Reproductive Development Reproductive development Intrauterine Development
advertisement
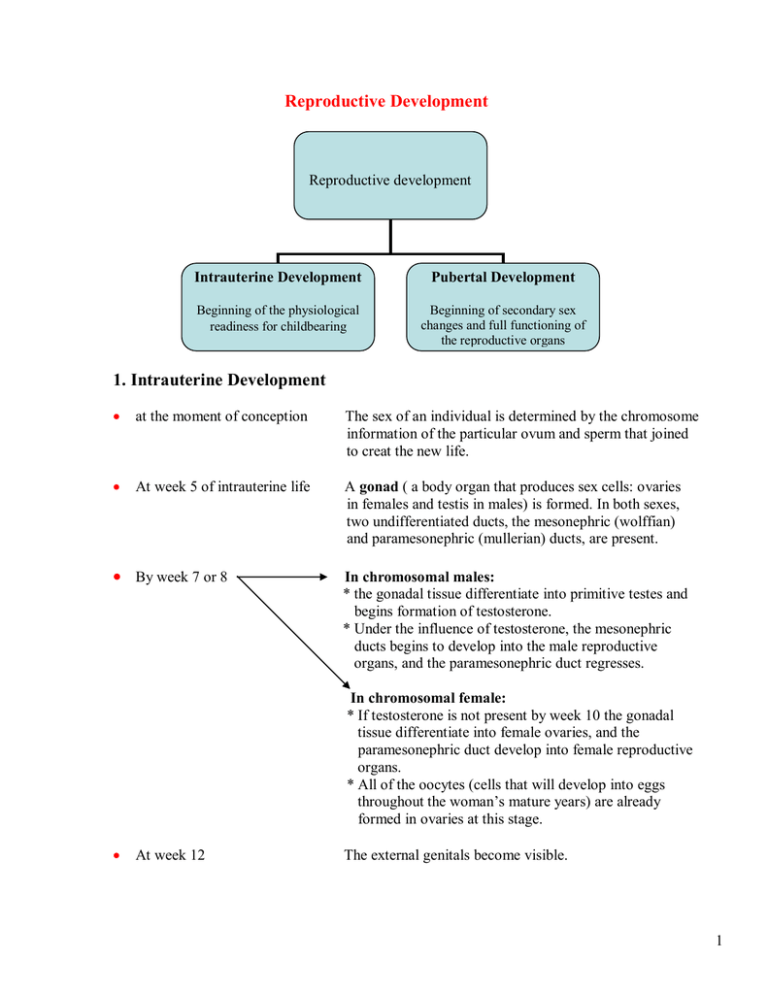
Reproductive Development Reproductive development Intrauterine Development Pubertal Development Beginning of the physiological readiness for childbearing Beginning of secondary sex changes and full functioning of the reproductive organs 1. Intrauterine Development at the moment of conception The sex of an individual is determined by the chromosome information of the particular ovum and sperm that joined to creat the new life. At week 5 of intrauterine life A gonad ( a body organ that produces sex cells: ovaries in females and testis in males) is formed. In both sexes, two undifferentiated ducts, the mesonephric (wolffian) and paramesonephric (mullerian) ducts, are present. By week 7 or 8 In chromosomal males: * the gonadal tissue differentiate into primitive testes and begins formation of testosterone. * Under the influence of testosterone, the mesonephric ducts begins to develop into the male reproductive organs, and the paramesonephric duct regresses. In chromosomal female: * If testosterone is not present by week 10 the gonadal tissue differentiate into female ovaries, and the paramesonephric duct develop into female reproductive organs. * All of the oocytes (cells that will develop into eggs throughout the woman’s mature years) are already formed in ovaries at this stage. At week 12 The external genitals become visible. 1 2. Pubertal Development: Puberty is the stage of life at which secondary sex changes begin. It begins when: Hypothalamus Synthesizes & releases Gonadotropin releasing hormone (GnRH) Triggers Anterior pituitary Releases Follicle-stimulating hormone (FSH) Luteinizing hormone (LH) initiate production of Estrogen & Progesterone Produces from Ovarian follicles Androgen Produces from Adrenal cortex & ovaries in female Adrenal cortex &testes in male 2 Role of androgen (on both sexes) Role of testosterone (in male) role of Estrogen (in female) - Muscular development - Development of testes, scrotum, penis, prostate, &seminal vesicles - Development of uterus fallopian tubes, & vagina; - Physical growth - Appearance of pubic, axillary, & facial hair. - Fat distribution & hair patterns. - Increase in sebaceous glands secretion - Laryngeal enlargement & voice Change. - Breast development. - Maturation of spermatozoa. - End the growth of long bones - Closure growth of long bones 3 Anatomy and Physiology of the Reproductive System Male Reproductive System External Structures: The external genital organs of the male include: 1. Penis: Composed of three cylindrical layers of erectile tissue. It serves as outlet for both the urinary and the reproductive tracts. The penile artery provides blood supply for the penis. 2. Scrotum: it is a rugated, skin-covered muscular pouch. It contains the testes, epididymis and the lower portion of the spermatic cord. Its function is to support the testes and help regulate the temperature of sperms. 3. Testes: They are two ovoid glands encased by protective white fibrous capsule and is composed of a number of lobules. Produce spermatozoa and testosterone (male hormone). 4 Internal Structure: The male internal reproductive organs are: 1. Epididymis: It is a tubule of each testis lead to a tightly coiled tube (20 ft. long). Responsible of conducting sperm from the testis to vas deferens. Sperms in the epididymis are immobile and incapable of fertilization. 2. Vas Deferens: An additional hollow tube surrounded by arteries and veins and protected by a thick fibrous coating. Carry sperms from the epididymis through the abdominal cavity to the seminal vesicles. Sperms are mature as the pass through vas deferens but still not mobile. 5 3. Seminal Vesicles: Two pouches that lies on the posterior surface of the bladder. Secret a viscous portion of the semen which has a high content of a basic sugar, protein, prostaglandins, and alkaline. Sperms become more mobile with this added fluid and favorable pH. Empty sperms into ejaculatory ducts. 4. Ejaculatory Ducts: The two ducts pass through the prostate gland and join the seminal vesicles with the urethra. 5. Prostate Gland: A chestnut-sized gland that lies just below the bladder. Secretes a thin alkaline fluid to protect sperm from being immobilized by the naturally low pH level of the urethra. 6. Bulbourethral Glands (Cowper’s glands): Two gland lie beside the prostate gland and by short ducts empty into the urethra. Also secrete an alkaline fluid that helps counteract the acid secretion of the urethra and ensure safe passage of spermatozoa. 6 Female Reproductive System External Structures: Consists of the following parts: 1. The mons pubis (mons veneris): a pad of fatty tissue overlying the symphysis pubis and covered by skin'and pubic hair. 2. The labia majora: two thick folds of skin and fat which pass from the mons pubis back to the perineum. 3. The labia minora: two skin folds enclosing the urethral and vaginal orifices. 4. The clitoris: a small rudimentary highly vascular and sensitive organ corresponding to the male penis 5. The vestibule: the area between the labia minora. It is perforated by the urethral and vaginal orifices and ducts of Bartholin's glands. 6. The urethral orifice: lies 2.5 cms posterior to clitoris, as a vertical cleft. The tiny orifices of the paraurethral ( skene's ) ducts lies on either side of the urethra . 7. The vaginal orifice (introitus of vagina): Occupies posterior two third of the vestibule, partially closed by hymen. It allows for passage of menstrual blood 8. Bartholin's glands: two small glands situated posteriorly close to the vaginal orifice. They secrete mucus which lubricates the vaginal orifice. 9. Fourchette: the membranous folds connecting the posterior ends of labia minora . 10. Perineum: the area extending between fourchette and anus. 7 Internal Structures The female internal organs are: 1. Two Ovaries. 2. Two Fallopian tubes. 3. The Uterus. 4. The vagina. Fig. 1: Female internal reproductive organs Fig.2: Anterior view of female internal reproductive organs. 8 1. Ovaries Structure: The ovaries are similar in origin to the testes in the male. Each ovary resembles a large almond in shape. They are grayish-white in color. Each ovary is approximately 4cm long x 2cm diameter and 1.5cm thick. Weight about 3 g. The surface of the ovary is smooth before menarche. After sexual maturity, scaring from repeated ruptures of follicles and ovulation results in roughened, nodular surface. Location and support: Ovaries are located on each side of the uterus, below and behind the fallopian tubes. They are held in place by two ligaments: the broad and the ovarian ligaments. 9 Layers (Divisions): A protective layer of surface epithelium. The cortex, filled with the ovarian and graafian follicles. The immature follicles mature into ova and produces estrogen and progesterone. The central medulla. Containing the nerves, blood vessels, lymphatic tissue and smooth muscle tissue. Blood Supply and lymphatics: Ovarian arteries carry blood supply from the aorta to the ovaries. The left ovarian vein empties into the left renal vein. The right drains into the inferior vena cava. The ovarian lymphatic drain into iliac periaortic nodes. Innervation: The nerve supply to the ovary is through T10 to L1, together with fibers of the pelvic sympathetic nervous system. Function: Produce and discharge mature ova (ovulation). Produce estrogen and progesterone in amounts required for normal growth, development, and function like initiate and regulate menstrual cycle. 10 2. Fallopian Tubes Structure: Each fallopian tube is a smooth hollow tunnel. It is approximately 10 cm in length, and. Anatomically divided into four separate parts: Interstitial: lies within the uterine wall and has the smallest lumen or tunnel (1mm in diameter). Isthmus: It is also narrow and small but firm much like the round ligament. This is the portion of the tube that is cut in the tubal ligation. Ampulla: it is the mid and the longest portion where the fertilization of an ova usually occur. Infundibulum: It is the most distal portion of tube from the uterus, and is funnelshaped. The rim of the funnel is covered by fimberia (small hair) that help to guide the ovum into the fallopian tube. Location: The fallopian tubes arise from each upper corner of the uterine body and extend outward and backward until each opens at the distal end next to an ovary. Layers: Outer coat of peritoneum. Connective tissue and circular muscle layer. The muscles produce a peristaltic motions to migrate the ova through the tube. The mucous membrane and ciliated lining: The mucous has a secretory function. It acts as a lubricant and also as a source of nourishment for the fertilized ova because it contains protein, water and salts. The ciliated lining aids in migration of the ova through the tube toward the uterine cavity. 11 3. Uterus Structure: It is a hollow, muscular, pear-shaped organ. With maturity the uterus is 5-7cm long, 5cm wide, and in its widest upper part 2.5cm deep. Its weight 60 gm. The uterus is divided into three parts: Fundus: The upper, rounded, prominence above the insertion of the fallopian tubes. Corpus (the body): the main portion, encircling the intrauterine cavity. Isthmus: The short and slightly constricted segment between the body and the cervix. Cervix (cervical canal): The lowest portion of the uterus. It representa about one third of the total uterine size. Half of it lies above the vagina and the other half extends into the vagina. Its junction at the Isthmus is the internal cervical os; the distal opening to the vagina id the external cervical os. Location and Support: It is located in the lower pelvis, posterior to the bladder and anterior to the rectum. It is not fixed in one location, it is free to enlarge without discomfort during pregnancy. The uterus is stabilized within the pelvic cavity by a number of paired ligaments (broad, round, uterosacral, and cardinal), and single ligaments (anterior and posterior) 12 Position: Normally with bladder empty the uterus in (anteversion) position, the uterus is tipped forward and slightly anteflexed (bend forward), with the corpus lying over the top of the posterior wall of the bladder. The cervix is directed downward and backward toward the tip of the sacrum. So it is usually at approximately a right angle to the plane of the vagina. Deviations of Uterine Position: Retroversion: a condition in which the fundus is tipped back. Anterflexion: a condition in which the body of the uterus is bent sharply forward at the junction with the cervix. Retroflexion: a condition in which the body of the uterus is bent sharply back just above the cervix. 13 Layers (Uterine wall) It is composed of (3) layers: Perimetrium: The outermost layer, offer added strength and support to the structure of the uterus. Myometrium: It is composed of smooth muscles arranged in (3) layers and extended in three directions (longitudinal, transverse, and oblique) make up the thick myometrium. These layers are: - Outer layer is composed of longitudinal fibers, which predominates in the fundus and provides power to expel the fetus. - Middle layer is composed of fibres interlaced with blood vessels in a figure (8) pattern. It is called a living ligature because its contraction after childbirth or abortion helps control blood loss. - Inner layer is composed of circular fibres, concentrated around the internal os to keep the cervix close during pregnancy. This layer is also concentrated where the fallopian tube join the uterine body to prevent the regurgitation of menstral blood out of the fallopian tubes during menstruation. Endometrium: It is a highly vascular lining of mucous membrane composed of three layers that undergoes cyclic changes with the menstrual cycle: -Superficial compact layer -Middle spongy layer -Basal layer that attaches the endometrium to the myometrium. 14 Uterine Blood Supply: Uterine arteries (90% of the blood supply). Ovarian arteries join the uterine arteries (adding 10% of the blood Supply). Uterine and Ovarian veins drain the blood from the uterus. Uterine Lymphatics: Uterine Lymphatics are extensive and composed of three network: at the base of the endometrium, within the myometrium, and under the uterine peritoneal. Drainage occurs at the isthmus, and near the fundus drainage joins that of ovarian and tubal lymphatics. Innervations: Parasympathetic fibers from the sacral nerves responsible for producing vasodilatation and inhibiting muscular contraction. Efferent sympathetic motor nerves (T5 to T10) cause vasoconstriction and muscular contraction. Functions: Cyclic menstruation with rejuvenation of the endometrium. Pregnancy. Labor. 15 4. Vagina Structure: Vagina is a thin-walled tube that is capable of great distention. The anterior wall of the vagina is 7-8 cm in length, while the length of the posterior wall is about 10 cm. The smooth muscle walls are lined with glandular mucous membrane which is responds to the estrogen and progesterone stimulation. Cells are lost from the mucosa’ especially during menstrual cycle and pregnancy. There are four fornices all around the protruding cervix: right, left, anterior, and posterior. The posterior fornix is the deepest. Location and Support: It is located in front of the rectum and behind the bladder and urethra. It extends from the external opening in the vestibule between the labia minora of the vulva to the cervix. It is supported mainly by its attachments to the pelvic floor musculature and fascia. Blood Supply: Blood supply from the descending branches of the uterine artery, the middle hemrrhiodal artery, and the internal pudendal arteries. Blood drain through the pudendal, external hemorrhoidal and uterine veins. Lymphatics: Upper vagina drain to the recovaginal septal, presacral, external iliac, and hypogastric nodes. Lower vagina drain to the superficial inguinal nodes. Innervation: The vagina is relatively insensitive, thus it is the source of less pain during the second stage of labor. 16