W O R K I N G Quality Indicators for
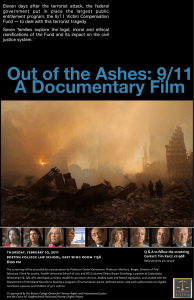
advertisement

WORKING P A P E R Quality Indicators for Preventive Care of the Vulnerable Elder DAVID C. RHEW PAUL G. SHEKELLE WR-178 August 2004 This product is part of the RAND Health working paper series. RAND working papers are intended to share researchers’ latest findings and to solicit informal peer review. They have been approved for circulation by RAND Health but have not been formally edited or peer reviewed. Unless otherwise indicated, working papers can be quoted and cited without permission of the author, provided the source is clearly referred to as a working paper. RAND’s publications do not necessarily reflect the opinions of its research clients and sponsors. is a registered trademark. QUALITY INDICATORS FOR PREVENTIVE CARE OF THE VULNERABLE ELDER David C. Rhew, MD Paul G. Shekelle, MD, PhD From the Greater Los Angeles VA Health Care System, Los Angeles, CA (D.C.R, P.G.S.); Zynx Health Incorporated, a subsidiary of Cedars-Sinai Health System, Beverly Hills, CA (D.C.R); RAND Health Sciences Program, Santa Monica, California (P.G.S.) This study was supported by a contract from Pfizer Inc to RAND. Corresponding author is Dr. Rhew at Greater Los Angeles VA Healthcare System, West Los Angeles VAMC, Division of Infectious Diseases 11301 Wilshire Blvd, #111F Los Angeles, CA 90073 (310) 268-3015 Word Count: 4,194 FAX: (310) 268-4928 e-mail: rhew@zynx.com INTRODUCTION It has been estimated that by the year 2030, there will be 70 million persons aged 65 or older living in the US, and that elders will represent 20% of the US population.(1) As the population continues to grow, conditions that commonly afflict elders will impact a larger number of people. Cancer is the leading cause of death among women age 60 to 79, and it is the second leading cause of death among men age 60 and older and among women age 80 and older.(2) Breast cancer is the second most common cause of death due to cancer for women age 60 to 79 and the third most common in women age 80 and older.(2) Incidence and survival rates from the Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute and breast cancer mortality data from the National Center for Health Statistics (NCHS) demonstrate that the age group continuing to experience an increase in breast cancer-specific mortality and for whom breast cancer-specific mortality rates are the highest are the 80 and 85+ years old age groups, respectively.(3) Colon cancer is the second most common cause of death due to cancer in women age 80 and older and the third most common cause in women age 60 to 79. It is also the third most common cause of death due to cancer in men age 60 and older.(2) Health-related issues such as excessive alcohol consumption, tobacco use, and lack of exercise are also common problems in the elderly. They are associated with significant morbidity and mortality and are potentially preventable. Four to 10% of elderly patients who present to their primary care physician are alcoholics(4-6), and one study in 1989 from the Health Care Financing Administration identified 87,147 hospitalizations related to alcohol consumption in elderly Medicare beneficiaries.(7) The hospitalization rate for alcohol-related 2 diagnoses in that year was similar to that for patients with myocardial infarction.(7) Data from the Third National Health and Nutrition Examination Survey (NHANES III) indicate that 10 to 20% of adults aged 65 to 84 years of age smoke(8), and more than 70% of all deaths attributable to smoking occur in adults aged 65 or older.(9) NHANES III data also indicate that 17 to 48% of persons aged 65 to 84 years of age live a sedentary lifestyle (ie, do not participate in leisure-time physical activity).(8) Lack of exercise is associated with increased risk of developing cancer, cardiovascular disease, and death.(10) Early detection and prevention of medical illness may reduce morbidity and mortality in the elderly population,(11) especially among those at greatest risk for developing and dying from disease. Thus, implementation of preventive care measures represents a potential opportunity to improve longevity and quality of life for vulnerable elders. In addition, screening for vulnerable elders focuses on identifying sources of potential and current dysfunction in order to initiate actions to improve function or delay or decrease disabilities. This paper evaluates the evidence concerning cancer screening and other preventive health measures for vulnerable elders, including comprehensive geriatric assessment, screening for problem drinking, and counseling about smoking cessation and exercise. METHODS The methods for developing these quality indicators, including literature review and expert panel consideration, are detailed in a preceding paper.(12) For preventive services, the structured literature review identified 7,885 titles, from which abstracts and articles were 3 identified that were relevant to this report. Based on the literature and the authors’ expertise, 15 potential quality indicators were proposed. RESULTS Of the 15 potential quality indicators, 8 were judged valid by the expert panel process (see ACOVE Quality Indicators) and 7 were not accepted. The literature summaries that support each of the indicators judged to be valid by the expert panel process are described below. Quality Indicator #1 Geriatric evaluation ALL vulnerable elders newly admitted to a physician practice should receive within six months the elements of a comprehensive geriatric assessment, BECAUSE such an assessment, combined with treatment of the identified conditions, improves outcomes. Supporting evidence: Comprehensive geriatric assessment (CGA) is defined as a multidimensional evaluation, in which problems are uncovered, described and explained, if possible, and in which the resources and strengths of the patient are catalogued, need for services identified, and a coordinated care plan developed to focus interventions on the patient’s problems.(13) It is particularly valuable when targeted to vulnerable or frail older people who have multiple health problems and are at high risk for functional decline or death. The medical elements of a CGA include special attention to cognition, physical function, affect, visual impairment, hearing impairment, malnutrition, incontinence and disorders of 4 balance and mobility. In addition, the practitioner or interdisciplinary team evaluates the psychological, social, economic and environmental status of the individual. Function is assessed at three levels, basic ADLs, IADLs (intermediate or “instrumental”) and advanced ADLs, by asking the patient or caregiver about the patient’s ability to perform the various activities. Questions should be appropriate to the condition of the patient. For example, if the patient is unable to walk, many of the IADLs and all of the advanced ADLs would become irrelevant and the focus would be on the basic ADLs. Several validated screening instruments may be used. The patient’s preferences for care are documented and advance directives discussed. Although a CGA may be carried out by an individual practitioner, it typically involves multiple health professionals working together. Participants regularly include a nurse or nurse practitioner, a social worker and a physician. Often a psychologist, pharmacist, occupational therapist, physical therapist or dietician contributes to the process. A 1993 meta-analysis identified 28 controlled clinical trials of Comprehensive Geriatric Assessment (CGA) programs, which are defined as programs that provide a comprehensive assessment of medications, functional status, cognition, affect, gait/balance, nutrition, social support system, and special senses, with referral for appropriate services and verification of treatment and follow-up services as needed.(14) Programs were classified as hospital-based geriatric evaluation and management units (GEM), inpatient geriatric consultation services (IGCS), home assessment services (HAS), hospital home assessment services (HHAS), or outpatient assessment services (OAS). Nearly 10,000 patients were studied among the 28 trials. Summary odds ratios for mortality were statistically significant for the following types of programs: GEM at six-month follow-up (OR = 0.65, 95% C.I. = 0.46 to 0.91) 5 IGCS at six-month follow-up (OR = 0.77, 95% C.I. = 0.62 to 0.96) HAS at 36-month follow-up (OR = 0.86, 95% C.I. = 0.75 to 0.99) Other time points and categories of programs had summary odds ratios for mortality favoring the intervention that did not reach conventional levels of statistical significance.(5) Similar effects, not all reaching statistical significance, were reported for the outcomes of living at home and for physical or cognitive function at six, 12, or 36 months. A meta-regression analysis indicated that direct medical control over implementation of the recommendations was associated with improvements in mortality and living situation. Since the publication of this meta-analysis at least 23 reports of clinical trials of CGA have been published.(15-37) Nine deserve comment here. Six randomized studies extended the findings of beneficial effects for hospital-based CGA to the outpatient setting. In all six reports, the patients studied were frail or vulnerable elders. The interventions included an in-home assessment by physician assistants, nurses,(15) or gerontologic nurses,(16) an outpatient GEM clinic,(17,18) a senior center-based, chronic illness self-management and disability prevention program,(19) and CGA delivered at a community-based clinic.(20) The follow-up time in the studies ranged from eight months to three years, with most studies reporting one-year outcomes. All studies reported better outcomes among patients randomized to receive CGA. Not all improvements in outcomes reached statistical significance. Typical results included the following: Improvements in the number of persons living outside of nursing homes (4% versus 10%, in one study)(16) Improvements in physical functioning (about five points difference between groups on the Medical Outcomes Study Short Form 36 PF-10 scale in one study)(20) 6 Improvements in affect and mood (eight-point difference between groups on the Center for Epidemiologic Studies Depression test score)(17) Another study found that the beneficial effects of a hospital-based CGA extended to three years after the intervention, with the proportion of persons independent in two or more activities of daily living greater among persons who received CGA (44%) than among controls (33%, p = 0.056).(21) There was also a statistically significant survival advantage relative to controls at two years of follow-up for persons who received CGA.(21) Two studies that reported no or limited benefit of CGA are worth noting here. The first study reported no effect on health or one-year survival of a in-hospital CGA consultation with limited follow-up.(22) This CGA program was targeted at persons with functional impairments, geriatric syndromes, certain medical conditions, and at those age 80 or older. The second study reported no effect on survival, hospital readmission, or nursing home placement at 60-day follow-up from a CGA begun in hospital and completed at home.(23) Many of the studies described above evaluated a hospital-based CGA program and most of the others investigated multidisciplinary outpatient CGA evaluations. The expert panel believed that requiring a multidisciplinary CGA was beyond the scope of available resources in many areas of the country. However, they maintained that the elements of the CGA evaluation were critical for the initial evaluation of any vulnerable elder in order to improve and preserve health and function. Recognizing that the CGA can be a time expensive procedure, the panel suggested that the elements of the CGA might be spread out over several clinic visits, allowing a 6-month period for their completion. From a practical perspective, many elements of a CGA can be accomplished in the course of a usual adult initial examination. If functional level is high (for example the patient is the president of the bridge club or plays tennis biweekly, indicating intact 7 social and physical function, respectively), then no additional testing and only minimal documentation would be needed. On the other hand, for subclinical abnormalities or to evaluate the extent of dysfunction, more complete evaluation of each of the components of the CGA would be needed. Quality Indicator #2 Follow-up of geriatric evaluation IF the elements of a comprehensive geriatric assessment (CGA) are performed, THEN followup should assure the implementation of recommendations, BECAUSE this is likely to increase the effectiveness of Comprehensive Geriatric Assessment in improving outcomes. Supporting evidence: Several lines of indirect evidence support a relationship between CGA efficacy and follow-up to assure implementation of the recommendations. First, programs that engage in follow-up to assure implementation of the recommendations have a theoretical advantage over programs that perform no such follow-up. Second, covariate analysis in the meta-analysis reported above demonstrated that medical control over implementation of the assessment recommendations was associated with improved effectiveness of CGA.(14) Medical control over implementation assures that the recommendations are indeed implemented (another alternative would be close follow-up between the CGA team and the primary care provider). Finally, lack of assurance of CGA recommendation implementation has been postulated to explain its lack of effectiveness in several trials that demonstrated minimal or no effect.(24-26) From a practical perspective, the expert panel reasoned that primary care providers should be capable of identifying and cataloging deficits in the elements of the CGA exam. While not 8 expected to be capable of treating each of the detected abnormalities, this provider would be responsible for issuing appropriate referrals and ensuring follow-up in a continuity relationship so that the patient’s function is preserved. Quality Indicator #3 Problem drinking- screening ALL vulnerable elders should be screened to detect problem drinking and hazardous drinking with a history of alcohol use using standardized screening questionnaires (e.g., CAGE, AUDIT) at least once, BECAUSE problem drinking is common in the elderly population, is responsible for a high frequency of alcohol-related hospitalizations in the United States, and can be identified by screening tests. Furthermore, brief physician advice can decrease alcohol use in older patients. Supporting evidence: We identified 7 prospective studies that used either a “goldstandard” reference standard or a controlled study design to screen for problem drinking in elders.(4,38-43) Five studies demonstrated that the AUDIT, CAGE, MAST, MAST-G, or UMAST questionnaires may be helpful in discriminating problem drinkers in the elderly population.(4,38-41) However, two studies(42,43) (plus an additional cross-sectional study(5)), showed that the CAGE, and MAST questionnaires had poor sensitivity for detecting problem drinking. A meta-analysis of studies evaluating alcohol screening tools for women demonstrated that the CAGE questionnaire was insensitive for detecting heavy drinking among Caucasian females, while the TWEAK and AUDIT questionnaires were adequate for African American or Caucasian women.(44) In addition, a review article of alcohol screening tools used in the elderly population concluded that the CAGE and MAST are the two most commonly used screening 9 tools and that the focus of screening tools should be expanded to include even lower levels of alcohol consumption.(45) An expert-opinion based recommendation by the U.S. Preventive Services Task Force stated that the AUDIT and CAGE questionnaires were appropriate screening tools for problem drinking.(46) Since the development of this indicator, a systematic review has demonstrated that the AUDIT and CAGE are the most effective screening tools. AUDIT is most effective in screening primary care patients for at-risk, hazardous, or harmful drinking, while CAGE is most effective in screening for alcohol abuse and dependency.(47) Also, a randomized controlled trial (Project GOAL- Guiding Older Adult Lifestyles) has demonstrated that brief physician advice consisting of two 10- to 15-minute counseling sessions can decrease alcohol use in patients aged 65 and older.(48) The beneficial effects of the intervention were maintained for the duration of the 12-month follow-up period. Quality Indicator #4 Tobacco screening ALL vulnerable elders should receive screening for tobacco use and nicotine dependence, BECAUSE implementing screening systems to identify smokers increases the rate of clinician intervention. Supporting evidence: One meta-analysis performed by the Agency for Healthcare Research and Quality (AHRQ) (previously known as the Agency for Healthcare Policy and Research (AHCPR)) reviewed the efficacy of screening for tobacco use. This study was originally published as part of an evidence-based clinical practice guideline in 1996(49), and was then updated in 2000(50) at which time no additional studies pertaining to screening for tobacco 10 use were identified and included. In this meta-analysis, pooled data from nine randomized controlled trials (RCTs) demonstrated that implementation of screening procedures to identify smokers increased the rate of clinician intervention (odds ratio [OR] = 3.1, 95% C.I. = 2.2 to 4.2). Data from three RCTs indicated that implementation of screening to identify smokers increased the rate of smoking cessation among those identified, but not significantly (OR = 2.0, 95% C.I. = 0.8 to 4.8). Furthermore, a recently published evidence-based consensus statement recommends that healthcare systems and clinicians should implement screening methods to identify, document, and treat all tobacco users at every visit.(51) Quality Indicator #5 Tobacco counseling and therapy IF a vulnerable elder uses tobacco regularly, THEN he or she should be offered counseling and/or pharmacologic therapy to stop tobacco use at least once, BECAUSE data from metaanalyses of randomized controlled trials, cost-analyses, and expert recommendations indicate that smoking cessation interventions are effective, may result in cost savings, and should be implemented for all smokers. Furthermore, observational data suggest that smoking cessation improves survival even among persons who stop smoking after age 70. Supporting evidence: Meta-analyses and systematic reviews have reviewed the effectiveness of various methods for smoking cessation.(49,50,52,53) One meta-analysis, performed in 1996 and updated without need for changes in 2000, by the AHRQ(49,50) demonstrated the following: 11 • Clinician advice to stop smoking increased the rate of smoking cessation (OR = 1.3, 95% C.I. = 1.1 to 1.6) (based on 7 RCTs). • Self-help (OR = 1.2, 95% C.I. = 1.0 to 1.6), individual counseling (OR = 2.2, 95% C.I. = 1.9 to 2.4), and group counseling (OR = 2.2, 95% C.I. = 1.6 to 3.0) were effective smoking cessation interventions (based on 25 RCTs). • Three- to ten-minute counseling sessions increased the rate of smoking cessation (OR = 1.4, 95% C.I. = 1.2 to 1.7), and counseling more than ten minutes was more effective than counseling ten minutes or less (OR = 2.4, 95% C.I. = 2.1 to 2.7), while counseling three minutes or less was least effective (OR = 1.2, 95% C.I. = 1.0 to 1.5) (based on 56 RCTs). • Interventions of two to less than four weeks’ duration were associated with an odds ratio for smoking cessation of 1.6 (95% C.I. = 1.3 to 2.0); interventions from four to eight weeks’ duration were associated with an odds ratio of smoking cessation of 1.6 (95% C.I. = 1.2 to 2.1); and interventions of more than eight weeks’ duration were associated with an odds ratio of smoking cessation of 2.7 (95% C.I. = 2.2 to 3.2) (based on 55 RCTs). • A total of two to three person-to-person contacts was associated with an odds ratio of smoking cessation of 2.0 (95% C.I. = 1.6 to 2.4), four to seven interventions were associated with an odds ratio of smoking cessation of 2.5 (95% C.I. = 2.2 to 2.9), and more than seven interventions were associated with an odds ratio of smoking cessation of 1.7 (95% C.I. = 1.2 to 2.5) (based on 55 RCTs). Another meta-analysis published in 1988 evaluated 108 smoking cessation interventions in 39 controlled trials and demonstrated that counseling, providing literature, and providing nicotine replacement resulted in a 6% higher rate of smoking cessation relative to controls.(53) A recently 12 published (2000) systematic review of 31 randomized trials demonstrated that brief physician advice for smoking cessation was effective for at least 6 months (absolute risk reduction 2.5%; odds ratio 1.69, 95% CI, 1.45 to 1.98).(52) Economic analyses demonstrated that implementing the 1996 AHRQ smoking cessation guidelines(54) and offering brief advice to stop smoking during routine office visits(55) were cost-effective measures. Evidence-based recommendations have stated that smoking cessation counseling should be provided to all smokers,(51,56,57) and the Department of Health and Human Services report of the Surgeon General concluded that, based on evidence from several prospective cohort and case-control studies, smoking cessation could significantly reduce morbidity and mortality, even among persons who stopped smoking after age 70.(58) Quality Indicator # 6 Physical activity- assessment and counseling ALL vulnerable elders should receive an assessment of their activity level and be provided with counseling to promote regular physical activity at least once, BECAUSE evidence exists that physical activity and fitness reduce overall morbidity and mortality. Supporting evidence: A meta-analysis,(59) three prospective observational studies,(6062) two retrospective studies,(63,64) and a review of the literature(65) demonstrated that physical activity decreases the risk of death among persons of all ages. Furthermore, several other studies showed that physical activity improves mental health, decreases bone loss, reduces the incidence for coronary heart disease, lowers blood pressure, reduces weight, and decreases the incidence of diabetes mellitus among elderly individuals.(66-73) Finally, an evidence-based 13 recommendation by the U.S. Preventive Services Task Force (USPSTF)(74) and a position statement by the American College of Sports Medicine (ASCM)(75) were identified that supported the policy of promoting exercise in elderly persons. Quality Indicator # 7 Colorectal cancer screening ALL vulnerable elders should be offered screening for colorectal cancer at least once with fecal occult blood testing (FOBT) or should have had sigmoidoscopy in the last 5 years or colonoscopy in the last 10 years, BECAUSE screening with these methods has been shown to decrease mortality. Supporting evidence: Randomized controlled trials of patients up to age 80 years have found that using multiphase screening for colorectal cancer with the FOBT as the first stage of screening resulted in a small but significant benefit for preventing cancer deaths.(76-79) A costeffectiveness analysis demonstrated that annual FOBT was the most cost-effective strategy for screening for colorectal cancer in elderly patients.(80) A case-control study demonstrated that patients who received sigmoidoscopy as a screening procedure experienced a survival benefit.(81) However, the effectiveness of screening flexible sigmoidoscopy has not yet been evaluated with randomized controlled trials. Two major organizations (the Canadian Task Force on the Periodic Health Examination [CTFPHE](82) and the U.S. Preventive Services Task Force [USPSTF])(83) performed evidence-based reviews of the literature (in 1994 and 1996, respectively) and came to different conclusions on this issue. The CTFPHE concluded that evidence was insufficient to include or exclude either multiphase screening with FOBT or 14 sigmoidoscopy from the Periodic Health Examination, while the USPSTF supported the use of either FOBT or sigmoidoscopy as a colon cancer screening tool for persons older than age 50. The age at which screening should be discontinued had not been established. Since the development of these indicators, new data support the belief that colonoscopy is significantly better than is sigmoidoscopy at detecting asymptomatic colon cancer.(84,85) However, colonoscopy is substantially more expensive and has greater morbidity associated with the procedure. Since the development of these indicators, Sonnenberg and colleagues have published a cost-analysis study using a hypothetical population and a computer model that demonstrated that screening for colorectal cancer with colonoscopy every 10 years starting at age 50 is a more cost-effective strategy than annual fecal occult blood testing or sigmoidoscopy every 10 years.(86) Nevertheless, it still remains to be determined which screening strategy is most cost-effective for persons age 65 and older. Future studies are necessary before colonoscopy can be considered the standard for colorectal screening in vulnerable elders. Quality Indicator #8 Breast cancer screening IF a vulnerable elderly woman is less than age 70, THEN she should be offered mammographic screening for breast cancer every 2 years, BECAUSE use of mammography decreases breast cancer mortality. Supporting evidence: Three meta-analyses reported a statistically significant reduction in risk of death from breast cancer among women up to age 70 to 74 who received screening mammography (relative risk [RR] = 0.70, 0.71, 0.74).(87-89) However, two randomized 15 controlled trials of screening mammography(90,91) reported statistically significant reductions in the risk of death due to breast cancer in women under age 70, but not in women age 70 or older, while two case-control studies provided inconclusive evidence as to whether mammography reduced breast cancer mortality among women age 65 and older.(92,93) An economic analysis indicated that offering screening to women over the age of 70 decreased its cost-effectiveness.(94) Finally, a retrospective analysis demonstrated that women age 65 to 74 benefited from screening mammography,(95) and an evidence-based review of the literature by the U.S. Preventive Services Task Force (USPSTF) recommended the use of screening mammography for women age 50 to 69.(96) Since the development of these indicators, Gotsche and Olsen identified in a meta-analysis that only two of eight RCTs (i.e., Malmo(91) and Canada(97)) were adequately randomized and pooled results from these two trials showed that screening with mammography had no effect on breast cancer mortality or total mortality.(98) However, one of the two studies(91) found that screening mammography reduced the risk of death due to breast cancer in women under age 70. Additionally, a recently published retrospective cohort study using population data from the SEER program demonstrated that women aged 67 and older who did not receive mammography were more likely to be diagnosed with breast cancer stage II or greater and also more likely to die from breast cancer than women of the same age range who were regular users of mammography.(99) DISCUSSION Screening and prevention in vulnerable elders includes more than the traditional measures thought of for the general population, such as cigarette smoking and cancer screening. Screening and prevention in vulnerable elders includes an evaluation for the presence of geriatric 16 syndromes such as urinary incontinence, diminished hearing and vision, and early cognitive impairment. These conditions are currently under-identified, and some treatments may reverse or at least ameliorate the progression of decline.Some screening and prevention measures, such as stopping cigarette use, stopping alcohol abuse, and increasing physical activity, render immediate benefits and age or other medical conditions in general should not preclude advocating their use. The decision to perform cancer screening, however, hinges on the life expectancy for the individual patient and the time needed for screening to achieve benefits. At least 5 years is needed in order for a group of average patients to accrue benefit from cancer screening. The average life expectancy for a 75 year old person is about 10 years.(100) Clearly, there is variability in life expectancy and patients with existing medical problems that significantly reduce their life expectancy are not good candidates for cancer screening. Some explicit definitions of such conditions are presented in the overview paper.(101) Providers will need to consider life expectancy, competing morbidities, and patient preferences, when considering recommending cancer screening for vulnerable elders. Additional measures related to screening not presented here appear either in the relevant condition-specific ACOVE papers (pneumonia, hearing, osteoporosis, etc.) or were considered here and not accepted, such as the use of PSA screening for prostate cancer, because of insufficient evidence and opinion supporting their use with improvements in patient outcomes. In summary, we identified eight indicators addressing the following topics: comprehensive geriatric assessment (2), problem drinking (1), tobacco use (2), physical activity (1), and screening for colorectal cancer (1) and breast cancer (1). These indicators can potentially 17 serve as a basis to compare the care provided by different health care delivery systems and for comparing the change in care over time. 18 ACKNOWLEDGEMENTS The authors thank Scott E. Sherman, M.D. for his review of an earlier version of the monograph containing the full set of proposed quality indicators and Patricia Smith for technical assistance. 19 REFERENCES (1) US Department of Health and Human Services. A Profile of Older Americans. Washington DC: American Association of Retired Persons and Administration on Aging; 1994. (2) American Cancer Society. CA: A Cancer Journal for Clinicians. Cancer Stat. 2001; 51:16-66. (3) Chu KC, Tarone RE, Kessler LG, Ries LA, Hankey BF, Miller BA, et al. Recent trends in U.S. breast cancer incidence, survival, and mortality rates. J Natl Cancer Inst. 1996;88:1571-79. (4) Buchsbaum DG, Buchanan RG, Welsh J, Centor RM, Schnoll SH. Screening for drinking disorders in the elderly using the CAGE questionnaire. J Am Geriatr Soc. 1992;40:662-65. (5) Jones TV, Lindsey BA, Yount P, Soltys R, Farani-Enayat B. Alcoholism screening questionnaires: are they valid in elderly medical outpatients? J Gen Intern Med. 1993;8:674-78. (6) Magruder-Habib K, Saltz CC, Barron PM. Age-related patterns of alcoholism among veterans in ambulatory care. Hosp Community Psychiatry. 1986;37:1251-55. (7) Adams WL, Yuan Z, Barboriak JJ, Rimm AA. Alcohol-related hospitalizations of elderly people. Prevalence and geographic variation in the United States. JAMA. 1993;270:1222-25. 20 (8) Sundquist J, Winkleby MA, Pudaric S. Cardiovascular disease risk factors among older black, Mexican-American, and white women and men: an analysis of NHANES III, 1988-1994. Third National Health and Nutrition Examination Survey. J Am Geriatr Soc. 2001;49:109-16. (9) US Department of Health and Human Services. SAMMEC 3.0 . Smoking-attributable mortality, morbidity, and economic costs. Rockville, MD: Centers for Disease Control and Prevention, Office on Smoking and Health; 1996. (10) Burke GL, Arnold AM, Bild DE, Cushman M, Fried LP, Newman A, et al. Factors associated with healthy aging: the cardiovascular health study. J Am Geriatr Soc. 2001;49:254-62. (11) Walsh JM. Cancer screening in older adults. West J Med. 1992;156:495-500. (12) Shekelle PG, MacLean CH, Morton SC, Wenger NS. Assessing the care of vulnerable elders: Methods for developing quality indicators. Ann Intern Med. 2001; [In press]. (13) Consensus Development Panel. National Institutes of Health consensus development conference statement: Geriatric assessment methods for clinical decision-making. J Am Geriatr Soc. 1988;36:342-7. (14) Stuck AE, Siu AL, Wieland GD, Adams J, Rubenstein LZ. Comprehensive geriatric assessment: a meta-analysis of controlled trials. Lancet. 1993;342:1032-36. 21 (15) Fabacher D, Josephson K, Pietruszka F, Linderborn K, Morley JE, Rubenstein LZ. An in-home preventive assessment program for independent older adults: a randomized controlled trial. J Am Geriatr Soc. 1994;42:630-638. (16) Stuck AE, Aronow HU, Steiner A, Alessi CA, Bula CJ, Gold MN, et al. A trial of annual in-home comprehensive geriatric assessments for elderly people living in the community. N Engl J Med. 1995;333:1184-89. (17) Burns R, Nichols LO, Graney MJ, Cloar FT. Impact of continued geriatric outpatient management on health outcomes of older veterans. Arch Intern Med. 1995;155:1313-18. (18) Toseland RW, O'Donnell JC, Engelhardt JB, Hendler SA, Richie JT, Jue D. Outpatient geriatric evaluation and management. Results of a randomized trial. Med Care. 1996;34:624-40. (19) Leveille SG, Wagner EH, Davis C, Grothaus L, Wallace J, LoGerfo M, et al. Preventing disability and managing chronic illness in frail older adults: a randomized trial of a community-based partnership with primary care. J Am Geriatr Soc. 1998;46:1191-98. (20) Reuben DB, Frank JC, Hirsch SH, McGuigan KA, Maly RC. A randomized clinical trial of outpatient comprehensive geriatric assessment coupled with an intervention to increase adherence to recommendations. J Am Geriatr Soc. 1999;47:269-76. (21) Rubenstein LZ, Josephson KR, Harker JO, Miller DK, Wieland D. The Sepulveda GEU Study revisited: long-term outcomes, use of services, and costs. Aging (Milano). 1995;7:212-17. 22 (22) Reuben DB, Borok GM, Wolde-Tsadik G, Ershoff DH, Fishman LK, Ambrosini VL, et al. A randomized trial of comprehensive geriatric assessment in the care of hospitalized patients. N Engl J Med. 1995;332:1345-50. (23) Siu AL, Kravitz RL, Keeler E, Hemmerling K, Kington R, Davis JW, et al. Postdischarge geriatric assessment of hospitalized frail elderly patients. Arch Intern Med. 1996;156:76-81. (24) Karppi P, Tilvis R. Effectiveness of a Finnish geriatric inpatient assessment. Two-year follow up of a randomized clinical trial on community-dwelling patients. Scand J Prim Health Care. 1995;13:93-98. (25) Karppi P. Effects of a geriatric inpatient unit on elderly home care patients: a controlled trial. Aging (Milano). 1995;7:207-11. (26) Hay WI, van Ineveld C, Browne G, Roberts J, Bell B, Mills M, et al. Prospective care of elderly patients in family practice. Is screening effective? Can Fam Physician. 1998;44:2677-87. (27) Clark F, Azen SP, Zemke R, Jackson J, Carlson M, Mandel D, et al., Occupational therapy for independent-living older adults. A randomized controlled trial. JAMA. 1997;278:1321-26. (28) Moore AA, Siu A, Partridge JM, Hays RD, Adams J. A randomized trial of office-based screening for common problems in older persons. Am J Med. 1997;102:371-78. 23 (29) Germain M, Knoeffel F, Wieland D, Rubenstein LZ. A geriatric assessment and intervention team for hospital inpatients awaiting transfer to a geriatric unit: a randomized trial. Aging (Milano). 1995;7:55-60. (30) Siu AL, Morishita L, Blaustein J. Comprehensive geriatric assessment in a day hospital. J Am Geriatr Soc. 1994;42:1094-99. (31) Trentini M, Semeraro S, Rossi E, Giannandrea E, Vanelli M, Pandiani G, et al. A multicenter randomized trial of comprehensive geriatric assessment and management: experimental design, baseline data, and six-month preliminary results. Aging (Milano). 1995;7:224-33. (32) Miller DK, Lewis LM, Nork MJ, Morley JE. Controlled trial of a geriatric case-finding and liaison service in an emergency department. J Am Geriatr Soc. 1996;44:513-20. (33) Slaets JP, Kauffmann RH, Duivenvoorden HJ, Pelemans W, Schudel WJ. A randomized trial of geriatric liaison intervention in elderly medical inpatients. Psychosom Med. 1997;59:585-91. (34) Pitkala K. The effectiveness of day hospital care on home care patients. J Am Geriatr Soc. 1998;46:1086-90. (35) Rubin CD, Sizemore MT, Loftis PA, de Mola NL. A randomized, controlled trial of outpatient geriatric evaluation and management in a large public hospital. J Am Geriatr Soc. 1993;41:1023-28. 24 (36) Silverman M, Musa D, Martin DC, Lave JR, Adams J, Ricci EM. Evaluation of outpatient geriatric assessment: a randomized multi-site trial. J Am Geriatr Soc. 1995;43:733-40. (37) Cavalieri TA, Chopra A, Gray-Miceli D, Shreve S, Waxman H, Forman LJ. Geriatric assessment teams in nursing homes: do they work? J Am Osteopath Assoc. 1993;93:1269-72. (38) Bradley KA, McDonell MB, Bush K, Kivlahan DR, Diehr P, Fihn SD. The AUDIT alcohol consumption questions: reliability, validity, and responsiveness to change in older male primary care patients. Alcohol Clin Exp Res. 1998;22:1842-49. (39) Joseph CL, Ganzini L, Atkinson RM. Screening for alcohol use disorders in the nursing home. J Am Geriatr Soc. 1995;43:368-73. (40) Willenbring ML, Christensen KJ, Spring WDJ, Rasmussen R. Alcoholism screening in the elderly. J Am Geriatr Soc. 1987;35:864-69. (41) Morton JL, Jones TV, Manganaro MA. Performance of alcoholism screening questionnaires in elderly veterans. Am J Med. 1996;101:153-59. (42) Moran MB, Naughton BJ, Hughes SL. Screening elderly veterans for alcoholism. J Gen Intern Med. 1990;5:361-64. (43) Fulop G, Reinhardt J, Strain JJ, Paris B, Miller M, Fillit H. Identification of alcoholism and depression in a geriatric medicine outpatient clinic. J Am Geriatr Soc. 1993;41:73741. 25 (44) Bradley KA, Boyd-Wickizer J, Powell SH, Burman ML. Alcohol screening questionnaires in women: a critical review. JAMA. 1998;280:166-71. (45) Fink A, Hays RD, Moore AA, Beck JC. Alcohol-related problems in older persons. Determinants, consequences, and screening. Arch Intern Med. 1996;156:1150-1156. (46) U.S. Preventive Services Task Force. Problem drinking. In: Guide to Clinical Preventive Services. Baltimore, MD: Williams & Wilkins; 1996:574-81. (47) Fiellin DA, Reid C, O'Connor PG. Screening for alcohol problems in primary care: a systematic review. Arch Intern Med. 2000;160:1977-89. (48) Fleming MF, Manwell LB, Barry KL, Adams W, Stauffacher EA. Brief physician advice for alcohol problems in older adults: a randomized community-based trial. J Fam Pract. 1999;48:378-84. (49) Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Goldstein MG, Gritz ER, et al. Smoking Cessation. Clinical Practice Guideline No 18. Publication No. 96-0692. Rockville, MD: Agency for Health Care Policy and Research, US Department of Health and Human Services;1996. (50) Fiore MC, Bailey WC, Cohen SJ, et al. Treating Tobacco Use and Dependence. A Clinical Practice Guideline. AHRQ Publication No.00-0032. Rockville, MD: US Department of Health and Human Services; 2000. (51) Fiore MC, Bailey WC, Cohen SJ, Dorfman SF, Fox BJ, Goldstein MG, et al. A clinical practice guideline for treating tobacco use and dependence: A US Public Health Service 26 report. The Tobacco Use and Dependence Clinical Practice Guideline Panel, Staff, and Consortium Representatives. JAMA. 2000;283:3244-54. (52) Silagy C. Physician advice for smoking cessation. Cochrane Database of Systematic Reviews; 2000. (53) Kottke TE, Battista RN, DeFriese GH, Brekke ML. Attributes of successful smoking cessation interventions in medical practice. A meta-analysis of 39 controlled trials. JAMA. 1988;259:2883-89. (54) Cromwell J, Bartosch WJ, Fiore MC, Hasselblad V, Baker T. Cost-effectiveness of the clinical practice recommendations in the AHCPR guideline for smoking cessation. Agency for Health Care Policy and Research. JAMA. 1997;278:1759-66. (55) Cummings SR, Rubin SM, Oster G. The cost-effectiveness of counseling smokers to quit. JAMA. 1989;261:75-79. (56) Raw M, McNeill A, West R. Smoking cessation: evidence based recommendations for the healthcare system. BMJ. 1999;318:182-85. (57) U.S.Preventive Services Task Force. Preventing tobacco use. In: Guide to Clinical Preventive Services: Report of the U.S. Preventive Services Task Force. Baltimore,MD: Williams & Wilkins; 1996:602-609. (58) Department of Health and Human Services. The Health Benefits of Smoking cessation: A Report of the Surgeon General. Publication No. DHHS (CDC) 90-8416. Rockville, MD: Department of Health and Human Services; 1990. 27 (59) Berlin JA, Colditz GA. A meta-analysis of physical activity in the prevention of coronary heart disease. Am J Epidemiol. 1990;132:612-28. (60) Lindsted KD, Tonstad S, Kuzma JW. Self-report of physical activity and patterns of mortality in Seventh-Day Adventist men. J Clin Epidemiol. 1991;44:355-64. (61) Paffenbarger RSJ, Hyde RT, Wing AL, Lee IM, Jung DL, Kampert JB. The association of changes in physical-activity level and other lifestyle characteristics with mortality among men. N Engl J Med. 1993;328:538-45. (62) Blair SN, Kohl HW, Barlow CE, Paffenbarger RSJ, Gibbons LW, Macera CA. Changes in physical fitness and all-cause mortality. A prospective study of healthy and unhealthy men. JAMA. 1995;273:1093-98. (63) Sherman SE, D'Agostino RB, Cobb JL, Kannel WB. Does exercise reduce mortality rates in the elderly? Experience from the Framingham Heart Study. Am Heart J. 1994;128:965-72. (64) Kaplan GA, Seeman TE, Cohen RD, Knudsen LP, Guralnik J. Mortality among the elderly in the Alameda County Study: behavioral and demographic risk factors. Am J Public Health. 1987;77:307-12. (65) Centers for Disease Control and Prevention. The effects of physical exercise on health and disease. In: 1997 Surgeon General's Report on Physical Activity and Health; 1997; 85-87. 28 (66) Berard A, Bravo G, Gauthier P. Meta-analysis of the effectiveness of physical activity for the prevention of bone loss in postmenopausal women. Osteoporos Int. 1997;7:33137. (67) Steptoe A, Edwards S, Moses J, Mathews A. The effects of exercise training on mood and perceived coping ability in anxious adults from the general population. J Psychosom Res. 1989;33:537-47. (68) Moses J, Steptoe A, Mathews A, Edwards S. The effects of exercise training on mental well-being in the normal population: a controlled trial. J Psychosom Res. 1989;33:4761. (69) Donahue RP, Abbott RD, Reed DM, Yano K. Physical activity and coronary heart disease in middle-aged and elderly men: the Honolulu Heart Program. Am J Public Health. 1988;78:683-85. (70) Cononie CC, Graves JE, Pollock ML, Phillips MI, Sumners C, Hagberg JM. Effect of exercise training on blood pressure in 70- to 79-yr-old men and women. Med Sci Sports Exerc. 1991;23:505-11. (71) Williamson DF, Madans J, Anda RF, Kleinman JC, Kahn HS, Byers T. Recreational physical activity and ten-year weight change in a US national cohort. Int J Obes Relat Metab Discord. 1993;17:279-86. (72) Helmrich SP, Ragland DR, Leung RW, Paffenbarger RSJ. Physical activity and reduced occurrence of non-insulin-dependent diabetes mellitus. N Engl J Med. 1991;325:147-52. 29 (73) Manson JE, Nathan DM, Krolewski AS, Stampfer MJ, Willett WC, Hennekens CH. A prospective study of exercise and incidence of diabetes among US male physicians. JAMA. 1992;268:63-67. (74) U.S.Preventive Services Task Force. Promoting physical activity. In: Guide to Clinical Preventive Services. Baltimore, MD: Williams & Wilkins; 1996; 618-23. (75) American College of Sports Medicine Position Stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 1998;30:992-1008. (76) Hardcastle JD, Chamberlain JO, Robinson MH, Moss SM, Amar SS, Balfour TW, et al. Randomised controlled trial of faecal-occult-blood screening for colorectal cancer. Lancet. 1996;348:1472-77. (77) Mandel JS, Bond JH, Church TR, Snover DC, Bradley GM, Schuman LM, et al. Reducing mortality from colorectal cancer by screening for fecal occult blood. Minnesota Colon Cancer Control Study. N Engl J Med. 1993;328:1365-71. (78) Kronborg O, Fenger C, Olsen J, Bech K, Sondergaard O. Repeated screening for colorectal cancer with fecal occult blood test. A prospective randomized study at Funen, Denmark. Scand J Gastroenterol. 1989;24:599-606. (79) Hardcastle JD, Thomas WM, Chamberlain J, Pye G, Sheffield J, James PD, et al. Randomised, controlled trial of faecal occult blood screening for colorectal cancer. Results for first 107,349 subjects. Lancet. 1989;1:1160-1164. 30 (80) Wagner JL, Herdman RC, Wadhwa S. Cost effectiveness of colorectal cancer screening in the elderly. Ann Intern Med. 1991;115:807-17. (81) Selby JV, Friedman GD, Quesenberry CPJ, Weiss NS. A case-control study of screening sigmoidoscopy and mortality from colorectal cancer. N Engl J Med. 1992;326:653-57. (82) Solomon MJ, McLeod RS. Periodic health examination, 1994 update: 2. Screening strategies for colorectal cancer. Canadian Task Force on the Periodic Health Examination. CMAJ. 1994;150:1961-70. (83) U.S.Preventive Services Task Force. Colorectal cancer. In: Guide to Clinical Preventive Services. Baltimore, MD: Williams & Wilkins; 1996; 88-103. (84) Lieberman DA, Weiss DG, Bond JH, Ahnen DJ, Harinder G, Chejfec G, et al. Use of colonoscopy to screen asymptomatic adults for colorectal cancer. N Engl J Med. 2000;343:162-68. (85) Imperiale TF, Wagner DR, Lin CY, Larkin GN, Rogge JD, Ransohoff DF. Risk of advanced proximal neoplasms in asymptomatic adults according to the distal colorectal findings. N Engl J Med. 2000;343:174. (86) Sonnenberg A, Delco F, Inadomi JM. Cost-effectiveness of colonoscopy in screening for colorectal cancer. Ann Intern Med. 2000;133:573-84. (87) Kerlikowske K, Grady D, Rubin SM, Sandrock C, Ernster VL. Efficacy of screening mammography. A meta-analysis. JAMA. 1995;273:149-54. 31 (88) Demissie K, Mills OF, Rhoads GG. Empirical comparison of the results of randomized controlled trials and case-control studies in evaluating the effectiveness of screening mammography. J Clin Epidemiol. 1998;51:81-91. (89) Nystrom L, Rutqvist LE, Wall S, Lindgren A, Lindqvist M, Ryden S, et al. Breast cancer screening with mammography: overview of Swedish randomised trials. Lancet. 1993;341:973-78. (90) Chen HH, Tabar L, Fagerberg G, Duffy SW. Effect of breast cancer screening after age 65. J Med Screen. 1995;2:10-14. (91) Andersson I, Aspegren K, Janzon L, Landberg T, Lindholm K, Linell F, et al. Mammographic screening and mortality from breast cancer: the Malmo mammographic screening trial. BMJ. 1988;297:943-48. (92) van D, Holland R, Verbeek AL, Hendriks JH, Mravunac M. Efficacy of mammographic screening of the elderly: a case-referent study in the Nijmegen program in The Netherlands. J Natl Cancer Inst. 1994;86:934-38. (93) van Dijek JA, Verbeek AL, Beex LV, Hendriks JH, Holland R, Mravunac M, et al. Mammographic screening after the age of 65 years: evidence for a reduction in breast cancer mortality. Int J Cancer. 1996;66:727-31. (94) Boer R, de Koning HJ, van Oortmarssen GJ, van der Maas PJ. In search of the best upper age limit for breast cancer screening. Eur J Cancer. 1995;31A:2040-2043. 32 (95) Gabriel H, Wilson TE, Helvie MA. Breast cancer in women 65-74 years old: earlier detection by mammographic screening. Am J Roentgenol. 1997;168:23-27. (96) U.S.Preventive Services Task Force. Breast cancer. In: Guide to Clinical Preventive Services. Baltimore, MD: Williams & Wilkins; 1996; 76-87. (97) Miller AB, Baines CJ, To T, Wall C. Canadian National Breast Screening Study: 1. Breast cancer detection and death rates among women aged 40 to 49 years. CMAJ. 1992;147:1459-76. (98) Gotzsche PC, Olsen O. Is screening for breast cancer with mammography justifiable? Lancet. 2000;355:129-34. (99) McCarthy EP, Burns RB, Freund K, Ash AS, Shwartz M, Marwill SL, et al. Mammography use, breast cancer stage at diagnosis, and survival among older women. J Am Geriatr Soc. 2000;48:1226-33. (100) Walter LC, Covinsky KE. Cancer Screening in Elderly Patients: A Framework for individualized decision making JAMA. 2001;285:2750-2756 (101) Wenger NS, Shekelle PG and the ACOVE investigators. Assessing Care of Vulnerable Elders: ACOVE Project Overview. Ann Intern Med. 2001; [In press]. 33