Benefit Change Highlights Comprehensive Choice POS II Plan Highlights
advertisement

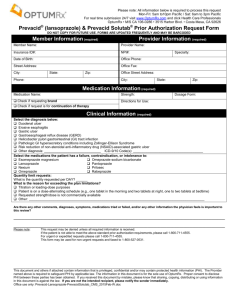
Benefit Change Highlights Comprehensive Choice POS II Plan Highlights Prescription Drugs Effective January 1, 2016 2015 In-Network Pharmacy Administrator Non-Network Caremark In-Network Non-Network OptumRx See Open Enrollment booklet for additional information HDHP Aetna Choice POS II Plan Highlights Effective January 1, 2016 2015 In-Network Calendar Year Out-of-Pocket Maximum Pharmacy Administrator Non-Network $5,000 / Employee Only $10,000 / Employee + Dependents In-Network Non-Network $4,500 / Employee Only $6,750 / Employee + Dependents $6,750 / Employee Only $10,125 / Employee + Dependents Family OOP applies to all members Family OOP applies to all members Caremark OptumRx See Open Enrollment booklet for additional information 2015 Effective January 1, 2016 Basic Life/AD&D Basic Life benefit 100% Employer-Paid Options: 2x annual base salary up to maximum of $1,500,000 100% Employer-Paid Options: 1) $50,000 benefit amount 2) 2x annual base salary up to maximum of $1,500,000 Buy Up Option: 3x annual base salary available on age-rate basis Buy Up Option: 3x annual base salary available on age-rate basis (rate sheet available on the Open Enrollment system) Voluntary Life/AD&D Carrier 2015 Effective January 1, 2016 Adam’s Group Insurance Prudential New and existing enrollees under the Voluntary Life and/or AD&D must complete a Prudential Beneficiary Form CA FLEX EMPLOYEES • 2 Additional Benefit Change Highlights CVS Caremark to OptumRx effective January 1, 2016 Frequently Asked Questions The Scripps Research Institute is working to make this as seamless a transition as possible for participants with minimal disruption for members. Below please find some commonly asked questions regarding the transition. For more information, please go to the TSRI intranet site. 1. Will I be receiving a new ID card? Yes, OptumRx will be sending out new ID cards prior to January 1st. 2. I am currently enrolled in the Aetna CA HMO. Does this change apply to me? No, it does not. This change applies to participants enrolled in the Comprehensive Choice POS II and HDHP Aetna Choice POS II plans. 3. Will I be receiving anything in the mail? Prior to January 1st, you will receive a welcome kit which will include your new ID card as well as a welcome letter and brochures to ease you into the transition. 4. Can I access my information online? Prior to January 1st, members may access the OptumRx Public Portal at https://ctr.benefits.catamaranrx.com/rxpublic/portal/memberMain?customer=CTRNS for basic information. Effective January 1st, members may access the Member Portal that will contain specific plan information. Members may register and log on at optumrx.com/myCatamaranRx. A mobile app is also available for members by scanning the QR Code to the right or downloading the mobile app through Apple App StoreSM or Google PlayTM. 5. My medication requires prior authorization. Will I need to go through this process again? Prior authorizations (unless expired or near expiration) will automatically transfer from CVS Caremark to OptumRx. 6. I am currently signed up for mail order. Will I need to sign up through OptumRx? For most members, mail order prescriptions will automatically transfer to OptumRx. However, for those with expired or close to expiring prescriptions, or prescriptions for controlled substances, members will need to sign up for mail order directly with Optum Rx. A mail order form will be included in the welcome kit or you may complete the process online through your member account. CA FLEX EMPLOYEES • 3