05 S p o t l i g h t ... P Proton and Ion Therapy
advertisement

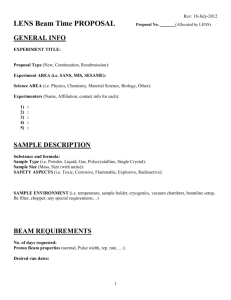
Institute of Physics and Engineering in Medicine Spotlight on 05 Proton and Ion Therapy Perspectives on: physics and engineering in medicine and biology Spotlight5.indd 1 Institute of Physics and Engineering in Medicine 29/01/2008 21:07:36 Proton and Ion Therapies provide cancer treatment with minimal side-effects Picture provided by Clatterbridge Centre for Oncology Picture provided by Clatterbridge Centre for Oncology The upper image shows a modulator wheel. Each vane is made from Perspex of a different thickness. Placing the wheel between patient and beam, and rotating it during the treatment, allows a single-energy beam to reach every depth within a tumour. The width and height of a tumour can be covered either by scanning across it, or by directing a widened beam at a brass collimator - like the one shown in the bottom image here - that only allows the beam to pass through the tumourshaped hole in its centre. Many forms of cancer can be treated with conventional radiotherapy in which beams of X-rays or gamma rays are directed at tumours. The energy deposited by the radiation kills some of the cancer cells, but also damages the healthy tissues the beam passes through on its journey to the tumour and further on through the body. This results in side effects such as diarrhoea and abnormal organ functioning, and the risk of inducing future cancers. The latest forms of ‘particle’ radiotherapy - proton therapy and ion therapy - promise to dramatically reduce the amount of collateral tissue damage, and hence many side effects, as most of their energy can be deposited within the cancer rather than in healthy tissues. Particle therapies use high-energy beams of protons (positively charged particles) or positive ions (in this case, atoms that have had all of their electrons removed). While able to treat a wide range of cancers, they are particularly suitable for treating small tumours that have been detected prior to the cancer spreading, and provide a viable alternative to risky surgical tumour removal from deep organs. Particle therapies also enable treatment of tumours that are inoperable and unsuitable for conventional radiotherapy because they are close to critical organs such as the spine or brain. In addition proton therapy has had considerable success treating small tumours in the eye. As well as reducing damage to healthy tissue, particle therapies can potentially be delivered in far fewer treatment sessions than established radiotherapy. For example in Japan the 30 or more sessions of conventional radiotherapy that small lung and liver cancers require has been replaced by a single particle beam treatment. 05 How Proton and Ion Therapy works Particle radiation kills cancer cells by altering their DNA. Changes such as DNA strand breakage are either the result of a direct hit from the radiation, or more usually occur after the water surrounding the DNA has been ionised by the radiation. Water molecules consist of two hydrogen atoms and an oxygen atom, but ionised water molecules can break up into hydrogen nuclei and hydroxyl radicals comprised of one oxygen atom and a single hydrogen atom. These hydroxyl radicals can transform back into water molecules by stealing hydrogen atoms out of a nearby DNA strand which, if a sufficient number of breaks occur close to each other, is irreparably damaged as a result. As charged particles pass through tissue they slow down and the slower they get the more ionisation they produce. So the beams of particles used in these therapies are made to stop within, and around the boundaries of, a cancer whose position and shape has been accurately determined via a CT or MRI scan. The particles therefore create by far the most ionisation (and direct DNA hits) in the cancer cells, rather than in the healthy cells passed en route. Higher energy charged particle beams can penetrate further into tissue than beams of lower energies, but some therapy beams have a fixed energy. So they can reach the required depths within the tumour, these beams are passed through a succession of different thickness materials before entering the patient. The extra distance travelled in each material reduces the beam penetration by a different amount, allowing a range of depths to be reached. For convenience the different thickness materials can be arranged as vanes on a ‘modulator wheel’ (see image top left). Particle beams must also cover the entire width and height of tumours. This is achieved either by scanning the beam across the tumour, or by widening the beam and using it in conjunction with a metal plate known as a collimator (see image bottom left). This is thick enough to stop the particles completely, and is custom-made so that the hole cut out of it matches the shape of the tumour. Placing the collimator immediately in front of the patient ensures that the only part of a widened beam that reaches the patient corresponds to the shape of their tumour. Proton and Ion Therapy Spotlight5.indd 2 29/01/2008 21:07:39 Picture provided by Clatterbridge Centre for Oncology The Clatterbridge Centre for Oncology in the Wirral has been successfully treating eye tumours since 1989, and was the world’s first hospital based proton therapy centre. In this picture a patient awaits treatment in a chair which can be positioned with enough precision to enable complete and consistent coverage of their tumour by the fixed beam. The UK’s National Physical Laboratory offers the ‘standard’ calibration of dose measuring equipment used in this system, and in several other systems in mainland Europe. In the future, different particles could be used to treat different types of cancer. For example carbon ions should prove better at killing large tumours with a reduced central blood supply than X-rays or protons, which rely on oxygen carried by the blood to enhance their effectiveness. Producing and guiding the particle beams The diagram on the back page shows the main stages of particle therapy delivery. First the protons or ions are accelerated up to the high energy required to travel into the body in either a cyclotron or synchrotron particle accelerator. (The left-hand cover image shows the superconducting cyclotron used to deliver proton radiation therapy at the Paul Scherrer Institute (PSI) in Switzerland.) Magnets are then used to bend the beam, guiding it from the accelerator into the treatment room. Additional magnets - in some cases mounted on metal gantries that can move 360º around the patient - then steer the beam into the tumour. (The righthand cover image shows the gantries and treatment couch at the PSI.) Wire chambers provide a check on beam position by measuring where the charged particles pass through them, while ionisation chambers check the strength of the beam by recording the amount of ionisation it produces in the air between the chamber plates. Advantages The major potential advantage of proton and ion therapies is that they substantially reduce damage to healthy tissues and organs. This not only lessens the likelihood of inducing new cancers, but also prevents effects such as weakening of bones that can lead to osteoporosis, and allows survival of more Spotlight5.indd 3 bone marrow so that patients can tolerate chemotherapy treatment better. It can also provide an alternative for patients unlikely to survive surgical tumour removal, or who have diseased organs - which might deteriorate further if irradiated - adjacent to cancers. With fewer side effects that require additional treatment, it should be possible to treat patients more quickly, reducing the overall cost of treating cancer as well as improving the patient experience. Availability in the UK The numbers of ‘high energy’ particle treatment centres (with beams with enough energy to reach any body area) in operation or being built are rapidly increasing in Japan (12), the USA (12), Italy (2), Germany (6), Switzerland (1), Austria (1), Sweden (1) and France (3). The UK lags behind this level of implementation with only one ‘low energy’ centre, the Clatterbridge Centre for Oncology, which uses proton therapy to treat eye tumours (see picture above). Although long term medical and cost effectiveness is unknown, early results indicate that particle therapies provide at least a similar treatment outcome to conventional radiotherapy, and have fewer side effects. Experts suggest that if the UK wishes to form part of the international effort to evaluate and optimise the procedure, either one large centre or 3-4 smaller centres need to be set up. These would be able to offer treatments as part of randomised clinical trials, which would compare the new therapies with standard radiotherapy. Each treatment centre would need its own cyclotron or synchrotron. To offset the initial cost of these accelerators, they could be used overnight to produce radioactive isotopes for nuclear medicine treatments and diagnosis, or to test satellite components by simulating the effects of cosmic radiation. In addition, medical physicists and clinicians need education and training in order to identify and refer suitable patients abroad for particle treatments, and potentially to UK centres in the future. 29/01/2008 21:07:40 05 Institute of Physics and Engineering in Medicine Perspectives on: physics and engineering in medicine and biology Siemens press picture Synchrotron (Particles up to 70% of light speed) Ion Source Carbon Scanning System Online Monitoring Monitor System Scanning Magnets Wire Chambers Ionization Chambers Target Volume Example Depth 5 cm: Proton 80 MeV Carbon 145 MeV/u Depth 25cm: Proton 195 MeV Carbon 375 MeV/u Radiation Control Cross-section through the irradiated tumor volume. Every section represents a different beam range. The treated elements are shown in green. Relative Dose 0 Depth The main stages involved in delivering particle beam radiotherapy. (This system can produce beams of varying energy, so does not need a modulator.) Worldwide there are five main suppliers of particle therapy equipment: Siemens, IBA, Mitsubishi, Hitachi and Varian. Perspectives is a series of publications which highlights new and emerging areas of research in physics and engineering, and discusses their application to the solution of problems in medicine and biology. Acknowledgement Much of the information in this perspective was kindly provided by Professor Bleddyn Jones and Dr Stuart Green (Birmingham Cancer Centre, University Hospital NHS Foundation Trust, Birmingham), Dr Hugo Palmans (National Physical Laboratory), and Dr Andrzej Kacperek (Clatterbridge Centre for Oncology NHS Foundation Trust, Wirral). Institute of Physics and Engineering in Medicine Fairmount House 230 Tadcaster Road York YO24 1ES United Kingdom Spotlight5.indd 4 Enquiries: Tel: +44 (0)1904 610821 Fax: +44 (0)1904 612279 office@ipem.ac.uk www.ipem.ac.uk Editor: Dr Sharon Ann Holgate, Design: Louise Southwell, © Institute of Physics and Engineering in Medicine. Cover photographs PSI, Villigen, Switzerland. Linear Accelerator Ion Source Proton 29/01/2008 21:07:42