B-1 (5⬘-AGT CTG GGT CAG ATC GAG CTC GGC CGC CTG TGC CGA GCC ACC CCC AGA ACC-3⬘). scFv 2S08b was amplified by using primer Tie-2-F (5⬘-TCT GGG GGT GGC TCG GCA CAG GCG GCC GAG CTC GAT CTG ACC CAG ACT-3⬘) and HSCG1234-B. Construct VRO5-CH2-CH3-VRO5: The Nterminal scFv VRO5 was used from the construct VR05-CH2CH3-VR05. CH2-CH3 was amplified by using CH-2-F and CH3B-2 (5⬘-AGT CTG GGT CAT CAC GAG CTC GGC CGC CTG TGC CGA GGC ACC CCC AGA ACC-3⬘). The C-terminal scFv was amplified by using VR05-F (5⬘-TCT GGG GGT GGC TCG GCA CAG GCG GCC GAG CTC GTG ATG ACC CAG ACT-3⬘) and dpseq. The N-terminal scFv and CH2-CH3 were combined by overlap extension PCR with primer ext (30) and CH3-B-1 or CH3-B-2, respectively. The C-terminal scFv was cloned into phagemid vector pComb3X between the SacI and SpeI sites. Finally, both constructs were combined by using the SacI sites and confirmed by DNA sequence analysis. The T2CH2-CH3-V2 control construct is described elsewhere (17). Assembly of Intradiabody Constructs in pAdTrackCMV and Generation of Adenoviral Plasmids by Homologous Recombination. The assem- bly of intradiabody constructs, the generation of adenoviral plasmids by homologous recombination, and the generation of high titer viral stocks was done essentially as described in ref. 17. Antibodies and Other Proteins. Recombinant human VEGF-R2 (KDR)兾Fc chimeric protein, recombinant mouse VEGF-R2 (Flk-1)兾Fc chimeric protein, recombinant human Tie-2兾Fc chimeric protein, mouse Tie-2兾Fc chimeric protein, biotinylated goat anti-human VEGF-R2 and Tie-2 polyclonal antibodies, and biotinylated normal goat IgG were purchased from R & D Systems. Rat anti-mouse CD31 (PECAM1) mAb, APCconjugated streptavidin, and biotinylated goat anti-rat IgG polyclonal antibodies were purchased from Pharmingen. Horseradish peroxidase-conjugated goat anti-human kappa antibody was from Southern Biotechnology Associates. Chimeric rabbit兾 human Fabs VR05 that binds to the extracellular domain of VEGF-R2 and 2SO8b that recognizes the extracellular domain of Tie-2 were generated as described in refs 26 and 27. Analysis of VEGF-R2 and Tie-2 Binding in ELISA. Binding studies by ELISA for Fab VR05 and 2S08b were performed as described in refs. 26–28. Conversion of a VEGF-R2 and Tie-2-Specific Fab into a scFv. Specific oligonucleotide primers (26, 29, 30) were used to amplify heavy chain variable domain and light chain variable domain gene segments from purified phagemid DNA of Fab VR05 and Fab 2S08b. Light chain variable domain segments of VR05 and 2S08b were amplified with ompseqgtg and RKB9Jo-BL. Heavy chain variable domain regions of VR05 and 2S08b were amplified with RSCVH1 or RSCVH4, respectively, and HSCG1234-B. Overlap extension PCR was done by using primers ompseq and RSC-B. The resulting overlap-PCR products encode a scFv in which the C-terminal light chain variable domain region is linked to the N-terminal heavy chain variable domain region through a peptide linker (SSGGGGSGGGGGGSSRSS). The scFv-encoding sequences were cloned into phagemid vector pComb3X by using 8294 兩 www.pnas.org兾cgi兾doi兾10.1073兾pnas.0503168102 VEGF-R2 and Tie-2 Surface Depletion with Intradiabodies. HUVEC or HMEC-1 cells (1.5 ⫻ 106) were infected with 50 multiplicity of infection (moi) (⬇65% of the cells were infected) of adenovirus-encoding VEGF-R2兾Tie-2 intradiabody, VEGF-R2兾 VEGF-R2 intradiabody, control intrabody T2V2, or no insert (mock). Cells were analyzed for Tie-2 and VEGF-R2 surface expression 3 days after infection by flow cytometry essentially as described in ref. 17. Formulas used for calculations of surface inhibition, after subtraction of the background of normal-goat IgG stained cells were: % of inhibition VEGF-R2 ⫽ (VEGFR2T2V2 ⫺ VEGF-R2intrabody)兾VEGF-R2T2V2 ⫻ 100 or % of inhibition Tie-2 ⫽ (Tie-2T2V2 ⫺ Tie-2intrabody)兾Tie-2T2V2 ⫻ 100. Endothelial Cell Tube Formation Assay. Endothelial cell tube formation assay was done essentially as described in ref. 17. Cell Proliferation Assay. M21 cells were seeded in 96-well plates in RPMI medium 1640, infected with different recombinant adenoviral constructs with mois ranging from 1 to 1,000, and the plate was incubated for 3 days at 37°C. [3H]thymidine (ICN Radiochemicals) at 0.5 Ci per well (1 Ci ⫽ 37 GBq) was added during the last 24 h of incubation. The cells were frozen at ⫺80°C overnight and subsequently processed on a multichannel automated cell harvester (Cambridge Technology, Cambridge, MA) and counted in a liquid scintillation -counter (Beckman Coulter). The background was defined by uninfected cells. The inhibition was calculated according to the following formula: % of inhibition ⫽ (background ⫺ infected cell count)兾background ⫻ 100. Cell proliferation was also measured by staining with trypan blue and counting the cell numbers by using a hemacytometer (for moi 200). Jendreyko et al. In Vivo Tumor Growth. For tumor growth experiments with s.c. Immunohistochemistry. Immunohistochemical localization was performed with rat anti-mouse CD31 by using a VECTASTAIN Elite peroxidase kit (Vector Laboratories) essentially as described in ref. 15. Results Chimeric Rabbit兾Human Fabs VR05 and 2S08b Bind to Human and Mouse Endothelial Cell Receptors VEGF-R2 and Tie-2. Using phage display (29), Fab VR05 against VEGF-R2 was previously selected from a chimeric rabbit兾human antibody library and subsequently purified to yield a nearly homogenous protein solution (27). The selection and purification of Fab 2S08b with specificity for Tie-2 was described in ref. 26. In ELISA, Fab VR05 bound to human and mouse VEGF-R2 and did not react with mouse or human VEGF-R1. In addition, Fab VR05 was able to block VEGF binding to human and mouse VEGF-R2 (27). Fab 2S08b bound to human and mouse Tie-2 and did not react with human Tie-1 (26). Flow cytometry analysis revealed that the VEGF-R2 epitope, recognized by VR05, is displayed on the surface of human (HUVEC) and mouse (MS1) cells and is an accessible target for antiangiogenic therapy. Surface plasmon resonance revealed that Fab VR05 binds both human and mouse VEGF-R2 with identical 3 nM affinity (27). Fab 2S08b recognized Tie-2 displayed by HUVEC and possessed a monovalent dissociation constant of 1.2 nM to human Tie-2 and 1 nM to mouse Tie-2 (26). Construction of Adenoviruses Encoding Bispecific, Tetravalent Intradiabody Against VEGF-R2 and Tie-2 and a Monospecific, Tetravalent Intradiabody Against VEGF-R2. Fabs VR05 and 2S08b were con- verted into scFv formats, with the light chain variable domain and heavy chain variable domain fragments covalently linked through a peptide linker consisting of 18 amino acids. Both scFv Fig. 1. Model of a bispecific, tetravalent intradiabody. Two scFv directed to Tie-2 and VEGF-R2, respectively, were linked through the second and third heavy chain constant domains of human IgG1 to form a 150-kDa dimer. Through the homophilic interaction of CH3, the N-terminal and C-terminal scFv modules are displayed bivalently. The N-terminal scFv module binds Tie-2 and the C-terminal scFv module binds VEGF-R2. An ER retention signal (KDEL) was appended at the C terminus. VR05 (VEGF-R2) and 2S08b (Tie-2) bound to their respective antigens as confirmed by ELISA (data not shown). Next, scFv VR05 and scFv 2S08b were linked through the second and third heavy chain constant domains of human IgG1. The scFv VR05 was also dimerized in the same manner. This reaction resulted in scFv-CH2-CH3-scFv expression cassettes, named VR05–2S08b and VR05-VR05, respectively. The scFv-CH2-CH3-scFv expression cassettes allowed production of a bifunctional tetravalent antibody construct from a single polypeptide. Through the homophilic interaction of CH3, two scFv-CH2-CH3-scFv molecules associate to form a 150-kDa dimer that displays the N-terminal and C-terminal regions of the scFv module bivalently as the intradiabody (Fig. 1). The scFv-CH2-CH3-scFv genes were cloned into a modified adenovirus shuttle vector pAdTrack CMV (31) by using two asymmetric SfiI sites. In these constructs, the scFv coding regions are flanked by a human light chain leader sequence at the 5⬘ end and a sequence encoding the HA-tag (YPYDVPDYA) and the ER retention signal (KDEL) at the 3⬘ end. The generation of replication-deficient recombinant adenoviruses was done essentially as described in ref. 31. The resulting recombinant adenoviruses were purified by CsCl banding, and final yields were between 4.5 ⫻ 1011 particles per ml and 1.3 ⫻ 1012 particles per ml. Effective Surface Depletion of VEGF-R2 and Tie-2 or VEGF-R2 with Intradiabodies. To determine the effect of the intradiabodies on the cell surface expression of VEGF-R2 and Tie-2, HUVEC and HMEC-1 cells were infected with adenovirus-encoding intradiabody with an moi of 50 and analyzed by flow cytometry on day 3 after infection. For HUVEC expressing the bispecific intradiabody, expression of VEGF-R2 was inhibited 98.6% and expression of Tie-2 was inhibited 91.2%. In HMEC-1, VEGF-R2 and Tie-2 expression were inhibited 92.1% and 92.5%, respectively (data not shown). When monospecific antibody to Fig. 2. Analysis of gene transfer of intradiabodies by recombinant adenovirus. HUVECs were infected with vectors for expression of anti-VEGF-R2兾Tie-2 intradiabody VR05–2S08 and anti-VEGF-R2 intradiabody VR05-VR05 and analyzed 3 days later. The flow cytometry histograms show the binding of anti-VEGF-R2 (bold line) and Tie-2 (dotted line) biotinylated polyclonal antibodies to HUVECs in intradiabody infected cells. Normal levels of VEGF-R2 and Tie-2 are shown on HUVECs (Left). Normal goat IgG was used as primary control antibody (thin line), and strepavidin-APC was used for detection. The y axis gives the number of events in linear scale; the x axis shows the fluorescence intensity in logarithmic scale. Jendreyko et al. PNAS 兩 June 7, 2005 兩 vol. 102 兩 no. 23 兩 8295 MEDICAL SCIENCES human xenotransplants, female athymic mice (nude兾nude) were used. Tumor induction was performed by s.c. injection of 2 ⫻ 106 human melanoma M21 cells into the right flanks of 18 nude mice on day 0. Tumors were allowed to establish for 12 days. On day 9, three groups of six mice were formed, and on day 12, each mouse received 4 ⫻ 108 pfu兾mouse (200 moi per initial tumor load) of adenovirus encoding one of the intradiabodies (VR05– 2S08b, VR05-VR05, or T2V2) administered peritumorally in PBS. Additional doses of 4 ⫻ 108 pfu per mouse were given on days 19 and 26. The resulting tumor was measured over the skin in two dimensions by using a slide caliper, and the tumor volume was calculated according to the following formula: volume ⫽ (longest axis) ⫻ (shortest axis)2 ⫻ 0.5. Toxicity was determined by determining the body weight of the mice once a week. All animals were killed after 30 days, and the tumors were completely dissected and weighed. Results are reported as mean weights ⫾ SD for each group. P values were determined by using a two-tailed t test assuming unequal variances. Differences were considered statistically significant at P ⬍ 0.05. Fig. 4. Cytotoxicity of adenovirus-delivered intradiabodies on M21 cells. M21 cells were seeded in 96-well plates and infected with different recombinant adenoviruses. Three days after infection, the extent of cell survival was determined by using a [3H]thymidine incorporation assay. In vitro proliferation of human melanoma cell line M21 was not inhibited by any intradiabody tested. erative effects of either the vector or the intradiabody format. As shown in Fig. 3, formation of capillaries in Matrigel was inhibited 63% (SD ⫾ 5) by the bispecific intradiabody (VEGF-R2兾Tie-2) and 27% (SD ⫾ 3) by the monospecific intradiabody (VEGFR2). Significantly, cells infected with the empty vector or the control intradiabody T2V2 were able to form capillaries to the same extent as uninfected cells. Effect of Intradiabodies on Cell Proliferation and Viability. To eval- Fig. 3. Inhibition of capillary tube formation in vitro. (A) HUVEC cells were infected with different recombinant adenoviruses for 3 days and then seeded in 96-well plates coated with Matrigel. After an incubation of 15.5 h, cells were stained and fixed. Uninfected cells (Upper Left) and cells infected with the control intradiabody T2V2 (Upper Right) formed capillary tubes. By contrast, cells infected with the intradiabody against VEGF-R2 (Lower Left) and with the intradiabody against VEGF-R2兾Tie-2 (Lower Right) were inhibited in their capability to form capillary tubes. (B) The number of tube branches in three independent wells per sample was counted, and averages are shown. The intradiabody against VEGF-R2兾Tie-2 inhibited capillary tube formation by 63 ⫾ 5%, whereas the intradiabody against VEGF-R2 inhibited formation by 27 ⫾ 3%. VEGF-R2 was expressed, the surface expression of human VEGF-R2 was inhibited 93.5% on HUVEC and 80% on HMEC-1 (Fig. 2). These results demonstrate the feasibility of expressing functional, bispecific or monospecific, and tetravalent antibodies intracellularly. Antiangiogenic Effect of Intradiabodies in Vitro. To test whether our intradiabody constructs could inhibit angiogenesis in vitro, we used a three-dimensional capillary tube formation assay. This in vitro assay has been used as a model of the early organization of new blood vessels and consistently recapitulates the process of angiogenesis in vivo. HUVEC were infected with each of the intradiabody-expression vectors at an moi of 20. Cells were transferred to the Matrigel-coated 96-well plate 3 days after infection to achieve maximum surface depletion of the targeted proteins. All cells were incubated in the presence of exogenous growth factors and serum (complete endothelial growth medium). Controls consisted of mock infected cells (empty vector) and a control intradiabody without specificity for any known target (T2V2). These controls were used to evaluate antiprolif8296 兩 www.pnas.org兾cgi兾doi兾10.1073兾pnas.0503168102 uate cytotoxicity related to intradiabody expression in the ER, HUVEC and M21 tumor cells were treated with different intradiabody constructs. Using mois ranging from 1 to 1,000, cells were infected with adenovirus encoding the ER-directed intradiabodies, and cell proliferation and survival were assessed through [3H]thymidine incorporation assay and trypan blue staining 3 days after infection. The [3H]thymidine incorporation assay used in HUVEC was described in ref. 17. As shown in Fig. 4, cell survival and proliferation of M21 cells infected with the therapeutic intradiabody were similar to cells infected with control intradiabody. M21 cell numbers analyzed by trypan blue staining and counting were reduced by 32% at an moi of 200 when compared with uninfected cells (data not shown). Thus, accumulation of the therapeutic intradiabody in the ER did not significantly affect cell viability relative to the control intradiabody and the antiangiogenic effects observed are not related to cytotoxic effects caused by ER stress. Antitumor and Antiangiogenic Activity of the Intradiabodies in Vivo. We next determined whether the blockade of two receptortyrosine kinases (VEGR-R2 and Tie-2) was more effective than inhibition of a single receptor (VEGF-R2) in the inhibition of tumor angiogenesis and tumor xenograft growth in vivo. Human melanoma M21 tumor cells were injected into nude mice, and tumors were allowed to grow until established. The mice were randomly divided into therapy and control groups. Three peritumoral injections of intradiabody-expression vectors were given on days 12, 19, and 26 after tumor cell inoculation. Beginning at day 15, a reduced tumor growth rate was observed in the M21 xenograft of nude mice treated with both VEGF-R2 and VEGFR2兾Tie-2 intradiabodies when compared with a control group of mice treated with T2V2 intradiabody (Fig. 5). On average, tumor growth was inhibited 92.2% (P ⬍ 0.01) by the bispecific VEGFR2兾Tie-2 intradiabody and 74.4% (P ⬍ 0.01) by the VEGF-R2 monospecific intradiabody when compared with the control Jendreyko et al. Fig. 5. Antitumor effect of the intradiabodies in vivo. Cultured M21 cells were inoculated s.c. into nude mice on day 0. After a palpable tumor was observed (day 9), the mice were divided randomly into three groups of six mice each. Adenovirus-encoding VR05–2S08b (anti-VEGF-R2兾Tie-2), VR05-VR05 (anti-VEGF-R2), or control intradiabody T2V2 was administered peritumorally once a week. (A) Results expressed as mean tumor volume ⫾ SD were calculated for each group at 3-day intervals from 9 to 30 days after grafting. (B) Tumor weight expressed as means ⫾ SD. intradiabody at day 30. Moreover, by day 30, a statistically significant difference in tumor growth inhibition could be observed between the group where both receptors were targeted and the group where VEGF-R2 alone was targeted (P ⬍ 0.01). Tumor weights were determined at killing in all mice on day 30 and confirmed the reduction in tumor growth during intradiabody treatment. These results indicate that blockade of the Tie-2 receptor can be used to enhance the effectiveness of VEGF-R2 inhibition of tumor growth. The effect of receptor down-regulation on tumor vascularization was also evaluated by determination of microvessel density. Cryostat-sectioned tumor slides were stained for murine CD31, and the number of discrete microvessels was compared in areas showing the highest vascularity of the tumor stroma (Fig. 6). Vascularization of tumors from animals treated with the bispecific VEGF-R2兾Tie-2 intradiabody was decreased more dramatically than was vacularization of tumors derived from the monospecific VEGF-R2 intradiabody treatment. In contrast, a striking induction of angiogenesis was observed in the control T2V2treated tumors, especially at the interface of tumor and mouse surrounding tissue (Fig. 6B). Discussion In the past decade, the use of scFv fragments as intrabodies has received considerable attention. Intrabodies have been used to Jendreyko et al. neutralize the function of endogenous target proteins by using several different strategies (24). Among these strategies, retention of cell surface receptors in the ER has been very successful. For example, intrabodies that retain one of the cell surface markers CD4, CCR5, ErbB-2, MHC I, or IL-2R␣ have demonstrated potency in cell-based studies as well as in human clinical trials. Significantly, these studies have addressed the targeting of a single protein. Given the biological redundancies common to both HIV-1 and cancer, the development of strategies that act to block multiple pathways is of prime importance (17). The VEGF兾VEGF-R2 complex and the Tie-2兾Ang2 complex are attractive targets for antiangiogenic agents from a therapeutic perspective. Two studies (8, 11) have demonstrated the inhibition of tumor growth by interference with the VEGF receptor pathway by means of soluble or dominant-negative receptor domains. Another report showed the inhibition of tumor growth by interference with the Tie-2 pathway by using similar approaches (13). Very recently we demonstrated that phenotypic knockdown of Tie-2 expression in mouse xenografts models impacts tumor vascularization and growth (15). The partial tumor growth inhibition we achieved by expression of an intrabody targeting the Tie-2 receptor indicated that blocking Tie-2 activation alone is not sufficient to completely halt tumor angiogenesis. It must be noted that the biological impact of receptor antagonism need not mirror the phenotype that results from receptor down-regulation of deletion. For example, antagonism of the integrin receptors ␣v3 and ␣v5 significantly impacts tumor growth and angiogenesis, whereas genetic knockout of these receptors has revealed that they are not essential for tumor growth and angiogenesis. PNAS 兩 June 7, 2005 兩 vol. 102 兩 no. 23 兩 8297 MEDICAL SCIENCES Fig. 6. Vascularization of transplanted tumors. (A) Tumor vascularization for one mouse from each treatment group. Shown are the tumor treated with control intradiabody T2V2 (Left), tumor treated with intradiabody against VEGF-R2 alone (VR05-VR05) (Center), and tumor treated with intradiabody against VEGF-R2兾Tie-2 (VR05–2S08b) (Right). (B) Cryostat sections of tumors grown from M21 xenographed mice were stained for the mouse endothelial marker CD31. Control T2V2-treated tumors developed a peritumorhypervasculature border zone (Upper Left) and luxuriant intratumor vasculature (Lower Left). In contrast, tumors treated with the intradiabody against VEGF-R2兾Tie-2 possessed a sparse vasculature (Lower Right) with markedly decreased vascularization in the border zone (Upper Right). Also shown are the peritumor border zone (Upper Center) and intratumoral vasculature (Lower Center) of mice treated with the intradiabody against VEGF-R2. Inhibition of cell surface expression of two independent mediators of angiogenesis, VEGF-R2 and Tie-2, should present advantages over targeting a single pathway. In a previous study, we developed a strategy to enable the targeting of two cell surface receptors and demonstrated that an ER-targeted intradiabody against VEGF-R2 and Tie-2 resulted in additive antiangiogenic effects in vitro (17). Qian et al. (32) reported recently that the combination of the histone deacetylase inhibitor NVP-LAQ824 and the VEGF receptor tyrosine kinase inhibitor PTK787兾ZK222584 was more effective than the single agents in inhibiting VEGFinduced angiogenesis in vitro and in vivo. NVP-LAQ824 inhibits the expression of angiogenesis-related genes such as angiopoietin-2, Tie-2, and survivin in endothelial cells and down-regulates hypoxiainducible factor 1-␣ and VEGF expression in tumor cells. In this study, we investigated whether an antitumor therapy directed specifically toward VEGF-R2 and Tie-2 was more efficient than targeting VEGF-R2 alone in vivo. Treatment with the adenovirus-delivered anti-mouse VEGF-R2兾Tie-2 intradiabody (VR05–2S08b) resulted in a 92.2% reduction in M21 melanoma growth in a nude mouse model, whereas tumors treated with the anti-mouse VEGF-R2 intradiabody (VR05-VR05) showed a reduction of only 74.4% over a period of 30 days. Thus, the specific and simultaneous blockade of the VEGF receptor pathway and the Tie-2 pathway resulted in more effective tumor growth and angiogenesis inhibition than blockade of the VEGF receptor pathway alone. In our recent study (15) with Tie-2 intrabodies, we demonstrated tumor growth inhibition of 75% in human Kaposi’s sarcoma (SLK) and 63% in human colon carcinoma (SW1222). Although the results in different cell types cannot be directly compared, they underscore the need for therapeutic strategies that act to block multiple pathways simultaneously. The inhibition of tumor growth was likely secondary to a blockade of tumor angiogenesis. This notion is supported by the decreased vascular density in the intradiabody-treated tumors, by the ability of those intradiabodies to recognize mouse VEGF-R2 and Tie2, and by the absence of significant cytotoxicity of therapeutic intradiabodies for cultured tumor cells at an moi of 200 used for in vivo tumor treatment. In histological staining, we observed a strong CD31 expression at the tumor boundary in regions of extensive tumor neovascularization (Fig. 6). These findings are consistent with a capillary sprouting from surrounding mouse normal tissues, tumor vessel elongation, and兾or formation of connections between tumor vessels and host vessels. CD31 expression was markedly inhibited in the VEGF-R2兾Tie-2 treatment groups and, to a lesser extent, in the VEGF-R2 treatment group when compared with the control T2V2-treated group. These results indicate that both the VEGF receptor pathway and the Tie-2 pathway are essential for the vascularization and tumor growth of M21 xenografts. This conclusion is in agreement with results of gene knockout experiments that revealed indispensable but distinct functions of the VEGF receptor Flk-1兾KDR and Tie-2 (33, 34). Flk-1兾KDR knockout mice lacked endothelial cells indicating that VEGF signaling through Flk-1兾KDR was essential for differentiation and survival of endothelial cells. In Tie-2-deficient mice, endothelial cells lacked the support of underlying periendothelial mesenchymal cells, resulting in collapse of the endothelial cells into the lumen of vessels that were preformed by tissue fold and vessel occlusion (35), implicating Tie-2 in vessel maturation and maintenance. Our study demonstrates the use of an ER-targeted, tetravalent intradiabody to inhibit expression of two endothelial surface receptors simultaneously in vivo. Although a major application for intrabodies might be in functional genomics, our results offer support for therapeutic application of intrabodies. The specific and simultaneous blockade of two independent angiogenic pathways, VEGF-R2 and Tie-2, was more effective than targeting a single angiogenic pathway, VEGF-R2. The greater in vivo antitumor effect of the combination therapy is the result of simultaneous targeting of independent pathways, supporting an argument for development of antiangiogenic drugs that interfere with both VEGF and Tie-2 pathways for the treatment of cancer. 1. Ferrara, N. & Alitalo, K. (1999) Nat. Med. 5, 1359–1364. 2. Hanahan, D. & Folkman, J. (1996) Cell 86, 353–364. 3. Yancopoulos, G. D., Davis, S., Gale, N. W., Rudge, J. S., Wiegand, S. J. & Holash, J. (2000) Nature 407, 242–248. 4. Ferrara, N. (2002) Nat. Rev. Cancer 2, 795–803. 5. Holash, J., Wiegand, S. J. & Yancopoulos, G. D. (1999) Oncogene 18, 5356–5362. 6. Thurston, G., Rudge, J. S., Ioffe, E., Zhou, H., Ross, L., Croll, S. D., Glazer, N., Holash, J., McDonald, D. M. & Yancopoulos, G. D. (2000) Nat. Med. 6, 460–463. 7. Holash, J., Maisonpierre, P. C., Compton, D., Boland, P., Alexander, C. R., Zagzag, D., Yancopoulos, G. D. & Wiegand, S. J. (1999) Science 284, 1994–1998. 8. Millauer, B., Shawver, L. K., Plate, K. H., Risau, W. & Ullrich, A. (1994) Nature 367, 576–579. 9. Kim, K. J., Li, B., Winer, J., Armanini, M., Gillett, N., Phillips, H. S. & Ferrara, N. (1993) Nature 362, 841–844. 10. Hurwitz, H., Fehrenbacher, L., Novotny, W., Cartwright, T., Hainsworth, J., Heim, W., Berlin, J., Baron, A., Griffing, S., Holmgren, E., et al. (2004) N. Engl. J. Med. 350, 2335–2342. 11. Goldman, C. K., Kendall, R. L., Cabrera, G., Soroceanu, L., Heike, Y., Gillespie, G. Y., Siegal, G. P., Mao, X., Bett, A. J., Huckle, W. R., et al. (1998) Proc. Natl. Acad. Sci. USA 95, 8795–8800. 12. Holash, J., Davis, S., Papadopoulos, N., Croll, S. D., Ho, L., Russell, M., Boland, P., Leidich, R., Hylton, D., Burova, E., et al. (2002) Proc. Natl. Acad. Sci. USA 99, 11393–11398. 13. Lin, P., Polverini, P., Dewhirst, M., Shan, S., Rao, P. S. & Peters, K. (1997) J. Clin. Invest. 100, 2072–2078. 14. Siemeister, G., Schirner, M., Weindel, K., Reusch, P., Menrad, A., Marme, D. & Martiny-Baron, G. (1999) Cancer Res. 59, 3185–3191. 15. Popkov, M., Jendreyko, N., McGavern, D. B., Rader, C. & Barbas, C. F., III (2005) Cancer Res. 65, 972–981. 16. Niu, Q., Perruzzi, C., Voskas, D., Lawler, J., Dumont, D. J. & Benjamin, L. E. (2004) Cancer Biol. Ther. 3, 402–405. 17. Jendreyko, N., Popkov, M., Beerli, R. R., Chung, J., McGavern, D. B., Rader, C. & Barbas, C. F., III (2003) J. Biol. Chem. 278, 47812–47819. 18. Marasco, W. A., Haseltine, W. A. & Chen, S. Y. (1993) Proc. Natl. Acad. Sci. USA 90, 7889–7893. 19. Beerli, R. R., Wels, W. & Hynes, N. E. (1994) J. Biol. Chem. 269, 23931–23936. 20. Deshane, J., Siegal, G. P., Alvarez, R. D., Wang, M. H., Feng, M., Cabrera, G., Liu, T., Kay, M. & Curiel, D. T. (1995) J. Clin. Invest. 96, 2980–2989. 21. Kramer, R. & Cohen, D. (2004) Nat. Rev. Drug Discov. 3, 965–972. 22. Beerli, R. R. & Barbas, C. F., III (2002) Nat. Biotechnol. 20, 135–141. 23. Tian, B., Bevilacqua, P. C., Diegelman-Parente, A. & Mathews, M. B. (2004) Nat. Rev. Mol. Cell Biol. 5, 1013–1023. 24. Marasco, W. A. (1997) Gene Ther. 4, 11–15. 25. Ades, E. W., Candal, F. J., Swerlick, R. A., George, V. G., Summers, S., Bosse, D. C. & Lawley, T. J. (1992) J. Invest. Dermatol. 99, 683–690. 26. Popkov, M., Mage, R. G., Alexander, C. B., Thundivalappil, S., Barbas, C. F., III & Rader, C. (2003) J. Mol. Biol. 325, 325–335. 27. Popkov, M., Jendreyko, N., Gonzalez-Sapienza, G., Mage, R. G., Rader, C. & Barbas, C. F., III (2004) J. Immunol. Methods 288, 149–164. 28. Steinberger, P., Andris-Widhopf, J., Buhler, B., Torbett, B. E. & Barbas, C. F., III (2000) Proc. Natl. Acad. Sci. USA 97, 805–810. 29. Barbas, C. F., III, Burton, D. R., Scott, J. K. & Silverman,G. J. (2001) Phage Display: A Laboratory Manual (Cold Spring Harbor Lab. Press, Plainview, NY). 30. Rader, C., Ritter, G., Nathan, S., Elia, M., Gout, I., Jungbluth, A. A., Cohen, L. S., Welt, S., Old, L. J. & Barbas, C. F., III (2000) J. Biol. Chem. 275, 13668–13676. 31. He, T.-C., Zhou, S., da Costa, L. T., Yu, J., Kinzler, K. W. & Vogelstein, B. (1998) Proc. Natl. Acad. Sci. USA 95, 2509–2514. 32. Qian, D. Z., Wang, X., Kachhap, S. K., Kato, Y., Wei, Y., Zhang, L., Atadja, P. & Pili, R. (2004) Cancer Res. 64, 6626–6634. 33. Dumont, D. J., Gradwohl, G., Fong, G. H., Puri, M. C., Gertsenstein, M., Auerbach, A. & Breitman, M. L. (1994) Genes Dev. 8, 1897–1909. 34. Shalaby, F., Rossant, J., Yamaguchi, T. P., Gertsenstein, M., Wu, X. F., Breitman, M. L. & Schuh, A. C. (1995) Nature 376, 62–66. 35. Patan, S. (1998) Microvasc. Res. 56, 1–21. 8298 兩 www.pnas.org兾cgi兾doi兾10.1073兾pnas.0503168102 This work was supported by National Institutes of Health Grant CA 86258. N.J. was supported in part by a Deutsche Forschungsgemeinschaft postdoctoral fellowship. Jendreyko et al.