New Born
advertisement

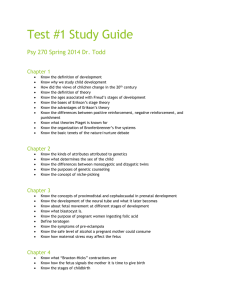
1 Abdulmahdi A. Hasan* *Ph,D, pediatric & psychiatric Mental Health Nursing New Born DELIVERY PREPARATION All needed equipment is available and working properly, Warmer- head often is in a slight Trendelenburg position to help facilitate drainage of airway secretions, Pre-warmed blankets, Cord clamp, Wall suction with a mucous trap, Bulb syringe, Timer with alarms at 1 and 5 minutes, Infant stethoscope, Scale, Erythromycin eye ointment, Vitamin K, and Identification bands. Emergency resuscitation equipment should be available, including: Oxygen mask and tubing; Ambu bag and mask; laryngoscope with both 0 and 1 blades; Endotracheal tubes sizes 2.5,3.0, 3.5, and 4.0; and resuscitation drugs including Narcan. Narcan is used in newborns to reverse respiratory suppression resulting from maternal pain medication. DELIVERY PREPARATION Review information about the mother’s prenatal history and labor to assess for potential risks during delivery. length of rupture of membranes, any meconium staining to the amniotic fluid, any signs of maternal infections prenatally or during labor, fetal heart monitoring such as decelerations, estimated gestational age, single or multiple gestation, and any maternal pain medications and when they were last dosed. Nurses always adhere to standard precautions 2 TRANSITION OF THE NEWBORN First 28 days of life, the baby is considered a newborn or neonate. Newborns face the challenge of adapting to extra uterine life. 1 Circulatory Changes Fetal circulation depends on patency of the foramen ovale (an opening between the right and left atria) and ductus arteriosus (an opening that allows blood to flow from the pulmonary artery into the aorta). These two openings allow most blood volume to bypass the dormant lungs and instead to move through the fetal side of the placenta, providing oxygen and eliminating carbon dioxide and wastes. At birth, once the cord is clamped, these two communicating openings must close for proper circulation. TRANSITION OF THE NEWBORN Newborn color at birth is typically pale or even cyanotic. As newborns begin breathing and circulation body color to become pinker. Common to have acrocyanosis or mottling. With acrocyanosis, the trunk remains pink, but the Extremities appear cyanotic. Acrocyanosis usually resolves after the first 24 hours. Mottling is a marbled appearance to the skin that often occurs when neonates are chilled slightly, such as when being undressed. Mottling also is related to circulatory labiality and dissipates over time. Thermoregulation Babies are born with a substance in the upper back called brown fat, which is a stored energy that they can use to generate heat. Term infants have more brown fat than preterm babies -a finite amount, however, and once they use it, they produce no more. Therefore, keeping newborns warm and avoiding cold stressing them are essential . The Four Types of Heat Loss in Newborns Evaporative, occurs immediately as they make contact with air temperature. Therefore, drying newborns immediately after birth is critical Conductive, heat from a warm object transfers to a cooler object through direct contact- use pre-warmed blankets and equipment. Radiant, occurs when heat is lost from a warm object to a cooler one not in contact with each other.- radiant warmers, 3 Convective, lose heat to cooler air- keep infants away from currents such as air conditioners and fans. Heat Loss in Newborns The surface area of head is very large compared to the surface area of the body. Placing a hat on the head can reduce heat loss. 2 Immediate Nursing Care Drying and Suctioning- mouth first, then nose-so you do not stimulate breathing and meconium aspiration. Meconium is the first stool that the neonate passes; it is very thick and sticky. Apgar Scoring Appearance (color), Pulse (heart rate), Grimace (irritability to suctioning), Activity (muscle tone), Respiration (breathing efforts). Each of these five items is scored as 0, 1, or 2 for a maximum total of 10. Apgar scores are given 1 and 5 minutes after birth. Never wait until 1 minute to decide if a neonate needs resuscitation. Immediate Nursing Care Measurements and Weight Eye Prophylaxis Vitamin K Administration Identification and Safety Suctioning of Stomach Contents Documentation Newborn Assessment Gestational Age Head-to-Toe Physical Assessment Assessment of Reflexes Ongoing Nursing Care Assessment and Monitoring Normal pulse rate ranges from 110 to 160 bpm, Normal respiratory rate ranges from 30 to 60 breaths per minute. 4 Take axillary temperature by placing the tip of the thermometer probe firmly in the axilla and holding it there for 3 minutes. Tympanic temperature probes, Hold the infant’s head still while performing a tympanic temperature. Blood pressure is normally low. Systolic readings from 50 to 80 mm Hg; diastolic readings from 30 to 50 mm Hg.- usual site used is the leg. blood glucose level-a heel stick or toe prick to obtain a drop of blood. 3 Bathing Cord Care After 24 to 48 hours, putting rubbing alcohol on the cord with every diaper change. The cord will dry and usually fall off in 10 to 14 days. Once it falls off, yellowish or greenish drainage may appear from the umbilicus. To help dry this drainage, continue to apply alcohol. Elimination 6 to 10 wet diapers per day. Elimination The first stool is meconium (discussed earlier). Then greenish to yellow and often seedy. Within a few days, the stool changes to mushy yellow or golden. The stool of a breastfed infant is somewhat less offensive in odor than that of a formula-fed infant.- Document Change diapers fairly frequently to limit skin exposure to urine and stool to help prevent diaper rashes. Discourage use of powder, which can pose an aspiration risk, trap moisture, and promote rashes. Screening Tests phenylketonuria (PKU), galactosemia, maple syrup urine disease, hypothyroidism, biotinidase deficiency hemoglobinopathy 5 glucose-6-phosphate dehydrogenase deficiency, and congenital adrenal hyperplasia. sickle cell trait. should not be done before 24 hours of life, and better after 48 to 72 hours of life. Circumcision Circumcision is surgical removal of the foreskin of the penis. Do not feed the infant right before the procedure, because feeding can lead to possible regurgitation and potential aspiration. Sterile gauze dressing remains in place for 24 hours or per doctor or midwife order. Inspect the site for bleeding often for the first few hours. And with every diaper change. Do not lay the infant on his abdomen for several hours after the procedure. Total healing takes approximately 1 week. Feeding Some hospitals have protocols stating that the first thing an infant can receive is sterile water. Newborns are fed “on demand.” Most newborns awaken every 2 to 4 hours to eat. Most newborns eat 1 to 3 ounces per feeding, often every 3 hours. Over a few weeks, Burp the infant after he or she has taken approximately 0.5 to 1 ounce of formula. Colostrums, the first breast milk the woman produces after delivery, is thick and yellowish. It contains many vitamins, minerals, protein, and fats and is high in antibodies. 2- 4 days Mothers may find that their breasts become larger, more firm, and tender. This is referred to as engorgement and typically lasts 24 to 48 hours. Sore Nipples. woman may rub some breast milk on the nipples after breastfeeding and allow it to air-dry. Women should wear cotton bras. They may use breast pads but must change these frequently to prevent constant moisture against the skin. should not use soap on the nipple because it is drying. 4 6 They can rub vitamin E oil on the nipples; need to wash it off before the infant feeds. Mastitis: Symptoms include redness, swelling, tenderness, feeling warm to the touch, and fever. Cause is bacteria from the infant’s mouth entering the breast through a crack on the nipple. Treatment is with antibiotics; infant can continue to breastfeed. Explaining Infant Behavior Involve fathers in the care of the infant. Having a baby is a life-altering event. The parents will no longer have the freedoms that they once had. The mother usually sees her physician or midwife 6 weeks after delivery. Promoting Bonding Bonding refers to the initial attachment process between newborn and parents. It should begin soon after delivery. Face-to-face Nurses also may choose to place the infant’s naked body against the mother’s naked chest for skin-to skin contact. This provides warmth for the infant and a sense of attachment between mother and child. Observe infant–parent interactions and assess for positive attachment. 5