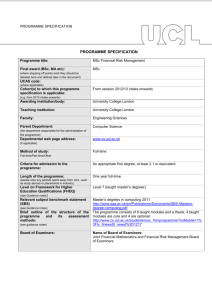
SIFT Annual Report 2012/13 UCL Medical School 1
advertisement

SIFT Annual Report 2012/13 UCL Medical School 1 2 University College London (UCL) Medical School is committed to excellence in education and has a strong reputation for teaching informed by cutting-edge research. The School has a distinguished cadre of academic staff who are at the forefront of international research in medical sciences and clinical medicine. UCL Medical School is one of the largest in the country with a total yearly intake of c.380 (c.330 in Year 1 and an additional 55 joining Year 4) undergraduate students on the MBBS programme and it has the widest range of intercalated BSc opportunities in the UK. The Medical School also offers postgraduate programmes and clinical training. UCL is London’s top ranked medical school according to the National Student Survey with an overall satisfaction of 94%. UCL Medicine graduates had an employment rate of 100% in the Foundation Programme for 2012. UCL Medical School is situated in the heart of London at three main campuses; the Bloomsbury campus, the Royal Free campus, and the Whittington campus; all with clinical facilities, teaching laboratories, lecture theatres, and libraries. We also work with a number of District General Hospitals (DGH), numerous mental health partners and over 200 GP practices. This infrastructure along with a dedicated team of internationally acknowledged world leaders and highly trained technical staff provides the ideal intellectual learning environment for medical students. Staff research activities, directed towards patient-centred outcomes, are supported by partnerships with NHS trusts. Several world famous clinical and research institutions are closely associated with the Medical School. UCL Partners, one of the first academic health science centres, was set up during 2009/10. There are 2 Higher Education Institutions and 5 NHS Trusts in its Academic Health Science Centre Partnership and 11 Higher Education Institutions and 24 NHS Trusts in its Academic Health Science Network Partnership. It works to translate cutting edge research and innovation into measureable health and wealth gain for patients and populations – in London, across the UK and globally. Status of this report This report has been prepared for the sole use by HE London, and no responsibility is taken by the Medical School to any director / member or officer in their individual capacity, or to any third party. 3 Contents Summary 3 Introduction 5 Detailed Report A. Student number time series information to highlight future bulge and fallow intakes 6 Student population as at 1 December 2012 6 Forecast for Autumn 2013 intake 7 Number of qualifiers in summer 2012 7 B. Summary of SIFT expenditure against budget 8 C. Reporting of quality assurance exercises 11 QA of Clinical Placement Providers 11 QA of the Medical School 17 D. Summary of developments, innovations, best practice to include significant future changes to the curriculum or any other important achievements Developments, innovations and best practice 18 Appendix 1 – Medical School governance – organograms Appendix 2 – Medical School governance – booklets 4 21 27 Introduction The Medical School is required to complete and return an annual report to Health Education London on the following MBBS (Bachelor of Medicine and Bachelor of Surgery degree) items: student numbers: totals for the preceding year, 2012/13; forecasts for the following year, 2013/14; and qualifier totals; summary of Undergraduate Tariff expenditure against budgets; quality assurance exercises; and developments, innovations, and best practice. This is the sixth annual report that has been prepared by the Medical School SIFT Office and the Quality Assurance Unit (QAU). It provides a summary of relevant Medical School data, with some discussion of strengths and weaknesses, and has an emphasis on areas we consider to be examples of good practice. The period this report covers (April 2012 – March 2013) has again been characterised by on-going uncertainties regarding the service landscape but it has also seen the introduction of the new Undergraduate Tariff, replacing SIFT and leading to significant funding changes for some trusts. The UCL MBBS Curriculum Review moved into its second phase of piloting and implementation with the introduction of New Year 4 and several new vertical spine courses. The General Medical Council (GMC) carried out a full QABME (Quality Assurance of Basic Education) visit in November 2012, as well as requiring the completion of a complex Annual Return. Once again, the increased scrutiny of the MBBS had a significant impact on the activities of the MBBS executive, the SIFT Office and the QAU. It is recommended that the Medical School be closely involved in the development of the new regulatory arrangements that come with commissioning and the additional requirements of the GMC. 5 6 8 C. Reporting of quality assurance exercises QA of Clinical Placement Providers i. Executive summary of the Medical School’s QA of Clinical Placement Providers in 2012/13 Quality Assurance Unit The purpose of the Quality Assurance Unit (QAU) is to ensure that high standards within teaching and learning processes for undergraduate medical programmes are recognised and rewarded, and problems identified and addressed. The Unit has oversight of all quality assurance and enhancement of the MBBS programme, including clinical placements. It was established in 2006 in response to recommendations made by the GMC, recognising that the area of quality assurance was not adequately resourced within the Medical School. The QAU employs a range of strategies to create a picture of the students’ educational experience across the whole curriculum. The QAU works in conjunction with the SIFT Office to ensure financial accountability. The site visit programme has changed over the recent years to involve ‘light touch visits’ visits in response to issues about serious concerns and a remote, self-assessment process for trusts was piloted, the analysis of which will be carried out during the coming academic year. The GMC visited the medical school in 2012. The New Curriculum (from September 2012) and simultaneous changes to organisational structures and management roles, plus the continued rise in regulatory demands has played a significant part and prompted a review of on-site quality assurance scrutiny. Student Feedback The QAU gathers feedback from students throughout the programme using a bespoke, on-line student evaluation questionnaire for each module. Data can be analysed by module and NHS site or GP practice. Trust QA visits – summary The QAU workload has expanded; in particular the mandatory QA reporting processes, and the resources associated with the historic visiting procedures was viewed as excessive. The GMC encourage a process of self-evaluation for both medical schools and providers of clinical placements. The Medical School considered a number of possible strategies and decided, prior to a formal review of QA planned for 2013 -2014, to follow a structure similar to that of the GMC; an annual, selfassessment exercise by trusts, triangulated with online student feedback and focused visits. Informal visits to some of the DGH education providers have been conducted by the Final Year lead, which include discussion of feedback on fourth year placements and resources. (see below, section ii.) The aims of these visits are to: share developments and review feedback ensure the quality of educational provision meets the requirements laid out in the Learning & Development Agreement, Tomorrow’s Doctors 2009, QABME report and any other guidelines issued by the School, the GMC, the SHA, College and the QAA; promote good relations with the Trust through dialogue, feedback, and support share good practice 9 ii. Description of the process used The light touch visits have been carried out by the Final Year Lead and team. These visits aimed to offer support to our NHS partners and maintain good relations. They followed a standard structure: meeting students to gather feedback, followed by a meeting with the Undergraduate Tutor, key clinical teachers and administrative staff. The Medical School Librarian and Academic Support Manager attended these meetings, and carried out a comprehensive review of library and IT resources. During 2012-13, and following the GMC’s QABME processes, the QAU piloted a Medical Education Providers’ Annual Return (MEPAR), a self-evaluation tool. The results of this pilot are being collated and analysis carried out. Initial findings indicate that the DGHs are meeting the required standards in teaching and supporting our students. Much of the information gathered has been useful in identifying areas of good practice and/or concern. Any shortcomings in the design of the MEPAR will be ironed out and it is anticipated that a new version will be circulated later this year. A Quality Assurance Project Officer has been employed to carry out a full review of the School’s QA processes including the MEPAR during 2013-14. Table 5 Overview of status of site visits and reviews of hospital trust (at July 2013) Site Date last visited Type of visit Comment Barnet December 2012 Focused Joint with Chase Farm Chase Farm December 2012 Focused Joint with Barnet Lister March 2013 Focused Extended = continuation of the Trust Undergraduate Teaching Committee led by the QA SIFT team Focused = final year with limited review of fourth year 10 iii. Strengths and areas in need of improvement in each trust visited Trust visited Strengths Areas in need of improvement Barnet and Chase Farm Barnet & Chase Farm are having difficulties due to the reorganisation of services. They are centralising on the Barnet site and coping as best they can. Barnet: Friendly, enthusiastic teachers Chase Farm: Numerous opportunities to present cases to senior doctors for feedback. Barnet & Chase Farm: Accommodation is no longer offered by this Trust With all East & North Herts NHS Trust undergraduates placements occurring at the Lister site, levels of overall student satisfaction have improved (particularly the pharmacy teaching). There is a good balance of lecture-based teaching and consultant-led, ward teaching The Trust provided the students with ‘dongles’ for accessing the internet and there were some problems with data allowance and speed when streaming information from the UCL Moodle site, etc.. Plans to provide WiFi in the accommodation are on course. Students requested an increase in registrar and/or consultant bedside teaching Lister North Middlesex North Middlesex has used some SIFT money to create undergraduate leads in the major areas and is investing in new educational facilities as part of its expansion. Excellent FY1 teaching 11 Barnet: More registrar / consultant bedside teaching Chase Farm: Some nominated teaching leads were unavailable to students. iv. Strengths / Areas in need of improvement for each Trust not visited The following information is derived from the information provided by the sites in combination with online student feedback for sites not visited since the last SIFT Annual Report was submitted. Table 7 Trust / date of last visit Basildon Strengths / Areas in need of improvement for each Trust Strengths Areas in need of improvement Excellent teaching from FY1s and FY2s. Some clinics were overcrowded Students appreciate the numerous opportunities to speak to patients unsupervised. Great quantity and quality of teaching. All professionals keen for students to get involved on the wards. Good opportunities for exposure to a variety of patients. Some bedside teaching groups were too large Royal Free 02/2012 Friendly staff. Plenty of bedside teaching. Organisation and administration excellent. MAU, vascular surgery and renal teaching highly praised by students. Overcrowding in dermatology clinics. Teaching cancellations and timetable clashes reported between clinical placements and tutorials. UCLH 20/10/2009 Positive student feedback. Good mix of seminars, clinics and ward-based teaching. Great clinical involvement. Excellent consultant- and registrar-led teaching and clinical exposure within specialties. Friendly staff and encouraging consultants, registrars and juniors. Good administration. Luton and Dunstable Watford Whittington 23/07/2009 Good organisation, friendly staff. Plenty of specialised teaching. High quality teaching by consultants/registrars/SpRs. Excellent clinical exposure within specialties. 12 Teaching cancellations reported in Neurology teaching. Some teaching cancellations and timetable clashes. No student common room. Internet facilities in the accommodation would be an invaluable addition More consultant-led bedside teaching More flexible approach from the administration team Minimal exposure to renal teaching. v. Common issues / Good practice As part of its review and reporting activities the QAU generates an annual summary of good practice which will be made available on the website. Table 8 1 Common issues / Good practice Site Subject/Department Good practice Barnet Hospital Lister hospital Final Year placements 3 Mock OSCE’s well received by students. Final Year placements Excellent pharmacology and pharmacy teaching by both Clinical Pharmacologists and Pharmacists. Teaching is structured and well organised and delivered (6x3hr sessions) and small group teaching. North Middlesex Hospital Year 5 and Final Year placements Sustained involvement and commitment from a lead consultant who contributes to all stages of the assessment process. UCL, Division of Medicine and Division of Surgery & Interventional Science VM Teaching Proactively seeks to improve curriculum delivery and quality of teaching using an in-house student feedback evaluation process. Actively developed therapeutics teaching across the MBBS programme. Examples include the introduction of the Integrated Medical Course and the introduction of therapeutics tutorials for Year 4 students (in 1 collaboration with UCL MedSoc ). This entails observation of clinical procedures/examinations followed by oral feedback and written feedback on the online student portfolio. Students have opportunities to convey any concerns they may have about their own performance or the assessment itself. At the end of each topic in the IMS the lead writes several single best answer scenarios of varying difficulty for the students. Whenever possible voting software is used with the aim of improving student involvement. MedSoc is run by UCL medical students. It organises events and activities across a number of sections from Global Medicine to Medical Leadership, General Practice and Public Health to Orthopaedics 13 UCLMS Medical Education The Patient and Public Involvement (PPI) in Medical Education project: Qualitative research seeking the lay perspective on how to engage the public. This project has approved a PPI framework to develop and promote this. The framework seeks to ensure that PPI is enshrined in all aspects of the Medical School, from representation in curriculum development and governance, in teaching and assessment and by joint working with other organisation involved in this field. Details can be found on the QAU website: http://www.ucl.ac.uk/medicalschool/quality/monitoring/ppi/ppi_medical_education Introduction of Lecture-casting and e-portfolio Implementation of Standards for IT and WiFi Access on Clinical Placements across DGHs 14 QA of the Medical School i.GMC: Review & Medical Schools Annual Return (MSAR) 2012-13 In 2012-13, as well as providing the MSAR, UCLMS was part of the GMC's regional review of London. The visit took place in November 2012 and the final reports are published on the QA website. Several areas of good practice were identified and no serious concerns were reported. The aim of the MSAR 2012/13 was to enable schools to revise the self-assessment of the status of its compliance, update cohort data (such as student demographics, fitness to practise and progression data) and to provide information on progress made in the last year. This return marked the signing off of all action points stemming from the 2004/5 Change Management Plan. All medical schools in the UK were again required to submit an Annual Return in December 2012. The General Medical Council has the statutory responsibility to set standards for basic medical education and to ensure that these standards are met. iii. Description of the internal governance processes of the Medical School The MBBS programme is managed through UCL Medical School, which is responsible for the leadership of MBBS educational strategy; curriculum development and planning; assessment policy and organisation; the setting and monitoring of standards and quality assurance; and for the MBBS Student Load Exercise and SIFT allocations. MBBS leadership roles within UCL Medical School include MBBS Sub Deans, Site Sub Deans and Student Support Tutors, each with responsibility for specific areas of MBBS management. Administrative support is provided by Medical Student Administration. MBBS teaching is commissioned from the School of Life and Medical Sciences (SLMS) divisions and funded through HEFCEt and tuition fee income. Faculties and divisions are responsible for managing local delivery of teaching in accordance with UCL Medical School guidance, and for appointing MBBS module and assessment leads to manage the delivery of education within the Division. Administrative support for Faculty and Divisional roles is provided by Faculty and Divisional Teaching Administrators. SLMS faculties and divisions are responsible for co-ordinating and supporting teaching delivery by NHS colleagues, and for ensuring consistency of teaching and assessment across Hospital Trusts and PCTs. Teaching provided by trusts is funded through SIFT. Administrative support is provided by divisional Teaching Administrators and/or trust administrators. Implementation of the new curriculum (NC) began at the start of the 2012-13 academic year. Integral to this process was the review of the School’s governance structures which have been adjusted to fit and support the NC properly. The new organisational structures and management roles for the MBBS programme can be seen clearly via the organograms in Appendix 1. Appendix 2 contains the booklets which explain the structures are subject to updates, final review and approval. 15 D. Summary of developments, innovations, best practice to include significant future changes to the curriculum or any other important achievements UCL Medical School (UCLMS) is a recognised international centre of excellence for medical education and education scholarship in both the undergraduate and postgraduate arenas. UCLMS has been the top scoring medical school in London in the UK’s National Student Survey for the last 4 years. th We have the 4 highest student satisfaction score in the UK, with 94% overall medical student satisfaction. We deliver a six year MBBS programme fully compliant with the UK’s General Medical Council document Tomorrow’s Doctors 2009, graduating approximately 400 doctors per year. Our MBBS 2012 curriculum was launched in all years of the programme in 2012 and was quality assured by the GMC in 2012/13 and so the last academic year has been a year of multidimensional change in the MBBS programme with change extending to governance structures, organisation, content, mode and venue of delivery and anticipated outcomes. These changes have included: The introduction to more rigorous formative assessments in the early years including the introduction of formative OSCE examinations The introduction of Introduction and Orientation Modules in all years to introduce students to the main themes of the year, how learning and assessment is organised and to plan the learning approach Introduction of integrated modules in year 4 better aligned to patient journeys through the healthcare system rather than to specialties more extensive development of vertical modules with learning in some areas such as mental health and anatomy and imaging extended of all years of the course and other key areas such as social determinants of health, safety and quality improvement and health informatics introduced Following a successful pilot in the previous academic year the introduction of an authentic professional e-portfolio based on the Foundation School portfolio, developed and supported by NES to all students in years 4 and 5 A re-organisation of the final year to allow an earlier sitting of finals with an opportunity for an in year re-sit. This has required the introduction of an innovative post finals student selected component (SSC) for four weeks tailored around preparation for practice In line with UCL requirements a more sustained and regular relationship with personal tutors A significant increase in the use of e-learning environments and technologies including the use of the Moodle VLE to consistently support all modules, the use of Videocapture technology for the vast majority of plenary sessions, the expansion of the interactive Case of the Month on line learning activity and the introduction of Q@UCLMS, a twitter based interactive case discussion The adoption of NHS Change day and the ‘ask one question’ approach across the whole school to encourage mindfulness of patient agendas and quality improvement Major priorities over the next year are to continue to embed and evaluate these new curriculum changes and to continue to implement the changes needed to support this new curricular approach both structurally and pedagogically. Anticipated changes for 2013/14 therefore include: Introduction of new Consolidation, Integration and feedback weeks into years 1 and 2 Extending the use of the NES e-portfolio to students in year 6 in 2013/14 Introduction of integrated modules in year 5 more aligned to the life-cycle than to specialties including the introduction of men’s health, extending teaching in palliative care and a new patient pathway in ‘Mother and Baby’ Further changes to the final year with the view to moving finals from its current position in early summer to Easter Improving the robustness of student support systems, both at the teacher/learner interface and at the medical school level 16 Improving teacher training in the domain of assessment and feedback Adapting the long running and highly successful student psychotherapy scheme into a longitudinal SSC to secure stable funding Extension of Case of the Month into year 5 Introduction of M learning via a pilot in the Royal Free campus, equipping learners with loaned tablet devices and appropriate software including e-textbooks to improve work-based learning and assessment A number of features of the new curriculum and running a fit for purpose contemporary medical school make extra demands on the current healthcare learning landscape and funding arrangements and are highlighted here for consideration: As the curriculum becomes more integrated it is difficult to allocate funding accurately to university discipline based departments and NHS speciality based groupings Rapid changes in the Healthcare landscape makes planning a placements-based curriculum for a large number of students difficult; of particular concern are impending changes to A&E departments and to providers in Barnet and Chase Farm and planned pan London changes in cardiology healthcare The increased use of the private and charity sector in areas such as women’s health and mental health and in services in palliative care means funding to private providers needs to be acknowledged as an approved use of SIFT funding The provision for each student of a clinician as a personal tutor for the last 3 years of the programme and the increased adoption of the portfolio and accompanying structured learning events (SLEs) places additional demands on NHS staff involved in delivery of the programme increasing reliance on high quality, accessible IT resources in Trust including student access to patient e-health records Funding of costs associated with running a complex , integrated placements-based programme with rigorous assessment, curricular and fitness to practice demands that cannot be delivered within Trusts such as: the portfolio, some specialist professional development learning, student support, occupational health and fitness to practise procedures, development of teaching materials and course design relevant to placements, contribution to formative assessment and feedback completed on the VLE, staff development and clinical summative assessments Deborah Gill, MBBS programme lead August 2013 17 Appendices Appendix 1 – Medical School governance – organograms Appendix 2 – Medical School governance – booklets 18 21 27 UCL Medical School - MBBS 2012-13 Academic Leadership 19 1213 Organogram 2 MBBS Leadership Vertical Modules Apr 2013 20 1213 MBBS 3 MBBS Leadership Clinical Placements Nov 12 21 UCL Medical School - MBBS 2012 Faculty Tutors, Student Support and Foundation Training 22 1213 Organogram 6 MBBS Committees and Chairs Apr 13 FMS Board of Examiners Faculty Tutor (UG) P Raven MBBS Board of Examiners Assessment Lead A Sturrock Y1 Sub Board of Examiners Y1-3 Lead M Gilbey Y2 Sub Board of Examiners Y1-3 Lead M Gilbey Y3/IBSc Sub Board of Examiners Dr B Cross Y4 Sub Board of Examiners Y4-6 Lead D Gill Y5 Sub Board of Examiners Y4-6 Lead D Gill Y6 Sub Board of Examiners Y1 Panel of Examiners Y2 Panel of Examiners IBSc Panels of Examiners Y4 Panel of Examiners Y5 Panel of Examiners Y1 Lead P Dilworth Y2 Lead L Ginsberg in Faculties in which programmes are registered Y4 Lead J McEwan Y5 Lead J Cartledge Y6 Panel of Examiners Assessment Lead A Sturrock Director of UCLMS J Dacre Y1 Standard Setting & Sub Panel (Clinical) Y1 Deputy Lead T Debnam Y2 Standard Setting & Sub Panel (Clinical) Y2 Deputy Lead K Woolf Y4 Standard Setting & Sub Panel (Clinical) Y4 Deputy Lead A Salama Y5 Standard Setting & Sub Panel (Clinical) Y5 Deputy Lead W Coppola Y6 Standard Setting & Sub Panel (Clinical) Y6 Lead A Lal 3 x OSCE Site Leads 3 x OSCE Site Leads RF OSCE Site Lead RF OSCE Site Lead Basildon OSCE Site Lead CTFs CTFs Module A Nominee CN Module Lead C Turner Site Sub Dean A Lal Whittington OSCE Site Lead Luton OSCE Site Lead UCLH OSCE Site Lead Module B Nominee Whittington OSCE Site Lead WHCD Module Lead M Whitten UG Tutor P Vetpillai Site Sub Dean J McEwan UCLH OSCE Site Lead UCLH OSCE Site Lead Module C Nominee CFHD Module Lead E Chung 23 RF OSCE Site Lead Site Sub Dean P Dilworth Whittington OSCE Site Lead Site Sub Dean C Fertleman UCL Medical School – MBBS 2012 Committees and Chairs 24 APPENDIX 2: BOOKLETS UCL Medical School MBBS Leadership Academic OVERVIEW OF LEADERSHIP AND MANAGEMENT ..........................................................................26 MBBS LEADERSHIP TEAM ............................................................................................................27 Director of UCL Medical School .........................................................................................27 Deputy Director of UCL Medical School/Lead for Undergraduate Programmes .....................27 MBBS leads years 1-3 and 4-6 ...........................................................................................28 Academic Lead (Assessment) ............................................................................................28 Academic Lead (Quality Assurance)...................................................................................29 Academic Lead (Vertical Modules) ....................................................................................30 MBBS SENIOR DELIVERY TEAM – YEAR AND MODULE LEADS AND SPECIALTY TEACHING LEADS.......30 MBBS Year Leads and Deputy Year Leads ..........................................................................30 MBBS Year Lead for Integrated BScs (Year 3) .....................................................................31 MBBS Module Leads.........................................................................................................33 MBBS Specialty Teaching Leads ........................................................................................34 MBPhD PROGRAMME.................................................................................................................35 Academic Lead (MBPhD) ..................................................................................................35 UCL DIVISIONAL UNDERGRADUATE EDUCATION TUTORS ..............................................................35 For organisational charts see: http://www.ucl.ac.uk/medicalschool/staff-students/committees 25 OVERVIEW OF LEADERSHIP AND MANAGEMENT UCL Medical School is responsible for the strategic direction and management of the MBBS programme which draws on academic leadership and operational oversight commissioned from the SLMS Faculties of Life Sciences, Brain Sciences, Medical Sciences and Population Health Sciences and from Central and Associated Provider Trusts, and clinical training commissioned from Central and Associated Provider Trusts. Within UCL Medical School: the MBBS Leadership Team is responsible for the strategic direction and development of the MBBS programme, for developing the national and international standing of UCL Medical School and for overseeing the innovation and management of all aspects of the undergraduate activity of the Medical School including: curriculum development, planning and innovation; assessment policy and organisation; commissioning of clinical placements; the setting and monitoring of standards and quality assurance; and the Student Load Exercise and SIFT allocations. Within SLMS Faculties and Central Provider Trusts: MBBS Senior Delivery Team is responsible for the academic and operational oversight of each year of the programme and the vertical modules running through the programme. Module Leads are responsible for academic and operational oversight of local delivery of teaching and providing appropriate assessment materials within their module in Years 1 and 2 and within their module and across 3 sites in Years 4 and 5. Specialty Leads are responsible for academic and operational oversight of specialty teaching and assessment within modules and across 3 sites in Years 4 and 5. 26 MBBS LEADERSHIP TEAM Director of UCL Medical School 6 notional PAs: UCLMS Administrative support: Division of UCLMS and Medical Student Administration Reporting to: Vice Provost Health and Dean of FMS Remit: Education strategy, policy and development Oversight of delivery of the MBBS degree programme Development and embedding of relationships with Faculties, Divisions and Trusts to encourage their contribution to undergraduate education Development and oversight of transparent and robust financial agreements for the delivery of undergraduate education (with SIFT and Student Load funded units) Embedding of quality assurance, quality control and audit of educational activity including mechanisms to relate estimated protected time to the quality and quantity of educational activity Liaison with Faculty and Medical Student Support Tutors Committees: o Chair of UCL Medical School Executive Committee o Chair of MBBS Teaching Committee o Chair of MBBS Board of Examiners o Member of MBBS Executive Committee o Member of FMS Teaching Committee and FMS Exam Board Deputy Director of UCL Medical School/Lead for Undergraduate Programmes 4 notional PAs, UCLMS Administrative support from Medical Student Administration Accountable to: Director of UCL Medical School Term of office: normally 5 years, renewable Deputise for director as required Provide support to director for strategic direction and development of undergraduate programme To further develop the national and international standing of UCL medical School oto embed a culture of excellence and innovation into undergraduate medical education, research and scholarship oTo encourage a culture of scholarship, research and publication in the undergraduate programmes oto develop a robust approach to scholarship within medical education oto ensure mechanism for knowledge transfer and outreach oto develop and embed relationships with internal and external collaborators oto further develop quality assurance, quality control and audit of educational, research and scholarship activities within the undergraduate activities of the medical school To oversee the innovation and management of all aspects of the undergraduate activity of the Medical School oOversight and strategic direction of senior delivery team and to chair relevant MBBS committees oRepresenting the undergraduate programmes on UCL committees where necessary oLiaison with faculty tutors and faculty vice dean for education oEnsuring the provision of high quality medical education oEnsuring that the undergraduate programme keeps pace with the evolving role of the doctor in the health care system Committees: oMember of UCL Medical School Executive Committee oChair of MBBS Executive Committee oMember of MBBS Teaching Committee 27 oMember of MBBS Board of Examiners oMember of FMS Teaching Committee and FMS Exam Board MBBS leads years 1-3 and 4-6 2 notional PAs: UCLMS Administrative support: Medical Student Administration Accountable to: Director of UCL Medical School via the Deputy Director /Lead for Undergraduate programmes Appointed by: Director of UCL Medical School in liaison with Deputy Director Term of Office: normally 5 years, renewable Deputise for Lead for Undergraduate programmes as required Provide support to Lead for Undergraduate programmes for strategic direction and development of undergraduate programme in relevant years To provide support to Lead for Undergraduate programmes for their role in oembedding a culture of excellence and innovation into undergraduate medical education, research and scholarship in the relevant years odeveloping and embedding relationships with internal and external collaborators To provide support to Lead for Undergraduate programmes in overseeing the innovation and management of all aspects of the undergraduate activity of the Medical School within To provide strategic leadership to the relevant year leads in their role in oensuring good quality teaching and support of learning in their year oassessment design and delivery ocoordination of QA of activities oLiaison with vertical modules leads Committees: oMember of MBBS Executive Committee oMember of relevant Teaching Committees oChair of relevant Examination Boards Academic Lead (Assessment) 2 notional PAs: UCLMS Administrative support: Medical Student Administration Accountable to: Deputy Director /Lead for Undergraduate programmes in liaison with the Director of UCL Medical School Appointed by: Director of UCL Medical School in liaison with Deputy Director Term of office: normally 5 years, renewable Remit: Overall responsibility for MBBS assessments Ensure compliance with MBBS assessment strategy and policy throughout the MBBS programme Oversee the implementation of MBBS assessments throughout the MBBS programme Responsibilities To set an appropriate assessment agenda To ensure that the decisions of the UCL Medical School Teaching Committee and MBBS Board of Examiners are implemented via the Year Boards/Panels of Examiners To liaise with Chairs of Year Boards of Examiners to ensure effective delivery of the assessments To liaise with Medical Student Administration (MSA) staff to ensure effective delivery of the MBBS assessments To review external examiners’ reports and to report annually to UCL on behalf of the Vice Dean/Vice Dean (Education) 28 To produce papers and working documents particularly in conjunction with ACME to further develop and improve medical assessments. To work with ACME concerning the implementation of assessment innovations. Committees: Member of UCL Medical School Executive Committee Member of MBBS Teaching Committee and relevant Sub Committees Deputy Chair of MBBS Board of Examiners Member of relevant Sub Boards and Panels of Examiners Academic Lead (Quality Assurance) 2 notional PAs: UCLMS Administrative support: Medical Student Administration Accountable to: Accountable to: Director of UCL Medical School via the Deputy Director /Lead for Undergraduate programmes Appointed by: Director of UCL Medical School in liaison with Deputy Director Term of office: normally 5 years, renewable Remit: To co-ordinate quality management and enhancement in the MBBS programme Responsibilities: To oversee academic standards and quality assurance and enhancement processes within the medical school To development of policy and practice in relation to such processes To monitor the activities of the Quality Assurance Agency for Higher Education and of other external bodies concerned with the assurance of quality and/or standards insofar as they impinge on the medical school and to advise the Director of UCL Medical School and Faculty and MBBS Committees accordingly. To promote the development at Faculty and Divisional levels of initiatives relating to quality enhancement and the enhancement of academic standards. To be responsible for the planning of the preparatory work involved in Internal Quality Audits of the medical school carried out under the auspices of University College London’s Internal Quality Review procedure. To plan and coordinate the work of the medical school in preparing for any “discipline audit trails” carried out by the Quality Assurance Agency in the course of Institutional Review that may involve the medical school. To plan and coordinate the work of the medical school in preparing for formal and informal visits by the education committees of the General Medical Council or other validating professional bodies. To promote discussion and sharing of good practice between the departments of the medical school in relation to quality assurance and enhancement. To review and oversee all QA in DGHs and Primary Care attachments To ensure delivery and review of student feedback evaluation questionnaires To submit to the Director of UCL Medical School and to FMS Teaching Committee regular reports in the form of minutes of the QMEC. To submit to the Faculty Board of Medical Sciences and to the College’s QMEC an annual report of the work of the QMEC in the MBBS Administer the Excellence in Medical Education awards Administer the Targeted Education Development and Intervention fund in line with identified QA priorities In liaison with the SIFT Office, to submit an annual report to the strategic health authority To generate research papers relating to student feedback 29 Committees: Member of MBBS Executive Committee Chair of the Quality Management and Enhancement Committee Member of MBBS Teaching Committee and relevant Sub Committees Member of MBBS Examination Board and relevant Sub Boards and Panels Academic Lead (Vertical Modules) 2 notional PAs: UCLMS Administrative support: Medical Student Administration Accountable to: Director of UCL Medical School via the Deputy Director /Lead for Undergraduate programmes Appointed by: Director of UCL Medical School in liaison with Deputy Director Term of office: normally 5 years, renewable Curriculum: Responsible for the strategic development of all VM teaching in the MBBS Supervision and support of all vertical modules activity including troubleshooting and responding to student feedback Responsibility for overseeing the recruitment, management and training of the Visiting VM tutors Ensure all VM course materials & learning resources including Moodle, are consistent with VM wide and MBBS wide strategy liaison with all relevant horizontal modules Committees: o Member of MBBS Executive Committee o Member of MBBS Teaching Committee and relevant Sub Committees o Member of MBBS Examination Board and relevant Sub Boards and Panels o Member of mQMEC o Chair of the Vertical Modules Teaching Committee o Member of relevant Vertical Modules Teaching Sub Committees Assessment: Ensure assessment design and delivery for progression tests and formative assessments Exam Boards: oMember of MBBS Board of Examiners oMember of relevant Sub Boards, Panels and Sub Panels of Examiners Quality Assurance: QA of VM activities MBBS SENIOR DELIVERY TEAM – YEAR AND MODULE LEADS AND SPECIALTY TEACHING LEADS MBBS Year Leads and Deputy Year Leads Academic Lead: 2 notional PAs: Division or Trust within overall PAs Administrative support: Medical Student Administration Accountable to: Academic Lead for Years 1-3 or 4-6 in liaison with the Deputy Director of UCLMS/MBBS Programme Lead Appointed by: MBBS Leads in liaison with Divisional Directors/Trust Executives Term of office: normally 5 years, renewable Year Leads may appoint Deputy Year Leads (1 notional PA) to assist with operational aspects of assessment and curriculum delivery Curriculum: 30 Deputize for Leads for Years 1-3 or 4-6 as required Responsible for all horizontal modules in named year including Introductory and Orientation Modules/intermodule weeks and core teaching weeks Ensuring good quality course materials delivery including Moodle Liaison with all vertical modules leads delivered in that year Committees: o Chair of relevant Teaching Sub Committees oMember of MBBS Teaching Committee Assessment: Ensuring assessment design and delivery for progression tests and formative assessments including: ooperational oversight of formative and summative assessments odeveloping question banks o compiling and editing papers o overseeing marking processes and the production of mark sheets and results ooverseeing standard setting osite lead for practical/clinical assessments (Years 2,4,5) oreceiving , acting on and reporting annually on comments from external examiners on the standard, conduct and outcome of examinations omaking recommendations for the award of prizes Exam Boards: oChair of relevant Examination Panels, Sub Panels and Standard Setting Groups oMember of MBBS Board of Examiners Quality Assurance: Coordination, monitoring and reporting annually on QA of activities in that year MBBS Year Lead for Integrated BScs (Year 3) 2 notional PAs: Division or Trust within overall PAs Administrative support: Medical Student Administration – Year 3/IBSc Assistant Administrator Accountable to: Academic Lead for Years 1-3 in liaison with the Deputy Director of UCLMS/MBBS Programme Lead Appointed by: MBBS Leads in liaison with Divisional Directors/Trust Executives Term of office: normally 5 years, renewable Year Leads may appoint a Deputy Year Lead (1 notional PA) to assist with operational aspects of assessment and curriculum delivery Curriculum: To oversee under the guidance of the Faculty Tutor all IBSc programmes To ensure that IBSc programmes of study are conducted in accordance with UCL regulations To co-ordinate the provision of IBScs To manage the allocation to IBSc programmes To monitor existing IBSc programmes and course unit components To consider changes to existing IBSc programme and course unit components and advise/liaise with departments regarding PAQs (Programme Amendment Questionnaires) and UPCAMs (Undergraduate Programme Component Amendment Forms). To consider new IBSc programmes and to liaise with respect to PIQs (Programme Initiation Questionnaires) and UPCs (Undergraduate Programme Component Questionnaires). To co-ordinate IBSc places and numbers To become SSCC academic lead for the Yr 3 IBSc booklet and website To participate in the IBSc SSCC To report specific issues to Teaching Committees in other Faculties providing IBScs 31 Committees: o Deputy Chair of the MBBS Year 3/IBSc Teaching Committee o Deputy Chair of MBBS Year 3/ IBSc SSCC o Member of MBBS Teaching Committee Assessment: To report specific issues to Teaching Committees in other Faculties providing IBScs To report formally, for MBBS monitoring, co-ordination and quality assurance of IBScs, to the MBBS Board of Examiners on IBSc examinations across all Faculties To report, on behalf of the MBBS, specific issues and an overall report of examinations to each Faculty which offer IBScs To work with the Faculty Tutor to develop procedures to ensure alignment with the new over arching MBBS board To oversee the outcome of the IBSc project prizes Committees: o Member of MBBS Examination Board o Member of each Faculty Board of Examiners which offer IBScs Quality Assurance: To monitor and report on quality assurance issues in IBSc programmes To comply with UCL requirements for AMR’s To attend the relevant exam related committees To receive student feedback questionnaires and to address generic issues relating to IBSc degrees To receive and monitor reports of internal quality audits and subject reviews, and to respond to any generic issues relating to IBSc degrees Participate in internal and external quality reviews Committees: o Member of mQMEC Additional Duties: Attendance at the IBSc fair Attendance at the IBSc graduation ceremonies To lead on the implementation of the UCL Personal tutor scheme for IBSc students. IBSc’s for non-UCL students To explore and develop a programme of IBSc’s for students external to UCL The Faculty Tutor has responsibility for: Curriculum: Overall planning and negotiation of student numbers with UCL Approving changes to existing IBSc programme and course unit components and approving PAQs (Programme Amendment Questionnaires) and UPCAMs (Undergraduate Programme Component Amendment Forms) Approving new IBSc programmes and PIQs (Programme Initiation Questionnaires) and UPCs (Undergraduate Programme Component Questionnaires) Formal reporting to the FMS Teaching Committee Committees: o Chair of the MBBS Year 3/IBSc Teaching Committee o Chair of the MBBS Year 3/IBSc SSCC o Member of MBBS Teaching Committee 32 Assessment: Formal reporting to FMS Board of Examiners Ensuring appropriate response and action to external examiners’ reports Exam Boards: o Chair of the MBBS Year 3/IBSc Examination Board o Member of MBBS Examination Board o Member of each Faculty Board of Examiners which offer IBScs Quality Assurance: Overseeing quality assurance issues in IBSc programmes Committees: o Member of mQMEC MBBS Module Leads 2 notional PAs – Divisional Student Load/Trust SIFT within overall PAs Admin support: Divisions/Trusts Accountable to: Academic Leads for Years 1-3 and 4-6 via the MBBS Year Leads Appointed by: Divisional Directors/Trust Executives in liaison with MBBS Leads Term of office: normally 5 years, renewable Module leads must hold a substantive or an honorary contract with UCL Curriculum: Academic and operational oversight of module teaching To co-ordinate, manage and implement module teaching and timetabling To develop teaching materials including on-line resources and e-learning To participate in curriculum review and implement curriculum development To implement curriculum changes as directed by MBBS Teaching Committee To ensure that the teaching students receive is compatible with the core curriculum To co-ordinate appropriate introduction/core teaching weeks To work with Site Sub Deans and Lead Clinical Teachers/Lead Specialty Teachers to ensure that each clinical firm across the main campuses and DGHs has a nominated Firm Tutor (Years 4-6) To work with clinical, specialty and firm leads and teachers to ensure consistency of teaching across firms and sites To work with Site Sub Deans and Lead Clinical Teachers/Lead Specialty Teachers to ensure that Firm Tutors perform the duties listed in their remit To liaise with Directors of Divisions and/or Divisional Undergraduate Tutors to ensure the appropriate allocation to the MBBS programme of Student Load funded resources Assessment: To co-ordinate in-course assessments, workplace based assessments, module/firm assessments To participate in writing and reviewing assessment materials To participate in standard setting To work with the Year Lead and Module Management Group to ensure the provision of high quality assessment materials from module and firm teachers for formative and summative written, practical and clinical examinations To work with the Year lead and Module Management Group to ensure participation by module and firm teachers in standard setting processes and clinical examinations In Years 4 and 5, to act as Site Lead for the summative clinical examinations Quality Assurance: To act upon student module feedback and report annually to QA To act upon external examiner’s comments and report annually to QA 33 Committees: Chair of Module Management Group Member of MBBS Teaching Committee Member of relevant Year Teaching Committee and Sub Committees Examination Boards: Member of relevant Year Panels and Sub Panels of Examiners Member of MBBS Board of Examiners MBBS Specialty Teaching Leads 1 notional PA – Divisional Student Load (UCL employees) or SIFT (Trust employees) within overall PA allocation Admin support: Divisions (UCL employees) or SIFT (Trust employees) Accountable to: Academic Leads for Years 1-3 and 4-6 via the MBBS Year Leads and Module Leads Appointed by: Divisional Directors/Trust Executives in liaison with MBBS Leads Term of office: normally 5 years, renewable Specialty teaching leads must hold a substantive or an honorary contract with UCL Curriculum: Academic and operational oversight of specialty teaching within modules To lead and co-ordinate specialty teaching across the MBBS programme and across teaching sites To work closely with local subject leads/clinical lead teachers in determining the curriculum for the speciality within the MBBS curriculum as a whole To review timetables and to work with local subject leads//clinical lead teachers to ensure consistency and equivalence of teaching across firms and sites To develop teaching materials including on-line resources and e-learning To participate in curriculum review and implement curriculum development To implement curriculum changes as directed by MBBS Teaching Committee To ensure that the teaching students receive is compatible with the core curriculum To co-ordinate appropriate introduction/core teaching weeks in collaboration with module leads To work with Site Sub Deans and Module Leads to ensure that each clinical firm across the main campuses and DGHs has a nominated Firm Tutor (Years 4-6) To work with clinical, specialty and firm leads and teachers to ensure consistency of teaching across firms and sites To work with Site Sub Deans and Module Leads to ensure that Firm Tutors perform the duties listed in their remit To liaise with Directors of Divisions and/or Divisional Undergraduate Tutors to ensure the appropriate allocation to the MBBS programme of Student Load funded resources Assessment: To co-ordinate in-course assessments, workplace based assessments, module/firm assessments To participate in writing and reviewing assessment materials To participate in standard setting To work with the Year Lead and Module Management Group to ensure the provision of high quality assessment materials for formative and summative written, practical and clinical examinations To work with the Year lead and Module Management Group to ensure participation by firm leads in standard setting processes and clinical examinations In Years 4 and 5, to act as Site Lead for the summative clinical examinations?? Quality Assurance: To act upon student feedback and report to QA 34 To act upon external examiner’s comments Committees: Member of relevant Module Management Groups Member of MBBS Teaching Committee Member of relevant Year Teaching Committee and Sub Committees Examination Boards: Member of relevant Year Panels and Sub Panels of Examiners Member of Year Sub Board of Examiners MBPhD PROGRAMME Academic Lead (MBPhD) 2 notional PAs – Divisional Student Load Admin support: FMS Administration/Graduate & MBPhD Administrator Accountable to: Director of UCL Medical School and the Dean of FMS Term of office: normally 5 years, renewable Remit: To manage the MBPhD Programme Committees: Chair of MBPhD Sub Committee Member of MBBS Teaching Committee Responsibilities: MBPhD Admissions and Publicity MBPhD Open day MBPhD Financial support Administration of clinical programme for students during research period Annual academic reviews with MB PhD students during research period MBPhD Web Site maintenance and development MB PhD Alumni support and liaison Annual newsletter UCL DIVISIONAL UNDERGRADUATE EDUCATION TUTORS Each Division is required by UCL to appoint a Divisional Education Tutor to manage education within the Division and to ensure compliance with Academic Services requirements by the Division. Remit: To oversee and ensure the effective operation of teaching and learning activities within the division To ensure compliance with UCL academic services requirements for teaching and for quality assurance Committees: Chair of the Divisional Undergraduate Teaching Committee Member of the Faculty Teaching Committee Member of the MBBS Teaching Committee Member of relevant MBBS Year Teaching Committees Member of relevant MBBS Module Management Groups 35 Responsibilities relating to the Faculty/Division: To contribute to the Faculty Learning and Teaching strategy To update annually the Divisional Learning and Teaching strategy incorporating elements from the MBBS Learning and Teaching strategy and to report the Divisional Learning and Teaching strategy to the relevant Graduate and Undergraduate Faculty Teaching Committee To update annually all programme specifications and report them to the relevant Graduate and Undergraduate Teaching Committee To ensure that Divisional Graduate and Undergraduate Teaching Committee meet regularly and submit minutes to the relevant Graduate and Undergraduate Faculty Teaching Committee To ensure that Student-Staff Consultant Committees meet regularly and submit minutes to the relevant Graduate and Undergraduate Faculty Teaching Committee To ensure that Divisional teaching and assessment policy comply with UCL and Faculty requirements. To ensure that Divisional quality assurance complies with UCL and Faculty requirements including the provision of annual Monitoring Reports and contribution to the MBBS AMR as appropriate To respond to IQR, SEQ and other feedback by implementing improvements in teaching To implement peer observation of teaching for all HEFCE funded staff and to submit an annual return to the relevant Graduate and Undergraduate Faculty Teaching Committee To ensure the appointment of a divisional administrative lead for teaching to co-ordinate Graduate/or Undergraduate teaching and to attend the relevant Faculty Teaching Committee To ensure provision of good quality administrative support for Graduate programmes and good quality administrative support at each campus for MBBS teaching Responsibilities relating to the MBBS programme: To ensure the implementation of the MBBS curriculum in liaison with the relevant Module Management Lead and in accordance with the MBBS Learning and Teaching Strategy, MBBS Teaching Committee, MBBS Board of Examiners, and the relevant Module Management Group To liaise with MMG leads and Directors of Divisions to ensure appropriate allocation of Student Load funded resources to the MBBS programme 36 UCL Medical School MBBS Leadership Vertical Modules Overview of Vertical Modules .....................................................................................................38 Leadership Roles.........................................................................................................................39 Academic Lead for Vertical Modules.........................................................................................39 Deputy Lead for Vertical Modules ............................................................................................39 Vertical Module leads.............................................................................................................40 Vertical Module Site leads.......................................................................................................41 Visiting Vertical Module Tutors....................................................................................................41 Person specification ................................................................................................................42 Practicalities ...........................................................................................................................43 For organisational charts see: http://www.ucl.ac.uk/medicalschool/staff-students/committees 37 Overview of Vertical Modules The vertical modules (VMs) make up almost 20% of the overall MBBS programme. Learning in the VMs is central to understanding medicine as an integrated whole. There are 11 VMs, each organised over six years: Student centred learning, patient centred learning 1.SSCs 2.Portfolio 3.Patient pathways The Integrated Vertical strands 4.Anatomy and imaging 5.Clinical skills and practical procedures 6.Pathological sciences 7.Use evidence 8.Use of medicines Overarching Themes 9.Mental health 10.Social determinants of health 11.Synthesis & professional practice The organisation of the VMs is complex, from both an administrative and academic perspective. There are 11 VMs, each organised over six years. VM teaching takes place both as centrally organised and ‘peel off’ activities in dedicated teaching sessions and activities fully integrated into the horizontal modules. Teaching methods include lectures, small groups, patient visitors, placements and SDL across a large number of learning venues. Close liaison and coordination is needed with all horizontal module leads and administrative teams, with the assessment team and with NHS teachers, university teachers, patients and a large number visiting VM tutors. Vertical modules learning is everybody’s business however academic oversight of the VMs as a whole is central to maintaining the MBBS vision; ensuring student facing resources and teaching are of the highest quality, ensuring all 11 VMs have good representation in the MBBS and coordinating ongoing developments. Equally, whilst VM administration will be shared with the relevant Medical Student Administration (MSA) year teams and Divisional subject teams, the core VM team within Medical Student Administration is responsible for co-ordinating timetabling, organisation, quality assurance, supporting the VM Lead and Deputy lead, co-ordinating the VM Moodle sites and VM documentation, co-ordinating the assessment requirements including the portfolio, guiding divisional administration in the delivery of the patient pathways and managing over 50 visiting tutors. Visiting VM tutors come from all sectors of the healthcare system: they are not all doctors. All visiting vertical modules tutors do have expertise in small group facilitation, uphold the very highest of standards as a teacher as befits a role as a teacher at UCL and are familiar with, and advocates of, Good Medical Practice. Depending on their exact role, visiting vertical modules tutors will have expertise in one or more of the vertical module domains. 38 Leadership Roles Academic Lead for Vertical Modules 2 notional PAs: UCLMS/Divisional Administrative support: Medical Student Administration Accountable to: Director of UCL Medical School via the Deputy Director /Lead for Undergraduate programmes Term of office: normally 5 years Remit Responsible for the strategic development of all VM teaching in the MBBS Supervision and support of all vertical modules activity including troubleshooting and responding to student feedback Responsibility for overseeing the recruitment, management and training of the Visiting VM tutors Ensure all VM course materials & learning resources including Moodle, are consistent with VM wide and MBBS wide strategy Ensure assessment design and delivery for progression tests and formative assessments QA of VM activities liaison with all relevant horizontal modules Committees: Member of MBBS Executive Committee Member of MBBS Teaching Committee and relevant Sub Committees Member of MBBS Examination Board and relevant Sub Boards and Panels Member of mQMEC Chair of the Vertical Modules Teaching Committee Member of relevant Vertical Modules Teaching Sub Committees Deputy Lead for Vertical Modules 1 notional PA: Divisional/SIFT Administrative support: Medical Student Administration Reporting to the Lead for Vertical Modules Remit Support for the VM lead in all his or her roles and deputising in his or her absence Particular responsibility for VM recruitment & training Particular responsibility for support of tutors delivering fully integrated module based VM activities Assistance with assessments Committees: Member of MBBS Teaching Committee and relevant Sub Committees Member of relevant MBBS Examination Sub Boards and Panels Member of mQMEC Deputy Chair of the Vertical Modules Teaching Committee Member of relevant Vertical Modules Teaching Sub Committees 39 Vertical Module leads 1 notional PA: Divisional/SIFT Administrative support: Divisional/Trust Accountable to: Academic Lead for Vertical Modules Term of office: normally 5 years Student Centred Learning, patient centred learning: Student Selected Components Portfolio Patient Pathways: Integrated and Community Care Cardiometabolic Cancer Medicine Mental Health Mother and baby Integrated Vertical strands: Anatomy and Imaging Clinical skills and practical procedures Pathological sciences(2 PAs - co-ordinating 5 disciplines) Use of evidence Use of medicines Overarching Themes: Mental Health Social Determinants of Health Synthesis and Professional Practice: Ethics and Law Clinical Communication Professional Practise Synthesis Curriculum: Academic and operational oversight of module teaching To co-ordinate, manage and implement module teaching and timetabling To develop teaching materials including on-line resources and e-learning To participate in curriculum review and implement curriculum development To implement curriculum changes as directed by MBBS Teaching Committee To ensure that the teaching students receive is compatible with the core curriculum To co-ordinate appropriate introduction/core teaching weeks To develop others in horizontal modules teaching roles to deliver the VMs in situ (where appropriate to the module) To liaise with Directors of Divisions and/or Divisional Undergraduate Tutors to ensure the appropriate allocation to the MBBS programme of Student Load funded resources Assessment: To participate in writing and reviewing assessment materials To participate in standard setting To work with Year Leads and Module Management Group to ensure the provision of high quality assessment materials from VM teachers for formative and summative written, practical and clinical examinations To work with Year leads and Module Management Groups to ensure participation by VM teachers in standard setting processes and clinical examinations 40 Quality Assurance: To act upon student module feedback and report annually to QA To act upon external examiner’s comments and report annually to QA Committees: Chair of Vertical Module Management Group Member of Vertical Modules Teaching Committee Examination Boards: Member of relevant Year Panels and Sub Panels of Examiners Vertical Module Site leads 2 notional PAs: Divisional/SIFT One person per site or job share Administrative support: Medical Student Administration Accountable to: Academic Lead for Vertical Modules Term of office: normally 5 years Remit: Liaison with site sub dean to ensure best possible student experience of site based VM teaching To maintain an overview of VM teaching in all years on the site To attend site specific education committees to represent the VMs Attendance during VM teaching at key times (e.g. visitor days, when giving lectures) Assist VM lead with the selection and training of visiting VM tutors: Interviewing and recruitment of site staff Training of site specific VM tutors as required Line management of visiting VM tutors: Assisting UCLMS HR/VM office with staff induction including ensuring staff know how to navigate UCL website , access and use My View and can use Moodle to carry out required tasks Ensuring probation is completed including compulsory training Assisting UCLMS HR/VM office to manage leave: Approving leave requests , ensuring A/L taken outside teaching time, enforcement of contracted working hours , working with VM office to ensure appropriate cover is provided Responsibility for understanding performance standards and upholding them including appraisal of tutors Acting as a focus for information exchange: cascade information to tutors, cascade feedback information to tutors, act as a source of feedback from tutors to VM office Committees: Member of Vertical Modules Teaching Committee Member of relevant Vertical Modules Teaching Sub Committees Visiting Vertical Module Tutors Accountable to: VM site lead To facilitate students’ learning through small group work during Vertical Modules (VM) teaching To prepare for and attend all teaching sessions as identified in their personalised job description negotiated at the beginning of each academic year 41 To work with relevant learning resources to deliver this teaching according to the instruction of the lead for vertical modules To attend any plenary sessions associated with small group work sessions Marking of a small number of VM course assessments , giving written feedback to students and checking the completion of the relevant VM related areas of the student portfolio To provide feedback on students performance where required To attend any relevant VM tutor training and to ensure they comply with the induction , probationary and ongoing appraisal requirement of visiting tutors within the medical school To understand the MBBS programme as a whole and the place of VM teaching, and their particular teaching sessions within it Any other duties that are within the scope, spirit and purpose of the job as requested by the lead for undergraduate programmes at UCL Medical School Person specification All visiting vertical module tutors will be expected to be committed to supporting learning within the MBBS programme. This includes and understanding of a commitment to the vision of the MBBS programme and the learning and teaching strategy of UCL Medical School. Requirements 1 . Criteria E / D* Assessed E A/I Excellent organisational and planning skills E A/I Excellent facilitation skills E A/I Ability and commitment to promote reflective practice E A/I Good presentation skills E A/I Good communication skills (written and verbal) E A/I Experience of teaching in healthcare settings, preferable in an undergraduate programme or a medicine programme E A/I Experience of using a virtual learning environment, preferably Moodle D A/I A good knowledge of the training of doctors E A/I A good knowledge of Good Medical Practice E A/I Education, Qualifications and Training A qualification in healthcare or related industries: doctors, basic medical scientists, behavioural scientists, nurses, professionals allied to medicine 2 . 3 . 4 . A / I* Skills, Ability Experience Knowledge 42 Good working knowledge of basic Microsoft Office software, (Word, Outlook etc) 5 . E A/I Ability to work both as a team member and independently E A/I Evidence of continuous professional development E A/I Personal qualities / aptitudes * E = Essential; D = Desirable; A = Application; I = Interview In addition, some visiting Vertical Modules tutors will undertake roles within one of more areas of particular expertise. The ability to undertake these more specialised roles will be assessed at application and/or interview. These VVMs with specific expertise will be expected to: Visiting VM tutors: Clinical communication Have expertise or previous experience of teaching clinical communication (E) Have expertise in giving detailed and specific feedback in simulated environments (D) Have experience of working with simulated patients (E) Visiting VM tutors: Ethics & Law Have expertise and previous experience of teaching in clinical ethics (E) Visiting VM tutors: Mental health Have expertise or previous experience of teaching in the field of mental health (E) Be able and confident in working with patients with mental health problems (E) Visiting VM tutors: professional practice and synthesis (specialist ‘synthesis’ session) Be a currently practising doctor (E) Visiting VM tutors: Social determinants of Health Have expertise and previous experience of teaching in one of the domains of the module (sociology, global health, public health, heath promotion )(E) Visiting VM tutors: Use of Evidence Have expertise in teaching medical statistics or related topics (E) Have an interest in working with medical learners in this field (E) Visiting VM tutors: personal tutoring Have a commitment to the pastoral and professional support of medical students (E) Have experience in personal tutoring in the university environment (E) Have the skills to be able to discuss important issues influencing student learning in both group and individual settings (E) Practicalities 1Contract a. Agree on an annual basis a personalised contract identifying all teaching and training sessions to be undertaken in the forthcoming academic year by xxxx at the latest b. Understand their contract and who their contacts are for contractual issues c. Know what your contracted hours are and ensure you complete them 43 d. e. f. g. Know your notice period and procedures for resigning Understand what your duties are and follow them Understand the performance standards expected of them Understand the structure of UCL Medical School and how their role fits in (the context of their work) h. Know where to find UCL policies that affect them i. Understand what can be expected of both VM and staffing administrators j. Complete staff induction: http://www.ucl.ac.uk/hr/new_starters/ k. Attend in house training as outlined in your contract 2Annual Leave a. Recognise that the contract agrees that all annual leave is taken outside of teaching time b. Contact the office in writing with leave requests c. Understand leave requests in teaching time are only granted where a replacement can be found d. Understand that any ‘swaps’ are agreed with the approval of the office/campus 3Sick Leave procedures a. Follow UCL guidance: http://www.ucl.ac.uk/hr/docs/sickness_absence.php b. Contact your named line manager and the VM office if you know in advance that you are unable to teach c. Contact your named line manager (or arrange for someone else to contact them on your behalf) if you are unable to make it in to teach on the day 4Access to UCL systems a. Tutors are responsible for making sure they have access to UCL systems including knowing how to reset and change passwords b. Know how to get and acquire a UCL staff ID card and replace it c. Be able to use Moodle (with support if necessary) to access course materials and review and mark submitted work on Moodle d. Tutors must be able and willing to regularly access their UCL email addresses 5On the day expectations a. Know your own personalised timetable b. Come prepared and in good time for sessions and know where teaching resources are kept on that site c. Have access to key contact numbers in case of room booking problems etc. d. Check the designated room before the start of session e. Attend any associated lectures that occur during your contracted sessions f. Understand duties as a visiting vertical modules teacher and performance s to standards expected 6Other a. Meet any deadlines for course work marking and feedback b. Know how to access to the library c. Be familiar with the student support system and how to feed into it as a UCL teacher 44 UCL Medical School MBBS Leadership Clinical Placements Overview of Clinical Placements Management .............................................................................46 Overview of Clinical Placements Leadership..................................................................................47 Outline of Clinical Placements Roles.............................................................................................47 Site Sub Deans (Central Trusts: Royal Free, Whittington, UCLH)...........................................47 Undergraduate Education Tutors/Leads (Main & Associated Trusts and Community/PCTs) ..49 Lead Clinical Teachers and Lead Specialty Teachers ............................................................49 Firm Leads/GP Leads ........................................................................................................50 Criteria for the Designation of University NHS Provider Trust/Teaching Hospital Status...................51 Trust Learning and Development Agreement - Undergraduate Medical Education Training .............52 For organisational charts see: http://www.ucl.ac.uk/medicalschool/staff-students/committees 45 Overview of Clinical Placements Management Lead Education Provider & Commissioner UCL Medical School Strategic direction and leadership of undergraduate medical education & commissioning of teaching, assessment and clinical placements University Local Education Providers SLMS Faculties of Life, Brain, Medical and Population Health Sciences NHS Local Education Providers University Provider Trusts and Primary Care Trusts Academic leadership and operational oversight of teaching and assessment in each year of the programme Undergraduate medical education, clinical placements and clinical assessments Lead Education Provider & Commissioner UCL Medical School is responsible for: strategic direction and leadership of the MBBS programme (MBBS Leadership Team) commissioning of academic leadership and operational management of MBBS teaching and assessment from SLMS Faculties and NHS Trusts commissioning of clinical placements quality assurance and monitoring of NHS Providers to ensure high quality learning and training student load calculations SIFT calculations University Local Education Providers The SLMS Faculties of Life, Brain, Medical and Population Health Sciences are responsible for providing: academic leadership academic content of modules and assessments co-ordination of year teaching and assessment (Year Leads) co-ordination of module teaching and assessment (Module Leads and Specialty Leads) teaching and assessment NHS Local Education Providers NHS Trusts are responsible, under Learning and Development Agreements, for providing: a high quality learning and training environment educational services and support, teaching staff, teaching and learning opportunities access to patients clinical attachments leadership and supervision clinical assessments as prescribed by UCL Medical School appropriate teaching space, clinical and teaching equipment student welfare and health and safety 46 Overview of Clinical Placements Leadership UCL Medical School MBBS Leadership Director of UCL Medical School Deputy Director of UCL Medical School and Lead for UG Programmes Academic Lead for Quality Assurance o QA monitoring and visits Sub Dean (Facilities) o monitoring of University and Central Trust undergraduate teaching facilities and resources o Chair of the MBBS Facilities and Resources Committee (Site Sub Dean (UCLH) Sub Dean (DGH Liaison) o monitoring of undergraduate teaching and assessment activities at District General Hospitals to ensure compliance with Medical School requirements o Deputy Chair of the Final Year Teaching Committee Sub Dean (Community and PCTs) o monitoring of undergraduate teaching and assessment activities in Community and Primary Care Trusts to ensure compliance with Medical School requirements o Chair of the Primary Care Teaching Committee University NHS Provider Trust Leadership Site Sub Deans (Central Trusts) / Undergraduate Education Tutors (Main & Associated Trusts) o co-ordination of undergraduate medical education and assessment locally o monitoring of undergraduate teaching facilities and resources locally o ensuring compliance with Trust LDAs o monitoring of firm leads locally and ensuring that firm leads implement teaching and assessment in accordance with Medical School requirements o specific responsibilities for Introductory and Orientation Modules and/or Clinical Assessments where hosted locally Lead Clinical Teachers / Lead Specialty Teachers o assisting the Site Sub Dean/Undergraduate Tutor locally o operational oversight and co-ordination of clinical/specialty training and assessment locally o ensuring that the academic content of clinical placement teaching locally complies with MBBS curriculum and assessment requirements o monitoring of firm leads locally within subject/specialty o ensuring that firm leads implement teaching and assessment in accordance with Medical School requirements and Trust LDAs Firm Leads / GP Leads o delivery of firm teaching and assessment o educational supervision of students undertaking clinical placements o support and welfare for students undertaking clinical placements Outline of Clinical Placements Roles Site Sub Deans (Central Trusts: Royal Free, Whittington, UCLH) 2 notional PAs: NHS Trusts/SIFT Administrative support: NHS Trusts/SIFT 47 Accountable to: Campus Director in liaison with the Director of UCL Medical School and the Medical Director of the Royal Free London FT Appointed by: Campus Director in liaison with UCLMS and local Trust Executives Term of office: normally 5 years Leadership: To co-ordinate Undergraduate Medical Education locally in accordance with Trust Learning and Development Agreements (see last section) To lead the implementation of MBBS teaching and assessment locally in accordance with Medical School requirements and in collaboration with MBBS Year and Module Leads, senior Trust staff, Clinical and Specialty Leads and Firm Leads To lead the implementation of curriculum change and development locally as directed by MBBS Executive Committee and MBBS Teaching Committee To monitor SIFT budgets locally Trust corporate responsibilities as set out by individual NHS Trusts Teaching: To provide academic leadership for the Skills Centre locally To be responsible for planning and implementing Introductory and Orientation Modules locally To participate in student support and welfare in liaison with the Medical School Student Support System Assessment: To oversee and facilitate the delivery of firm assessments and supervised learning events To support the nominated Medical School leads for Year 4 and Year 5 in the delivery of clinical assessments locally, including ensuring suitable facilities and local examiner recruitment To lead the delivery of the Final MBBS clinical examinations locally Quality assurance: To work collaboratively with the Academic Lead for Quality Assurance to ensure appropriate action in response to issues raised through MBBS quality monitoring and assurance mechanisms Committees: Chair of Trust Undergraduate Education Committees Member of MBBS Executive Committee Member of MBBS Teaching Committee and relevant Sub Committees Exam Boards: Member of MBBS Board of Examiners Member of relevant Sub Boards and Panels of Examiners 48 Undergraduate Education Tutors/Leads (Main & Associated Trusts and Community/PCTs) Accountable to local Trust Executives Term of office: local arrangements Leadership: To co-ordinate Undergraduate Medical Education in accordance with Trust Learning and Development Agreements (see last section) To lead the implementation of MBBS teaching and assessment locally in accordance with Medical School requirements and working in collaboration with MBBS Year and Module Leads and senior Trust staff, Clinical and Specialty Leads and Firm/GP Leads To lead the implementation of curriculum change and development locally as directed by MBBS Executive Committee and MBBS Teaching Committee Trust corporate responsibilities as set out by individual NHS Trusts To monitor SIFT budgets locally To lead the delivery of MBBS clinical examinations locally (Basildon, Luton, North Middlesex) To participate in student welfare and support locally and in liaison with the Medical School Student Support system Committees: Chair of Trust Undergraduate Education Committees Member of MBBS Teaching Committee and relevant Sub Committees Lead Clinical Teachers and Lead Specialty Teachers 1 notional PA: Divisional Student Load (University employees) or SIFT (Trust employees) Administrative support: Divisions (University employees) or SIFT (Trust employees) Accountable to: UCL Heads of Division in liaison with the Director of UCL Medical School Appointed by: UCL Heads of Division in liaison with Trust staff with responsibility for approval of job plans Term of office: local arrangements Teaching: To co-ordinate teaching and assessment within specialty To ensure compliance with Trust LDAs To work closely with Year and Module Leads to review and coordinate timetables and curriculum content to ensure that there is equivalence in the teaching provided for all students at all sites To work closely with the Year and Module Leads to ensure that the teaching students receive is compatible with the core and speciality curriculum To work closely with the Year and Module Leads to produce and develop teaching materials including on-line resources and e-learning To ensure the appointment of firm leads for all teaching firms To ensure that firm leads implement teaching according to Medical School requirements To co-ordinate and implement local teaching and timetabling within their subject To co-ordinate and implement appropriate Introductory and Orientation Modules within their subject To co-ordinate the implementation of curriculum changes and developments within their subject To participate in student support and welfare Assessment: To work closely with Year Leads, Module Leads and Undergraduate Education Leads to ensure uniformity in the delivery of high quality assessments and equivalence in standards of assessment and grading at all sites 49 To co-ordinate supervised learning events/workplace-based assessments and module/firm reports/grades To contribute to formative and summative assessments by writing and reviewing written and OSCE questions To participate in standard setting processes for the written papers To participate in clinical examinations To ensure participation by all firms in written and clinical assessment requirements and examining Quality Assurance: To act upon student feedback where this has identified issues with local teaching which require attention To provide returns regarding teaching quality to QMEC where requested Committees: Member of Trust Undergraduate Education Committee Member of relevant Year Teaching Committee Member of relevant Module Management Group Examination Boards: Member of relevant Examination Sub Boards and Panels Firm Leads/GP Leads Firm Leads - 1 notional PA: Divisional Student Load (University employees) or SIFT (Trust employees) GP Leads – local arrangements Administrative support: Divisions (University employees) or SIFT (Trust employees) Accountable to: Site Sub Deans (Central Trusts)/Undergraduate Education Tutors (Main and Associated Trusts)/ Undergraduate Education Leads (Community and PCTs) Appointed by: Site Sub Deans (Central Trusts)/Undergraduate Education Tutors (Main and Associated Trusts)/ Undergraduate Education Leads (Community and PCTs) in liaison with MBBS Year and Module Leads Term of office: local arrangements Teaching: To lead, co-ordinate and manage firm teaching locally in accordance with UCL Medical School requirements To ensure that the aims and objective of the firm’s teaching are concordant with the aims and objectives of the MBBS Teaching Committee and the School and will facilitate students’ achievement of the goals of the curriculum To co-ordinate and develop teaching materials including on-line resources and e-learning To ensure that firm handbooks are updated annually, contain all the required information, are prepared in a uniform style and are available to students at the appropriate time. To meet students on the first day of the attachment and provide any necessary orientation To agree the firm timetable with the Module and Specialty Leads To ensure that there is adequate programmed teaching To ensure that the firm timetable is followed and the teaching programme is delivered appropriately To participate in student support and welfare Assessment: To co-ordinate and deliver firm assessments locally including supervised learning events/workplace based assessments and firm reports To ensure that students receive appropriate and timely feedback on their performance on the attachment 50 To participate in and to ensure firm participation in the provision and review of written and OSCE questions for formative and summative assessments To participate in and to ensure firm participation in standard setting processes To participate in and to ensure firm participation in clinical examinations Quality Assurance: To respond to student feedback and comments on the attachment, and to explain to both the Module Lead and the students what steps have been or will be taken to deal with matters raised by the students and the School Committees: Member of Trust Undergraduate Education Committee Member of relevant Year Teaching Committee Member of relevant Module Management Group Examination Boards: Member of relevant Examination Panels and Sub Panels (Clinical) Criteria for the Designation of University NHS Provider Trust/Teaching Hospital Status Applications are considered by the Dean and the Director of UCL Medical School on the basis of: Quantity and complexity of undergraduate teaching activity carried out by the Trust Provision of appropriate facilities and infrastructure Quality of undergraduate teaching carried out by the Trust Contribution to curriculum and assessment development and innovation Contribution to the leadership of the MBBS programme Contribution to the wider academic area of medical education Conditions of designation include: It is reviewed at 5 year intervals It is subject to satisfactory performance in UCL quality assurance mechanisms The inclusion of a University nominee as a voting Non-Executive Director on the Trust Board or the Board of Governors or a named Trust representative with: o An understanding of the university regulatory processes, not necessarily at UCL o An active interest in the quality of education provided by Trust to undergraduates underpinned by clear lines of communication and responsibility within the Trust o Experience in the delivery of medical education to medical students o Knowledge of the funding of medical and other healthcare education in the UK o Knowledge of the changes in education in the wider NHS, with an understanding of the potential impact on undergraduate medical students A notice period of at least one academic year is mandatory in the event of removal of or downgrading of University designation by the Medical School or withdrawal from University designation by the Trust Recommendations for designation are approved by the MBBS Teaching Committee and reported to the University of London’s Medical Studies Committee. Once confirmed as designated, a Main Provider Trust is encouraged to use the terms “University Hospital NHS Trust” and/or “UCL Medical School Clinical Teaching Hospital” in conjunction with or as part of its existing logo on letterheads and signs, and on any other documentation or display which might be relevant from time to time. Associated Provider Trusts are encouraged to use the terms “University Hospital NHS Trust” and/or “Associated with UCL Medical School”. 51 Main University NHS Provider Trusts Criteria include: This must be an exclusive relationship with UCL for the MBBS programme Approximately 75 undergraduate FTEs per annum In certain circumstances, contribution in other areas listed above may be taken into account where FTEs fall below this level Associated University NHS Provider Trusts Criteria include: Approximately 20 undergraduate FTEs per annum In certain circumstances, contribution in other areas listed above may be taken into account where FTEs fall below this level Main provider of a specialist service to undergraduate education A NHS Provider Trust falling below these student numbers but acting as a substantial centre of research or postgraduate teaching might exceptionally be nominated for designation as a University Provider Trust. Trust Learning and Development Agreement - Undergraduate Medical Education Training SCHEDULE 4 Medical Service Increment For Teaching (“Medical SIFT”) This 0 (Medical Service Increment for Teaching (“Medical SIFT”) is applicable where the Health Service Body provides Undergraduate Medical Education Training to Medical Students. Purpose of this Schedule 1. The Parties acknowledge the principle that education, training and learning are integral to the delivery of the core business of the Health Service Body and to ensure the provision of high quality teaching staff to deliver this training. 2. Medical Schools under the Medical SIFT Agreements have obligations to provide resources, to supervise and to monitor Undergraduate Medical Education Training to which Medical SIFT Funding relates. Accordingly the provision of Undergraduate Medical Education Training requires a collaborative approach between the Medical Schools, the Authority and the Health Service Body. 3. This 0 (Medical Service Increment for Teaching (“Medical SIFT”) outlines obligations of the Health Service Body in relation to provision of Medical SIFT Services and the terms under which the Authority provides funding to the Health Service Body for the provision of the Medical SIFT Services. 4. Medical Placement Services The Health Service Body is required to: 4.1 Teaching Programmes 4.1.1 ensure the adequate provision of high quality teaching staff to enable Medical Students to acquire the skills and knowledge as specified in course documentation provided by the relevant Medical Schools; 4.1.2 provide a range of teaching and learning opportunities that meet the minimum specifications laid down by the relevant Medical Schools; 4.1.3 ensure access to the necessary range of cases to support the achievement of the learning outcomes of the clinical attachments. These will include a balanced mixture of elective and acute emergency conditions, common conditions plus direct referrals 52 from general practitioners, and illnesses appropriate to the clinical specialty in which the Medical Student is based; 4.2 4.1.4 ensure that Medical Students are given an appropriate mix of teaching types e.g. practical skills, small groups and ward rounds; and 4.1.5 ensure that the form of delivery of clinical training is agreed with the relevant Medical Schools. Access to Patients 4.2.1 4.3 ensure appropriate access to patients on wards, outpatients, day wards and operating theatres by Medical Students and ensure that patients are aware of their rights in relation to having Medical Students present during their treatment. Patients should be informed that Medical Students, as part of their training, will be present and may contribute in their care and that they may request that Medical Students are not present. Clinical teaching should comply with the relevant Medical School’s policy on the rights of patients in medical education. Booklets of introductory advice for patients must provide an explanation of the importance of clinical teaching and what it might involve as specified by the document ‘Medical Students in Hospitals - A guide on their access to patients and clinical work’ prepared by the NHSME in April 1991. Clinical Standards and Guidelines ensure that all Medical Student clinical attachments meet specific standards and guidelines as defined by the relevant Medical Schools and which must: 4.4 4.3.1 have an identified firm leader and course co-ordinator, with appropriate administrative/secretarial support, to act as the focus for Medical Students assigned to that clinical attachment and to facilitate teaching and provide pastoral care. The leader and administrative staff should have appropriate time identified in their job plans for these activities; 4.3.2 provide complete and detailed timetables for each Medical Student to be made available on the first day of each clinical attachment, a copy of which must be sent to the relevant Medical School; 4.3.3 liaise with appropriate Medical School colleagues to ensure that Medical Students receive learning objectives and logbooks relating to the clinical attachment; 4.3.4 have an identified person to liaise with the Health Service Body’s undergraduate teaching co-ordinator by the beginning of the Academic Year to ensure that all teachers receive a copy (printed or electronic) of the relevant handbooks including Medical Students’ timetables and learning objectives; 4.3.5 look after Medical Student welfare including personal tutoring and monitoring attendance and where appropriate referring Medical Students with attendance and/or welfare problems to the faculty tutor (or person of equivalent standing); and 4.3.6 require the Medical Students to evaluate the Health Service Body using forms provided by the relevant Medical School, and ensure that copies of evaluation forms are forwarded by the Medical Students to the relevant Medical School within the timescale specified by the relevant Medical Schools. Assessments 53 4.4.1 4.5 4.6 Teaching Staff and Support 4.5.1 ensure sufficient time for teaching and related activities (preparation, assessment, organisation, examination etc) is included in the job plans of all relevant staff; 4.5.2 provide administrative and other support for Medical Placement Teachers involved in Undergraduate Medical Education Training, including the provision of teaching material and the payment of travel expenses incurred as a result of teaching-related activities; 4.5.3 ensure that Undergraduate Medical Education Training is included in the job plans of new consultant appointments and of those existing consultants that they have responsibility for the Undergraduate Medical Education Training of Medical Students and that a Programmed Activity, specifically for Undergraduate Medical Education Training, is allocated for each Medical Student the Health Service Body receives unless otherwise agreed with the relevant Medical Schools. It may be that some consultants will wish to have more than one teaching session, while others may not wish to offer undergraduate teaching, but the Health Service Body shall ensure that teaching provision is at the level of the funding provided for the Services provided under this 0 (Medical Service Increment for Teaching (“Medical SIFT”)). The job plan should specify that the core contribution must include, as appropriate, teaching ward rounds, bedside teaching sessions, seminar teaching, teaching in outpatient clinics and the community, and acting as a clinical examiner. It may also, optionally, include delivering lectures, supervising SSMs, facilitating PBLs, interviewing for Medical Student intake and acting as a course or examination organiser. If the job plan indicates that some or all of the teaching will take place during clinical service, for example in a out patient clinic, then the clinical load should be appropriately reduced, for example with fewer patients booked, to allow effective teaching to take place; and 4.5.4 ensure that contributions to teaching and teaching excellence is recognised by the Health Service Body and featured in annual reviews/appraisals for individuals with education included in the contract or job plan. The Health Service Body may wish to consider recognition of contribution to teaching in the award of discretionary points. Teaching Space 4.6.1 4.7 provide regular assessment (e.g. end of firm assessments, case studies, projects etc) according to the guidelines laid down by the relevant Medical Schools to measure how well the Medical Students have achieved the objectives of the clinical attachment, provide feedback to Medical Students and ensure that Medical Student performance is reviewed by consultants and junior staff throughout the clinical attachment. Copies of assessment forms must be forwarded to the relevant Medical Schools within the timescale specified by the relevant Medical Schools. This information forms a vital record of a Medical Student’s progress and achievement. ensure the provision of appropriate teaching space or designation of clinical space for teaching purpose, adjacent to the main clinical areas available for Undergraduate Medical Education Training (wards, out-patients, day surgery units etc) for teaching sessions to take place with a group of Medical Students and which allows Medical Students to clerk patients where necessary. Library and Knowledge Management 54 4.8 4.9 4.7.1 ensure that Medical Students have access to a library, meeting the standards as defined in Part A of this 0 (Library Services for Medical Students on Placement in the NHS); 4.7.2 ensure Medical Students have access to personal computing facilities on the Health Service Body’s placements site. These facilities should include: access to standard applications (word processing, web browser, email, etc); the ability to access their remote desktop; and the ability to print. These facilities should be readily available to Medical Students during normal working hours and as much out of hours access as is reasonably possible. This responsibility includes the provision and maintenance of appropriate information systems hardware to provide Medical Students access to computing facilities; and 4.7.3 provide Medical Students with passwords for secure access to electronic medical record and electronic radiography systems used in the Health Service Body and ensure that the Medical Students are aware of their responsibilities and the security arrangements relating to this. Facilities and Transport 4.8.1 provide residential accommodation or travel assistance for Medical Students in accordance with the recommendations contained in ‘LIVING AND WORKING CONDITIONS FOR HOSPITAL DOCTORS IN TRAINING’ – HSC 2000/036. This would not normally apply if the Health Service Body is co-located with a campus of a Medical School; 4.8.2 provide residential accommodation of an appropriate standard when Medical Students are ‘on-call’. The room shall include a desk, sufficient lighting, sheets, towels and reasonable access to a telephone; 4.8.3 provide transport for Medical Students who are placed in accommodation relating to a clinical attachment away from the unit or where Undergraduate Medical Education Training arranged by the Health Service Body takes place on more than one site; 4.8.4 provide access to catering for Medical Students’ meals during their clinical attachment to the unit of the Health Service Body, including the availability of meals at night; 4.8.5 provide a rest room/common room for Medical Students during their clinical attachment; and 4.8.6 provide lockers for Medical Students during their clinical attachment. Equipment 4.9.1 4.10 provide appropriate equipment such as functioning bleeps, theatre clothing and clinical and laboratory equipment to facilitate teaching and learning. As appropriate, protective equipment should be provided to enable Medical Students to take standard health and safety precautions, e.g. gloves, vacutainers, sharps disposal bins etc. Health and Safety Procedures 4.10.1 ensure that Medical Students are provided with the same degree of Health and Safety support as the Health Service Body’s employees including access to the local emergency assessment and treatment services after accidents; 55 4.10.2 ensure that Medical Students are not asked to, or allowed to, undertake tasks in contravention of the relevant Medical School’s health and safety policies (e.g. not being asked to carry out sharps procedures on patients known to be infected with HIV or HCV or other blood-borne infection) and that any accidents or incidents involving Medical Students are reported to the relevant Medical School; 4.10.3 ensure that the Occupational Health department of the Health Service Body provides the relevant Medical School with a confidential report on clinical assessment and outcome of any consultation by a Medical Student following an inoculation accident or exposure to a contagious disease; 4.10.4 ensure that Medical Students are provided with up-to-date, timely and appropriate information on the Health Service Body’s health and safety policy as part of their induction to the Health Service Body including information on: 4.10.4.1 personal protective equipment requirements. Health Service Body provide white coats for Students and where they can be obtained from? is the Health Service Body’s policy on wearing prone clinical procedures? For example, does the use by visiting Medical A further example: what gloves during exposure- 4.10.4.2 vaccination requirements, for example does the Health Service Body have any requirements in addition to those of the appropriate Medical Schools which requires Medical Students to be routinely immunised against, inter alia, TB, Rubella and hepatitis B (including anti-body tests to identify and follow-up non-responders) before commencing clinical studies?; 4.10.4.3 inoculation accident requirements. For example: who is responsible for providing initial assessment and treatment and longer term follow-up and where can they be found?; how Medical Students can access HIV exposure prophylaxis after a high-risk incident; to whom Medical Students should report accidents and where they should go for emergency assessment and treatment services, and arrangements for obtaining help in the evening and at weekends; 4.10.4.4 ‘Needle-Stick’ incident requirements. The Health Service Body should provide initial assessment and treatment following ‘needle stick’ injury and have the incident reported to the Health Service Body’s Occupational Health department for immediate follow up; and 4.10.4.5 contagious diseases requirements. For example: 4.10.4.5.1 who is responsible for follow-up of staff after possible inadvertent exposure to tuberculosis? 4.10.4.5.2 are attached Medical Students included in any contact tracing/follow-up exercises? 4.10.4.5.3 to whom should Medical Students report if they have a contagious infection, e.g. chicken pox? 4.10.5 inform the officer in charge of health and safety for Medical Students in the Medical School if the Health Service Body wishes to impose any vaccination or immunity assessment requirements in addition to those of the Medical Schools as described at 56 Paragraph 4.10.4.2 above, giving sufficient notice to enable the requirement to be acted upon; 4.10.6 ensure that staff are aware of the health and safety requirements outlined in Paragraph 4.10 (Health and Safety Procedures) above and ensure appropriate representation on the Health Service Body’s health and safety committee of the person responsible for the health and safety of Medical Students when they are on site; and 4.10.7 include Medical Students in the Health Service Body’s ‘Whistleblowing and Bullying and Harassment’ policies. 5. Facilities Services The Health Service Body is required to: 5.1 Management of Teaching Activities and Clinical Services 5.1.1 have a named member of staff who has responsibility for co-ordinating Undergraduate Medical Education Training and who has a timetable which allows him/her to dedicate an appropriate amount of time as agreed with the relevant Medical School to the administration of undergraduate medical teaching. The Facilities Funding allocation should support a teaching budget for the undergraduate coordinator, to be spent directly on personnel and/or facilities supporting undergraduate medical education. Spend should be planned in conjunction with the Medical Schools; 5.1.2 have a named member of the administrative staff who will support the co-ordinator in the management and organisation of all Undergraduate Medical Education Training; 5.1.3 provide a learning environment in which high quality Undergraduate Medical Education Training thrives; 5.1.4 have a level and quality of staff which supports the expectation that both academic and Health Service Body staff will participate in the conduct of Undergraduate Medical Education Training and undertake national and international responsibilities where appropriate; 5.1.5 ensure that the contracts of junior medical staff and any other clinical staff involved in Undergraduate Medical Education Training include reference to the expectation and duty to teach; 5.1.6 actively support the participation of consultant teaching staff in staff development and training programmes to enhance the quality of medical education for Medical Students. All consultants involved in teaching Medical Students will be expected to have undertaken accredited teacher training and will undergo peer review of their teaching activities every three (3) years and would be expected to expand or review their own development in this area. The result of appraisals and review of teaching should be monitored by the Health Service Body’s undergraduate co-ordinator and reported to the Medical Schools at the end of each Financial Year; 5.1.7 ensure that the needs of Undergraduate Medical Education Training are taken into account when patient through-put is planned, e.g. in out-patient clinics; 57 5.2 5.1.8 ensure that the needs of Undergraduate Medical Education Training are taken into account in the planning and consultation of changes to service delivery and changes in the location of services; 5.1.9 ensure that the Health Service Body’s medical staff participate in the preparation, organisation and conduct of Medical Student assessments and examinations and should be expected to help in the recruitment of patients and material for such examinations; 5.1.10 ensure that no clinical teaching space is redesignated without consultation with and agreement of the appropriate Medical Schools; and 5.1.11 ensure adequate provision of individual mentoring and advice for Medical Students and where appropriate by appointing local clinical staff as Medical Student advisors. Assessments and Examinations 5.2.1 ensure the adequate provision of facilities and staff to conduct routine in-course assessment and university qualifying examinations including undergraduate clinical and oral examinations and Objective Structured Clinical Examinations (“OSCEs”). This should include provision of the following: 5.2.1.1 a clinician (minimum consultant grade or equivalent grade) nominated by the Health Service Body to oversee clinical examinations and recruit patients. This clinician will oversee the provision of ‘maps’ showing the location of numbered beds and sitting cases, lists of patients and their diagnoses, history and physical signs of each patient for examiners. The Health Service Body must appoint a locum to cover the clinician’s duties while s/he is preparing for and overseeing the examination (the Health Service Body is expected to cover this cost); 5.2.1.2 adequate numbers of appropriately qualified staff to prepare for and conduct the examination and provide care to patients participating in the examination. The Health Service Body must make it clear to such staff that this activity is part of their normal duties paid for by the Health Service Body and that separate payment should not be claimed from the Medical Schools. If agency staff are employed for this purpose, payment must be made by the Health Service Body; 5.2.1.3 patients recruited to participate in the examination. The Health Service Body must pay the costs associated with the provision and care of such patients, e.g. secretarial costs incurred in ‘pulling’ and copying patients’ notes and contacting patients, patients’ travelling expenses including patients’ transport costs where the patients are used in teaching sessions, portering costs, payment to specialists employed to look after paediatric patients taking part in the examination, and the costs of refreshments for patients and Health Service Body staff involved in the examination; 5.2.1.4 suitable, appropriately furbished space including rooms for examiners, patients and Medical Students and equipment such as beds, couches, chairs, screens, linen etc in order to conduct all aspects of the examination. The Health Service Body must provide written confirmation of the examination location at least four (4) months before the examination takes place and must cover any costs associated with setting up wards and other accommodation used for the examination (including staffing costs); and 58 5.2.2 5.3 Diagnostic Investigation Facilities 5.3.1 5.4 5.5 give notice in writing at least three (3) years before the examination is due to take place if it is unable to provide the requested space; the examination location must be confirmed at least four (4) months before the examination takes place. If, due to major building works or site reconfiguration, the Health Service Body foresees any difficulties in meeting the commitments that it has made it must initiate discussion with the Medical Schools, in writing, as soon as possible and at least twelve (12) months before the date of the examination. Any costs associated with setting up wards and accommodation used for the examination (including staffing costs) shall be covered by the Health Service Body. provide and maintain diagnostic investigation facilities which will take account of the additional requirements associated with the conduct of Undergraduate Medical Education Training. Medical Records, Library and Knowledge Systems 5.4.1 ensure the provision of medical records and information systems sensitive to the needs arising from Undergraduate Medical Education Training and ensure that all Medical Students are aware of local patient confidentiality agreements and, as appropriate, the requirements of the DPA; 5.4.2 ensure that the provision of any teaching and teaching support facilities (including local Health Service Body-managed library and information services) by the Health Service Body takes account of the needs arising from Undergraduate Medical Education Training activity. This should include the provision and maintenance of an infrastructure to support new developments in medical education, including facilities for participating in video lectures, IT and library facilities for staff and Medical Students as specified by the Medical Schools and clinical skills laboratories as appropriate; and 5.4.3 provide appropriate financial contribution to the academic library and information services. This should be in accordance with the arrangements as set out in the library service agreements in cases where such agreements exist between the Medical Schools and the Authority. Structure and Planning 5.5.1 ensure that a managerial and administrative structure exists which allows for appropriate dialogue and planning to take place between the Health Service Body and the Medical Schools on issues related to medical education and research. The undergraduate co-ordinator, and Medical Placement Teachers should attend Medical School committee meetings as appropriate; 5.5.2 provide a financial overview at the end of the Financial Year to the Medical Schools summarising Medical SIFT expenditure. In addition, details should be given of how incremental Clinical Placement Funding and Facilities Funding has been spent; 5.5.3 consult with the Medical Schools regarding planning and proposals for expenditure of Facilities Funding; 5.5.4 undertake joint planning with the Medical Schools in the construction of business plans to take account of Undergraduate Medical Education Training and development needs; and 59 5.5.5 6. inform the Medical Schools regarding any significant planned changes to service provisions, new capital projects and estate management issues that may impact on medical undergraduate teaching and learning. Monitoring and Liability The Health Service Body acknowledges as follows: 7. 6.1 the obligations of the Health Service Body as set out in this 0 (Medical Service Increment for Teaching (“Medical SIFT”)) (the “Health Service Body Medical Obligations”) shall be monitored by the Medical Schools in accordance with the terms and conditions of the relevant Medical SIFT Agreement, as amended from time to time. Copies of the relevant Medical SIFT Agreements are available on written request from the Authority; 6.2 monitoring of compliance of the Health Service Body Medical Obligations by the Medical Schools, as procured by the Authority, will include the use of Medical Student feedback, examination results, clinical log books, Medical SIFT site visits and other monitoring processes as they are developed. There will be feedback provided to the Health Service Body regarding the outlined monitoring procedures through meetings between the head of the Medical Schools or his/her designate and the undergraduate co-ordinator for the Health Service Body, together with such teaching representatives as may be appointed within the Health Service Body to oversee medical undergraduate teaching. In addition the Health Service Body acknowledges that there may be external monitoring through the GMC, Quality Assurance agencies and other such bodies; 6.3 as defined in the ‘SIFT Operational Guidance HSG (95)59’ and ‘Guidance for NHS Trusts on costing for SIFT Contracts HSG (95)60’ the Health Service Body shall be required to produce an annual statement of Medical SIFT accountability. This should list the physical, human and financial resources, both fixed and variable, that have been supported by Medical SIFT Funding and the amounts paid for each resource during the relevant Financial Year; and 6.4 the Health Service Body shall ensure that all Medical SIFT clinical work undertaken by Medical Students is closely supervised by a registered medical practitioner, who is deemed to be employed by the Health Service Body. The Health Service Body as the employer therefore undertakes that it will indemnify the Medical Schools against all proceedings, costs, expenses, liabilities, injury, death, loss or damage arising out of the breach or negligent performance or failure in performance by the Health Service Body of its obligations set out in this 0 (Medical Service Increment for Teaching (“Medical SIFT”)). Funding 7.1 Subject to Paragraphs 7.2 to 7.4 of this 0 (Medical Service Increment for Teaching (“Medical SIFT”)), Medical SIFT Funding shall be paid by the Authority to the Health Service Body in accordance with Error! Reference source not found. (Funding). 7.2 Medical SIFT Funding shall be comprised of Clinical Placement Funding and Facilities Funding. 7.3 Clinical Placement Funding shall be paid by the Authority to the Health Service Body for the provision by the Health Service Body of the Medical Placement Services to Medical Students at the Health Service Body. The level of Clinical Placement Funding shall be determined by the number of Medical Students for whom the Health Service Body provides the Medical Placement Services. 60 7.4 Facilities Funding shall be paid by the Authority to the Health Service Body for the provision by the Health Service Body of the Facilities Services for Medical Students at that Health Service Body. 61 UCL Medical School MBBS Leadership Faculty Tutors, Student Support & Foundation Training OVERVIEW OF FACULTY TUTOR AND STUDENT SUPPORT SYSTEMS................................................63 Faculty Tutors Years 1-3 and Years 4-6 ..............................................................................63 Lead for Careers and Foundation School Transition ............................................................65 Lead for Elective Approval and Health and Safety ..............................................................66 Foundation School Director...............................................................................................66 Vice Dean for Professional Affairs .....................................................................................67 Student Support Tutors.....................................................................................................67 Student Counsellors..........................................................................................................68 Departmental Equal Opportunities Liaison Officer..............................................................68 For organisational charts see: http://www.ucl.ac.uk/medicalschool/staff-students/committees 62 OVERVIEW OF FACULTY TUTOR AND STUDENT SUPPORT SYSTEMS UCL Faculty Tutors are appointed by the Provost to undertake duties relating to general academic and pastoral oversight of all students in the Faculty including admissions and widening participation, personal tutors, academic matters, student recruitment, registration and progression, complaints and grievances, and quality management within the faculty. The duties of Faculty Tutors are prescribed by the Provost and linemanagement is delegated to the Dean of the Faculty. For the Faculty of Medical Sciences: 2 Faculty Tutors are appointed: Faculty Tutor (Years 1-3) which is a full-time post under UCL’s Faculty Tutor structures and conditions; and Faculty Tutor (Years 4-6) which is a part-time post combined with clinical commitments under the clinical consultant’s contract. The Faculty Tutors work together to coordinate their remit across the programme and to attend or to represent the Faculty on the other’s behalf at College Committees. By authority delegated by the Dean, the Faculty Tutors are line-managed by the Director of UCL Medical School In addition to the duties prescribed by the Provost, the Faculty Tutors in FMS are responsible for managing a team of academic staff and clinicians providing student support relating to: oCareers/Foundation School Transition o Fitness to Practise investigations in UCL Medical School oHealth and Safety on Elective oStudent Counselling Faculty Tutors Years 1-3 and Years 4-6 Faculty Tutor Years 1-3: 1 x 10 notional PAs: FMS Faculty Tutor Years 4-6: 1 x 6 notional PAs: FMS Administrative support: FMS/Medical Student Administration Reporting to the Director of UCL Medical School Student Support and Progress: UCL Responsibilities: a) exercise the general academic and pastoral oversight of all students (undergraduate, graduate taught and graduate research students) in the Faculty; b) together with the Dean, provide leadership on the implementation of Faculty Learning and Teaching Strategies and the development and management of new programmes, ensuring also that programmes and course units are reviewed and withdrawn as they become redundant. c) contribute to the setting of Faculty quotas and targets, manage the admissions process and procedures so as to ensure that the Faculty meets its quotas and targets and conforms with UCL policies, coordinating the work of the support staff administering the procedure and liaising with the Dean, Faculty Graduate Tutor, Senior Tutor, Academic Registrar and the UCL Admissions Office, as appropriate d) manage and monitor the Personal Tutor Scheme, ensuring the delivery of the key skills agenda and careers advice and providing advice and direction to students experiencing difficulties (academic, financial, medical or personal); 63 e) as a member of the Faculty Management Team, contribute to the strategic management of the Faculty and act as Sub-Dean for the Faculty (in accordance with Statute 8). f) contribute a Faculty view in discussions relating to a range of student matters including registration, fees, examinations and other academic matters working closely with the Academic Registrar and officers of the Registry; g) represent UCL in student recruitment activities and events (Open Days, Schools Conferences, Schools Visits and other Widening Participation and international student recruitment initiatives etc.) organised by Educational Liaison and ensure appropriate representation at such events; h) ensure that each student's registration, academic progress and examination entry details satisfy the relevant degree or diploma or certificate regulations; i) advise students who are academically insufficient or who have failed major examinations as to their possible future actions, and, under authority delegated from the Provost (in accordance with Statute 11), suspend or exclude them from further registration at UCL, in conjunction with the Dean of Students and Faculty Graduate Tutor, as appropriate; j) handle complaints and grievances in liaison with the Dean of Students and the Senior Tutor; k) monitor and co-ordinate all aspects of student progress, liaising with Faculty Officers, tutors and teaching staff on issues concerning the general pastoral and academic Student Support of students in the Faculty l) ensure that relevant Faculty staff are aware of and comply with UCL policy and current legislation and liaise as necessary with UCL Officers on such issues and their implementation; m) co-ordinate the activities of the Faculty Graduate Tutor in the exercise of their duties; n) take responsibility with the Dean for the operation of all aspects of the Quality Management and Enhancement measures and procedures within the Faculty’s remit including the monitoring of Examination Boards; o) chair a number of Faculty and UCL committees (such as the Faculty Teaching committee(s), UCL Grievance Panels, Examination Irregularities Panels and Internal Quality Review Teams) or give oral reports at them on a regular basis; p) represent the Faculty as an ex officio member at a range of UCL committees and sub-committees, and serve on other UCL committees, sub-committees, working groups and panels when asked to do so; q) keep up to date with all issues surrounding the student experience generally and be conversant with all current UCL policies and procedures relating to the recruitment, admission and academic progress and pastoral well-being of the student body and develop/implement new procedures and protocols in collaboration with the Dean, Senior Tutor and Vice-Provost (Academic & International). Ensure that policies and procedures are effectively disseminated across, and followed within the Faculty; r) contribute to the teaching effort within the Faculty and ensure appropriate training of admissions staff in liaison with the Organisational and Staff Development Team and the Centre for Learning and Teaching as appropriate. s) draft, edit and audit content for the undergraduate and graduate prospectuses, the UCAS Handbook, documents for Schools Conferences, other publications and website material in conjunction with the Faculty Graduate Tutor, working with the Educational Liaison Team which has responsibility for publishing; 64 MBBS Responsibilities: To oversee the Student Support System and Clinics To oversee Careers/Foundation School Transition To oversee Fitness to Practise investigations in UCL Medical School To oversee Health and Safety on Electives To oversee Student Counselling To oversee Foundation School Trainees in Difficulty Admissions and Widening Participation: UCL Responsibilities: a. under powers delegated from the Provost on the authority of Statute 11, make on behalf of the Academic Registrar offers of admission to undergraduate degree courses within the Faculty, and authorise, after consultation with the Senior Tutor as appropriate, the making of offers of admission of applicants from nontraditional backgrounds; b. co-ordinate the activities of Admissions Staff, Admissions Tutors and Departmental/Degree Programme Tutors on all issues concerning the admission, induction and progress of undergraduate students in the Faculty; c. communicate on behalf of the Faculty and UCL with Local Authorities, professional, regulatory and statutory bodies, other funding bodies, other universities, commercial organisations and the media etc. on all issues concerning the registration and progress of undergraduate students within the Faculty; d. attend, or nominate a representative to attend, the Final Boards of Examiners Meetings for undergraduate degree and taught Masters degree programmes. MBBS Admissions Responsibilities: To manage admissions to Y1 of MBBS programme and the Admissions Office (Faculty Tutor Years 1-3) To manage widening participation activities (Faculty Tutor Years 1-3) To manage admissions to Y4 of the MBBS programme (Faculty Tutor Years 4-6) To manage admissions to the MBPhD programme (Faculty Tutor Years 4-6) MBBS Committees: Chair of the Admissions Board (Faculty Tutor Years 1-3) Deputy Chair of MBBS Student Support Committee (Faculty Tutor Years 4-6) Chair of Student Support Tutor meetings (Faculty Tutor Years 4-6) Member of MBBS Executive Committee Member of FMS Teaching Committee Member of FMS Board of Examiners Member of MBBS Teaching Committee and relevant Sub Committees Member of MBBS Board of Examiners and relevant Sub Boards/Panels Member of MBBS Student Staff Consultative Committees Member of Initial Fitness to Practise Panel (Faculty Tutor Years 4-6) Member of the MBPhD Teaching Sub Committee (Faculty Tutor Years 4-6) Lead for Careers and Foundation School Transition 2 notional PAs: UCLMS Administrative support: Medical Student Administration 65 Accountable to: Faculty Tutor (Years 4-6) Term of office: normally 5 years Remit: Overall responsibility for the co-ordination of Careers advice and Foundation School transition throughout the MBBS programme Responsibilities to oversee all matters relating to Careers and Foundation School transition to develop a structured careers support system from Year 1 to Year 5 of the MBBS programme to lead the careers sessions during Year Preparation for Practice Weeks to lead the provision of advice relating to foundation school applications to lead the provision of advice relating to ST training and choice of medical speciality to liaise with UCL careers service to draw on UCL provision and advice on self-presentation on paper and at interview to advise and co-ordinate policies relating to foundation school applications including ranking methods to oversee the calculation and issue of foundation application rankings to oversee transfer of information to foundation school to develop a dedicated Medical School careers website Committees: Chair of Careers and Foundation School Transition Committee Ex officio member of MBBS Teaching Committee Lead for Elective Approval and Health and Safety 2 notional PAs: UCLMS Administrative support: Medical Student Administration Accountable to: Faculty Tutor (Years 4-6) Term of office: normally 5 years Remit: Management of elective attachment for UCL students Management of in-coming elective student programme Responsibilities To oversee the elective attachment To implement health and safety policies To implement academic requirements To approve electives To allocate elective bursaries To manage and develop the v elective programme for students from other medical schools Committees: Member of MBBS Teaching Committee Member of Year 6 Teaching Committee Member of MBBS Student Support Committee Foundation School Director 1 notional PA: UCLMS + 4 notional PAs: North Central Thames Deanery Admin support:Foundation School Manager (80% NT Deanery/20% UCL Medical School) 66 Foundation School Deputy Manager and Quality Assurance (100% NCT Deanery) Foundation School Data Manager School (80% NT Deanery/20% UCL Medical School) Foundation School Administrative Assistant (60% NCT Deanery/40% UCL Medical School) Accountable to: Director of UCL Medical School for UCLMS remit Remit: Lead the Foundation School Admission to Foundation Schools, Foundation Year 1 and Year 2 Progress reports & feedback for UCL graduates Full Registration with GMC for UCL graduates Committees: Member of MBBS Teaching Committee Member of the Year 6 Teaching Committee Vice Dean for Professional Affairs 1 notional PA: UCLMS Administrative support: Medical Student Administration Accountable to: Faculty Tutor (Years 4-6) Term of office: normally 5 years Remit: Fitness to Practise Investigations ACCEA Revalidation To investigate and give advice of Staff FtP issues and complaints from MBBS students To represent UCL on student FtP panels both internally and externally To lead on internal Fitness to Practise investigations To review applications, lead and Chair the UCL ACCEA committee for clinical academic staff and to recommend nominations To review applications and represent UCL on the UCLH ACCEA committee To advise SLMS on revalidation Committees: Chair the MBSB Student Support Committee Member of Initial Fitness to Practise Panels Student Support Tutors 1 notional PA: UCLMS/Trust Administrative support: Medical Student Administration Accountable to: Faculty Tutors Years 1-3 and Years 4-6 Term of office: normally 5 years Remit: To assist the Faculty Tutors in student matters relating to Student Support and guidance To assist the Faculty Tutors in academic matters including registration, fees and assessments To assist the Faculty Tutors in student matters relating to admissions To assist the Faculty Tutors in any other tasks, duties and responsibilities within the scope, spirit and purpose of the role 67 Responsibilities: in association with the Faculty Tutors to provide the lead on the three main teaching sites for pastoral care of clinical students to conduct Student Support Clinics to be responsible for accurate recording of student interviews, whilst gaining consent for information passed on, and preserving student confidentiality. to collaborate with the Faculty Tutors to review student’s academic progress and ensure that each student’s registration, academic progress and examination entry details satisfy the regulations for the MBBS degrees to counsel students who have failed examinations as to their future action to advise students who have difficulty in paying their fees, and make recommendations to the Faculty Tutors about assistance from student hardship funds to counsel students and make recommendations to the Faculty Tutors concerning interruption of studies and exceptional leave to advise students and liaise with the Faculty Tutors concerning fitness to practise issues to deputise for the Faculty Tutors as necessary in the administration of the course, by becoming a signatory where possible, and writing student references to assist the Faculty Tutors in any other tasks, duties and responsibilities within the scope, spirit and purpose of the role Committees: Member of MBBS Student Support Committee Member of MBBS Student Support Tutors Committee Member of MBBS Teaching Committee and relevant Sub Committees Member of MBBS Board of Examiners and relevant Sub Committees Member of MBBS Staff Student Liaison Committees Member of MBBS Admissions Board Student Counsellors 1 notional PA: UCLMS Administrative support: Medical Student Administration Accountable to: Faculty Tutors Years 1-3 and Years 4-6 Term of office: normally 5 years Remit: To conduct student counselling clinics for MBBS students To assist the Faculty Tutors in student matters relating to Student Support and guidance To assist the Faculty Tutors in any other tasks, duties and responsibilities within the scope, spirit and purpose of the role Departmental Equal Opportunities Liaison Officer Medical Student Administration Accountable to: Director of UCL Medical School via the Head of Medical Student Administration Remit: to help the Head of Department with the implementation of UCL's Equal Opportunities Policies and practice at a departmental level. This will include assisting the department with developing and implementing departmental Equality Action Planning initiatives, assisting disabled colleagues with 68 applications to the Access to Work Scheme and in Science, Engineering and Technology (SET) departments, assisting the department with initiatives that advance the careers of women in SET. to be a local resource within the department to whom staff and students can come for information and advice, distributing and drawing attention to new equality developments and legislative change and ensuring staff and students are conversant with UCL's EO policies and procedures being the first point of contact for personal equal opportunities issues within the department liaising with the Head of Department about implementation of equal opportunity good practice within the department and corporately to provide valuable feedback about equal opportunity implementation at a departmental level, on any specific issues, problems or successes within your department. 69 UCL Medical School MBBS Leadership Assessments 1) OVERVIEW OF MBBS ASSESSMENT MANAGEMENT ...................................................................71 2) LEADERSHIP ROLES .................................................................................................................72 Academic Lead (Assessment) ............................................................................................72 MBBS Academic Leads Years 1-3 and 4-6 ...........................................................................72 MBBS Year Leads and Deputy Year Leads ..........................................................................73 MBBS Module Leads and Subject/Specialty Leads ..............................................................73 Standard Setting Leads.....................................................................................................74 OSCE Leads ......................................................................................................................74 OSCE Site Leads................................................................................................................74 OSCE Deputy Site Leads ....................................................................................................75 70 1) OVERVIEW OF MBBS ASSESSMENT MANAGEMENT UCL Medical School is responsible for assessment strategy, policy, innovation and development and for coordinating the appropriate delivery of in-course, formative and summative assessments. This is achieved by providing high level assessment leadership and drawing on operational oversight and implementation commissioned from the SLMS Faculties of Life Sciences, Brain Sciences, Medical Sciences and Population Health Sciences and from Central and Associated Provider Trusts. Within UCL Medical School: The Director of UCL Medical School and the Deputy Director/UG Programme Lead are responsible for assessment strategy, policy and quality assurance across the programme. The Director of UCL Medical School chairs the MBBS Board of Examiners and the Final MBBS Board of Examiners which determines qualification. The Academic Lead for Assessment is responsible for advising on assessment design, innovation and good practice; for ensuring compliance with MBBS assessment strategy and policy; and for ensuring compliance with agreed examination formats, style and presentation. The Academic Lead for Assessment chairs the MBBS Board of Examiners, the Year 6 Panel of Examiners and OSCE Sub Panels. The Academic Leads for Years 1-3 and 4-6 are responsible for ensuring appropriate academic content and standards in their part of the programme and for operational oversight of examinations. The Academic Leads for Years 1-3 and 4-6 chair the Sub Boards of Examiners which determine progression to the next year of the programme. Within SLMS Faculties and NHS Trusts: The Academic Leads for Years 1-6 are responsible for the co-ordination and implementation of the examinations in their year of the programme, for ensuring appropriate academic content, standards and balance, and for ensuring appropriate action in response to feedback from external examiners. The Academic Leads for Years 1-6 chair the Panels which compile the papers and oversee the Sub Panels of Examiners which compile the OSCEs. Academic Year Leads may appoint Deputy Year Leads to oversee operational aspects of assessment delivery. The Module and Specialty Leads in each year of the programme are responsible for providing appropriate assessment materials within their module and specialty, for ensuring participation by module and specialty teachers in question writing, standard setting and practical/clinical examinations. Normally Module Leads act as OSCE Site Leads in Years 4 and 5 and Site Education Leads act as OSCE Site Leads in Year 6. Module and specialty Teachers in each year of the programme are responsible for participating in question writing, standard setting and examining. Individuals drawn from the modules are responsible for chairing Standard Setting Groups and Sub Panels of Examiners (Clinical). 71 2) LEADERSHIP ROLES Academic Lead (Assessment) 2 notional PAs: UCLMS Administrative support: Medical Student Administration Accountable to: the Director of UCL Medical School via the Deputy Director/Lead for Undergraduate programmes Term of office: normally 5 years Responsibilities: To advise on assessment design, innovation and good practice To inform and ensure compliance with MBBS assessment strategy and policy and to set an appropriate assessment agenda To ensure that the decisions of the UCL Medical School Teaching Committee and MBBS Board of Examiners are implemented via the Year Boards/Panels of Examiners To maintain oversight of question banks and ensure compliance with agreed question formats and styles To ensure that standard setting processes are applied correctly To ensure standard presentation and accuracy of assessment documentation including mark schemes To oversee and facilitate the implementation of MBBS assessments throughout the MBBS programme To ensure that Sub Boards of Examiners are conducted correctly To oversee quality assurance including ensuring appropriate review of external examiners’ reports by Year assessment leads, ensuring appropriate responses and action, and reporting annually to UCL on assessment in all parts of the programme Examination Boards: Member of Faculty Board of Examiners Chair of MBBS Board of Examiners Chair of Year 6 Panel and Sub Panel of Examiners and Member of relevant Sub Boards and Panels of Examiners MBBS Academic Leads Years 1-3 and 4-6 2 notional PAs to cover curriculum and assessment roles: UCLMS Administrative support: Medical Student Administration Accountable to: Director of UCL Medical School via the Deputy Director /Lead for Undergraduate programmes Term of office: normally 5 years Responsibilities: To oversee assessment standards and academic content in Years 1-2 and Years 4-6 To ensure appropriate assessment standards and academic content in Years 1-2 and 4-6 To maintain operational oversight of assessment in Years 1-2 and Years 4-6 To oversee standard setting and ensure that appropriate pass marks are set To determine progression to the next year of the programme Examination Boards: Chair of relevant Examination Sub Board Member of relevant Examination Panels and Sub Panels 72 MBBS Year Leads and Deputy Year Leads 2 notional PAs to cover curriculum and assessment roles: Division or Trust Administrative support: Medical Student Administration Accountable to: Deputy Director/Lead for UG Programmes via the Academic Lead for Years 1-3 or 4-6 Term of office: normally 5 years Year Leads may appoint Deputy Year Leads to assist with operational aspects of assessments. Responsibilities: Ensuring assessment design and delivery for progression tests and formative assessments including: odeveloping question banks oblueprinting written assessments and clinical assessments ocompiling and editing question papers ooverseeing marking processes and the production of mark sheets and results ooverseeing standard setting oreceiving , acting on and reporting annually on comments from external examiners on the standard, conduct and outcome of examinations omaking recommendations for the award of prize Examination Boards: Chair of relevant Examination Panels Member of relevant Sub Panels and Standard Setting Groups Member of MBBS Board of Examiners MBBS Module Leads and Subject/Specialty Leads Module Leads: 2 notional PAs to cover curriculum and assessment responsibilities– Divisional Student load/Trust SIFT Specialty Leads: 1 notional PA to cover curriculum and assessment responsibilities– Divisional Student load/Trust SIFT Admin support: Divisions/Trusts Accountable to: Academic Leads for relevant year Responsibilities: To co-ordinate in-course assessments, workplace based assessments, module/firm assessments To participate in writing and reviewing assessment materials To participate in standard setting To provide appropriate assessment materials for formative and summative assessments To work with the Year Lead and Module Management Group to ensure the provision of high quality assessment materials from module and firm teachers for formative and summative written, practical and clinical examinations To work with the Year lead and Module Management Group to ensure participation by module and firm teachers in standard setting processes and clinical examinations To act upon external examiner’s comments and ensure appropriate follow up action In Years 4 and 5, Module Leads act as Site Leads for the clinical examinations Examination Boards: Member of MBBS Board of Examiners Member of Year Sub Board of Examiners 73 Chair of relevant Year Panels and Sub Panels of Examiners Standard Setting Leads Within overall curriculum and assessment responsibilities – Divisional Student load/Trust SIFT Admin support: Divisions/Trusts Accountable to: Academic Leads for relevant year To co-ordinate standard setting for relevant year of the programme Examination Boards: Member of Year Sub Board of Examiners Member of relevant Year Panels and Sub Panels of Examiners Chair of relevant Standard Setting Group OSCE Leads Within overall curriculum and assessment responsibilities – Divisional Student load/Trust SIFT Admin support: Divisions/Trusts Accountable to: Academic Leads for relevant year To co-ordinate the clinical examinations for relevant years of the programme Examination Boards: Member of Year Panel of Examiners Chair of the Year Sub Panel of Examiners (Clinical) OSCE Site Leads Within the role of Site Sub Dean for Year 6 and within the role of Module Leads for Year 5 and Year 4. Admin support: Divisions/Trusts Accountable to: Academic Leads for relevant year Assisted by Deputy Site Leads drawn from UCLMS CTFs Responsibilities: To lead and co-ordinate the delivery of clinical assessments locally To ensure the provision of appropriate venues and facilities To ensure sufficient and appropriate recruitment of local examiners To oversee recruitment of patients by Deputy Site Leads To oversee preparation of patient summaries and other materials by Deputy Site Leads To conduct examiner briefings prior to each OSCE circuit To cover for absent examiners where necessary To ensure OMR mark sheets are filled in according to regulations and to discuss with examiners any irregularities in the mark-sheets or conduct of the examination so that corrective action can be taken To rotate through the stations in reverse order to provide quality control for examiners. To liaise with and facilitate QS monitoring by External Examiners at the OSCEs To make a report of any examination incidents affecting the performance of examiners or candidates to the Sub Board of Examiners To act upon student feedback where this has identified issues which require attention To review and respond to external examiners’ comments and ensure appropriate follow up action Examination Boards 74 : Member of MBBS Board of Examiners Member of relevant Sub Boards Member of relevant Year Panels of Examiners Member of relevant Year Sub Panels (Clinical) OSCE Deputy Site Leads Drawn from CTFs within ULCMS Responsibilities: To assist OSCE Site Leads with the delivery of clinical assessments locally To contribute to OSCE station writing and review To prepare scenario materials To prepare candidate and examiner instructions To facilitate and ensure the delivery of examiner and candidate briefings prior to each circuit To assist with recruitment of examiners locally To ensure that OSCE sites and stations are set up appropriately To cover for absent examiners where necessary Discuss with the examiners any irregularities in the mark-sheets or the conduct of the examination so that corrective action can be taken as soon as possible. Once the examination is running smoothly, rotate through the stations in reverse order to provide quality control for examiners. 75 Compiled and edited by: Professor Jane Dacre, UCL Medical School Ms Gaynor Jones, Medical Student Administration (MSA) MBBS Committees UCL Faculty Teaching Committees ................................................................................................77 UCL Divisional Teaching Committees/MBBS Teaching Committee.............................................79 Admissions and Widening Participation Board.............................................................................81 Teaching Committees......................................................................................................................82 Vertical Modules Teaching Committee ............................................................................................82 Year Teaching Committees...............................................................................................................82 Year 3/IBSc Steering Committee ......................................................................................................83 Horizontal and Vertical Module Management Groups....................................................................84 Horizontal and Vertical Module Implementation Groups ...............................................................85 MBPhD Committee...........................................................................................................................85 Educational Facilities and Resources Committee.........................................................................86 Quality Management and Enhancement Committee .....................................................................87 Student Support...............................................................................................................................88 Student Support Committee .............................................................................................................88 Careers and Foundation School Transition Committee.................................................................89 UCL/MBBS Staff-Student Consultative Committees (UCL Academic Manual) ............................90 For organisational charts and chairs of committees see: http://www.ucl.ac.uk/medicalschool/staffstudents/committees 76 UCL Faculty Teaching Committees The following are terms of reference set out in UCL’s Academic Manual. The following should be regarded as core terms of reference for FTCs. Faculties may have separate UG and Graduate Teaching Committees. This list of items should not be regarded as exhaustive. Subject to any general or particular direction which may be prescribed from time to time by the Academic Committee and/or the relevant Faculty Teaching Committee(s), the Faculty Teaching Committee(s) will normally be expected: 1. Within the framework of the UCL Learning and Teaching Strategy, to define, develop and review a facultylevel learning and teaching strategy and/or oversee the definition, development and review of divisionallevel learning and teaching strategies by divisions within the faculty. 2. Within the framework of Academic Committee statements of policy and good practice in respect of quality management and enhancement (QME), to define, develop and keep under regular review faculty QME processes and mechanisms. 3. To keep under review the teaching provision across the faculty and to provide a forum for discussion of issues raised by Divisional Teaching Committees (DivTC). 4. To consider the academic and resource implications of new degree programmes from divisions within the faculty and, if and when satisfied, submit these for consideration by the Academic Committee's Programme Development Executive Sub-Committee (or relevant sub-group thereof). For undergraduate Medicine, proposals for new intercalated degree programmes which contribute to the MBBS programme but are taught in other faculties should be endorsed by the MBBS Teaching Committee. 5. To consider the academic and resource implications of proposals for new or amended course units from divisions within the faculty and, if and when satisfied, submit these to the Registry for approval. 6. To receive and consider programme reviews from divisions within the faculty and, if and when satisfied, submit these to the Academic Committee's Programme Development Executive Sub-Committee (or relevant sub-group thereof). For undergraduate Medicine, including IBSc’s, this is via Divisional Teaching Committees reporting through the MBBS Teaching Committee 7. To receive, in accordance with UCL policy2, reports from DivTCs on the operation of peer observation of teaching and ensure that any issues arising from such reports are followed-up appropriately with the DivTC(s) concerned. For undergraduate Medicine, this is via Divisional Teaching Committees reporting via the MBBS Teaching Committee 8. To receive analyses from DivTCs of the results of student evaluation questionnaires. For undergraduate Medicine, this is via the Medicine Quality Management and Enhancement Committee. 9. To monitor the proceedings of the DivTCs by routinely receiving the Minutes of meetings. For undergraduate Medicine, this is via the MBBS Teaching Committees and Module Management Groups. 10. To monitor the minutes and proceedings of DivTCs and to ensure that such committees have student representatives, as required by UCL policy. For undergraduate Medicine, this is via the MBBS Teaching Committee. 11. To receive reports on or to consider, as appropriate, relevant issues arising from meetings of Academic Committee3. 12. To report to Academic Committee by the submission of Minutes of each meeting of the FTC to the officers of Academic Committee. 13. To report to the Faculty Board (if required by the Board). 77 Constitution The following should be regarded as comprising minimum requirements for the constitution of a FTC: Undergraduate Dean and/or Vice Dean Faculty Tutor Chairs of DivTCs and/or Divisional Undergraduate Tutors One member of staff from each department within the faculty which offers a BSc programme (e.g., Chair of DivTC and/or Departmental Tutor) Graduate Dean and/or Vice Dean Faculty Graduate Tutor One member of staff from each department within the faculty (e.g., Chair of DivTC and/or Departmental Tutor) Chairs of steering committees of inter-faculty or inter-departmental programmes for which the parent department is from within the faculty. Student Membership: The FTC should include at least one undergraduate and one postgraduate student member4. Committee chairs and/or secretaries should meet the student representatives in advance of the first committee meeting, in order to brief them on the committees' works and proceedings and to put the students at ease and introduce them to key committee members. Committee Secretary FMS Graduate Administrator 1. The term 'faculty' as used in this document should therefore be understood to mean 'faculty' or 'PGI'. 2. UCL's policy on peer observation of teaching is at Document E19 of the Academic Manual at http://www.intranet.ucl.ac.uk/staffandstudent/reference/acman/PartE/E19.html 3. It is recommended that receipt of a report on the proceedings of the most recent meeting(s) of Academic Committee (or other relevant institutional-level committees) should be a standing item on the agendas for meetings of FTCs. 4. If the FTC agenda includes business which the Chair feels should not be discussed in the presence of student members, there should be a separate, Reserved Area of Business section of the agenda. 78 UCL Divisional Teaching Committees/MBBS Teaching Committee The following are core Terms of Reference for Divisional Teaching Committees (DivTCs) set out in UCL’s Academic Manual. Subject to any general or particular direction which may be prescribed from time to time by the Academic Committee and/or the relevant Faculty Teaching Committee(s), the Divisional Teaching Committee will normally be expected: 1. Within the framework of the UCL learning and teaching strategy, to define and develop a departmental learning and teaching strategy and to review annually the strategy and progress being made towards the achievement of its aims. 2. Within the framework of Academic Committee and Faculty Teaching Committee statements of policy and good practice in respect of quality management and enhancement (QME), to define, develop and keep under regular review departmental QME processes and mechanisms. 3. To consider and approve proposals to institute, amend, revise or withdraw courses or programmes, for forwarding to the appropriate faculty committees or officers 4. To oversee arrangements within the division for course and programme review, according to the programme review processes and timetable defined by the relevant Faculty Teaching Committee(s). 5. To devise individual course/programme student questionnaires according to guidance prescribed by the Faculty Teaching Committee and/or the UCL Guidelines for Good Practice (Gold Book). 6. To receive and monitor the findings of analyses of student questionnaires and to define and keep under review mechanisms for feedback to students on the outcome of such questionnaires. 7. To review annually the division’s arrangements for Induction Week. 8. To receive the divisions Self-evaluative Statement for Internal Quality Review (IQR) and approve this for forwarding to the IQR team. 9. To report to the Head of Department (either via the Departmental Staff Meeting or through such other mechanism as the Head of Department sees fit) by submission of the Minutes of each meeting of the Committee to the Head. 10. To report to the Faculty Teaching Committee(s) concerned by submission of Minutes of each meeting of the Committee to the officers of the relevant Faculty Teaching Committee(s). MBBS Teaching Committee devolves specific responsibilities for the MBBS programme to the MBBS Sub Committees which report to it, and devolves responsibility for overseeing IBSc programmes which are taught in other departments to the IBSc Steering Committee which reports to it. The following are additional terms of reference specific to MBBS Teaching Committee: 1. To review the academic and resource implications of the MBBS programme overall and to monitor HEFCET allocations and budgets in liaison with the divisions that contribute to the programme. 2. To ensure adequate liaison with NHS Teaching Trusts in the development and delivery of local teaching within NHS premises and by NHS staff, and to ensure similar liaison with other providers. 3. To oversee the management of student numbers in the MBBS programme including MBBS entry to Year 1 and Year 4 (Oxbridge), Year 3/IBSc numbers and MBPhD numbers. 4. To oversee and approve arrangements for GMC visits and inspections. 5. To liaise with the North Central Thames Foundation School in their provision of F1 and F2 jobs and the related application process. 79 6. To oversee the appointment procedures for FY posts and, as far as it is possible, the arrangements for monitoring the quality of FY posts for their clinical experience and training content via the Careers/Foundation School Transition Committee. 7. To oversee the management of admissions to the MBBS programme via the MBBS Admissions Board. 8. To oversee the management of IBSc programmes via the Year 3/IBSc Steering Group. 9. To oversee the management of the MBBS curriculum via the MBBS Teaching Committees and Module Management Groups. 10. To oversee the management of quality assurance processes and quality assurance visits via the MBBS Quality Management and Enhancement Committee. 11. To oversee the management of educational facilities and resources via the MBBS Educational Facilities Committee. 12. To oversee the management of SIFT liaison and strategy and to monitor the SIFT allocations and budgets via the MBBS Executive Group. 13. To oversee the management of student support via the MBBS Student Support Committee. 14. To oversee the management of the MBPhD programme via the MBPhD Committee. 15. To receive the minutes of the MBBS Staff Student Consultative Committees and to ensure that concerns are addressed appropriately. 16. To report minutes to SLMS Faculty Teaching Committees to enable Faculties to monitor the implementation of MBBS teaching commissioned in their faculty and to take appropriate actions. 17. To be responsible for all matters relating to the design, development, delivery, evaluation and review of the MBBS curriculum. 18. To consider proposals for curriculum innovation submitted by the Academic Centre for Medical Education and the MBBS Teaching Committees. 19. To consider the recommendations of the Year 1 and Year 2, Year 3, Year 4 and Year 5 Sub-Boards of Examiners and the UCL Medical School Board of Examiners and issues arising from in-course assessment, progression and Final Examinations for students enrolled on the MBBS course. 20. To ensure the satisfactory discharge of the School's responsibilities under the Medical Act 1983 and to advise the Dean of the Medical School on the curricular implications of government initiatives, General Medical Council recommendations and NHS Workforce Confederation initiatives. 21. To have an overview of MBBS publications and learning resources Meetings The DivTC should normally meet at least once in the Autumn Term each year and at least once in the Spring Term each year. Departments are encouraged to convene the DivTC more frequently if they see fit to do so. Faculty monitoring of DivTC operations As indicated in the core terms of reference, FTCs (UG and Graduate) should routinely receive the Minutes of DivTC meetings. Membership 80 Chair: Director of UCL Medical School Deputy Director/UG Programme Lead Academic Lead (Years 1-3 and 4-6) Academic Lead (Vertical Modules) Academic Lead (Assessments) Academic Lead (Quality Assurance) Site Sub Deans (RF, Whit, UCLH, DGH, Community) Year Leads Careers/Foundation School Transition Lead Electives Lead IBSc Lead MBPhD Lead Horizontal Module Leads Vertical Module Leads Faculty Tutors Years 1-3 and 4-6 Vice Dean (Professional Affairs) Medical School Student Support Tutors Foundation School Director Head of Medical Student Administration Deputy Heads of MSA MSA QA Administrator MSA VM Administrator MSA Year Administrators Library representatives Elected representatives from the 4 SLMS Faculties Student representatives Committee Secretary Deputy Head of MSA (Years 4-6) Admissions and Widening Participation Board Terms of Reference To receive data and analysis relating to recent UCAS admissions cycles To review admissions requirements To review the performance of current students and to evaluate the effects of changes to admission policies on the intake of students Membership Chair: Faculty Tutor (Years 1-3)/Admissions Lead Deputy Chair: Faculty Tutor (Years 4-6) Director of UCL Medical School Deputy Director of UCL Medical School/UG Programme Lead Vice Dean for Education (Life Sciences) Faculty Tutor (Life Sciences) Medical School Support Tutors Lead for Careers/Foundation School Transition Academic Lead (Vertical Modules) MBBS Year Leads UCL Head of Admissions UCLMS representatives Student representative(s) Committee secretary Principle Admissions Officer 81 Teaching Committees Vertical Modules Teaching Committee Terms of Reference Teaching To receive the minutes of the MBBS Teaching Committee and to ensure compliance with policies and recommendations from the MBBS Teaching Committee To make recommendations to MBBS Teaching Committee on matters relating to the design, development and delivery of the Vertical Module components of the MBBS To receive the minutes of Vertical Module Management Groups, to report relevant issues to MBBS Teaching Committee, and to monitor actions required and actions taken To report minutes to Divisional Teaching Committees where appropriate and to monitor action required and taken by divisions To ensure that the VM teaching that the students receive is compatible with the curriculum To co-ordinate the VM Study Guides and Moodle sites Quality Assurance To receive the minutes of the Quality Management and Enhancement Committee (mQMEC) To ensure compliance with QA recommendations and requirements To ensure that appropriate quality assurance mechanisms are in place in each module To review student feedback To co-ordinate and return annual monitoring reports to the Quality Unit Membership Chair:Academic Lead (Vertical Modules) Deputy: Academic Leads (Years 1-3 and 4-6) Vertical Module Leads/Chairs of Vertical Module Management Groups Year Leads Medical Student Administration representatives Student representative(s) Committee secretary Vertical Modules Administrator Year Teaching Committees Terms of Reference Teaching To receive the minutes of the MBBS Teaching Committee and to ensure compliance with policies and recommendations from the MBBS Teaching Committee To make recommendations to MBBS Teaching Committee on matters relating to the design, development and delivery of relevant modules To receive the minutes of relevant Module Management Groups/Trust UG Teaching Committees, to report relevant issues to MBBS Teaching Committee, and to monitor actions required and actions taken To co-ordinate and monitor all aspects of teaching delivery and ensure that the requirements of the MBBS curriculum are fulfilled To co-ordinate Year Guides and other relevant publications and on-line resources To report minutes to Divisional Teaching Committees where appropriate and to monitor action required and taken by divisions To receive minutes and reports from the relevant Staff Student Consultative Committee and to ensure appropriate actions are taken in response to student concerns Quality Assurance To receive the minutes of the Quality Management and Enhancement Committee (mQMEC) To ensure compliance with QA recommendations and requirements 82 To ensure that appropriate quality assurance mechanisms are in place in each module To review and act upon student feedback To co-ordinate and return annual monitoring reports to the Quality Unit Membership Chair: Year Lead Deputy: Academic Lead (Years 1-3 or 4-6) Director of UCL Medical School Deputy Director/UG Programme Lead Academic Lead (Assessment) Academic Lead (Quality Assurance) Academic Lead (Vertical Modules) Horizontal Module Leads Site Sub Deans Faculty Tutors (Years 1-3 and 4-6) MSA Deputy Heads (Years 1-3 or 4-6) MSA Year Administrators MSA QA Administrator MSA VM Administrator MSA IT/Timetabling Administrator (Y1/Y2 only) Cruciform Education Facilities Manager (Y1/Y2 only) Library representatives Medical Student representatives Additional representation in Year 6: Trust UG Tutors Foundation School Director Foundation School Manager SIFT Officer Committee Secretary Deputy Head of MSA for Years 1 and 2 MSA Year Leads for Years 4, 5 and 6 Year 3/IBSc Steering Committee Terms of Reference The Year 3/IBSc Steering Committee is responsible for managing and monitoring all aspects of the IBSc programmes conducted in any Faculty or Division in accordance with UCL regulations and in accordance with policies and procedures agreed for the MBBS programme. The Year 3/IBSc Steering Committee reports to the MBBS Teaching Committee on matters relating to the curriculum, and to the MBBS Examination Board on matters relating to assessments. Proposals for new or amended programmes of study are received and approved by UCL Education Committee. The Year 3/IBSc Lead is responsible for the overall management of IBSc programmes, admissions and student quotas within agreed MBBS policies. Faculty Tutors are responsible for courses within their Faculty. Teaching To ensure that IBSc programmes of study irrespective of Faculty are conducted in accordance with the regulations for each programme of study and are appropriate to the award of the IBSc. To monitor existing IBSc programmes and course unit components. To consider changes to existing IBSc programme and course unit components and to approve PAQs (Programme Amendment Questionnaires) and UPCAMs (Undergraduate Programme Component Amendment Forms). To consider new IBSc programmes and to liaise where necessary regarding PIQs (Programme Initiation Questionnaires) To determine and review the application process 83 To manage IBSc places and admissions To update the IBSc booklet and website annually Assessments To ensure that assessment procedures within the Faculty hosting an IBSc are administered in accordance with College and individual programme regulations and in a proper and impartial manner. To ensure that Boards of Examiners are set up for every IBSc programme Faculty and to make appropriate arrangements for the examination of programmes shared with other faculties. To ensure recommendations have been made to the College Board of Examiners for the Internal External and Visiting Examiners, Chairs and Deputy Chairs for each Board of Examiners. To approve and monitor a unified marking scheme, including schemes for Award of Honours or undergraduate degrees, for each Board of Examiners. To receive the Minutes from meetings at which recommendations for the final award are made from each Board of Examiners. To receive and approve recommendations for the deans list, Faculty Medal, Jackson Lewis and HAB Simons awards and inform Graduation and student awards office. To receive and approve applications for postponement of the award of Honours for undergraduate degrees. To receive and consider the responses of Chairs of Board of Examiners to visiting Examiners’ reports. To receive reports from the Board of Examiners of any problems related to the operation of the procedures of the Board of Examiners and to monitor any action taken by Boards in respect of such problems. To receive information and monitor distribution of degree classification for each programme To provide a summary for the Faculty Boards of Examiners of the responses made to visiting examiners reports and to ensure that appropriate action has been taken where required Quality Assurance To receive reports from internal quality and subject reviews and annual monitoring reports and to ensure and monitor required action To receive student feedback questionnaires and to address generic issues relating to the IBSc degrees To receive minutes from IBSc Staff Student Consultative Committees and to address any generic issues Membership Chair: Year 3/IBSc Lead Academic Leads (Years 1-3 and 4-6) Year Leads Faculty Tutors (all faculties offering IBScs) IBSc Tutors (all programmes) Student Representatives Committee Secretary Year 3/IBSc Administrator Horizontal and Vertical Module Management Groups Terms of Reference Teaching To report on and make recommendations about module teaching and content to the relevant Year Teaching Committee To co-ordinate and monitor all aspects of module teaching delivery and ensure that the requirements of the MBBS curriculum are fulfilled To co-ordinate module guides other relevant publications and on-line resources To review module/site timetables to ensure that there is equivalence in the teaching provided at each site To report minutes to Divisional Teaching Committees where appropriate and to monitor action required and taken by divisions 84 To ensure integration within the module and with other components of the programme Assessment To ensure submission of appropriate written questions for formative and summative assessments To ensure submission of appropriate OSCE stations for formative and summative assessments To ensure and monitor participation in question writing, standard setting and OSCE examining by module teachers To ensure and monitor participation in OSCE examining by module teachers To co-ordinate and monitor delivery of required in-course and module assessments and to ensure that students are assessed to a common standard Quality Assurance To ensure compliance with QA recommendations and requirements To ensure that appropriate quality assurance mechanisms are in place in each module To review and act upon student feedback To return annual monitoring reports for the module to the relevant Year Teaching Committee Membership Chair: Module Lead Deputy Chair: Deputy Module Lead Academic Leads (Years 1-3 or 4-6) Horizontal Module teachers relevant to module Vertical Module teachers relevant to module Faculty Tutors (Years 1-3 or 4-6) MSA administrators Divisional MBBS teaching/placements administrators Committee Secretaries Module Administrators/Co-ordinators Horizontal and Vertical Module Implementation Groups Module Implementation Groups may be constituted as working groups reporting to Module Management Groups. Terms of Reference To report to MMGs To advise and to report to MMGs on the design of new modules To advise and to report to MMGs on the implementation of components To develop new initiatives and innovations To timetable and implement teaching on behalf of MMGs Membership Module Lead Representatives drawn from the MMG Representatives from other modules by invitation Divisional Module Administrator/Co-ordinator Committee Secretaries Module Administrators/Co-ordinators MBPhD Committee Terms of Reference 85 To report to the MBBS Teaching Committee and to advise on matters relating to admission to, design, development, delivery, assessment and quality assurance of the MBPhD programme. To co-ordinate and transmit to MBBS Teaching Committee issues arising from the MBPhD Programme. To receive details of PhD funding arrangements. To oversee the MBPhD Alumni Scheme. The Committee shall meet three times per year (October, January and May). Membership Chair: Academic Lead (MBPhD) Director of UCL Medical School Deputy Director/UG Programme Lead Faculty Tutor (Years 4-6) MBPhD Programme Director Director, Division of Medicine MBPhD Administrator Director of Medical School Management Head of Medical Student Administration Student Representative Committee Secretary MBPhD Administrator Educational Facilities and Resources Committee Terms of Reference To send representation to the SLMS Facilities and Resources Committee, via the Director of UCL Medical School, to ensure support and provision of facilities to meet the needs of the MBBS curriculum To report to and to make recommendations to the MBBS Teaching Committee, MBBS Quality and Management and Enhancement Committee and SLMS Deans concerning the facilities and resources required to deliver the MBBS curriculum To monitor and review the provision, function, and support of educational facilities across all medical school and NHS sites and through all stages of the curriculum To consider and advise on how best the provision of facilities can meet the needs of the medical curriculum To receive notice and to address problems relating to facilities and physical resources at NHS sites via the site sub-deans/ trust undergraduate teaching committees To receive notices concerning library facilities and resources To receive notices concerning IT and e-Learning facilities resources To set up from time to time specific working groups to review the needs of the curriculum and level of support required and advise on how best this can be delivered to match educational needs with appropriate resources The committee will meet three times a year Membership Chair: Site Sub Dean (UCLH) Director of UCL Medical School Site Sub Deans (Royal Free, Whittington, UCLH) Academic Leads (Years 1-3 and 4-6) Year Leads Clinical Skills Centre Manager (UCLH Campus) Cruciform Centre Manager Head of Medical Student Administration MSA IT/Timetabling Administrator Joint Academic Support Managers: Biomedicine, UCL Library Services SIFT Officer SLMS Facilities and Resources Committee representative Faculty Manager (FMS) 86 Student representative(s) Committee Secretary UCLMS Estates and Staffing Administrator Quality Management and Enhancement Committee Terms of Reference Overall function The Medical School Quality Management & Enhancement Committee (mQMEC) is responsible for the overview of academic standards and quality assurance and enhancement processes within the Medical School and in the development of policy and practice in relation to such processes. The mQMEC reports to the MBBS Teaching Committee, the Dean of the Faculty of Medical Sciences, the Faculty Undergraduate Teaching Committees of Brain Sciences, Life Sciences, Population Health Sciences and Medical Sciences. Main objectives and functions The main objectives and functions of the Quality Management and Enhancement Committee are subject to any general or particular direction that may, from time to time, be given by the Director of the Medical School and the Faculty Teaching Committees of Brain Sciences, Life Sciences, Population Health Sciences and Medical Sciences. The Committee will monitor the activities of the Quality Assurance Agency for Higher Education and of other external bodies concerned with the assurance of quality and/or standards insofar as they impinge on the Medical School and to advise the Director, the UCL Education Committee, the MBBS Teaching Committee and the Faculty Teaching Committee accordingly. The Committee will promote the development at Faculty and Departmental levels of initiatives relating to quality enhancement and the enhancement of academic standards. The Committee is responsible for the planning of the preparatory work involved in Internal Quality Audits of the Medical School carries out under the auspices of University College London’s Internal Quality Review procedure. The Committee will plan and coordinate the work of the Medical School in preparing the formal or informal visits by the education committees of the General Medical Council or other validating professional bodies. The Committee will promote discussion and sharing of good practice between the departments of the Medical School in relation to quality assurance and enhancement. The Committee will discuss any issues raised by the on-line student evaluation feedback. Organisation and structure The members of the Committee are appointed ex officio, and include the Vice Chair, UCL Education Committee, who is in a position to feed back to College QMEC. The Committee will meet regularly on quarterly basis. The Committee is serviced by the Quality Assurance Unit 87 Membership Chair: Academic Lead (Quality Assurance) Deputy Chair: Academic Lead (Years 1-3) Director of Medical Education Deputy Director/UG Programme Lead Academic Lead (Years 4-6) Academic Lead (Vertical Modules) Year Leads Chairs of MBBS Sub Committees Site Sub Deans (x5 – RF, Whitt, Bloom, DGH and Community) Faculty Tutors (Years 1-3 and 4-6) Careers and Foundation School Transition Student Support Tutors Head of Medical Student Administration Deputy Heads of MSA (Years 1-3 and 4-6) MSA VM Lead SIFT Manager Student Representatives (x4) o Junior President o Senior President o Vice-President (Education, Yrs 4-6) o Medical & Postgraduate Student Officer Committee Secretary Quality Assurance Unit Manager The Chairperson is appointed ex officio. In the absence of the Chairperson and Deputy Chairperson the meeting of the Committee will be cancelled. Records The Quality Assurance Unit will prepare and maintain written records of the Committee’s activities, including agendas and minutes of all Committee meetings. This record will be stored electronically on the S: drive and published on the QA website. Student Support Student Support Committee Terms of Reference To report to and make recommendations to MBBS Teaching Committee concerning all aspects of student support including: Occupational Health provision Careers and Foundation School Transition Criminal Record Bureau disclosures Fitness to practise issues Immunisation requirements Welfare, health and conduct issues relating to individual students To act consistently within the Terms of Reference of the UCL Student Support Co-ordinating Committee: Subject to any general or particular direction that may from time to time be given by the Academic Committee, the Student Welfare Co-ordinating Committee is charged by Council: 1. To consider and determine policy statements in respect of all aspects of the welfare of undergraduate and graduate students of UCL. 88 2. To collate information on student welfare and to communicate to departments relevant information to ensure that all students are aware of the full range of welfare activities both within and outside UCL that are available to them. 3. To ensure that those concerned with student welfare work in a structured, co-ordinated and cooperative manner to provide the best service to students. 4. To develop policies and good practice advice on dealing with student welfare problems. 5. To identify and advise UCL on issues where the need to improve student welfare is likely to make additional resource demands. 6. To liaise with other committees and areas of UCL that have activity related to student welfare by cross representation. 7. To report to the Academic Committee (i) by submission of an annual report on the work of the Student Welfare Co-ordinating Committee, and (ii) by submission to Academic Committee Officers of the minutes of each meeting of the Student Welfare Co-ordinating Committee. Membership Chair: Vice Dean (Professional Affairs) or Faculty Tutor Deputy Chair: Faculty Tutor (Years 4-6) Director of UCL Medical School Deputy Director/UG Programme Lead Faculty Tutor (Years 1-3) Medical School Student Support Tutors Head, UCL Student Counselling Service OASIS Manager Occupational Health Representative GP Representative Deputy Head of MSA (Years 1-3) MSA Year Administrators Student Representatives Committee Secretary Deputy Head of MSA (Student Support) Careers and Foundation School Transition Committee Terms of Reference To report and make recommendations to the MBBS Student Support Committee To oversee all matters relating to Careers and Foundation School transition To develop a structured careers support system from Year 1 to Year 6 of the MBBS programme To co-ordinate careers sessions during Year Introduction and Orientation Modules To co-ordinate the provision of advice relating to foundation school applications To co-ordinate the provision of advice relating to ST training and choice of medical speciality To liaise with UCL careers service to draw on UCL provision and advice on self-presentation on paper and at interview To advise and co-ordinate policies relating to foundation school applications including ranking methods To oversee calculation and issue of foundation application rankings To oversee the National Transfer of Information process to the Foundation School in liaison with the Faculty Tutor To oversee student applications for Special Circumstances in liaison with the Faculty Tutor To manage the dedicated Medical School careers website Membership: Chair: Academic Lead (Careers and Foundation School Transition) Deputy Chair: UCL Careers Advisor Director of UCL Medical School 89 Deputy Director/UG Programme Lead Faculty Tutors (Years 1-3 and 4-6) Medical School Student Support Tutors Academic Leads (Yeas 1-3 and 4-6) Academic Lead (Vertical Modules) Year Leads Head of Medical Student Administration Foundation School Manager UCL Careers Advisor Student Representative(s) Committee Secretary: Foundation School Manager UCL/MBBS Staff-Student Consultative Committees (UCL Academic Manual) UCL Practice 1. UCL Regulation for Management 14.5 provides as follows: 'In each academic Department there shall be a Staff-Student Consultative Committee, except that in the Faculty of Medical Sciences a single StaffStudent Consultative Committee shall operate for the MBBS programme as a whole. Each Staff-Student Consultative Committee shall meet at least twice in each academic year. The Head of the Department or, within FMS the Director of UCL Medical School, shall ensure that the constitution and the procedures of this Committee are acceptable to the staff and students of the Department or Faculty. The minutes of each meeting of each such committee shall be forwarded to the Dean of Students, as Chair of the UCL Joint Staff Student Committee (JSSC), for receipt on behalf of the UCL JSSC'. 2. The JSSC also requests that Departments: a) ensure that DSSCC agendas and minutes are produced and circulated to a standard, time-frame (it is recommended that a two week time-frame for production of the minutes from the date of the meeting is a reasonable expectation); b) ensure that DSSCC agendas include a standing item “matters arising from the minutes”, to ensure that feedback on action points raised at previous meetings is reported; c) record in the minutes of each meeting of the Departmental Staff-Student Consultative Committee (DSSCC) the names of those in attendance, giving titles and, for student members, year of study; d) record in the minutes any action to be taken and by whom; e) ensure that the minutes are signed by at least one student member of the DSSCC; f) ensure that the minutes are displayed within the Department and are placed on the departmental web-site; g) submit the minutes of the DSSCC to Departmental Staff Meetings for consideration and action where necessary; h) ensure that committee chairs and/or secretaries should meet the student representatives in advance of the first committee meeting, in order to brief them on the committees' works and proceedings and to put the students at ease and introduce them to key committee members; i) ensure that the DSSCC is aware of the existence and terms of reference of the JSSC; j) ensure an appropriate* level of administrative support from departments to DSSCCs to ensure that they operate to a consistent level and standard; *‘appropriate' is here defined as ‘not a student taking the minutes but a member of administrative staff'. 3. The JSSCC submits an annual summary to the UCL Academic Committee of the operation of the above arrangements. 90 4. At its meeting on 29 November 2000, JSSC agreed the following constitution and terms of reference for 1 DSSCCs . Constitution Head of Department (or Deputy)/Programme Director/Senior member of academic staff; at least one member of staff responsible for undergraduate students; at least one member of staff responsible for taught Masters students*; at least one member of staff responsible for research students*; at least one undergraduate student from each year of study; at least one taught masters student*; at least one graduate research student*; at least one part-time student, where appropriate; the Departmental UCL Union Council representative. * Not required where there is a separate committee for graduate students. Terms of reference to discuss follow-up action resulting from previous DSSCC meetings, in particular any matter which was referred to the Departmental Staff meeting; to comment upon the outcome of degree programme and course evaluation questionnaires and any consequent follow-up action; to receive notification of any Departmental changes with respect to teaching, admissions, and assessment; to comment upon any significant changes to Departmental policy which would have a direct consequence for teaching, admissions, and assessment; to comment upon safety within the Department; to comment upon physical resources within the Department e.g. computer/library facilities etc.; to make students aware of the Departmental Equal Opportunities Liaison Officer. Arrangements for inter-departmental degree programmes 5. Degree programmes that are inter-departmental (with contributions from more than two departments) are required to have a separate, programme based, Staff Student Consultative Committee. Regulations for Management 14.6 and 14.7 provide as follows: 14.6 Subject to the provisions of Regulation 14.7 below, there shall be, for each combined studies degree programme operating within UCL and involving more than two Departments of UCL, a Staff-Student Consultative Committee, which shall meet at least twice in each academic year. The academic staff responsible for the co-ordination of such a degree programme shall ensure that the constitution and procedures of this committee are acceptable to the staff and students involved in the degree programme. The minutes of each meeting of each such committee shall be forwarded to the Dean of Students, as Chair of the UCL Joint Staff-Student Committee, for receipt on behalf of the UCL Joint Staff-Student Committee. 14.7 Where the academic staff responsible for the co-ordination of a combined studies degree programme operating within UCL and involving more than two Departments of UCL consider that it will not be appropriate for a separate Staff-Student Consultative Committee to operate for the degree programme in question, those staff shall ensure that the views of students following the programme can be expressed instead either through (i) the Staff-Student Consultative Committees of the Departments concerned, as prescribed in Regulation 14.4, or through (ii) an annual meeting which all students following the programme shall be invited to attend, or through both (i) and (ii). 6. At its meeting on 29 November 2000, JSSC agreed the following constitution and terms of reference for 1 programme based SSCCs . Constitution The Programme Co-ordinator; The Programme Tutor(s); at least one student from each year of study; at least one part-time student, where appropriate; the Departmental UCL Union Council representative(s). Terms of Reference to discuss follow-up action resulting from previous meetings, in particular any matter which was referred to a Departmental Staff meeting; to comment upon the outcome of degree programme and course evaluation questionnaires and any consequent follow-up action; 91 to receive notification of any Departmental changes with respect to teaching, admissions, and assessment; to comment upon any significant changes to Departmental policy which would have a direct consequence for teaching, admissions, and assessment; to comment upon safety within the Department(s); to comment upon physical resources within the Department(s) e.g. computer/library facilities etc.; to make students aware of the Departmental Equal Opportunities Liaison Officer(s). Details of Faculty practice 7. Faculty of Arts and Humanities Faculty practice accords with College practice as a minimum requirement, though many Departments meet considerably more often than twice in each academic year. For Combined Studies degrees, the relevant Departmental Teaching Committees report regularly to the appropriate Combined Studies Steering Committees concerning matters raised at SSCCs. Faculty guidelines for steering committees now stipulate that Combined Studies Steering Committees must address any concerns or complaints raised by students taking their particular degree programme(s). 8. Faculty of Social and Historical Sciences Faculty practice accords with College practice as a minimum requirement, though all its Departments have committees which meet more often than twice in each academic year. 9. Faculty of Laws This single Department Faculty has one Staff-Student Committee which reports to Departmental meetings (which have the same membership as Faculty Board meetings). Any matters needing further consideration are referred to Faculty Teaching Committees (FTCs). 10. Faculty of Mathematical and Physical Sciences Within the Faculty, DSSCCs meet at least once per term and keep minutes. The FTC expects to receive copies of the minutes. The FTC also considers any issues and advises the Dean of Students (as Chair of JSSC) on any action that may be necessary. 11. Faculty of Engineering Typically, DSSCCs meet twice a year and consist of two or three academic staff (usually including the Departmental Tutor), plus one or two students from each undergraduate year and each postgraduate course. The student-staff ratio on these committees is therefore greater than 2:1. Some Departments have a student chair, and all produce formal minutes. Action is usually recorded under matters arising. To date all action has been by Departmental staff, except when dissatisfaction with a course from outside the Faculty requires the Departmental Tutor to approach the outside Department concerned on behalf of the DSSCC. 12. Faculty of the Built Environment Each section within The Bartlett - Architecture, Construction Management, Planning, Bartlett School of Graduate Studies, and Development Planning Unit - holds two Staff-Student Committees per year, to which all students and staff associated with that section are invited. The meeting considers issues raised in course questionnaires, and any other issues that students and staff wish to raise. All meetings are minuted. Minutes are signed by a student and displayed in the department. Minutes are received by the FTC, and are also passed to the Faculty Tutor, and then forwarded to the Dean of Students. 13. Faculty of Life Sciences (Biological and Medical) For BSc and Postgraduate students, there are no Faculty guidelines on the composition of Staff-Student Committees beyond those required by College regulations. The Faculty's Teaching Committees (BSc and Postgraduate) have no routine involvement, but monitor student questionnaires and feedback from tutors. Faculty representatives attend departmental teaching committees and therefore hear SSCC issues. 14.Faculty of Medical Sciences For Graduate taught and research programmes, Divisional Graduate Staff Student Consultative Committees report to a Faculty Graduate Staff Student Consultative Committee, which reports to the JSSC. Minutes are reported to the Faculty Graduate Teaching and Research Committee to ensure that student issues are actioned. For the MBBS programme, which is managed by UCL Medical School within FMS and taught across 4 different Faculties, there are 2 staff-student committees which reflect the structure and length of the curriculum. These committees (Year 1 and Year 2 SSCC and Years 3,4,5 SSCC) report minutes to the Faculty of Medical Sciences Teaching Committee and also report minutes to the MBBS Teaching Committee which takes action regarding student issues. These committees meet each term and membership is made up largely, but not exclusively, from the executive of the Medical Students Union. The proportion of student to staff members is of the order of 2:1. Academic membership includes the Faculty Tutor, Medical School Support Tutors and Year/Module leads from all years of the MBBS programme. 1. Approved by Academic Committee on 11 June 2001. 92 93 Compiled and edited by: Professor Jane Dacre, UCL Medical School Ms Gaynor Jones, Medical Student Administration (MSA) MBBS Assessments and Examination Boards Governance.............................................................................................................................................96 Strategy and Principles ..........................................................................................................................96 Policies and protocols.............................................................................................................................97 Standard setting for written assessments ..........................................................................................97 Standard setting for clinical examinations (OSCEs) ............................................................................97 Normalising of Marks..........................................................................................................................98 Marks affected by examination incidents and irregularities ..............................................................98 Marks affected by special examination provision ..............................................................................98 Internal Examiners .................................................................................................................................99 External Examiners.................................................................................................................................99 Examination Boards .............................................................................................................................100 Faculty Board of Examiners ..............................................................................................................100 MBBS Board of Examiners.................................................................................................................102 MBBS Sub Boards of Examiners ........................................................................................................103 MBBS Sub Board of Examiners Year 3/IBSc Steering Group .............................................................104 MBBS Panels of Examiners................................................................................................................104 MBBS Sub Panels of Examiners (Clinical) ..........................................................................................105 MBBS Standard Setting Groups ........................................................................................................105 Format of Assessments ........................................................................................................................107 Years 1 and 2.....................................................................................................................................107 Year 3/IBSc ........................................................................................................................................110 Year 4 ................................................................................................................................................110 Year 5 ................................................................................................................................................112 Year 6 ................................................................................................................................................115 Mark Schemes ......................................................................................................................................118 Years 1 and 2.....................................................................................................................................118 Year 3 ................................................................................................................................................121 Year 4 ................................................................................................................................................123 Year 5 ................................................................................................................................................126 Year 6 ................................................................................................................................................129 Awards of Merit and Distinction..........................................................................................................132 University of London Gold Medal ........................................................................................................134 94 For organisational charts see: http://www.ucl.ac.uk/medicalschool/staff-students/committees 95 Governance UCL regulations and procedures including membership and responsibilities of College Boards of Examiners, conditions of appointment and responsibilities of examiners; procedures in respect of breach of examination regulations etc are set out at: http://www.ucl.ac.uk/registry/UCLStaff/Pink_Book/ All MBBS assessments are managed through UCL Medical School and report through the MBBS Board of Examiners. IBSc examinations are managed within their Faculty structures and interface with MBBS governance and management through the Year 3/ IBSc Steering Group which reports to the MBBS Board of Examiners. The MBBS Board of Examiners reports to the Faculty of Medical Sciences which reports to UCL Examination Board. UCL Medical School is represented at the UCL Board of Examiners by the Faculty Tutors (Medicine Years 1-3 and year 4-6). The MBBS Board of Examiners is responsible for assessment policy, strategy and quality assurance. The MBBS Sub Boards of Examiners are responsible for determining results and progression or qualification. The MBBS Panels and Sub Panels of Examiners are responsible for the academic content and the delivery of assessments. Strategy and Principles We aim to provide a suite of assessment instruments which are up to date, fit for purpose, and reflect current best practice. Our processes and assessment schedules and regulations are reviewed and updated annually, and submitted to UCL Examinations Board for review. We have a robust appeals process, which is available to students, and published on the UCLMS website. Our strategy is to provide a system of assessments which are robust, fair and consistent, and withstand challenge. Our assessment design draws on principles discussed and statements agreed by an international group at the Association for Medical Education in Europe International Conference in 2004: 1. Our assessment decisions are ideally based on multiple instruments. 2. The assessment is based on a mix of skills and subject area. 3. The methods and content of the assessment are transparent and communicated to the students before the beginning of that academic year. 4. Assessments are defensible in Court. 5. All Clinical fail marks are qualified by comments from assessors. 6. The tests are both cross sectional (at the end of the year) and longitudinal (throughout the year). 7. Tests are as cost effective as possible. 8. Mitigating circumstances are considered prior to Examination Boards. 9. All Clinical assessors are briefed on the test and expected level of attainment of the students prior to the assessment. 10. Assessors are encouraged to assess, and advised not to teach during an assessment. 11. The end goal is to test the achievement of competency. 12. Compensation is employed between instruments. 13. Decisions on pass/fail criteria are made using criterion referencing. 14. The overall aim of the assessment is to generate optimal educational impact on the course and to encourage students to learn what the Faculty believes they need to. 15. Not every assessment occasion is a decision moment as data is collected throughout the year. 16. The assessment programme is as rigorous, sharp, and clear as possible. 17. The final judgment is based on various sources but still has a judgment element to it during the examination board. 18. Resit assessments in the clinical years are avoided where possible. Assessments in all parts of the course were reviewed for the new MBBS curriculum in 2012 and the following principles agreed locally: There will be a consistent, centrally-managed approach to assessment throughout the six year programme. 96 The medical school will take a programmatic approach to assessment: viewing the assessments as a whole across the programme. Assessment methods will be selected according to evidence in published literature and internationally recognised best practice. All summative assessments will show adequate evidence of validity, ensuring meaningful interpretation of summative assessment scores. Assessment design will include blueprinting to the curriculum and planned outcomes, item writing, banking of items, assessment item scrutiny, standard setting, post assessment review and student and examiner feedback. Formative assessment will be frequent and constructive, enabling students to receive timely feedback on their performance throughout the programme. Formative assessments will be built into all elements of the curriculum and will be primarily for the benefit of the student’s learning. Where formative assessments will have the additional aim of tracking student progress, this will be transparent to staff and students. Student progress will be monitored in-course, with the aim of identifying and supporting students experiencing personal or academic difficulties. These systems will include evidence of engagement with formative assessment, monitoring of certain in-course assessments, maintenance of a portfolio, personal tutor feedback and performance in work-place based assessments (WPBAs) Overarching assessment features of the new MBBS curriculum A programmatic approach has been used to ensure the programme as a whole utilises a suitable spread of assessment types and to ensure adequate validity, reliability and feasibility and a spread of assessment load across the programme. The assessment programme as a whole and individual assessments are transparent with detailed information available to staff and students about assessment methods, pass marks, sample items and mark sheets. All years include an element of in-course assessment including the maintenance of an extensive and authentic portfolio. Satisfactory engagement with the course and in-course assessment is a requirement for entry into end of year assessments. The iBSc year will include the maintenance of a portfolio alongside assessments tailored to the programme of study. Formative assessments and feedback are a feature of all years of the programme as are opportunities to practice for summative assessments. All years have an end of year summative progression test: this will be a combination of a multiple item practical examination and a written examination consisting of a single best answer questions in all years. As these are high stakes examinations, good reliability of all summative assessment tools has been demonstrated. All assessments are integrated and both the practical and written assessments need to be passed to progress. Resit examinations will be held for unsuccessful students at key stages of the course: in years 1, 2 and Finals. Policies and protocols Standard setting for written assessments Standard setting for written assessments uses a modified Angoff approach. A group of approximately 8-10 teachers reviews each question individually and each member of the group indicates the percentage of “just passing” candidates they think would answer the question correctly. The chair of the standard setting group reviews questions for which the range of scores is high and a final mark is agreed in collaboration with the standard setters. The pass mark for the examination is the mean of the question scores. Standard setting for clinical examinations (OSCEs) The pass mark for the clinical examinations is calculated using a borderline group method of standard setting. A global judgement for overall performance on each OSCE station is given in addition to the station score. Pass Borderline Pass Borderline Fail 97 Fail All station scores for all candidates whose global judgements are in the Borderline Pass and Borderline Fail groups are totalled and averaged. The pass mark for the OSCE is the mean of these station scores. Normalising of Marks Marks for OSCEs taken over a number of days may be normalised if T Tests show a significant difference between sessions. =TTEST(range 1, range 2,2,2) If the difference is significant (p<0.05), a normalising equation developed by Dr Richard Morris, a statistician in the Department of Primary Care and Population Sciences, is applied to the OSCEs taken by each cohort of students to ensure equity: X represents the individual candidate’s score Y represents the mean of the mean scores for each cohort Z represents the mean score for the same cohort as X XxY Z iv)Calculation of pass mark at resit written examinations At re-sit written examinations where the cohort is too small for the calculation of standard errors of measurement to be reliable, re-sit papers will draw on validated questions taken by a whole year cohort. v)Calculation of pass mark at resit clinical examinations At resit clinical examinations, to ensure the reliability of the pass mark where cohort sizes are small, resit examinations will draw on validated questions and the pass mark will be determined by the borderline regression method using scores taken from the most recent occasion on which a station was taken by a whole year cohort. Marks affected by examination incidents and irregularities In cases where the score for an individual station is not available, the average of the candidate’s scores for the other stations will be taken. Examples include: Station discounted because of an examination irregularity Station discounted because of an examination incident Station discounted because the statistics show that the station has performed badly Mark sheet not completed or incorrectly completed by examiner Mark sheet missing In cases where there is a problem with a station in one circuit of the OSCE and this potentially affects the fairness of the assessment for other students, the marks achieved in that station will be removed for the whole cohort. An example of this is if an examiner has filled in a number of OSCE mark sheets incorrectly. Marks affected by special examination provision In cases where a candidate is unable to attempt a station, a mark of 0 will be awarded in accordance with the Medical School’s policy for special provision at clinical examinations and with the GMC’s requirement for competent performance as a doctor irrespective of any disability. Full details of at: http://www.ucl.ac.uk/medicalschool/staff-students/general-information/a-z/#support-cards 98 Internal Examiners Years 1 and 2 Internal examiners are drawn from each of the main academic disciplines represented in Years 1 and 2, from qualified doctors, nurses and from allied healthcare professionals as determined at item writing and confirmed during the OSCE blueprinting process as appropriate for the complexity of the station and the competencies being tested. Year 3/IBSc Internal examiners are appointed to individual IBSc programmes according to UCL BSc regulations. Year 4 Internal examiners may be drawn from fully registered doctors and from allied healthcare professionals as determined at item writing and confirmed during the OSCE blueprinting process as appropriate for the complexity of the station and the competencies being tested. Year 5 Internal examiners may be drawn from Consultant staff, GPs, CCT holders, Specialist Trainees at Grade 3 or higher and from allied healthcare professionals including Midwifery Tutors and Sexual Health Advisors as determined at item writing and confirmed during the OSCE blueprinting process as appropriate for the complexity of the station and the competencies being tested. Specialist Trainees at Grade 1 and 2 may be used in emergencies. Year 6 Short Station OSCE Examiners may be drawn from Consultant staff, GPs, CCT holders, Specialist Trainees at Grade 3 or higher and from allied healthcare professionals as determined at item writing and confirmed during the OSCE blueprinting process as appropriate for the complexity of the station and the competencies being tested. Specialist Trainees at Grade 1 and 2 may be used in emergencies. Year 6 Long Station OSCE Internal examiners for the Long Station OSCE may be drawn from Consultant Staff, GPs or CCT holders. Specialist Trainees at Grade 3 or higher may be used in emergencies. External Examiners External examiners are appointed in accordance with UCL examination regulations and must have completed 3 years as an undergraduate examiner at their own institution to be eligible to act as an external examiner at UCL. Appointment as an external examiner is renewable annually for a period of up to 4 consecutive years. External examiners in Years 1 and 2 may be drawn from academic staff and in Years 4-6 from clinical academic or consultant staff at consultant level in Years 4-6. Remit: To ensure that the standard of the programme of study is appropriate for the relevant year of the MBBS programme. To ensure that the assessment procedures have been carried out and decisions arrived at in a proper and impartial manner. To ensure that the standard of the examination is such that the University as a Licensing Body has fulfilled its obligations to the General Medical Council. 99 To approve the form and content, as far as is practicable, of the proposed written assessments and criterion-referenced mark schemes. To approve the form and content, as far as is practicable, of the proposed OSCE papers and mark schemes To view the OSCE on one or more sites. To attend the Sub Board of Examiners held at the end of the year to determine progression or qualification. To recommend to the Sub Board of Examiners, in the event of a disagreement, the final result to be derived from the assessments with regard to progression or qualification. Such a recommendation will be carefully considered by the Sub Board of Examiners, but the decision shall be arrived at by a majority vote of those present at the Progression Meeting. To report annually on the standard and conduct of the examination, the effectiveness of the assessments and any lessons to be drawn from them. Years 1 and 2 A minimum of 7 external examiners are appointed annually from the main disciplines represented in Years 1 and 2: oAnatomy oBiochemistry oNeuroscience oPharmacology oPhysiology oPsychology/Social Sciences oVertical Modules Year 3/IBSc External examiners are appointed to individual IBSc programmes according to UCL BSc regulations . Year 4 A minimum of 2 external examiners are appointed annually from the main specialties represented in Year 4: oMedicine oSurgery/Orthopaedics Year 5 A minimum of 6 external examiners are appointed annually from the main specialties represented in Year 5: oPaediatrics oGeneral Practice oWomen’s Health oCommunicable Diseases oPsychiatry oNeurology Year 6 A minimum of 8 external examiners are appointed annually from the main specialities represented in Year 6: oPathological Sciences oGeneral Medicine oSurgery/Orthopaedics oClinical Pharmacology and Therapeutics oPublic Health /Epidemiology oGeneral Practice o2 x Clinical Educationalists Examination Boards Faculty Board of Examiners Membership of Faculty Boards of Examiners (UCL Regulations for Boards of Examiners Section 4): 100 4.1 The members of each Faculty Board of Examiners for undergraduate programmes shall be the Chairs of Boards of Examiners in the Faculty responsible for assessing undergraduate programmes and the Faculty Tutor/Sub-Dean of the Faculty or his/her nominee. 4.2 The members of each Faculty Board of Examiners for taught graduate programmes shall be the Chairs of Boards of Examiners in the Faculty responsible for assessing taught graduate programmes and the Faculty Tutor/Sub-Dean of the Faculty or his/her nominee. 4.3 Each Faculty Board of Examiners shall have a Chair and a Deputy Chair. The same person, normally the Dean, shall be the Chair of both the undergraduate and taught graduate Faculty Boards of Examiners. If it is decided that the undergraduate and graduate Faculty Board of Examiners should each have a different Chair, it is suggested that the Chair of each should be the Deputy Chair of the other, in order to maintain links between the two Boards. If the nature of the Faculty requires it, it is acceptable for both Faculty Boards of Examiners, undergraduate and graduate, to meet at the same time under one Chair. 4.4 Internal and External Examiners appointed to Boards of Examiners at UCL shall have the right to attend meetings of the relevant Faculty Board of Examiners and the right to speak but not to vote at such meetings, but may be requested by the Chair of the Faculty Board of Examiners to withdraw temporarily if their nominations as examiners are the subject of discussion. 4.5 The quorum of a Faculty Board of Examiners shall be one-fifth of the membership including the Chair or Deputy Chair. Responsibilities (UCL Regulations for Boards of Examiners Section 5): 5.1 The primary responsibility of each Faculty Board of Examiners, whether at undergraduate or graduate level, shall be to ensure that assessment procedures within the Faculty are administered in accordance with UCL and programme regulations and in a proper and impartial manner. In carrying out this responsibility Faculty Boards of Examiners shall meet at least once a year and undertake the following duties: Duties: 5.1 Each Faculty Board of Examiners will need to meet in the first term. By this time most of the reports from External Examiners for undergraduate programmes for the previous year should have been received and considered by the Boards of Examiners and could therefore be considered by the Faculty Board of Examiners together with any responses. 5.2 be responsible for ensuring that Boards of Examiners are set up for every programme within the Faculty leading to an award and that Boards of Examiners are set up for any other programme for which the Faculty Board of Examiners deems this necessary and to make appropriate arrangements for the examination of programmes shared with other Faculties; 5.3 recommend to the UCL Board of Examiners the External Examiners for each Board of Examiners for which the Faculty Board of Examiners is responsible; 5.4 approve marking schemes, including in the case of the undergraduate Board Schemes for the Award of Honours, for each Board of Examiners for which the Faculty Board of Examiners is responsible; 5.5 receive the Minutes of the meeting at which recommendations for the final award are made from each Board of Examiners for which the Faculty Board of Examiners is responsible; 5.5 It will normally be sufficient for the Chair of the Faculty Board to receive the Minutes and report that they have been received to the Board. The full Faculty Board of Examiners, however, has the right to view, where it deems such action appropriate, any set of Minutes from the Boards of Examiners for which it is responsible. 101 5.6 recommend for approval to the UCL Board of Examiners awards, including, where appropriate, the award of Honours. 5.7 approve, in the case of the Faculty Boards of Examiners responsible for undergraduate programmes, applications for postponement of the award of Honours; 5.8 receive and consider the responses of Chairs of Boards of Examiners to External Examiner reports; 5.9 receive reports from the Boards of Examiners of any problems related to the operation of the procedures of Boards of Examiners and of any action taken by Boards in respect of such problems; 5.10 consider any general issues which arise from the foregoing; 5.11 provide a summary for the UCL Board of Examiners and the Faculty of the responses made to External Examiner reports for the Boards for which it is responsible; 5.11 In practice, the Chair of each Faculty Board will produce and send this summary to the Policy Officer (Examiners), Registry, who will forward it to the UCL Board of Examiners. A proforma has been produced by the Registry for this purpose (see UCL Appendix 2). 5.12 report annually (via its Minutes) on its business to the UCL Board of Examiners and the Faculty and pass on to the UCL Board of Examiners any matters which are not Faculty-specific or which give cause for serious concern. In the Event of an Emergency 5.13 In the event that the assessment of students, the award of degrees to students and/or decisions on progression from one year of the degree programme to the next are affected by an emergency, the Procedures in the event of an Emergency Affecting the Work of Boards of Examiners should be invoked. The Procedures and advice on them are at Appendix 9. MBBS Board of Examiners Members: Chair: Academic Lead for Assessment Faculty Tutor (Medical Sciences – Years 4-6) Faculty Tutor (Medical Sciences - Years 1-3) Academic Lead (Assessment) Chairs of Year Sub Boards of Examiners Chairs of Year Panels of Examiners Chair of IBSc Steering Committee Chairs of IBSc Exam Boards in Faculty of Medical Sciences Members of UCL Medical Student Administration MBBS Exam Liaison Officers IBSc Exam Liaison Officer Responsibilities: The primary responsibility of the MBBS Board of Examiners is to ensure that assessment procedures for the MBBS are administered in accordance with UCL and programme regulations and in a proper and impartial manner and that the IBSc components of the 6 year programme meet the requirements of the overall programme. The MBBS Board of Examiners reports to the Faculty of Medical Sciences Board of Examiners, but has responsibility for monitoring and reporting on all required items relating to the MBBS, programme including Year 3/IBSc, taught in all Faculties. The MBBS Sub Boards of Examiners are responsible for determining final results and progression to the next year of the programme or qualification. The MBBS Panels and Sub Panels are responsible for operational oversight of MBBS assessments. The Year 3 Exam Sub Board/IBSc Steering Committee is responsible for oversight of the IBSc components. 102 Duties: For MBBS Years 1,2,4,5,6: UCL governance: To approve external examiner appointments To determine the MBBS mark schemes To receive the minutes of meetings at which recommendations for final awards are made To receive and consider the responses of Chairs of Boards of Examiners to External Examiner reports To receive reports from the Boards of Examiners of any problems related to the operation of the procedures of Boards of Examiners and of any action taken by Boards in respect of such problems To consider any general issues which arise from the foregoing To prepare, on behalf of and to present to, the FMS Board of Examiners, a Chair’s summary, proforma UCLAppendix2, to be sent to the Policy Officer (Examiners), Registry, who will forward it to the UCL Board of Examiners). To report annually (via its Minutes) on its business to the UCL Board of Examiners via FMS Board of Examiners and pass on to the UCL Board of Examiners via FMS Board of Examiners any matters which are not Faculty-specific or which give cause for serious concern. MBBS governance: To determine MBBS assessment policy and strategy To oversee the MBBS Sub Boards and Panels of Examiners To approve appointments of internal examiners To ensure that the standard of the assessment is appropriate To ensure that individual disciplines are properly represented To approve the mark schemes for each year To receive and approve the minutes of the Panels/Sub Boards of Examiners and recommendations concerning progression To receive reports from external examiners and responses from Panels/Sub Boards of Examiners and to monitor and ensure appropriate follow up action For Year 3/IBSc: UCL governance, on behalf of FMS Board of Examiners, for programmes registered in FMS: To approve external examiner appointments To receive the minutes of meetings at which recommendations for final awards are made To receive and consider the responses of Chairs of Boards of Examiners to External Examiner reports To receive reports from the Boards of Examiners of any problems related to the operation of the procedures of Boards of Examiners and of any action taken by Boards in respect of such problems To consider any general issues which arise from the foregoing To prepare, on behalf of and to present to, the FMS Board of Examiners, a Chair’s summary, proforma UCLAppendix2, to be sent to the Policy Officer (Examiners), Registry, who will forward it to the UCL Board of Examiners). To report annually (via its Minutes) on its business to the UCL Board of Examiners via FMS Board of Examiners and pass on to the UCL Board of Examiners via FMS Board of Examiners any matters which are not Faculty-specific or which give cause for serious concern. MBBS governance: To approve IBSc harmonised mark schemes To receive an overall summary from the Year 3/IBSc Sub Board of Examiners, of the responses of Chairs of Boards of Examiners to External Examiners reports on IBSc programmes in all faculties for the purposes of MBBS monitoring, quality assurance and commissioning of IBSc programmes. The summary will be forwarded to all Faculty Boards of Examiners which host IBSc programmes. MBBS Sub Boards of Examiners Membership Chair: o Years 1 and 2 - Academic Lead (Years 1-3) 103 o Years 4 and 5 - Academic Lead (Years 4-6) o Year 6 – Director of UCL Medical School Director of UCL Medical School Deputy Director/Lead for UG Programmes Academic Lead (Assessment) Academic Leads and Deputy Leads for relevant year of programme Academic Lead and Deputy Lead (Vertical Modules) Faculty Tutor (Medicine - Years 1-3) Faculty Tutor (Medicine - Years 4-6) Student Support Tutors UCL Medical School representatives A minimum of one external examiner Horizontal and Vertical Module Leads for relevant years of programme Medical Student Administration Examinations Liaison Officers for relevant years of programme Responsibilities: MBBS Sub Boards of Examiners are responsible for overseeing assessment processes and for determining progression or qualification. Sub Boards report to the MBBS Board of Examiners. Duties: To receive examination results To determine student progression to the next year of the programme or qualification To determine awards of distinction in Medical Sciences, Clinical Sciences and Clinical Practice To determine awards of merit To determine awards of prizes To confirm termination of studies for students who are not eligible to continue To determine recommendations for applications for suspension of regulations or discretionary attempts for students with extenuating circumstances who have failed at their final attempt To make recommendations to the MBBS Board of Examiners about assessment format and content To receive, act and report annually on comments from the external examiners on the standard, conduct and outcome of the examinations, and their comparability with other medical schools MBBS Sub Board of Examiners Year 3/IBSc Membership Chair: Academic Lead (Year 3) Deputy Director of UCL Medical School/Lead for UG Programmes Academic Lead (Years 1-3) Chairs of IBSc Exam Boards in all relevant faculties Medical Student Administration Examinations Liaison Officers (Year 3) Duties: to determine the IBSc harmonised mark scheme and ensure that the mark scheme is appropriate for MBBS students to monitor and report on IBSc examinations in all relevant faculties for the purposes of MBBS quality assurance and commissioning to monitor and consider the responses of Chairs of Boards of Examiners, from all faculties which host IBSc programmes, to External Examiner reports on the standard, conduct and outcome of the examinations for the purposes of MBBS quality assurance and commissioning to prepare an overall summary of IBSc examinations in all faculties for MBBS Board of Examiners and to report the summary to each Faculty Board of Examiners which offers IBSc programmes MBBS Panels of Examiners Membership 104 Chair: Academic Lead for relevant year of programme Academic Lead (Years 1-3) Academic Lead (Years 4-6) Academic Lead (Assessment) Horizontal and Vertical Module Leads Medical Student Administration Examinations Liaison Officers Module Administrators where relevant Duties: to oversee examination processes and delivery to oversee recruitment of examiners to determine the academic content of assessments to manage question banks to compile and blueprint the written papers to approve the OSCE to be responsible for the standard setting process to act on comments from the external examiners on the standard, conduct and outcome of the examinations, and their comparability with other medical schools MBBS Sub Panels of Examiners (Clinical) Membership Chair: Deputy Academic Lead for relevant Year Academic Lead (Assessment) Academic Lead for relevant Year Academic Lead for Vertical Modules Deputy Academic Lead for Vertical Modules OSCE Site Leads o Module Leads in Years 4 and 5 o Site Sub Deans in Year 6 Representation from Horizontal and Vertical Modules Medical Student Administration Examinations Liaison Officers Module Administrators where relevant Skills Centre Staff UCLMS Clinical Training Fellows Duties: to design the clinical assessments to oversee the delivery of clinical assessments to set and blueprint the clinical assessments to co-ordinate delivery at each site to act on comments from the external examiners on the standard, conduct and outcome of the examinations, and their comparability with other medical schools MBBS Standard Setting Groups Membership Chair: o Years 1 and 2 - Academic Lead (Years 1-3) o Years 4-6 - Academic Lead (Assessment) Academic Lead for relevant year of programme UCLMS Clinical Training Fellows Minimum of 8 teachers of varying seniority drawn from horizontal and vertical modules Medical Student Administration Examinations Liaison Officers for relevant year of programme 105 Terms of Reference To review the questions set by the Panels of Examiners To agree a mark for each item using the Angoff method To determine the pass mark for each paper based on the mean of the agreed scores for each item 106 Format of Assessments Years 1 and 2 Assessment in Years 1 and 2 is overseen by the Years 1 and 2 Sub Board of Examiners and the Years 1 and 2 Panel of Examiners. Standard Setting Groups are responsible for setting the pass marks using the modified Angoff method. The Years 1 and 2 mark scheme can be found at: http://www.ucl.ac.uk/medicalschool/staffstudents/assessments Formative Assessments Formative assessments are held at intervals throughout the academic year. The main objective of the formatives is to stimulate efficient learning. The formatives include examples of all the question formats used in the end-of-year summative assessments and so provide good practice for these examinations. Students are invited to discuss their performance in formative assessments with their personal tutor and may request an appointment with a Student Support Tutor if they wish. Year 1 Foundations of Health and Medical Practice: on-line SBA (Single Best Answer) Year 1Infection and Defence: on-line SBA Year 1Fluids, Nutrition and Metabolism: on-line SBA Year 2Movement and Musculoskeletal Biology: on-line SBA Year 2Neuroscience and behaviour: on-line SBA Year 2Reproduction, Genetics and Development: on-line SBA In Course Assessments Compulsory in-course assessments are held during Intermodular Week in February. The objectives of the incourse assessments are to stimulate efficient learning and to provide students with the opportunity to experience assessments under examination conditions. Students are invited to discuss their performance in in-course assessments with their personal tutor and may request an appointment with a Student Support Tutor if they wish. Year 1Intermodular week (February): SBA, Data Interpretation/Practical, OSCE (Objective Structured Clinical Examination) Year 2Intermodular week (February): SBA, Data Interpretation/Practical, OSCE Summative Assessments Integrated summative assessments are held at the end of the academic year in May/June. The assessments comprise 2 SBA papers, a Data Interpretation paper and a Practical/Anatomy spot test. Students who are unsuccessful at their first attempt are normally required to re-sit in July and are required to resit the full diet of examinations. All the assessment exercises are designed to provide an integrated assessment of students’ abilities across modules, spines and disciplines, and test intellectual and practical skills rather than simple recall of factual information. 3 styles of question are used:1.Single Best Answer (SBA) 2.Data Interpretation (Written) 3.Practical (Anatomy Spot) Year 1 MBBS 1001 MBBS 1002 MBBS 1004 Year 2 MBBS 2001 MBBS 2002 MBBS2004 Single Best Answer Paper Single Best Answer Paper Data Interpretation Paper 107 2 hours 2 hours 2 hours rd 1/3 of total marks rd 1/3 of total marks rd 1/3 of total marks Practical/Anatomy Spot 1 hour Sample question styles Samples of the different styles of questions are available on the Medical School intranet site at: http://www.ucl.ac.uk/medicalschool/staff-students/assessments/ Feedback Formative assessments: on-line feedback is part of each formative assessment. misconceptions’ are posted on Moodle. Notes on ‘common In-course assessments: marks and quartile rankings are given in February as an indication of performance against the cohort. Summative assessments: overall marks and quartile rankings are issued to students for the summative assessments and copied to Personal Tutors. Quartile rankings are indicative at this stage and do not contribute to the final ranking for Foundation School applications. 1. Students who fail the summative assessments in May/June are encouraged to discuss their performance with their Personal Tutor and may request an appointment to see a Student Support Tutor individually if they wish. Students who fail at the second attempt are required to attend a compulsory appointment with the Faculty Tutor and a Student Support Tutor and are not normally eligible to continue on the programme. Required Course Work Before entry to the examinations for Year 1 or Year 2, a candidate must have completed the full prescribed course of study to the satisfaction of the Faculty Tutor (Medical Sciences) and submitted a portfolio containing marks for all required course work and student selected components. Required course work in Year 1 includes 2 x Student Selected Components. Required course work in Year 2 includes 1 x Student Selected Component and 1 x Patient Pathway. A candidate whose portfolio is incomplete may be precluded from entering the examinations. A candidate who is found, after examination entry has been confirmed, to have submitted an incomplete portfolio, will not be permitted to progress to the next year of the programme until all requirements are fulfilled. Extenuating circumstances Students who wish to bring to the attention of the Sub Board of Examiners circumstances which may affect or may have affected their performance in assessments or examinations must complete an extenuating circumstances form and submit the form, together with appropriate documentation e.g. a medical certificate or doctor’s letter, as soon as possible and not later than 7 days after the date of the last examination, and prior to the Examination Board in accordance with UCL procedures. Any extenuating circumstances received after this period will not be considered. Extenuating circumstances are considered at a Pre-Examination Board Meeting and scores awarded depending on the severity of the circumstances in accordance with UCL guidelines and tariffs. Scores are recorded on the mark sheet presented to the examiners at the meeting of the Years 1 and 2 Sub Board of Examiners. Further information and an ECP form may be found at: http://www.ucl.ac.uk/medicalschool/staffstudents/assessments/ Where a candidate declares extenuating circumstances after the meeting of the Examination Board, consideration is given, in accordance with UCL Student Grievance Procedures, only where examiners could not reasonably have been made aware of special circumstances (eg illness) which may have significantly affected performance. In these exceptional circumstances, the Medical School takes advice from external examiners in deciding the level of support and the final result. Re-sit examinations 108 Students who fail the Year 1 or Year 2 summative examinations may normally present themselves for reexamination on one occasion only and will be required to take all parts of the examination. Where a candidate has 2 failed attempts at the Year 1 or Year 2 summative assessments, consideration is given at the Examination Board to supporting an application to the UCL Dean of Students (Academic) for a suspension of regulations to permit an exceptional 3rd attempt. Representations made after the Examination Board cannot be considered as applications must have the support of the full Examination Board including external examiners. Students should be aware that candidates who have previously failed and repeated 2 years of the M.B.,B.S. programme, excluding Year 3, and who fail Year 5 will be required to leave the course. MBBS Examination regulations 5.1 There will be summative examinations at the end of Year 1 and at the end of Year 2. 5.2 Fitness to Practise concerns will be considered by the Sub Boards of Examiners in determining results. 5.3 The examinations will consist of a series of integrated written and practical assessments, with a variety of formats, covering each module and discipline. 5.4 The pass marks will be determined by criterion-referenced standard setting. 5.5 The overall result will indicate a pass or fail designation for each candidate. 5.6 Candidates will be required to observe the instructions for conduct of examinations in the Examination Programme Guide for Candidates. 5.7 Before entry to the examinations for Year 1 or Year 2, a candidate must have completed the full prescribed course of study to the satisfaction of the Faculty Tutor (Medical Sciences), and submitted a portfolio containing marks for all required course work and student selected components, and satisfied the examiners in all preceding parts. A candidate whose portfolio is incomplete may be precluded from entering the examinations. 5.8 A candidate who is found, after examination entry has been confirmed, to have submitted an incomplete portfolio, will not be permitted to progress to the next year of the programme until all requirements are fulfilled. 5.9 In Year 1, candidates are required to sit all sections of the examination in May/June, unless extenuating circumstances approved by the Faculty Tutor prevent this, in which case the candidate will be required to sit all sections in July. Candidates who do not sit examinations in May/June without an acceptable reason, approved by the Faculty Tutor, will be deemed to have made an attempt at the examination and will be permitted to present themselves for re-examination on one occasion only. Candidates who, for the first time, sit the examinations for Year 1 in July and are unsuccessful, will be required to present themselves for re-examination in the following May/June as a non-registered student unless the Faculty requires the candidate to pursue a further course of study. 5.10 In Year 1, candidates who fail may normally present themselves for re-examination on only one occasion. They will be required to take all parts of the examination at the resit examination. Candidates who fail at the first attempt may be required to pursue a course of study prescribed by the Faculty Tutor before being permitted to re-enter the examination. 5.11 In Year 2, candidates are required to sit all sections of the examination in May/June, unless extenuating circumstances approved by the Faculty Tutor prevent this, in which case the candidate will be required to sit all sections in July. Candidates who do not sit examinations in May/June without an acceptable reason, approved by the Faculty Tutor, will be deemed to have made an attempt at the examination and will be permitted to present themselves for re-examination on one occasion only. Candidates who, for the first time, sit the examinations for Year 2 in July and are unsuccessful, will be required to present themselves for re-examination in the following May/June as a non-registered student unless the Faculty requires the candidate to pursue a further course of study. 109 5.12 In Year 2, candidates who fail may normally present themselves for re-examination on only one occasion. They will be required to take all parts of the examination at the resit examination. Candidates who fail at the first attempt may be required to pursue a course of study prescribed by the Faculty Tutor before being permitted to re-enter the examination. Year 3/IBSc IBSc examinations are managed by individual Programme Leads following UCL regulations and requirements. Year 4 Assessment in Year 4 comprises in-course assessments in the form of portfolio requirements and module assessments and a summative examination at the end of Year 4 which takes the form of an integrated Single Best Answer paper and an Objective Structured Clinical Examination (OSCE). In-course assessments must be completed before entering the summative examination. The summative examination must be passed to progress to Year 5. An assessment of professionalism and fitness to practise underlies all parts of the MBBS course and assessments. Mark schemes and progression criteria include provision for teachers and examiners to report fitness to practise concerns if any aspect of a candidate’s performance during the course or assessments gives cause for concern about behaviour, attitude or fitness to practise. Fitness to practise concerns are considered by Faculty Tutors and by Examination Boards and can lead to a student failing to progress or to qualify. The Year 4 mark scheme can be found at: http://www.ucl.ac.uk/medicalschool/staffstudents/assessments/year4 Information about Reports of Fitness to Practise Concerns can be found at: http://www.ucl.ac.uk/medicalschool/staff-students/general-information/a-z/ Under the MBBS regulations: oBefore entry to the examinations, a candidate must have completed the full prescribed course of study to the satisfaction of the Faculty Tutor (Medical Sciences), and submitted a portfolio containing marks for all required course work, student selected components and clinical placements, and must have satisfied the examiners in all preceding parts. A candidate whose portfolio is incomplete may be precluded from entering the examinations. oA candidate who is found, after examination entry has been confirmed, to have submitted an incomplete portfolio, will not be permitted to progress to the next year of the programme until all requirements are fulfilled. oCandidates are required to complete all sections of the examinations in one diet and at the times designated by the Medical School oCandidates who fail the assessments will be required to repeat Year 4 and to pass the associated assessments before proceeding to Year 5. Candidates who fail at the second attempt will be asked to leave the School. oStudents should be aware that candidates who have previously failed and repeated 2 years of the M.B.,B.S. programme, excluding Year 3, and who fail Year 5 will be required to leave the course. oCandidates following the M.B.Ph.D. programme are required to complete the Year 4 summative assessments. 1. Written Assessment – Formative and Summative Week 30 Formative Assessment On-line clinical problem solving assessment comprising 75 integrated case-based single best answer questions (SBA) blueprinted against the Year 4 course components and Good Medical Practice and covering the following broad headings: 110 Pathogenesis and Prevention of Disease – enabling clinical problems to be considered from the perspective of Pathological Sciences, disordered physiology, genetics, public health and epidemiology Data interpretation – containing illustrated clinical material and integrating elements of Pathological Sciences with a clinical scenario All Vertical Modules Integrated Clinical Care including: o General Medicine o Respiratory and Community Medicine o Cardiology and Surgery o Acute Medicine and Liaison Psychiatry o Movement and Principles of Surgery o Digestive Health and Principles of Surgery o Metabolic and Renal Medicine and Principles of Surgery o Neurosciences with Surgery o Infectious Diseases/Haematology with Surgery End-of-Year Summative Assessment 1 x 3 hour clinical problem solving paper comprising 150 integrated case-based single best answer questions (SBA) blueprinted against the Year 4 course components and Good Medical Practice and covering the following broad headings: Pathogenesis and Prevention of Disease – enabling clinical problems to be considered from the perspective of Pathological Sciences, disordered physiology, genetics, public health and epidemiology Data interpretation – containing illustrated clinical material and integrating elements of Pathological Sciences with a clinical scenario All Vertical Modules Integrated Clinical Care including: o General Medicine o Respiratory and Community Medicine o Cardiology and Surgery o Acute Medicine and Liaison Psychiatry o Movement and Principles of Surgery o Digestive Health and Principles of Surgery o Metabolic and Renal Medicine and Principles of Surgery o Neurosciences with Surgery o Infectious Diseases/Haematology with Surgery Sample questions may be found at http://www.ucl.ac.uk/medicalschool/current-students/assessments/index.htm All papers are computer marked. There is no negative marking. 2. Clinical Assessment A clinical assessment comprising a short station OSCE with a minimum of 15 stations held at the end of Year 4. 3. Module Assessment Required in-course clinical assessments held during and at the end of each module include: Module Reports completed by educational supervisors at the end of each module which draw on: Procedure Cards Interim reports from firm teachers at appropriate points Supervised Learning Events Clinical Performance/Attitudes Supervised Learning Events Each student should complete in each module a minimum of: 3 Clinical assessment Exercises (CEX) and 2 Case Based Discussions (CBD) or Case Note Reviews (CNR) 111 The Clinical assessment Exercise is a snapshot of the student-patient interaction. The observation may be of any interaction between a student and a patient, including taking a history, examination, patient counseling etc, (depending upon the firm/ module) allowing assessment of the clinical skills, attitudes and behaviours of students essential to a high quality history and examination. The encounters should try to represent a range of clinical problems, and each module will specify any required activities to ensure that students are exposed to core conditions/competencies. The Case Based Discussion should be used by a student to have a focused discussion around a patient they have seen with a doctor who then assesses them on the basis of that discussion. The patient is not normally present. The aim of the CBD is to enable an assessor to provide systematic assessment and structured feedback. The student should select a case record from patients they have seen and of whom they have some knowledge. The discussion will start from and be centered on the student’s clerking and is designed to assess clinical decision-making and the application or use of medical knowledge in the care of the patient. It should enable the discussion of the ethical and legal framework of practice, and it allows students to discuss the management and treatment plans for that patient. The student chooses the timing, the cases and the assessor, but normally a consultant or GP should be the assessor for at least one of these exercises in each module. The Case Note Review format allows the clerking to be assessed without the student being present and is designed to fit in with those firms who cannot ensure that a teacher is always available to assess the student in person. Students should produce hand written contemporaneous notes on hospital paper, as if they were going to be filed in a patient record, and including diagnosis/ management plan and reflection on each case. They should not write an essay on a related topic and not have spent hours typing it up on a word processor. One of the aims for this assessment is to look at written communication. Case Note Review no longer has its own specific form, but can be recorded on a CBD form. Feedback Immediate feedback should be provided after each encounter by the observer assessing the student. This should be done using the anchor statements and areas for development and an action plan should be agreed for each encounter. Documentation The documentation required for each of these assessments is accessed via e-portfolio, an electronic undergraduate portfolio. Each student has their own personal account and access to all the supervised learning event forms needed. Clinical performance and attitudes These assessments are carried out during each module and comprise interim reports from firm teachers at appropriate points and an overall evaluation by the firm lead at the end of the module. The firm lead is responsible for reviewing all information available and for evaluating and commenting on: Communication skills Clinical method including examination and reasoning skills Clinical knowledge and management Professional attitudes and team work Approach to learning and punctuality Organisation and resilience under stress Failure to achieve satisfactory performance in any of these areas will result in referral to the Faculty Tutor. Students whose attendance in one module is inadequate may only proceed to the end-of-year assessments with the permission of the Faculty Tutor/Medical School Support Tutor. Students whose attendance in more than one module is inadequate will not normally be permitted to enter the end-of-year assessments. Students with unexplained missing Module Report forms, missing supervised learning events or a missing Training Record Card will be placed in Group 2 (Fail) at the Year 4 Exam Board. Year 5 112 Assessment in Year 5 comprises in-course assessments in the form of portfolio requirements and module assessments and a summative examination at the end of the year which takes the form of 2 integrated Single Best Answer papers and 1 Objective Structured Clinical Examination (OSCE). In-course assessments must be completed before entering the summative examination. The summative examination must be passed to progress to Year 6. An assessment of professionalism and fitness to practise underlies all parts of the MBBS course and assessments. Mark schemes and progression criteria include provision for teachers and examiners to report fitness to practise concerns reports if any aspect of a candidate’s performance during the course or assessments gives cause for concern about behaviour, attitude or fitness to practise. Fitness to practise concerns are considered by Faculty Tutors and by Examination Boards and can lead to a student failing to progress or to qualify. The Year 5 mark scheme can be found at: http://www.ucl.ac.uk/medicalschool/staffstudents/assessments/year5 Information about Fitness to Practise Concerns can be found at: http://www.ucl.ac.uk/medicalschool/staffstudents/general-information/a-z/ Under the MBBS regulations: oBefore entry to the examinations, a candidate must have completed the full prescribed course of study to the satisfaction of the Faculty Tutor (Medical Sciences), and submitted a portfolio containing marks for all required course work, student selected components and clinical placements, and must have satisfied the examiners in all preceding parts. A candidate whose portfolio is incomplete may be precluded from entering the examinations. oA candidate who is found, after examination entry has been confirmed, to have submitted an incomplete portfolio, will not be permitted to progress to the next year of the programme until all requirements are fulfilled. oCandidates are required to complete all sections of the examinations in one diet and at the times designated by the Medical School oCandidates who fail the assessments will be required to repeat Year 5 and to pass the associated assessments before proceeding to Year 6. Candidates who fail at the second attempt will be asked to leave the School. oCandidates who have previously failed and repeated 2 years of the M.B.,B.S. programme, excluding Year 3, and who fail Year 5 will be required to leave the course. oCandidates following the M.B.Ph.D. programme are required to complete the summative assessments 1. Written Assessment – Papers A and B Two clinical problem solving papers comprising integrated case-based single best answer questions (SBA) blueprinted against the MBBS course requirements and good medical practice and covering the following broad headings: Child and Family Health with Dermatology Clinical Neurosciences Women’s Health and Communicable Diseases Paper A3 hours150 Single Best Answer questions each with 5 items Paper B3 hours150 Single Best Answer questions each with 5 items Sample questions can be found at http://www.ucl.ac.uk/medicalschool/current-students/assessments/year-5 . All papers are computer-marked. There is no negative marking. 113 2. Clinical Assessment – Part C A clinical assessment comprising a short station OSCE with a minimum of 21 stations held at the end of Year 5. 3. Module and in-course Assessment Required in-course clinical assessments during each module include: Placement Reports completed by educational supervisors at the end of each attachment: Child and Family Health with Dermatology o Core Paediatrics o General Paediatrics o Core General Practice o GP Child Health Clinical Neurosciences o General Psychiatry o Specialist Psychiatry o Neurology o GP Mental Health Women’s Health and Communicable Diseases o Base O&G including Base Midwifery o Away O&G o Communicable Diseases o GP Women’s Health Placement Reports draw on: Training Record Cards Supervised Learning Events (SLE) oAt least 5 to be completed per module Clinical Performance/Attitudes Supervised Learning Events Each student should complete in each module a minimum of 5 SLEs as prescribed by the module requirements. These can take the form of: Clinical assessment Exercises (CEX) Case Based Discussions (CBD) The Clinical assessment Exercise is a snapshot of the student-patient interaction. The observation may be of any interaction between a student and a patient, including taking a history, examination, patient counseling etc, (depending upon the firm/ module) allowing assessment of the clinical skills, attitudes and behaviours of students essential to a high quality history and examination. The encounters should try to represent a range of clinical problems, and each module will specify any required activities to ensure that students are exposed to core conditions/competencies. The Case Based Discussion should be used by a student to have a focused discussion around a patient they have seen with a doctor who then assesses them on the basis of that discussion. The patient is not normally present. The aim of the CBD is to enable an assessor to provide systematic assessment and structured feedback. The student should select a case record from patients they have seen and of whom they have some knowledge. The discussion will start from and be centered on the student’s clerking and is designed to assess clinical decision-making and the application or use of medical knowledge in the care of the patient. It should enable the discussion of the ethical and legal framework of practice, and it allows students to discuss the management and treatment plans for that patient. The student chooses the timing, the cases and the assessor, but normally a consultant or GP should be the assessor for at least one of these exercises in each module. 114 Feedback Immediate feedback should be provided after each encounter by the observer assessing the student. This should be done using the anchor statements and areas for development and an action plan should be agreed for each encounter. Documentation The documentation required for each of these assessments is accessed via e-portfolio, an electronic undergraduate portfolio. Each student has their own personal account and access to all the supervised learning event forms needed. Clinical performance and attitudes These assessments are carried out during each module and comprise interim reports from firm teachers at appropriate points and an overall evaluation by the firm lead at the end of the module. The firm lead is responsible for reviewing all information available and for evaluating and commenting on: Communication skills Clinical method including examination and reasoning skills Clinical knowledge and management Professional attitudes and team work Approach to learning and punctuality Organisation and resilience under stress Failure to achieve satisfactory performance in any of these areas will result in referral to the Faculty Tutor. Students whose attendance in one module is inadequate may only proceed to the end-of-year assessments with the permission of the Faculty Tutor/Medical School Support Tutor. Students whose attendance in more than one module is inadequate will not normally be permitted to enter the end-of-year assessments. Students with unexplained missing Placement Reports, missing supervised learning events or a missing Training Record Card will be placed in Group 2 (Fail) at the Year 5 Exam Board. Year 6 The Final MBBS examination is an integrated written and clinical assessment in Medicine, Surgery, Pathological Sciences, Use of Medicines and Public Health. It includes assessment of general professional skills including communication, ethics, practical and clinical skills. The subject range is focused on knowledge, skills and attitudes needed for FY1. The main examination is held in May of Year 6 and a resit examination is held in June of Year 6. An assessment of professionalism and fitness to practise underlies all parts of the MBBS course and assessments. Mark schemes and progression criteria include provision for teachers and examiners to submit reports if any aspect of a candidate’s performance during the course or assessments gives cause for concern about behaviour, attitude or fitness to practise. Fitness to Practise reports are considered by Faculty Tutors and by Examination Boards and can lead to a student failing to progress or to qualify. The Final MBBS mark scheme can be found at: http://www.ucl.ac.uk/medicalschool/currentstudents/assessments/year-6 Information about Fitness to Practise reports can be found at: https://www.ucl.ac.uk/medicalschool/currentstudents/faqs/ Under the MBBS regulations: Before entry to the final examinations in Year 6, a candidate must have completed the full prescribed course of study to the satisfaction of the Faculty Tutor (Medical Sciences), and submitted a portfolio containing marks all required course work, student selected components and clinical placements, and must have satisfied the examiners in all preceding parts. A candidate whose portfolio is incomplete may be precluded from entering the examinations. 115 A candidate who is found, after examination entry has been confirmed, to have submitted an incomplete portfolio, or who fails to submit post-examination requirements, will not be awarded the degrees of M.B.,B.S. until all requirements are fulfilled. Candidates are required to complete all sections of the examinations for Year 6 in one diet and at the times designated by the Medical School. The regulations governing resit attempts can be found in the MBBS regulations at http://www.ucl.ac.uk/medicalschool/staff-students/general-information The Final MBBS examination is in 2 parts: Written assessment – Papers A and B 2 clinical problem solving papers comprising integrated case-based single best answer questions (SBA) blueprinted against the MBBS course requirements and good medical practice and covering the following broad headings: Pathogenesis and Prevention of Disease – enabling clinical problems to be considered from the perspective of Pathological Sciences, disordered physiology, genetics, public health and epidemiology Data Interpretation – containing illustrated clinical material and integrating elements of Pathological Sciences with a clinical scenario. Acute Clinical Conditions – covering the common presenting emergencies in an A/E Department and in a GP Surgery; their relevant symptoms and signs, and investigations; their management, including the use of medicines, observations and continuing care Chronic Clinical Conditions – covering presentation and management of chronic clinical conditions in hospital and primary care. Paper A3 hours150 Single Best Answer questions each with 5 items Paper B3 hours150 Single Best Answer questions each with 5 items Sample questions can be found at http://www.ucl.ac.uk/medicalschool/current-students/assessments/Year 6. All papers are computer-marked. There is no negative marking. Clinical Assessment- Part C A Long Station OSCE (LSO) assessing clinical method and a Short Station OSCE (SSO) assessing more specific conditions and practical procedures. Long Station OSCE Generic, standardised marking schedules are used throughout the assessment, and any concerns about fitness to practise are also reported. Sample mark sheets may be found on the Medical School website at http://www.ucl.ac.uk/medicalschool/staff-students/assessments/year-6/long-station-osce. Station 1 - History taking. Students take an observed history from a real patient and discuss differential diagnosis and management. Station 2 – Physical examination. This comprises examination of the cardiovascular, respiratory and abdominal systems in rotation, 10 minutes per system. Station 3 – Physical examination This comprises examination of the locomotor system, neurological system and a surgical examination, 10 minutes per system. Station 4 – Professional Skills. This comprises 3 integrated stations covering aspects of Professional Skills which may include communication skills, ethics and law, evaluation of evidence and health promotion.10 minutes per station. Station 1 – 30 minutes 116 Observed History TakingCandidate 1 Candidate 2 Candidate 3 Station 2 – 30 mins, 10 minutes per system Physical Examination: Cardiovascular Candidate 4 Chest Candidate 5 Abdomen Candidate 6 Station 3 – 30 minutes, 10 minutes each system Physical Examination: Locomotor Candidate 7 Neurology Candidate 8 SurgeryCandidate 9 Station 4 – 30 minutes, 10 minutes per task Integrated Professional Skills stations: 1Candidate 10 2 Candidate 11 3 Candidate 12 Short Station OSCE The Short Station OSCE consists of approximately 20 x 5 or 10 minute stations covering some short clinical cases, e.g. ophthalmology, practical procedures, therapeutics, and emergency medicine, history taking. 117 Mark Schemes Years 1 and 2 The Years 1 and 2 Sub Board of Examiners is responsible for overseeing assessment in Years 1 and 2 and for determining progression to the next year of the programme. The Years 1 and 2 Panel of Examiners, which reports to the Years 1 and 2 Sub Board of Examiners, is responsible for delivering the assessments in Years 1 and 2. The following mark scheme applies to examinations in Year 1 and in Year 2. 1.3 components, each of equal weight, comprising: MBBS1001/MBBS2001100 Single Best Answer (SBA) questions (2 hours) MBBS1002/MBBS2002100 Single Best Answer (SBA) questions (2 hours) MBBS1004/MBBS2004Data Interpretation (2 hours) + Practical (1 hour) 2. The pass mark for each of the 3 components is determined by standard setting using a modified Angoff method. A group of teachers reviews each question individually and each member of the group indicates the percentage of “just passing” candidates they think would answer the question correctly. The chair of the standard setting group reviews questions for which the range of scores is high and a final mark is agreed in collaboration with the standard setters. The pass mark for each component of the examination is the mean of the question scores. 3. The pass marks having been agreed, an aggregate score is calculated as the sum of the pass marks for each of the 3 components. 4. 5. Pass/Fail is determined by the aggregate score for the 3 components. A scaled mark is calculated for IBSc purposes after determining Pass/Fail for the MBBS using the criteria set out in the harmonised mark scheme for Year 3/IBSc. Pass/Fail Criteria 6. Candidates are placed into 1 of 3 groups according to the criteria below for discussion at the Board of Examiners to determine the final results. Group 1 (Pass) Candidates who meet all the following criteria are placed in Group 1 (Pass): the aggregate mark for the 3 components equals or exceeds the aggregate standard set pass mark for the 3 components the mark for each individual component equals or exceeds the standard set pass mark or is below the standard set pass mark for that component by not more than 1 standard error of measurement a completed portfolio including all required coursework has been submitted Group 2 (Fail) Candidates who do not meet the criteria to be placed in Group 1 (Pass) are placed in Group 2 (Fail) providing that they meet both the following criteria: the aggregate mark for the 3 components falls no more than 1 standard error of measurement below the aggregate standard set pass mark for the 3 components the mark for each individual component is below the standard set pass mark for that component by not more than 2 standard errors of measurement or if: or if: 118 an incomplete portfolio has been submitted These candidates will be discussed at the Years 1 and 2 Sub Board of Examiners’ Meeting in the light of their overall performance in the examination, their course and assessment record throughout the MBBS course, Fitness to Practise concerns and any relevant extenuating circumstances. These candidates will normally fail but may, in exceptional circumstances, be passed at the discretion of the Sub Board of Examiners. Results should be recorded on the mark sheet as “P” (Pass) or “F” (Fail). Candidates who fail and are eligible for a further attempt will be required to resit all parts of the examinations for Year 1 or Year 2 at the next possible occasion. Group 3 (Clear Fail) Candidates who do not meet the criteria to be placed in Group 1 or Group 2 are placed in Group 3 (Fail). These will be candidates to whom one or more of the following apply: the aggregate mark for the 3 components falls more than 1 standard error of measurement below the aggregate standard set pass mark for the 3 components the mark for an individual component is below the standard set pass mark for that component by more than 2 standard errors of measurement Candidates who are eligible for a further attempt will be required to resit all parts of the examinations for Year 1 or Year 2 at the next possible occasion. As the method for calculating the error around the cohort marks is in the process of being introduced (SEM); the School will follow a transition plan during the first year of implementation. If the implementation of the SEM rules creates an unexpected and unacceptable failure rate, the School will apply the model previously used. If this decision were to be made, it would need the full support of the Examination Board. Examiners’ Meetings 7. A pre-exam board meeting between the Chair of the Years 1 and 2 Sub Board of Examiners, the Deputy Chair of the Years 1 and 2 Sub Board of Examiners, the Chair of the Years 1 and 2 Panel of Examiners, and the Faculty and Welfare Tutors will be held without knowledge of individual candidate marks to consider the overall results, extenuating circumstances submitted in accordance with UCL regulations, and any examination irregularities or incidents reported during the examinations. Extenuating circumstances will be awarded a tariff of A, B, C or X according to UCL guidelines, a standardised report for each candidate in Group 2 and for re-sit candidates in Group 3 will be compiled, and a recommendation of strong support, some support or no support will be agreed and reported to the Years 1 and 2 Sub Board of Examiners. 8. A meeting of the Years 1 and 2 Sub Board of Examiners will take place to confirm the marks of all candidates and to review candidates in Group 2 and Group 3 in the light of the recommendations from the pre-exam board meeting. The decisions of the Sub Board are final. The results will be reported to the Faculty of Medical Sciences Board of Examiners. 9. Where a candidate has 2 failed attempts at the Year 1 or Year 2 summative assessments, consideration will be given at the Examination Board to supporting an application to UCL for a suspension of regulations to permit an exceptional 3rd attempt. Applications are considered by the Dean of Students. Representations made after the Examination Board cannot be considered as applications must have the support of the full Examination Board including external examiners. 10. Where a candidate declares extenuating circumstances after the meeting of the Examination Board, consideration is given, in accordance with UCL Student Grievance Procedures, only where examiners could not reasonably have been made aware of special circumstances (eg illness) which may have significantly affected performance. In these exceptional circumstances, the Medical School takes advice from external examiners in deciding the level of support and the final result. 119 11. The Sub Board will determine recommendations for the award of merits and distinctions as follows: Certificates of Merit will be awarded to approximately the top quintile of the cohort based on the overall outcomes of the assessments in each year will be restricted to candidates who have passed all components of the examination will be restricted to scores obtained at the first sitting will be recorded on the Medical School academic transcript Distinction in Medical Sciences will be awarded to approximately the top decile of the cohort based on the overall outcomes of the assessments in Year 1 and Year 2 will be restricted to candidates who have passed all components of the examination will be restricted to scores obtained at the first sitting will be recorded on the Medical School academic transcript will be recorded on the University MBBS Degree Certificate 12. 13. The Years 1 and 2 Sub Board of Examiners will determine recommendations for the awards of Medical School prizes in accordance with the regulations for each award. MBBS regulations 5.1 There will be summative examinations at the end of Year 1 and at the end of Year 2. 5.2 Fitness to Practise concerns will be considered by the Sub Boards of Examiners in determining results. 5.3 The examinations will consist of a series of integrated written and practical assessments, with a variety of formats, covering each module and discipline. 5.4 The pass marks will be determined by criterion-referenced standard setting. 5.5 The overall result will indicate a pass or fail designation for each candidate. 5.6 Candidates will be required to observe the instructions for conduct of examinations in the Examination Programme Guide for Candidates. 5.7 Before entry to the examinations for Year 1 or Year 2, a candidate must have completed the full prescribed course of study to the satisfaction of the Faculty Tutor (Medical Sciences), and submitted a portfolio containing marks for all required course work and student selected components, and satisfied the examiners in all preceding parts. A candidate whose portfolio is incomplete may be precluded from entering the examinations. 5.8 A candidate who is found, after examination entry has been confirmed, to have submitted an incomplete portfolio, will not be permitted to progress to the next year of the programme until all requirements are fulfilled. 5.9 In Year 1, candidates are required to sit all sections of the examination in May/June, unless extenuating circumstances approved by the Faculty Tutor prevent this, in which case the candidate will be required to sit all sections in July. Candidates who do not sit examinations in May/June without an acceptable reason, approved by the Faculty Tutor, will be deemed to have made an attempt at the examination and will be permitted to present themselves for re-examination on one occasion only. Candidates who, for the first time, sit the examinations for Year 1 in July and are unsuccessful, will be required to present themselves for re-examination in the following May/June as a non-registered student unless the Faculty requires the candidate to pursue a further course of study. 5.10 In Year 1, candidates who fail may normally present themselves for re-examination on only one occasion. They will be required to take all parts of the examination at the resit examination. Candidates who fail at the first attempt may be required to pursue a course of study prescribed by the Faculty Tutor before being permitted to re-enter the examination. 120 5.11 In Year 2, candidates are required to sit all sections of the examination in May/June, unless extenuating circumstances approved by the Faculty Tutor prevent this, in which case the candidate will be required to sit all sections in July. Candidates who do not sit examinations in May/June without an acceptable reason, approved by the Faculty Tutor, will be deemed to have made an attempt at the examination and will be permitted to present themselves for re-examination on one occasion only. Candidates who, for the first time, sit the examinations for Year 2 in July and are unsuccessful, will be required to present themselves for re-examination in the following May/June as a non-registered student unless the Faculty requires the candidate to pursue a further course of study. 5.12 In Year 2, candidates who fail may normally present themselves for re-examination on only one occasion. They will be required to take all parts of the examination at the resit examination. Candidates who fail at the first attempt may be required to pursue a course of study prescribed by the Faculty Tutor before being permitted to re-enter the examination. Year 3 Harmonised IBSc mark st 14. A scaled mark based on 1 sitting MBBS marks is calculated for IBSc purposes after determining the results for the MBBS examinations and the re-sit examinations. The scaled mark is based on the aggregate mark using the following formula: 50 + (50 X B/100) where 50 = the IBSc pass mark and where B = the percent of the candidate’s mark above the pass mark for the MBBS Worked example: If B = 20% then scaled mark for IBSc purposes = 50 + (50 X 20/100) = 50 + (50 X 0.2) = 60 Group 1 Pass - overall MBBS mark (MBBS1005/2005) scaled to a nominal 50% pass mark. Group 2 Pass - scaled mark capped at 50 [at the discretion of the Phase 1 Sub Board of Examiners, candidates in this group may carry their full scaled mark as calculated for the Group 1 category ] Group 2 Fail - scaled mark capped at 49 oThis result is reported for BSc purposes as CP (Condoned Pass) in accordance with UCLs harmonised mark schemes for candidates who pass the MBBS examinations at a second or subsequent attempt and are eligible to continue on the course. oThis result is reported for BSc purposes as F (Fail) for candidates who fail the MBBS examinations at a second or subsequent attempt and are required to leave the course. Group 3 Fail - scaled mark capped at 45 oThis result is reported for BSc purposes as CP (Condoned Pass) in accordance with UCLs harmonised mark schemes for candidates who pass the MBBS examinations at a second or subsequent attempt and are eligible to continue on the course. oThis result is reported for BSc purposes as F (Fail) for candidates who fail the MBBS examinations at a second or subsequent attempt and are required to leave the course. 121 15. The harmonised IBSc marks for all candidates are determined at the MBBS Re-sit Sub Board of Examiners in July. 16. First sitting MBBS marks are used for the calculation of the IBSc except in documented cases of extenuating circumstances where the MBBS Sub Board of Examiners has discretion to allow a subsequent result to carry forward. 17. The award of the IBSc degree is based on a 12 course unit programme comprising: Year 1 MBBS 4 course units Year 2 MBBS 4 course units Year 3 IBSc 4 course units 18. The final IBSc award is calculated using a ratio of 1:1:6 where Y1 = 1, Y2 = 1, IBSc = 6. 122 Year 4 The Year 4 Sub Board of Examiners is responsible for overseeing assessment in Year 4 and for determining progression to Year 4. The Year 4 Panel of Examiners, which reports to the Year 4 Sub Board of Examiners, is responsible for delivering the assessments in Year 4. Assessment in Year 4 comprises 3 components: required in-course assessments, summative written assessments and summative clinical assessments. Marks in the Year 4 examinations contribute to the final rankings for Foundation School applications. Progression to Year 5, quartile ranks and the awards of merit are based on the total marks for the written and clinical components only. Professionalism and Reports of Fitness to Practise An assessment of professionalism and fitness to practise underlies all parts of the MBBS course and assessment. Mark schemes and progression criteria include provision for teachers and examiners to report fitness to practise concerns if any aspect of a candidate’s performance during the course or assessments gives cause for concern about behaviour, attitude or fitness to practise. Fitness to practise concerns are considered by Faculty Tutors and by Examination Boards and can lead to a student failing to progress or to qualify. Students whose attendance in one module is inadequate are required to see the Faculty Tutor or one of the Student Support Tutors to explain their absence and may only enter the Year 4 assessments with the permission of the Faculty Tutor. Students whose attendance in more than one module is inadequate will not normally be permitted to enter the end-of-year assessments. Written Assessment (MBBS3001) 1. 1 Single Best Answer (SBA) paper, total marks expressed as a percentage. 2. The pass mark is determined by standard setting using a modified Angoff method. A group of teachers reviews each question individually and each member of the group indicates the percentage of “just passing” candidates they think would answer the question correctly. The chair of the standard setting group reviews questions for which the range of scores is high and a final mark is agreed in collaboration with the standard setters. The pass mark for the written examination is the mean of the question scores. Clinical Assessment (MBBS3002) 3. 1 short station Objective Structured Clinical Examination (OSCE), at least 15 stations, total marks expressed as a percentage. 4. The pass mark for the clinical examinations is calculated using a borderline group method of standard setting. A global judgement for overall performance on each OSCE station is given in addition to the station score. Pass Borderline Pass Borderline Fail Fail All station scores for all candidates whose global judgements are in the Borderline Pass and Borderline Fail groups are totalled and averaged. The pass mark for the OSCE is the mean of these station scores. 5. The written and clinical assessments are equally weighted. 123 Module Assessment (MBBS3003) 6. 3 end-of-module assessments. Pass/Fail Criteria 7. Candidates are placed into 1 of 3 groups according to the criteria below for the Sub Board of Examiners to determine the final results. Group 1 (Pass) Candidates who meet all the following criteria are placed in Group 1 (Pass): the written assessment mark equals or exceeds the standard set pass mark the clinical assessment mark equals or exceeds the standard set pass mark 3 end-of-module assessments each including required supervised learning events have been submitted or satisfactory evidence certified in advance of the Examiners’ Meeting by the Educational Supervisor or nominee or the Faculty Tutor or nominee that any missing assessments were outside the student’s control no more than 1 Fitness to Practise Concern has been upheld during the year Group 2 (Fail) Candidates who do not meet the criteria to be placed in Group 1 (Pass) are placed in Group 2 (Fail) if they meet both of the following criteria: the written assessment mark is not more than 1 standard error of measurement below the standard set pass mark the clinical assessment mark is not more than 1 standard error of measurement below the standard set pass mark or if: the candidate has failed to submit 1 or more of the 3 end-of-module assessments and has not provided satisfactory evidence certified in advance of the Examiners’ Meeting by the Educational Supervisor or nominee or the Faculty Tutor or nominee that any missing assessments were outside the student’s control 2 or more Fitness to Practise Concerns have been upheld during the year These candidates will be discussed at the Year 4 Sub Board of Examiners’ Meeting in the light of their overall performance in the examination, their course and assessment record throughout the MBBS course, and any relevant extenuating circumstances. These candidates will normally fail but may, in exceptional circumstances, be passed at the discretion of the Sub Board of Examiners. Results should be recorded as: Pass with a Directed Elective (DE) These candidates will be required to take a directed elective at an approved teaching hospital in the UK in order to provide the best chances of success in finals. In exceptional circumstances and under the supervision of the Sub Dean (Electives), consideration may be given to requests to take an elective abroad providing that the elective is at a teaching hospital with a western case mix similar to that seen in the UK and that 6 consecutive weeks are spent at the same teaching hospital. Amended July 13 to reflect change in timing of finals: Pass with directed study in Year 6 (DE) These candidates will be required to take 2 periods of directed study in Year 6 to maximise their chances of success in finals. The periods of directed study will replace the SSCs prior to finals and will draw on subjects covered in Year 4 and examined in finals, will offer appropriate opportunities to consolidate basic clinical skills and knowledge, and will be directed at gaining further experience in areas of weakness identified in the Year 4 examinations. 124 Fail (F) Candidates who are eligible for a further attempt will be required to repeat Year 4 and to resit all parts of the examination at the next possible occasion. Group 3 (Clear Fail) Candidates who do not meet the criteria to be placed in Group 1 or Group 2 are placed in Group 3 (Clear Fail). These will be candidates to whom one or more of the following apply: the written assessment mark is more than 1 standard error of measurement below the standard set pass mark the clinical assessment mark is more than 1 standard error of measurement below the pass mark Candidates who are eligible for a further attempt will be required to repeat Year 4 and to resit all parts of the examination at the next possible occasion. As the method for calculating the error around the cohort marks is in the process of being introduced (SEM); the School will follow a transition plan during the first year of implementation. If the implementation of the SEM rules creates an unexpected and unacceptable failure rate, the School will apply the model previously used. If this decision were to be made, it would need the full support of the Examination Board. Examiners’ Meetings 8. A pre-exam board meeting between the Chair of the Year 4 Sub Board of Examiners, the Chair of the Year 4 Panel of Examiners and the Faculty and Student Support Tutors will be held without knowledge of individual candidate marks to consider the overall results, extenuating circumstances submitted in accordance with UCL regulations, fitness to practise concerns reported by teachers and examiners, and any examination irregularities or incidents reported during the examinations. Extenuating circumstances will be awarded a tariff of A,B,C or X according to UCL guidelines, a standardised report for each candidate in Group 2 and for re-sit candidates in Group 3 will be compiled, and a recommendation of strong support, some support or no support will be agreed and reported to the Year 4 Sub Board of Examiners. Fitness to practise concerns issued by teachers and already ratified by the Faculty Tutor will be upheld. Fitness to practise concerns issued by examiners will be considered and upheld where issued in accordance with the instructions on the forms or discounted if not issued properly or if the concerns have already been addressed in the mark scheme. 9. A meeting of the Year 4 Sub Board of Examiners will take place to consider and confirm the marks of all candidates and to review candidates in Group 2 and Group 3 in the light of the recommendations from the pre-exam board meeting. The decisions of the Sub Board of Examiners are final. The results will be reported to the Faculty of Biomedical Sciences Board of Examiners. 10. The Sub Board will determine recommendations for the award of merit as follows: will be awarded on the basis of the overall outcomes of the assessments in Year 4 will be awarded to approximately the top quintile of the cohort will be restricted to scores obtained at the first sitting will be determined each year by the Year 4 Sub Board of Examiners may be rescinded, at the discretion of the Sub Board, for candidates who have received one or more fitness to practise concerns will be recorded on the Medical School academic transcript 11. The Sub Board will determine recommendations for the awards of Medical School prizes in accordance with the regulations for each award. 12. Under the MBBS regulations: A candidate who is found, after examination entry has been confirmed, to have submitted an incomplete portfolio, will not be permitted to progress to the next year of the programme until all requirements are fulfilled. 125 Candidates who fail at the second attempt will be asked to leave the School. Final mark sheets 13.Results are recorded on the final mark sheet as: PPass FFail MMerit DEDirected Elective X Result not yet available (includes, for example, plagiarism or exam irregularity where the result of a hearing is awaited. Must be amended later on the mark sheet and MSSR to the appropriate result) NG Not graded (for ungraded clinical attachments) NRNot received (for missing firm grades/logbook marks) ABSAbsent WDWithdrawn 14.Quartile position is recorded on the final mark sheet as: 75-100%(Top quartile) 50-75% 25-50% 0-25%(Bottom quartile) 15. A notification of results sheet is emailed to each candidate and to their personal tutor and a copy is filed on the student record. Year 5 The Year 5 Sub Board of Examiners is responsible for overseeing assessment in Year 5 and for determining progression to Year 6. The Year 5 Panel of Examiners, which reports to the Year 5 Sub Board of Examiners, is responsible for delivering the assessments in Year 5. Assessment in Year 5 comprises 3 components: required in-course assessments, summative written assessments and summative clinical assessments. Marks in the Year 5 examinations contribute to the final rankings for Foundation School applications. Progression to Year 6, quartile ranks and the awards of merit and distinction are based on the total marks for the written and clinical assessments only. Professionalism and Fitness to Practise An assessment of professionalism and fitness to practise underlies all parts of the MBBS course and assessment. Mark schemes and progression criteria include provision for teachers and examiners to report fitness to practise concerns if any aspect of a candidate’s performance during the course or assessments gives cause for concern about behaviour, attitude or fitness to practise. Fitness to practise concerns are considered by Faculty Tutors and by Examination Boards and can lead to a student failing to progress or to qualify. Students whose attendance in one module is inadequate are required to see the Faculty Tutor or one of the Student Support Tutors to explain their absence and may only enter the Year 5 assessments with the permission of the Faculty Tutor. Students whose attendance in more than one module is inadequate will not normally be permitted to enter the end-of-year assessments. Written Assessment (MBBS4001) 1. 2 Single Best Answer (SBA) papers, equally weighted, total marks expressed as a percentage. 126 2. The pass mark is determined by standard setting using a modified Angoff method. A group of teachers reviews each question individually and each member of the group indicates the percentage of “just passing” candidates they think would answer the question correctly. The chair of the standard setting group reviews questions for which the range of scores is high and a final mark is agreed in collaboration with the standard setters. The pass mark for the written examination is the mean of the question scores. Clinical Assessment (MBBS4002) 3. 1 short station Objective Structured Clinical Examination (OSCE), at least 21 stations, total marks for the clinical assessment expressed as a percentage. 4. The pass mark for the clinical examination is calculated using a borderline group method of standard setting. A global judgement for overall performance on each OSCE station is given in addition to the station score. Pass Borderline Pass Borderline Fail Fail All station scores for all candidates whose global judgements are in the Borderline Pass and Borderline Fail groups are totalled and averaged. The pass mark for the OSCE is the mean of these station scores. 5. The written and clinical assessments are equally weighted. Pass/Fail Criteria 6. Candidates are placed into 1 of 3 groups according to the criteria below for the Sub Board of Examiners to determine the final results. Group 1 (Pass) Candidates who meet all the following criteria are placed in Group 1 (Pass): the written assessment mark equals or exceeds the standard set pass mark the clinical assessment mark equals or exceeds the standard set pass mark all required placement reports have been submitted or satisfactory evidence certified in advance of the Examiners’ Meeting by the Educational Supervisor or nominee or the Faculty Tutor or nominee that any missing assessments were outside the student’s control no more than 1 Fitness to Practise Concern has been upheld during the year Group 2 (Fail) Candidates who do not meet the criteria to be placed in Group 1 (Pass) are placed in Group 2 (Fail) if they meet both the following criteria: the written assessment mark is not more than 1 standard error of measurement below the standard set pass mark the clinical assessment mark is not more than 1 standard error of measurement below the standard set pass mark or if: the candidate has failed to submit 1 or more of the required placement reports and has not provided satisfactory evidence certified in advance of the Examiners’ Meeting by the Educational Supervisor or nominee or the Faculty Tutor or nominee that any missing assessments were outside the student’s control 2 or more Fitness to Practise Concerns have been upheld during the year 127 These candidates will be discussed at the Year 5 Examiners’ Meeting in the light of their overall performance in the examination, their course and assessment record throughout the MBBS course, and any relevant extenuating circumstances. These candidates will normally fail but may, in exceptional circumstances, be passed at the discretion of the Sub Board of Examiners. Results should be recorded as “P” (Pass) or “F” (Fail). Group 3 (Clear Fail) Candidates who do not meet the criteria to be placed in Group 1 or Group 2 are placed in Group 3 (Clear Fail). These will be candidates to whom one or more of the following apply: the written assessment mark is more than 1 standard error of measurement below the standard set pass mark the clinical assessment mark is more than 1 standard error of measurement below the standard set pass mark 3 or more Fitness to Practise Concerns have been upheld during the year Candidates who are eligible for a further attempt will be required to repeat Year 5 and to re-sit all parts of the Year 5 examination at the next possible occasion. As the method for calculating the error around the cohort marks is in the process of being introduced (SEM); the School will follow a transition plan during the first year of implementation. If the implementation of the SEM rules creates an unexpected and unacceptable failure rate, the School will apply the model previously used. If this decision were to be made, it would need the full support of the Examination Board. Examiners’ Meetings 8. A pre-exam board meeting between the Chair of the Year 5 Sub Board of Examiners, the Chair of the Year 5 Panel of Examiners and the Faculty and Student Support Tutors will be held without knowledge of individual candidate marks to consider the overall results, extenuating circumstances submitted in accordance with UCL regulations, Fitness to Practise Concerns submitted by teachers and examiners, and any examination irregularities or incidents reported during the examinations. Extenuating circumstances will be awarded a tariff of A,B,C or X according to UCL guidelines, a standardised report for each candidate in Group 2 and for re-sit candidates in Group 3 will be compiled, and a recommendation of strong support, some support or no support will be agreed and reported to the Year 5 Sub Board of Examiners. Fitness to Practise Concerns issued by teachers and already ratified by the Faculty Tutor will be upheld. Fitness to Practise Concerns issued by examiners will be considered and upheld where issued in accordance with the instructions on the forms or discounted if not issued properly or if the concerns have already been addressed in the mark scheme. 9. A meeting of the Year 5 Sub Board of Examiners will take place to consider and confirm the marks of all candidates and to review candidates in Group 2 and Group 3 in the light of the recommendations from the pre-exam board meeting. The decisions of the Sub Board of Examiners are final. The results will be reported to the MBBS Board of Examiners. 10. The Sub Board will determine recommendations for the award of Distinction in Clinical Science as follows: 11. will be awarded to approximately the top decile of the cohort will be awarded on the basis of the overall outcomes of the Year 4 and Year 5 assessments using a ratio of 60:40 in favour of Year 4 scores will be restricted to scores obtained at the first sitting will be determined by the Year 5 Sub Board of Examiners may be rescinded, at the discretion of the Sub Board, for candidates who have received one or more fitness to practise forms will be recorded on the Medical School academic transcript will be recorded on the University MBBS Degree Certificate The Sub Board will determine recommendations for the award of merit as follows: 128 will be awarded on the basis of the overall outcomes of the assessments in Year 5 will be awarded to approximately the top quintile of the cohort will be restricted to scores obtained at the first sitting will be determined each year by the Year 5 Sub Board of Examiners may be rescinded, at the discretion of the Sub Board, for candidates who have received one or more fitness to practise forms will be recorded on the Medical School academic transcript 12. The Sub Board will determine recommendations for the awards of Medical School prizes in accordance with the regulations for each award. 13. Under the MBBS regulations: A candidate who is found, after examination entry has been confirmed, to have submitted an incomplete portfolio, will not be permitted to progress to the next year of the programme until all requirements are fulfilled. Candidates who fail at the second attempt will be asked to leave the School. Candidates who have previously failed and repeated 2 years of the M.B.,B.S. programme, excluding Year 3, and who fail Year 5 will be required to leave the course. Final mark sheets 14.Results are recorded on the final mark sheet as: PPass FFail MMerit X Result not yet available (includes, for example, plagiarism or exam irregularity where the result of a hearing is awaited. Must be amended later on the mark sheet and MSSR to the appropriate result) NG Not graded (for ungraded clinical attachments) NRNot received (for missing firm grades/logbook marks) ABSAbsent WDWithdrawn 15.Quartile position is recorded on the final mark sheet as: 75-100%(Top quartile) 50-75% 25-50% 0-25%(Bottom quartile) 16. A notification of results sheet is emailed to each candidate and to their personal tutor and a copy is filed on the student record. Year 6 The Year 6 Sub Board of Examiners is responsible for overseeing assessment in Year 6 and for awarding the final MBBS qualification. The Year 6 Panel of Examiners, which reports to the Year 6 Sub Board of Examiners, is responsible for delivering the assessments in Year 6. Professionalism and Fitness to Practise Concerns An assessment of professionalism and fitness to practise underlies all parts of the MBBS course and assessment. Mark schemes and progression criteria include provision for teachers and examiners to report Fitness to Practise concerns if any aspect of a candidate’s performance during the course or assessments gives cause for concern about behaviour, attitude or fitness to practise. Fitness to Practise concerns are considered by Faculty Tutors and by Examination Boards and can lead to a student failing to progress or to qualify. 129 Students whose attendance is inadequate are required to see the Faculty Tutor or one of the Student Support Tutors to explain their absence and may only enter the assessments with the permission of the Faculty Tutor. Written Assessment (MBBS5001) 1. 2 Single Best Answer papers, equally weighted, total marks expressed as a percentage. 2. The pass mark is determined by standard setting using a modified Angoff method. A group of teachers reviews each question individually and each member of the group indicates the percentage of “just passing” candidates they think would answer the question correctly. The chair of the standard setting group reviews questions for which the range of scores is high and a final mark is agreed in collaboration with the standard setters. The pass mark for the written examination is the mean of the question scores. Clinical Assessment (MBBS5002) 3. 2 clinical Objective Structured Clinical Examinations (OSCEs), long and a short station, equally weighted, marks for each OSCE and total marks for the clinical assessment expressed as a percentage. 4. The pass mark for each clinical examination is calculated using a borderline group method of standard setting. A global judgement for overall performance on each OSCE station is given in addition to the station score. Pass Borderline Pass Borderline Fail Fail All station scores for all candidates whose global judgements are in the Borderline Pass and Borderline Fail groups are totalled and averaged. The pass mark for each OSCE is the mean of these station scores. 5. The written and clinical assessments are equally weighted. Pass/Fail Criteria Candidates are placed into 1 of 3 groups according to the criteria below for the Sub Board of Examiners to determine the final results. 6. Candidates are placed into the following groups: Group 1 (Pass) Candidates who meet all the following criteria are placed in Group 1 (Pass): the written assessment mark equals or exceeds the standard set pass mark the clinical assessment mark equals or exceeds the standard set pass mark the mark for each OSCE is below the standard set pass mark for that OSCE by not more than 1 standard error of measurement no more than 2 Fitness to Practise Concerns have been upheld during the year Group 2 (Fail) Candidates who do not meet the criteria to be placed in Group 1 (Pass) are placed in Group 2 (Fail) if they meet all the following criteria: the written assessment mark is not more than 1 standard error of measurement below the standard set pass mark the clinical assessment mark is not more than 1 standard error of measurement below the standard set pass mark 130 the mark for each OSCE is not more than 2 standard errors of measurement below the standard set pass mark for that OSCE or if: 3 or more Fitness to Practise Concerns have been upheld during the year These candidates will be discussed at the Final Examiners’ Meeting in the light of their overall performance in the examination, their course and assessment record throughout the MBBS course, and any relevant extenuating circumstances. These candidates will normally fail but may, in exceptional circumstances, be passed at the discretion of the Sub Board of Examiners. Results should be recorded as “P” (Pass) or “F” (Fail). Candidates who fail and are eligible for a further attempt will be required to resit all parts of the Final MBBS Examination at the next possible occasion. Group 3 (Clear Fail) Candidates who do not meet the criteria to be placed in Group 1 or Group 2 are placed in Group 3 (Clear Fail). These will be candidates to whom one or more of the following apply: the written assessment mark is more than 1 standard error of measurement below the standard set pass mark the clinical assessment mark is more than 1 standard error of measurement below the standard set pass mark the mark for an OSCE is more than 2 standard errors of measurement points below the standard set pass mark for that OSCE Candidates who are eligible for a further attempt will be required to resit all parts of the Final MBBS Examination at the next possible occasion. As the method for calculating the error around the cohort marks is in the process of being introduced (SEM); the School will follow a transition plan during the first year of implementation. If the implementation of the SEM rules creates an unexpected and unacceptable failure rate, the School will apply the model previously used. If this decision were to be made, it would need the full support of the Examination Board. Examiners’ Meetings 7. A pre-exam board meeting between the Chair of the Faculty Board of Examiners, the Chair of the Year 6 Sub Board of Examiners, the Chair of the Year 6 Panel of Examiners and the Faculty and Student Support Tutors will be held without knowledge of individual candidate marks to consider the overall results, extenuating circumstances submitted in accordance with UCL guidelines, Fitness to Practise Concerns submitted by teachers and examiners, and any examination irregularities or incidents reported during the examinations. Extenuating circumstances will be awarded a tariff of A,B,C or X according to UCL guidelines, a standardised report for each candidate in Group 2 and for re-sit candidates in Group 3 will be compiled, and a recommendation of strong support, some support or no support will be agreed and reported to the Year 6 Sub Board of Examiners. Fitness to Practise Concerns issued by teachers and already ratified by the Faculty Tutor will be upheld. Fitness to Practise Concerns issued by examiners will be considered and upheld where issued in accordance with the instructions on the forms or discounted if not issued properly or if the concerns have already been addressed in the mark scheme. 8. A meeting of the Year 6 Sub Board of Examiners will take place to confirm the marks of all candidates and to review candidates in Group 2 and Group 3 in the light of the recommendations from the pre-exam board meeting. The decisions of the Sub Board of Examiners are final. The results will be reported to the Faculty of Biomedical Sciences Board of Examiners. 9. The Sub Board will determine recommendations for the award of distinctions and merits as follows: Distinction in Clinical Practice will be awarded to approximately the top decile of the cohort based on the overall outcomes of the assessments in Year 6 will be restricted to scores obtained at the first sitting 131 will be recorded on the University MBBS degree certificate may be rescinded, at the discretion of the Year 6 Sub Board of Examiners, for candidates who have received one or more fitness to practise forms Award of Merit will be awarded to approximately the top quintile of the cohort based on the overall outcomes of the assessments in Year 6 will be restricted to scores obtained at the first sitting will be recorded on the Medical School academic transcript may be rescinded, at the discretion of the Year 6 Sub Board of Examiners, for candidates who have received one or more fitness to practise forms 10. The Sub Board will determine recommendations for the awards of Medical School prizes in accordance with the regulations for each award. 11. In accordance with the MBBS regulations:, A candidate who is found, after examination entry has been confirmed, to have submitted an incomplete portfolio, or who fails to submit post-examination requirements, will not be awarded the degrees of M.B.,B.S. until all requirements are fulfilled. Candidates who fail are required to present themselves for re-examination at the next possible occasion. Candidates who fail to qualify on completion of Year 6 may present themselves for re-examination in the following academic session after completing a minimum period of 5 months’ clinical study. In exceptional circumstances, candidates who fail after a repeat period of study may be permitted to make one further attempt, at the discretion of the Faculty Tutor (Medical Sciences), providing that this additional, discretionary attempt is within 12 months of completing the M.B.,B.S. programme of study. Candidates must have qualified within 12 months of completing the M.B.,B.S. programme of study. Final Mark Sheets 12. Results should are recorded on the final mark sheet as: PPass FFail DDistinction MCertificate of Merit X Result not yet available (includes, for example, plagiarism or exam irregularity where the result of a hearing is awaited. This mark should be amended when agreed on the mark sheet and in MSSR to the appropriate result) ABSAbsent WDWithdrawn 13. Notification of results is emailed to each candidate and to their personal tutor and a copy is filed on the student record. The notification of results sheet includes: Written assessment pass mark Candidate written assessment mark Clinical assessment pass mark Candidate clinical assessment mark Long and Short Station OSCE pass marksCandidate Long and Short station OSCE marks Number of Fitness to Practice reports issued Result Distinction/Merit/Pass/Fail Awards of Merit and Distinction Years 1 and 2 (Medical Sciences) Certificates of Merit in Year 1 132 will be awarded on the basis of the overall outcomes of the assessments for Year 1 will be awarded to approximately the top quintile of the cohort will be restricted to candidates who have passed all components of the examination will be restricted to scores obtained at the first sitting will be determined at the end of Year 1 by the Year 1Sub Board of Examiners will be recorded on the Medical School academic transcript Certificates of Merit in Year 2 will be awarded on the basis of the overall outcomes of the assessments for Year 2 will be awarded to approximately the top quintile of the cohort will be restricted to candidates who have passed all components of the examination will be restricted to scores obtained at the first sitting will be determined at the end of Year 2 by the Year 2 Sub Board of Examiners will be recorded on the Medical School academic transcript Distinction in Medical Sciences will be awarded to approximately the top decile of the cohort in Year 2 based on the overall outcomes of the assessments in Year 1 and Year 2 will be restricted to candidates who have passed all components of the examination will be restricted to scores obtained at the first sitting will be determined at the end of Year 2 by the Year 2 Sub Board of Examiners may be rescinded, at the discretion of the Sub Board, for candidates who have received one or more fitness to practise forms will be recorded on the Medical School academic transcript will be recorded on the University MBBS Degree Certificate Years 4 and 5 (Clinical Sciences) Certificates of Merit Year 4 Year 5 will be awarded on the basis of the overall outcomes of the assessments in Year 4 will be awarded to approximately the top quintile of the cohort will be restricted to scores obtained at the first sitting will be determined each year by the Year 4 Sub Board of Examiners may be rescinded, at the discretion of the Sub Board, for candidates who have received one or more fitness to practise forms will be recorded on the Medical School academic transcript will be awarded on the basis of the overall outcomes of the assessments in Year 5 will be awarded to approximately the top quintile of the cohort will be restricted to scores obtained at the first sitting will be determined each year by the Year 5 Sub Board of Examiners may be rescinded, at the discretion of the Sub Board, for candidates who have received one or more fitness to practise forms will be recorded on the Medical School academic transcript Distinction in Clinical Science will be awarded to approximately the top decile of the cohort will be awarded on the basis of the overall outcomes of the Year 4 and Year 5 assessments using a ratio of 60:40 in favour of Year 4 scores will be determined by the Year 5 Sub Board of Examiners may be rescinded, at the discretion of the Sub Board, for candidates who have received one or more fitness to practise forms will be recorded on the Medical School academic transcript will be recorded on the University MBBS Degree Certificate Year 6 (Clinical Practice) 133 Certificates of Merit will be awarded on the basis of the overall outcomes of the assessments in Year 6 will be awarded to approximately the top quintile of the cohort will be restricted to scores obtained at the first sitting will be determined by the Year 6 Sub Board of Examiners may be rescinded, at the discretion of the Sub Board, for candidates who have received one or more fitness to practise forms will be recorded on the Medical School academic transcript Distinction in Clinical Practice will be awarded on the basis of the overall outcomes of the assessments in Year 6 will be awarded to approximately the top decile of the cohort will be restricted to scores obtained at the first sitting will be determined by the Year 6 Sub Board of Examiners may be rescinded, at the discretion of the Sub Board, for candidates who have received one or more fitness to practise forms will be recorded on Medical School academic transcript will be recorded on the University MBBS degree transcript is not affected by performance in Student Selected Components, nor by performance in Years 1-6 of the programme. University of London Gold Medal Nominations for University of London Gold Medal vivas are determined by the Year 5 Panel of Examiners. To be eligible, candidates must have achieved a Distinction in Clinical Practice. The ratio of candidates from each school is 1:75. The examination takes the form of a viva conducted by a board of 6 examiners acting in pairs. Each candidate spends 10 minutes at each of the 3 tables and is interviewed for 5 minutes by each Examiner, so the overall examination of each candidate lasts for 30 minutes. The subjects represented are: Pathological Sciences, Medicine, Surgery, Use of Medicines and Therapeutics, Obstetrics and Gynaecology and Paediatrics. The criteria to be examined are: knowledge; clinical context and therapeutic relevance and evidence-base; social and community context and relevance; recent advances; judgement and reasoning. The Gold Medal winner is also awarded a prize of £500. The runner-up is awarded the Betuel Prize and £200. Candidates taking finals under UCL regulations who are nominated for and attend the vivas are issued a certificate stating “Proxime Accessit” to the Gold Medal. Candidates taking finals under the regulations of the University of London who are nominated for and attend the vivas are recorded as “Proxime Accessit to the Gold Medal” on University of London degree certificates. 134 135