N u r s
advertisement

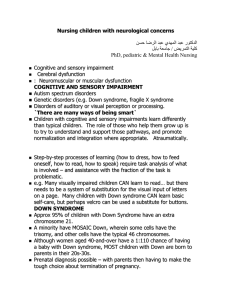
Nursing children with neurological concerns Nursing 315 October 2011 Reading: Review A&P of brain and spinal cord (refer to what you learned in Bio 251 & 252) Principles and practices of neuro assessment (refer to what you learned in N275) Perry, Hockenberry et al Chapters: 42: Cognitive and sensory impairment 51: Cerebral dysfunction 55: Neuromuscular or muscular dysfunction COGNITIVE AND SENSORY IMPAIRMENT Autism spectrum disorders Genetic disorders (e.g. Down syndrome, fragile X syndrome Disorders of auditory or visual perception or processing. `There are many ways of being smart` Children with cognitive and sensory impairments learn differently than typical children. The role of those who help them grow up is to try to understand and support those pathways, and promote normalization and integration where appropriate. Atraumatically. Step-by-step processes of learning (how to dress, how to feed oneself, how to read, how to speak) require task analysis of what is involved – and assistance with the fraction of the task is problematic. e.g. Many visually impaired children CAN learn to read… but there needs to be a system of substitution for the visual input of letters on a page. Many children with Down syndrome CAN learn basic self-care, but perhaps velcro can be used a substitute for buttons. DOWN SYNDROME Approx 95% of children with Down Syndrome have an extra chromosome 21. A minority have MOSAIC Down, wherein some cells have the trisomy, and other cells have the typical 46 chromosomes. Although women aged 40-and-over have a 1:110 chance of having a baby with Down syndrome, MOST children with Down are born to parents in their 20s-30s. Prenatal diagnosis possible – with parents then having to make the tough choice about termination of pregnancy. Characteristics of children with Down syndrome: Head/face: --rounded, small head (bradycephaly) --speckling of irides (brushfield’s spots) --short pinna, small ears --depressed nasal bridge --inner epicanthal folds --high, arched narrow palate --protruding tongue --short, broad neck Body: --shortened rib cage, short stature --congenital heart defects common --hypotonia (“like a rag-doll”) --wide space b/w big and second toe --transverse palmar (“simian”) crease --increase risk of hypothyroidism and leukemia Intellectual --average IQ around 50 Incidence: 1 per 800-1000 live births. Lifespan: more than 80% survive to age 55 years and beyond. No treatment exists to change the genetic makeup; but there are treatments and approaches to the multiple associated health issues: increased rates of congenital heart disease, hypotonia, hypothyroidism. You are working with an Early Intervention service and 5year-old Justin has just been referred to you. You want to help him develop his muscle tone, to encourage expression and to build his vocabulary. How will you do that. FRAGILE X SYNDROME Caused by an abnormal gene on the long arm of the X chromosome. Women can be carriers (the healthy X chromosome dominates) but men exhibit the trait. Classic physical findings include a long face with prominent jaw (prognathism), large protruding ears, and behavioral manifestations such as outbursts, hyperactivity, short attention span Speech and language therapies Modifications in teaching Occupational therapy Rx: Serotonin agents such as Carbamazepine (Tegretol) or Fluoxetine (Prozac) to control outbursts * Rx: CNS stimulants to improve attention span and decrease hyperactivity AUTISM SPECTRUM DISORDERS Immune and-or environmental factors interact with a genetic disorder of prenatal or postnatal brain development. What we see: some combination of difficulties in regulating motion and some parts of memory, delayed speech, atypical social interaction often starting with difficulties establishing eye contact, persistence of infantile reflexes, epileptic seizures. Incidence: 1 in 150 children are living with ASD (CDC, 2007). Screening for normal speech: 12 months… at least—babbling, gesturing 18 months… at least—a few single words 24 months… at least some two-word phrases A group of diverse disorders including: autism Asperger`s Pervasive Developmental Disorder Not Otherwise Specified (PDD-NOS). Diagnostic criteria (APA, DSM-4) includes: marked impairment in social interaction qualititative impairments in communication restricted repetitive and stereotyped patterns of behavior, interests, and activities (see p. 1200 of Perry et al text) The majority – but not all – children with autism have some degree of intellectual impairment, but also may have atypical abilities… and may excel in music, puzzle-building, mathematics. Most children with autism will require lifelong supports. Families need support. Videos of children and families living with autism. E.g Autism every day. 7-minute youtube video PERCEPTUAL DISORDERS Visual impairment Hearing impairment Dyslexia, dyscalculia, dysgraphia Auditory processing disorders Visuo-spatial processing disorders (nonverbal learning disabilities) VISUAL IMPAIRMENTS Can be caused by Genetic conditions such as: albinism, TaySachs disease Prenatal and perinatal infections such as: CMV, toxoplasmosis, herpes, chlamydia Ocular trauma Retinoblastoma. Unilateral (usually) or bilateral ocular tumors. Retinopathy of prematurity Amblyopia (strabismus, or e.g., or any cause of unilateral vision impairment leads the brain to receive images only from the stronger eye… so that the weaker eye is essentially unused … and corresponding visual centers in the brain also do not develop. HEARING IMPAIRMENTS Common – an estimated 3:1000 infants have some degree of hearing loss Types: Conductive hearing loss Sensorineural hearing loss Mixed Causes: genetic predisposition, anatomic malformations, perinatal infection such as CMV or toxoplasmosis, ototoxicity from certain antibiotics such as gentamycin used in treating pediatric infections, chronic ear infections, Down syndrome. Conductive hearing loss can be partially remedied with hearing aids, that amplify sound. Sensorineural hearing loss – cochlear implants. Children with sensorineural hearing loss have damaged the auditory nerves of the inner ear. The cochlear implants bypass these and stimulate surviving deeper auditory nerve fibers to send signals to the brain. Working with visually impaired children: dependance on auditory and tactile stimuli for orientation to time and space educational adaptations CEREBRAL DYSFUNCTION (chap 51) Trauma to the head, brain tumors, seizure disorders, and CNS infections all have neurological effects and sequelae. Head trauma remains a significant cause of death and permanent disability in children. Neurological assessment -- pupillary response eye opening in response to stimulus best motor response to stimulus best response to auditory or visual stimulus hand grip: equal, unequal LOC: alert; sleepy; irritable; disoriented; combative; lethargic; agitated… Muscle tone: normal; arching; spastic; flaccid; weak; decorticate; decerebrate… Fontanel: soft; flat; sunken; tense; bulging; closed Mood: content; quiet; withdrawn; flat; hostile Eye movement: normal; nystagmus; strabismus… Pediatric versions of Glasgow coma scale are available. Similar, but small children may not typically be oriented to time and place though verbal children usually can state their first name. See p. 1553 of text. TRAUMAS Head traumas acceleration & deceleration traumas subdural and epidural hematomas concussion skull fracture Post-traumatic syndromes post-concussion syndrome cranial nerve palsies seizure disorders Infants and young children have soft and not-quite-fused skulls. This presents a special plasticity to the brain, and overall, children can survive brain injury better than adults. However, their still-developing brains are especially vulnerable. Also, their comparatively large head size in rt the rest of their bodies means the head is particularly vulnerable to trauma. Underlying causes of symptoms is often related to not only to the actual injury or disease process and bruising/bleeding, but to the swelling that occurs, or blockage in the normal flow of cerebral spinal fluid through the ventricles of the brain… in the closed bony cranium. All of these events result in INCREASED INTRACRANIAL PRESSURE (IIP)… irritable, high-pitched unconsolable cry; tense and bulging fontanels; distended scalp veins; vomiting unrelated to feeding; headache; seizures; bradycardia; drowsiness; flexion or extension posturing… coma. Blunt trauma to the head in acceleration/deceleration impact results in bruising of the brain and tissues at the point of impact (coup), and directly opposite this (contrecoup). Trauma may also cause deformation of the head, with destruction of bone, brain, and other tissue. Care of children with head injury involves sustaining vital signs, possibly neurosurgery , possibly corticosteroid medication to reduce swelling. Support for families. While extent of tissue damage can be described, neurological outcomes are often unclear. Post-traumatic syndromes include hydrocephalus from damage to structures, cranial nerve palsies, sensory or motor deficits, emotional lability, behavior disturbances. CONCUSSION The most common head injury is concussion, a transient neuronal dysfunction, with instantaneous loss of awareness and responsiveness that lasts minutes to hours. May result in loss of consciousness – but not necessarily. Concussion is defined as a traumatically induced alteration in mental status. Confusion and amnesia follow. Pathogenesis of concussion is still a bit unclear, but may be a result of shearing forces that cause stretching, compression, and tearing of nerve fibers. POST-CONCUSSION SYNDROME can last for weeks to months. Involve symptoms of impaired memory, headache, behavioral disturbances. NEUROLOGICAL INFECTIONS Menigitis Encephalitis Reye’s syndrome Rabies MENINGITIS An acute inflammation of the meninges and CSF. Most common among under-fives. Recent immunizations against Hib (Haemophilus influenza type B) has successfully reduced the incidence of meningitis. However, meningitis can be caused by other organisms as well—bacterial or viral, such as Staphylococccus aureus, Escherichia coli, Neisseria meningitidis (meningococcus). The most common route of infection is vascular dissemination from foci of infection elsewhere. Baby with meningococcal infection Symptoms: sudden illness; arching; nuchal rigidity; irritability; vomiting unrelated to feeding; thermo instability; mottling; alterations in behavior and consciousness. Meningitis is a medical emergency. Dx: lumbar puncture for CSF Treatment: Sustain vital signs Isolation precautions IV access and hydration IV antibiotics (start with two broad-spectrum antibiotics; once culture and sensitivity results are back, one may suffice) Corticosteroids (e.g. dexamethasone) to reduce swelling 10 – 15% of bacterial meningitis is fatal. Outcomes depend on duration of illness before antibiotic therapy; type of organism; age of child; and adequacy of treatment. ENCEPHALITIS Can involve direct inflammation of the brain by a virus (e.g. herpes) or postinfectious inflammation after infection. Early symptoms are vague… fever, irritability… but these evolve to headache, dizziness, nuchal rigidity, changing levels of consciousness and possibly seizures Mild to severe forms. Tx: antiviral medications such as Acyclovir Prognosis is highly variable. Some children recover completely. Others have lifelong neurological sequelae. SEIZURE DISORDERS (EPILEPSY) Seizures are caused by excessive and disorderly neuronal discharges in the brain. Many forms…from subtle and transient to severe and continuous. Multiple possible causes – acute trauma or infection, toxins, tumors; metabolic disorders such as hypoglycemia or hypocalcemia; residual damage from past traumas… Types: simple partial seizures with motor signs (tonic/clonic movements of part of the body) simple partial seizures with sensory signs (numbness, tingling, prickling, pain, or paresthesia in part of the body) complex partial seizures (psychomotor seizures – such as transient amnesia or confusion; inability to respond to environment tonic-clonic seizures (formerly known as grand mal) involving a tonic phase (stiffening; eyes rolling up; apnea…); a clonic phase (from a few seconds to a half hour or longer, usually about 30 seconds) of violent jerking, incontinence…), and a post-ictal phase. Status epilepticus Series of seizures at intervals too brief to allow the child to regain consciousness between the time one event ends and another begins. A medical emergency as it can lead to respiratory arrest. Absence seizures (formerly called petit mal) involving brief loss of consciousness and may go unrecognized or be confused with “daydreaming”. Atonic and akinetic seizures (“drop attacks” with sudden loss of tone) Infantile spasms (sudden muscle spasms, possible rolling of eyes upwards in an infant) Videos Babyblue video of partial motor seizures http://www.bing.com/videos/search?q=video+child+seizur e&qpvt=video+child+seizure&FORM=VDRE# Video of child having tonic-clonic seizure What happens in children with seizure disorders? In response to physiological stimuli, such as cellular dehydration, severe hypoglycemia, electrolyte disturbances, sleep deprivation, emotional stress, or endocrine changes… hyperexcitable cells activate normal cells, and the impulse spreads thoughout… causing changes in sensorimotor perception and level of consciousness. Caring for a child having a seizure: Do not move or forcibly restrain him/her Support airway with positioning Remain calm, stay with the child, protect from injury. Isolate from view of curious bystanders 911 for status epilepticus ER treatment of status epilepticus involves support of respirations and vital signs (ABC) rectal diazepam / valium IV access IV antiepileptics: lorazepam/ ativan or diazepam/ valium or fosphenytoin/ cerebrex or phenobarbitol / phenobarb Treatment: Usually pharmacological, but it may take numerous drug adjustments to find the right dose of the right drug to control seizures while limiting side-effects. e.g. phenytoin (dilantin) valproic acid (depakene) Neuromuscular dysfunctions (chapter 55) Cerebral palsy Myelomeningocoele Congenital hydrocephalus Anencephaly Spinal muscular atrophy Werdnig-Hoffman Disease Kugelberg-Welander Disease Duchenne Muscular Dystrophy CEREBRAL PALSY http://www.youtube.com/watch?v=uFaw8etxMw8 YouTube: TomRogers123 8 minute video wherein a 13 year boy teaches us about what CP is. CEREBRAL PALSY (CP) A group of permanent disorders of the development of movement and posture, causing activity limitation, that are caused by nonprogressive disturbances that occurred in the fetal or infant brain. In addition to motor disturbances, CP also involves some combination of differences in sensation, perception, communication, cognition, secondary musculoskeletal conditions, and epilepsy Many children with CP have normal-or-better intellectual abilities. Causes: prenatal or perinatal asphyxia; low birth weight and prematurity; intrauterine infections; meningitis; shaken baby syndrome… Improvements in survivorship of very low birth weight babies has also resulted in a rise in the number of children with CP. Different types: spastic or pyramidal (>70%). involving hypertonicity and poor control of posture, balance, and coordinated movement. dyskinetic. Writhing and twisting movements ataxic or extrapyramidal. Wide gait; rapid repetitive movements mixed. Goals of care: To establish locomotion and communication. To gain optimal appearance To correct associated defects such as contractures as soon as possible To adapt educational opportunities To provide for social interaction with other affected and unaffected children. Orthopedic devices to aid locomotion include: Physical therapy Orthopedic surgery to correct contractures Pharmocotherapy for muscle relaxation Pharmacotherapy for seizure control Voice-activated computer technology Voice synthesizers for children who cannot speak Dental hygiene Protective headgear Recreational activities Supporting children and families… You are a nurse at a children’s hospital Ortho Unit. Bethany, age 6, who has spastic quadriplegic CP, is admitted for ortho surgery to correct some bony contractures of her lower limbs. Her voice is dysarthric. She is of normal intellect, and is frustrated when you cannot make out what she is saying. Her mother understands her words. No sibs. The dad left the family two years ago to start another family, and mom quit her job to be a full-time caregiver. The family receives social assistance. Plan? For Bethany? For her mom? NEURAL TUBE DEFECTS Normally, the spinal cord is covered by meninges and a column of bone, fusing in early fetal life. MYELODYSPLAGIA refers to any malformation of the spinal canal and spinal cord. NEURAL TUBE DEFECTS result from myelodysplagia and can occur at any point along the spinal tract, involving some or all of it. Can involve: Spina bifida occulta Meningocoele Myelomeningocoele Anencephaly MYELOMENIGOCOELE (spina bifida) What we see is some degree of motor and sensory loss in areas innervated at or below the lesion, affecting – to varying degrees – movement, sensation, and/or continence. Depending on the degree of downward-herniation of the spinal contents, children with spina bifida commonly also have congenital noncommunicating hydrocephalus. The downward traction tends to obstruct the flow of CSF between the ventricles of the brain. HYDROCEPHALUS http://www.youtube.com/watch?v=Tk6HyxSI4Ag ANENCEPHALY DUCHENNE MUSCULAR DYSTROPHY YouTube: iangriff2007 3 minute video wherein a teenager with Duchenne teaches us about his condition. Duchenne Muscular Dystrophy is the most severe and most common form. An X-linked recessive disorder affecting males almost exclusively… females are carriers. Boys with DMD usually have apparently normal development through infancy and early childhood… with evidence of muscle weakness appearing b/w ages 3-7. Early signs: waddling gait, lordosis, frequent falls, inability to ride a bicycle… Loss of independent ambulation by age 9-11. Slow but relentless progressive muscle weakness throughout the teenage years. Death occurs from failure of respiratory muscles or infection. Best lifespan: into early adulthood. Survival can be extended by respiratory support such as tracheostomy and suctioning… How to maximize independence in teenage boys with DMD? Genetic counseling for families affected. YOUR feelings about caring for children with serious neurological disorders? Societal stigmas? Countering societal stigmas?