Chemical and Drug Poisoning-Part Two Iron:
advertisement
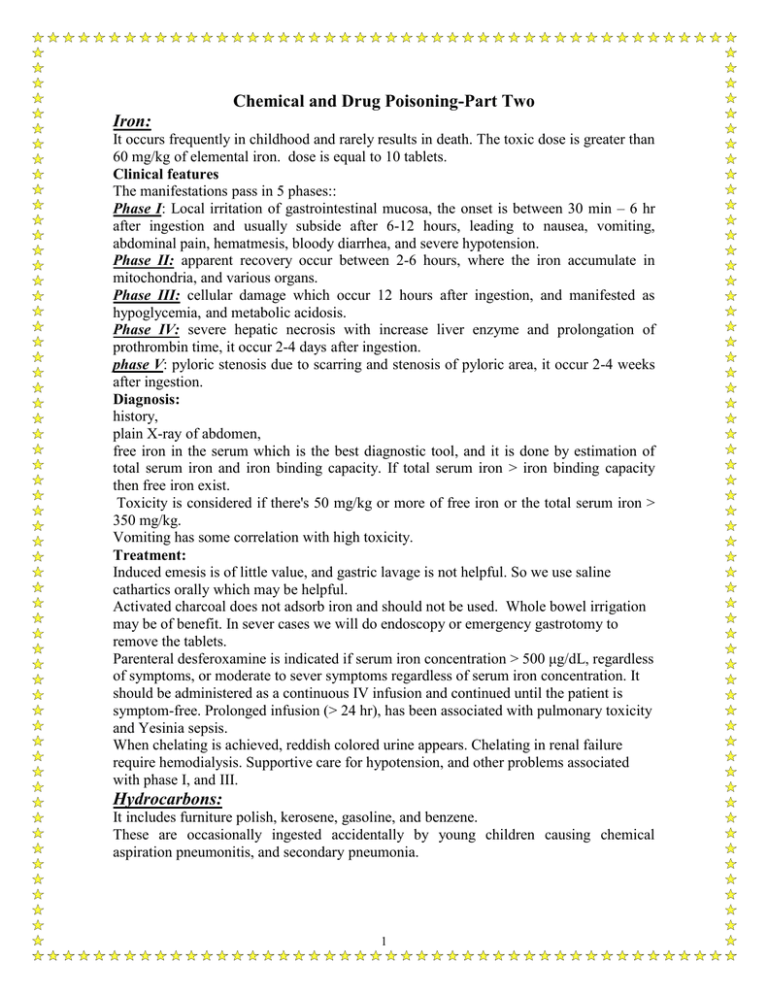
Chemical and Drug Poisoning-Part Two Iron: It occurs frequently in childhood and rarely results in death. The toxic dose is greater than 60 mg/kg of elemental iron. dose is equal to 10 tablets. Clinical features The manifestations pass in 5 phases:: Phase I: Local irritation of gastrointestinal mucosa, the onset is between 30 min – 6 hr after ingestion and usually subside after 6-12 hours, leading to nausea, vomiting, abdominal pain, hematmesis, bloody diarrhea, and severe hypotension. Phase II: apparent recovery occur between 2-6 hours, where the iron accumulate in mitochondria, and various organs. Phase III: cellular damage which occur 12 hours after ingestion, and manifested as hypoglycemia, and metabolic acidosis. Phase IV: severe hepatic necrosis with increase liver enzyme and prolongation of prothrombin time, it occur 2-4 days after ingestion. phase V: pyloric stenosis due to scarring and stenosis of pyloric area, it occur 2-4 weeks after ingestion. Diagnosis: history, plain X-ray of abdomen, free iron in the serum which is the best diagnostic tool, and it is done by estimation of total serum iron and iron binding capacity. If total serum iron > iron binding capacity then free iron exist. Toxicity is considered if there's 50 mg/kg or more of free iron or the total serum iron > 350 mg/kg. Vomiting has some correlation with high toxicity. Treatment: Induced emesis is of little value, and gastric lavage is not helpful. So we use saline cathartics orally which may be helpful. Activated charcoal does not adsorb iron and should not be used. Whole bowel irrigation may be of benefit. In sever cases we will do endoscopy or emergency gastrotomy to remove the tablets. Parenteral desferoxamine is indicated if serum iron concentration > 500 μg/dL, regardless of symptoms, or moderate to sever symptoms regardless of serum iron concentration. It should be administered as a continuous IV infusion and continued until the patient is symptom-free. Prolonged infusion (> 24 hr), has been associated with pulmonary toxicity and Yesinia sepsis. When chelating is achieved, reddish colored urine appears. Chelating in renal failure require hemodialysis. Supportive care for hypotension, and other problems associated with phase I, and III. Hydrocarbons: It includes furniture polish, kerosene, gasoline, and benzene. These are occasionally ingested accidentally by young children causing chemical aspiration pneumonitis, and secondary pneumonia. 1 The lower the viscosity and the higher the volatility of the hydrocarbon compound the greater is pulmonary toxicity. Inhalation of 0.1-0.2 ml is capable to involve large surface areas of the lung. Pathogenesis: They are aspirated during swallowing, vomiting, and gastric lavage. Ingestion of large amounts of these compounds is unusual because of bad taste. They interact with pulmonary surfactant causing alveolar collapse. Pulmonary changes are oedema, inflammation, and hemorrhage. Clinical features: Pulmonary manifestations lead to coughing immediately or within 2-5 min and vomiting within hours. There may be temperature elevation (38-40 C°), which may persist for 10 days, and may be associated with leukocytosis. The onset of symptoms may be delayed 12-24 hours which include dyspnea, decrease resonance, bronchial breathing, cripitation, hypoxemia, and cyanosis. The pulmonary involvement is discovered more frequently by chest X-ray, than by physical examination. X-ray findings appear few hours after ingestion which is commonly seen after 6 hours, but may be delayed 8-12 hours, peaking in 48-72 hr. Chest X-ray may remain abnormal long after the patient is clinically normal, and should not be used to guide acute treatment. Pneumatocele may appear on chest X-ray 2-3 wk after exposure. Within 2-5 days recovery occur in most cases. Systemic symptoms: CNS (somnolence, convulsion, ataxia, and coma). Heart (myocardial sensitization, CHF). Liver (hepatic toxicity). Irritation of GIT (hematemesis, and abdominal pain). Hematological toxicity (agranulocytosis). Skin burn. Complications: Pneumothorax. Subcutaneous emphysema. Pleural effusion. Empyema. Pneumatocele. Systemic infection with bacterimia or viremia. Treatment: No patient should be send home in < 6 hours even if there are no symptoms. Patients who are symptomatic when they are first examined and those who become symptomatic after 4 hours of examination and all patients who ingest toxic agent like furniture polish should be admitted. Induction of vomiting or gastric lavage is contraindicated because of risk of aspiration unless it contains a poison or large amount is ingested in which nasogastric suction is done with caution or done with cuffed endotracheal tube. No pulmonary therapy is indicated before development of symptoms. 2 Routine antibiotic is not recommended. It is indicated for secondary pneumonia which is detected by reappearance of fever within the third- fifth day after ingestion which is treated by penicillin G and tobramycin. Steroid should be avoided because they are not effective and may increase the risk of infection. Supportive measure which include O2, physiotherapy, ventilatory assistance and catheterization. Parents should be reminding to keep these compounds out of children. Prognosis: Depend on volume of ingestion or aspiration, specific agent and adequacy of medical care. Most children survive without complications. Some of them progress rapidly to respiratory failure and death. Digoxin: Digoxin can be a serious poison in children, with only a few tablets being fatal. Activated charcoal is useful. These children should be monitored very closely, probably in an intensive care unit, with careful ECG monitoring. Beta-blockers such as propranolol should be used in severe cases, with atropine if there is heart block. The serum potassium should not be allowed to go too low or too high. Digoxin-specific antibody fragments are now available for the reversal of life-threatening overdosage (Digibind). Tricyclic antidepressants: Tricyclic antidepressants such as amitriptyline are serious poisons for young children. Symptoms can develop as early as 30 min after ingestion, with serious symptoms within 6 hr of ingestion. CNS effects occur more frequently than do cardiovascular effects. Drowsiness, lethargy or coma is reported in 30% of pediatric cases. Coma usually resolves within few hr, but may last > 24hr.Seizures develop in 15% of cases, which are usually brief and resolve with out treatment. Cardiac effects such as sinus tachycardia, hypotension and conduction disorders and death by their direct effect on the myocardium. There may be blurred vision and dry mouth from the anticholinergic effects. Activated charcoal should be used. There is no specific antidote for tricyclic ingestion. The ECG should be monitored for at least 6 hrafter exposure. No treatment is indicated if there is adequate tissue perfusion and blood pressure. Metabolic acidosis should be corrected. Convulsions should be treated with diazepam. Life-threatening arrhythmias should be treated with propranolol. As tricyclics are protein bound active methods of elimination such as hemodialysis do not remove significant amounts of the drug. Acids: tend to cause inflammation and ulceration at the pylorus rather than the esophagus. This may lead to stenosis. Alkalis: such as caustic soda and dishwasher powder can cause burns to the mouth and esophageal ulceration, leading to stricture. For both acids and alkalis emesis or lavage should not be undertaken, nor any chemical antidotes as the heat of the reaction may increase injury. The extent of the injury should be assessed by endoscopy at an early stage. Steroids should be used to suppress the inflammation (prednisolone 2 mg/kg/day). Mercury poisoning 3 This common disorder was called ‘pink disease’ because of the color of the extremities or ‘acrodynia’ because of the accompanying pain. It was largely due to the use of mercurycontaining teething powders which have now been withdrawn. There was anorexia, loss of weight and hypotonia as well as the characteristic painful red or pink extremities. A differential diagnosis of this condition is the red extremities of neglected children. Treatment of mercury poisoning is by the deep IM injection of dimercaprol Cough medicines: Most cough medicines do not cause serious symptoms in the doses available to children. Medicines based on antihistamines may cause drowsiness and anticholinergic effects. Drowsiness will usually not need treatment but if coma occurs resuscitative measures should be used. Medicines based on codeine should be regarded as potentially toxic. Ibuprofen: Ibuprofen and other non-steroidal anti-inflammatory agents only seldom cause symptoms in children. Symptoms usually develop within 4-6 hr of ingestion and resolve within 24 hr. It may include nausea, vomiting, epigastric pain, followed by drowsiness, lethargy, and ataxia, metabolic acidosis, coma, transient apnea, renal failure, hypotension, and seizure can occur with large overdoses. Other reported effects include nystagmus, diplopia, tinnitus, and transient deafness. Renal function studies and acid-base balance should be monitored. Treatment: good supportive care Dishwashing liquid and shampoo: Are only toxic in large doses. Vomiting occurs in large doses. A period of observation may be needed. Disinfectants: Serious cases are unusual Nail varnish remover (acetone (: Observation for a period should be all that is needed but nausea and vomiting may occur, going on to coma if large amounts are taken. Salbutamol: There may be peripheral vasodilatation, muscle tremors and agitation. Serious symptoms are rare although severe hypokalemia and arrhythmias have been seen. Rat or mouse poison: The common ingredients of rat or mouse poison (warfarin or dichlorolose) are usually non-toxic in the doses taken by children. The exact type of poison should be identified using the poisons center and in most cases the child can be sent home after a short period of observation. If large amounts of warfarin are ingested vitamin K can be used but this is not needed in most cases. Talc: Talc is only toxic if inhaled. It may cause retching and choking due to pulmonary edema. Cases of ingestion only need a short period of observation to make certain that inhalation did not occur. 4 Benzodiazepines – tranquilizers and hypnotics such as diazepam (Valium) and nitrazepam (Mogadon): These can cause drowsiness and coma, but problems are unusual in accidental ingestion. In very young children respiratory depression may need treatment with artificial ventilation. Carbamazepine: This drug has some anticholinergic activity. Paradoxically convulsions and violent reactions may occur as well as cardiac problems such as heart block. Activated charcoal is useful to adsorb carbamazepine. Diphenoxylate (the active constituent in Lomotil, the antidiarrheal agent ): This compound has an opiate-like action, which causes prolonged respiratory depression. Treatment is with the opiate antagonist naloxone (10 mg/kg as i.v. bolus). There may be a transient improvement followed by relapse and cases should be observed for at least 36 h and repeated doses of naloxone given as necessary. Hyoscine: Hyoscine may cause dilated pupils, dry mouth, tachycardia and delirium due to anticholinergic effects. Observation will be all that is needed with most patients. Mefenamic acid (Ponstan): This drug rarely causes problems in young children. Activated charcoal is effective. Convulsions can be treated with diazepam. Metoclopramide: In overdose this drug causes extrapyramidal signs, drowsiness and vomiting. If extrapyramidal signs develop antiparkinsonian drugs such as procyclidine can be used. Theophylline: Theophylline can cause restlessness, agitation, vomiting, convulsions, coma, hypotension, hypokalemia and ventricular tachycardia. Activated charcoal can be used. Convulsions can be treated with diazepam. Food poisoning Salmonella species: This is salmonella typhi murium. The source is from meat and dairy products, like milk, cheese, egg, cream, cake , because of improper storage or made of these food. It is dried by heating. Clinical features: I.P. = 6 -72 hours, and the mean is 24 hours. Sudden onset of nausea, vomiting, crampy abdominal pain in the periumblical area and 5 the right lower quadrant followed by mild to severe watery diarrhea, and some times by dysenteric diarrhea. Moderate fever about 38.5 – 39 C° affects about 70% of patients. some children develop severe disease with high fever, headache, drowsiness, confusion, meningesmus sign, seizure and abdominal distension. The symptoms subside within 2-7 days in healthy child, mortality is rare. It is dangerous in neonate, and immunocompromized patients. Treatment: Is symptomatic (correction of dehydration, and electrolytes disturbacces), antibiotics for toxic patient we give third generation cephalosporins, cotrimoxazol, ampicillin, or chloramphinicol. Staphylococcus aureus: Caused by enterotoxigenic A, B, C, and D, which are heat stable. The source is improper storage of cocked food, and poor hygiene. The handlers of food might carry the microorganism because it could be found in nose and mouth, usually large number of patients are affected. I.P. = 1-6 hours. There will be sudden severe vomiting, watery diarrhea, low or absent fever. symptoms rarely persist > 12 -24 hours. Shock, and death rarely occur, antibiotics is useless because it is caused by toxin and the treatment is supportive. Botulism: It is acute flaccid paralytic illness caused by neurotoxin produced by clostridium botilinium which is the most poisonous substance that block neuromuscular transmission, and cause death through airway, and respiratory muscle paralysis. This is a rare form of food poising affect infants only caused by ingestion of improper caned food with exposure to low degree of temperature. Peak age is between 2-4 mouths of age. The risk factor is ingestion of honey. Breast feeding provide protection. Constipation is common. Illness is usually begin 18 – 36 hours after ingestion of infected food. Lethargy, weakness, cry, poor appetite, and dysphagia. Treatment: A- Supportive care by: 1- positioning by placing face up on a rigid bed , the head is tilted 30 degrees, a small cloth roll is placed under the cervical vertebrae. 2- About half of patients require endotracheal intubation, which is best done prophylactically. The patients have tolerated months of intubation with out a need for tracheotomy. 3- Feeding by nasogastric or nasojujenal tube, expressed breast milk is the most desirable food for infants. 4- Providing auditory, tactile, and visual stimuli, is beneficial. 5- Full hydration and stool softener such as lactulose. B- Human botulism immune globulin: single IV infusion of 50mg/kg, should be given as soon as possible C- antibiotics, for treatment of secondary infections like cotrimoxazol. Aminoglycoside should be avoided because it may potentiate blocking action of toxin on neuromuscular junction. 6 7